Abstract
Purpose: Syndemics, or the co-occurrence and interaction of health problems, have been examined extensively among young men who have sex with men, but their existence remain unexamined, to our knowledge, among sexual-minority (i.e., lesbian, gay, and bisexual) women. Thus, we investigated if syndemics were present among young sexual-minority women, and if sexual-orientation discrimination was an independent variable of syndemic production.
Methods: A total of 467 sexual-minority women between the ages of 18 and 24 completed a cross-sectional online survey regarding their substance use, mental health, sexual behaviors, height, weight, and experiences of discrimination. We used structural equation modeling to investigate the presence of syndemics and their relationship to sexual-orientation discrimination.
Results: Heavy episodic drinking, marijuana use, ecstasy use, hallucinogen use, depressive symptoms, multiple sexual partners, and history of sexually transmitted infections (STIs) comprised syndemics in this population (chi-square=24.989, P=.201; comparative fit index [CFI]=0.946; root mean square error of approximation [RMSEA]=0.023). Sexual-orientation discrimination is significantly and positively associated with the latent syndemic variable (unstandardized coefficient=0.095, P<.05), and this model fit the data well (chi-square=33.558, P=.059; CFI=0.914; RMSEA=0.029). The reverse causal model showed syndemics is not an independent variable of sexual-orientation discrimination (unstandardized coefficient=0.602, P>.05).
Conclusions: Syndemics appear to be present and associated with sexual-orientation discrimination among young sexual-minority women. Interventions aimed at reducing discrimination or increasing healthy coping may help reduce substance use, depressive symptoms, and sexual risk behaviors in this population.
Key words: : depressive symptoms, discrimination, sexual-minority women, sexually transmitted infections, substance use
Introduction
Young sexual-minority women (YSMW; including lesbians, gays, and bisexuals, and women with same-sex behaviors, attractions or relationships) are disproportionately burdened by a variety of mental and physical health problems.1–17 Multiple studies of adolescents demonstrate that YSMW are at greater risk for depression, smoking, heavy episodic drinking, and other illicit drug use compared to their heterosexual counterparts.2–9 Additionally, YSMW are at least as likely as heterosexual women to engage in risky sexual behavior and acquire sexually transmitted infections (STIs).10–14 Research also consistently finds that, compared to heterosexuals, sexual-minority women are at higher risk of overweight and obesity,15 and these weight disparities begin in adolescence and early adulthood.16,17
These disparate health problems and risk behaviors among YSMW are likely interrelated, as they are often found to interact or co-occur with each other in other populations. In the general population, for example, both depression and heavy alcohol use have positive relationships with obesity.18–21 Depression and substance use are also associated morbidities among youth; notably, these relationships are stronger for girls than boys,22 and among boys, are stronger for sexual-minority individuals than heterosexuals.23 Research on the co-occurrences of multiple health disparities among YSMW is limited. However, studies show depression and substance use are associated with sexual risk behaviors among YSMW,24 and depression is prospectively associated with alcohol use.25 Thus, existing empirical evidence suggests that these disparate health problems are not unrelated, but likely co-occur among YSMW.
Syndemics theory offers a holistic approach to investigating the aforementioned epidemics that disproportionately burden YSMW. Counter to traditional biomedical approaches examining a single health problem or disease, syndemics theory aims to characterize how multiple health problems co-occur and interact—forming a syndemic that exacerbates overall well-being in a population.26,27 For example, among young and adult sexual-minority men, empirical investigations show how co-occurring health problems and risk behaviors, like depressive symptoms and substance use, explain differences in HIV serostatus and risk behaviors.27,28 Syndemics can consist of “somewhat different components, correlates, and expressions across different places and populations.”29 Because there is no research, to our knowledge, about the existence of syndemics among YSMW, a first step is to examine the relatedness, or co-occurrences, of health problems more prevalent among YSMW than heterosexuals.
Another important component of syndemics theory is elucidating how sociocultural mechanisms (e.g., adversity, marginalization) produce and perpetuate co-occurring epidemics within certain populations. One sociocultural phenomenon salient to the lives of YSMW is sexuality-related discrimination. As a group, sexual-minority people report significant levels of discrimination,30 and sexual-minority women report greater levels of everyday and lifetime discrimination than other women.31 Furthermore, the limited body of research on sexual-orientation discrimination indicates that sexual-minority individuals' exposure to discrimination is positively correlated with mental health problems and substance use disorders.30–33 For sexual-minority men, studies show how experiences of sexual-orientation discrimination throughout the life-course are positively related to syndemics.34,35 Because young sexual-minority men and women report experiencing similar stressors (e.g., sexual-orientation discrimination) and similar health disparities (e.g., mental health problems, substance use), there is evidence to suggest that, if syndemics are present among YSMW, sexual-orientation discrimination is a significant correlate of syndemics.
This study investigated syndemics in a population of YSMW. First, we examined if syndemics were present and comprised of the most concerning and disparate health problems and behaviors experienced by YSMW. Second, we tested if sexual-orientation discrimination was associated with syndemics.
Methods
Study design and population
The current investigation uses data from a cross-sectional online survey conducted in 2011 (the Michigan Smoking and Sexuality Study [MSASS]; henceforth referred to as “Parent Study”). The Parent Study included women 18–24 years old who identified as a sexual minority (i.e., lesbian, bisexual, queer, or something else other than heterosexual/straight) or who had sexual experiences with a woman in the past year. However, since the current investigation examines sexual-orientation discrimination, we restricted analyses to women who self-identified as a sexual minority (i.e., reported a non-heterosexual identity), as those who have had sexual experiences with women but do not identify as a sexual minority may not face the same type of social stressors as self-identified YSMW.36 The Parent Study invited participants to complete the web-survey using multiple forums, including Facebook ads and peer referral. Recruitment efforts were focused largely in Michigan, but did not require Michigan residence. Thus, half the sample currently resided in Michigan, while the second half lived in other states. Recruitment methods are described in detail by Johns et al. (2013) in the American Journal of Community Psychology.37 To reduce biases attributable to fraud and/or duplication during online data collection, the Parent Study used best practices38 to remove duplicates and falsified entries from the final sample. Study data were protected by a Certificate of Confidentiality. All study procedures were approved by the University of Michigan Institutional Review Board.
Measures and Variables
Demographics
Women were asked questions about their age, race/ethnicity, neighborhood type (i.e., urban, rural, suburban, other), and highest education attained. Women were asked to report their sexual identity/identities from a checklist: heterosexual; lesbian or gay; bisexual; queer; other; or, “I don't use a label.” For women who reported more than one identity, we asked them to select a primary identity using the following item: “If you had to pick one of the above labels to best represent the way you think about yourself, which would it be? Heterosexual; Lesbian or Gay; Bisexual; Queer; Other; No Label.” Heterosexuals were removed from this analysis, and we collapsed participants who selected “Queer,” “Other,” and “No Label” into a single category titled “Other.”
Health problems and behaviors
We examined 11 health behaviors, symptoms, and problems disproportionately experienced among YSMW. Heavy episodic drinking was measured with the question, “Think back over the last two weeks. How many times have you had five or more drinks in a row?”39 We dichotomized this variable as any versus no heavy episodic use. Cigarette smoking was asked with the question, “Do you now smoke cigarette every day, some days, or not at all?” We dichotomized this variable as any smoking (Every Day or Some Days) versus no smoking (Not At All).
Individual questions asked about 30-day use of marijuana, ecstasy, hallucinogens, cocaine, methamphetamines, ketamine, gamma-hydroxybutyrate (GHB), crack, heroin, and pharmaceutical drugs not prescribed to them by a physician. From these items, we created five dichotomous drug use variables: marijuana use; ecstasy use; hallucinogen use; other illicit drug use (this was aggregated because the numbers of participants who reported using each individual drug were small [n's ranged from 1 to 10]); and prescription drug misuse.
Depressive symptoms were collected via the 10-item Center for Epidemiology Studies Short Depression Scale (CES-D 10).40 We used depressive symptoms as a continuous variable, ranging from 0 to 26 in our sample. Higher scores indicated more depressive symptoms (α=0.73).
Women were asked individual questions about oral, vaginal, or anal sex with specific partners (i.e., women, men, transgender men, and transgender women). Participants who reported having sex with two or more partners in the past 30 days were coded as having multiple sexual partners. Participants were also asked, “Have you ever been told by a medical person that you had a sexually transmitted disease (STD) such as gonorrhea (GC, “clap”), syphilis, Chlamydia, genital warts, HPV, herpes, or hepatitis B?” Response options were dichotomous (Yes/No) for any STI.
To examine overweight/obesity, participants reported their height (in feet and inches) and weight (in pounds). We calculated body mass index (BMI; defined as weight in kilograms divided by the square of height in meters), and used a predetermined cutoff points of 25 and higher to categorize respondents as overweight/obese.41
Sexual-orientation discrimination
Multiple items assessed sexual-orientation discrimination. Past-month discrimination was measured using questions adapted from an experiences of racial discrimination scale to include experiences of discrimination based on sexual orientation.42 Nine questions asked about whether or not they had encountered specific instances of discrimination in the past 30 days. If participants responded affirmatively to an item, they were asked if they perceived this to be related to their sexual orientation or other characteristics (e.g., gender, race/ethnicity, age). We summed all items that participants deemed the oppressive act was due to their sexual orientation. Scores ranged from 0 to 8, with higher scores indicating more discrimination. Past-year discrimination was measured with the following question, “People sometimes feel they are discriminated against or treated badly by other people. In the past 12 months, have you felt discriminated against because someone thought you were gay, lesbian, bisexual, or transgender?”43 Response options were dichotomous as “Yes/No.”
Data analysis
Descriptive statistics described sociodemographics, health problems, health behaviors, and sexual-orientation discrimination for the whole analytic sample. We used Pearson correlation coefficients and tests to examine bivariate associations for health problems, behaviors, and discrimination. Descriptive analyses were conducted in SAS 9.3 (Cary, NC).
Structural equation models were fit to investigate our primary research questions in a two-step model building approach. First, we examined which health problems and behaviors, if any, comprised a single latent syndemic variable. In the second step, we tested if sexual-orientation discrimination was a correlate of the syndemic latent variable. Maximum likelihood estimation with robust adjustment was used to investigate all models because data were multivariate non-normal because of the inclusion of multiple dichotomous variables.44 Model fit was assessed using several statistics appropriate for multivariate non-normal data, including Satorra-Bentler Chi-square tests, Comparative Fit Index (CFI), and Root Mean Square Error of Approximation (RMSEA).45,46 We considered CFIs greater than or equal to 0.9 and RMSEAs less than or equal to 0.6 to be a good fit of the data.46 To compare subsequent steps of our model building process, we used Satorra-Bentler chi-square model comparison tests.47 Structural equation modeling was conducted in EQS 6.2 (Encino, CA).
A total of 14 participants were excluded from the present investigation: five participants identified as heterosexual; one did not answer the race/ethnicity question; and eight did not complete the depressive symptoms questions. The final analytic sample size was n=467 (97.1% of participants who completed surveys).
Results
Table 1 summarizes the demographic characteristics of the analytic sample, as well as the prevalence of health problems, health behaviors, and sexual-orientation discrimination.
Table 1.
Sociodemographic Characteristics, Psychosocial and Physical Health Problems, and Sexual-Orientation Discrimination Among Young Sexual-Minority Women (n=467)
| Total | ||
|---|---|---|
| n | % | |
| Sociodemographic characteristics | ||
| Sexual Orientation | ||
| Lesbian | 258 | 55.2% |
| Bisexual | 155 | 33.2% |
| Other | 54 | 11.6% |
| Race/Ethnicity | ||
| White/European American | 326 | 69.8% |
| Black/African American | 54 | 11.6% |
| Latina/Hispanic | 29 | 6.2% |
| Mixed/Other | 58 | 12.4% |
| Age, mean (standard deviation) | 21.4 | (1.8) |
| Neighborhood | ||
| Urban | 254 | 54.4% |
| Rural | 86 | 18.4% |
| Suburban | 115 | 24.6% |
| Other | 12 | 2.6% |
| Education | ||
| High School degree or less | 71 | 15.2% |
| Some college, technical degree, or associates degree | 253 | 54.2% |
| College degree or more | 143 | 30.6% |
| Health problems and behaviors | ||
| Heavy episodic drinking | 228 | 48.8% |
| Smoking | 359 | 76.9% |
| Marijuana use | 149 | 31.9% |
| Ecstasy use | 17 | 3.6% |
| Hallucinogen use | 16 | 3.4% |
| Prescription drug misuse | 47 | 10.1% |
| Other illicit drug use | 24 | 5.1% |
| Depressive symptoms, mean (standard deviation) | 13.4 | (4.6) |
| Multiple sexual partners | 88 | 18.8% |
| Sexually transmitted infection history | 23 | 4.9% |
| Overweight/obesity | 112 | 24.0% |
| Sexual-orientation discrimination variables | ||
| Past-month discrimination, mean (standard deviation) | 0.8 | (1.5) |
| Past-year discrimination | 173 | 37.0% |
| Total | 467 | 100.0% |
Correlations among syndemic conditions
Table 2 provides the correlation matrix for variables used in the structural equation models. Among the syndemic variables, 28 of the 55 bivariate pairs were positively and significantly correlated with each other. For example, marijuana use was associated with heavy episodic drinking (r=0.14), ecstasy use (r=0.21), hallucinogen use (r=0.17), prescription drug misuse (r=0.31), multiple sexual partners (r=0.19), and STI history (r=0.14). Additionally, past-month and past-year sexual-orientation discrimination were correlated with each other (r=0.36).
Table 2.
Means, Standard Deviations, and Correlations of Model Variables Among Young Sexual-Minority Women (n=467)
| Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Health Problems and Behaviors | ||||||||||||||
| 1. Heavy episodic drinking | 0.49 (0.50) | 1.00 | ||||||||||||
| 2. Smoking | 0.77 (0.42) | 0.17*** | 1.00 | |||||||||||
| 3. Marijuana use | 0.32 (0.47) | 0.14** | −0.05 | 1.00 | ||||||||||
| 4. Ecstasy use | 0.04 (0.19) | 0.06 | 0.11* | 0.21*** | 1.00 | |||||||||
| 5. Hallucinogen use | 0.03 (0.18) | 0.05 | 0.02 | 0.17*** | 0.28*** | 1.00 | ||||||||
| 6. Prescription drug misuse | 0.10 (0.30) | 0.10* | 0.00 | 0.31*** | 0.16*** | 0.29*** | 1.00 | |||||||
| 7. Other illicit drug use | 0.05 (0.22) | 0.04 | 0.13** | −0.06 | 0.11* | 0.06 | 0.02 | 1.00 | ||||||
| 8. Depressive symptoms | 13.40 (4.61) | 0.06 | 0.22*** | 0.02 | 0.02 | 0.11* | 0.15** | 0.06 | 1.00 | |||||
| 9. Multiple sexual partners | 0.19 (0.39) | 0.08 | 0.04 | 0.19*** | 0.11* | 0.12** | 0.11* | 0.06 | 0.08 | 1.00 | ||||
| 10. Sexually transmitted infection history | 0.05 (0.22) | 0.02 | −0.02 | 0.14** | −0.04 | 0.12** | 0.19*** | −0.01 | 0.09* | 0.07 | 1.00 | |||
| 11. Overweight/obesity | 0.24 (0.43) | −0.10* | −0.35*** | 0.11* | −0.03 | 0.00 | 0.20*** | −0.09 | −0.01 | 0.00 | 0.13** | 1.00 | ||
| Sexual-Orientation Discrimination Variables | ||||||||||||||
| 12. Past-year discrimination | 0.37 (0.48) | 0.10* | −0.05 | 0.14** | 0.02 | 0.00 | 0.05 | 0.00 | 0.03 | 0.06 | −0.07 | 0.06 | 1.00 | |
| 13. Past-month discrimination | 0.79 (1.55) | 0.00 | −0.07 | 0.11* | 0.06 | 0.03 | 0.11* | −0.02 | 0.15*** | 0.06 | −0.03 | 0.17*** | 0.36*** | 1.00 |
P<.05; **P<.01; ***P<.001.
SD, standard deviation.
Latent syndemic variable
Table 3 shows our model building process for the syndemic variable. In Model 1 we tested if all health problems and behaviors comprised a syndemic variable. This model did not fit the data well according to all the fit indices (χ2=140.042, P<.001; CFI=0.512; RMSEA=0.068). In Model 2, we removed variables with non-significant loadings from Model 1 (i.e., smoking, other illicit drug use, and overweight/obesity). Model 2 significantly improved model fit (χ2 difference=135.575, P<.001) and fit the data well according to all indices (χ2=24.989, P=.201; CFI=0.946; RMSEA=0.023). This showed that heavy episodic drinking, marijuana use, ecstasy use, prescription drug misuse, depressive symptoms, multiple sexual partners, and STI history comprise the latent syndemic variable.
Table 3.
Unstandardized Coefficients and Fit Statistics for Structural Equation Models of Syndemics Among Young Sexual-Minority Women (n=467)
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| b | b | b | b | |
| Measurement Model | ||||
| Syndemic Factor | ||||
| Heavy episodic drinking | 1.000 | 1.000 | 1.000 | 1.000 |
| Smoking | 0.166 | – | – | – |
| Marijuana use | 2.586** | 2.472** | 2.503** | 2.503** |
| Ecstasy use | 0.736* | 0.724* | 0.709** | 0.709** |
| Hallucinogen use | 0.963* | 0.937* | 0.899** | 0.899** |
| Prescription drug misuse | 2.066** | 1.865** | 1.846** | 1.846** |
| Other illicit drug use | 0.144 | – | – | – |
| Depressive symptoms | 0.371* | 9.596* | 10.04* | 10.038* |
| Multiple sexual partners | 1.174* | 1.142* | 1.146** | 1.146** |
| Sexually transmitted infection history | 0.629* | 0.567* | 0.535* | 0.535* |
| Overweight/obesity | 0.771 | – | – | – |
| Sexual-Orientation Discrimination Factor | ||||
| Past-year discrimination | – | – | 1.000 | 1.000 |
| Past-month discrimination | – | – | 4.698* | 4.697* |
| Structural Model | ||||
| Discrimination Factor → Syndemic Factor | – | – | 0.095* | – |
| Syndemic Factor → Discrimination Factor | – | – | – | 0.602 |
| Model fit | ||||
| Satorra-Bentler χ2 (df) | 140.042 (44)*** | 24.989 (20) | 47.762 (34) | 47.762 (34) |
| Satorra-Bentler difference test, χ2 (df) | – | 135.575 (24)a*** | 24.258 (14)b* | 22.257 (14)b* |
| CFI | 0.512 | 0.946 | 0.914 | 0.914 |
| RMSEA | 0.068 | 0.023 | 0.029 | 0.029 |
| (90% Confidence Interval) | (0.056, 0.081) | (0.000, 0.048) | (0.000, 0.048) | (0.000, 0.048) |
Compared to Model 1.
Compared to Model 2.
P<.05; **P<.01; ***P<.001.
df, degrees of freedom; CFI, comparative fit index; RMSEA, root mean square error of approximation.
Sexual-orientation discrimination and the syndemic latent variable
In Model 3 (Table 3), we added sexual-orientation discrimination as the latent independent variable (IV) and syndemics as the latent dependent variable (DV). Model 3 fit the data well according to all the fit indices (χ2=33.558, P=.059; CFI=0.914; RMSEA=0.029). Furthermore, the structural model showed that the sexual-orientation discrimination latent variable was associated with the syndemic latent variable (unstandardized coefficient=0.095, P<.05).
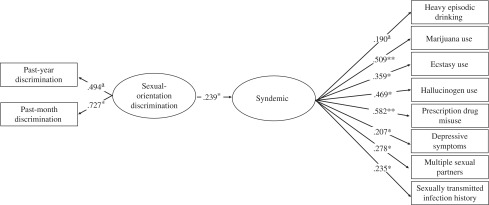
Because data were cross-sectional, we also fit the reverse causation model with syndemics as the latent IV and sexual-orientation discrimination as the latent DV. Results from this model, located in Model 4 (Table 3), showed that syndemics were not an IV of sexual-orientation discrimination (unstandardized coefficient=0.602, P>.05). Thus, the structural model was best fit as we theoretically proposed, and Model 3—with sexual-orientation discrimination as the IV and syndemics as the DV—was our final model; Figure 1 presents a visual representation of our final model and includes its standardized coefficients.
FIG. 1.
Standardized loadings for the structural equation model of syndemics among young sexual-minority women (n=467). afixed parameters; *P<0.05; **P<0.01.
Discussion
By using the syndemics framework, our study synthesizes several critical health problems for YSMW, a marginalized and vulnerable group, into a single conceptual model. Our study provides evidence that heavy episodic drinking, drug use, depressive symptoms, and sexual behaviors comprise a syndemic among YSMW. These findings demonstrate that co-occurring health problems are not solely germane to sexual-minority men,27,28,34,35 but exist among YSMW as well. Moreover, syndemics occur at an early age, which may have harmful public health implications throughout the life-course, especially if these epidemics continue to accumulate and sustain themselves as women age.
Our study also shows that experiences of sexual-orientation discrimination are positively associated with syndemics. Our findings extend previous investigations30–33 about the relationship between discrimination and individual health outcomes to suggest that discrimination produces a cluster of health problems. This further confirms that discrimination is a powerful sociocultural mechanism—and is associated with multiple health problems among stigmatized populations.48
Though the syndemic latent variable in our study appeared to include several health problems disproportionately affecting YSMW, two critical health problems unexpectedly did not fit the syndemic model: smoking and overweight/obesity. This interesting finding may be driven by two unique, yet related, factors. First, the relationship between smoking and obesity is complex. Among the general population, cross-sectional studies find that light-to-moderate smokers weigh less than nonsmokers,49 and smoking cessation is associated with substantial weight gain.50 Heavy smoking, though, is associated with higher BMI,51 and individuals at all levels of smoking intensity gain more weight over time than nonsmokers.52 Literature on the smoking-weight relationship among sexual-minority women is weaker. Smoking initiation among adolescent girls is associated with body image and weight gain concerns,53 although several studies report that lesbians are less likely to be concerned with weight and body image than heterosexual women.54,55 We are aware of one study on smoking and weight among lesbian adults, which showed smoking was unassociated with BMI.56 However, in our study overweight/obesity was inversely correlated with smoking (r = −0.35, P<.001), which could be because, compared to smokers, non-smokers have higher physical fitness and greater muscle strength, and consequently have higher BMI. To gain a better understanding of this relation, physical activity and nutritional behaviors (which were unavailable to us) should be examined as part of overweight/obesity and syndemics in future studies. Second, as we describe below, our study may be prone to sampling and self-report biases.
Our study is not without limitations. This study uses a cross-sectional design and does not permit the analysis of strict causal relationships or dynamics. However, our study partially addresses this limitation by examining the data in the hypothesized direction (i.e., sexual-orientation discrimination leading to syndemics) and reverse causal direction. Our study was a convenience sample of YSMW and may be prone to sampling bias. For example, participants in our sample had a substantially higher prevalence of any smoking compared to similarly aged sexual-minority women in other studies.5–8 Moreover, only 24% of our sample was overweight/obese, which is lower than national estimates in the general population of 18- to 24-year-olds57 and counter to previous studies suggesting YSMW are more likely to be overweight/obese compared to their heterosexual counterparts.3,58–62 Alternatively, the lower prevalence of overweight/obese in our study might also be attributable to self-report bias,63 as all measures were self-reported by participants. Finally, perceived discrimination is challenging to measure accurately because how individuals report discrimination can be influenced by a variety of factors, including social environment, race/ethnicity, perceptions, and attributions. To overcome this, we combined two different measures of sexual-orientation discrimination to create a single latent variable measuring this construct. Additional methodologies, samples, and analyses can remedy these limitations. However, our current investigation is a first step in determining that health disparities interact and produce risk among YSMW.
Despite its limitations, our study has several implications for public health interventions. Given the correlation between discrimination and syndemics, implementation of structural interventions that aim to increase support and acceptance of YSMW may greatly reduce the prevalence and long-term health costs of disparities in this population. This recommendation is consistent with prior research indicating how living in a supportive social context is protective against psychological distress and substance use among sexual-minority youth.64–66 For example, studies of sexual-minority youth living in supportive counties (defined as the inclusion of sexual orientation in school-wide anti-bullying policies and the presence of a religious climate that is supportive of homosexuality) find that they report fewer suicide attempts and lower rates of alcohol abuse.64,65 Our study's research findings suggest that similar types of structural interventions may be able to reduce a host of health problems in YSMW.
Also, because our study found that health behaviors and problems were interrelated, behavior change interventions for YSMW may be more effective if they include modules with a more holistic approach, focusing on health problems beyond the primary targeted behavioral change outcome. For example, including information about depression and sexual risk behaviors in substance use interventions may help increase their overall effectiveness. Additionally, interventions targeting one specific behavior may be able to simultaneously improve other unique, but related, health behaviors. Our study's findings also suggest that interventions focused on YSMW should include modules about sexual-orientation discrimination. Providing YSMW with information and skills to properly cope with sexual-orientation discrimination in a healthy way and reduce related stress might have the added benefit of alleviating related health problems. Our study's findings and the syndemics framework may prove useful in designing and implementing interventions aimed at improving the health of YSMW.
Conclusions
Altogether, our study provides strong evidence that sexual-minority women are vulnerable to syndemic production beginning early in the life-course. Syndemics is an important framework for public health researchers and practitioners to utilize when planning, implementing, and evaluating future research and intervention studies. In the marginalized and underserved population of YSMW, syndemics theory highlights the existence—and drivers—of numerous overlapping health problems and, if used carefully, can help attain health equity.
Acknowledgments
We posthumously thank Kevin H. Kim for double checking our analyses–and for being an incredible statistician, professor, and mentor. The current investigation was supported by F31DA037647 from the National Institutes of Health. R.W.S.C. conceptualized this study, while all authors made substantial contributions to the design, analysis, interpretation, and writing. The Parent Study was funded through an award made to J.A.B. through the University of Michigan Comprehensive Cancer Center (P30CA046592). This article is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Institute of Medicine: The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, D.C.: National Academies Press, 2011 [PubMed] [Google Scholar]
- 2.Marshal MP, Dietz LJ, Friedman MS, et al. : Suicidality and depression disparities between sexual minority and heterosexual youth: A meta-analytic review. J Adolesc Health 2011;49:115–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valanis BG, Bowen DJ, Bassford T, et al. : Sexual orientation and health: Comparisons in the women's health initiative sample. Arch Fam Med 2000;9:843–853 [DOI] [PubMed] [Google Scholar]
- 4.Gilman SE, Cochran SD, Mays VM, et al. : Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. Am J Public Health 2001;91:933–939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blosnich J, Jarrett T, Horn K: Disparities in smoking and acute respiratory illnesses among sexual minority young adults. Lung 2010;188:401–407 [DOI] [PubMed] [Google Scholar]
- 6.Blosnich JR, Jarrett T, Horn K: Racial and ethnic differences in current use of cigarettes, cigars, and hookahs among lesbian, gay, and bisexual young adults. Nicotine Tob Res 2011;13:487–491 [DOI] [PubMed] [Google Scholar]
- 7.McCabe SE, Boyd C, Hughes TL, d'Arcy H: Sexual identity and substance use among undergraduate students. Subst Abus 2003;24:77–91 [DOI] [PubMed] [Google Scholar]
- 8.McCabe SE, Hughes TL, Bostwick W, Boyd CJ: Assessment of difference in dimensions of sexual orientation: Implications for substance use research in a college-age population. J Stud Alcohol Drugs 2005;66:620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marshal MP, Friedman MS, Stall R, et al. : Sexual orientation and adolescent substance use: A meta‐analysis and methodological review. Addiction 2008;103:546–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saewyc EM, Bearinger LH, Blum RW, Resnick MD: Sexual intercourse, abuse and pregnancy among adolescent women: Does sexual orientation make a difference? Fam Plann Perspect 1999;31:127–131 [PubMed] [Google Scholar]
- 11.Corliss HL, Austin SB, Roberts AL, Molnar BE: Sexual risk in “mostly heterosexual” young women: Influence of social support and caregiver mental health. J Womens Health 2009;18:2005–2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh D, Fine DN, Marrazzo JM: Chlamydia trachomatis infection among women reporting sexual activity with women screened in Family Planning Clinics in the Pacific Northwest, 1997 to 2005. Am J Public Health 2011;101:1284–1290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herrick AL, Marshal MP, Smith HA, et al. : Sex while intoxicated: A meta-analysis comparing heterosexual and sexual minority youth. J Adolesc Health 2011;48:306–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gorgos LM, Marrazzo JM: Sexually transmitted infections among women who have sex with women. Clin Infect Dis 2011;53 Suppl 3:S84–91 [DOI] [PubMed] [Google Scholar]
- 15.Bowen DJ, Balsam KF, Ender SR: A review of obesity issues in sexual minority women. Obesity 2008;16:221–228 [DOI] [PubMed] [Google Scholar]
- 16.Austin SB, Ziyadeh NJ, Corliss HL, et al. : Sexual orientation disparities in purging and binge eating from early to late adolescence. J Adolesc Health 2009;45:238–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jun HJ, Corliss HL, Nichols LP, et al. : Adult body mass index trajectories and sexual orientation: The Nurses' Health Study II. Am J Prev Med 2012;42:348–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tolstrup JS, Halkjaer J, Heitmann BL, et al. : Alcohol drinking frequency in relation to subsequent changes in waist circumference. Am J Clin Nutr 2008;87:957–963 [DOI] [PubMed] [Google Scholar]
- 19.Yeomans MR: Alcohol, appetite and energy balance: Is alcohol intake a risk factor for obesity? Physiol Behav 2010;100:82–89 [DOI] [PubMed] [Google Scholar]
- 20.Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M: Alcohol consumption and body weight: A systematic review. Nutr Rev 2011;69:419–431 [DOI] [PubMed] [Google Scholar]
- 21.Sutin AR, Zonderman AB: Depressive symptoms are associated with weight gain among women. Psychol Med 2012;42:2351–2360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fleming CB, Mason WA, Mazza JJ, et al. : Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychol Addict Behav 2008;22:186. [DOI] [PubMed] [Google Scholar]
- 23.Mustanski B, Andrews R, Herrick A, et al. : A syndemic of psychosocial health disparities and associations with risk for attempting suicide among young sexual minority men. Am J Public Health 2014;104:287–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Herrick A, Kuhns L, Kinsky S, et al. : Demographic, psychosocial, and contextual factors associated with sexual risk behaviors among young sexual minority women. J Am Psychiatr Nurses Assoc 2013;19:345–355 [DOI] [PubMed] [Google Scholar]
- 25.Pesola F, Shelton KH, Bree M: Sexual orientation and alcohol problem use among UK adolescents: An indirect link through depressed mood. Addiction 2014;109:1072–1080 [DOI] [PubMed] [Google Scholar]
- 26.Singer M, Clair S: Syndemics and public health: Reconceptualizing disease in bio-social context. Med Anthropol Q 2003;17:423–441 [DOI] [PubMed] [Google Scholar]
- 27.Stall R, Mills TC, Williamson J, et al. : Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health 2003;93:939–942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mustanski B, Garofalo R, Herrick A, Donenberg G: Psychosocial health problems increase risk for HIV among urban young men who have sex with men: Preliminary evidence of a syndemic in need of attention. Ann Behav Med 2007;34:37–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singer M: Introduction to Syndemics: A Critical Systems Approach to Public and Community Health. Hoboken, NJ: Jossey-Bass, 2009 [Google Scholar]
- 30.McCabe SE, Bostwick WB, Hughes TL, et al. : The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. Am J Public Health 2010;100:1946–1952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mays VM, Cochran SD: Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. Am J Public Health 2001;91:1869–1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS: The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: A prospective study. Am J Public Health 2010;100:452–459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McLaughlin KA, Hatzenbuehler ML, Keyes KM: Responses to discrimination and psychiatric disorders among Black, Hispanic, female, and lesbian, gay, and bisexual individuals. Am J Public Health 2010;100:1477–1484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Herrick AL, Lim SH, Plankey MW, et al. : Adversity and syndemic production among men participating in the Multicenter AIDS Cohort Study: A life-course approach. Am J Pub Health 2013;103:79–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dyer TP, Shoptaw S, Guadamuz TE, et al. : Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Health 2012;89:697–708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bradford J, Ryan C, Rothblum ED: National Lesbian Health Care Survey: Implications for mental health care. J Consult Clin Psychol 1994;62:228. [DOI] [PubMed] [Google Scholar]
- 37.Johns MM, Pingel ES, Youatt EJ, et al. : LGBT community, social network characteristics, and smoking behaviors in young sexual minority women. Am J Commun Psychol 2013;52:141–154 [DOI] [PubMed] [Google Scholar]
- 38.Bauermeister JA, Pingel E, Zimmerman M, et al. : Data quality in HIV/AIDS web-based surveys: Handling invalid and suspicious data. Field Method 2012:1525822X12443097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wechsler H, Davenport A, Dowdall G, et al. : Health and behavioral consequences of binge drinking in college: A national survey of students at 140 campuses. JAMA 1994;272:1672–1677 [PubMed] [Google Scholar]
- 40.Radloff LS: The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401 [Google Scholar]
- 41.Centers for Disease Control Prevention: About BMI for adults. 2011. Available at http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html (accessed June20, 2014.)
- 42.Meyer IH, Frost DM, Narvaez R, Dietrich JH: Project Stride Methodology and Technical Notes. 2006. Available at http://www.columbia.edu/∼im15/method/stridemethod.pdf (accessed June6, 2014)
- 43.Almeida J, Johnson RM, Corliss HL, et al. : Emotional distress among LGBT youth: The influence of perceived discrimination based on sexual orientation. J Youth Adolesc 2009;38:1001–1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Satorra A, Bentler PM: Some robustness properties of goodness of fit statistics in covariance structure analysis. Proc Bus Econ Stat Amer Statis Assoc 1986;549–554 [Google Scholar]
- 45.Satorra A, Bentler PM: Corrections to test statistics and standard errors in covariance structure analysis. von Eye A, Clogg CC, Eds. In: Latent Variables Analysis: Applications for Developmental Research. Thousand Oaks, CA: Sage, 1994, pp 399–419 [Google Scholar]
- 46.Hu L, Bentler PM: Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling 1999;6:1–55 [Google Scholar]
- 47.Satorra A, Bentler PM: A scaled difference chi-square test statistic for moment structure analysis. Psychometrika 2001;66:507514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hatzenbuehler ML, Phelan JC, Link BG: Stigma as a fundamental cause of population health inequalities. Am J Public Health 2013;103:813–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Klesges RC, Meyers AW, Klesges LM, La Vasque ME: Smoking, body weight, and their effects on smoking behavior: A comprehensive review of the literature. Psychol Bull 1989;106:204–230 [DOI] [PubMed] [Google Scholar]
- 50.Williamson DF, Madans J, Anda RF, et al. : Smoking cessation and severity of weight gain in a national cohort. NEJM 1991;324:739–745 [DOI] [PubMed] [Google Scholar]
- 51.Chiolero A, Faeh D, Paccaud F, Cornuz J: Consequences of smoking for body weight, body fat distribution, and insulin resistance. Am J Clin Nutr 2008;87:801–809 [DOI] [PubMed] [Google Scholar]
- 52.Colditz G, Segal M, Myers A, et al. : Weight change in relation to smoking cessation among women. J Smoking Rel Dis 1992;3:145–153 [Google Scholar]
- 53.Cawley J, Markowitz S, Tauras J: Lighting up and slimming down: The effects of body weight and cigarette prices on adolescent smoking initiation. J Health Econ 2004;23:293–311 [DOI] [PubMed] [Google Scholar]
- 54.Herzog DB, Newman KL, Yeh CJ, Warshaw M: Body image satisfaction in homosexual and heterosexual women. Int J Eat Disord 1992;11:391–396 [Google Scholar]
- 55.Moore F, Keel PK: Influence of sexual orientation and age on disordered eating attitudes and behaviors in women. Int J Eat Disord 2003;34:370–374 [DOI] [PubMed] [Google Scholar]
- 56.Yancey AK, Cochran SD, Corliss HL, Mays VM: Correlates of overweight and obesity among lesbian and bisexual women. Prev Med 2003;36:676–683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Centers for Disease Control and Prevention (CDC): Behavioral Risk Factor Surveillance System Survey Data, 2012. Available at http://apps.nccd.cdc.gov/brfss/ (accessed June6, 2014)
- 58.Dilley JA, Simmons KW, Boysun MJ, et al. : Demonstrating the importance and feasibility of including sexual orientation in public health surveys: Health disparities in the Pacific Northwest. Am J Public Health 2010;100:460–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fredriksen-Goldsen KI, Emlet CA, Kim HJ, et al. : The physical and mental health of lesbian, gay male, and bisexual (LGB) older adults: The role of key health indicators and risk and protective factors. Gerontologist 2013;53:664–675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boehmer U, Bowen DJ: Examining factors linked to overweight and obesity in women of different sexual orientations. Prev Med 2009;48:357–361 [DOI] [PubMed] [Google Scholar]
- 61.Boehmer U, Bowen DJ, Bauer GR: Overweight and obesity in sexual-minority women: evidence from population-based data. Am J Public Health 2007;97:1134–1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Conron KJ, Mimiaga MJ, Landers SJ: A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health 2010;100:1953–1960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Clarke P, Sastry N, Duffy D, Ailshire J: Accuracy of self-reported versus measured weight over adolescence and young adulthood: Findings from the National Longitudinal Study of Adolescent Health, 1996–2008. Am J Epidemiol 2014;180:153–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hatzenbuehler ML, Keyes KM: Inclusive anti-bullying policies and reduced risk of suicide attempts in lesbian and gay youth. J Adolesc Health 2013;53:S21–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hatzenbuehler ML, Keyes KM, McLaughlin KA: The protective effects of social/contextual factors on psychiatric morbidity in LGB populations. Int J Epidemiol 2011;40:1071–1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bauermeister JA: How statewide LGB policies go from “under our skin” to “into our hearts”: Fatherhood aspirations and psychological well-being among emerging adult sexual minority men. J Youth Adolesc 2013:43;1295–1305 [DOI] [PMC free article] [PubMed] [Google Scholar]