Abstract
Study Objectives:
Emerging evidence suggests that insomnia may disrupt reward-related brain function—a potentially important factor in the development of depressive disorder. Adolescence may be a period during which such disruption is especially problematic given the rise in the incidence of insomnia and ongoing development of neural systems that support reward processing. The present study uses longitudinal data to test the hypothesis that disruption of neural reward processing is a mechanism by which insomnia symptoms—including nocturnal insomnia symptoms (NIS) and nonrestorative sleep (NRS)—contribute to depressive symptoms in adolescent girls.
Method:
Participants were 123 adolescent girls and their caregivers from an ongoing longitudinal study of precursors to depression across adolescent development. NIS and NRS were assessed annually from ages 9 to 13 years. Girls completed a monetary reward task during a functional MRI scan at age 16 years. Depressive symptoms were assessed at ages 16 and 17 years. Multivariable regression tested the prospective associations between NIS and NRS, neural response during reward anticipation, and the mean number of depressive symptoms (omitting sleep problems).
Results:
NRS, but not NIS, during early adolescence was positively associated with late adolescent dorsal medial prefrontal cortex (dmPFC) response to reward anticipation and depressive symptoms. DMPFC response mediated the relationship between early adolescent NRS and late adolescent depressive symptoms.
Conclusions:
These results suggest that NRS may contribute to depression by disrupting reward processing via altered activity in a region of prefrontal cortex involved in affective control. The results also support the mechanistic differentiation of NIS and NRS.
Citation:
Casement MD, Keenan KE, Hipwell AE, Guyer AE, Forbes EE. Neural reward processing mediates the relationship between insomnia symptoms and depression in adolescence. SLEEP 2016;39(2):439–447.
Keywords: insomnia, nonrestorative sleep, depression, affective processing, fMRI, adolescence
Significance.
Insomnia is associated with the onset of depression during adolescence, but the mechanisms of this relationship are not well established. One possibility is that adolescents with insufficient sleep process positive events differently than adolescents with adequate sleep. The results from this study are consistent with a neurodevelopmental model of depression in which insomnia symptoms during early adolescence contribute to later depressive symptoms by disrupting reward-related brain function. Future research should try to determine whether nonrestorative sleep and nocturnal insomnia symptoms have unique effects on the development of reward-related circuitry and depression during adolescence.
INTRODUCTION
Insomnia—recurrent and persistent difficulty with falling asleep, staying asleep, or non-restorative sleep with associated daytime distress or functional impairment1–3—dramatically increases risk for depression.4–6 In fact, some researchers argue that insomnia causes depression.7 Evidence for this assertion comes from longitudinal, epidemiological studies, in which a diagnosis of insomnia doubles the risk for subsequent depression onset,8 as well as intervention studies, in which improvements in depressive symptoms are observed following treatment for insomnia.9–11 Although the relationship between insomnia and depression is likely bidirectional, there is persuasive evidence that insomnia often precedes the onset of depression and should be regarded as an important etiological factor.12
Adolescence is a key developmental period in which to understand the link between insomnia and depression, in part because this is when insomnia and depression often present for the first time.13,14 Symptoms of insomnia and depression are also common in adolescence, particularly among adolescent girls.13–16 Moreover, because insomnia12 and depression17 are both recurrent disorders, their onset during adolescence is associated with a more protracted and debilitating disease course relative to an onset later in life. Elucidating the pathophysiology of insomnia and depression and the direction of association between these disorders during adolescence is essential for primary and secondary intervention. Existing data indicate that, consistent with associations in adults, there is a bidirectional relationship between adolescent insomnia and depression; however, the most common pattern during adolescence is for insomnia to precede and predict depression onset.18–20
Despite robust evidence for the positive association between insomnia and depression in adolescence, the mechanisms by which insomnia contributes to depression are not well established. One possibility is that hyperarousal and insufficient sleep in insomnia disrupt the function of corticolimbic circuitry such as the prefrontal cortex (PFC), striatum, and amygdala, and thereby compromise affective reactivity and regulation.21,22 Consistent with this proposition, insomnia, poor sleep quality, and experimentally induced sleep deprivation all predict disrupted reactivity to affective stimuli, and sleep deprivation additionally shows robust negative effects on mood.19,23–25 Furthermore, disruption of approach-related systems may be particularly central to the development of depression, and several studies indicate that partial sleep restriction produces greater decrements in positive/approach-related affect than in negative affect.26–30 There is also emerging evidence that neural response to approach-related cues such as rewards is disrupted in adolescents with poor sleep quality, and following sleep deprivation in both adolescents and adults.31–33 Collectively, these data suggest a triadic link between adolescent insomnia, neural response to rewards, and depression, but this model has not been formally evaluated.
In the present study, we tested the hypothesis that disruption in neural response to rewards is a mechanism by which insomnia symptoms during early adolescence contribute to depressive symptoms in later adolescence in a sample of girls enriched for depression risk. We evaluated insomnia symptoms, including nocturnal insomnia symptoms (NIS; difficulty falling and staying asleep) and nonrestorative sleep (NRS; feeling poorly rested upon awakening), for five consecutive years during early adolescence. NIS and NRS are both included in widely used insomnia diagnostic criteria1–3 and they have comparable levels of association with depressive symptoms.34 However, there is ongoing debate as to whether NRS should be a distinct diagnostic entity.34–36 Therefore, NRS and NIS were examined in combination and separately. When participants were 16 years of age, we assessed neural response during anticipation of reward in four approach-related regions of interest (ROIs): the striatum, which is key to reward motivation37; the medial prefrontal cortex (mPFC), which is instrumental in affective control and evaluation of the self-relevance of rewards38–40; the orbitofrontal cortex (OFC), which is implicated in reward valuation41; and the amygdala, which is involved in reward representation.42 Depressive symptoms were assessed in early adolescence at age 9 years and late adolescence at ages 16 and 17 years. These data were used to examine associations between early adolescent insomnia symptoms and later neural response during reward anticipation and depressive symptoms (excluding sleep-related items), adjusting for depressive symptoms in early adolescence. Meta-analytic results indicate that depression is typically associated with decreased response to reward in the striatum and increased response in the dorsal mPFC (dmPFC).43 Therefore, we expected insomnia symptoms during early adolescence to predict decreased striatal and increased dmPFC response to rewards and greater depressive symptoms in late adolescence. Furthermore, we expected neural response to rewards to mediate the relationship between insomnia symptoms and depressive symptoms.
METHODS
Participants
Participants were drawn from the Pittsburgh Girls Study -Emotions Sub-study (PGS-E)—a longitudinal study of precursors to depression that includes functional magnetic resonance imaging (fMRI) during adolescence. Previously published neuroimaging papers with the PGS-E sample are described briefly in the supplemental material. Of the 123 girls included in the present analysis, 65% were Black, 27% were White, and 8% identified as multi-racial. Sixty percent of the study families received some form of public assistance when the girls were between the ages of 9 and 12; 26% of the families received public assistance continuously during that period. Criteria for major depressive disorder (MDD) were met by 18 participants during the first PGS-E assessment at age 9, three participants when they were scanned at age 16, and two participants at age 17.
The PGS-E sample was recruited from the youngest cohort of participants in a larger longitudinal study, the Pittsburgh Girls Study (PGS), after screening high for depressive symptoms (n = 135) or being randomly selected from PGS participants who did not screen high for depressive symptoms (n = 128).44 Of the 263 families eligible to participate in the PGS-E, 232 (88.2%) agreed to participate and completed the first assessment when the girls were 9 years of age. PGS-E participants were assessed annually until 13 years of age, and again between 16 and 17 years of age. Retention in each year through age 13 was greater than 89%, and was above 74% at ages 16–17. Of the 147 girls who completed the fMRI scan, 24 participants were excluded from fMRI analysis. Reasons for exclusion included: > 25% of volumes with movement > 3 standard deviation (SD) from the subject's mean, > 0.5 mm scan-to-scan translation, or > 0.01 degrees of scan-to-scan rotation (n = 5); incidental findings (n = 1); < 80% striatum coverage (n = 13); poor quality scan (n = 1); or failure to respond on ≥ 80% of the trials or inappropriate response timing (n = 4). The distribution of race, public assistance, insomnia symptoms, and depressive symptoms for girls whose data was included in fMRI analyses was representative of the full PGS-E sample. The PGS-E protocol was approved and monitored by the University of Pittsburgh Institutional Review Board and performed in accordance with relevant guidelines and regulations.
Symptom Assessment
The Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS)45 provided a measure of insomnia and depression symptoms across early to late adolescence. The K-SADS is a semi-structured interview that was administered separately to the girls and their primary care-givers at each PGS-E assessment by research assistants who were trained and monitored by a licensed clinical psychologist (K.K.). The 3 K-SADS items that assess NIS (difficulty falling asleep, middle of the night awakening, early morning awakening) and the single item that assesses NRS (feeling unrested upon awakening) were scored using three-point scales (1 = “not present,” 2 = “subthreshold,” 3 = “threshold”). Symptoms of insomnia were considered present if they were endorsed by either the girl or her primary caregiver. We counted the total number of insomnia (INS: NIS+NRS), NIS, and NRS items at threshold for each assessment year (range = 0 to 4 for INS; 0 to 3 for NIS, 0 to 1 for NRS). The mean counts of INS, NIS, and NRS across ages 9 through 13 years were used as predictors in regression analyses (INS mean = 0.43, SD = 0.48; NIS mean = 0.27, SD = 0.35; NRS mean = 0.15, SD = 0.24). Due to the positive skew of INS, NIS, and NRS scores, these values were natural log transformed for analyses (constant of 0.5 was added to scores to eliminate “0” values prior to log transformation). There was a small but significant correlation between NIS and NRS scores in this sample (r = 0.25, P < 0.05).
Each of the 9 symptoms of depression was assessed using a 3-point scale (1 = “not present,” 2 = “subthreshold,” 3 = “threshold”) regardless of whether disturbance in mood or anhedonia were endorsed. Symptoms of depression were considered present if they were endorsed by either the girl or her primary caregiver. The count of depressive symptoms at threshold, omitting sleep problems, was calculated for each assessment year (range: 0 to 8). A mean count of depressive symptoms across ages 16 and 17 years was used in regression analyses (with log-transformation). Age 16 and 17 depression scores were combined due to the low count of depressive symptoms in this sample during later adolescence (Age 16: mean = 0.87, SD = 1.16; Age 17: mean = 0.79, SD = 1.07). The count of depressive symptoms at age 9 was used as a covariate to adjust for baseline depression. K-SADS ratings were also used to determine whether participants met Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)2 criteria for MDD.
Reward Processing Task
Neural response to rewards was measured using a Reward Guessing Task.46 Participants were instructed to guess whether the value of a visually presented card, with possible value from 1–9, would be greater or less than five. In the event-related task design, each trial began with the presentation of a blank card. Participants had 4 s to guess the value of the card via button press. The type of trial was then displayed for 6 s using an image with hands shuffling cards overlaid on an upward facing yellow arrow to indicate potential reward trials or a downward facing yellow arrow to indicate potential loss trials. This was followed by the presentation of the “actual” card value for 500 ms, feedback on the trial outcome for 500 ms (a green upward-facing arrow for win, a red downward- facing arrow for loss, or a yellow circle for a no-change outcome), and a crosshair displayed for 9 s. There were 24 trials, 20 s each, administered over a single 8 min run. Trials were presented in pseudorandom order and outcomes were predetermined with a balanced number of trial types (12 potential reward, 12 potential loss; 6 win, 6 loss, and 12 no-change outcomes). Participants were told that they would receive their winnings after the scan ($1 per win outcome, 50¢ per loss); in fact, all participants received $10.
MRI Acquisition, Processing, and Analysis
Neuroimaging was conducted on a Siemens 3.0 T Tim Trio scanner. Functional images were acquired using a gradient echo planar imaging (EPI) sequence that included 39 axial slices (3.1 mm wide) beginning at the cerebral vertex and extending across the entire cerebrum and most of the cerebellum (TR/TE = 2000/28 ms, field of view = 20 cm, matrix = 64 × 64). Scanning parameters were selected to optimize BOLD signal quality while maximizing whole brain coverage. A reference EPI scan was acquired before fMRI data collection to visually inspect for artifacts (e.g., ghosting) and ensure adequate signal across the entire volume. In addition, a 160-slice high-resolution sagittally acquired T1-weighted anatomical image was collected for co-registration and normalization of functional images (TR/TE = 2300/2.98 ms, field of view = 20 cm, matrix = 256 × 240).
Preprocessing and analysis of imaging data were conducted using Statistical Parametric Mapping (SPM8; http://www.fil.ion.ucl.ac.uk/spm) software. Anatomical images were auto-segmented in SPM8 prior to analysis. Functional image preprocessing included: (1) slice timing correction to the middle volume in the time-series; (2) spatial realignment to the first volume in the time series to correct for head motion; (3) spatial normalization to Montreal Neurological Institute (MNI) stereotaxic space using a 12-parameter affine model; and (4) image smoothing using a Gaussian filter set at 6 mm full-width half-maximum to minimize noise and individual differences in gyral anatomy. Voxel-wise signal was ratio-normalized to the whole-brain global mean. In addition, Artifact Detection Toolbox (ART; http://www.nitrc.org/projects/artifact_detect/) software was used to detect functional volumes with movement > 3 SD from the subject's mean, > 0.5 mm scan-to-scan translation, or > 0.01 degrees of scan-to-scan rotation. Preprocessed data were inspected prior to second-level analysis to ensure that all participants had fewer than 25% of volumes with excessive movement detected by ART, good scan quality, and ventral striatum coverage of at least 80%. Temporal censoring based on ART output was used to remove motion artifacts in first-level analysis for the remaining 123 participants.47
Second-level random effects models were used to estimate neural response to rewards while accounting for scan-to-scan and between-participant variability. For each participant, condition effects were calculated at each voxel using paired t-tests for reward anticipation > baseline. Reward anticipation was defined as the 12 potential win intervals that included 8 s total: the 6 s potential win arrow, 500 ms number feedback, 500 ms outcome feedback, and the first second of fixation. The reward anticipation period extended 2 s beyond the potential-win arrow to account for the typical timing of the hemodynamic response relative to neural activity and to capture as much of the reward anticipation response as possible while avoiding substantial overlap with BOLD response to reward outcome events. The last 3 s of fixation for all 24 trials served as the baseline condition. By averaging the last 3 s of fixation across all the outcome events (6 win, 6 loss, 12 no-change), the baseline condition served as a relatively neutral comparison for contrasts with reward anticipation.
Analysis of imaging data was restricted to a composite mask that included four reward-related ROIs: the striatum, mPFC, OFC, and amygdala. All 4 ROIs were defined using PickAtlas 3.0.3 (http://fmri.wfubmc.edu/software/PickAtlas). The striatal ROI was defined as a sphere with a 20 mm radius, centered on the Talairach coordinates of x = 0, y = 10 and z = −10, and encompassing the ventral and dorsal striatum bilaterally (including nucleus accumbens). The mPFC ROI was defined as a sphere with a 25 mm radius, centered on Talairach coordinates x = 0, y = 42, z = 18, and encompassing BA32 and medial regions of BA9 and BA10. Spheres were used for the striatal and mPFC ROIs because this approach focuses analyses on the striatum and medial regions of BAs 9 and 10 more precisely than atlas-based anatomical masks of those regions (especially for mPFC, which includes medial sections of large prefrontal regions such as BA10). The OFC was defined as BA11 and BA47 with a dilation of 2, and the amygdala was defined using the human PickAtlas label. AlphaSim (http://afni.nimh.nih.gov/afni/) cluster extent thresholds were calculated a priori to determine the minimum functional cluster size necessary to maintain a corrected P < 0.05 across the composite functional mask of all 4 ROIs (cluster extent threshold: 175 voxels) and the secondary functional masks that were generated for the conjunction analyses described below.
Regression analyses were performed in SPM8 to determine whether insomnia scores were associated with reward-related BOLD response in the four ROIs. An initial regression used the mean INS score as the independent variable of interest and a second regression included NIS and NRS as separate independent variables. To adjust for the potential influence of baseline depression, the count of depressive symptoms at study entry (age 9) was included as a covariate. In addition, to adjust for the potential influence of concurrent insomnia symptoms on reward-related BOLD response, a supplementary regression analysis was performed that included mean NIS and NRS scores in late adolescence (ages 16 and 17) as additional covariates. Regression analyses were repeated in SPSS to generate unstandardized regression coefficients (B), standard errors (SE), and effect sizes (R2). To accomplish this, functional masks from SPM regressions of reward response on insomnia scores were saved and used as functional ROIs for main effect t-tests of reward-related BOLD response. Next, main effect beta values for the average BOLD response within each functional mask were extracted using the “eigenvariate” tool in SPM, and regressions were performed in SPSS.
To test the insomnia-reward-depression link, we used conjunction analyses in SPM48 and bootstrap tests of mediation in SPSS.49 Conjunction analyses determined whether depression scores during late adolescence were associated with reward-related neural response in regions that were also associated with early adolescent insomnia scores. To accomplish this, reward-related BOLD response was regressed on the mean depressive symptom count within the insomnia-related functional ROIs described above. Next, mediation analyses were performed in SPSS. To accomplish this, a second set of functional masks was created from SPM regressions of reward response on the mean count of depressive symptoms. These masks were then used as functional ROIs for main effect t-tests of reward-related BOLD response, and main effect beta values for the average BOLD response within each functional mask were extracted from SPM. Finally, insomnia scores in early adolescence (X1) were used to predict depression scores in late adolescence (Y) when reward-related BOLD response was included as a mediator (M) and depression scores at study entry were included as a covariate (X2) using the SPSS PROCESS macro.49 Bootstrap tests of mediation use repeated random sampling (n = 1,000) with replacement to estimate the indirect effect of X on Y.
RESULTS
Reward-Related BOLD Response
ROI and whole-brain results for within-subject t-tests of BOLD response during reward anticipation (reward anticipation > baseline) are available in the supplemental material (Tables S1 and S2). These results confirm that the mPFC, striatum, and OFC had increased response during reward anticipation compared to baseline. The amygdala did not show a significant differential response to reward anticipation versus baseline. Whole-brain results are presented to describe regions that were responsive to reward outside of the pre-defined ROIs.
Association between Insomnia Symptoms and Reward-Related BOLD Response
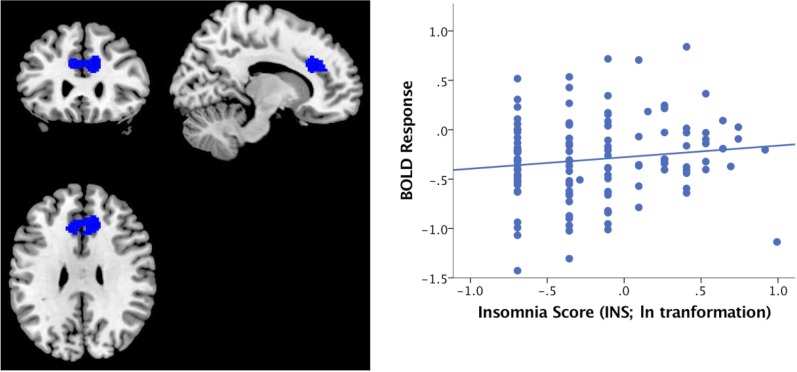
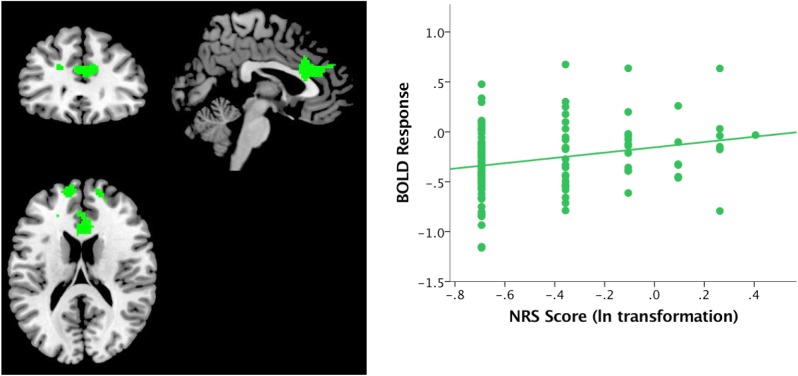
Participants with higher INS scores had greater BOLD response in the dmPFC during anticipation of monetary rewards (BA 8/9/32 cluster size = 585, t120 = 3.41, Pcorrected < 0.05, MNI coordinates of maximum voxel: 12, 28, 30, B = 0.26, SE = 0.09, R2Adjusted = 0.06); see Figure 1. In a second regression with NIS and NRS scores entered as separate predictors, higher NRS scores were associated with greater reward-related BOLD response in the dmPFC (BA 8/9/10/24/32 cluster size = 1366, t 119 = 4.59, Pcorrected < 0.05, MNI coordinates of maximum voxel: 2, 18, 26, B = 0.36, SE = 0.10, R2Adjusted = 0.09), and NIS was not significantly associated with reward-related BOLD response; see Figure 2. The positive association between early adolescent NRS scores and reward-related BOLD response in the dmPFC remained significant after accounting for late adolescent NIS and NRS (see Results in supplemental material).
Figure 1.
Positive association between INS scores during early adolescence and reward-related BOLD response during late adolescence.
Figure 2.
Positive association between NRS scores during early adolescence and reward-related BOLD response during late adolescence.
Association between Reward-Related BOLD Response and Depressive Symptoms
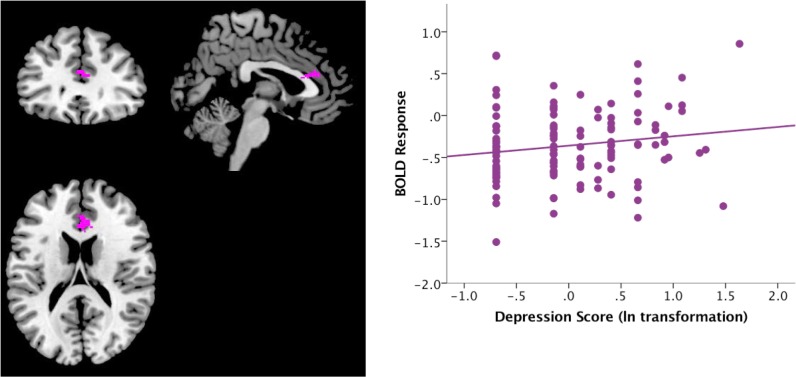
Conjunction analyses indicated that depression scores during late adolescence were not significantly associated with BOLD response during reward anticipation in the dmPFC subregion that was associated with INS scores. However, higher depression scores during late adolescence were associated with greater reward-related BOLD response in the dmPFC subregion that was associated with NRS (BA 32 cluster size = 129, t120 = 3.17, P corrected < 0.05, MNI coordinates of maximum voxel: 2, 32, 18, B = 0.17, SE = 0.07, R2Adjusted = 0.05); see Figure 3. This positive association remained significant after accounting for late adolescent NIS and NRS (see Results in supplemental material).
Figure 3.
Positive association between late adolescent depression scores and reward-related BOLD response in the dmPFC region that was also associated with early adolescent NRS scores.
Mediation of NRS-Depression Association by Reward-Related BOLD Response
NRS scores during early adolescence were positively associated with the depression scores in later adolescence (B = 0.39, R2Adjusted = 0.03, P < 0.05). Bootstrap tests of mediation indicated that greater dmPFC response during reward anticipation significantly mediated the relationship between NRS and non-sleep depressive symptoms (B = 0.09, 95% CI: 0.02, 0.27, P < 0.05). NRS did not have a direct effect on depressive symptoms after accounting for reward anticipation response in the dmPFC (B = −0.03, 95% CI: −0.39, 0.33, P > 0.05), indicating full mediation. Greater dmPFC response during reward anticipation also mediated the relationship between early adolescent NRS and late adolescent non-sleep depressive symptoms after adjusting for late adolescent NIS and NRS (see Results in supplemental material).
DISCUSSION
The results from the current study provide support for a neurobiologically-based developmental model linking earlier insomnia symptoms to later depressive symptoms via reward response in the dmPFC. NRS during early adolescence was associated with increased dmPFC response during anticipation of rewards and more depressive symptoms in later adolescence. Furthermore, dmPFC response mediated the association between NRS and depression, supporting our hypothesis that altered function in this region is a mechanism for the influence of nonrestorative sleep on the development of depression. However, we did not find the anticipated association between NIS and reward-related brain function. Furthermore, while the composite measure of insomnia (INS: NIS+NRS) was positively associated with reward-related BOLD response in a more constrained set of dmPFC regions, reward response in these regions was not significantly associated with depression. Collectively, these results suggest that adolescents with NRS may be especially susceptible to disruptions in neural reward processing and affect.
The link between NRS, increases in reward-related dmPFC response, and increased depressive symptoms is consistent with a recent meta-analytic synthesis of fMRI studies of reward-related processing in depression.43 In addition, the positive association between NRS and reward-related response in the mPFC is somewhat consistent with research by Mullin et al.,32 which demonstrated that sleep deprived young adults had greater reward-related response in the mPFC than participants who were not sleep deprived, though the cluster identified by Mullin was in a more rostral region of the mPFC than the dmPFC cluster identified in the present research. Disruption of the mPFC specifically is consistent with theories that sleep disruption may be particularly detrimental to cortical regions that integrate and regulate arousal and affective processes.22,50 It is also consistent with the proposition from neurodevelopmental theories that the PFC, which continues to mature through the mid-twenties, should be especially sensitive to the effects of adolescent homeostatic stressors such as sleep disturbance.51–56 The dmPFC is postulated to be instrumental in evaluating the self-relevance and social value of rewards,38–40 and increased response in this region may indicate that individuals with NRS compensate for dmPFC disruption by allocating greater resources to evaluating the personal relevance or relative value of potential rewards compared to those without NRS. The association between NRS and reward anticipation response could indicate that NRS disrupts self-relevant affective evaluation when anticipating stimuli typically deemed as rewarding. This interpretation is consistent with dual-process theories of reasoning which postulate that associative and hypothetical reasoning are especially prone to homeostatic stressors.57,58
Notable characteristics of the study sample include the common incidence of insomnia symptoms, particularly NRS, during early adolescence and the decrease in the incidence of MDD between age 9 and later adolescence. While the point prevalence of MDD in the sample at ages 16 and 17 (2.03%) is consistent with the point prevalence of depression in epidemiologic studies of adolescents (3.37% [95% CI: 1.35, 5.39]),59 we expected the prevalence of depression to increase between early and late adolescence, particularly given that half of the PGS-E sample was selected for high levels of depressive symptoms at baseline and the prevalence of depression at age 9 (14.6%) was higher than in the general adolescent population. The slight decrease in the incidence of MDD in this sample could reflect symptom habituation or adaptation to chronic stressors, such as poverty60 or negative parenting experiences,46 during a period of continued neurodevelopment. Despite the potential floor effect of MDD during late adolescence, we found an association between NRS in early adolescence and later depressive symptoms. We were not able to evaluate the association between NRS and clinically significant depression in this study given the low incidence of late adolescent MDD, but this is a key area for future research.
This study has several strengths as well as some limitations. One strength is the large sample size with five years of insomnia symptom assessment prior to the fMRI scan. In combination with the assessments of depressive symptoms at the time of the scan and one-year post-scan, the longitudinal design allowed us to evaluate our mediational model with temporal precedence from NRS to later reward processing to depressive symptoms. Moreover, the link between NRS and later reward processing and depressive symptoms was present after adjusting for depressive symptoms at baseline. However, one limitation of this study is the absence of a baseline assessment of reward processing, therefore, we cannot rule out the possibility that “changes” in neural reward circuitry were at stable levels as a trait or preceded the onset of insomnia symptoms. Cross-lagged models using concurrent measurement of all three constructs—NRS, neural reward processing, and depression—over time and in large samples could be applied in future research to further delineate the direction of these associations.
We also recognize that compromised neural reward processing may result from experiences other than insomnia (e.g., poverty,60 negative parenting experiences,46 stressful life events61,62) and disruptions in reward-related neural response are implicated in multiple forms of psychopathology (e.g., problematic substance use, attention deficit disorder, schizophrenia).63–68 The analyses in the current study tested the a priori hypothesis that neural reward processing would mediate the relationship between insomnia and depressive symptoms, but we did not evaluate whether insomnia symptoms are uniquely associated with neural reward processing and depression after adjusting for other early experiences, psychopathology symptoms, or neural and cognitive processes. One reason for this approach is the large number of potential covariates and the lack of clear justification for their inclusion. Models that incorporate multiple potential moderators (e.g., parenting experiences, stressful life events), mediators (e.g., reward processing, cognitive style), and outcomes (e.g., depression, problematic substance use) are best accomplished by research that has adequate power for covariance structure analysis.
There are also some limitations in our measures of insomnia symptoms and reward processing. The K-SADS is not a standard measure of insomnia and it has not been validated for this purpose. It does, however, assess the four cardinal symptoms of insomnia, and the interview format is consistent with the widespread use of unstandardized interviews to diagnose insomnia. The format allows the interviewer to ask follow-up questions and apply clinical judgment before scoring the symptoms as present or absent. This may be particularly important during adolescence when sleep tends to be short in duration and timed differently on weekdays and weekends.69 For example, adolescents often wake feeling poorly rested because they do not allow themselves enough opportunity for sleep; the interview format of the K-SADS allowed us to assess whether nonrestorative sleep was present even when the participant had sufficient sleep opportunity. However, we cannot rule out the possibility that the NRS reported in this sample was due to insufficient sleep duration or other sleep disorders such as sleep disordered breathing or sleep movement disorders. In addition, NRS was indexed using a single KSADS item and there is ongoing debate as to whether NRS is a symptom of insomnia or a distinct diagnostic entity.34–36 NRS has been included in widely used insomnia diagnostic criteria,1–3 criteria that were applied for the vast majority of studies linking insomnia to depression. Future research linking insomnia to depression should use validated indices of NIS and NRS and attempt to determine whether NIS and NRS have similar34 or differential36 predictive value.
This is the first study to explicitly test the triadic links between insomnia symptoms, neural reward processing, and depressive symptoms in a prospective design. Our results provide preliminary evidence that NRS contributes to depression by altering reward-related dmPFC function. If this pattern of results bears out in subsequent research, it will be worthwhile to consider primary interventions for depression that include screening for NRS and secondary interventions that target sleep disturbance—for example, with cognitive behavioral therapy for insomnia—and hedonic response—for example, with behavioral activation. Providing these interventions to adolescents, particularly in early adolescence, may protect reward-related neural circuitry and decrease the incidence of depression. The application of these interventions with measurement of reward-related neural response would be an exciting area for future research.
DISCLOSURE STATEMENT
This was not an industry supported study. This research was supported by the National Institutes of Health (R01-MH093605, R01-MH66167, R01-MH56630, R01-HD067185, and K01-MH103511). The study sponsor had no role in the design, analysis or interpretation of the study data, the writing of the report, or the decision to submit the manuscript for publication. The authors have indicated no financial conflicts of interest. The work for this study was performed at University of Pittsburgh, Pittsburgh, PA.
ACKNOWLEDGMENTS
The authors thank Rose McAloon and Amy Hoffmann for assistance with data collection, processing, and management while at the University of Pittsburgh. We are also grateful to the families participating in the Learning About Girls' Emotions Study.
REFERENCES
- 1.American Academy of Sleep Medicine. Westchester, IL: American Academy of Sleep Medicine; 2005. The International Classification of Sleep Disorders, 2nd ed.: Diagnostic and coding manual. [Google Scholar]
- 2.American Psychiatric Association. Arlington, VA: American Psychiatric Association; 2000. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. text revision. [Google Scholar]
- 3.Edinger JD, Bonnet MH, Bootzin RR, et al. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27:1567–96. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 4.Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiat. 2005;66:1254–69. doi: 10.4088/jcp.v66n1008. [DOI] [PubMed] [Google Scholar]
- 5.Taylor DJ, Lichstein KL, Durrence HH. Insomnia as a health risk factor. Behav Sleep Med. 2003;1:227–47. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- 6.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 7.Turek FW. Insomnia and depression: if it looks and walks like a duck…. Sleep. 2005;28:1362–3. [PubMed] [Google Scholar]
- 8.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–9. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Manber R, Bernert RA, Suh S, Nowakowski S, Siebern A, Ong JC. CBT for Insomnia in patients with high and low depressive symptom severity: adherence and clinical outcomes. J Clin Sleep Med. 2011;7:645–52. doi: 10.5664/jcsm.1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–95. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fava M, McCall WV, Krystal A, et al. Eszopiclone co-administered with fluoxetine in patients with insomnia coexisting with major depressive disorder. Biol Psychiat. 2006;59:1052–60. doi: 10.1016/j.biopsych.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 12.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSMIV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117:e247–56. doi: 10.1542/peds.2004-2629. [DOI] [PubMed] [Google Scholar]
- 14.Kessler RC, Berglund PA, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiat. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 15.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31:1351–6. [PMC free article] [PubMed] [Google Scholar]
- 16.Ohayon MM, Roberts RE, Zulley J, Smirne S, Priest RG. Prevalence and patterns of problematic sleep among older adolescents. J Am Acad Child Adolesc Psychiat. 2000;39:1549–56. doi: 10.1097/00004583-200012000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Kovacs M. Depressive disorders in childhood: an impressionistic landscape. J Child Psychol Psychiat. 1997;38:287–98. doi: 10.1111/j.1469-7610.1997.tb01513.x. [DOI] [PubMed] [Google Scholar]
- 18.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiat Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Roberts RE, Duong HT. Depression and insomnia among adolescents: a prospective perspective. J Affect Disord. 2013;148:66–71. doi: 10.1016/j.jad.2012.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. J Psychosom Res. 2002;53:561–9. doi: 10.1016/s0022-3999(02)00446-4. [DOI] [PubMed] [Google Scholar]
- 21.Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. 2010;14:227–38. doi: 10.1016/j.smrv.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 22.Dahl RE. The regulation of sleep and arousal: development and psychopathology. Dev Psychopathol. 1996;8:3–27. [Google Scholar]
- 23.Soffer-Dudek N, Sadeh A, Dahl RE, Rosenblat-Stein S. Poor sleep quality predicts deficient emotion information processing over time in early adolescence. Sleep. 2011;34:1499–508. doi: 10.5665/sleep.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van der Helm E, Gujar N, Walker MP. Sleep deprivation impairs the accurate recognition of human emotions. Sleep. 2010;33:335–42. doi: 10.1093/sleep/33.3.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pilcher JJ, Huffcutt AI. Effects of sleep deprivation on performance: a meta-analysis. Sleep. 1996;19:318–26. doi: 10.1093/sleep/19.4.318. [DOI] [PubMed] [Google Scholar]
- 26.Watson D. Mood and Temperament. New York, NY: Guilford Press; 2000. [Google Scholar]
- 27.Fowles DC. A motivational theory of psychopathology. In: Spaulding W, editor. Nebraska Symposium on Motivation: Integrated views of motivation and emotion (Vol. 41) Lincoln, NE: University of Nebraska Press; 1994. pp. 181–238. [PubMed] [Google Scholar]
- 28.Haack M, Mullington J. Sustained sleep restriction reduces emotional and physical well-being. Pain. 2005;119:56–64. doi: 10.1016/j.pain.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 29.Talbot LS, McGlinchey E, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: changes in affect. Emotion. 2010;10:831–41. doi: 10.1037/a0020138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Siegle GJ, Buysse DJ. Relationships between affect, vigilance, and sleepiness following sleep deprivation. J Sleep Res. 2008;17:34–41. doi: 10.1111/j.1365-2869.2008.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holm SM, Forbes EE, Ryan N, Phillips ML, Tarr JA, Dahl RE. Reward-related brain function and sleep in pre/early pubertal and mid/late pubertal adolescents. J Adol Health. 2009;45:326–34. doi: 10.1016/j.jadohealth.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mullin BC, Phillips ML, Siegle GJ, Buysse DJ, Forbes EE, Franzen PL. Sleep deprivation amplifies striatal activation to monetary reward. Psychol Med. 2013;43:2215–25. doi: 10.1017/S0033291712002875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gujar N, Yoo SS, Hu PT, Walker MP. Sleep deprivation amplifies reactivity of brain reward networks, biasing the appraisal of positive emotional experiences. J Neurosci. 2011;31:4466–74. doi: 10.1523/JNEUROSCI.3220-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roth T, Zammit G, Lankford A, et al. Nonrestorative sleep as a distinct component of insomnia. Sleep. 2010;33:449–58. doi: 10.1093/sleep/33.4.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilkinson K, Shapiro C. Nonrestorative sleep: symptom or unique diagnostic entity? Sleep Med. 2012;13:561–9. doi: 10.1016/j.sleep.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 36.Zhang J, Lamers F, Hickie IB, He JP, Feig E, Merikangas KR. Differentiating nonrestorative sleep from nocturnal insomnia symptoms: demographic, clinical, inflammatory, and functional correlates. Sleep. 2013;36:671–9. doi: 10.5665/sleep.2624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berridge KC, Robinson TE. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Rev. 1998;28:309–69. doi: 10.1016/s0165-0173(98)00019-8. [DOI] [PubMed] [Google Scholar]
- 38.Amodio DM, Frith CD. Meeting of minds: the medial frontal cortex and social cognition. Nat Rev Neurosci. 2006;7:268–77. doi: 10.1038/nrn1884. [DOI] [PubMed] [Google Scholar]
- 39.Lemogne C, Delaveau P, Freton M, Guionnet S, Fossati P. Medial prefrontal cortex and the self in major depression. J Affect Disord. 2012;136:e1–11. doi: 10.1016/j.jad.2010.11.034. [DOI] [PubMed] [Google Scholar]
- 40.Etkin A, Egner T, Kalisch R. Emotional processing in anterior cingulate and medial prefrontal cortex. Trends Cogn Sci. 2011;15:85–93. doi: 10.1016/j.tics.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kringelbach ML. The human orbitofrontal cortex: linking reward to hedonic experience. Nat Rev Neurosci. 2005;6:691–702. doi: 10.1038/nrn1747. [DOI] [PubMed] [Google Scholar]
- 42.Baxter MG, Murray EA. The amygdala and reward. Nat Rev Neurosci. 2002;3:563–73. doi: 10.1038/nrn875. [DOI] [PubMed] [Google Scholar]
- 43.Zhang W-N, Chang S-H, Guo L-Y, Zhang K-L, Wang J. The neural correlates of reward-related processing in major depressive disorder: a meta-analysis of functional magnetic resonance imaging studies. J Affect Disord. 2013;151:531–9. doi: 10.1016/j.jad.2013.06.039. [DOI] [PubMed] [Google Scholar]
- 44.Keenan K, Hipwell AE, Chung T, et al. The Pittsburgh Girls Study: overview and initial findings. J Clin Child Adolesc Psychol. 2010;39:506–21. doi: 10.1080/15374416.2010.486320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kaufman J, Birmaher B, Brent DA, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiat. 1997;36:980–8. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 46.Casement MD, Guyer AE, Hipwell AE, et al. Girls' challenging social experiences in early adolescence predict neural response to rewards and depressive symptoms. Dev Cogn Neurosci. 2014;8:18–27. doi: 10.1016/j.dcn.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Siegel JS, Power JD, Dubis JW, et al. Statistical improvements in functional magnetic resonance imaging analyses produced by censoring high-motion data points. Hum Brain Mapp. 2013:1981–96. doi: 10.1002/hbm.22307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nichols T, Brett M, Andersson J, Wager T, Poline J-B. Valid conjunction inference with the minimum statistic. Neuroimage. 2005;25:653–60. doi: 10.1016/j.neuroimage.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 49.Hayes AF. New York, NY: Guilford Press; 2013. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. [Google Scholar]
- 50.Goldstein AN, Walker MP. The role of sleep in emotional brain function. Annu Rev Clin Psychol. 2014;10:679–708. doi: 10.1146/annurev-clinpsy-032813-153716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Forbes EE, Dahl RE. Neural systems of positive affect: relevance to understanding child and adolescent depression? Dev Psychopathol. 2005;17:827–50. doi: 10.1017/S095457940505039X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nelson E, Leibenluft E, McClure EB, Pine DS. The social re-orientation of adolescence: a neuroscience perspective on the process and its relation to psychopathology. Psychol Med. 2005;35:163–74. doi: 10.1017/s0033291704003915. [DOI] [PubMed] [Google Scholar]
- 53.Andersen SL, Teicher MH. Stress, sensitive periods and maturational events in adolescent depression. Trends Neurosci. 2008;31:183–91. doi: 10.1016/j.tins.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 54.Davey CG, Yücel M, Allen NB. The emergence of depression in adolescence: development of the prefrontal cortex and the representation of reward. Neurosci Biobehav Rev. 2008;32:1–19. doi: 10.1016/j.neubiorev.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 55.Arnsten AFT, Rubia K. Neurobiological circuits regulating attention, cognitive control, motivation, and emotion: disruptions in neurodevelopmental psychiatric disorders. J Am Acad Child Adolesc Psychiatry. 2012;51:356–67. doi: 10.1016/j.jaac.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 56.Spear LP. Adolescent neurodevelopment. J Adolesc Health. 2013;52:S7–S13. doi: 10.1016/j.jadohealth.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Evans JSBT. In two minds: dual-process accounts of reasoning. Trends Cogn Sci. 2003;7:454–9. doi: 10.1016/j.tics.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 58.Kahneman D. A perspective on judgment and choice: mapping bounded rationality. Am Psychol. 2003;58:697–720. doi: 10.1037/0003-066X.58.9.697. [DOI] [PubMed] [Google Scholar]
- 59.Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol. 1993;102:133–44. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- 60.Romens SE, Casement MD, McAloon RL, et al. Adolescent girls' neural response to reward mediates the relation between childhood financial disadvantage and depression. J Child Psychol Psychiatry. 2015;56:1177–84. doi: 10.1111/jcpp.12410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Casement MD, Shaw DS, Sitnick S, Musselman SC, Forbes EE. Life stress in adolescence predicts early adult reward-related brain function and alcohol dependence. Soc Cogn Affect Neurosci. 2014;10:416–23. doi: 10.1093/scan/nsu061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dillon DG, Holmes AJ, Birk JL, Brooks N, Lyons-Ruth K, Pizzagalli DA. Childhood adversity is associated with left basal ganglia dysfunction during reward anticipation in adulthood. Biol Psychiatry. 2009;66:206–13. doi: 10.1016/j.biopsych.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wrase J, Schlagenhauf F, Kienast T, et al. Dysfunction of reward processing correlates with alcohol craving in detoxified alcoholics. Neuroimage. 2007;35:787–94. doi: 10.1016/j.neuroimage.2006.11.043. [DOI] [PubMed] [Google Scholar]
- 64.Hasler BP, Sitnick S, Shaw DS, Forbes EE. An altered neural response to reward may contribute to alcohol problems among late adolescents with an evening chronotype. Psychiat Res. 2013;214:357–64. doi: 10.1016/j.pscychresns.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Scheres A, Milham MP, Knutson B, Castellanos FX. Ventral striatal hyporesponsiveness during reward anticipation in attention-deficit/hyperactivity disorder. Biol Psychiat. 2007;61:720–4. doi: 10.1016/j.biopsych.2006.04.042. [DOI] [PubMed] [Google Scholar]
- 66.Strohle A, Stoy M, Wrase J, et al. Reward anticipation and outcomes in adult males with attention-deficit/hyperactivity disorder. Neuroimage. 2008;39:966–72. doi: 10.1016/j.neuroimage.2007.09.044. [DOI] [PubMed] [Google Scholar]
- 67.Simon JJ, Biller A, Walther S, et al. Neural correlates of reward processing in schizophrenia--relationship to apathy and depression. Schizophr Res. 2010;118:154–61. doi: 10.1016/j.schres.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 68.Juckel G, Schlagenhauf F, Koslowski M, et al. Dysfunction of ventral striatal reward prediction in schizophrenia. Neuroimage. 2006;29:409–16. doi: 10.1016/j.neuroimage.2005.07.051. [DOI] [PubMed] [Google Scholar]
- 69.Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21:871–81. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.