Abstract
Exposure science is a holistic concept without prejudice to exposure source. Traditionally, measurements aimed at mitigating environmental exposures have not included exposures in the workplace, instead considering such exposures to be an internal affair between workers and their employers. Similarly, occupational (or industrial) hygiene has not typically accounted for environmental contributions to poor health at work. Many persons spend a significant amount of their lifetime in the workplace, where they maybe exposed to more numerous chemicals at higher levels than elsewhere in their environment. In addition, workplace chemical exposures and other exogenous stressors may increase epigenetic and germline modifications that are passed on to future generations. We provide a brief history of the development of exposure science from its roots in the assessment of workplace exposures, including an appendix where we detail current resources for education and training in exposure science offered through occupational hygiene organizations. We describe existing successful collaborations between occupational and environmental practitioners in the field of exposure science, which may serve as a model for future interactions. Finally, we provide an integrated vision for the field of exposure science, emphasizing interagency collaboration, the need for complete exposure information in epidemiological studies, and the importance of integrating occupational, environmental, and residential assessments. Our goal is to encourage communication and spur additional collaboration between the fields of occupational and environmental exposure assessment. Providing a more comprehensive approach to exposure science is critical to the study of the “exposome”, which conceptualizes the totality of exposures throughout a person’s life, not only chemical, but also from diet, stress, drugs, infection, and so on, and the individual response.
Keywords: education, exposure science, exposure assessment, exposome, risk
DEVELOPMENT OF THE FIELD OF EXPOSURE SCIENCE
The concepts of occupational hygiene, also known as industrial hygiene, date back to Percivall Pott in the 18th century, Ramazzini in the seventeenth century, and Agricola in the sixteenth century, or even further to Pliny the Elder in the first century and perhaps, even earlier than this1, but the application of quantitative exposure science does not have the same long history.2,3 The development of quantitative exposure science was driven by the illnesses and injuries arising from occupation, particularly during the late nineteenth and early twentieth centuries when they became widely recognized and studied. Much of what we consider quantitative exposure science today dates to the rigorous and arduous studies in the 1950s by Oldham and Roach of British mine workers.4–6 These investigators developed methods to directly measure dust concentrations in the breathing zone of workers. They went into the mines to deploy those methods using the concept of repeated, random sampling. At the same time, they recorded job titles and tasks. Thus, they created the first comprehensive job-exposure matrix (JEM). This JEM allowed prediction of risk through statistical modeling while integrating and prioritizing intervention.
From these seminal studies of exposure science grew the modern occupational (industrial) hygiene paradigm of “anticipation, recognition, evaluation, control, and confirmation” of protection from hazards in the workplace. Occupational hygiene has always been responsive to complaints from workers and those responsible for their welfare, an early example being the investigation by the UK government during the early twentieth century of the arsenic production industry in the United Kingdom as a result of complaints from local church parish offices that felt they were supporting persons disabled by work-related injuries.7,8 Since the 1970s, there has been an increased focus on prevention, which led David Fraser, in a 1984 Cummings Memorial lecture at the American Industrial Hygiene Conference,9 to suggest that “… the industrial hygienist is playing in a different kind of ballgame than we knew in the past. He [sic] must now be involved before the material reaches his plant, must understand the process in which the material will be used, have anticipated the worst possible situations and have a game plan to control and eventually dispose of the substance” (italics added). In 1994, Harry Ettinger, then-President of the American Industrial Hygiene Association added “anticipation” to the recognition, evaluation, and control paradigm, to formally encourage the industrial hygiene community to proactively apply its growing body of knowledge and experience. The concept of anticipation impressed Gochfeld10 sufficiently to suggest that it should be accorded higher importance in occupational medicine as well. More recently, “confirm” (with reevaluation as needed) was added to complete the life cycle approach to occupational hygiene.11
A landmark event was the publication in 2002 of a “white paper” on assessment methods by the National Institute for Occupational Safety and Health (NIOSH) National Occupational Research Agenda (NORA) committee on Exposure Assessment, entitled Exposure Assessment Methods: Research Needs and Priorities.12 The “white paper” authors identified 104 research needs and opportunities, which they grouped into four major categories: study design, exposure assessment methods, toxicology, and education. They offered this definition of occupational exposure: “Occupational exposure is the condition of being subjected through employment to a chemical, physical, or biological agent, or to a specific process, practice, behavior, or organization of work.” They further noted: “Exposure is distinguished from dose, but both form part of a continuous process by which an agent reaches a specific receptor site within the body, where it participates in toxic interactions.”
“Exposure Assessment Methods” was subdivided into four parts:
Hazard identification: establishing the existence of a hazard through field observations and/or laboratory analysis of the exposures and/or adverse health effects.
Exposure characterization: describing the qualities of a given environment, such as the magnitude, frequency, duration, and physical properties of an exposure, the potential for contact with the human body, and the toxicity related to its chemical form or physical state.
Exposure evaluation: determining the significance of an exposure relative to known or perceived risks.
Exposure estimation: developing an approximate exposure value for an individual or a statistical distribution of exposure values for groups of workers exposed to similar conditions.
Although the term exposure assessment predates exposure science, they are not identical and exposure science is a wider concept. As recently defined by the National Research Council13, Exposure Science is “the collection and analysis of quantitative and qualitative information needed to understand the nature of contact between receptors (such as people or ecosystems) and physical, chemical, or biologic stressors. Exposure science strives to create a narrative that captures the spatial and temporal dimensions of exposure events with respect to acute and long-term effects on human populations and ecosystems”. The NRC report is organized into a series of major topics for describing the exposure science field:
A vision for exposure science in the twenty-first century: establishing a view for the future where exposure science “…extends from the point of contact between stressor and receptor inward into the organism and outward to the general environment.”;
Applications of exposure science: exploring the “…fundamental role in the development and application of epidemiology, toxicology, and risk assessment… for protecting human and ecosystem health”;
Demands of exposure science: supporting “…policy decisions for managing potentially harmful exposures without adversely affecting economic activities, personal liberties, and the health of people”;
Scientific and technologic advances: developing new technology for “…obtaining reliable estimates of exposures of large populations on multiple scales of space and time… emissions or transformation, products from a source, …locations of receptors (personal or ecosystem), …and activity levels of the receptors.”
Promoting and sustaining public trust in exposure science: developing “…broad public support for gathering information on human and environmental exposures.” and sharing “… values of and expectations for exposure science.”
Realizing the vision: recognizing that “…Embedded in the integrative nature of human and environmental systems… there are no boundaries between organisms (including humans) and their environment or between the internal environment of the human body and the external environment.”
The overall views presented in the NIOSH report of 200212 and the NRC report of 201213 are the underlying framework for the present commentary. Herein, we expand on the major topics listed above by discussing the present relevance of occupational exposure science to future progress in the overall field.
Exposure science as a discipline is at last coming into its own2,3, and those who may have once labeled themselves as practitioners of exposure assessment might rather be referred to as scientists than assessors. Examples of the considerable current resources available for education and training in exposure science offered through occupational hygiene organizations are provided in Appendix 1.
SUCCESSFUL COLLABORATIONS IN EXPOSURE SCIENCE
The majority of people in nearly all communities go to work at some point during their lives (Figure 1). For example, the 2012 employment to population ratio for all persons aged 15 through 64 in the G7 countries was nearly 70%.14 The role of occupational factors in public health ought to be more widely recognized, but occupational hygiene is often considered an internal affair between workers and managers at specific locations. Environmental hygiene (or health) is more expansive, but for many practitioners, environmental concerns do not extend to the workplace. Thus, occupational exposures typically are not included where the general health of populations is being monitored for response to environmental pollutants. Similarly, environmental contributions to poor health at work are not considered in traditional occupational hygiene. The work of occupational hygiene organizations has led to better managed exposures, especially in the developed world. Reduced exposures have resulted in lower rates of diseases associated with occupation. As just a single example, epidemiological studies of viscose rayon workers showed a two- to fivefold excess in mortality from cardiovascular disease (CVD) in workers exposed to carbon disulfide in a 1968 study, whereas reduction in exposure in later years reduced the risk of CVD to those of control groups—that is, the effect on the cardiovascular system was reversible.15 However, chemical exposures in the workplace remain significant because of the many person years spent at work. In addition, workplace exposures may have effects even at lower doses. Toxicologists are recognizing that hormone and hormone-like chemicals may have a disproportionate effect on toxicity at low doses, whereas greater doses may actually blunt the same effects through antagonistic mechanisms.16–19 Exposures to uncontrolled workplace stressors at all life stages can result in reduced fecundity in both males and females through genetic and epigenetic mechanisms. Thus, exposures in the workplace cannot be ignored in a full assessment of community exposures. Numerous studies have focused on occupational cohorts to identify potential risks of workplace exposures, although the “healthy worker effect” (where workers tend to be in better health than the average population) does limit the generalizability of the findings to the community as a whole.20
Figure 1.

A young man near the beginning of his working life at a lead-acid battery recycling facility.
Development of Requirements for Chemical Exposure Information
A central example is the knowledge gap resulting from the introduction of thousands of new chemicals into the market each year. The first use of any of these novel chemicals occurs in the workplace in the manufacture of products. These products are then distributed, sold, and used by customers. The current safety paradigm in the European Union requires the identification and control of exposures resulting from the manufacture, distribution, sale, use, and disposal of products. Hence, the European Union has introduced comprehensive legislation known as REACH, for the Registration, Evaluation, Authorization, and restriction of CHemicals. These regulations have been in force since 1 June 2007, and apply to an estimated 30,000 substances that are manufactured or imported (1 metric tonne or more). An industry must demonstrate that a chemical can be employed safely for a specific use: manufacturers, importers, and (for the first time) downstream users will be required to provide information to end-users to manage risk. Each chemical, along with the corresponding risk assessment, must be registered in a database of European CHemicals Agency (ECHA) in three phases over 11 years.21 To develop risk assessments, two things are necessary: information on toxicity and information on exposure. Models must be used to assess exposure because it would be a monumental task to measure exposures for all chemicals at all stages of a product.22 Various countries in Europe, alone or collaboratively, have been developing models for both rapid (Tier 1) and in-depth (Tier 2) exposure assessments. A sizable task remains to evaluate the effectiveness of these models.23
Inclusion of Exposure Data in the National Health and Nutrition Examination Survey (NHANES)
The evaluation of source–exposure and exposure–disease relationships may be greatly improved by increasing collection and evaluation of biomarker data. NHANES is a major program of the National Center for Health Statistics (NCHS). NCHS is part of the CDC (as is NIOSH) and has the responsibility for producing vital and health statistics for the Nation. NHANES is designed to assess the health and nutritional status of adults and children in the United States. The survey is unique in that it combines interviews and physical examinations. The NHANES program began in the early 1960s and has been conducted as a series of surveys focusing on different population groups or health topics. In 1999, the survey became a continuous program that has a changing focus on a variety of health and nutrition measurements to meet emerging needs. The survey examines a nationally representative sample of about 5000 persons each year. These persons are located in counties across the country, 15 of who are visited each year. Analysis of biological samples is carried out primarily by the National Center for Environmental Health (NCEH). An occupational questionnaire has been part of NHANES for more than a decade. Since 2007, spirometry data and additional questions regarding occupational exposure to dust have been included at the request of investigators from the Division of Respiratory Diseases in NIOSH.
Collaborative Investigations on Exposure to Endocrine Disruptors
The societal demands for exposure data arise from the aspirations of individuals and communities to maintain local environments, personal health, the health of workers, and the global environment. Generally, the focus is on short-term health consequences, especially acute injuries. In addition, there is an increasing need to address health effects of low-level exposures to chemical, biologic, and physical stressors over years or decades. One example is the recognition that certain persistent chemicals can act as disruptors of the endocrine system, and that this disruption may not follow traditionally accepted assumptions of monotonic dose–response relationships.16–18 With respect to low-level exposures to potential endocrine disruptors, a new paradigm for research into exposure assessment and health effects is the consortium-based science model applied to Bisphenol A (BPA).24 This model involves the National Institute of Environmental Health Sciences (NIEHS) and the National Toxicology Program (NTP), and uses NHANES data. NIOSH has undertaken the occupational part of the exposure study. It was considered essential to include occupational exposure because workers who directly handle BPA where it is produced or processed maybe exposed to significantly higher levels of BPA than the general population. The study aims to evaluate the levels of BPA exposure among occupationally exposed people and to identify factors contributing to occupational exposures. The NIEHS/NTP and NIOSH have developed a study protocol to assess the routes and levels of exposure among such workers. In the study, researchers will collect and analyze urine samples, as well as samples of BPA in the air and on workers’ hands during their work shifts. In addition to BPA, the NIEHS has developed a further research consortium aimed at evaluating the health effects of exposure to nanomaterials. This consortium, entitled the Engineered Nanomaterials Grand Opportunity consortium, includes NIOSH.25 These consortia represent a new wave of collaboration in extramural research, often in concert with the intramural efforts at the NIEHS.
Integration of Multiple Fields in the Concept of the Exposome
The “exposome” conceptualizes the totality of environmental exposures throughout a person’s life, including such factors as diet, stress, drug use, and infection.26 The exposome offers an intriguing direction for exposure science in which occupational, environmental, and even residential exposures will have to be considered as part of the mix. Exposure science could follow a bottom-up or a top-down approach. To explore the exposome, it makes sense to employ a top-down approach based on biomonitoring, ideally in addition to a bottom-up approach that samples air, water, food, and so on.26 Nontargeted biomarker research is the epitome of combining occupational and environmental exposure science, as there is no preconception of the origins of the stressors or their downstream preclinical indicators. Blood sampling is the most common approach and that used in NHANES. However, for some biomarkers, simpler and less invasive techniques may be available, including exhaled breath monitoring.27 We note that exposures at vulnerable points in the life stage, for example, childhood or old age, may be more important in the development of disease response than considerably larger exposures during an individual’s working life. In addition, differences in age-related physiology may considerably alter the received dose from an exposure. For example, breathing patterns in the young can substantially alter the penetration and deposition of aerosols in the respiratory tract compared with the breathing patterns of working adults.28 Hence, an integrated vision of exposure science should account for all routes of exposure at all life stages, information that is critical to the concept of the exposome. Lioy and Rappaport29 have recently defined a need for measurements intended to find unknown sources of hazards resulting in disease, which is consistent with the exposome concept. Such measurements would be distinct from measurements intended for traditional exposure assessment/science purposes, such as dose response, risk assessment/management, and source characterization. However, they stress that both approaches have merit. A combination of the two offers particular advantages for both identifying and preventing hazardous exposures, and thereby mitigating diseases.30
AN INTEGRATED VISION OF EXPOSURE SCIENCE
In 2012, the National Research Council issued a report13 entitled “Exposure Science in the 21st Century—A Vision and a Strategy.” In this report, the authors note (Page 31): “Finally, even though occupational settings still dominate exposures to many important stressors in some populations, no effort to integrate them into population exposure-reduction strategies is under way” and it concludes with a key finding that “… an expanded, and integrated vision of exposure science… is needed”. Indeed, an expanded, integrated vision is essential to the greater development of exposure science. Our goal in this article is to encourage communication and spur collaboration between those in the fields of occupational exposure assessment and environmental exposure assessment. Below, and in the associated Figure 2, we offer a number of suggestions to further engender such an integrated approach to exposure science.
Figure 2.
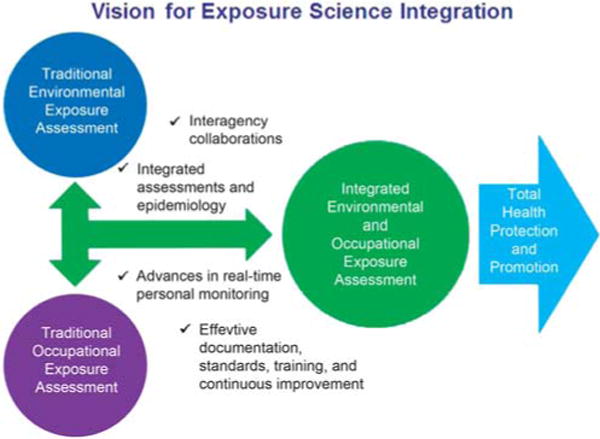
Suggested exposure science opportunities to build and sustain integrated environmental and occupational exposure assessment for total health protection and promotion.
Foster Interagency Collaboration
Budding research collaborations in exposure science need to be supported at all levels by all federal agencies. A successful transagency collaboration is Tox21, a toxicology program that involves EPA, the National Institutes of Health (NIH), and recently the Food and Drug Administration.31,32 NIH, FDA, and CDC are all part of the Department of Health and Human Services (HHS). This agreement between the EPA and HHS for meetings on research collaboration is an initiative coming from the very top of these organizations (Secretary Kathleen Sebelius of HHS; EPA Administrator Gina McCarthy.) Such agreements hold great promise for the future of integrative research and planning. In their report, the NRC committee suggested that Tox21 be extended to exposure science to create Exposure21.13 They stated that “in addition to the engagement of those stakeholders involved in Tox21, engagement of other federal agencies—such as the US Geological Survey, CDC (home of NIOSH, NCHS and NCEH), the National Oceanic and Atmospheric Administration, the National Science Foundation (NSF), and the National Aeronautics and Space Administration—would promote access to and sharing of data and resources on a broader scale.” More recently, a Federal Working Group, Exposure Sciences 21 has been formed. Nearly 25 federal agencies are a part of the working group. The working group is being formed by the Toxics and Risk Subcommittee of the Committee on Environment, Natural Resources, and Sustainability of the National Science and Technology Council. The goal of the working group is to promote federal participation and collaboration in exposure sciences.
Include Exposure Information in Epidemiological Studies
Large, population-based, prospective epidemiologic investigations are potential resources for evaluating health risks of exposures covering both the workplace and external environment. A review of the collection and use of occupational data in funded population-based cardiovascular studies in the United States was conducted recently.33 Most (83%) of the 30 studies reviewed collected some descriptive occupational data. More than half (60%) collected some data on workplace hazards. In 80 publications identified, occupational data were used in analyses, yet most often only as a marker of socioeconomic status. More detailed occupational exposure information would have been desirable. A minimum set of items to include in such epidemiologic studies are: (1) employment status; (2) industry, occupation, and job tenure; (3) job strain and/or effort-reward imbalance; (4) work schedule demands (shift, work hours, work-life conflict); and (5) tobacco smoke exposure.33 Compliance with the use of personal protective equipment is another important component in understanding actual dose. Collaborative opportunities could be further developed to make optimal use of existing prospective data from these population-based studies to address the role of current and emerging workplace exposures in a variety of chronic health conditions.
Integrate Occupational, Environmental, and Residential Assessments
Recently, there have been a number of examples of how occupational, environmental, and residential issues are intertwined. Workers have been and are still exposed to traditional hazards such as radiation, lead, and asbestos. Therefore, consideration of equivalent nonoccupational exposures, such as radiation from granite countertops, lead from casting bullets at home, and asbestos in attic insulation has benefitted from relevant historical occupational perspectives. Workers can bring home hazardous agents, such as lead or asbestos, on their clothing thereby increasing exposures and risks of disease among family members including respiratory problems, neurologic disorders, and fatal poisonings.34 An example of an overlap in assessment is in the Kootenai National Forest surrounding the Superfund site around the former vermiculite mine and processing plant near Libby, MT. Trunks of trees and forest-floor “duff” and soil have been found to be contaminated with fine fibers of amphibole minerals.35 Although it is possible to assess risks to these workers purely from the occupational perspective, the EPA has been engaged in a number of risk screening and removal activities in the area. Forest Service workers are local residents; as a result, their residential, recreational, and occupational environments all contribute to their total exposure. Risk-assessment techniques described in various EPA guidance documents and environmental exposure and risk assessments developed with those techniques may be considered when designing and applying workplace investigation procedures and interpreting results.36
Other situations in which there have been occupational, environmental, and residential exposures include disasters such as the destruction of the World Trade Centers, where asbestos and slag wool insulation as well as dust from concrete, glass, and metals from the collapsed buildings led to exposures of recovery workers, bystanders outside, and homeowners where contamination had been blown into residences through shattered windows. This event highlighted the differences in prevailing paradigms of exposure assessment between the environmental and occupational exposure research communities as reflected in the resulting scientific literature.37,38 The two exposure disciplines have been more comprehensively united on other occasions; for example, when the US Air Force became concerned about jet fuel exposures on military bases, both occupational and environmental (incidental) exposures were studied and documented together and ultimately provided useful case–control contrasts and paths for future study.39,40 In the Gulf of Mexico oil release of 2010, exposures to crude oil and oil dispersing and cleaning products were documented in recovery workers as well as local populations around the Gulf.41 Fracking is an oil and gas recovery operation where occupational exposures, such as to silica sand, have been documented.42 There are also issues such as naturally occurring radioactive material, benzene, and other hydrocarbons in the recovered fluid, and diesel exhaust which may spill over into environmental and residential issues.43 Climate change is something that will affect all people whether at work or not, and further joint research projects are under consideration in this area as well.44
Develop and Deploy Real-Time Personal Monitoring Methods
Exposure science in the future will include tools for real-time personal monitoring. Such a tool is envisioned in the recent challenge from the EPA and HHS (NIEHS) known as “My Air, My Health”.45 Real-time monitoring tools lead to important questions at the interface between environment and occupation. For example, one can imagine a personal diesel exhaust monitor in which nanosensor arrays currently under development46 measure a person’s environmental exposure during their commute to work. But what happens when they arrive at work, to clock-in as a driver at a bus garage? Should workplace diesel exhaust exposure be regarded as somehow different? This interface between occupation and environment is further blurred when the diesel bus driver idles the engine while waiting for school children to be released. Such childhood exposures can greatly exceed ambient levels of diesel particulate and have been linked to asthma and bronchitis in children.47 This example is one of many that can be envisioned and we fervently hope that future exposure assessment will integrate workplace and environmental exposure. However, effective documentation, standards, training, and continuous improvement will be necessary to build and sustain these new capabilities. A major issue is presented by the availability of wearable sensors with displays of real-time information. Although some individuals maybe happy to allow this information to be uploaded and considered remotely by an expert, others will want to comprehend the information and even base decisions on it. Thus, it may become necessary to consider the education of workers and other citizens, who may not be expert in the interpretation of risk from real-time exposure measurements, which maybe difficult in the absence of widely accepted protocols among experts. NIOSH is at the forefront of tackling this issue as a part of the development and evaluation of a real-time Personal Dust Monitor for use by miners48 and data interpretation is also a focus of both the NIOSH direct-reading exposure assessment methods and EPA air sensors and health initiatives.
CONCLUSION
In this evolving discipline of exposure science, occupational and environmental exposures should be considered as integrative through first principle and not as an afterthought. In many areas, practitioners are already recognizing and capitalizing on the value of this paradigm, and the ideas and opportunities presented in this article can serve as a model to help advance it further. It is necessary also to acknowledge the challenges of integration, which include the potential to confuse issues with consequent impact on prioritization of responses.
Acknowledgments
Thanks to Dr. Cecil “Buzz” Birchfiel (NIOSH) for his input on cardiovascular mortality studies. We thank Dr. Meg Bouvier for assistance in preparing this manuscript and Dr. Leigh Cash (Los Alamos National Laboratory), Dr. Gayle DeBord (NIOSH), and Dr. John Decker (NIOSH) for review and comments.
APPENDIX 1
Occupationally Based Educational Resources in Exposure Science
National Institute for Occupational Safety and Health (NIOSH)
Through the Occupational Safety and Health Act of 1970, NIOSH was established separately from the Occupational Safety and Health Administration under the Department of Health, Safety, and Welfare, now Health and Human Services (HHS). NIOSH is one of the Institutes in the Centers for Disease Control and Prevention (CDC). The mission of NIOSH is to produce new scientific knowledge and provide practical solutions vital to reducing risks of injury and death in traditional industries, such as agriculture, construction, and mining. NIOSH also supports research to predict, prevent, and address emerging problems that arise from dramatic changes in the twenty-first century workplace and workforce. NIOSH partners with diverse stakeholders to study how worker injuries, illnesses, and deaths occur. NIOSH scientists design, conduct, and support targeted research, both inside and outside the institute. NIOSH and its partners support the U.S. economic strength and growth by moving research into practice through concrete and practical solutions, recommendations, and interventions for the building of a healthy, safe and capable workforce. NIOSH supports the training of occupational health and safety professionals to build capacity and meet increasing needs for a new generation of skilled practitioners, supporting academic institutions through an extramural program that includes Training Program Grants, funding for Education and Research Centers and Agricultural Centers, and grants to individual investigators. All NIOSH training courses contain an exposure assessment component, even though the word “exposure” may not be explicit in the course title. NIOSH also has extensive resources based on its publications, available through the NIOSHTIC-2 database, for example, “A Manual for Occupational Exposure Sampling Strategy”,49 which is currently under revision.
American Industrial Hygiene Association (AIHA)
Within the occupational hygiene community, exposure assessment has formed the core of managing exposures in the workplace.50 A balanced and logical approach for examining the collective exposures in the workplace environment was initially outlined with the first edition of “A Strategy for Occupational Exposure Assessment” published in 1991.51 Updated in the second edition in 2000, it was quickly followed by a progression of Professional Development Courses (PDCs) created and offered by members of the AIHA. These PDCs on occupational exposure assessment were offered as face-to-face training at national association events, and later in more current formats, such as video broadcast, webinars, and electronic file sharing. At present, AIHA offers a formal progression of coursework built on the model of exposures management as promoted in the 3rd edition, retitled “Assessing and Managing Occupational Exposures”. Its goal is to abate harmful exposures and focuses on a ranking scheme that prioritizes limited and valuable resources, with subsequent investigation of lower-ranked (but highly uncertain) exposures. Additional courses guide the practitioner through more advanced concepts of statistical theory, use of Bayesian decision making, and tools with which to further inform and defend professional judgments. A listing of relevant PDC offerings is available from the AIHA Exposure Assessment Strategies Committee website under the heading “Exposure Assessment Strategies PDCs”.52
National Institute of Environmental Health Sciences (NIEHS)
For the past 19 years, NIEHS, in cooperation with 20 grant awardees, has designed and administered the Worker Education Training Program (WETP). This innovative program is designed to help employers meet the Occupational Safety and Health Administration (OSHA) requirements under the Hazardous Waste Operation and Emergency Response regulations (CFR 1910.120). By encouraging training for difficult-to-reach populations, the program addresses issues associated with literacy, language, and unique aspects of adult education. WETP was instrumental in training workers during the response to the World Trade Center attacks, hurricanes Katrina and Rita, the Gulf Oil Spill, and Superstorm Sandy. Details of the WETP training programs are available online.53
International Occupational Hygiene Association (IOHA)
The international occupational health community has also collaborated to share content. Thirteen member societies of the IOHA, all 11 national certification bodies, and IOHA itself are now cooperating in a new international training and qualification system. The structure broadens access to occupational hygiene education and training worldwide and complements existing professional accreditation schemes. Currently, there are 46 training providers approved in the scheme. As of the end of June 2013, almost 200 courses had been delivered in more than 32 countries, with nearly 2400 examinations taken in seven languages.54 This engagement of students, particularly in developing countries, helps address the worldwide need to combat occupational illness. It is creating the foundation for sustainable growth in the provision of occupational hygiene services worldwide. Aylesbury and Bailey were instrumental in bringing together a group of senior hygienists to review the needs of industry. The resulting position paper55, reflecting the perspective of major multinational companies, resulted from widespread consultation with a diverse group of global stakeholders. The Occupational Hygiene Training Association (OHTA), a not-for-profit organization, was created to operate the system. Complete lesson plans, student handouts, and presentation materials cover conventional topics such as occupational health and principles and application of the hierarchy of controls. They also cover specialty programs such as asbestos and fiber exposures, noise, heat stress, and ergonomics. The OH learning website provides free downloads of educational materials and details of training events (http://www.ohlearning.com/).
Footnotes
The authors declare no conflict of interest
CONFLICT OF INTEREST
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry. This work was reviewed by the U.S. EPA and approved for publication.
References
- 1.Harper M. The possible toxic metal exposures of pre-historic bronze workers. Br J Ind Med. 1987;44:652–656. doi: 10.1136/oem.44.10.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lioy PJ. Exposure science: a view of the past and milestones for the future. Environ Health Perspect. 2010;118:1081–1090. doi: 10.1289/ehp.0901634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pleil JD, Blount BC, Waidyanatha S, Harper M. Establishing exposure science as a distinct scientific discipline. J Expo Sci Environ Epidemiol. 2012;22:317–319. doi: 10.1038/jes.2012.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oldham PD, Roach SA. A sampling procedure for measuring industrial dust exposure. Br J Ind Med. 1952;9:112–119. doi: 10.1136/oem.9.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oldham PD. The nature of the variability of dust concentrations at the coal-face. Br J Ind Med. 1953;10:227–234. doi: 10.1136/oem.10.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roach SA. A method of relating the incidence of pneumoconiosis to airborne dust exposure. Br J Ind Med. 1953;10:220–226. doi: 10.1136/oem.10.4.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harper M. Occupational health aspects of the arsenic extractive industry in Great Britain (1868–1925) Br J Ind Med. 1988;45:602–605. doi: 10.1136/oem.45.9.602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harper M, Pössel Miranda G. Management of health risks in the arsenic production industry. Ann Occup Hyg. 1990;34:471–482. doi: 10.1093/annhyg/34.5.471. [DOI] [PubMed] [Google Scholar]
- 9.Fraser DA. Recognition, evaluation and control: the acceleration of the process. Am Ind Hyg Assoc J. 1984;45:573–576. doi: 10.1080/15298668491400296. [DOI] [PubMed] [Google Scholar]
- 10.Gochfeld M. Chronological history of occupational medicine. J Occup Environ Med. 2005;47:96–114. doi: 10.1097/01.jom.0000152917.03649.0e. [DOI] [PubMed] [Google Scholar]
- 11.Hoover MD, Armstrong T, Blodgett T, Fleeger AK, Logan PW, McArthur B, et al. Leadership perspective. Confirming our IH decision-making framework Synergist. 2011;22:10. [Google Scholar]
- 12.National Institute for Occupational Safety and Health (NIOSH) Exposure Assessment Methods: Research Needs and Priorities. NIOSH; Cincinnati (OH): 2002. (Publication No. 2002-126). [Google Scholar]
- 13.National Research Council. Exposure Science in the 21st Century: A Vision and a Strategy. National Academies Press; Washington (DC): 2012. p. 196. [PubMed] [Google Scholar]
- 14.Organization for Economic Cooperation and Development (OECD) OECD StatExtracts. Available at http://stats.oecd.org/Index.aspx?DatasetCode=LFS_SEXAGE_I_R. (accessed on 21 March 2014)
- 15.Benowitz NL. Cardiotoxicity in the workplace. State Art Rev Occup Med. 1992;7:465–478. [PubMed] [Google Scholar]
- 16.EPA. Endocrine Disruptor Research: State-of-the-Science Non-Monotonic Dose Response Curve Report – Low Dose Effects. US Environmental Protection Agency; 2013. Available at http://epa.gov/ncct/edr/non-monotonic.html. (accessed on 21 March 2014) [Google Scholar]
- 17.Genovese G, Reguira M, Da Cuña RH, Ferreira MF, Varela ML, Lo Nostro FL. Nonmonotonic response of vitellogenin and estrogen receptor α gene expression after octylphenol exposure of Cichlasoma dimerus (Perciformes, Cichlidae) Aquatic Toxicol. 2014;156:30–40. doi: 10.1016/j.aquatox.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 18.Liang Q, Gao X, Chen Y, Hong K, Wang H-S. Cellular mechanism of the non-monotonic dose response of Bisphenol A in rat cardiac myocytes. Environ Health Perspect. 2014;122:601–608. doi: 10.1289/ehp.1307491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ball E. Birnbaum presents plenary at meeting of Canadian toxicology group. [Internet] Environmental Factor. Available at http://www.niehs.nih.gov/news/newsletter/2014/1/spotlight-birnbaum/index.htm. (accessed on 1 April 2014)
- 20.Li C-Y, Sung F-C. A review of the healthy worker effect in occupational epidemiology. Occup Med. 1999;49:225–229. doi: 10.1093/occmed/49.4.225. [DOI] [PubMed] [Google Scholar]
- 21.European Chemicals Agency. Guidance on information requirements and chemical safety assessment. Chapter R.14: Occupational exposure estimation. ECHA-2010-G-09-EN Vers. 2.1. Nov, 2012. European Chemicals Agency; Helsinki, Finland: 2014. Available at http://echa.europa.eu/documents/10162/13632/information_requirements_r14_en.pdf. (accessed on 21 March 2014) [Google Scholar]
- 22.Tielemans E, Warren N, Schneider T, Tischer M, Ritchie P, Goede H, et al. Tools for regulatory assessment of occupational exposure – development and challenges. J Exp Sci Environ Epidemiol. 2007;17:S72–S80. doi: 10.1038/sj.jes.7500604. [DOI] [PubMed] [Google Scholar]
- 23.The ETEAM-project. Available at http://www.eteam-project.eu/. (accessed on 3 December 2014)
- 24.Birnbaum LS, Bucher JR, Collman GW, Zeldin DC, Johnson AF, Schug TT, et al. Consortium-based science: The NIEHS’s multipronged, collaborative approach to assessing the health effects of bisphenol A. Environ Health Perspect. 2012;120:1640–1644. doi: 10.1289/ehp.1205330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schug TT, Nadadur SS, Johnson AF, Nano GO. Consortium – a team science approach to assess engineered nanomaterials: reliable assays and methods. Environ Health Perspect. 2013;121:A176–A177. doi: 10.1289/ehp.1306866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rappaport SM. Implications of the exposome for exposure science. J Exp Sci Environ Epidemiol. 2011;21:5–9. doi: 10.1038/jes.2010.50. [DOI] [PubMed] [Google Scholar]
- 27.Pleil JD, Stiegel MA. Evolution of environmental exposure science: using breath-borne biomarkers for “discovery” of the human exposome. Anal Chem. 2013;85:9984–9990. doi: 10.1021/ac402306f. [DOI] [PubMed] [Google Scholar]
- 28.Brown JS, Gordon T, Price O, Asgharian B. Thoracic and respirable particle definitions for human health risk assessment. Particle Fibre Toxicol. 2013;10:12. doi: 10.1186/1743-8977-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lioy PJ, Rappaport SM. Exposure science and the exposome: an opportunity for coherence in the environmental health sciences. Environ Health Perspect. 2011;119:A466–A467. doi: 10.1289/ehp.1104387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rappaport SM, Lioy PJ. An integrated approach to the exposome: Rappaport and Lioy respond. Environ Health Perspect. 2012;120:A104. doi: 10.1289/ehp.1104719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Collins FS, Gray GM, Bucher JR. Transforming environmental health protection. Science. 2008;319:906–907. doi: 10.1126/science.1154619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schmidt CW. TOX21: new dimensions of toxicity testing. Environ Health Perspect. 2009;117:A348–A353. doi: 10.1289/ehp.117-a348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MacDonald LA, Cohen A, Baron S, Burchfiel CM. Occupation as socioeconomic status or environmental exposure? A survey of practice among population-based cardiovascular studies in the United States. Am J Epidemiol. 2009;169:1411–1421. doi: 10.1093/aje/kwp082. [DOI] [PubMed] [Google Scholar]
- 34.National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention. Report to Congress on Workers’ Home Contamination Study Conducted Under the Workers’ Family Protection Act (29 U.S.C. 671a) NIOSH; Cincinnati, OH, USA: 1995. (Publication 95-123). Available at http://www.cdc.gov/niosh/pdfs/95-123.pdf. (accessed on 3 December 2014) [Google Scholar]
- 35.Hart J, Spear T, Ward T, Baldwin C, Salo M, Elashheb M. An evaluation of potential occupational exposure to asbestiform amphiboles near a former vermiculite mine. J Environ Public Health. 2009:10. doi: 10.1155/2009/189509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harper M, Butler C, Berry D, Wroble J. Where occupation and environment overlap: US Forest Service worker exposure to Libby Amphibole fibers. J Occup Environ Hyg. 2015 doi: 10.1080/15459624.2014.989362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lorber MN, Gibb H, Grant L, Pinto J, Pleil JD, Cleverly D. Assessment of inhalation exposures and potential health risks that resulted from the collapse of the World Trade Center towers. Risk Anal. 2007;27:1203–1221. doi: 10.1111/j.1539-6924.2007.00956.x. [DOI] [PubMed] [Google Scholar]
- 38.Prezant DJ, Weiden M, Banauch GI, McGuiness G, Rom WN, Aldrich TK, et al. Cough and bronchial responsiveness in firefighters at the World Trade Center site. N Engl J Med. 2002;347:806–815. doi: 10.1056/NEJMoa021300. [DOI] [PubMed] [Google Scholar]
- 39.Pleil JD, Smith LB, Zelnick SD. Personal exposure to JP-8 jet fuel and exhaust at Air Force bases. Environ Health Perspect. 2000;108:183–192. doi: 10.1289/ehp.00108183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zeiger E, Smith L. The First International Conference on the Environmental Health and Safety of Jet Fuel. Environ Health Perspect. 1998;106:763–764. doi: 10.1289/ehp.98106763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kitt MM, Decker JA, Delaney L, Funk R, Halpin J, Tepper A, et al. Protecting workers in large-scale emergency responses: NIOSH experience in the Deepwater Horizon response. J Occup Environ Med. 2011;53:711–715. doi: 10.1097/JOM.0b013e31822543b6. [DOI] [PubMed] [Google Scholar]
- 42.Esswein E, Kiefer M, Snawder J, Breitenstein M. Worker exposure to crystalline silica during hydraulic fracturing. 2012 doi: 10.1080/15459624.2013.788352. Available at http://blogs.cdc.gov/niosh-science-blog/2012/05/23/silica-fracking/. (accessed on 1 April 2014) [DOI] [PubMed]
- 43.Howarth RW, Ingraffea A, Engelder T. Natural gas: should fracking stop? Nature. 2011;477:271–275. doi: 10.1038/477271a. [DOI] [PubMed] [Google Scholar]
- 44.Schulte PA, Chun H. Climate change and occupational safety and health: establishing a preliminary framework. J Occup Environ Hyg. 2009;6:542–554. doi: 10.1080/15459620903066008. [DOI] [PubMed] [Google Scholar]
- 45.US Environmental Protection Agency. My Air, My Health: HHS/EPA Challenge. [Internet]. Available at http://epa.gov/research/challenges/. (accessed on 3 December 2014)
- 46.Mulchandani A, Myung NV, Deshusses MA, Cocker D, Wang J, Bakkaloglu B, et al. Nanosensor array for real-time monitoring of diesel and gasoline exhaust exposure. Epidemiol. 2008;19:S62. [Google Scholar]
- 47.Public Health Institute. Asthma and Diesel. PHI; Oakland, CA: 2014. Available at http://www.phi.org/uploads/application/files/xq1rssien18tmqtavs3k97m6ojp-p6reyhgmy3ajnh9jhcjy93r.pdf. (accessed on 21 March 2014) [Google Scholar]
- 48.Peters RH, Vaught C, Hall EE, Volkwein JC. Miners’ Views About Personal Dust Monitors. National Institute for Occupational Safety and Health (NIOSH); Pittsburgh, PA, USA: 2014. p. 47. (Information Circular 9501. DHHS (NIOSH) Publication No. 2008-110, 2008). 47 pp. Available at http://www.cdc.gov/niosh/mining/UserFiles/works/pdfs/2008-110.pdf. (accessed on 19 March 2014) [Google Scholar]
- 49.Leidel NA, Busch KA, Lynch JR. Occupational Exposure Sampling Strategy Manual. DHEW/NIOSH; Cincinnati, OH, USA: 2014. (Publication 77-173). Available at http://www.cdc.gov/niosh/docs/77-173/pdfs/77-173.pdf (accessed on 18 March 2014) [Google Scholar]
- 50.Ignacio L, Bullock WH. A Strategy for Assessing and Managing Occupational Exposures. 3rd. American Industrial Hygiene Association; Fairfax, VA, USA: 2006. [Google Scholar]
- 51.Hawkins NC, Norwood SK, Rock JC. A Strategy for Occupational Exposure Assessment. 1st. American Industrial Hygiene Association Press; Akron, OH, USA: 1991. [Google Scholar]
- 52.American Industrial Hygiene Association Exposure Assessment Strategies Committee. 2014 https://www.aiha.org/get-involved/VolunteerGroups/Pages/Exposure-Assessment-Strategies-Committee.aspx. (accessed on 3 December 2014)
- 53.National Institute for Environmental Health Sciences (NIEHS) About Worker Education and Training Program. 2014 http://www.niehs.nih.gov/careers/hazmat/about_wetp/. (accessed on 3 December 2014)
- 54.Alesbury RJ, Bailey SR. Addressing the needs for international training, qualifications, and career development in occupational hygiene. Ann Occup Hyg. 2014;58:140–151. doi: 10.1093/annhyg/met068. [DOI] [PubMed] [Google Scholar]
- 55.Alesbury RJ, Bailey SR, Bianchi A, Booher L, Burgess L, Dobbie J. Discussion paper on industry needs for occupational hygiene. 2006 Available at http://www.ohlearning.com/community/files/Discussion%20Paper%20on%20Industry%20Needs%20for%20Occupational%20Hygiene%20Final_1.doc. (accessed on 3 December 2014)


