Abstract
Objectives
To investigate arterial spin-labelling (ASL) cerebral blood flow (CBF) changes in predementia stages of Alzheimer’s disease (AD).
Methods
Data were obtained from 177 patients with subjective complaints, mild cognitive impairment and AD from the Amsterdam Dementia Cohort. AD stages were based on diagnosis and cerebrospinal fluid biomarkers amyloid-β (Aβ) and total-tau (tau). General-linear-models were used to assess relationships between AD stages and total and regional CBF, correcting for age and sex.
Results
Decreasing CBF was related to more advanced AD stages in all supratentorial regions (p for trend < 0.05). Post-hoc testing revealed that CBF was lower in AD compared to controls and stage-1 predementia patients (i.e. abnormal Aβ and normal tau) in temporal and parietal regions, and compared to stage-2 predementia patients (i.e. abnormal Aβ and tau) in temporal regions. CBF values of stage-2 predementia patients were numerically in between those of stage-1 predementia patients and AD.
Conclusion
The continuing decrease of CBF along the continuum of AD indicates the potential of ASL-CBF as a measure for disease progression.
Key Points
• Decreasing CBF relates to more advanced AD stages in all supratentorial regions.
• The reduction of CBF does not reach a bottom level.
• ASL-CBF has potential as a measure for disease progression in AD.
Keywords: Arterial spin-labelling MRI, Cerebral blood flow/cerebral perfusion, Alzheimer’s disease, Prodromal AD, Disease progression
Introduction
The first pathological signs of Alzheimer’s disease (AD), in the form of amyloid-β1-42 (Aβ) plaque deposition, can be detected up to decades before clinical symptoms first occur [1]. However, these very early pathological signs of AD do not correlate with disease progression in clinical AD [2]. Neuronal and synaptic function measures, such as CSF total-tau (tau) and 18F-fluorodeoxyglucose positron emission tomography (FDG-PET), are thought to start changing later on in the disease process. Moreover, they are thought to relate to cognitive performance, and to continue to change along the disease process, which might make them more suitable for monitoring disease progression [2–4].
Arterial spin-labelling (ASL) is a functional magnetic resonance imaging (MRI) technique that measures cerebral blood flow (CBF) by using magnetically labelled arterial blood that flows through the carotid and vertebral arteries as an endogenous contrast medium. Important advantages of ASL are its non-invasiveness and short acquisition time at higher magnetic field strengths, which allows routine clinical application in the workup of dementia when ASL is added to the standard dementia imaging protocol.
Recently, new diagnostic and scientific criteria for clinical AD and its predementia stages have been introduced by the National Institute on Aging and the Alzheimer’s Association (NIA-AA) [5–7]. For scientific purposes, these criteria offer the possibility of subdividing subjects with normal cognition, such as patients with subjective complaints (SC), and patients with mild cognitive impairment (MCI) into different predementia AD stages using Aβ and neuronal injury biomarkers.
In a previous study we showed that ASL discriminated AD patients from controls, and that regional CBF values of MCI patients were numerically in between those of controls and AD patients [8]. In the current study we aimed to further investigate CBF along the course of AD, by studying CBF of patients in different predementia stages, based on the NIA-AA criteria [5–7].
Methods
Subjects
In this cross-sectional study we included 275 patients (107 AD patients, 64 MCI patients and 104 SC patients) from the memory clinic-based Amsterdam Dementia Cohort. All patients visited our memory clinic between October 2010 and June 2012, underwent brain MRI according to the dementia protocol described below, and had cerebrospinal fluid (CSF) available for analysis of CSF biomarkers. All patients underwent a standard dementia screening that included medical history, physical and neurological examinations, screening laboratory tests, lumbar puncture, neuropsychological testing and brain MRI. Clinical diagnosis was established by consensus in a multidisciplinary team. AD patients met the NINCDS-ADRDA criteria for probable AD [9], and also met the core clinical criteria for probable AD proposed by the NIA-AA workgroup [6]. MCI patients fulfilled the Petersen criteria [10, 11]. Patients were considered to have subjective complaints when clinical investigations and neuropsychological test performance were normal. Patients with a history of head trauma or intracranial tumours were excluded. The local Institutional Review Board approved the study. All patients provided written informed consent.
MRI acquisition
MRI examinations were performed on a 3T whole body MR system (SignaHDxt, GE Medical Systems Milwaukee, WI, USA) using an 8-channel head coil. Structural images included a sagittal 3D T1-weighted sequence (IR-FSPGR, echo time=3.0ms, repetition time=7.8ms, inversion time=450ms, flip angle=12°, matrix 256×256, 176 slices, voxel size 1×0.9×0.9mm) for anatomical information, and a sagittal 3D fluid attenuated inversion recovery (FLAIR) sequence (CUBE, echo time=123.6 ms, repetition time=8000 ms, inversion time=2351 ms, echo-train length=230, acquisition matrix 224x224, reconstruction matrix 256×256, 132 slices, voxel size 1.2×1×1mm) to determine the severity of white matter hyperintensities (WMH) using the Fazekas scale [12]. Pseudo-continuous ASL (PCASL) [13, 14] perfusion images (3D-FSE acquisition with background suppression, post-label delay 2.0s, echo time=9 ms, repetition time=4.8 s, spiral readout eight arms × 512 samples; 36×5.0mm axial slices, 3.2×3.2mm in-plane resolution, reconstructed pixel size 1.7×1.7mm, acquisition time 4 min) were calculated using a single-compartment model [15] after the subtraction of labelled from control images. More details are provided in an earlier study by Binnewijzend et al. [8].
Pre-processing and MRI data analysis
Both T1-weighted and PCASL images were corrected for gradient non-linearities in all three directions. Further data analyses were carried out using FSL (version 4.1; http://www.fmrib.ox.ac.uk/fsl). Pre-processing of T1 images consisted of non-brain tissue removal [16], linear registration to standard space [17] and tissue segmentation [18] yielding partial volume estimates. Gray matter volumes, normalized for subject head size (NGMV), were calculated with the SIENAX software tool [16]. The CBF maps [8] were linearly registered to the brain-extracted T1 images. The brain mask was used to calculate uncorrected mean whole brain CBF. Partial volume estimates were transformed to the ASL data space and used in a regression algorithm [19], using a Gaussian kernel of 9.5-mm full width at half maximum, to create partial volume corrected (PVC) cortical CBF maps. Partial volume estimates were subsequently used as a weighting factor to calculate mean cortical CBF. The MNI152 atlas and the Harvard-Oxford cortical atlas (both part of FSL) were used to create regions of interest (ROIs) of the frontal, temporal, parietal, precuneus and posterior cingulate (PPC), occipital and cerebellar brain areas, to extract mean regional uncorrected and PVC cortical CBF values.
CSF analysis
CSF was obtained by lumbar puncture of the L3/L4 or L4/L5 intervertebral space, using a 25-gauge needle, and collected via a syringe in 12-ml polypropylene tubes (Sarstedt). A small amount of CSF was used for routine analysis, including total cells (leucocytes and erythrocytes), total protein and glucose. Within 2 hours, CSF samples were centrifuged at 2100 × g for 10 min at 4°C and the supernatant was transferred into a second polyprolylene tube (Sarstedt) and stored at −20°C until AD biomarker analysis. CSF amyloid-β1-42 and total-tau were measured with Innotest (Innogenetics) sandwich enzyme-linked immunosorbent assay as described previously [20]. The team involved in the CSF analysis was not aware of the clinical diagnosis.
Definition of AD stages
Patients were divided into AD stages based on the combination of both syndrome diagnosis and CSF biomarker values, considering Aβ below 550 ng/L, and tau above 375 ng/L as abnormal (i.e. positive) [20]. For AD, only patients with a high likelihood of having an AD pathophysiology were included. AD patients with normal Aβ and/or tau values (n= 41) were excluded. For predementia stages, we collapsed MCI and preclinical stages to overall predementia AD stages to ensure sufficient power. Only patients fitting in the biomarker stages were included. Therefore, MCI patients with normal Aβ values (n=42) and SC patients with normal Aβ and abnormal tau values (n=13) were excluded.
Subsequently, MR images of all patients were visually inspected. One AD patient was excluded because registration of the ASL images to T1 images failed, possibly due to sub-optimal quality of the ASL images. One other AD patient was excluded because of haemochromatosis.
This resulted in the following four study groups: 80 SC patients with normal CSF Aβ and tau (controls, stage 0), 13 predementia patients (six SC, seven MCI) with abnormal CSF Aβ and normal CSF tau (stage 1), 20 predementia patients (five SC, 15 MCI) with abnormal CSF Aβ and tau (stage 2) and 64 clinically demented AD patients with abnormal CSF Aβ and tau (stage 3).
Statistics
Statistical analyses were performed using IBM SPSS Statistics for Mac (Version 19.0., IBM Corp., Armonk, NY, USA). For continuous measures, differences between groups were assessed using one-way analyses of variance (ANOVA) with post-hoc Bonferroni tests to correct for multiple comparisons. A chi-squared test was used to compare frequency distributions of sex in all study groups, and syndrome diagnosis (i.e. SC or MCI) in the predementia groups. General linear models (GLMs) were used to assess the relationships between AD stages (entered as continuous measure to assess the dose-response effect) and total and regional uncorrected and PVC cortical CBF, correcting for the effect of age and sex. Post-hoc, univariate GLMs (total CBF) and multivariate GLMs (regional CBF) with Bonferroni tests were performed to compare CBF values of different AD stages, correcting for the effect of age and sex (model 1), and additionally for WMH (model 2). Linear regression analyses were performed across groups and within the study groups to assess relationships between CBF (independent variable) and cognition, using MMSE-scores (dependent variable). Age and sex, and additionally WMH, were entered into the model as covariates.
Results
Demographics, MRI findings and CSF results are presented in Table 1. Stage-2 predementia patients and stage-3 AD dementia patients were older than controls. Patients with AD dementia had lower MMSE-scores compared to all the other groups. Stage-2 predementia patients and AD dementia patients had more WMH than controls. NGMV was lower in AD dementia patients compared to controls and stage-1 predementia patients, and NGMV was lower in stage-2 predementia patients compared to controls. Finally, by definition, CSF Aβ was lower in all groups compared to controls, and CSF tau was higher in AD dementia patients and stage-2 predementia patients compared to controls and stage-1 predementia patients.
Table 1.
Patient characteristics, magnetic resonance imaging (MRI) findings and cerebrospinal fluid (CSF) data
| Control | Predementia | AD | ||
|---|---|---|---|---|
| Stage 0 | Stage 1 | Stage 2 | Stage 3 | |
| Number | 80 | 13 | 20 | 64 |
| Age (y)a | 58±9 | 64±7 | 66±5* | 66±7* |
| Females, no. (%) | 31 (39) | 5 (39) | 9 (45) | 34 (53) |
| Diagnosis (MCI), no. (%) | - | 7 (54) | 15 (75) | - |
| MMSEa,b | 28±2 | 28±2 | 26±2 | 21±4*,¥,§ |
| WMHa | 0.6±0.7 | 1.2±0.9 | 1.2±0.8* | 1.1±0.8* |
| NGMV (mL)a | 780±53 | 770±55 | 733±63* | 711±46*,¥ |
| CSF Aβ1-42(ng/L)a | 986±188 | 444±89* | 442±70* | 459±68* |
| CSF tau (ng/L)a | 220±73 | 292±75 | 782±370*,¥ | 796±340*,¥ |
a Data are given as mean ± standard deviation
bMini Mental State Examination (MMSE) scores of two controls were excluded because they were obtained by means of an interpreter
Stage 0: Aβ-/tau- patients with subjective complaints (SC), Stage 1: Aβ+/tau- patients with SC and mild cognitive impairment (MCI), Stage 2: Aβ+/tau+ patients with SC and MCI, Stage 3: Aβ+/tau+ patients with AD
*p<0.05 compared to controls, ¥ p<0.05 compared to stage-1 predementia patients, § p<0.05 compared to stage-2 predementia patients
AD Alzheimer’s disease, WMH white matter hyperintensities (based on Fazekas-score), NGMV normalized grey matter volume
Total CBF differences
With increasing AD stage, both uncorrected whole brain and PVC cortical CBF decreased (p for trend < 0.01) (Table 2). Post-hoc tests showed that AD dementia patients had lower uncorrected whole brain CBF compared to controls and stage-1 predementia patients, and lower PVC cortical CBF compared to controls. There were no differences in CBF between predementia patients and controls. Additional correction for WMH did not change the group differences.
Table 2.
Region-of-interest based cerebral blood flow (CBF) values
| Control | Predementia | AD | ||
|---|---|---|---|---|
| Stage 0 | Stage 1 | Stage 2 | Stage 3 | |
| Uncorrected whole brain CBF*** | 32±5 | 32±5 | 30±5 | 28±5a,b |
| PVC cortical CBF** | 48±8 | 48±7 | 45±8 | 43±8a |
| Regional uncorrected cortical CBF | ||||
| Frontal* | 22±5 | 21±5 | 20±4 | 19±4 |
| Temporal*** | 26±5 | 26±5 | 24±4 | 21±4a,b,c |
| Parietal*** | 29±5 | 28±5 | 26±5 | 24±5a,d |
| PPC*** | 38±7 | 37±7 | 34±6 | 31±6a,b |
| Occipital*** | 35±7 | 34±6 | 32±7 | 29±7a,d |
| Cerebellum | 26±5 | 26±6 | 25±6 | 25±5 |
| Regional PVC cortical CBF | ||||
| Frontal* | 49±9 | 49±8 | 47±9 | 43±9 |
| Temporal** | 44±7 | 44±6 | 42±8 | 39±7a,d |
| Parietal*** | 55±9 | 55±9 | 51±10 | 47±10a,d |
| PPC*** | 63±11 | 62±10 | 58±11 | 55±11a,d |
| Occipital** | 55±9 | 54±9 | 51±12 | 49±10a |
| Cerebellum | 40±9 | 41±0 | 36±8 | 38±10 |
Results are given as mean ± standard deviation. If analysis of variance was p<0.05 a post-hoc Bonferroni test was performed. Shown results are corrected for age and sex
*p<0.05, **p<0.01 and ***p<0.001
a p <0.05 compared to controls
b p<0.05 compared to stage-1 predementia patients
c p<0.05 compared to stage-2 predementia patients
d p<0.1 compared to stage-1 predementia patients
Stage 0: Aβ-/tau- patients with subjective complaints (SC), Stage 1: Aβ+/tau- patients with SC and mild cognitive impairment (MCI), Stage 2: Aβ+/tau+ patients with SC and MCI, Stage 3: Aβ+/tau+ patients with AD
AD Alzheimer’s disease, PPC precuneus and posterior cingulated, PVC partial volume corrected
Differences in regional CBF patterns
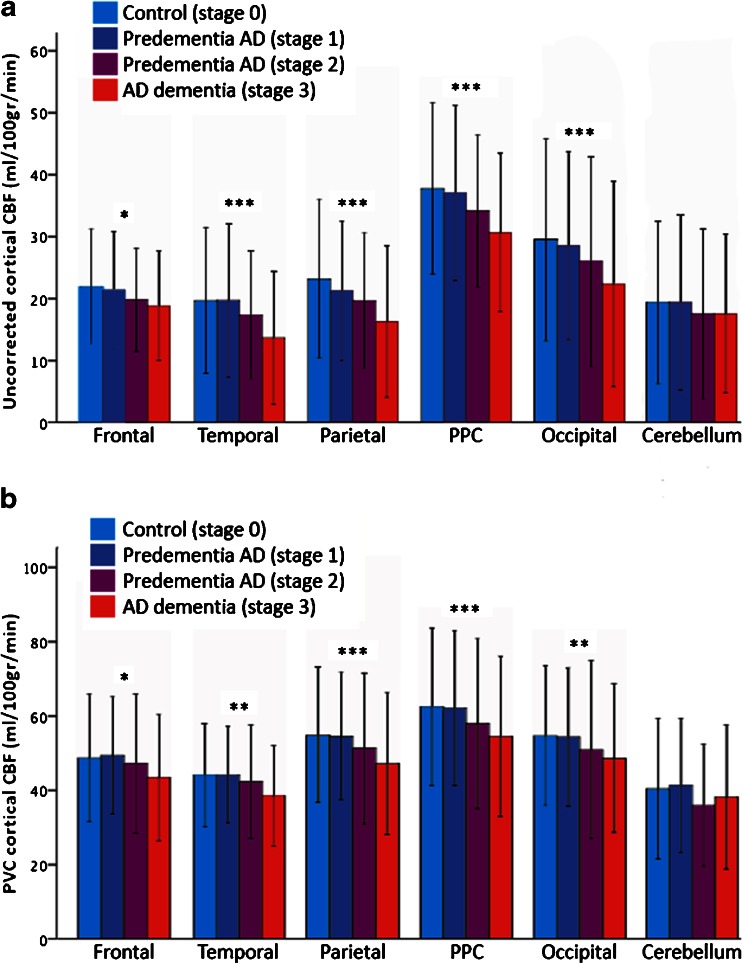
As expected, regional PVC cortical CBF values were much higher than regional uncorrected cortical CBF values, as the latter also contains cerebrospinal fluid and maybe even some edges of white matter (Table 2). A more advanced AD stage was related to lower regional CBF in all regions except the cerebellum. Relationships were most prominent in the temporal, parietal, PPC and occipital regions for uncorrected cortical CBF, and in the parietal and PPC regions for PVC cortical CBF (p for trend < 0.001; Fig. 1). Post-hoc, uncorrected cortical and PVC cortical CBF were lower in temporal, parietal, PPC and occipital regions in AD dementia patients compared to controls (Table 2). Furthermore, uncorrected cortical CBF was lower in AD dementia patients compared to stage-1 predementia patients in the temporal, parietal (trend), PPC and occipital (trend) regions, and compared to stage-2 predementia patients in the temporal lobes. AD dementia patients showed a trend towards lower PVC cortical CBF values compared to stage-1 predementia patients in the temporal, parietal, PPC and occipital regions. No between-group CBF differences were found in the frontal lobes and the cerebellum, and there were no CBF differences between stage-2 predementia patients, stage-1 predementia patients and controls. Additional correction for WMH did not change the group differences.
Fig. 1.
Lower regional cerebral blood flow (CBF) is associated with advancing Alzheimer’s disease (AD) stage. Bar graphs display mean regional uncorrected CBF (a) and mean partial volume corrected (PVC) cortical CBF (b) for the different AD stages, per brain region. Error bars represent standard deviations (±2SD). Dose-response relationships between CBF and AD stage were detected using general-linear models (AD stage entered as a continuous measure), resulting in a p for trend < 0.05 in all brain regions except the cerebellum. The most prominent relationships between decreasing CBF and advancing AD stage were found in the posterior supratentorial brain regions (p for trend < 0.001). PPC precuneus and posterior cingulate cortex. *p for trend < 0.05, **p for trend < 0.01, ***p for trend < 0.001
Relationship between CBF and cognition
Across groups, uncorrected whole brain CBF and PVC cortical CBF were related to cognitive performance in all brain regions, except the cerebellum (Table 3). When we investigated correlations within each stage separately, in AD dementia patients this relationship was seen in the temporal and parietal regions (uncorrected cortical and PVC cortical CBF; trends), and in the frontal lobes (PVC cortical CBF; trend). Stage-2 predementia patients showed a relationship between uncorrected CBF and cognition in the occipital lobes (trend). After additional adjustment for WMH (model 2), the essence of the results remained unchanged, with the addition that in stage-1 predementia patients a relationship between cognitive performance and uncorrected CBF in the occipital lobes reached significance (standardized beta 0.70, p<0.05).
Table 3.
Relationship between cerebral blood flow (CBF) and cognition (Mini-Mental State Examination scores)
| Across groups | Control | Predementia | AD | ||
|---|---|---|---|---|---|
| Stage 0 | Stage 1 | Stage 2 | Stage 3 | ||
| Uncorrected whole brain CBF | 0.33** | −0.01 | 0.22 | −0.20 | 0.21+ |
| PVC cortical CBF | 0.27** | −0.02 | 0.30 | −0.21 | 0.19 |
| Regional uncorrected cortical CBF | |||||
| Frontal | 0.23* | −0.06 | −0.03 | 0.05 | 0.18 |
| Temporal | 0.38** | 0.02 | 0.22 | −0.03 | 0.21+ |
| Parietal | 0.40 | −0.01 | 0.22 | 0.16 | 0.24+ |
| PPC | 0.40** | 0.03 | 0.28 | −0.17 | 0.17 |
| Occipital | 0.34** | 0.12 | 0.25§ | −0.35+ | 0.18 |
| Cerebellum | 0.09 | −0.05 | 0.24 | −0.30 | −0.04 |
| Regional PVC cortical CBF | |||||
| Frontal | 0.24* | −0.07 | 0.18 | −0.21 | 0.23+ |
| Temporal | 0.31** | −0.02 | 0.26 | −0.13 | 0.22+ |
| Parietal | 0.32** | −0.02 | 0.41 | −0.18 | 0.21+ |
| PPC | 0.29** | 0.01 | 0.46 | −0.28 | 0.16 |
| Occipital | 0.23* | 0.04 | 0.44 | −0.30 | 0.11 |
| Cerebellum | 0.08 | −0.04 | 0.13 | −0.05 | 0.02 |
*p<0.01, **p<0.001, +p<0.1; adjustment for age and sex (model 1)
§A relationship between cognition and uncorrected CBF in the occipital lobes (standardized beta 0.70; p<0.05) was detected after additional adjustment for white matter hyperintensities (Fazekas-scores; model 2)
Stage 0: Aβ-/tau- patients with subjective complaints (SC), Stage 1: Aβ+/tau- patients with SC and mild cognitive impairment (MCI), Stage 2: Aβ+/tau+ patients with SC and MCI, Stage 3: Aβ+/tau+ patients with AD
AD Alzheimer’s disease, PPC precuneus and posterior cingulated, PVC partial volume corrected
Discussion
The main finding of this study was that lower CBF was observed with more advancing stages of AD across the spectrum from normal cognition to AD dementia. Furthermore, CBF was related to cognitive performance across AD stages and within the stage-3 AD group.
To date, several ASL studies have detected CBF decreases in AD, most prominently in the bilateral parietal cortex and the precuneus and posterior cingulate cortex [8, 21, 22]. Based on the currently widely supported suggestion that neuronal dysfunction occurs prior to the stage of clinical AD, the aim of this study was to investigate ASL-measured CBF of Aβ positive non-demented patients in different disease stages [5, 7]. This resulted in the finding that, compared to Aβ and tau negative controls, ASL-CBF was decreased in AD dementia patients, but not in predementia AD patients. Temporo-parietal CBF was lower in AD dementia patients than in stage-1 predementia patients, in particular for uncorrected cortical CBF, but to a lesser extent also for PVC cortical CBF. Stage-2 predementia patients showed no decreased CBF compared to controls, but their CBF did not differ from AD dementia patients either. In fact, quantitative CBF values of stage-2 predementia patients were numerically in between the CBF values of stage-1 predementia patients and stage-3 AD dementia patients. These findings are in accordance with the idea that CBF alterations, as a sign of neuronal dysfunction, occur further along the disease process than the accumulation of Aβ, but before the stage of clinical dementia.
This is the first study comparing ASL-measured CBF of predementia AD stages with study groups based on CSF biomarker profiles [5–7]. Previous ASL studies investigating cerebral perfusion in MCI detected parietal and medial temporal hypoperfusion in a less prominent and widespread pattern than the hypoperfusion found in AD compared to controls [8, 21–26]. However, none of these studies reported amyloid status of the MCI patients. This leaves room for the possibility that other CBF-decreasing non-AD pathology caused regional CBF changes in MCI, such as DLB, which has previously been shown to also be related to severe CBF decreases [27, 28]. In our study, we therefore used biomarkers to define our study groups, allowing us to examine changes in CBF across the entire spectrum of AD.
In the current hypothetical biomarker models for AD, FDG-PET is considered the main functional neuroimaging tool to assess neuronal injury in terms of hypometabolism in AD [3, 4, 29]. Since glucose metabolism and perfusion are closely related, ASL is a potential alternative for the visualization of cerebral and neuronal function [30–32]. However, the relationship between perfusion and metabolism has not yet been thoroughly investigated in the predementia stages of AD. One PET study by Drzezga et al. [33] found lower regional glucose metabolism in Aβ-positive healthy controls compared to Aβ-negative controls, suggesting a relationship between Aβ and glucose metabolism. This is not consistent with our finding that ASL-measured CBF did not change with the presence of amyloid pathology in a very early stage of AD. Direct comparisons of FDG-PET measured glucose metabolism and ASL-measured cerebral perfusion in predementia AD are needed to clarify whether glucose metabolism and cerebral perfusion are directly related or consecutive processes.
In a previous study we showed that cognitive performance was related to ASL-measured CBF in AD [8]. In the current study we also found this relationship within the AD dementia group, albeit in fewer regions and less strong. This discrepancy may be due to the fact that in the current study, AD patients were selected based on CSF biomarkers in addition to clinical diagnosis, possibly causing less variability in both cognition and CBF within the AD dementia group compared to our previous study, in which the AD population also contained subjects with normal or borderline normal CSF Aβ and tau values. Besides a trend towards a significant relationship between occipital CBF and cognition in the stage-2 predementia group (in the unexpected direction), no relationships between CBF and cognition were found in the Aβ positive predementia groups. However, it is not inconceivable that a lack of power contributed to this negative result. After adjustment for WMH, a relationship between uncorrected CBF in the occipital lobes and cognition did appear within the stage-1 predementia group.
This study has several strengths and limitations. First, the study groups were selected based on both clinical diagnosis and CSF biomarkers. This limited our sample sizes, but at the same time resulted in quite homogeneous study groups, strongly reducing the effect of perfusion changes caused by for example neurodegeneration of non-AD origin. Since the criteria for clinical stages in preclinical and prodromal AD show strong similarities, and implementing all stages in a sequential manner is not easily done, we chose to reduce the number of study groups by combining preclinical and prodromal patient groups with identical biomarker profiles. A quantitative 3D pseudo-continuous ASL sequence with whole-brain coverage was used to study CBF. Furthermore, both CBF without correction for partial volume effects (representative for clinical practice) and PVC cortical CBF (actual gray matter CBF) were studied. The inclusion of subjects with subjective complaints instead of healthy controls might be considered a limitation. However, controls were only included if they had normal biomarkers, strongly decreasing the likelihood that they would have preclinical AD. Additional potential limitations related to image technique include the fact that ASL scan quality could not be assured completely. Although the perfusion images were visually of good quality, the labelling efficiency was not assessed formally. Furthermore, we did not scan with several delay times to account for differences in travel times between groups. However, in line with recently published recommendations [14], a delay time of 2.0 s (instead of 1.5 s) was used to alleviate the effect of delayed blood arrival in the brain in our study groups [34].
In conclusion, we found lower CBF with advancing NIA-AA-based stages of AD. Aβ-positive predementia patients with normal CSF tau levels showed no reduction in ASL-measured CBF, endorsing the idea that CBF changes are not directly related to Aβ deposition. Furthermore, the continuing decrease along the continuum of AD shows that the reduction of CBF does not reach a bottom level, but is associated with decline severity, suggesting that ASL-measured CBF may be used as a measure for disease progression.
Acknowledgments
The authors thank Ajit Shankaranarayanan of GE Healthcare for providing the 3D pseudo-continuous ASL sequence that was used to obtain data for this paper.
The scientific guarantor of this publication is Frederik Barkhof. The authors of this manuscript declare relationships with the following companies: M.A.A. Binnewijzend, M.R. Benedictus J.P.A. Kuijer and W.M. van der Flier report no disclosures. C.E. Teunissen serves on the advisory board of Innogenetics and Roche. She has received speaker honorarium on a symposium organised by Teva. N.D. Prins serves on the advisory board of Boehringer Ingelheim and Envivo. He has been a speaker at symposia organised by Janssen and Novartis. NDP has a senior fellowship at the Alzheimer Center of the VU University Medical Center Amsterdam, partly supported by Vereniging AEGON and receives research support from the Brain Foundation of The Netherlands and Alzheimer Nederland. NDP receives no personal compensation for the activities mentioned above. M.P. Wattjes serves as a consultant for Biogen-Idec. Dr. Wattjes receives research support from Biogen Idec, Bayer Healthcare, Roche and Janssen Cilag. Dr. Wattjes serves as an editorial board member of European Radiology. B.N.M. van Berckel receives research support from the Alzheimer Assistance Foundation, the Center for Translational Molecular Imaging, the Alzheimer Association, De Hersenstichting Nederland and the Internationale Stichting Alzheimer Onderzoek. Dr. van Berckel receives no personal compensation from these organizations. P. Scheltens receives grant support (for the institution; the Alzheimer Center of the VU University Medical Center Amsterdam, see also below) from GE Healthcare, Danone Research and MERCK. In the past 2 years he has received speaker's fees (paid to the institution) from Lilly, GE Healthcare, Lundbeck, Danone and Jansen AI-Pfizer. He is co-editor-in-chief of Alzheimer Research &Therapy. F. Barkhof serves on the editorial boards of Brain, European Radiology, Radiology, Multiple Sclerosis and Neuroradiology and serves as a consultant for Bayer-Schering Pharma, Sanofi-Aventis, Biogen-Idec, TEVA, Synthon BV, Merck-Serono, Jansen Research, Novartis and Roche. Dr. Barkhof receives research support from the Dutch MS Society (EU-FP7). Dr. Barkhof has received consulting fees or honoraria for the consultancy mentioned above. Dr. Barkhof has received speaker's fees from the Serono Symposia Foundation.
The study was supported by the Alzheimer Center of the VU University Medical Center Amsterdam, The Netherlands. Research from the Alzheimer Center of the VU University Medical Center Amsterdam is part of the neurodegeneration research programme of the Neuroscience Campus Amsterdam. The Alzheimer Center of the VU University Medical Center Amsterdam is supported by Alzheimer Nederland and Stichting VUmc funds. The clinical database structure was developed with funding from Stichting Dioraphte.
One of the authors has significant statistical expertise (WM van der Flier). Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Some study subjects or cohorts have been previously reported in:
a) Binnewijzend MA, Kuijer JP, Benedictus MR, van der Flier WM, Wink AM, Wattjes MP et al. Cerebral blood flow measured with 3D pseudocontinuous arterial spin-labeling mr imaging in alzheimer disease and mild cognitive impairment: a marker for disease severity. Radiology 2013;267:221-30.
b) Binnewijzend MA, Kuijer JP, van der Flier WM, Benedictus MR, Moller CM, Pijnenburg YA et al. Distinct perfusion patterns in Alzheimer's disease, frontotemporal dementia and dementia with Lewy bodies. Eur Radiol 2014;24:2326-33.
Methodology: retrospective, cross-sectional study, performed at one institution.
Abbreviations
- Aβ
Amyloid beta
- NGMV
Normalized grey matter volume
- PCASL
Pseudo-continuous aterial spin-labelling
- PPC
Precuneus and posterior cingulated
- PVC
Partial volume corrected
- P-tau
Phosphorylated-tau
- SC
Subjective complaints
- T-tau
Total-tau
- WMH
White matter hyperintensities
References
- 1.Jack CR, Jr, Lowe VJ, Weigand SD, Wiste HJ, Senjem ML, Knopman DS, et al. Serial PIB and MRI in normal, mild cognitive impairment and Alzheimer's disease: implications for sequence of pathological events in Alzheimer's disease. Brain. 2009;132:1355–1365. doi: 10.1093/brain/awp062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jagust WJ, Landau SM, Shaw LM, Trojanowski JQ, Koeppe RA, Reiman EM, et al. Relationships between biomarkers in aging and dementia. Neurology. 2009;73:1193–1199. doi: 10.1212/WNL.0b013e3181bc010c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jack CR, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, et al. Hypothetical model of dynamic biomarkers of the Alzheimer's pathological cascade. Lancet Neurol. 2010;9:119–128. doi: 10.1016/S1474-4422(09)70299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jack CR, Jr, Knopman DS, Jagust WJ, Petersen RC, Weiner MW, Aisen PS, et al. Tracking pathophysiological processes in Alzheimer's disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207–216. doi: 10.1016/S1474-4422(12)70291-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:270–279. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, et al. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:280–292. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Binnewijzend MA, Kuijer JP, Benedictus MR, van der Flier WM, Wink AM, Wattjes MP, et al. Cerebral blood flow measured with 3D pseudocontinuous arterial spin-labeling MR imaging in Alzheimer disease and mild cognitive impairment: a marker for disease severity. Radiology. 2013;267:221–230. doi: 10.1148/radiol.12120928. [DOI] [PubMed] [Google Scholar]
- 9.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–944. doi: 10.1212/WNL.34.7.939. [DOI] [PubMed] [Google Scholar]
- 10.Petersen RC, Stevens JC, Ganguli M, Tangalos EG, Cummings JL, DeKosky ST. Practice parameter: early detection of dementia: mild cognitive impairment (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1133–1142. doi: 10.1212/WNL.56.9.1133. [DOI] [PubMed] [Google Scholar]
- 11.Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256:183–194. doi: 10.1111/j.1365-2796.2004.01388.x. [DOI] [PubMed] [Google Scholar]
- 12.Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer's dementia and normal aging. AJR Am J Roentgenol. 1987;149:351–356. doi: 10.2214/ajr.149.2.351. [DOI] [PubMed] [Google Scholar]
- 13.Dai W, Garcia D, de BC, Alsop DC. Continuous flow-driven inversion for arterial spin labeling using pulsed radio frequency and gradient fields. Magn Reson Med. 2008;60:1488–1497. doi: 10.1002/mrm.21790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alsop DC, Detre JA, Golay X, Gunther M, Hendrikse J, Hernandez-Garcia L, et al. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med. 2014 doi: 10.1002/mrm.25197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buxton RB, Frank LR, Wong EC, Siewert B, Warach S, Edelman RR. A general kinetic model for quantitative perfusion imaging with arterial spin labeling. Magn Reson Med. 1998;40:383–396. doi: 10.1002/mrm.1910400308. [DOI] [PubMed] [Google Scholar]
- 16.Smith SM. Fast robust automated brain extraction. Hum Brain Mapp. 2002;17:143–155. doi: 10.1002/hbm.10062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jenkinson M, Smith S. A global optimisation method for robust affine registration of brain images. Med Image Anal. 2001;5:143–156. doi: 10.1016/S1361-8415(01)00036-6. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Brady M, Smith S. Segmentation of brain MR images through a hidden Markov random field model and the expectation-maximization algorithm. IEEE Trans Med Imaging. 2001;20:45–57. doi: 10.1109/42.906424. [DOI] [PubMed] [Google Scholar]
- 19.Asllani I, Borogovac A, Brown TR. Regression algorithm correcting for partial volume effects in arterial spin labeling MRI. Magn Reson Med. 2008;60:1362–1371. doi: 10.1002/mrm.21670. [DOI] [PubMed] [Google Scholar]
- 20.Mulder C, Verwey NA, van der Flier WM, Bouwman FH, Kok A, van Elk EJ, et al. Amyloid-beta(1-42), total tau, and phosphorylated tau as cerebrospinal fluid biomarkers for the diagnosis of Alzheimer disease. Clin Chem. 2010;56:248–253. doi: 10.1373/clinchem.2009.130518. [DOI] [PubMed] [Google Scholar]
- 21.Dai W, Lopez OL, Carmichael OT, Becker JT, Kuller LH, Gach HM. Mild cognitive impairment and alzheimer disease: patterns of altered cerebral blood flow at MR imaging. Radiology. 2009;250:856–866. doi: 10.1148/radiol.2503080751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson NA, Jahng GH, Weiner MW, Miller BL, Chui HC, Jagust WJ, et al. Pattern of cerebral hypoperfusion in Alzheimer disease and mild cognitive impairment measured with arterial spin-labeling MR imaging: initial experience. Radiology. 2005;234:851–859. doi: 10.1148/radiol.2343040197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bangen KJ, Restom K, Liu TT, Wierenga CE, Jak AJ, Salmon DP, et al. Assessment of Alzheimer's disease risk with functional magnetic resonance imaging: an arterial spin labeling study. J Alzheimers Dis. 2012;31(Suppl 3):S59–S74. doi: 10.3233/JAD-2012-120292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chao LL, Buckley ST, Kornak J, Schuff N, Madison C, Yaffe K, et al. ASL perfusion MRI predicts cognitive decline and conversion from MCI to dementia. Alzheimer Dis Assoc Disord. 2010;24:19–27. doi: 10.1097/WAD.0b013e3181b4f736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fleisher AS, Podraza KM, Bangen KJ, Taylor C, Sherzai A, Sidhar K, et al. Cerebral perfusion and oxygenation differences in Alzheimer's disease risk. Neurobiol Aging. 2009;30:1737–1748. doi: 10.1016/j.neurobiolaging.2008.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim SM, Kim MJ, Rhee HY, Ryu CW, Kim EJ, Petersen ET, et al. Regional cerebral perfusion in patients with Alzheimer's disease and mild cognitive impairment: effect of APOE epsilon4 allele. Neuroradiology. 2013;55:25–34. doi: 10.1007/s00234-012-1077-x. [DOI] [PubMed] [Google Scholar]
- 27.Binnewijzend MA, Kuijer JP, van der Flier WM, Benedictus MR, Moller CM, Pijnenburg YA, et al. Distinct perfusion patterns in Alzheimer's disease, frontotemporal dementia and dementia with Lewy bodies. Eur Radiol. 2014;24:2326–2333. doi: 10.1007/s00330-014-3172-3. [DOI] [PubMed] [Google Scholar]
- 28.Fong TG, Inouye SK, Dai W, Press DZ, Alsop DC. Association cortex hypoperfusion in mild dementia with Lewy bodies: a potential indicator of cholinergic dysfunction? Brain Imaging Behav. 2011;5:25–35. doi: 10.1007/s11682-010-9108-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frisoni GB, Fox NC, Jack CR, Jr, Scheltens P, Thompson PM. The clinical use of structural MRI in Alzheimer disease. Nat Rev Neurol. 2010;6:67–77. doi: 10.1038/nrneurol.2009.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen Y, Wolk DA, Reddin JS, Korczykowski M, Martinez PM, Musiek ES, et al. Voxel-level comparison of arterial spin-labeled perfusion MRI and FDG-PET in Alzheimer disease. Neurology. 2011;77:1977–1985. doi: 10.1212/WNL.0b013e31823a0ef7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jueptner M, Weiller C. Review: does measurement of regional cerebral blood flow reflect synaptic activity? Implications for PET and fMRI. Neuroimage. 1995;2:148–156. doi: 10.1006/nimg.1995.1017. [DOI] [PubMed] [Google Scholar]
- 32.Musiek ES, Chen Y, Korczykowski M, Saboury B, Martinez PM, Reddin JS, et al. Direct comparison of fluorodeoxyglucose positron emission tomography and arterial spin labeling magnetic resonance imaging in Alzheimer's disease. Alzheimers Dement. 2012;8:51–59. doi: 10.1016/j.jalz.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grimmer T, Faust M, Auer F, Alexopoulos P, Forstl H, Henriksen G, et al. White matter hyperintensities predict amyloid increase in Alzheimer's disease. Neurobiol Aging. 2012;33:2766–2773. doi: 10.1016/j.neurobiolaging.2012.01.016. [DOI] [PubMed] [Google Scholar]
- 34.Campbell AM, Beaulieu C. Pulsed arterial spin labeling parameter optimization for an elderly population. J Magn Reson Imaging. 2006;23:398–403. doi: 10.1002/jmri.20503. [DOI] [PubMed] [Google Scholar]