Abstract
Objective
To investigate the clinical and perioperative characteristics of patients ≥ 75 who undergoing percutaneous coronary intervention (PCI) and to evaluate the risk factors related to short-term post-PCI mortality in this specific patients group.
Methods
1,035 consecutive subjects who underwent PCI from December 2011 to November 2013 were divided into four categories: (1) patients with stable angina (SA) ≥ 75 years (n = 58); (2) patients with SA < 75 years (n = 218); (3) patients with acute coronary syndrome (ACS) ≥ 75 years (n = 155); (4) patients with ACS < 75 years (n = 604). A multivariable logistic regression analysis was conducted to detect risk factors of six-month mortality in patients ≥ 75 years who had undergone PCI. Clinical comorbidities, in-hospital biochemical indicators, perioperative data, in-hospital and six-month outcomes were analyzed and compared among the four groups.
Results
Compared with the younger group, patients ≥ 75 years were more likely to have hypertension, history of stroke, chronic obstructive pulmonary disease, peripheral vascular disease, cardiogenic shock and malignant arrhythmia, and they were admitted to hospital with relative lower weight, hemoglobin, albumin, triglyceride, higher creatinine, uric acid, urea nitrogen and pro-BNP. Left main artery lesions, multi-vessel, calcified lesions, chronic totally occlusion were also more likely to be seen in the elderly group. Univariate analysis revealed that age ≥ 85 years, cardiogenic shock or severe arrhythmia at admission, emergency PCI, prior stroke and chronic kidney disease were related to six-month mortality in elderly patients ≥ 75 years who underwent PCI. Multivariable logistic regression showed that cardiogenic shock or severe arrhythmia at admission, chronic kidney disease and prior stroke were independent risk factors predicting six-month mortality in elderly patients ≥ 75 years who had undergone PCI.
Conclusions
Our data showed that, compared with patients under 75 years, elderly patients (≥ 75 years) who had undergone PCI had a relative higher risk of mortality, and more often accompanied with multi-comorbidities, severer admission conditions and complex coronary lesions. Better evaluation of risk factors and more intensively care should be taken to patients ≥ 75 years who had undergone PCI therapy to reduce complications.
Keywords: Outcome, Percutaneous coronary intervention, The elderly
1. Introduction
China is facing a rapidly increasing aging population like many other developing countries, and it is estimated that almost 150 million Chinese will be over 75 years of age by 2050.[1] The incidence of ischemic heart disease (IHD) and percutaneous coronary intervention (PCI) are also consistently growing. In fact, patients ≥ 75 accounted for about 40% of the deaths caused by IHD.[2] Furthermore, age has been reported closely related to higher mortality and incidence of complications after PCI.[3],[4] Although age alone is not a contraindication to PCI, there is a lack of evidence regarding the optimal management of elderly patients undergoing PCI, especially in Chinese patients. Thus, there is a need to evaluate the safety and effectiveness of PCI in the specific patient group. The purpose of this research was to investigate clinical and angiographic characteristics of elderly patients who underwent PCI and assess risk factors related to post-PCI deaths and complications in patients ≥ 75 years of age.
2. Methods
2.1. Data sources and inclusion criteria
We retrospectively scanned 2,522 consecutive coronary heart disease patients admitted to the Cardiology Department of Shanghai Changzheng Hospital between December 2011 and November 2013, according to the criteria recommended by the 2013 ESC and ACCF/ASA guidelines.[5]–[7] Data were collected through clinical and PCI records, including demographic characteristics, PCI procedure details, medical history, and in-hospital complications. The followed-up was to gain the data on mortality and complications at six months. 573 patients who didn't undergo intervention process (patients' rejection, adopting other medical therapy, or transfer, etc.), 885 patients with digital subtraction angiography (DSA), and 30 patients whose in-hospital data and follow-up information were missing were excluded. 1,035 patients were finally included in this research. The patients aged between 30 and 92 years (64 ± 11 years). Among them, 213 patients were ≥ 75 (20.6%). The following cardiovascular risk factors were evaluated: hypertension, diabetes mellitus, chronic kidney failure, chronic obstructive pulmonary disease, peripheral vascular disease (PAD), dyslipidemia, stroke history, prior myocardial infarction, prior revascularization [PCI or coronary artery bypass grafting (CABG)], smoking, as well as in-hospital conditions including arrhythmia, cardiogenic shock. We also assessed the diagnosis of disease precisely, such as in-hospital biochemical biomarkers, and angiographic results of angioplasty.
2.2. Definitions
Emergency PCI was defined as PCI operated within 6 h after onset of ischemic symptoms of the heart. Diabetes included both type I and type II diabetics. Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or antihypertensive therapy at admission. Chronic kidney disease (CKD) was defined as abnormalities of kidney structure or function (imaging examination or biochemical examination), present for ≥ 3 months or a glomerular filtration rate < 60 mL/min per 1.73 m2 based on patients' medical history or renal replacement therapy at admission. Cardiogenic shock at admission was defined as systolic blood pressure < 90 mmHg or Killip IV grade at admission. Severe arrhythmia included ventricular fibrillation/flutter, atrial fibrillation/flutter, supraventricular tachycardia (SVT), ventricular tachycardia (VT), high-grade A-V block, bradycardia with heart rate < 45 beats/min. In-hospital outcomes included death, contrast-induced nephropathy, hemorrhagic complications and arrhythmia complications. Six-month outcomes included death, nonfatal myocardial infarction, revascularization including target vessel revascularization (TVR) and target lesion revascularization (TLR), as well as the composite outcome of major adverse cardiovascular event (MACE), which was defined as being any of the above individual outcomes.
2.3. Statistical analyses
All data were analyzed using SPSS 18.0. Binary data were presented by percentage, while qualitative data were presented as mean ± SD. Comparison of the two groups was performed using a chi-square test. Univariable and multivariable logistic regression were used in analyzing risk factors related to outcomes of PCI in patients ≥ 75. Risk factor correlations were considered significant in multivariable logistic regression if P < 0.10, and were considered significant in univariable logistic regression if P < 0.05.
3. Results
3.1. Baseline demographic characteristics
The baseline demographic characteristics of the research population are given in Table 1. The whole population was divided into four categories: (1) patients with SA ≥ 75 years (n = 58, 5.6%); (2) patients with SA < 75 years (n = 218, 21.0%); (3) patients with acute coronary syndrome (ACS) ≥ 75 years (n = 155, 15.0%); (4) patients with ACS < 75 years (n = 604, 58.4%). The male gender was predominant in all groups, and smoking was more prevalence in the younger patients. For ACS patients, there was a higher prevalence of hypertension (74.8% vs. 65.1%, P < 0.05), CKD (7.1% vs. 3.5%, P < 0.05), chronic obstructive pulmonary disease (COPD) (7.1% vs. 2.3%, P < 0.01), and PAD (11.0% vs. 6.1%, P < 0.05) in the elderly group. History of stroke, prior revascularization (PCI or CABG), cardiogenic shock and severe arrhythmia at admission were also more common in the elderly group. However, only hypertension, COPD and prior stroke showed a difference between patients ≥ 75 years old and < 75 years old with SA.
Table 1. Baseline demographic characteristics of the population.
| ACS |
SA |
|||||
| ≥ 75 yrs n = 155 |
< 75 yrs n = 604 |
P | ≥ 75 yrs n = 58 |
< 75 yrs n = 218 |
P | |
| Age (yrs) | 79.24 ± 3.51 | 59.81 ± 8.76 | < 0.01 | 78.72 ± 2.72 | 61.83 ± 7.55 | < 0.01 |
| Weight (Kg) | 61.94 ± 8.20 | 69.3 ± 10.27 | < 0.01 | 66.69 ± 9.59 | 69.76 ± 12.07 | < 0.05 |
| Female | 62 (40.0%) | 113 (18.7%) | < 0.01 | 17 (29.3%) | 55 (25.2%) | 0.318 |
| Smoking | 34 (21.9%) | 338 (56.0%) | < 0.01 | 15 (25.9%) | 91 (41.7%) | < 0.05 |
| Comorbidities | ||||||
| Hypertension | 116 (74.8%) | 393 (65.1%) | < 0.05 | 49 (84.5%) | 148 (67.9%) | < 0.01 |
| Diabetes mellitus | 40 (25.8%) | 131 (21.7%) | 0.282 | 15 (25.9%) | 72 (33.0%) | 0.342 |
| Chronic kidney disease | 11 (7.1%) | 21 (3.5%) | < 0.05 | 1 (1.7%) | 4 (1.8%) | 0.955 |
| Chronic obstructive pulmonary disease | 11 (7.1%) | 14 (2.3%) | < 0.01 | 6 (10.3%) | 5 (2.3%) | < 0.05 |
| Peripheral vascular disease | 17 (11.0%) | 37 (6.1%) | < 0.05 | 10 (17.2%) | 21 (9.6%) | 0.103 |
| Dyslipidemia | 10 (6.5%) | 63 (10.4%) | 0.134 | 4 (6.9%) | 21 (9.6%) | 0.519 |
| Related medical history | ||||||
| Prior myocardial infarction | 6 (3.9%) | 44 (7.3%) | 0.126 | 5 (8.6%) | 32 (14.7%) | 0.229 |
| Prior Stroke | 25 (16.1%) | 45 (7.5%) | < 0.01 | 14 (24.1%) | 14 (6.4%) | < 0.01 |
| Prior PCI/CABG | 5 (3.2%) | 48 (7.9%) | < 0.05 | 5 (8.6%) | 27 (12.4%) | 0.426 |
| Cardiogenic shock at admission | 26 (16.8%) | 28 (4.6%) | < 0.01 | 2 (3.4%) | 5 (2.3%) | 0.982 |
| Severe arrhythmia at admission | 33 (21.3%) | 59 (9.8%) | < 0.01 | 9 (15.5%) | 17 (7.8%) | 0.074 |
ACS: acute coronary syndrome; CABG: coronary artery bypass grafting; MACE: major adverse cardiovascular event; PCI: percutaneous coronary intervention; SA: stable angina.
3.2. Biochemical variables at admission
Biochemical variables at admission are shown in Table 2. Admission conditions were worse in patients ≥ 75 years with ACS. Compared with patients < 75 years, the elderly had lower hemoglobin (121.059 ± 28.70 g/L vs. 137.32 ± 28.70 g/L P < 0.01), platelet counts and albumin, higher creatinine, uric acid, urea nitrogen and pro-BNP (1750.49 ± 2222.81 pg/mL vs. 756.33 ± 1400.55 pg/mL, P < 0.01). However, blood lipids were better in the elderly group with relative lower triglyceride (1.35 ± 0.70 mmol/L vs. 1.72 ± 1.14 mmol/L P < 0.01) and higher high density lipoprotein (HDL) (1.06 ± 0.33 mmol/L vs. 0.97 ± 0.35 mmol/L P < 0.05). Same results could be seen among SA patients with lower plasma cholesterol (3.73 ± 0.77 mmol/L vs. 4.10 ± 1.00 mmol/L P < 0.05), triglyceride (1.37 ± 0.76 vs. 1.86 ± 1.20 mmol/L P < 0.01) and low density lipoprotein (LDL) (2.21 ± 0.68 mmol/L vs. 2.50 ± 0.8 mmol/L, P < 0.05).
Table 2. Biochemical variables at admission and surgical data of the population.
| ACS |
SA |
|||||
| ≥ 75 yrs |
< 75 yrs |
P | ≥ 75 yrs |
< 75 yrs |
P | |
| n = 155 | n = 604 | n = 58 | n = 218 | |||
| Hemoglobin (g/L) | 121.059 ± 28.70 | 137.32 ± 28.70 | < 0.01 | 128.53 ± 27.13 | 137.67 ± 22.47 | < 0.01 |
| Platelet (×109/L) | 180.03 ± 57.37 | 210.64 ± 71.15 | < 0.01 | 190.70 ± 55.27 | 198.88 ± 59.04 | 0.344 |
| Blood glucose (mmol/L) | 6.93 ± 2.79 | 6.79 ± 2.94 | 0.603 | 6.04 ± 1.97 | 6.24 ± 2.43 | 0.646 |
| Plasma cholesterol (mmol/L) | 3.91 ± 0.96 | 3.96 ± 1.02 | 0.535 | 3.73 ± 0.77 | 4.10 ± 1.00 | < 0.05 |
| Triglyceride (mmol/L) | 1.35 ± 0.70 | 1.72 ± 1.14 | < 0.01 | 1.37 ± 0.76 | 1.86 ± 1.20 | < 0.01 |
| HDL (mmol/L) | 1.06 ± 0.33 | 0.97 ± 0.35 | < 0.05 | 1.04 ± 0.27 | 1.02 ± 0.36 | 0.704 |
| LDL (mmol/L) | 2.44 ± 0.77 | 2.45 ± 0.81 | 0.88 | 2.21 ± 0.68 | 2.50 ± 0.87 | < 0.05 |
| Albumin (g/L) | 38.65 ± 7.72 | 41.28 ± 5.94 | < 0.01 | 41.95 ± 5.07 | 42.20 ± 4.53 | 0.716 |
| ALT* (U/L) | 52.37 ± 199.47 | 38.78 ± 32.38 | 0.408 | 26.62 ± 19.24 | 27.05 ± 16.40 | 0.864 |
| AST* (U/L) | 94.04 ± 146.59 | 66.68 ± 112.15 | < 0.05 | 33.84 ± 27.64 | 25.56 ± 14.99 | < 0.05 |
| Bilirubin* (μmol/L) | 13.99 ± 7.10 | 14.24 ± 6.45 | 0.698 | 13.81 ± 8.75 | 13.69 ± 8.88 | 0.928 |
| LDH* (U/L) | 636.76 ± 1182.63 | 471.56 ± 520.44 | 0.174 | 204.08 ± 66.94 | 249.69 ± 168.84 | < 0.05 |
| Creatinine (μmol/L) | 86.34 ± 33.74 | 75.48 ± 35.63 | < 0.01 | 83.95 ± 21.18 | 77.03 ± 43.78 | 0.244 |
| Uric acid (μmol/L) | 350.36 ± 120.22 | 327.99 ± 118.83 | < 0.05 | 355.17 ± 90.06 | 332.99 ± 117.21 | 0.204 |
| Urea nitrogena | 6.82 ± 2.74 | 5.84 ± 3.09 | < 0.01 | 6.19 ± 2.12 | 6.03 ± 1.88 | 0.586 |
| CK# (U/L) | 686.74 ± 1239.19 | 640.75 ± 1265.52 | 0.704 | 103.78 ± 73.33 | 94.62 ± 82.36- | 0.494 |
| CK-MB# (U/L) | 72.01 ± 125.48 | 70.55 ± 141.08 | 0.910 | 18.93 ± 10.21 | 16.93 ± 9.29 | 0.203 |
| Elevation of TnT# | 70 (47.3%) | 234 (41.9%) | 0.235 | 3 (6.1%) | 15 (7.7%) | 0.951 |
| Pro-BNP# (pg/mL) | 1750.49 ± 2222.81 | 756.33 ± 1400.55 | < 0.01 | 731.80 ± 1081.07 | 516.33 ± 1193.67 | 0.384 |
| SBP (mmHg) | 129.34 ± 22.37 | 128.52 ± 19.97 | 0.679 | 137.57 ± 21.77 | 130.30 ± 16.71 | < 0.05 |
| DBP (mmHg) | 75.80 ± 12.48 | 79.79 ± 12.22 | < 0.01 | 76.55 ± 9.01 | 79.12 ± 12.58 | 0.146 |
*Data missing for 1.5% (16) of the population. #Data missing for 13% (136) of the population. ACS: acute coronary syndrome; ALT: alanine aminotransferase; AST: aspartate aminotransferase; CK: creatine kinase; CK-MB: creatine kinase isoenzyme-MB; DBP: diastolic blood pressure; HDL: high density lipoprotein; LDH: lactate dehydrogenase; LDL: low density lipoprotein; pro-BNP: pro-brain natriuretic peptide; SA: stable angina; SBP: systolic blood; TnT: troponin T.
3.3. Procedure characteristics
Coronary disease was more severe in the elderly that presented with ACS, with multi-vessel disease (85.2% vs. 73.8% P < 0.01) and significantly more frequent in left circumflex artery (LCX) and Right coronary artery (RCA) lesions, calcified lesions and chronic total occlusion (12.9% vs. 6.0%, P < 0.01) than younger patients. However, these differences weren't seen in SA patients. Furthermore, Intra-aortic balloon pump (IABP) was more frequently used in the elderly group (3.9% vs. 1.2%, P < 0.05). Procedure characteristics are shown in Table 3.
Table 3. Angiographic and procedural characteristics.
| ACS |
SA |
|||||
| ≥ 75 yrs |
< 75 yrs |
P | ≥ 75 yrs |
< 75 yrs |
P | |
| n = 155 | n = 604 | n = 58 | n = 218 | |||
| Emergency PCI | 48 (31.0%) | 141 (23.3%) | 0.050 | - | - | - |
| Radial approach | 110 (71.0%) | 506 (83.8%) | < 0.01 | 46 (79.3%) | 189 (86.7%) | 0.160 |
| Drug-eluting stent u-se | 148 (95.5%) | 582 (96.4%) | 0.471 | 55 (94.8%) | 213 (97.7%) | 0.613 |
| Stent implantation | ||||||
| Diseased vessels | ||||||
| LAD | 149 (96.1%) | 555 (91.9%) | 0.069 | 249 (90.2%) | 196 (89.9%) | 0.738 |
| LCX | 105 (67.7%) | 356 (58.9%) | < 0.05 | 37 (63.8%) | 141 (64.7%) | 0.900 |
| RCA | 119 (76.8%) | 398 (65.9%) | < 0.05 | 177 (64.1%) | 141 (64.7%) | 0.713 |
| Multi-vessel disease | 132 (85.2%) | 446 (73.8%) | < 0.01 | 44 (75.9%) | 162 (74.3%) | 0.193 |
| Double vessel | 42 (27.1%) | 184 (30.5%) | 24 (41.4%) | 64 (29.4%) | ||
| Triple vessel | 90 (58.1%) | 262 (43.4%) | 20 (34.5%) | 98 (45.0%) | ||
| Left main lesion | 14 (9.0%) | 36 (6.0%) | 0.169 | 0 | 11 (5.0%) | 0.171 |
| Chronic total occlusion | 20 (12.9%) | 36 (6.0%) | < 0.01 | 1 (1.7%) | 13 (6.0%) | 0.332 |
| Myocardial bridge | 9 (5.8%) | 56 (9.3%) | 0.169 | 6 (10.3%) | 15 (6.9%) | 0.545 |
| Calcified lesion | 42 (27.1%) | 96 (15.9%) | < 0.01 | 15 (25.9%) | 45 (20.7%) | 0.401 |
| IABP use | 6 (3.9%) | 7 (1.2%) | < 0.05 | - | - | - |
ACS: acute coronary syndrome; CTO: chronic total occlusion; IABP: intra-aortic balloon pump; LAD: left anterior descending coronary artery; LCX: left circumflex coronary artery; PCI: percutaneous coronary intervention; RCA: right coronary artery; SA: stable angina.
3.4. Clinical outcomes
In-hospital and six-month follow-up were completed for all 1,035 patients. In-hospital mortality was 3.3% in patient ≥ 75 years and 1.0% in the younger group and all deaths of patients ≥ 75 years occurred in ACS patients. Overall mortality at six months was 6.1% in the elderly group and 1.9% in patients < 75 years. Hemorrhagic complications and contrast nephropathy were more common in the elderly patients with ACS, compared with younger patients. However, there was no difference between the two age groups in nonfatal myocardial infarction, revascularization and MACEs at six months, regardless of ACS or SA. Kaplan Meier analysis of cumulative survival (Figure 1) and event-free survival (death, myocardial infarction and revascularization, Figure 2) demonstrated significant differences in survival among the four groups. Univariable analysis OR determined that age ≥ 85 years (OR = 5.155, P = 0.024), emergency PCI (OR = 7.385, P = 0.006), chronic kidney failure (OR = 8.444, P = 0.02), cardiogenic shock at admission (P < 0.001), severe arrhythmia at admission (P < 0.001), prior stroke (OR = 5.219, P = 0.015) were all associated with a higher mortality rate at six months in elderly patients ≥ 75 years old who underwent PCI (Table 4). Multivariate logistic analysis identified chronic kidney failure, cardiogenic shock at admission, severe arrhythmia at admission and prior stroke as independent predictors of six-month mortality.
Figure 1. Kaplan-Meier survival curve of cumulative survival at six months for whole study population.
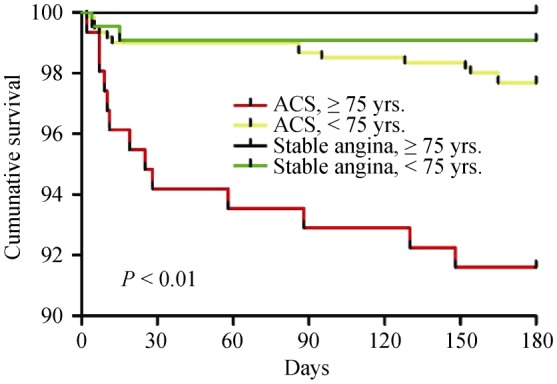
ACS: acute coronary syndrome.
Figure 2. Kaplan-Meier survival curve of event-free (death, myocardial infarction and revascularization) survival for whole study population.
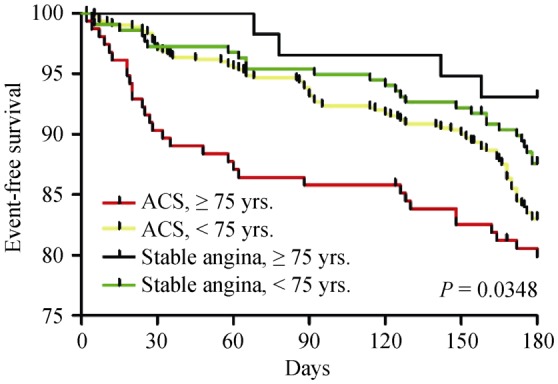
ACS: acute coronary syndrome.
Table 4. In-hospital and six-month outcomes of PCI.
| ACS |
P | SA |
P | |||
| ≥ 75 yrs |
< 75 yrs |
75 yrs |
< 75 yrs |
|||
| n = 155 | n = 604 | n = 58 | n = 218 | |||
| In-hospital events | ||||||
| In-hospital deaths | 7 (4.5%) | 6 (1.0%) | < 0.01 | 0 | 2 (0.9%) | 1.00 |
| Hemorrhagic complications | 14 (9.0%) | 26 (4.3%) | < 0.05 | 4 (6.9%) | 8 (3.7%) | 0.478 |
| Hematoma, pseudoaneurysm or other vascular complication | 12 | 24 | 4 | 8 | ||
| Retroperitoneal hematoma | 1 | 2 | 0 | 0 | ||
| Coronary artery perforation | 1 | 0 | 0 | 0 | ||
| Acute stent thrombosis | 2 (1.3%) | 6 (1.0%) | 1.00 | - | - | - |
| Arrhythmia complications | 5 (3.2%) | 11 (1.8%) | 0.44 | 2 (0.7%) | 0 | 1.00 |
| Contrast nephropathy | 7 (4.5%) | 3 (0.5%) | < 0.01 | 1 (1.7%) | 1 (0.5%) | 0.377 |
| Six-month events | ||||||
| Six-month deaths | 13 (8.4%) | 14 (2.3%) | < 0.01 | 0 | 2 (0.9%) | 1.00 |
| Cardiac death | 12 (7.7%) | 11 (1.8%) | 0 | 2 (0.9%) | ||
| Others | 1 (0.6%) | 3 (0.5%) | 0 | 0 | ||
| Myocardial infarction | 5 (3.2%) | 6 (1.0%) | 0.090 | 2 (3.4%) | 2 (0.9%) | 0.196 |
| Revascularization | 21 (13.5%) | 91 (15.1%) | 0.635 | 5 (8.6%) | 23 (10.6%) | 0.665 |
| MACEs | 31 (20.0%) | 102 (16.9%) | 0.363 | 4 (6.9%) | 27 (12.4%) | 0.239 |
ACS: acute coronary syndrome; MACE: major adverse cardiovascular event; SA: stable angina.
4. Discussion
This single center retrospective study was conducted with a cohort of 1,035 patients who underwent PCI, with 213 patients ≥ 75 years. Our study showed that over 20% patients undergoing PCI are elderly patients ≥ 75 years old, consistent with a recent study conducted among patients with acute myocardial infarction.[8] In fact, the proportion of elderly patients ≥ 75 years who underwent nonemergency PCI had increased from 8.7% in 2000 to 13.7% in 2007, according to the research by the Scottish Coronary Revascularization Register.[9] Additionally, another register suggested that PCI for ST-segment elevated myocardial infarction among patients ≥ 80 years reached 31.2% in 2010, compared to 9.2% in 2001.[10] Elderly patients have gradually become a more important category of patients in the PCI practice.
Table 5. Effects of multiple variables on six-month mortality in univariate and multivariate logistic regression analysis.
| Univariate analysis |
Multivariate analysis |
|||||
| OR | 95% CI | P | OR | 95% CI | P | |
| Age ≥ 85 yrs | 5.155 | 1.238−21.459 | 0.024 | |||
| Cardiogenic shock at admission | 11.933 | 3.760−37.876 | < 0.001 | 5.819 | 1.471−23.015 | 0.012 |
| Severe arrhythmia at admission | 9.055 | 2.852−28.747 | < 0.001 | 11.275 | 2.503−50.778 | 0.002 |
| Chronic kidney failure | 8.444 | 2.214−32.201 | 0.02 | 9.038 | 1.271−64.247 | 0.028 |
| Previous stroke | 5.219 | 1.713−15.896 | 0.015 | 5.222 | 1.262−21.603 | 0.023 |
| Emergency PCI | 7.385 | 2.343−23.273 | 0.001 | |||
PCI: percutaneous coronary intervention.
In the last decade, it had been proven by a series of studies,[11]–[13] that performing PCI on elderly patients ≥ 75 years may not yield as much risk as had been previously imagined, in spite of the fact that nearly all of these studies focused exclusively on patients with acute myocardial infarction. Our study also confirmed PCI as a relatively safe strategy for coronary heart disease management among patients ≥ 75 years with acceptable in-hospital mortality (3.3%) and six-month mortality (6.1%). However, there still exists some hesitation among cardiologists in using PCI as treatment for myocardial infarction among patients ≥ 75 years, due to the concern of a high rate of complications, relatively unfavorable outcomes, and a high prevalence of complex comorbidities.[14]
In this study, we have included patients with coronary heart disease presenting as SA—an under researched group by previous studies. Our data suggested a significant difference of clinical and perioperative characteristics between patients ≥ 75 years and patients < 75 years, with elderly patients having more comorbidities and complex coronary diseases than their younger counterparts. Hypertension, chronic kidney disease, COPD, and peripheral vascular disease were more common among patients ≥ 75 years, which would be understandable given the fact that these pathologies are associated with an advanced age. There were a higher number of active smokers and male patients in the younger group, possibly for the reason that more elderly patients had quit smoking, and women, in general, have a relative longer life expectancy than men.[15] It was also found that cardiogenic shock and severe arrhythmia at admission were more common among the elderly patients, indicating a graver impact of coronary heart disease on the elderly, in accordance with our findings of a greater incidence of multi-vessel disease, calcified lesions and chronic total occlusion among patients ≥ 75 years old. All of the above mentioned conditions increase the difficulty of PCI procedure and probability of adverse outcomes.[16] However, prior revascularization (PCI or CABG) was more prevalent in the younger group, partly for the reason that younger patients had a relatively higher incidence of prior myocardial infarction (9.2% vs. 5.2%, P = 0.07) and patients who experienced two episodes of myocardial infarction could seldom live a life longer than 75 years.
Despite the difference in clinical characteristics, the major problems associated with PCI in elderly patients ≥ 75 years old were high mortality and incidence of complications. Studies suggested that patient ≥ 75 years undergoing PCI had a higher incidence of procedure complications and worse outcomes, be they in-hospital, short-term or long-term ones.[3], [9] One of the most worrisome perioperative complications has been contrast-induced nephropathy, which was reported to occur in 2% to 25% of all patients receiving PCI treatment.[17] Although the incidence of contrast-induced nephropathy in our study was lower than results from a previous large cohort study of patients,[18] which reported an incidence of 9.4%, we still found that it was significantly higher among the elderly patients (3.8% vs. 0.5%, P = 0.01), which was correlated with a relatively higher level of serum creatinine, uric acid and urea nitrogen, and with chronic kidney disease that was seen more often among the elderly. Several factors including volume of contrast-medium > 200 mL, anemia, eGFR < 60 mL/min per 1.732 were found related to contrast-induced nephropathy.[17],[19] Therefore, measures like evaluating kidney function, reducing the volume of contrast-medium, and alleviating anemia may be helpful. With pre-emptive hydration treatment, the incidence of contrast-induced nephropathy could be reduced.[20] Mortality of the elderly patients undergoing PCI varied considerably with different types of coronary heart diseases. The in-hospital and six-month mortality of patients with ACS was 4.5% and 8.4% respectively, among which ST-segment elevated myocardial infarction was the worst, with a six-month mortality rate of 15.9%, whereas among those with SA, the in-hospital mortality was 0% and so was six-month counterpart mortality. Our results correlated well with previous studies by Teplisky, et al.[21] and Sillano, et al.[22]
In our study, we identified cardiogenic shock and severe arrhythmia at admission, chronic kidney disease, and prior strokes as independent risk factors for six-month mortality among elderly patients undergoing PCI for coronary artery disease, partly in alignment with the result of a study done by Bauer, et al.[3] which regarded age, female gender, hemodynamic instability, STEMI, prior stroke, chronic renal failure, congestive heart failure, and diabetes mellitus as independent risk factors for in-hospital mortality among patients ≥ 75 years old undergoing PCI for acute coronary syndrome. One study reported that independent risk factors of in-hospital adverse events among elderly patients (> 65 years) who underwent primary PCI included Killip > 1, post-thrombolysis in myocardial infarction < 3 and admission blood glucose levels.[23] Another study that surveyed over four million patients with acute myocardial infarction identified intra-aortic balloon pump use, acute renal failure, acute cerebrovascular disease, age ≥ 80 years, peripheral vascular disease, gastrointestinal bleeding, female gender, congestive heart failure, chronic lung disease, weekend admission and multi-vessel PCI as independent risk factors of in-hospital mortality among elderly patients who underwent PCI.[10] The difference of various risk factors for mortality among elderly patients in these studies may be attributable to ethnicity and selection criteria of patients. However, all these results indicated that renal deficiency (be it acute or chronic), hemodynamic instability, and complex coronary lesions are the main causes of adverse outcomes among elderly patients even with optimal reperfusion therapy for their coronary artery disease.
4.1. Limitations
Several limitations should be taken into consideration when the results of this study are interpreted. Relative small sample size may be the main limitation in our study, which might affect the results of logistic regression analysis of multiple risk factors and Kaplan-Meier survival analysis. Secondly, the time of follow-up is relative short, which may not uncover the long-term clinical characteristics and outcomes of elderly patients following PCI. Furthermore, the fact that the population is sourced from a single hospital and the patients are all ethnically Chinese, also are limitations of this study generalizability.
4.2. Conclusions
PCI has become safer and more effective in elderly patients ≥ 75 years old. This is possibly due to extensive use of drug-eluting stents and standardization of medical treatment adjunctive PCI procedure.[24] Age should not be a contraindication when patients are being considered for PCI treatment. Nevertheless, mortality and incidence of adverse outcomes are significantly higher in this special patients group, compared with the younger patient populations. Cardiogenic shock and severe arrhythmia at admission, chronic kidney disease, prior stroke were strongly related to in-hospital and short-term mortality outcomes among patients ≥ 75 years. These observations revealed the complexity of the multiple factors influencing PCI in elderly patients, which needs more researches to find effective measures to improve the survival and outcome after PCI procedure.
Acknowledgments
This study was supported by the Science and Technology Commission of Shanghai Municipality (No.13411950202).
References
- 1.Flaherty JH, Liu ML, Ding L, et al. China: the aging giant. J Am Geriatr Soc. 2007;55:1295–1300. doi: 10.1111/j.1532-5415.2007.01273.x. [DOI] [PubMed] [Google Scholar]
- 2.Moran AE, Forouzanfar MH, Roth GA, et al. Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the Global Burden of Disease 2010 study. Circulation. 2014;129:1483–1492. doi: 10.1161/CIRCULATIONAHA.113.004042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauer T, Mollmann H, Weidinger F, et al. Predictors of hospital mortality in the elderly undergoing percutaneous coronary intervention for acute coronary syndromes and stable angina. Int J Cardiol. 2011;151:164–169. doi: 10.1016/j.ijcard.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Thomas MP, Moscucci M, Smith DE, et al. Outcome of contemporary percutaneous coronary intervention in the elderly and the very elderly: insights from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium. Clin Cardiol. 2011;34:549–554. doi: 10.1002/clc.20926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Task Force Members. Montalescot G, Sechtem U, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949–3003. doi: 10.1093/eurheartj/eht296. [DOI] [PubMed] [Google Scholar]
- 6.American College of Emergency Physicians, Society for Cardiovascular Angiography and Interventions. O'Gara PT, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:485–510. doi: 10.1016/j.jacc.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 7.Writing Committee Members. Jneid H, Anderson JL, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2012;126:875–910. doi: 10.1161/CIR.0b013e318256f1e0. [DOI] [PubMed] [Google Scholar]
- 8.Caretta G, Passamonti E, Pedroni PN, et al. Outcomes and predictors of mortality among octogenarians and older with ST-segment elevation myocardial infarction treated with primary coronary angioplasty. Clin Cardiol. 2014;37:523–529. doi: 10.1002/clc.22313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnman C, Oldroyd KG, Mackay DF, et al. Percutaneous coronary intervention in the elderly: changes in case-mix and periprocedural outcomes in 31,758 patients treated between 2000 and 2007. Circ Cardiovasc Interv. 2010;3:341–345. doi: 10.1161/CIRCINTERVENTIONS.109.928705. [DOI] [PubMed] [Google Scholar]
- 10.Khera S, Kolte D, Palaniswamy C, et al. ST-elevation myocardial infarction in the elderly—temporal trends in incidence, utilization of percutaneous coronary intervention and outcomes in the United States. Int J Cardiol. 2013;168:3683–3690. doi: 10.1016/j.ijcard.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 11.Ciszewski A, Karcz M, Kepka C, et al. Primary angioplasty in patients > or = 75 years old with ST-elevation myocardial infarction - one-year follow-up results. Kardiol Pol. 2008;66:828–836. [Article in English, Polish] [PubMed] [Google Scholar]
- 12.Wenaweser P, Ramser M, Windecker S, et al. Outcome of elderly patients undergoing primary percutaneous coronary intervention for acute ST-elevation myocardial infarction. Catheter Cardiovasc Interv. 2007;70:485–490. doi: 10.1002/ccd.21128. [DOI] [PubMed] [Google Scholar]
- 13.Sakai K, Nagayama S, Ihara K, et al. Primary percutaneous coronary intervention for acute myocardial infarction in the elderly aged ≥ 75 years. Catheter Cardiovasc Interv. 2012;79:50–56. doi: 10.1002/ccd.22810. [DOI] [PubMed] [Google Scholar]
- 14.Forman DE, Chen AY, Wiviott SD, et al. Comparison of outcomes in patients aged < 75, 75 to 84, and ≥ 85 years with ST-elevation myocardial infarction (from the ACTION Registry-GWTG) Am J Cardiol. 2010;106:1382–1388. doi: 10.1016/j.amjcard.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 15.Shrestha R, Xu J, Xie D, et al. Comparison of clinical outcomes of Chinese men and women after coronary stenting for coronary artery disease: a multi-center retrospective analysis of 4,334 patients. J Biomed Res. 2014;28:368–75. doi: 10.7555/JBR.28.20120127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hsu JT, Kyo E, Chu CM, et al. Impact of calcification length ratio on the intervention for chronic total occlusions. Int J Cardiol. 2011;150:135–141. doi: 10.1016/j.ijcard.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44:1393–1399. doi: 10.1016/j.jacc.2004.06.068. [DOI] [PubMed] [Google Scholar]
- 18.Khera S, Kolte D, Aronow WS, et al. Trends in acute kidney injury and outcomes after early percutaneous coronary intervention in patients ≥ 75 years of age with acute myocardial infarction. Am J Cardiol. 2013;112:1279–1286. doi: 10.1016/j.amjcard.2013.06.008. [DOI] [PubMed] [Google Scholar]
- 19.Fu N, Li X, Yang S, et al. Risk score for the prediction of contrast-induced nephropathy in elderly patients undergoing percutaneous coronary intervention. Angiology. 2013;64:188–194. doi: 10.1177/0003319712467224. [DOI] [PubMed] [Google Scholar]
- 20.Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/ AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44–e122. doi: 10.1016/j.jacc.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 21.Teplitsky I, Assali A, Lev E, et al. Results of percutaneous coronary interventions in patients > or =90 years of age. Catheter Cardiovasc Interv. 2007;70:937–943. doi: 10.1002/ccd.21263. [DOI] [PubMed] [Google Scholar]
- 22.Sillano D, Resmini C, Meliga E, et al. Retrospective multicenter observational study of the interventional management of coronary disease in the very elderly: the NINETY. Catheter Cardiovasc Interv. 2013;82:414–421. doi: 10.1002/ccd.24406. [DOI] [PubMed] [Google Scholar]
- 23.Ekmekci A, Uluganyan M, Tufan F, et al. Impact of admission blood glucose levels on prognosis of elderly patients with ST elevation myocardial infarction treated by primary percutaneous coronary intervention. J Geriatr Cardiol. 10:310–316. doi: 10.3969/j.issn.1671-5411.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rao SV, Hess CN, Dai D, et al. Temporal trends in percutaneous coronary intervention outcomes among older patients in the United States. Am Heart J. 2013;166:273–281. doi: 10.1016/j.ahj.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]


