Abstract
Objective:
The deleterious effect of multiple-substance use on driving performance is well established, but relatively little research has examined the patterns of drug use among multiple-substance users and its relationship to both alcohol use and adverse driving outcomes.
Method:
The current study used latent class analysis to examine subgroups of substance users among a population of drivers who screened positively for 2 or more of 13 substances other than alcohol (N = 250). A series of logistic regression analyses was conducted to examine demographic predictors of latent class assignment and class association with adverse driving outcomes.
Results:
Four distinct subclasses of users were identified among multiple-substance-using drivers: Class 1 consisted of individuals who demonstrated high levels of all substances indicators (5%). The second class demonstrated high levels of marijuana and cocaine use and lower levels of all other substances (27%). The third class screened high for marijuana and nonmedical prescription opiate analgesics use (36%), whereas the last class demonstrated high nonmedical prescription opiate analgesics and benzodiazepine use (32%). Drivers in Class 2 (marijuana and cocaine users) were more likely to be younger and have a positive breath alcohol concentration than drivers in any other class.
Conclusions:
Because multidrug users show dissimilar characteristics, the propensity of researchers to lump all multiple-substance users together may either erroneously attribute the potentially profound impact of those in the marijuana and cocaine use class to all multiple-substance users or dilute their specific contribution to crash risk.
The nonmedical (i.e., not as directed by a physician) and/or recreational use of marijuana has seen a steady rise in recent years (Bostwick, 2012) to the point where marijuana is now the single most used illicit substance and has been found to be more widely used in the United States than in other parts of the world (United Nations Office on Drugs and Crime, 2011). In fact, in 2013, 8.1 million people age 12 and older reported using marijuana almost daily—up from 5.5 million just 5 years earlier; in addition, 19.1% of 18- to 25-year-olds in the United States reported having used marijuana in the prior year—up from 16.6% just 5 years earlier (Substance Abuse and Mental Health Services Administration, 2014). Furthermore, there is increasing momentum to legalize marijuana (Saad, 2014), likely resulting from increased social acceptance of the substance and its use. A few states (i.e., Alaska, Colorado, Oregon, and Washington) have implemented laws that make the possession and use of marijuana legal under state law (Office of National Drug Control Policy [ONDCP], 2014). In addition, 23 other states and Washington, DC, have passed laws allowing an individual to defend him- or herself against criminal charges of marijuana possession if that marijuana is used for one of a variety of specified medical conditions (ONDCP, 2014).
However, an extensive body of research has discussed the propensity of those using marijuana to use other substances as well (Bonn-Miller & Zvolensky, 2009; Nakawaki & Crano, 2012; Olthuis et al., 2013; Scherer et al., 2013b). This phenomenon has been studied in terms of marijuana and the concurrent use of other substances such as alcohol (Blows et al., 2005; Penning et al., 2010; Scherer et al., 2013b), cocaine (Higgins et al., 2007; Lindsay et al., 2009; Scherer et al., 2013a), and opioids (Subramaniam et al., 2010), which could potentially compound detrimental effects (Midanik et al., 2007). This is of particular concern when examining everyday activities such as driving. Indeed, although marijuana use itself has been associated with only slightly increased crash risk (Laumon et al., 2005; Li et al., 2012), drivers who use “multiple-drug combinations” have been found to be in the highest crash risk category (Hels et al., 2011). Further, some previous research has indicated that the crash contribution of marijuana alone disappeared after controlling for the presence of other substances (Penning et al., 2010), indicating that it may be the propensity of marijuana users to partake in multiple substances that is of particular concern when addressing impaired driving.
The growing popularity of marijuana may make it particularly likely to be used concurrently with other substances while driving. In fact, drivers ages 21 to 25 years are approximately 2.5 times more likely to use marijuana and other drugs and drive rather than to drink alcohol and drive (Fergusson et al., 2008). Given the documented risk associated with drivers who use multiple substances, understanding the demographic that is more likely to engage in concurrent substance use while driving could be critical in the creation and implementation of successful interventions to attempt to curtail this trend.
In addition, it is important to establish which groups of multiple-substance users are associated with the most risky behavior. For example, prior research has established the adverse impact of alcohol on driving performance (Blomberg et al., 2009; Borkenstein et al., 1974; Voas et al., 2012; Zador et al., 2000), and multiple-substance users are more likely than non-multiple-substance users to consume alcohol (Stinson et al., 2005). However, the propensity of researchers to lump all multiple-substance users together may inadvertently indicate that all multiple-substance users are equally dangerous and likely to consume alcohol regardless of the combination of substances. In fact, relatively little is known about how different groups of multiple-substance users compare to one another on measures of alcohol consumption and/or crash involvement. That is, it is unclear in the literature whether individuals who use multiple substances are as likely to consume alcohol, consume alcohol before driving, or be involved in crashes regardless of what combination of substances is being used. These are particularly important considerations given the growing public acceptance of marijuana and the subsequent increased probability of concurrent substance use while driving.
Despite the need for greater understanding of marijuana and concurrent substance use by drivers, research in this field has faced common obstacles. Of particular note has been the inherent difficulty of obtaining adequate data from substance-using drivers. Primarily, research on substance use while driving has frequently been collected from crash sites, hospitals, or arrest records. These sample sites, however, only identify individuals who used substances and then either were sent to the hospital for an injury or otherwise had an encounter with the police and subsequently do not provide an accurate picture of driving populations. Here, we examine a more representative data set to provide information on multiple-substance use among a national sample of drivers in the United States. Specifically, we will analyze that data to identify latent subgroups of multiple-substance users that are qualitatively different from each other and whose members share similar patterns in terms of which substances they use. Once these subgroups are established, we will compare them to determine differences among both driver characteristics and adverse driving outcomes (i.e., driving after drinking, history of drunk driving, and prior crash involvement). By doing so, we will gain a clearer understanding of whether certain subgroups of multiple-substance users are prone to alcohol consumption and/or adverse driving outcomes.
Method
The present study is a secondary analysis of the 2007 National Roadside Survey (NRS) data (Lacey et al. 2009). The NRS was a field study conducted throughout the 48 contiguous United States, examining rates of substance use among a random sample of daytime and nighttime weekend drivers. Participants completed self-report measures on demographics, substance use, and driving statistics and took biological measures including breath tests, oral fluid samples, and blood samples to screen for traces of a variety of substances. Data gathered by the NRS represent one of the first national prevalence estimates of substance use among active motor vehicle operators. For the current study, we used a subset of the total sample that provided demographic and substance use data on more than one substance (excluding alcohol). As the 2007 NRS is described in great detail elsewhere (Lacey et al., 2009), it will be outlined below only as it is directly relevant to the current study.
In the current research, we examined all active motor vehicle operators who tested positive on a biological measure of more than one substance. The sample was composed primarily of men (n = 157; 62.8%) and those who identified as White (n = 154; 61.6%). The average age of the participants was 33.62 years (SD = 13.43). Participants were randomly selected drivers at designated roadside survey stations (see Lacey et al., 2009, for additional information on survey sites and selection process). Drivers were flagged down by police officers who directed them to study personnel. Participants were told the study data were both anonymous and confidential and provided informed consent. Participants then completed questionnaires assessing prior use of 24 different substances and were asked to provide breath, oral fluid, and blood samples. Only data from NRS participants who screened positive for two or more substances were used in the current analyses. Participants were remunerated depending on their level of participation in the study ($5 to complete survey, an additional $10 to provide oral fluid samples, and an additional $50 to provide blood samples).
Measures
General demographics.
Participants self-reported demographic information including age, sex, race, and highest education level attained. Study personnel recorded the time of day in which data were gathered.
Substance use information.
Participants provided breath samples to determine breath alcohol concentration (BrAC) and provided oral fluid and/or blood samples, which were forwarded to the Immunalysis Corp. in Pomona, CA, for screening using enzyme-linked immunosorbent assays (ELISA) followed by verification of positive samples with mass spectral detection using liquid chromatography–mass spectrometry. In instances where participants provided invalid breath samples, oral fluid or blood samples were used in determining alcohol concentration. Approximately 50 substances were covered by this analysis (see Lacey, 2009, for detailed list), but in the current study the only substances examined were opiate analgesics (i.e., codeine, hydrocodone, meperidine, morphine, oxycodone, propoxyphene, and tramadol), tetrahydrocannabinol (THC—the principal psychoactive constituent found in marijuana), cocaine, heroin, methadone, lysergic acid diethylamide (LSD), methylenedioxymethamphetamine (MDMA [Ecstasy]), methamphetamine (meth), gamma hydroxybutyrate (GHB), phencyclidine (PCP), ketamine, benzodiazepines, and barbiturates.
Statistical analyses
Latent class analysis (LCA) is a method of data reduction used to identify groupings of individuals who show similar patterns or profiles of behavior (McCutcheon, 1987). LCA is commonly used in substance use and misuse research (Harrell et al., 2012; Schwartz et al., 2010). M-Plus 6.0 (Muthén & Muthén, 2010) was used for LCA modeling.
Based on software guidelines, we initially used 500 random starts to have high likelihood of obtaining global, rather than local, maxima. In the event the log likelihood was not replicated a minimum of five times, the number of starts was increased until this threshold was met (Muthén & Muthén, 2010). Multiple fit statistics are reported including Bayesian Information Criterion (BIC; Schwarz, 1978), Lo–Mendell–Rubin adjusted likelihood ratio test (LMR; Lo et al., 2001), and the parametric bootstrap likelihood ratio test (BLRT; MacLachlan & Peel, 2000). A lower BIC is generally preferred. LMR and BLRT both evaluate the increase in model fit between the k-1 and k class models (Nylund et al., 2007). In Monte Carlo simulations, the BLRT outperforms both the LMR and the BIC, but the LMR is more robust under a variety of model and distributional assumptions (Nylund et al., 2007). These fit statistics provide helpful guidelines for evaluating and choosing between models, but the choice of latent class solution was ultimately informed by substantive criteria involving the meaningfulness of the solution in terms of current drug use epidemiology (Petras & Masyn, 2010). Given established trends of reduced risk perception and increased usage of marijuana, class solution selection was also guided by usefulness in evaluating and discriminating between classes relevant to marijuana usage.
Entropy is reported as well. Although not designed for use in class selection, entropy was used to assess the utility of the classes and the appropriateness of the use of most likely latent class membership (MLLCM). Entropy ranges from 0 to 1, with higher scores representing better class separation (Celeux & Soromenho, 1996). MLLCM was used to export individual class membership to IBM SPSS Version 21.0 (IBM Corp., Armonk, NY). MLLCM can be an appropriate approach if entropy is high. A series of logistic regression analyses was conducted to determine differences between latent classes, demographics, BrAC levels, and driving statistics. With the exception of analyses that used these variables as predictors, all analyses controlled for race, sex, age, and time of day.
Latent class indicators
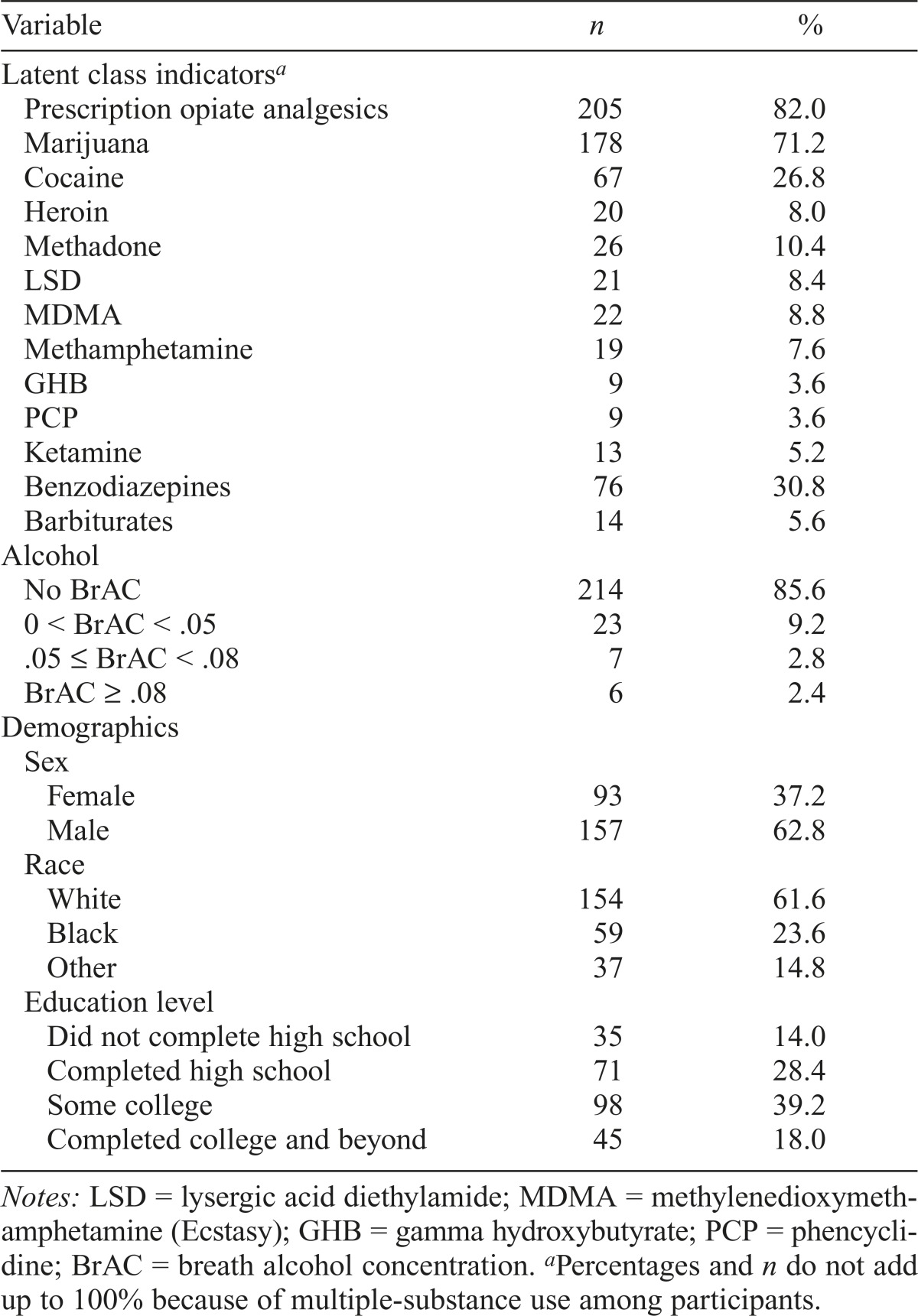
Latent classes were determined using presence of a variety of illicit and prescription substances (see Lacey et al., 2009, for a complete description) as indicated by screening of oral fluid and/or blood samples. Because of the relatively high rates of alcohol use in the NRS data set, alcohol was omitted as a latent class indicator. Latent class indicators and demographics are noted in Table 1.
Table 1.
Characteristics of positive screening among 250 active motor vehicle operators
| Variable | n | % |
| Latent class indicatorsa | ||
| Prescription opiate analgesics | 205 | 82.0 |
| Marijuana | 178 | 71.2 |
| Cocaine | 67 | 26.8 |
| Heroin | 20 | 8.0 |
| Methadone | 26 | 10.4 |
| LSD | 21 | 8.4 |
| MDMA | 22 | 8.8 |
| Methamphetamine | 19 | 7.6 |
| GHB | 9 | 3.6 |
| PCP | 9 | 3.6 |
| Ketamine | 13 | 5.2 |
| Benzodiazepines | 76 | 30.8 |
| Barbiturates | 14 | 5.6 |
| Alcohol | ||
| No BrAC | 214 | 85.6 |
| 0 < BrAC < .05 | 23 | 9.2 |
| .05 ≤ BrAC < .08 | 7 | 2.8 |
| BrAC ≥ .08 | 6 | 2.4 |
| Demographics | ||
| Sex | ||
| Female | 93 | 37.2 |
| Male | 157 | 62.8 |
| Race | ||
| White | 154 | 61.6 |
| Black | 59 | 23.6 |
| Other | 37 | 14.8 |
| Education level | ||
| Did not complete high school | 35 | 14.0 |
| Completed high school | 71 | 28.4 |
| Some college | 98 | 39.2 |
| Completed college and beyond | 45 | 18.0 |
Notes: LSD = lysergic acid diethylamide; MDMA = methylenedioxymethamphetamine (Ecstasy); GHB = gamma hydroxybutyrate; PCP = phencyclidine; BrAC = breath alcohol concentration.
Percentages and n do not add up to 100% because of multiple-substance use among participants.
Results
Class membership
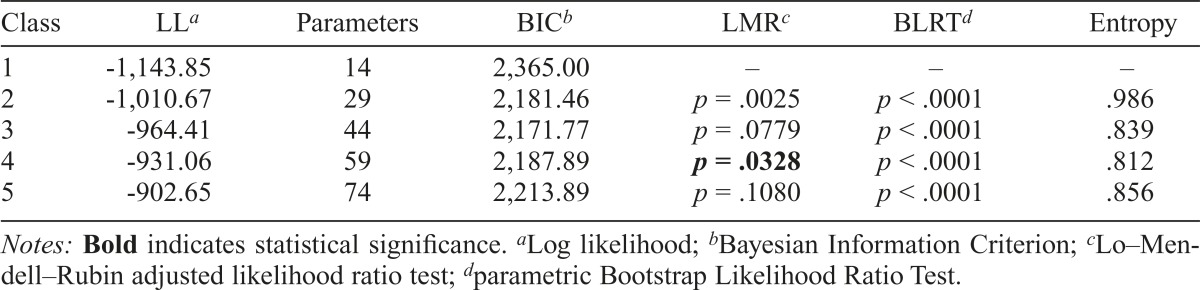
As seen in Table 2, according to the LMR, the two- and four-class models performed superior to the one- and three-class models, respectively (both p < .05), whereas there was a trend for the three-class model to perform superior to the two-class model (p = .078). In the two-class model, the first class consisted of individuals who had high probabilities of using all substances (5.3%), whereas the second class consisted of drivers who had high probabilities of using marijuana with cocaine (94.7%). BIC supported a three-class model, but evaluation of the three-and four-class models showed that substantive differences emerged, suggesting that the four-class model would yield more useful information, particularly in relation to marijuana use. The three-class model consisted of a class of individuals who demonstrated high probabilities of using all substances (5.3%), a class in which participants demonstrated high probabilities of using opiate analgesics and benzodiazepines (36.5%), and a third class in which participants demonstrated high probabilities of using primarily opiate analgesics and marijuana (58.2%). However, the four-class model was chosen given the results of the LMR and the increased specificity related to marijuana use, which was a goal of the analysis. The five-class model was not significantly better than the four-class model (p = .108).
Table 2.
Fit statistics for a latent class analysis of positive screening for five substances among active motor vehicle operators
| Class | LLa | Parameters | BICb | LMRc | BLRTd | Entropy |
| 1 | -1,143.85 | 14 | 2,365.00 | – | – | – |
| 2 | -1,010.67 | 29 | 2,181.46 | p = .0025 | p < .0001 | .986 |
| 3 | -964.41 | 44 | 2,171.77 | p = .0779 | p < .0001 | .839 |
| 4 | -931.06 | 59 | 2,187.89 | p = .0328 | p < .0001 | .812 |
| 5 | -902.65 | 74 | 2,213.89 | p = .1080 | p < .0001 | .856 |
Notes: Bold indicates statistical significance.
Log likelihood;
Bayesian Information Criterion;
Lo–Mendell–Rubin adjusted likelihood ratio test;
parametric Bootstrap Likelihood Ratio Test.
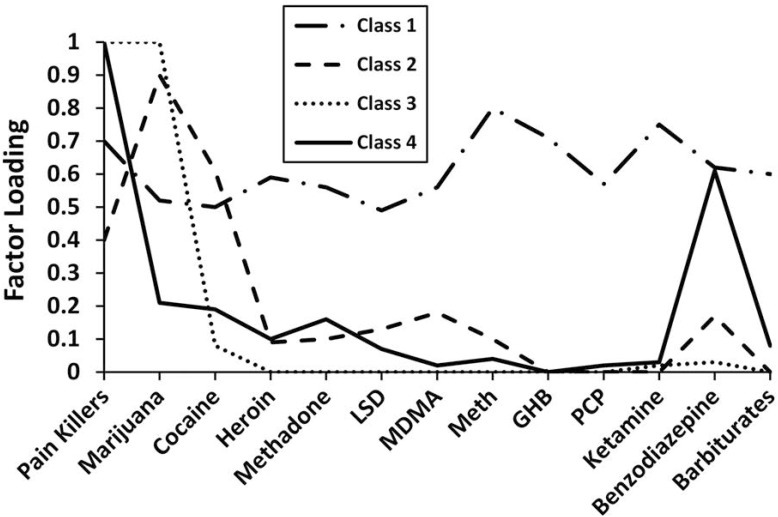
Class composition is better visualized in Figure 1. As noted in the figure, the first class of the four-class model, consisting of 5.2% of the sample, included high probabilities of positive screening for all substances examined in the current study. Thus, we refer to this class here as the polysubstance use (POLY) class. The second class, consisting of 27.2% of the sample, included participants with high probabilities of a positive screening for marijuana and cocaine with relatively low prevalence of any other substance. Thus, we refer to this class here as the marijuana and cocaine (MJ/CN) class. The third class, consisting of 35.6% of the sample, included participants with high probabilities for screening positive in their marijuana and opiate analgesics use. Thus, we refer to this class as the marijuana and opiate analgesics (MJ/OA) class. Finally, the fourth class, which consisted of 32% of the sample, included participants who screened positive for prescription opiate analgesics and benzodiazepines. Thus, we refer to the fourth class as the prescription opiate analgesics and benzodiazepines (POAB) class.
Figure 1.
Latent class factor loadings by substance use. Class 1 is the polysubstance (POLY) class and accounts for 5.2% of the study sample. Class 2 is the marijuana and cocaine (MJ/CN) class and accounts for 27.2% of the study sample. Class 3 is the marijuana and opiate analgesics (MJ/OA) class and accounts for 35.6% of the study sample. Finally, Class 4 is the prescription opiate analgesics and benzodiazepines (POAB) class and accounts for 32.0% of the study sample. LSD = lysergic acid diethylamide; MDMA = methylenedioxymethamphetamine (Ecstasy); meth = methamphetamine; GHB = gamma hydroxybutyrate; PCP = phencyclidine.
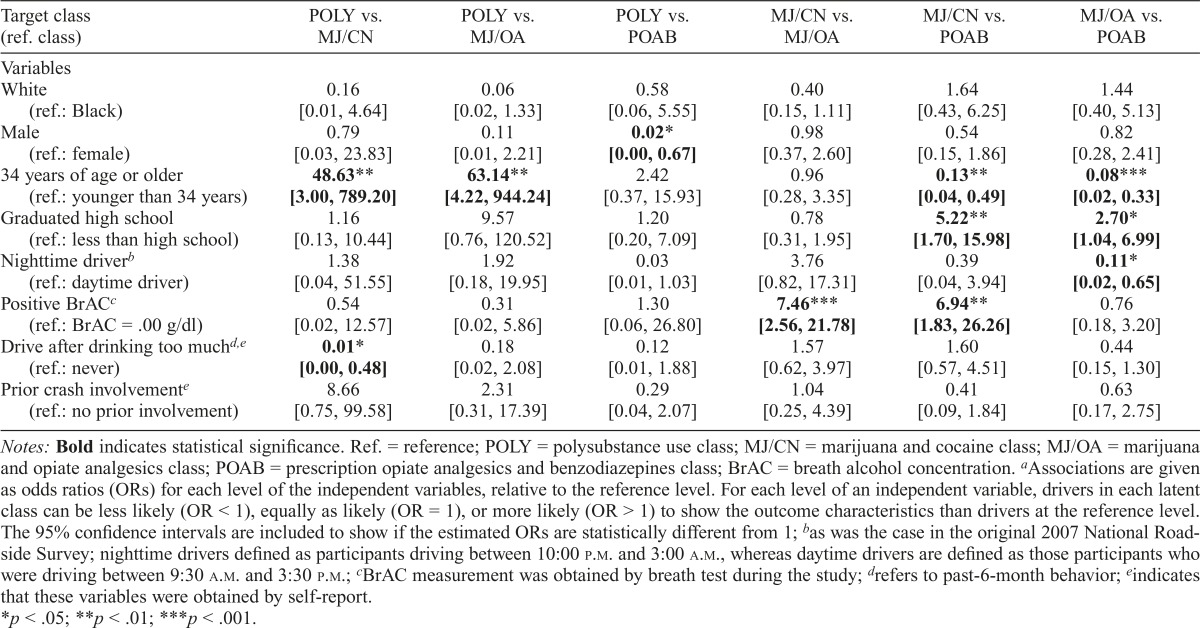
Table 3 shows the associations between latent class membership and demographic and driving characteristics. Members of the POLY class were more likely to be 34 years of age or older than those who tested positive for both marijuana and cocaine (the MJ/CN class, adjusted odds ratio [AOR] = 48.63) or for marijuana and opiate analgesics (the MJ/OA class, AOR = 63.14). Members of the POLY class also were less likely to be male than those in the POAB class (AOR = 0.02).
Table 3.
Associationsa between latent class membership and demographic and driving characteristics in a sample of 250 active motor vehicle operators
| Target class (ref. class) | POLY vs. MJ/CN | POLY vs. MJ/OA | POLY vs. POAB | MJ/CN vs. MJ/OA | MJ/CN vs. POAB | MJ/OA vs. POAB |
| Variables | ||||||
| White | 0.16 | 0.06 | 0.58 | 0.40 | 1.64 | 1.44 |
| (ref.: Black) | [0.01, 4.64] | [0.02, 1.33] | [0.06, 5.55] | [0.15, 1.11] | [0.43, 6.25] | [0.40, 5.13] |
| Male | 0.79 | 0.11 | 0.02* | 0.98 | 0.54 | 0.82 |
| (ref.: female) | [0.03, 23.83] | [0.01, 2.21] | [0.00, 0.67] | [0.37, 2.60] | [0.15, 1.86] | [0.28, 2.41] |
| 34 years of age or older | 48.63** | 63.14** | 2.42 | 0.96 | 0.13** | 0.08*** |
| (ref.: younger than 34 years) | [3.00, 789.20] | [4.22, 944.24] | [0.37, 15.93] | [0.28, 3.35] | [0.04, 0.49] | [0.02, 0.33] |
| Graduated high school | 1.16 | 9.57 | 1.20 | 0.78 | 5.22** | 2.70* |
| (ref.: less than high school) | [0.13, 10.44] | [0.76, 120.52] | [0.20, 7.09] | [0.31, 1.95] | [1.70, 15.98] | [1.04, 6.99] |
| Nighttime driverb | 1.38 | 1.92 | 0.03 | 3.76 | 0.39 | 0.11* |
| (ref.: daytime driver) | [0.04, 51.55] | [0.18, 19.95] | [0.01, 1.03] | [0.82, 17.31] | [0.04, 3.94] | [0.02, 0.65] |
| Positive BrAC | 0.54 | 0.31 | 1.30 | 7.46*** | 6.94** | 0.76 |
| (ref.: BrAC = .00 g/dl) | [0.02, 12.57] | [0.02, 5.86] | [0.06, 26.80] | [2.56, 21.78] | [1.83, 26.26] | [0.18, 3.20] |
| Drive after drinking too muchd,e | 0.01* | 0.18 | 0.12 | 1.57 | 1.60 | 0.44 |
| (ref.: never) | [0.00, 0.48] | [0.02, 2.08] | [0.01, 1.88] | [0.62, 3.97] | [0.57, 4.51] | [0.15, 1.30] |
| Prior crash involvementc | 8.66 | 2.31 | 0.29 | 1.04 | 0.41 | 0.63 |
| (ref.: no prior involvement) | [0.75, 99.58] | [0.31, 17.39] | [0.04, 2.07] | [0.25, 4.39] | [0.09, 1.84] | [0.17, 2.75] |
Notes: Bold indicates statistical significance. Ref. = reference; POLY = polysubstance use class; MJ/CN = marijuana and cocaine class; MJ/OA = marijuana and opiate analgesics class; POAB = prescription opiate analgesics and benzodiazepines class; BrAC = breath alcohol concentration.
Associations are given as odds ratios (ORs) for each level of the independent variables, relative to the reference level. For each level of an independent variable, drivers in each latent class can be less likely (OR < 1), equally as likely (OR = 1), or more likely (OR > 1) to show the outcome characteristics than drivers at the reference level. The 95% confidence intervals are included to show if the estimated ORs are statistically different from 1;
as was the case in the original 2007 National Roadside Survey; nighttime drivers defined as participants driving between 10:00 p.m. and 3:00 a.m., whereas daytime drivers are defined as those participants who were driving between 9:30 a.m. and 3:30 p.m.;
BrAC measurement was obtained by breath test during the study;
refers to past-6-month behavior;
indicates that these variables were obtained by self-report.
p < .05;
p < .01;
p < .001.
Compared with members of the POAB class, members of the MJ/CN class as well as those of the MJ/OA class were significantly less likely to be 34 years of age or older (AOR = 0.13 and AOR = 0.08, respectively). Members of both the MJ/CN class and the MJ/OA class were more than five times and almost three times more likely to have completed a high school education than the POAB class (AOR = 5.22 and AOR = 2.70, respectively).
Members of the MJ/CN class were about seven times more likely to have a positive BrAC at the time they were participating in the study than those in the POAB and MJ/ OA classes (AOR = 6.94 and AOR = 7.46, respectively). Members of the POLY class were also significantly less likely than those in the MJ/CN class to have too much to drink before driving (AOR = 0.01). There were no statistical differences in self-reports of prior crash involvement noted in the current study.
Discussion
The primary endeavor in the current research was to examine demographic associations with multiple-substance use among a national sample of drivers in the United States. Although rates of substance use among drivers has been previously examined in the literature (e.g., Fergusson et al., 2008; Hels et al., 2001; Lacey et al., 2009; Penning et al., 2010; Scherer et al., 2013b; Voas et al., 2013; Ward & Dye, 1999), the current study provides the opportunity to examine multiple-substance use among drivers in greater detail by allowing for comparisons among different combinations of substances.
This is of particular interest as much of the extant research examining substance use among drivers has a tendency to collapse various multiple-substance use categories into a single category for all multiple-substance users (e.g., Hels et al., 2001; Lacey et al., 2009), due in large part to the scarcity of individuals who use multiple substances relative to the number of individuals who use only one substance.
In this way, researchers treat participants who use two substances the same as those who use five or more substances. In the current study, although most multiple-substance-using drivers screened positive for two primary substances, we found that only 5.2% (or 13 drivers) screened positive for all substances measured in the 2007 NRS.
A finding of this effort is that drivers who fell into the MJ/CN class were approximately 7 times more likely than drivers in the MJ/OA or POAB classes to have a positive BrAC (i.e., BrAC > .0). Numerous studies have demonstrated the profound impact of BrAC on crash involvement (e.g., Blomberg et al., 2009; Flowers et al., 2008; Zador et al., 2000), so the finding that people who use marijuana in conjunction with cocaine have significantly higher likelihood of a positive BrAC than drivers in all other classes but POLY is of particular interest. Even if the likelihood of being BrAC positive among the drivers in the MJ/CN class was not significantly different from those in the POLY class (perhaps because of the relative small sample of POLY class drivers), the MJ/CN drivers reported a higher frequency of drinking and driving than those in the POLY class. Thus, we found that, among all multiple-substance users, those who simultaneously consumed marijuana and cocaine were more likely to also have consumed alcohol and, therefore, were more prone to be involved in a crash. Moreover, our findings indicate that MJ/CN drivers not only are among the most likely to drink and drive, but also tend to be younger (and therefore less experienced/riskier drivers) than drivers in some other groups, which further compounds their crash risk.
This finding is particularly interesting in light of previous research which found that although the impact of THC alone on driving performance was not significant, when THC was combined with alcohol, driving impairment was greater than when either substance was used independently (Penning et al., 2010). As such, a particularly interesting finding is that drivers in the MJ/CN class were significantly more likely to both consume alcohol and drive after they felt they consumed too much alcohol. This, coupled with their youth (and inexperienced driving), may make drivers in the MJ/CN class at particular crash risk even among multiple-substance users who are already at an elevated rate of crash risk (Hels et al., 2011).
A second finding of this effort is that not all multiple-drug users are equal. Therefore, the propensity of researchers to lump all multiple-substance users together may erroneously be attributing the potentially profound impact of those in the MJ/CN use class to all multiple-substance users. Alternatively, the potentially high contribution of MJ/ CN drivers to crash risk might be diluted if these drivers are lumped together with other multidrug users. This may dictate a need for future research to stratify multiple-substanceusing classes into more descriptive categories when possible or else note the potential confounding effect of including individuals who use more than two substances with dual substance users.
A priori, we expected the POLY users class to be the most likely to be involved in crashes given the potentially compounding effect of three or more substances. Notably, however, the current study did not find that the drivers in the sample differed in their prior crash involvement. This may be a result of the reduced sample size of drivers in the POLY class (only 5.2% of the sample, or 13 drivers). Regardless, future research with greater sample sizes and/or access to accurate crash data could provide more accurate information to answer this question.
An interesting question hinted at in the literature pertains to the illegal nature of marijuana. It is unclear based on current research whether the legal status of marijuana may have played a role in the concurrent use of substances. That is, marijuana use has previously been linked to other substance use through its illegality. In the process of procuring marijuana illegally, individuals may have an increased exposure opportunity to other illegal substances, which may subsequently make it more likely that they will try other illegal substances (Wagner & Anthony, 2002). If this is correct, then over time the rates of concurrent substance use among marijuana users may decline in states where it has been legalized and the corresponding exposure opportunity decreased. To get at this question, it would have been interesting to conduct a longitudinal comparison of the NRS to examine the impact of marijuana legalization on the rates of concurrent substance use while driving. Although such data were not available at the time of the current study, future research should examine how the legalization of marijuana affected the latent classes discussed in this article. Previous research has found that the impact of marijuana on crash rates was not significant after controlling for concurrent substance use (Penning et al., 2010), and marijuana users may be at particular risk for developing concurrent substance use because of increased exposure opportunity (Wagner & Anthony, 2002) inherent in procuring the substance illegally. It would be feasible, then, that if we were able to follow participants who fell into the MJ/CN class and the MJ/OA class, we would see a transition out of that class into using only one substance as they no longer needed to acquire the substance illegally and thereby reduced their exposure opportunity to other substances. This, in turn, could reduce their likelihood for crash involvement. Because this was not possible to address in the current research, examining this question must be reserved for future endeavors.
Our findings suggest that future prevention efforts should be better targeted to the different types of multidrug users. The relevancy of this finding is compounded by the increasing social acceptance of marijuana (Miech et al., 2015), suggesting the need to communicate the risks caused by the consumption of marijuana in conjunction with alcohol and stimulants.
The current research has several limitations that must be considered for proper interpretation of the findings reported within. First, as a secondary data analysis, the current research is vulnerable to the limitations of the parent study. The 2007 NRS was the first study in the United States to test for both alcohol and other drugs among a sample of drivers. To ensure optimal sampling of these substances, data were collected on Friday and Saturday nights when drugged driving was deemed to be most prevalent. As such, drug and alcohol use during other times of the week may vary from what is reported here. The current study also only examined the presence of psychoactive substances, not whether these were impairing the drivers. Simply screening positive for a substance may not indicate sufficient quantities for impairment, and clearly impairment would be of greater concern than the mere presence of a substance (or multiple substances, as is the case in the current study). Future research should examine rates of impairment among polysubstance-using drivers. Further, the current research uses a cross-sectional design. Although such a design was appropriate to answer the research questions posited herein, it cannot be used for making causal inferences for which additional research may be necessary. Cross-sectional studies are useful in stimulating future research and further scientific understanding, as was the goal in the current study. Finally, the current study stratified the original NRS population to examine only drivers who screened positive for multiple substances. As a result, some of the latent classes have relatively few members, which may have reduced power available for the analyses conducted thereafter.
In addition, the current study must rely on self-report to gather data on adverse driving outcomes (i.e., prior crash involvement, prior drinking and driving), which may be subject to under-reporting. Ideally, self-report information in any study should be corroborated with another source of information to ensure accuracy. For the purposes of the current research, however, this was deemed a necessary risk for two reasons. First, corroborating prior crash and drunk driving information with arrest records, crash data, and/or hospitalization records would provide support for very few cases (i.e., only providing information on drugged drivers who had encountered a problem when driving) and may potentially introduce a new source of selection bias. Second, prior research by Darke (1998) concluded that using self-report measures was a valid and reliable method when gathering data on prior substance use.
Despite these limitations, however, the current research has several strengths that should be noted. First, the 2007 NRS used biological assessment of substance use (breath tests, blood and oral fluid sampling)—the gold standard in substance use assessment—rather than relying on simple self-report. Furthermore, by using a random sample of drivers on the road, the NRS was able to avoid the selection bias prevalent in study samples drawn from crash sites, hospitalizations, and police involvement, which may inaccurately represent rates of substance use among drivers. Last, the use of LCA in the current study allows researchers to identify subclasses of multiple-substance users not previously possible, allowing researchers to begin to examine the subtle differences among multiple-substance-using drivers.
In conclusion, the current study provides support for the idea that not all multiple-substance users are the same, and simply grouping them together in a single category may inaccurately represent their impact on various outcome measures. In fact, among multiple-substance users, only about 5% of drivers used more than two primary substances. These drivers were also less likely to report operating a motor vehicle after having too much to drink. Conversely, drivers who used primarily marijuana and cocaine were more likely to both have a positive BrAC and report driving after acknowledging having had too much to drink. Given the well-documented contribution of alcohol consumption to crash rates, and considering the compounding effect of the other substances in their system, this group represents a different sample than other multiple-substance users and may be of particularly high risk for crash involvement.
References
- Blomberg R. D., Peck R. C., Moskowitz H., Burns M., Fiorentino D. The Long Beach/Fort Lauderdale relative risk study. Journal of Safety Research. 2009;40:285–292. doi: 10.1016/j.jsr.2009.07.002. doi:10.1016/j.jsr.2009.07.002. [DOI] [PubMed] [Google Scholar]
- Blows S., Ivers R. Q., Connor J., Ameratunga S., Woodward M., Norton R. Marijuana use and car crash injury. Addiction. 2005;100:605–611. doi: 10.1111/j.1360-0443.2005.01100.x. doi:10.1111/j.1360-0443.2005.01100.x. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller M. O., Zvolensky M. J. An evaluation of the nature of marijuana use and its motives among young adult active users. American Journal on Addictions. 2009;18:409–416. doi: 10.3109/10550490903077705. doi:10.3109/10550490903077705. [DOI] [PubMed] [Google Scholar]
- Borkenstein R. F., Crowther R. F., Shumate R. P., Ziel W. B., Zylman R. The role of the drinking driver in traffic accidents. Blutalkohol, 11, Supplement. 1974;1:1–132. [Google Scholar]
- Bostwick J. M. Blurred boundaries: The therapeutics and politics of medical marijuana. Mayo Clinic Proceedings. 2012;87:172–186. doi: 10.1016/j.mayocp.2011.10.003. doi:10.1016/j.mayocp.2011.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celeux G., Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification. 1996;13:195–212. doi:10.1007/BF01246098. [Google Scholar]
- Darke S. Self-report among injecting drug users: A review. Drug and Alcohol Dependence. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. doi:10.1016/ S0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Fergusson D. M., Horwood L. J., Boden J. M. Is driving under the influence of cannabis becoming a greater risk to driver safety than drink driving? Findings from a longitudinal study. Accident Analysis and Prevention. 2008;40:1345–1350. doi: 10.1016/j.aap.2008.02.005. doi:10.1016/j.aap.2008.02.005. [DOI] [PubMed] [Google Scholar]
- Flowers N. T., Naimi T. S., Brewer R. D., Elder R. W., Shults R. A., Jiles R. Patterns of alcohol consumption and alcohol-impaired driving in the United States. Alcoholism: Clinical and Experimental Research. 2008;32:639–644. doi: 10.1111/j.1530-0277.2008.00622.x. doi:10.1111/j.1530-0277.2008.00622.x. [DOI] [PubMed] [Google Scholar]
- Harrell P. T., Mancha B. E., Petras H., Trenz R. C., Latimer W. W. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug and Alcohol Dependence. 2012;122:220–227. doi: 10.1016/j.drugalcdep.2011.10.001. doi:10.1016/j.drugalcdep.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hels T., Bernhoft I. M., Lyckegaard A., Houwing S., Hagenzieker M., Legrand S.-A., Verstraete A. Risk of injury by driving with alcohol and other drugs (Deliverable D2.3.5) 2011 Retrieved from http://www.druid-project.eu/Druid/EN/deliverales-list/downloads/Deliver-able_2_3_5.pdf;jsessionid=6D91B2E0941E61B302EA4BDDB7361B10.live1041?_blob=publicationFile&v=1.
- Higgins S. T., Heil S. H., Dantona R., Donham R., Matthews M., Badger G. J. Effects of varying the monetary value of voucher-based incentives on abstinence achieved during and following treatment among cocaine-dependent outpatients. Addiction. 2007;102:271–281. doi: 10.1111/j.1360-0443.2006.01664.x. doi:10.1111/j.1360-0443.2006.01664.x. [DOI] [PubMed] [Google Scholar]
- Lacey J. H., Kelley-Baker T., Furr-Holden D., Voas R., Moore C, Brain-ard K., Berning A. 2007 National Roadside Survey of Alcohol and Drug Use by Drivers: Methodology (Report No. DOT HS 811 237) Washington, DC: National Highway Traffic Safety Administration, U.S. Department of Transportation; 2009. Retrieved from http://www.nhtsa.gov/staticfiles/nti/pdf/811237.pdf. [Google Scholar]
- Laumon B., Gadegbeku B., Martin J.-L., Biecheler M.-B the SAM Group. Cannabis intoxication and fatal road crashes in France: Population based case-control study. BMJ. 2005;331:1371–1376. doi: 10.1136/bmj.38648.617986.1F. doi:10.1136/bmj.38648.617986.1F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M.-C., Brady J. E., DiMaggio C. J., Lusardi A. R., Tzong K. Y., Li G. Marijuana use and motor vehicle crashes. Epidemiologic Reviews. 2012;34:65–72. doi: 10.1093/epirev/mxr017. doi:10.1093/epirev/mxr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay J. A., Stotts A. L., Green C. E., Herin D. V., Schmitz J. M. Cocaine dependence and concurrent marijuana use: A comparison of clinical characteristics. American Journal of Drug and Alcohol Abuse. 2009;35:193–198. doi: 10.1080/00952990902933860. doi:10.1080/00952990902933860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y., Mendell N. R., Rubin D. B. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. doi:10.1093/biomet/88.3.767. [Google Scholar]
- MacLachlan G., Peel D. Finite mixture models: Wiley Series in Probability and Statistics. New York, NY: John Wiley and Sons; 2000. [Google Scholar]
- McCutcheon A. L. Latent class analysis. Thousand Oaks, CA: Sage; 1987. [Google Scholar]
- Midanik L. T., Tam T. W., Weisner C. Concurrent and simultaneous drug and alcohol use: Results of the 2000 National Alcohol Survey. Drug and Alcohol Dependence. 2007;90:72–80. doi: 10.1016/j.drugalcdep.2007.02.024. doi:10.1016/j.drugalcdep.2007.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R. A., Johnston L., O’Malley P. M., Bachman J. G., Schulenberg J., Patrick M. E. Trends in use of marijuana and attitudes toward marijuana among youth before and after decriminalization: The case of California 2007-2013. International Journal on Drug Policy. 2015;26:336–344. doi: 10.1016/j.drugpo.2015.01.009. doi:10.1016/j.drugpo.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. Mplus user’s guide. 6th ed. Los Angeles, CA: Authors; 2010. [Google Scholar]
- Nakawaki B., Crano W. D. Predicting adolescents’ persistence, non-persistence, and recent onset of nonmedical use of opioids and stimulants. Addictive Behaviors. 2012;37:716–721. doi: 10.1016/j.addbeh.2012.02.011. doi: 10.1016/j.addbeh.2012.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund K. L., Asparouhov T., Muthén B. O. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14:535–569. doi:10.1080/10705510701575396. [Google Scholar]
- Office of National Drug Control Policy. Marijuana resource center: State laws related to marijuana. Washington, DC: Author; 2014. Retrieved from https://www.whitehouse.gov/ondcp/state-laws-related-to-marijuana. [Google Scholar]
- Olthuis J. V., Darredeau C., Barrett S. P. Substance use initiation: The role of simultaneous polysubstance use. Drug and Alcohol Review. 2013;32:67–71. doi: 10.1111/j.1465-3362.2012.00470.x. doi:10.1111/j.1465-3362.2012.00470.x. [DOI] [PubMed] [Google Scholar]
- Penning R., Veldstra J. L., Daamen A. P., Olivier B., Verster J. C. Drugs of abuse, driving and traffic safety. Current Drug Abuse Reviews. 2010;3:23–32. doi: 10.2174/1874473711003010023. doi:10.2174/1874473711003010023. [DOI] [PubMed] [Google Scholar]
- Petras H., Masyn K. In: General growth mixture analysis with antecedents and consequences of change. Handbook of quantitative criminology. Piquero A., Weisburd D., editors. New York, NY: Springer; 2010. pp. 69–100. [Google Scholar]
- Saad L. Majority continues to support pot legalization in U.S. 2014, November 6 Retrieved from http://www.gallup.com/poll/179195/majority-continues-support-pot-legalization.aspx.
- Scherer M., Trenz R. C., Harrell P., Altintoprak E., Mancha B., Latimer W. W. Desistance from problematic alcohol use without treatment among active heroin and cocaine users. Addiction Research & Theory. 2013a;21:227–234. doi:10.3109/16066359.2012.705400. [Google Scholar]
- Scherer M., Voas R. B., Furr-Holden D. Marijuana as a predictor of concurrent substance use among motor vehicle operators. Journal of Psychoactive Drugs. 2013b;45:211–217. doi: 10.1080/02791072.2013.804230. doi:10.1080/02791072.2013.804230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz B., Wetzler S., Swanson A., Sung S. C. Subtyping of substance use disorders in a high-risk welfare-to-work sample: A latent class analysis. Journal of Substance Abuse Treatment. 2010;38:366–374. doi: 10.1016/j.jsat.2010.03.001. doi:10.1016/jjsat.2010.03.001. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. doi:10.1214/aos/1176344136. [Google Scholar]
- Stinson F. S., Grant B. F., Dawson D. A., Ruan W. J., Huang B., Saha T. Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2005;80:105–116. doi: 10.1016/j.drugalcdep.2005.03.009. doi:10.1016/j.drugalcdep.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Subramaniam G. A., Ives M. L., Stitzer M. L., Dennis M. L. The added risk of opioid problem use among treatment-seeking youth with marijuana and/or alcohol problem use. Addiction. 2010;105:686–698. doi: 10.1111/j.1360-0443.2009.02829.x. doi:10.1111/j.1360-0443.2009.02829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H-48, HHS Publication No. (SMA) 14–4863. Rockville, MD: Author; 2014. Retrieved from http://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf. [Google Scholar]
- United Nations Office on Drugs and Crime. World drugs report. New York, NY: Author; 2011. [Google Scholar]
- Voas R. B., Lacey J. H., Jones K., Scherer M., Compton R. Drinking drivers and drug use on weekend nights in the United States. Drug and Alcohol Dependence. 2013;130:215–221. doi: 10.1016/j.drugalcdep.2012.11.007. doi:10.1016/j.drugalcdep.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voas R. B., Torres P., Romano E., Lacey J. H. Alcohol-related risk of driver fatalities: An update using 2007 data. Journal of Studies on Alcohol and Drugs. 2012;73:341–350. doi: 10.15288/jsad.2012.73.341. doi:10.15288/jsad.2012.73.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner F. A., Anthony J. C. Into the world of illegal drug use: Exposure opportunity and other mechanisms linking the use of alcohol, tobacco, marijuana, and cocaine. American Journal of Epidemiology. 2002;155:918–925. doi: 10.1093/aje/155.10.918. doi:10.1093/aje/155.10.918. [DOI] [PubMed] [Google Scholar]
- Ward N. J., Dye L. Cannabis and driving: A review of the literature and commentary. London, England: Department of the Environment, Transport and the Regions; 1999. [Google Scholar]
- Zador P. L., Krawchuk S. A., Voas R. B. Alcohol-related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: An update using 1996 data. Journal ofStudies on Alcohol. 2000;61:387–395. doi: 10.15288/jsa.2000.61.387. doi:10.15288/jsa.2000.61.387. [DOI] [PubMed] [Google Scholar]