Abstract
The aim of this study was to examine the incidence and trends of clinically relevant venous thromboembolism (VTE) including deep vein thrombosis (DVT) and pulmonary embolism (PE) after hip and knee replacement arthroplasty (HKRA) in Korea. Between January 1 and December 31, 2010, 22,127 hip replacement arthroplasty (HRA) patients and 52,882 knee replacement arthroplasty (KRA) patients were enrolled in the analysis using the administrative claims database of the Health Insurance Review and Assessment Service (HIRA). All available parameters including procedure history and clinically relevant VTE during the 90 days after HKRA were identified based on diagnostic and electronic data interchange (EDI) codes. The overall incidence of VTE, DVT, and PE during the 90 days was 3.9% (n=853), 2.7% (n=597), and 1.5% (n=327) after HRA, while the incidence was 3.8% (n=1,990), 3.2% (n=1,699), and 0.7% (n=355) after KRA. The incidence of VTE after HKRA was significantly higher in patients who had previous VTE history (odds ratio [OR], 10.8 after HRA, OR, 8.5 after KRA), chronic heart failure (2.1, 1.3), arrhythmia (1.8, 1.7), and atrial fibrillation (3.4, 2.1) than in patients who did not. The VTE incidence in patients with chemoprophylaxis was higher than that in patients without chemoprophylaxis. The incidence of VTEs revealed in this retrospective review was not low compared with the results of the studies targeting other Asian or Caucasian populations. It may warrant routine prevention including employment of chemoprophylaxis. However, the limitation of the reviewed data mandates large scale prospective investigation to affirm this observation.
Keywords: Venous Thromboembolism, Replacement Arthroplasty, Hip, Knee, Chemoprophylaxis, Korea
Graphical Abstract
INTRODUCTION
Postoperative venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is a serious and potentially life-threatening complication and an important safety issue in acute care hospitals (1). Among major surgical procedures, hip and knee replacement arthroplasty (HKRA) carries the greatest risk of VTE. In the absence of prophylactic therapy, the incidence of postoperative VTE is particularly high after lower extremity arthroplasty. The incidence of imaging-confirmed asymptomatic DVT was known to vary from 42% to 57% after hip arthroplasty, and from 41% to 85% after knee arthroplasty. The incidence of PE varies from 0.9% to 28% after hip arthroplasty, and from 1.5% to 10% after knee arthroplasty (2). Clinically significant symptomatic VTE has been reported to be less common (2,3).
It has been suggested that there is a substantially lower incidence of VTE after HKRA in Asian populations compared with Western populations (4,5,6). However, in recent multicenter prospective studies performed in Asia, incidences of VTE after major orthopedic surgery including arthroplasty were comparable to those in Western populations (7,8,9). Moreover, there are few reports on the incidence of clinically-relevant symptomatic VTE after HKRA in East Asian patients (5,6). To determine to use thromboprophylactic agents routinely after HKRA, a study of symptomatic VTE in a large number of patients is necessary. There is marked discrepancy among reference studies. Major confounding factors might be various diagnostic modalities with different sensitivity, monitoring duration, lack of information on the use of mechanical device, study design, and surgeon vigilance.
In this study, we evaluated nationwide data regarding the incidence of VTE after HKRA in Korea using the administrative claims database of the Health Insurance Review and Assessment Service (HIRA), which comprises fully adjudicated medical and pharmacy claims for 50 million beneficiaries in Korea. Every clinic, hospital, and pharmacy in Korea is obliged to submit patient data regarding healthcare services and medical costs to the HIRA for reimbursement (10). Therefore, almost all clinically-relevant VTE events can be identified by analyzing the HIRA database.
The aim of this study was to examine the incidence and trends of clinically-relevant VTE including PE among patients who had undergone HKRA in Korea.
MATERIALS AND METHODS
Data source
We analyzed the Korean National Health Insurance (NHI) claims database from HIRA, which examines the accuracy of claims for NHI and National Medical Aid (NMA) programs. The NHI database includes the entire Korean population (approximately 96.6% of the entire 48.6 million population as well as registered foreign-nationals) as a compulsory insurance system, with exceptions for cases applicable to the NMA program covering the remaining 3.4% of the population and foreign military personnel. The claims data covered by NMA program are also reviewed by HIRA. Thus, nearly all information about patients is available from the HIRA database. Information in the HIRA database includes a unique identification number for each patient, age, sex, and all medical services rendered, along with the diagnostic code (based on the International Classification of Diseases, ICD, Tenth Edition), all prescription medications dispensed (based on code for drug ingredient), and procedure history (based on electronic data interchange [EDI] code). Additional information includes hospital type where the surgery was performed and the duration of hospitalization.
Study population and baseline characteristics
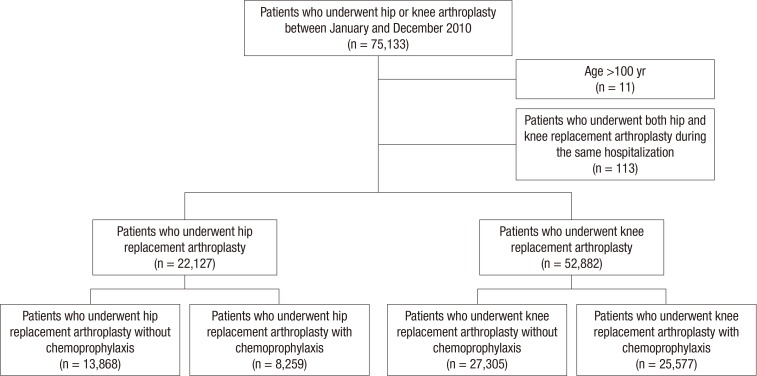
We identified 22,127 patients who underwent hip replacement arthroplasty (HRA) and 52,882 patients who underwent knee replacement arthroplasty (KRA) at 882 hospitals nationwide between January 1 and December 31, 2010. The date of index surgery was defined as the initiation date of hospitalization for HKRA on claims registry data. HRA procedure codes included N0715 for primary bipolar hip hemiarthroplasty, N0711 for primary total hip arthroplasty, N1715 and N1725 for revision partial hip arthroplasty (acetabular or stem revision only), and N1711 and N1721 for revision total hip arthroplasty. KRA procedure codes included N2712 (primary unicompartmental knee arthroplasty), N2072 (primary total knee arthroplasty), N4712 and N4722 (revision partial knee arthroplasty), N3712 and N3722 (revision total knee arthroplasty). Patients over 100 yr of age and those who received HRA and KRA at the same hospitalization were excluded. The use of pharmacological VTE prophylaxis such as aspirin, fondaparinux, rivaroxaban, and low molecular weight heparin (LMWH) was identified for each patient. 37.3% of 22,127 HRA patients (n=8,259) and 48.4% of 52,882 KRA patients (n=25,577) had received chemoprophylaxis. The results of the patients in chemoprophylaxis group were assessed and compared with those of 13,868 HRA patients (62.7%) and 27,305 KRA patients (51.6%) who had not received chemoprophylaxis (Fig. 1). All clinically relevant VTE during hospitalization and 90 days after HKRA were recorded using the ICD-10 code classification (180, 182 for DVT; 126 for PE). Baseline characteristics and potential risk factors including patient age, sex, comorbidities, and surgery characteristics were summarized using descriptive statistics such as proportion, mean, and standard deviation. Items for baseline characteristics and preoperative morbidities of the patients were listed with reference to the Korean Guideline for the Prevention of VTE in 2010, Guideline for the Prophylaxis of Venous Thromboembolism in Hip Surgery Patients in 2011, American Academy of Orthopaedic Surgery (AAOS) guideline in 2011, 9th edition of the American College of Chest Physicians (ACCP) evidence-based clinical practice guideline, NICE guideline in 2010, and the literature. All listed items were reviewed by statisticians and clinical experts.
Fig. 1. Selection process and flowchart of study population. A flowchart shows the selection process of study population. A total of 22,127 patients who underwent hip replacement arthroplasty (HRA) and 52,882 patients who underwent knee replacement arthroplasty (KRA) at 882 hospitals nationwide were finally enrolled in the analysis between January 1 and December 31, 2010. Multiple hospitalizations were defined as one episode of hospitalizaton if the interval between the two successive hospitalizations was less than 2 days. Index procedure: the first replacement arthroplasty during the study period. Index date: the first date of hospitalization during which the index replacement arthroplasty was performed.
Statistical analyses
Hospital type was categorized into four groups (tertiary hospital, general hospital, hospital, and clinic). Independent t-test was used for comparison of continuous variables, and chi-square test or Fisher's exact test was used for categorical variables. The chi-square test of independence was used to evaluate the difference in the incidence among arthroplasty type; and the cumulative incidence of VTE was analyzed with the Kaplan-Meier method. Multivariate logistic regression was used to calculate the adjusted odds ratio. Chi-square test was performed to compare the incidence between patients with and without comorbidities. A P value <0.05 was considered statistically significant. SAS® statistical software version 9.2 (SAS Institute, Cary, NC, USA) was used for data management and statistical analyses.
Ethics statement
This study protocol was reviewed and approved by the institutional review board of the National Evidence-based Healthcare Collaborating Agency (NECAIRB 12-004-1) and Seoul National University Hospital (E-1304-066-482). The board waived informed consent from involved subjects.
RESULTS
The percent of female patients with knee replacement was higher than that with hip replacement. The age of most patients with hip replacement was evenly distributed between 45 and 84 yr, while more than half of the patients with knee replacement (52.1%) were between 65- and 74-yr-of-age. Hypertension showed the highest prevalence (57.1% to 72.5%) among past medical morbidities. Diabetes, coronary artery stenosis, malignancy and stroke also showed high prevalence. Most hip and knee replacements were performed in general and secondary level hospitals, whereas more hip replacements were performed in tertiary general hospitals (35.0%) than hospitals (22.8%) in the group receiving chemoprophylaxis. More than half of HRAs were primary bipolar hip hemiarthroplasty (57.2%) and one-third was primary total hip arthroplasty (32.3%). Regarding KRA, unilateral primary total knee arthroplasty comprised 54.2% of surgeries and bilateral total knee arthroplasty 39.3%. It was unknown whether the bilateral surgeries were simultaneous or staged. Regional anesthesia was used in 87.9% and packed red blood cells were transfused in 83.1%. In 96.1% of HKRA cases, platelets were not transfused. The mean duration of anesthesia was 2.9 hr for HRA and 2.8 hr for KRA. Gender ratio, age, VTE history, diabetes, stroke, hypertension, coronary artery stenosis, arrhythmia, anticoagulation therapy, surgical characteristics, and RBC transfusion differed between the group with chemoprophylaxis and the group without chemoprophylaxis among baseline characteristics (Table 1).
Table 1. Baseline characteristics of patients with hip and knee replacement.
| Parameters | Patients with knee replacement | Patients with knee replacement | ||||
|---|---|---|---|---|---|---|
| Chemoprophylaxis (-) (n = 13,868) |
Chemoprophylaxis (+) (n = 8,259) |
P value* | Chemoprophylaxis (-) (n = 27,305) |
Chemoprophylaxis (+) (n = 25,577) |
P value* | |
| No. (%) | No. (%) | No. (%) | No. (%) | |||
| Gender | 0.001 | 0.001 | ||||
| Male | 5,445 (39.3) | 3,052 (37.0) | 3,553 (13.0) | 2,927 (11.4) | ||
| Female | 8,423 (60.7) | 5,207 (63.0) | 23,752 (87.0) | 22,650 (88.6) | ||
| Age (yr)‡ | ||||||
| Mean ± SD | 68.6±15.2 | 69.6±14.2 | <0.001 | 68.5±7.7 | 68.6±7.0 | 0.333 |
| ≤ 44 | 1,145 (8.3) | 547 (6.6) | <0.001† | 141 (0.5) | 36 (0.1) | <0.001† |
| 45 ≤ age ≤ 64 | 3,433 (24.8) | 1,900 (23.0) | 7,070 (25.9) | 6,595 (25.8) | ||
| 65 ≤ age ≤ 74 | 3,456 (24.9) | 2,254 (27.3) | 14,222 (52.1) | 13,860 (54.2) | ||
| 75 ≤ age ≤ 84 | 4,077 (29.4) | 2,572 (31.1) | 5,700 (20.9) | 4,939 (19.3) | ||
| ≥ 85 | 1,757 (12.7) | 986 (11.9) | 172 (0.6) | 147 (0.6) | ||
| Past medical history | ||||||
| Venous thromboembolic event (<3 yr) | 317 (2.3) | 308 (3.7) | < 0.001 | 644 (2.4) | 759 (3.0) | < 0.001 |
| Surgical site infection (<3 yr) | 536 (3.9) | 328 (4.0) | 0.693 | 487 (1.8) | 424 (1.7) | 0.267 |
| Diabetes (<3 yr) | 5,600 (40.4) | 3,622 (43.9) | < 0.001 | 12,172 (44.6) | 11,817 (46.2) | < 0.001 |
| Stroke (<3 yr) | 2,534 (18.3) | 1,746 (21.1) | < 0.001 | 3,449 (12.6) | 3,216 (12.6) | 0.842 |
| Renal disease (<3 yr) | 800 (5.8) | 567 (6.9) | 0.001 | 1,305 (4.8) | 1,253 (4.9) | 0.522 |
| Hypertension (<3 yr) | 7,912 (57.1) | 5,322 (64.4) | < 0.001 | 18,691 (68.5) | 18,551 (72.5) | < 0.001 |
| Coronary artery stenosis ( < 3 yr) | 2,819 (20.3) | 2,216 (26.8) | <0.001 | 6,545 (24.0) | 6,683 (26.1) | < 0.001 |
| Chronic heart failure, congestive heart failure (<3 yr) | 1,012 (7.3) | 794 (9.6) | < 0.001 | 2,003 (7.3) | 1,819 (7.1) | 0.321 |
| Arrhythmia (<3 yr) | 828 (6.0) | 629 (7.6) | < 0.001 | 1,862 (6.8) | 1,900 (7.4) | 0.007 |
| Atrial fibrillation ( < 3 yr) | 455 (3.3) | 486 (5.9) | < 0.001 | 736 (2.7) | 750 (2.9) | 0.100 |
| Malignancy (≤3 yr) | 1,616 (11.7) | 970 (11.7) | 0.837 | 2,230 (8.2) | 2,043 (8.0) | 0.450 |
| Varicose vein (<3 yr) | 127 (0.9) | 99 (1.2) | 0.043 | 708 (2.6) | 724 (2.8) | 0.092 |
| Hormone therapy (≤1 yr) | 368 (2.7) | 247 (3.0) | 0.140 | 892 (3.3) | 857 (3.4) | 0.590 |
| Anticoagulation therapy (<6 mo) | 751 (5.4) | 718 (8.7) | < 0.001 | 1,109 (4.1) | 1,386 (5.4) | < 0.001 |
| Surgical characteristics | ||||||
| Hospital pattern (level of reference) | <0.001 | <0.001 | ||||
| Tertiary general hospital | 2,569 (18.5) | 2,890 (35.0) | 3,259 (11.9) | 3,320 (13.0) | ||
| General hospital | 6,209 (44.8) | 3,444 (41.7) | 7,176 (26.3) | 6,382 (25.0) | ||
| Hospital | 4,798 (34.6) | 1,887 (22.8) | 15,336 (56.2) | 15,407 (60.2) | ||
| Clinic | 292 (2.1) | 38 (0.5) | 1,534 (5.6) | 468 (1.8) | ||
| Type of surgery | <0.001† | <0.001† | ||||
| HRA: Primary bipolar hip hemiarthroplasty | 8,256 (59.5) | 4,399 (53.3) | ||||
| HRA: Primary total hip arthroplasty | 4,248 (30.6) | 2,904 (35.2) | ||||
| HRA: Revision partial hip arthroplasty | 508 (3.7) | 364 (4.4) | ||||
| HRA: Revision total hip arthroplasty | 856 (6.2) | 592 (7.2) | ||||
| KRA: Primary unicompartmental knee arthroplasty | 735 (2.7) | 580 (2.3) | ||||
| KRA: Unilateral primary total knee arthroplasty | 15,784 (57.8) | 12,869 (50.3) | ||||
| KRA: Bilateral primary total knee arthroplasty | 9,600 (35.2) | 11,169 (43.7) | ||||
| KRA: Revision partial knee arthroplasty | 364 (1.3) | 334 (1.3) | ||||
| KRA: Revision total knee arthroplasty | 822 (3.0) | 625 (2.4) | ||||
| Anesthesia§ | <0.001† | <0.001† | ||||
| Regional anesthesia | 11,209 (80.8) | 6,450 (78.1) | 24,512 (89.8) | 23,744 (92.8) | ||
| General anesthesia | 2,659 (19.2) | 1,809 (21.9) | 2,793 (10.2) | 1,833 (7.2) | ||
| RBC transfusion (unit) | ||||||
| Mean±SD | 3.5±2.8 | 4.0±3.1 | <0.001 | 3.5±2.1 | 4.3±2.7 | <0.001 |
| 0 | 2,198 (15.8) | 1,205 (14.6) | <0.001† | 5,498 (20.1) | 3,782 (14.8) | <0.001† |
| 0<RBC≤3 | 7,520 (54.2) | 3,792 (45.9) | 12,948 (47.4) | 9,918 (38.8) | ||
| >3 | 4,150 (29.9) | 3,262 (39.5) | 8,859 (32.4) | 11,877 (46.4) | ||
| Platelet transfusion (unit) | ||||||
| Mean±SD | 8.7±13.7 | 7.4±11.2 | 0.728 | 6.3±8.9 | 6.1±9.7 | <0.001 |
| 0 | 12,802 (92.3) | 7,535 (91.2) | <0.001† | 26,612 (97.5) | 25,110 (98.2) | <0.001† |
| 0<Platelet concentrate≤3 | 521 (3.8) | 341 (4.1) | 389 (1.4) | 263 (1.0) | ||
| 3<Platelet concentrate≤10 | 293 (2.1) | 246 (3.0) | 190 (0.7) | 141 (0.6) | ||
| >10 | 252 (1.8) | 137 (1.7) | 114 (0.4) | 63 (0.2) | ||
| Duration of anesthesia (hr)∥ | ||||||
| Mean±SD | 2.9±2.0 | 3.0±2.1 | 0.242 | 2.9±1.7 | 2.7±1.7 | <0.001 |
| <2.5 | 2,188 (15.8) | 1,223 (14.8) | 0.005† | 3,124 (11.4) | 3,994 (15.6) | <0.001† |
| 2.5≤duration<4 | 6,845 (49.4) | 4,262 (51.6) | 9,843 (36.0) | 7,912 (30.9) | ||
| ≥4 | 4,810 (34.7) | 2,767 (33.5) | 14,044 (51.4) | 13,660 (53.4) | ||
†Independent t-test for continuous variables; †Chi-square test or Fisher's exact test for categorical variables; ‡Age at Index date of arthroplasty; §Defined as general anesthesia if inhalant was used; ∥No record of anesthesia duration : hip (n=32), Knee (n=305).
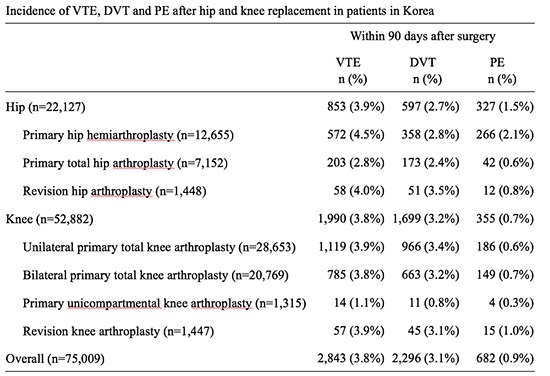
The overall incidence of VTE, DVT, and PE during the 90 days after HRA was 3.9% (853 of 22,127), 2.7% (597 of 22,127), and 1.5% (327 of 22,127), respectively. During hospitalization, 70.3% of VTE, 69.7% of DVT, 66.7% of PE developed. After KRA, the incidence of VTE, DVT, and PE during 90 days was 3.8% (1,990 of 52,882), 3.2% (1,699 of 52,882), and 0.7% (355 of 52,882). During hospitalization, 77.7% of VTE, 79.5% of DVT, and 63.7% of PE developed (Table 2).
Table 2. Incidence of VTE in hospitalization and within 90 days after hip and knee replacement.
| Type of surgery | Within 90 days after surgery | In hospitalization | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VTE | P value* | DVT | P value* | PE | P value* | VTE | P value* | DVT | P value* | PE | P value* | |
| Hip (n=22,127) | 853 (3.9%) | 597 (2.7%) | 327 (1.5%) | 600 (2.7%) | 416(1.9%) | 218 (1.0%) | ||||||
| Primary hip hemiarthroplasty (n=12,655) | 572 (4.5%) | <0.001 | 358 (2.8%) | 0.040 | 266 (2.1%) | <0.001 | 381 (3.0%) | 0.002 | 232 (1.8%) | 0.028 | 175 (1.4%) | <0.001 |
| Primary total hip arthroplasty (n=7,152) | 203 (2.8%) | 173 (2.4%) | 42 (0.6%) | 157 (2.2%) | 132 (1.8%) | 30 (0.4%) | ||||||
| Revision hip arthroplasty (n=1,448) | 58 (4.0%) | 51 (3.5%) | 12 (0.8%) | 47 (3.2%) | 41 (2.8%) | 8 (0.6%) | ||||||
| Knee (n=52,882) | 1,990 (3.8%) | 1,699 (3.2%) | 355 (0.7%) | 1547 (2.9%) | 1,351(2.6%) | 226 (0.4%) | ||||||
| Unilateral primary total knee arthroplasty (n=28,653) | 1,119 (3.9%) | <0.001 | 966 (3.4%) | <0.001 | 186 (0.6%) | 0.097 | 867 (3.0%) | <0.001 | 769 (2.7%) | <0.001 | 114 (0.4%) | 0.293 |
| Bilateral primary total knee arthroplasty (n=20,769) | 785 (3.8%) | 663 (3.2%) | 149 (0.7%) | 615 (3.0%) | 528 (2.5%) | 100 (0.5%) | ||||||
| Primary unicompartmental knee arthroplasty (n=1,315) | 14 (1.1%) | 11 (0.8%) | 4 (0.3%) | 11 (0.8%) | 8 (0.6%) | 3 (0.2%) | ||||||
| Revision knee arthroplasty (n=1,447) | 57 (3.9%) | 45 (3.1%) | 15 (1.0%) | 42 (2.9%) | 35 (2.4%) | 8 (0.6%) | ||||||
| Overall (n=75,009) | 2,843 (3.8%) | 2,296 (3.1%) | 682 (0.9%) | 2,147 (2.9%) | 1,767 (2.4%) | 444 (0.6%) | ||||||
*Chi-square homogeneous test for comparing the incidence among types of arthroplasties within the category of hip or knee. VTE, Venous thromboembolism; DVT, Deep vein thrombosis; PE, Pulmonary embolism.
Postoperative VTE and PE occurred the most frequently after primary hip hemiarthroplasty; and the incidence of DVT was the highest after revision hip arthroplasty. PE incidence after hemiarthroplasty was more than twice that of primary total or revision hip arthroplasty. VTE incidence after KRA was similar among unilateral primary total knee arthroplasty, bilateral primary total knee arthroplasty, and revision knee arthroplasty. DVT occurred the most frequently after unilateral primary total knee arthroplasty; and PE incidence was the highest after revision knee arthroplasty. VTE, DVT and PE incidence of primary unicompartmental knee arthroplasty was the lowest among various types of knee surgery (Table 2).
Chemoprophylaxis was used for VTE prevention more frequently in KRA (48.4%) than in HRA (37.3%). The incidence of VTE of the group with chemoprophylaxis was compared with that of the group without chemoprophylaxis. VTE, DVT and PE incidence was significantly higher in the group with chemoprophylaxis. Every incidence by the type of surgery was higher in chemoprophylaxis group except for PE incidence after the revision knee arthroplasty (Table 3).
Table 3. Comparison of the VTE incidence according to chemoprophylaxis use after hip and knee replacement.
| Type of surgery | VTE | DVT | PE | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Chemoprophylaxis | P value* | Chemoprophylaxis | P value* | Chemoprophylaxis | P value* | ||||
| (-) | (+) | (-) | (+) | (-) | (+) | ||||
| Hip (n = 22,127) | 274 (2.0%) | 579 (7.0%) | < 0.001 | 177 (1.35%) | 420 (5.1%) | < 0.001 | 121 (0.9%) | 206 (2.5%) | < 0.001 |
| Primary hip hemiarthroplasty | 198 (2.4%) | 374 (8.5%) | < 0.001 | 116 (1.4%) | 242 (5.5%) | < 0.001 | 102 (1.2%) | 164 (3.7%) | < 0.001 |
| Primary total hip arthroplasty | 58 (1.4%) | 145 (5.0%) | < 0.001 | 46 (1.1%) | 127 (4.4%) | < 0.001 | 15 (0.4%) | 27 (0.9%) | 0.002 |
| Revision total hip arthroplasty | 13 (1.5%) | 45 (7.6%) | < 0.001 | 11 (1.3%) | 40 (6.8%) | < 0.001 | 3 (0.4%) | 9 (1.5%) | 0.016 |
| Knee (n = 52,882) | 406 (1.5%) | 1,584 (6.2%) | < 0.001 | 326 (1.2%) | 1,373 (5.4%) | < 0.001 | 103 (0.4%) | 252 (1.0%) | < 0.001 |
| Unilateral primary total knee arthroplasty | 250 (1.6%) | 869 (6.8%) | < 0.001 | 201 (1.3%) | 765 (5.9%) | < 0.001 | 58 (0.4%) | 128 (1.0%) | < 0.001 |
| Bilateral primary total knee arthroplasty | 132 (1.4%) | 653 (5.8%) | < 0.001 | 107 (1.1%) | 556 (5.0%) | < 0.001 | 36 (0.4%) | 113 (1.0%) | < 0.001 |
| Primary unicompartmental knee arthroplasty | 2 (0.3%) | 12 (2.1%) | 0.002† | 2 (0.3%) | 9 (1.6%) | 0.014† | 0 (0.0%) | 4 (0.7%) | 0.038† |
| Revision knee arthroplasty | 20 (2.4%) | 37 (5.9%) | < 0.001 | 14 (1.7%) | 31 (5.0%) | < 0.001 | 9 (1.1%) | 6 (1.0%) | 0.802 |
| Overall (n = 75,009) | 680 (1.7%) | 2,163 (6.4%) | <0.001 | 503 (1.2%) | 1,793 (5.3%) | <0.001 | 224 (0.5%) | 458 (1.4%) | <0.001 |
*Chi-square homogeneous test for comparing the incidence between chemoprophylaxis (-) group and chemoprophylaxis (+) group; †Fisher' exact test. VTE, Venous thromboembolism; DVT, Deep vein thrombosis; PE, Pulmonary embolism.
The incidence of VTE, DVT, and PE after HKRA was significantly higher in patients who had previous VTE history, chronic heart failure, arrhythmia, and atrial fibrillation than those in patients who did not have those risk factors (Tables 4 and 5). Previous VTE history was the strongest risk factor of VTE and PE for both HRA (OR, 10.8 and 9.7) and KRA (OR, 8.5 and 8.6).
Table 4. Incidence of VTE after hip replacement in patients with significant risk factors.
| Risk factors | VTE | DVT | PE | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. (%) | OR (CI) | P value* | No. (%) | OR (CI) | P value* | No. (%) | OR (CI) | P value* | |
| VTE history | |||||||||
| Yes (n = 317) | 121 (19.4) | 10.8 (8.4-13.8) | < 0.001 | 84 (13.4) | 9.2 (6.9-12.0) | < 0.001 | 53 (8.5) | 9.7 (6.9-13.5) | < 0.001 |
| No (n = 13,551) | 732 (3.4) | 513 (2.4) | 274 (1.3) | ||||||
| Chronic heart failure | |||||||||
| Yes (n = 1,012) | 114 (6.3) | 2.1 (1.7-2.6) | < 0.001 | 63 (3.5) | 1.5 (1.2-2.0) | 0.002 | 58 (3.2) | 2.8 (2.1-3.8) | < 0.001 |
| No (n = 12,856) | 739 (3.6) | 534 (2.6) | 269 (1.3) | ||||||
| Arrhythmia | |||||||||
| Yes (n = 828) | 84 (5.8) | 1.8 (1.4-2.2) | < 0.001 | 56 (3.8) | 1.7 (1.2-2.2) | < 0.001 | 38 (2.6) | 2.1 (1.5-3.0) | < 0.001 |
| No (n = 13,040) | 769 (3.7) | 541 (2.6) | 289 (1.4) | ||||||
| Atrial fibllation | |||||||||
| Yes (n = 455) | 78 (8.3) | 3.4 (2.6-4.4) | < 0.001 | 46 (4.9) | 2.6 (1.9-3.6) | < 0.001 | 42 (4.5) | 4.7 (3.3-6.6) | < 0.001 |
| No (n = 13,413) | 775 (3.7) | 551 (2.6) | 285 (1.3) | ||||||
*Chi-square test for comparing the incidence between patients with and without disease history. VTE, Venous thromboembolism; DVT, Deep vein thrombosis; PE, Pulmonary embolism.
Table 5. Incidence of VTE after knee replacement in patients with significant risk factors.
| Risk factors | VTE | DVT | PE | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. (%) | OR (CI) | P value* | No. (%) | OR (CI) | P value* | No. (%) | OR (CI) | P value* | |
| VTE history | |||||||||
| Yes (n = 644) | 241 (17.2) | 8.5 (7.2-10.1) | < 0.001 | 199 (14.2) | 7.5 (6.3-9.0) | < 0.001 | 57 (4.1) | 8.6 (6.3-11.6) | < 0.001 |
| No (n = 26,661) | 1,749 (3.4) | 1,500 (2.9) | 298 (0.6) | ||||||
| Chronic heart failure | |||||||||
| Yes (n = 2,003) | 182 (4.8) | 1.3 (1.1-1.5) | 0.001 | 132 (3.5) | 1.1 (0.9-1.3) | 0.479 | 62 (1.6) | 2.7 (2.0-3.6) | < 0.001 |
| No (n = 25,302) | 1,808 (3.7) | 1,567 (3.2) | 293 (0.6) | ||||||
| Arrhythmia | |||||||||
| Yes (n = 1,862) | 206 (5.5) | 1.7 (1.4-1.9) | < 0.001 | 172 (4.6) | 1.6 (1.3-1.9) | < 0.001 | 45 (1.2) | 2.0 (1.4-2.8) | < 0.001 |
| No (n = 25,443) | 1,784 (3.6) | 1,527 (3.1) | 310 (0.6) | ||||||
| Atrial fibllation | |||||||||
| Yes (n = 736) | 101 (6.8) | 2.1 (1.7-2.6) | < 0.001 | 78 (5.2) | 1.8 (1.4-2.3) | < 0.001 | 29 (2.0) | 3.3 (2.2-4.9) | < 0.001 |
| No (n = 26,569) | 1,889 (3.7) | 1,621 (3.2) | 326 (0.6) | ||||||
*Chi-square test for comparing the incidence between patients with and without disease history. VTE, Venous thromboembolism; DVT, Deep vein thrombosis; PE, Pulmonary embolism.
DISCUSSION
The incidence of clinically relevant VTE, DVT and PE following HKRA was 3.8%, 3.1%, and 0.9%, respectively in the present study. More than half of the VTEs occurred during hospitalization. DVT was found more frequently after KRA whereas the incidence of PE after HRA was higher than that after KRA. Chemoprophylaxis was done for VTE prevention more frequently in KRA than HRA. The difference between prophylaxis and non-prophylaxis group makes it difficult to draw firm conclusion on the matter of routinely using chemoprophylaxis. Incidence of postoperative VTE varies extensively in the literature, not only by ethnic differences and the characteristics of the population, but also by the diagnostic modalities such as venography, CT scan, or duplex ultrasonography, presence of symptoms, the location of the thrombosis, the postoperative monitoring duration, and the use of mechanical preventive devices. The results may have been biased similarly in this study.
With all these limitations considered, however, the most important finding was that the incidence of VTE, DVT and PE was not low compared to the incidence in other Asian or Western population studies. This interpretation is mainly based upon the high incidence of VTE in the group of patients who received chemoprophylaxis. The incidence of VTE and DVT that was 7.0%, 5.1% for HRA and 6.2%, 5.4% for KRA, and the incidence of PE that was 2.5% and 1.0% was comparable to those in the high incidence population in the literature. VTE incidence after HKRA decreased dramatically in the past two to three decades and several recent studies showed 0.5%-4.5% PE rate after HRA and 0.0~1.0% after KRA without chemoprophylaxis (11). Even lower rates were shown in a systematic review where symptomatic VTE and PE were 0.5%-1.1% and 0.1%-0.3% respectively with chemoprophylaxis (1). A Western population-based registry data has shown clinically significant VTE as 2.3% after total hip arthroplasty and 1.8% after total knee arthroplasty (12). A meta-analysis of Asian population studies revealed the pooled rate of proximal DVT as 8.9% using venography and 5.9% by ultrasonography (13). Symptomatic PE was 0.6% in the same study. Overall VTE in this study included events diagnosed with various modalities although they lacked specific information for individual patient. As indicated in other studies with similar methodology, HIRA database has also possibilities that clinicians had diagnosed the patients as having VTE by clinical suspicion only, not by using objective diagnostic methods (14).
Along with the possible overestimation of the VTE incidence, there is also possibility of underestimation in this study as there was no way to identify the number of undiagnosed VTE in the population. The observed VTE incidence in the group without prophylaxis was comparable with the relatively low incidence from several Asian studies. A meta-analysis showed a pooled incidence rate as low as 5.8% for proximal DVT diagnosed by venography and 1.9% for symptomatic DVT after KRA in Asian patients which coincides with the results of non-prophylaxis group in the present study (6). Recent Asian studies showed that the incidence of all DVT was 8%-49% in patients not receiving chemoprophylaxis (15,16,17). The relatively low incidence of VTE in Asian studies has prompted the disagreement on routine chemoprophylaxis after HKRA (18,19,20). The low incidence of VTE in Asians is known to be attributed to the low incidence of obesity and hyperlipidemia as well as the scarcity of some genetic factors (4,19). The current practice includes early postoperative mobilization, the use of stockings and pneumatic compression pumps which may help prevent VTE (21,22).
Given that the rate of symptomatic PE and sudden death are the ultimate targets of VTE prophylaxis and whether an ethnic difference in the incidence of PE exists is still inconclusive, it is vital to explore the incidence of these parameters. The incidence of fatal PE in Western studies appears to have decreased dramatically when compared to the past records due to early mobilization. In one study by Charnley, the PE was 7.8%, despite various approaches of chemical prophylaxis (23). Reported estimates of symptomatic PE in a more recent meta-analysis with Western populations were 0%-1.5% after HRA and 0%-1.3% after KRA with or without chemoprophylaxis (24,25). Data of the Scottish Arthroplasty Registry revealed an incidence of fatal PE during 90 days was 0.2% after HRA and 0.2% after KRA (12). Several studies conducted in the United Kingdom with over 1,000 patients reported rates of fatal PE varying from 0.1%-0.4% without chemical prophylaxis after HKRA (26,27). For Asian subjects, two large-scale trials reported rates of symptomatic PE as 0.5% and 0.4% (7,8). Two recent meta-analyses showed that the rate of symptomatic PE was 0.6% (0%-2.5%) and 0.01% (0.01%-2.9%) (6,13). The observed PE incidence ranging from 0.0 to 3.7% in the present study corresponded to approximately one third that of VTE and this incidence was not low regardless of chemoprophylaxis. The PE incidence in the patients with prophylaxis was rather comparable to that reported in numerous earlier Western studies, whether they were symptomatic or not.
It is notable that overall VTE incidence during 90 days was lower after KRA than after HRA. Bipolar hip hemiarthroplasty and revision surgery of the knee carried a higher risk of VTE and PE occurrence than total hip replacement surgery, revision hip replacement arthroplasty and other type of knee replacement surgeries. Higher incidence of overall VTE after KRA than HRA has been demonstrated in many Western and Asian populations studies (1,7,8,28). High incidence of VTE and PE in bipolar hip hemiarthroplasty is explained in part by the fact that it corresponds to the surgery for hip fracture. Hip fracture surgery has shown greater risk for VTE than THA (7,8). We also should note that the gap between HRA and KRA became smaller or the rates were reversed concerning proximal or symptomatic DVT or PE in those studies (12,13). It may be due to the size and location of thrombi and postoperative mobilization. The size of their thrombi were smaller and less occlusive after KRA, which caused fewer symptoms than HRA (29).
Another finding was that 20% to 35% of VTE occurred after discharge from the hospital. It has already been proposed that the prophylaxis must be continued after discharge as the risk persists. This vigilance is heightened if the hospitalization is rather short-term as in most western countries where the DVT prophylaxis is mainly post-discharge procedure. The exact duration and selection criteria of at-risk patients for post-discharge chemoprophylaxis, however, is uncertain. The current ACCP thromboprophylaxis guideline recommends extension of prophylactic period for up to 35 days (30). Duration of chemoprophylaxis should be determined considering the cumulative incidence of postoperative VTE that changes with prophylaxis. There is general agreement that the risk of VTE is the highest soon after HKRA during hospitalization and the incidence of asymptomatic DVT decreases as the duration of postoperative prophylaxis increases (31). We should also consider the duration of hospitalization in Asian studies is generally longer than that reported in Western studies. In an Asian multicenter study including 835 patients, no symptomatic VTE occurrence was evident between hospital discharge and 3 months after surgical procedure, in which study the duration of hospital stay was 12-15 days (8). In the current study, the mean duration of hospital stay was 19.2 days for primary total hip replacement arthroplasty and 20.2 days for total knee replacement arthroplasty including bilateral cases.
Previous history of VTE, chronic heart failure, arrhythmia, and atrial fibrillation were risk factors identified in this study. They are well known factors from other studies (32). The odds ratio of the incidence of VTE for patients with previous VTE history in this study was 10.8 after HRA and 8.5 for KRA patients when compared to subjects without VTE history. This finding justifies the routine use of chemical prophylaxis for those selected patients. However, the individualized therapy that depends on risk factors has not yet been endorsed in western guidelines because the risk of orthopedic replacement surgery far outweighs patient-specific factors. A study conducted before 1990 reported that 'hospitalization with recent surgery' resulted in an odds ratio of 22 (33). The current clinical practice guidelines by the Korean Society of Thrombus and Hemostasis in 2014 stratified the joint replacement surgery as moderate risk group with weak recommendation of prophylaxis whereas they stratified the joint replacement surgery with previous VTE as high risk group (34).
This study has several limitations and weaknesses. The inherent limitation was that the evaluation of data relied solely on the EDI code input by the individual hospital; and the integrity of the information in the registry may vary depending on each hospital. The integrity of the data had been tested by correlating the authentic data in individual hospital and the input information, but the correlation was not possible. Also, only the items to be reimbursed by the insurance were involved, which meant that mechanical prophylaxis including pneumatic pumps and stockings was not included as they were not reimbursed by the insurance coverage. Subsequent over- or under-estimation of VTE incidence due to various factors is the serious limitation of this study. The data did not include the exact date and time of prophylaxis initiation, duration of prophylactic treatment, or the date of surgery. The timing of prophylactic treatment initiation can affect the efficacy of the anticoagulation along with the incidence of bleeding after hip surgery (35). Body mass index was not estimated as weight or height had not been recorded in the registry. Symptom severity of each patient was evaluated by the surgeon of each hospital and the criteria for positive symptomatic DVT or PE was not standardized.
In conclusion, this nationwide database enables an estimation of the incidence of total venous thromboembolic disease occurring in Korea after HKRA. The incidence of VTEs in this retrospective review was not low compared with the results of the studies targeting other Asian and Caucasian populations. It may warrant routine prevention including employment of chemoprophylaxis. However, the inconsistency and limitation of the data indicates true incidence may not have been revealed regardless of potential risks. A nationwide prospective investigation involving a large-scale controlled trial is required to affirm this reviewed data and to develop the necessary recommendations.
Footnotes
Funding: This study was supported by grants from the National Evidence-based Healthcare Collaborating Agency (NECA-B-12-003) and from the Seoul National University Hospital Research Fund (grant 3020130080).
DISCLOSURE: The authors declare that they have no potential conflicts of interest for this study.
AUTHOR CONTRIBUTION: Conception and design of the work: Lee, S, Ahn J, Yoo JJ. Acquisition of data: Hwang JI, Kim Y, Ahn J. Analysis of data: all authors. Drafting the manuscript: Lee S, Kim Y, Yoon PW, Ahn J. Revising and approval of the manuscript: all authors.
References
- 1.Januel JM, Chen G, Ruffieux C, Quan H, Douketis JD, Crowther MA, Colin C, Ghali WA, Burnand B IMECCHI Group. Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee arthroplasty among patients receiving recommended prophylaxis: a systematic review. JAMA. 2012;307:294–303. doi: 10.1001/jama.2011.2029. [DOI] [PubMed] [Google Scholar]
- 2.Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133:381S–453S. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 3.Eikelboom JW, Karthikeyan G, Fagel N, Hirsh J. American Association of Orthopedic Surgeons and American College of Chest Physicians guidelines for venous thromboembolism prevention in hip and knee arthroplasty differ: what are the implications for clinicians and patients? Chest. 2009;135:513–520. doi: 10.1378/chest.08-2655. [DOI] [PubMed] [Google Scholar]
- 4.Kim YH, Kim JS. The 2007 John Charnley Award. Factors leading to low prevalence of DVT and pulmonary embolism after THA: analysis of genetic and prothrombotic factors. Clin Orthop Relat Res. 2007;465:33–39. doi: 10.1097/BLO.0b013e318156bfac. [DOI] [PubMed] [Google Scholar]
- 5.Kang BJ, Lee YK, Kim HJ, Ha YC, Koo KH. Deep venous thrombosis and pulmonary embolism are uncommon in East Asian patients after total hip arthroplasty. Clin Orthop Relat Res. 2011;469:3423–3428. doi: 10.1007/s11999-011-1979-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee WS, Kim KI, Lee HJ, Kyung HS, Seo SS. The incidence of pulmonary embolism and deep vein thrombosis after knee arthroplasty in Asians remains low: a meta-analysis. Clin Orthop Relat Res. 2013;471:1523–1532. doi: 10.1007/s11999-012-2758-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leizorovicz A, Turpie AG, Cohen AT, Wong L, Yoo MC, Dans A SMART Study Group. Epidemiology of venous thromboembolism in Asian patients undergoing major orthopedic surgery without thromboprophylaxis. The SMART study. J Thromb Haemost. 2005;3:28–34. doi: 10.1111/j.1538-7836.2004.01094.x. [DOI] [PubMed] [Google Scholar]
- 8.Piovella F, Wang CJ, Lu H, Lee K, Lee LH, Lee WC, Turpie AG, Gallus AS, Planès A, Passera R, et al. Deep-vein thrombosis rates after major orthopedic surgery in Asia. An epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. J Thromb Haemost. 2005;3:2664–2670. doi: 10.1111/j.1538-7836.2005.01621.x. [DOI] [PubMed] [Google Scholar]
- 9.Leizorovicz A SMART Venography Study Steering Committee. Epidemiology of post-operative venous thromboembolism in Asian patients. Results of the SMART venography study. Haematologica. 2007;92:1194–1200. doi: 10.3324/haematol.10819. [DOI] [PubMed] [Google Scholar]
- 10.Lee YK, Ha YC, Park C, Yoo JJ, Shin CS, Koo KH. Bisphosphonate use and increased incidence of subtrochanteric fracture in South Korea: results from the National Claim Registry. Osteoporos Int. 2013;24:707–711. doi: 10.1007/s00198-012-2016-8. [DOI] [PubMed] [Google Scholar]
- 11.Kim KI, Kang DG, Khurana SS, Lee SH, Cho YJ, Bae DK. Thromboprophylaxis for deep vein thrombosis and pulmonary embolism after total joint arthroplasty in a low incidence population. Knee Surg Relat Res. 2013;25:43–53. doi: 10.5792/ksrr.2013.25.2.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howie C, Hughes H, Watts AC. Venous thromboembolism associated with hip and knee replacement over a ten-year period: a population-based study. J Bone Joint Surg Br. 2005;87:1675–1680. doi: 10.1302/0301-620X.87B12.16298. [DOI] [PubMed] [Google Scholar]
- 13.Kanchanabat B, Stapanavatr W, Meknavin S, Soorapanth C, Sumanasrethakul C, Kanchanasuttirak P. Systematic review and meta-analysis on the rate of postoperative venous thromboembolism in orthopaedic surgery in Asian patients without thromboprophylaxis. Br J Surg. 2011;98:1356–1364. doi: 10.1002/bjs.7589. [DOI] [PubMed] [Google Scholar]
- 14.Jang MJ, Bang SM, Oh D. Incidence of venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost. 2011;9:85–91. doi: 10.1111/j.1538-7836.2010.04108.x. [DOI] [PubMed] [Google Scholar]
- 15.Chen CJ, Wang CJ, Huang CC. The value of D-dimer in the detection of early deep-vein thrombosis after total knee arthroplasty in Asian patients: a cohort study. Thromb J. 2008;6:5. doi: 10.1186/1477-9560-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ko PS, Chan WF, Siu TH, Khoo J, Wu WC, Lam JJ. Deep venous thrombosis after total hip or knee arthroplasty in a "low-risk" Chinese population. J Arthroplasty. 2003;18:174–179. doi: 10.1054/arth.2003.50040. [DOI] [PubMed] [Google Scholar]
- 17.Sudo A, Sano T, Horikawa K, Yamakawa T, Shi D, Uchida A. The incidence of deep vein thrombosis after hip and knee arthroplasties in Japanese patients: a prospective study. J Orthop Surg (Hong Kong) 2003;11:174–177. doi: 10.1177/230949900301100212. [DOI] [PubMed] [Google Scholar]
- 18.Yokote R, Matsubara M, Hirasawa N, Hagio S, Ishii K, Takata C. Is routine chemical thromboprophylaxis after total hip replacement really necessary in a Japanese population? J Bone Joint Surg Br. 2011;93:251–256. doi: 10.1302/0301-620X.93B2.25795. [DOI] [PubMed] [Google Scholar]
- 19.Kim YH, Yoo JH, Kim JS. Factors leading to decreased rates of deep vein thrombosis and pulmonary embolism after total knee arthroplasty. J Arthroplasty. 2007;22:974–980. doi: 10.1016/j.arth.2007.03.033. [DOI] [PubMed] [Google Scholar]
- 20.Won MH, Lee GW, Lee TJ, Moon KH. Prevalence and risk factors of thromboembolism after joint arthroplasty without chemical thromboprophylaxis in an Asian population. J Arthroplasty. 2011;26:1106–1111. doi: 10.1016/j.arth.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Pearse EO, Caldwell BF, Lockwood RJ, Hollard J. Early mobilisation after conventional knee replacement may reduce the risk of postoperative venous thromboembolism. J Bone Joint Surg Br. 2007;89:316–322. doi: 10.1302/0301-620X.89B3.18196. [DOI] [PubMed] [Google Scholar]
- 22.Daniel J, Pradhan A, Pradhan C, Ziaee H, Moss M, Freeman J, McMinn DJ. Multimodal thromboprophylaxis following primary hip arthroplasty: the role of adjuvant intermittent pneumatic calf compression. J Bone Joint Surg Br. 2008;90:562–569. doi: 10.1302/0301-620X.90B5.19744. [DOI] [PubMed] [Google Scholar]
- 23.Johnson R, Green JR, Charnley J. Pulmonary embolism and its prophylaxis following the Charnley total hip replacement. Clin Orthop Relat Res. 1977;(127):123–132. [PubMed] [Google Scholar]
- 24.Freedman KB, Brookenthal KR, Fitzgerald RH, Jr, Williams S, Lonner JH. A meta-analysis of thromboembolic prophylaxis following elective total hip arthroplasty. J Bone Joint Surg Am. 2000;82-A:929–938. doi: 10.2106/00004623-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Westrich GH, Haas SB, Mosca P, Peterson M. Meta-analysis of thromboembolic prophylaxis after total knee arthroplasty. J Bone Joint Surg Br. 2000;82:795–800. doi: 10.1302/0301-620x.82b6.9869. [DOI] [PubMed] [Google Scholar]
- 26.Warwick D, Williams MH, Bannister GC. Death and thromboembolic disease after total hip replacement. A series of 1162 cases with no routine chemical prophylaxis. J Bone Joint Surg Br. 1995;77:6–10. [PubMed] [Google Scholar]
- 27.Ansari S, Warwick D, Ackroyd CE, Newman JH. Incidence of fatal pulmonary embolism after 1,390 knee arthroplasties without routine prophylactic anticoagulation, except in high-risk cases. J Arthroplasty. 1997;12:599–602. doi: 10.1016/s0883-5403(97)90131-5. [DOI] [PubMed] [Google Scholar]
- 28.Geerts WH, Heit JA, Clagett GP, Pineo GF, Colwell CW, Anderson FA, Jr, Wheeler HB. Prevention of venous thromboembolism. Chest. 2001;119:132S–175S. doi: 10.1378/chest.119.1_suppl.132s. [DOI] [PubMed] [Google Scholar]
- 29.Ascani A, Radicchia S, Parise P, Nenci GG, Agnelli G. Distribution and occlusiveness of thrombi in patients with surveillance detected deep vein thrombosis after hip surgery. Thromb Haemost. 1996;75:239–241. [PubMed] [Google Scholar]
- 30.Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, Ortel TL, Pauker SG, Colwell CW. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th Ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e278S–e325S. doi: 10.1378/chest.11-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kearon C. Duration of venous thromboembolism prophylaxis after surgery. Chest. 2003;124:386S–392S. doi: 10.1378/chest.124.6_suppl.386s. [DOI] [PubMed] [Google Scholar]
- 32.Pedersen AB, Sorensen HT, Mehnert F, Overgaard S, Johnsen SP. Risk factors for venous thromboembolism in patients undergoing total hip replacement and receiving routine thromboprophylaxis. J Bone Joint Surg Am. 2010;92:2156–2164. doi: 10.2106/JBJS.I.00882. [DOI] [PubMed] [Google Scholar]
- 33.Heit JA, Silverstein MD, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ., 3rd Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med. 2000;160:809–815. doi: 10.1001/archinte.160.6.809. [DOI] [PubMed] [Google Scholar]
- 34.Bang SM, Jang MJ, Kim KH, Yhim HY, Kim YK, Nam SH, Hwang HG, Bae SH, Kim SH, Mun YC, et al. Prevention of Venous Thromboembolism, 2nd Edition: Korean Society of Thrombosis and Hemostasis Evidence-Based Clinical Practice Guidelines. J Korean Med Sci. 2014;29:164–171. doi: 10.3346/jkms.2014.29.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Strebel N, Prins M, Agnelli G, Büller HR. Preoperative or postoperative start of prophylaxis for venous thromboembolism with low-molecular-weight heparin in elective hip surgery? Arch Intern Med. 2002;162:1451–1456. doi: 10.1001/archinte.162.13.1451. [DOI] [PubMed] [Google Scholar]