Abstract
Cyclic vomiting syndrome (CVS) is a functional disorder characterized by stereotypical episodes of intense vomiting separated by weeks to months. Although it can occur at any age, the most common age at presentation is 3-7 years. There is no gender predominance. The precise pathophysiology of CVS is not known but a strong association with migraine headaches, in the patient as well as the mother indicates that it may represent a mitochondriopathy. Studies have also suggested the role of an underlying autonomic neuropathy involving the sympathetic nervous system in its pathogenesis. CVS has known triggers in many individuals and avoiding these triggers can help prevent the onset of the episodes. It typically presents in four phases: a prodrome, vomiting phase, recovery phase and an asymptomatic phase until the next episode. Complications such as dehydration and hematemesis from Mallory Wise tear of the esophageal mucosa may occur in more severe cases. Blood and urine tests and abdominal imaging may be indicated depending upon the severity of symptoms. Brain magnetic resonance imaging and upper gastrointestinal endoscopy may also be indicated in certain circumstances. Management of an episode after it has started ('abortive treatment') includes keeping the patient in a dark and quiet room, intravenous hydration, ondansetron, sumatriptan, clonidine, and benzodiazepines. Prophylactic treatment includes cyproheptadine, propranolol and amitriptyline. No mortality has been reported as a direct result of CVS and many children outgrow it over time. A subset may develop other functional disorders like irritable bowel syndrome and migraine headaches.
Keywords: Cyclic vomiting, Vomiting
INTRODUCTION
The syndrome of cyclic vomiting syndrome (CVS) was first described by a British pediatrician Samuel Jones Gee in 1882. It is a distinct clinical entity, one of several disorders of motility resulting from disturbed regulation between the gut and the brain. The syndrome is characterized by stereotypical and repeated episodes of vomiting with symptom-free intervals of weeks to months.
DIAGNOSTIC CRITERIA
Using Rome III diagnostic criteria, the disorder has been estimated to have an annual community prevalence of 0.2% to 1.0% [1,2,3]. An Irish study reported an incidence of 3 per 100,000 [4]. The median age of onset of symptoms varies from 3.5 to 7 years but it can occur at any age from infancy to adulthood [4,5,6,7]. Nearly half (46%) of children have symptoms at or below 3 years of age [4]. No gender predominance has been described [4,5,6]. A study reported an average loss of 24 school days per year and an annual cost of care exceeding 17,000 US dollars [8]. There may be a delay in diagnosis of 13 to 40 months [4,5]. However, with early diagnosis and initiation of therapy the average duration of episodes can be brought down to 4.1 to 0.8 days and the number of emergency room visits from 2.3 to 0.6 times per year [5].
For diagnosis all of the following criteria should be fulfilled:
Two or more periods (cycles) of intense, unremitting nausea and paroxysmal vomiting, lasting hours to days within a 6-month period.
At least four episodes of vomiting per hour with a median of 6 per hour at the peak.
Stereotypical episodes in each patient.
Episodes separated by weeks to months.
Symptoms not attributable to any other condition.
PATHOPHYSIOLOGY
The syndrome is a complex, multifactorial disorder of the brain-gut axis of as yet unclear pathogenesis, often associated with other episodic conditions like migraine headaches and abdominal migraine [9]. A familial aggregation with maternal history of migraine headaches is common. Some features of the syndrome are suggestive of a mitochondriopathy.
An underlying autonomic neuropathy in CVS has been suggested based on an overwhelming majority (90%) of adult patients who have impairment of the sympathetic nervous system (vasomotor and sudomotor) but a normal parasympathetic nerve function [10]. It has been hypothesised that central corticotrophin-releasing factor activation may play a role which may be involved in endocrine autonomic and visceral changes seen in these patients [11].
Gene studies have shown association with two single nucleotide polymorphism (SNP) of mitochondrial DNA (mtDNA): 16519T and 3010A that adversely affect energy metabolism (AT genotype) [12,13,14]. As many as 71% of children below 12 years of age with CVS have the 16519T SNP.
Psychologically, emotional stress and anticipatory anxiety may trigger an episode. A high prevalence of internalizing psychiatric disorders, especially anxiety disorders was found in children with CVS as well as in their parents.
Triggering factors that may precipitate an episode include exposure to cold, allergies, sinus problems, emotional stress or excitement, anxiety or panic attack, intake of foods like chocolate or cheese, overeating, going to bed immediately after a meal, hot weather, physical exhaustion, menstruation or motion sickness.
PRESENTATION
Clinically, four phases of the illness can be recognised:
A prodromal phase with a feeling that an episode is about to start, followed by intense sweating and nausea with or without abdominal pain, and a pale appearance. This phase lasts from a few minutes to several hours.
The vomiting phase with nausea, vomiting and retching lasting 20 to 30 minutes at a time, may be subdued and responsive, immobile and unresponsive or writhing and moaning with intense abdominal pain. This phase can last from hours to days and is the longest.
The recovery phase begins with cessation of vomiting and retching, improving appetite and gradual or immediate return of energy.
A phase of wellness between episodes when the child is symptom free.
Associated symptomatology may include retching or making an attempt to vomit, heaving or gagging, appetite loss, abdominal pain, diarrhea, fever, dizziness, headache and photophobia (sensitivity to light).
As a complication, hematemesis may occur from bleeding from a tear in the mucosal junction of the esophagus and the stomach (Mallory-Weiss tear).
DIFFERENTIAL DIAGNOSIS
Differential diagnosis of CVS includes the cannabinoid hyperemesis syndrome which may mimic CVS. Chronic use of cannabis can be paradoxically associated with repeated episodes of severe vomiting, nausea and abdominal pain. Compulsive, long hot water baths or shower result in temporary relief of symptoms in cannabinoid hyperemesis syndrome [15,16]. The proposed mechanisms are delayed gastric emptying through brain and enteric CB 1 receptor stimulation, thermoregulatory disturbances via the limbic system, or CB 1 receptor-mediated vasodilatation of the splanchnic bed [17,18]. Warm bathing and the subsequent cutaneous vasodilatation may decrease the available circulatory volume in the splanchnic bed thereby alleviating the symptoms [19]. Other proposed mechanisms include balancing hypothermic effects of tetrahydrocannabinol. Immediate discontinuation will stop recurrence of symptoms.
Another condition that may present with cyclic vomiting is eosinophilic esophagitis (EoE) [20]. It is a relatively new disease first described by Landres et al. [21] in 1978 and increasingly recognized all over the world in the past decade or two. EoE is a chronic inflammatory condition of the esophagus, characterized histologically by eosinophilic infiltration, with esophageal mucosal biopsy specimens showing 15 or more eosinophils per high power field (HPF) [22]. There is usually a history of asthma, environmental or food allergies and is more common in males. Dysphagia and food impaction are common presenting symptoms but vomiting has also been described especially in younger children. Endoscopic biopsies are necessary to confirm the diagnosis of EoE and must be distinguished from gastroesophageal reflux disease. Some cases of EoE are responsive to a proton pump inhibitor [23]. Management includes avoidance of allergic foods and environmental allergens and topical (swallowed) fluticasone or steroids [24].
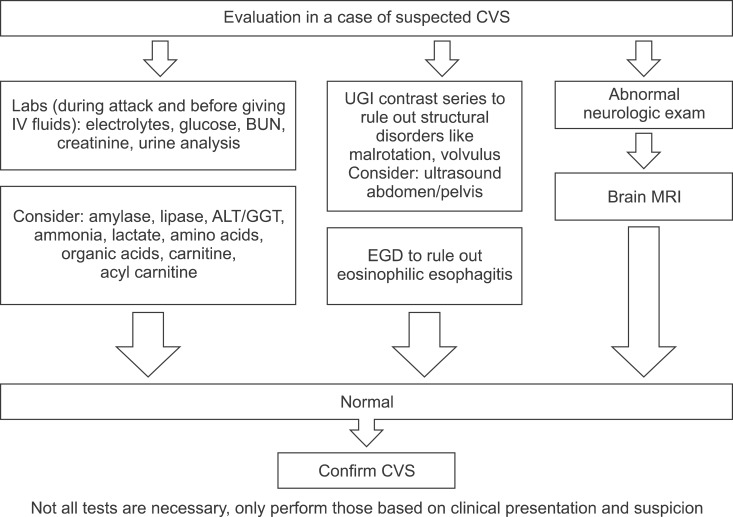
EVALUATION (Fig. 1)
Fig. 1. Evaluation of a child with suspected cyclic vomiting syndrome (CVS). Labs: laboratory tests, IV: intravenous; BUN: blood urea nitrogen, ALT/GGT: alanine aminotransferase/gamma glutamyl transferase, UGI: upper gastrointestinal series, EGD: esophagogastroduodenoscopy, MRI: magnetic resonance imaging.
If the symptoms do not fulfil the diagnostic criteria of CVS or there is suspicion of another etiology for the vomiting, an evaluation to exclude other diagnoses may be undertaken. This would include the following:
Blood: Electrolytes, glucose, blood urea nitrogen, creatinine, amino acids, alanine aminotransferase, gamma glutamyltransferase, lactate, ammonia, plasma carnitine and acylcarnitine, amylase and lipase
Urine for D-aminolevulinic acid, organic acids, ketones and porphilinogen to rule out metabolic disorders
Imaging to include: upper gastrointestinal (GI) radiographic imaging, abdominal ultrasound or computed tomography scan to exclude structural or inflammatory disorders of the GI tract
Brain magnetic resonance imaging, upper GI endoscopy and urine toxicology may be warranted in certain situations
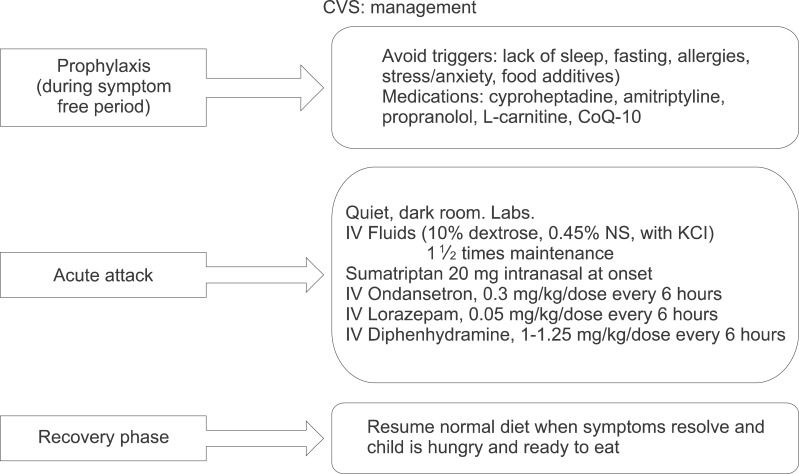
MANAGEMENT (Fig. 2)
Fig. 2. Management of a child with cyclic vomiting syndrome (CVS). CoQ-10: coenzyme Q-10, Labs: laboratory tests, IV: intravenous, NS: normal saline, KCl: potassium chloride.
Management of CVS aims essentially at prophylaxis therapy for preventing episodes and therapy for aborting an attack after it has started [25].
Preventive management is primarily avoidance of triggers; adequate sleep to prevent exhaustion; treating allergies and sinus problems and instituting measures for reducing stress and anxiety. Feeding advice should include avoidance of foods with additives and those known to trigger episodes [26]. Eating small carbohydrate-containing snacks between meals, before exercise and at bedtime should be advised. Prophylactic treatment options include medications and supplements during symptom free periods. For children 5 years old or less, the medication of choice is cyproheptadine at 0.25-0.5 mg/kg/day, dose divided two or three times a day. The second choice is propranolol at 0.25-1.0 mg/kg/day, dose divided two or three times a day. For those above 6 years of age, amitriptyline at 1.0 to 1.5 mg/kg at bedtime is the first choice, followed by propranolol. Pizotifen, phenobarbital, topiramate, valproic acid, gabapentin and levetiracetam have also been reportedly tried with mixed results [27,28]. Supplements that have been shown to help include L-carnitine 50-100 mg per day divided into 2 or 3 doses to a maximum of 1 gm thrice a day, and coenzyme Q-10, 10 mg per kg per day in two or three divided doses up to a maximum of 100 mg thrice a day [29,30].
At the onset of an episode, abortive therapy should be instituted as soon as possible. Sleeping and resting in a quiet and dark room during the episode is helpful. Ondansetron may be used initially for milder symptoms. Early use of intranasal sumatriptan can abort an attack in a third of patients and use of subcutaneous sumatriptan in over half of them (54%) [31]. Clonidine alone as a pill (0.1 or 0.2 mg) or as a transdermal patch (0.2 or 0.3 mg per day) may also be tried. Alternatively, a combination of clonidine with a benzodiazepine (midazolam or lorazepam) can be administered in more severe cases [32,33]. Another option is alternating promethazine suppository (12.5, 25 or 10 mg) with diazepam rectal gel (2.5, 5 or 10 mg) every 4-6 hours. If the symptoms persist beyond 24 hours and the child is unable to maintain hydration, intravenous fluids may be indicated.
PROGNOSIS
Prognosis of CVS from a study of 28 patients, 17 with adult-onset and 11 with childhood-onset, revealed that 61.9% of patients showed a gradual improvement in symptoms and 23.8% had complete resolution after a mean of 7 years [34]. No deaths from the syndrome have been reported.
CONCLUSION
In conclusion, CVS should be considered in any child with repeated episodes of vomiting with periods of wellness between episodes. Awareness and early suspicion of CVS is key to reducing the time to diagnosis and potentially limiting the use of low-yield testing. More data is needed to investigate the pathogenesis of CVS and evaluate treatment response and outcome.
The Cyclic Vomiting Syndrome Association, at www.cvsaonline.org, has excellent information for patients and their families.
References
- 1.Saps M, Nichols-Vinueza DX, Rosen JM, Velasco-Benítez CA. Prevalence of functional gastrointestinal disorders in Colombian school children. J Pediatr. 2014;164:542–545.e1. doi: 10.1016/j.jpeds.2013.10.088. [DOI] [PubMed] [Google Scholar]
- 2.Devanarayana NM, Adhikari C, Pannala W, Rajindrajith S. Prevalence of functional gastrointestinal diseases in a cohort of Sri Lankan adolescents: comparison between Rome II and Rome III criteria. J Trop Pediatr. 2011;57:34–39. doi: 10.1093/tropej/fmq039. [DOI] [PubMed] [Google Scholar]
- 3.Van Tilburg MAL, Walker LS, Palsson OS, Kim SM, Spiegel BM, Siller RC, et al. Prevalence of child/adolescent functional gastrointestinal disorders in a national U.S. community sample. Gastroenterology. 2014;146(5 Suppl 1):S143–S144. [Google Scholar]
- 4.Fitzpatrick E, Bourke B, Drumm B, Rowland M. The incidence of cyclic vomiting syndrome in children: population-based study. Am J Gastroenterol. 2008;103:991–995. quiz 996. doi: 10.1111/j.1572-0241.2007.01668.x. [DOI] [PubMed] [Google Scholar]
- 5.Liao KY, Chang FY, Wu LT, Wu TC. Cyclic vomiting syndrome in Taiwanese children. J Formos Med Assoc. 2011;110:14–18. doi: 10.1016/S0929-6646(11)60003-X. [DOI] [PubMed] [Google Scholar]
- 6.Lin YP, Ni YH, Weng WC, Lee WT. Cyclic vomiting syndrome and migraine in children. J Formos Med Assoc. 2011;110:382–387. doi: 10.1016/S0929-6646(11)60056-9. [DOI] [PubMed] [Google Scholar]
- 7.Withers GD, Silburn SR, Forbes DA. Precipitants and aetiology of cyclic vomiting syndrome. Acta Paediatr. 1998;87:272–277. doi: 10.1080/08035259850157318. [DOI] [PubMed] [Google Scholar]
- 8.Li BU, Balint JP. Cyclic vomiting syndrome: evolution in our understanding of a brain-gut disorder. Adv Pediatr. 2000;47:117–160. [PubMed] [Google Scholar]
- 9.Symon DN, Russell G. The relationship between cyclic vomiting syndrome and abdominal migraine. J Pediatr Gastroenterol Nutr. 1995;21(Suppl 1):S42–S43. doi: 10.1097/00005176-199501001-00012. [DOI] [PubMed] [Google Scholar]
- 10.Venkatesan T, Prieto T, Barboi A, Li B, Schroeder A, Hogan W, et al. Autonomic nerve function in adults with cyclic vomiting syndrome: a prospective study. Neurogastroenterol Motil. 2010;22:1303–1307. e339. doi: 10.1111/j.1365-2982.2010.01577.x. [DOI] [PubMed] [Google Scholar]
- 11.Taché Y. Cyclic vomiting syndrome: the corticotropin-releasing-factor hypothesis. Dig Dis Sci. 1999;44(8 Suppl):79S–86S. [PubMed] [Google Scholar]
- 12.Zaki EA, Freilinger T, Klopstock T, Baldwin EE, Heisner KR, Adams K, et al. Two common mitochondrial DNA polymorphisms are highly associated with migraine headache and cyclic vomiting syndrome. Cephalalgia. 2009;29:719–728. doi: 10.1111/j.1468-2982.2008.01793.x. [DOI] [PubMed] [Google Scholar]
- 13.Boles RG, Zaki EA, Lavenbarg T, Hejazi R, Foran P, Freeborn J, et al. Are pediatric and adult-onset cyclic vomiting syndrome (CVS) biologically different conditions? Relationship of adult-onset CVS with the migraine and pediatric CVS-associated common mtDNA polymorphisms 16519T and 3010A. Neurogastroenterol Motil. 2009;21:936–e72. doi: 10.1111/j.1365-2982.2009.01305.x. [DOI] [PubMed] [Google Scholar]
- 14.Boles RG, Adams K, Li BU. Maternal inheritance in cyclic vomiting syndrome. Am J Med Genet A. 2005;133A:71–77. doi: 10.1002/ajmg.a.30524. [DOI] [PubMed] [Google Scholar]
- 15.Wallace D, Martin AL, Park B. Cannabinoid hyperemesis: marijuana puts patients in hot water. Australas Psychiatry. 2007;15:156–158. doi: 10.1080/10398560701196778. [DOI] [PubMed] [Google Scholar]
- 16.Chang YH, Windish DM. Cannabinoid hyperemesis relieved by compulsive bathing. Mayo Clin Proc. 2009;84:76–78. doi: 10.4065/84.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong BS, Camilleri M, Busciglio I, Carlson P, Szarka LA, Burton D, et al. Pharmacogenetic trial of a cannabinoid agonist shows reduced fasting colonic motility in patients with nonconstipated irritable bowel syndrome. Gastroenterology. 2011;141:1638–1647. 1647.e1–1647.e7. doi: 10.1053/j.gastro.2011.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sullivan S. Cannabinoid hyperemesis. Can J Gastroenterol. 2010;24:284–285. doi: 10.1155/2010/481940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patterson DA, Smith E, Monahan M, Medvecz A, Hagerty B, Krijger L, et al. Cannabinoid hyperemesis and compulsive bathing: a case series and paradoxical pathophysiological explanation. J Am Board Fam Med. 2010;23:790–793. doi: 10.3122/jabfm.2010.06.100117. [DOI] [PubMed] [Google Scholar]
- 20.Noel RJ, Putnam PE, Rothenberg ME. Eosinophilic esophagitis. N Engl J Med. 2004;351:940–941. doi: 10.1056/NEJM200408263510924. [DOI] [PubMed] [Google Scholar]
- 21.Landres RT, Kuster GG, Strum WB. Eosinophilic esophagitis in a patient with vigorous achalasia. Gastroenterology. 1978;74:1298–1301. [PubMed] [Google Scholar]
- 22.Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, Bonis PA, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:3–20. doi: 10.1016/j.jaci.2011.02.040. [DOI] [PubMed] [Google Scholar]
- 23.Wen T, Dellon ES, Moawad FJ, Furuta GT, Aceves SS, Rothenberg ME. Transcriptome analysis of proton pump inhibitor-responsive esophageal eosinophilia reveals proton pump inhibitor-reversible allergic inflammation. J Allergy Clin Immunol. 2015;135:187–197. doi: 10.1016/j.jaci.2014.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Papadopoulou A, Koletzko S, Heuschkel R, Dias JA, Allen KJ, Murch SH, et al. ESPGHAN Eosinophilic Esophagitis Working Group and the Gastroenterology Committee. Management guidelines of eosinophilic esophagitis in childhood. J Pediatr Gastroenterol Nutr. 2014;58:107–118. doi: 10.1097/MPG.0b013e3182a80be1. [DOI] [PubMed] [Google Scholar]
- 25.Li BU, Lefevre F, Chelimsky GG, Boles RG, Nelson SP, Lewis DW, et al. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition consensus statement on the diagnosis and management of cyclic vomiting syndrome. J Pediatr Gastroenterol Nutr. 2008;47:379–393. doi: 10.1097/MPG.0b013e318173ed39. [DOI] [PubMed] [Google Scholar]
- 26.Paul SP, Barnard P, Soondrum K, Candy DC. Antimigraine (low-amine) diet may be helpful in children with cyclic vomiting syndrome. J Pediatr Gastroenterol Nutr. 2012;54:698–699. doi: 10.1097/MPG.0b013e31824ca0a2. [DOI] [PubMed] [Google Scholar]
- 27.Aanpreung P, Vajaradul C. Cyclic vomiting syndrome in Thai children. J Med Assoc Thai. 2002;85(Suppl 2):S743–S748. [PubMed] [Google Scholar]
- 28.Hikita T, Kodama H, Nakamoto N, Kaga F, Amakata K, Ogita K, et al. Effective prophylactic therapy for cyclic vomiting syndrome in children using valproate. Brain Dev. 2009;31:411–413. doi: 10.1016/j.braindev.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 29.Boles RG, Lovett-Barr MR, Preston A, Li BU, Adams K. Treatment of cyclic vomiting syndrome with co-enzyme Q10 and amitriptyline, a retrospective study. BMC Neurol. 2010;10:10. doi: 10.1186/1471-2377-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Calcar SC, Harding CO, Wolff JA. L-carnitine administration reduces number of episodes in cyclic vomiting syndrome. Clin Pediatr (Phila) 2002;41:171–174. doi: 10.1177/000992280204100307. [DOI] [PubMed] [Google Scholar]
- 31.Hikita T, Kodama H, Kaneko S, Amakata K, Ogita K, Mochizuki D, et al. Sumatriptan as a treatment for cyclic vomiting syndrome: a clinical trial. Cephalalgia. 2011;31:504–507. doi: 10.1177/0333102410390398. [DOI] [PubMed] [Google Scholar]
- 32.Palmer GM, Cameron DJ. Use of intravenous midazolam and clonidine in cyclical vomiting syndrome: a case report. Paediatr Anaesth. 2005;15:68–72. doi: 10.1111/j.1460-9592.2005.01369.x. [DOI] [PubMed] [Google Scholar]
- 33.Sato T, Igarashi N, Minami S, Okabe T, Hashimoto H, Hasui M, et al. Recurrent attacks of vomiting, hypertension and psychotic depression: a syndrome of periodic catecholamine and prostaglandin discharge. Acta Endocrinol (Copenh) 1988;117:189–197. doi: 10.1530/acta.0.1170189. [DOI] [PubMed] [Google Scholar]
- 34.Lee LY, Abbott L, Moodie S, Anderson S. Cyclic vomiting syndrome in 28 patients: demographics, features and outcomes. Eur J Gastroenterol Hepatol. 2012;24:939–943. doi: 10.1097/MEG.0b013e328354fc83. [DOI] [PubMed] [Google Scholar]