Abstract
Objective:
Although the primary focus of clinical trials is on between-group comparisons during treatment, these studies can also yield insights into which patient characteristics predict longer term outcomes. Our goal was to identify predictors of good outcome during the 1-year follow-up in the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) Study.
Method:
We constructed classification trees and a deterministic forest to predict no heavy drinking days during the last 8 weeks of the 1-year follow-up in COMBINE, based on more than 100 baseline predictors and drinking outcomes during the treatment phase of the study. The COMBINE sample was randomly split into a training and a validation data set. Logistic regression models were fit to compare the predictive performance of tree-based methods and classical methods.
Results:
A small tree with only two splits and four nodes based on abstinence and good clinical outcome during treatment had fair classification accuracy in the training and the validation samples: area under the curve (AUC) of 71% and 70%, respectively. Drinking outcomes during treatment were the strongest predictors in the deterministic forest. Logistic regression analyses based on four main effects (good clinical outcome, level of drinking during treatment, age at onset of alcohol dependence, and feeling more energetic) had slightly better classification accuracy (AUC = 74%).
Conclusions:
End-of-treatment outcomes were the strongest predictors of long-term outcome in all analyses. The results emphasize the importance of optimizing outcomes during treatment and identify potential subgroups of individuals who require additional or alternative interventions to achieve good long-term outcome.
Clinical trials focus on between-group comparisons during treatment, but these studies can also yield insights into which patient characteristics predict longer term outcomes. In alcohol research, several patient-related factors have been found to predict better long-term drinking outcomes following treatment completion. For example, greater motivation and self-efficacy to change drinking (Allen et al., 1998; Bertholet et al., 2010; Ludwig et al., 2013; Staines et al., 2003); stronger commitment to an abstinence goal (Bodin & Romelsjö, 2006); a larger, sober support network (Bertholet et al., 2010; Bond et al., 2003; Stout et al., 2012); lower cravings to drink (Bottlender & Soyka, 2004); greater involvement in 12-step self-help groups (Bodin & Romelsjö, 2006; Staines et al., 2003); and better within-treatment drinking outcomes (Breslin et al., 1997) are associated with higher abstinence rates 6 months or more after treatment.
These predictors are often considered one at a time and their relationship to each other is ignored. Furthermore, classical statistical approaches such as regression are often limited to testing main effects and lower order interactions and consider a few potential predictors. In contrast, tree-based methods (Breiman et al., 1984; Zhang & Singer, 2010) allow simultaneous consideration of many predictors, empirical derivation of the strongest predictors of good outcome, and identification of variable interactions. Tree-based methods are easier to use in clinical settings because they require evaluation of simple decision rules rather than mathematical equations. In alcohol research, tree-based techniques have been used mainly in epidemiological studies (Müller et al., 2008; Vik et al., 2006; Ye et al., 2005). We recently used these methods to identify patient characteristics associated with a good drinking outcome during treatment (Gueorguieva et al., 2014). Tree-based methods share the advantages of other techniques—such as principal component analysis (Jolliffe, 1986), partial least squares (Helland, 1990), and neural networks (Abdi et al., 1999)—that allow large numbers of predictors to be considered simultaneously. Compared with these other techniques, trees have the advantage of simple graphical presentation of the results.
The focus of the current study was to identify predictors of good long-term drinking outcomes in the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) Study (Anton et al., 2006). COMBINE was designed to assess the benefits of combining pharmacological treatment (naltrexone, acamprosate) and behavioral interventions (medication management [MM], Pettinati et al., 2004; combined behavioral intervention [CBI], Miller, 2004). The primary analyses (Anton et al., 2006) revealed that either naltrexone (+MM) or CBI (+MM) improved outcomes during treatment. Only the naltrexone effect on heavy drinking remained significant during the 1-year follow-up. Improvements in secondary nondrinking outcomes were maintained and in general were nondifferentiated by treatment (LoCastro et al., 2009).
The COMBINE baseline assessments were selected to capture domains that were thought to be predictors or moderators of outcomes (COMBINE Study Research Group, 2003). Of all baseline predictors, consecutive days of abstinence before treatment and drinking goal were identified and validated internally and externally (Mann et al., 2013) as robust predictors of no heavy drinking days (NHDD) during the last 8 weeks of treatment (Gueorguieva et al., 2014). The goal of the current investigation was to identify combinations of predictors of NHDD during follow-up from among the baseline predictors and outcomes measured during treatment.
Method
The COMBINE Study (The Combine Study Group, 2001–2004) enrolled 1,383 abstinent alcohol-dependent patients. Eight groups (n = 1,226) received MM and either placebos, naltrexone, acamprosate, or naltrexone + acamprosate, and 1,220 of these participants had at least some drinking data collected during treatment. Half of these groups received the CBI. A ninth group that received CBI alone with no pills is not included in this report.
Long-term outcome
Abstinence from heavy drinking has been recommended as an outcome in clinical trials because it is associated with reduced risk of alcohol-related consequences while allowing for improvements in drinking short of abstinence (Falk et al., 2010). In the present study, we examined NHDD during the last 8 weeks of the 1-year follow-up in COMBINE to determine predictors of long-term outcome. Missing data were coded as heavy drinking in the primary analyses. Secondary analyses were performed to assess sensitivity of conclusions to assumptions about missing data. The first set of sensitivity analyses was restricted to participants who had drinking data at follow-up. The second set of sensitivity analyses was performed after coding missing data as not heavy drinking rather than as heavy drinking.
Predictors
We considered more than 100 potential predictors, including treatment condition, drinking outcomes, compliance outcomes during treatment, and baseline measures from multiple domains. These domains include demographics; alcoholism severity and withdrawal symptoms; alcohol consumption measures; alcohol craving; physical health; tobacco and other drug use; legal involvement; expectations of treatment efficacy; self-efficacy; motivation; and goals for drinking, mood, craving, and quality of life. Detailed information about the predictors can be obtained from the authors and is available as supplemental online material to Gueorguieva et al. (2014). Categorical predictors that had missing values had an additional missing category created. Continuous predictors had missing values imputed using multiple imputation.
Training and validation samples
A random two thirds of the COMBINE data were used for tree development (training sample: TS) and the remainder for tree validation (validation sample: VS). Participants with missing long-term outcomes (40 in the TS and 30 in the VS) were excluded. The TS consisted of 769 participants, and the VS consisted of 381 participants.
Tree construction
The Willows program (Zhang et al., 2009) was used to construct a tree with two steps: tree growing and tree pruning.
Tree growing.
The TS was split into two parts so that each subsample was as homogeneous as possible with respect to the outcome based on the entropy statistic. This means that one of the subsamples had a high rate of NHDD and the other had a low rate of NHDD. Each of the two subsamples was further split in two according to the same criterion. The algorithm proceeded recursively until no further splits were possible. At each step, all predictors and all possible splits were evaluated one at a time to select the best split. The predictor variable and the threshold (for continuous variables) that led to the best split were selected. We imposed the restriction of at least 20 participants in each subsample. Each subsample corresponds to a node, and each split corresponds to a branching out of a node in the constructed tree (see Results).
Tree pruning.
Once the full tree on the TS was grown, branches of the tree were pruned if the subsamples that they defined were not significantly different in terms of outcome according to the chi-square statistic for 2 × 2 contingency tables, calculated for the association between the predictor and the outcome in the corresponding tree node. We used a conservative alpha level of .00001 to avoid overfitting.
Performance of the algorithm in both the TS and the VS was assessed using the area under the curve (AUC) of the receiver operating curve, showing sensitivity versus 1-specificity for the classification of participants in outcome categories.
Deterministic forest
Because different combinations of predictors may lead to similar prediction accuracy, we also constructed a deterministic forest in the TS to identify the strongest predictors of the outcome. Deterministic forests consist of multiple trees based on the most important splits that are determined when each variable is evaluated for its ability to separate subjects into homogeneous groups with respect to the outcome. We considered the top 20 splits of the entire sample and the top 3 splits of each of the two subsamples at the first level of the tree, giving rise to 180 (20 × 3 × 3) trees in the forest. We present the top predictors in the forest based on how many times they appear as sample splitters in the forest. These are considered the most important predictors because they most often identify subsets of the sample with good outcome. Although individual trees pick only a small subset of all potential predictors, forests include the majority of the predictors, but only a few predictors are present in almost all trees.
Logistic regression
Hierarchical stepwise logistic regression analyses were performed in the TS, with the most important predictors within each domain identified at the first step and then only significant effects from each domain entered in a second-stage stepwise logistic regression. We used a significance level of .10 for entry and for staying in the model. The performance of the final logistic model in the TS and the VS was evaluated using the AUC.
Results
Classification trees
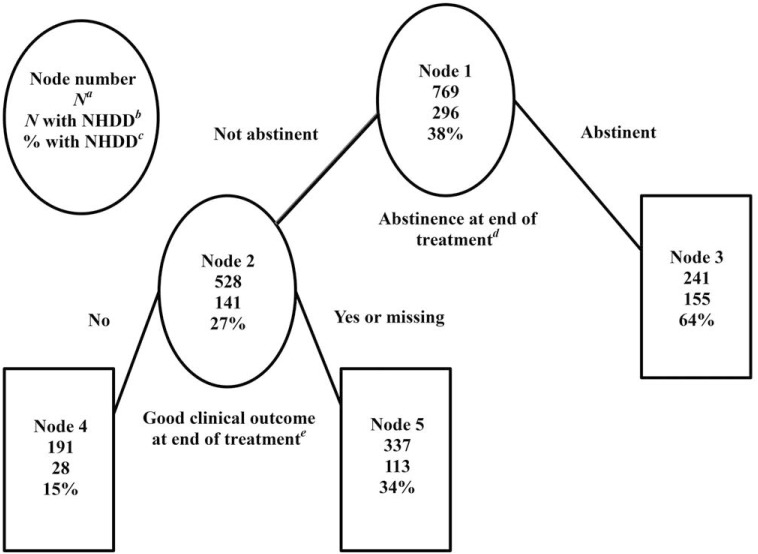
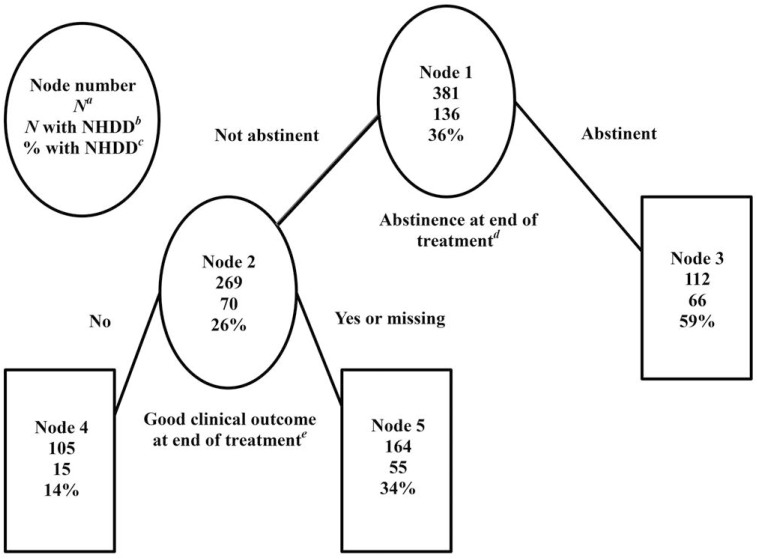
The constructed tree in the TS had only five nodes, with splits on abstinence during the last 8 weeks of treatment and good clinical outcome (Figure 1a). The VS data were directly categorized using the constructed tree (Figure 1b). Abstinence was defined as no self-reported drinking; good clinical outcome was defined as abstinence or moderate drinking without problems as described in the parent study (Anton et al., 2006; Cisler & Zweben, 1999) and in the figure legend.
Figure 1a.
Tree predicting no heavy drinking days during the last 8 weeks of follow-up pruned at α = .00001 in the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) Study training sample (N = 769). aN = number of subjects; bN with NHDD = number of subjects with no heavy drinking days during the last 8 weeks of the 1-year follow-up; c% with NHDD = percentage of subjects with no heavy drinking days during the last 8 weeks of the 1-year follow-up; dabstinence at end of treatment = no drinking during the last 8 weeks of the 16-week double-blind treatment period; egood clinical outcome at end of treatment = moderate drinking without problems. Moderate drinking was defined as a maximum of 11 drinks (for women) or 14 drinks (for men) per week, with no more than 2 days on which more than 3 drinks (for women) or 4 drinks (for men) were consumed. Problems were defined as endorsing three or more items on a standardized questionnaire assessing physical, social, and psychological consequences of drinking.
Figure 1b.
Tree predicting no heavy drinking days during the last 8 weeks of follow-up in the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) Study validation sample (N = 381). aN = number of subjects; bN with NHDD = number of subjects with no heavy drinking days during the last 8 weeks of the 1-year follow-up; c% with NHDD = percentage of subjects with no heavy drinking days during the last 8 weeks of the 1-year follow-up; dabstinence at end of treatment = no drinking during the last 8 weeks of the 16-week double-blind treatment period; egood clinical outcome at end of treatment = moderate drinking without problems. Moderate drinking was defined as a maximum of 11 drinks (for women) or 14 drinks (for men) per week, with no more than 2 days on which more than 3 drinks (for women) or 4 drinks (for men) were consumed. Problems were defined as endorsing three or more items on a standardized questionnaire assessing physical, social, and psychological consequences of drinking.
The final trees show that large percentage of participants who maintained abstinence during the last 8 weeks of treatment had NHDD during follow-up (Node 3, 64% in the TS and 59% in the VS). At the other extreme, small percentage of participants who were unable to maintain abstinence and did not meet the criteria for a good clinical outcome during treatment (i.e., either they exceeded moderate drinking limits or reported alcohol-related consequences) had NHDD during follow-up (Node 4, 15% in the TS and 14% in the VS). Only about a third of participants who failed to maintain abstinence but drank moderately with few consequences had NHDD (34% in both samples). The receiver operating curve had AUC = 71% in the TS and 70% in the VS, suggesting a fair level of classification accuracy based on only two drinking outcomes during treatment.
The first sensitivity analysis (restricted to participants with drinking data at follow-up) resulted in a tree with the same structure as shown in Figure 1a, whereas the second sensitivity analysis (when missing data at follow-up were coded as not heavy drinking) resulted in a tree with only one split on abstinence from heavy drinking during the last 8 weeks of treatment (not shown). Thus, in both sensitivity analyses, only drinking outcomes during treatment were identified as tree splitters in the final trees.
Deterministic forest
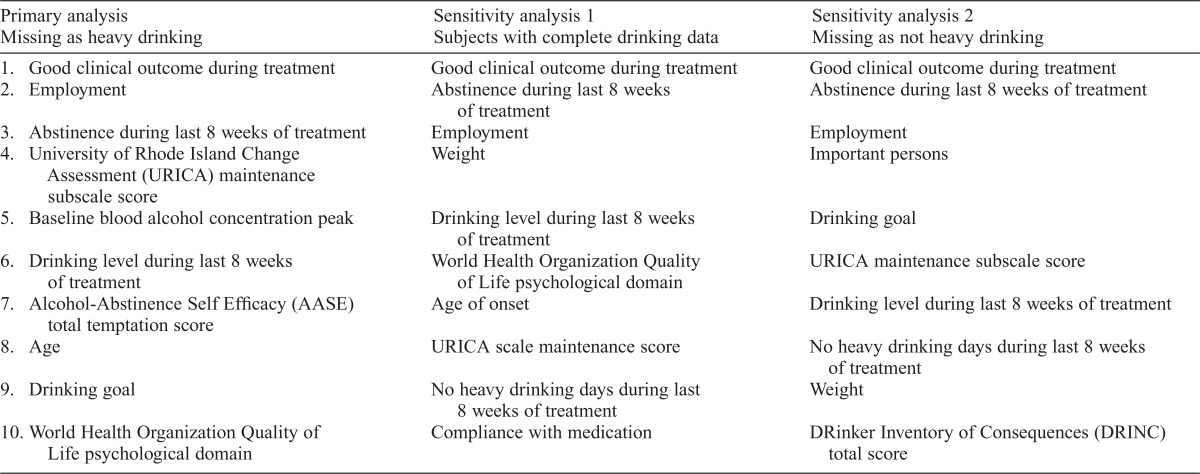
The deterministic forest in the primary analysis (i.e., when missing drinking data were treated as heavy drinking) identified 77 predictors that were used to define subsamples in at least 1 of the 180 trees in the forest. The top 10 variables in the primary and sensitivity analyses are shown in Table 1. All considered measures of drinking during treatment (abstinence, NHDD, good clinical outcome, and drinking level) were among the top 10 variables in at least one deterministic forest. In particular, abstinence and good clinical outcome were among the top three predictors in all analyses. The predictors not shown in Table 1 appear in less than half of the trees in the corresponding forests.
Table 1.
Top 10 predictors used in node splitting in the deterministic forests built on the training sample in primary and sensitivity analyses
| Primary analysis Missing as heavy drinking | Sensitivity analysis 1 Subjects with complete drinking data | Sensitivity analysis 2 Missing as not heavy drinking |
| 1. Good clinical outcome during treatment | Good clinical outcome during treatment | Good clinical outcome during treatment |
| 2. Employment | Abstinence during last 8 weeks of treatment | Abstinence during last 8 weeks of treatment |
| 3. Abstinence during last 8 weeks of treatment | Employment | Employment |
| 4. University of Rhode Island Change Assessment (URICA) maintenance subscale score | Weight | Important persons |
| 5. Baseline blood alcohol concentration peak | Drinking level during last 8 weeks of treatment | Drinking goal |
| 6. Drinking level during last 8 weeks of treatment | World Health Organization Quality of Life psychological domain | URICA maintenance subscale score |
| 7. Alcohol-Abstinence Self Efficacy (AASE) total temptation score | Age of onset | Drinking level during last 8 weeks of treatment |
| 8. Age | URICA scale maintenance score | No heavy drinking days during last 8 weeks of treatment |
| 9. Drinking goal | No heavy drinking days during last 8 weeks of treatment | Weight |
| 10. World Health Organization Quality of Life psychological domain | Compliance with medication | DRinker Inventory of Consequences (DRINC) total score |
Logistic regression
Stepwise model fitting in the TS resulted in four significant main effects. Good clinical outcome during treatment (yes vs. no, odds ratio [OR] = 3.20, 95% CI [1.90, 5.38]), drinking level during the last 8 weeks of treatment (abstinent vs. heavy drinking, OR = 3.17, 95% CI [2.08, 4.84]); (abstinent vs. drinking but not heavily, OR = 3.06, 95% CI [1.88, 4.98]), older age at onset (OR = 1.02, 95% CI [1.00, 1.03]), and feeling more energetic (higher score on the Profile of Mood States vigor subscale, OR = 1.05, 95% CI [1.01, 1.09]) were associated with a higher chance of NHDD at follow-up. The AUC for these data was 74% in both the TS and the VS. The two sensitivity analyses identified the same predictors (not shown).
Discussion
In summary, we identified predictors of good outcome during follow-up and compared the performance of tree-based methods and logistic regression. The strongest predictors of NHDD at follow-up were end-of-treatment drinking outcomes. Treatments were not predictive of long-term outcome, but they might have had an indirect effect via end-of-treatment drinking outcomes. In general, pharmacotherapies for alcohol dependence are not expected to have a long-term effect after discontinuation, and maintenance treatment may be needed for those with good initial response (O’Malley et al., 2003). In contrast, longer term effects of CBI could be expected (Carroll et al., 1994), but our analysis did not find lasting CBI effects. Our results are consistent with prior studies that showed within-treatment drinking predicted longer term outcomes (Breslin et al., 1997; Maisto et al., 1998; Öjehagen et al., 1994; Weisner et al., 2003).
Logistic regression revealed that the age at onset of alcohol dependence and feeling energetic were independent predictors that did not show up in our individual tree and showed up infrequently in the deterministic forest. This may be because of the limitation of individual trees to identify more than one main effect. Only the first split in a tree identifies a main effect, whereas all subsequent splits correspond to interactions among predictors. Thus, the first split usually picks up the strongest main effect, and other predictors that may have main effects may not be chosen as subsequent splitting variables because they do not interact with other variables. Although multiple main effects are identified in forests that consist of individual trees, only the strongest main effects are identified in the different trees, and weaker main effects may not be identified at all. Whereas logistic regression models focus on identification of independent effects of covariates and lower order interactions, tree-based methods can discover important combinations of predictors among a large pool of covariates. In the current study, both methods did not discover unexpected predictors or combinations of predictors of long-term outcome. The consistency of the results of the two methods speaks to the robustness and potential generalizability of the findings.
Among the advantages of tree-based methods over classical approaches (i.e., fewer assumptions, simultaneous consideration of many predictors, computational efficiency, ease of interpretation), perhaps ease of implementation is the most appealing. The results are summarized in the form of trees with decision rules that can be easily understood. Following the decision rules at each split, new patients can be rapidly classified by evaluating several logical conditions. Based on our results, a clinician can classify patients at the end of treatment in one of the terminal nodes, assess their prognosis based on the proportion of participants with good outcome in this node, and suggest maintenance or augmentation treatment as necessary. In adaptive designs, investigators can use tree-based participant classification at the end of a treatment phase to inform switching or augmentation strategies in the next phase. Participants who fail to abstain during treatment and who report drinking-related problems or drinking that exceeds moderate levels are expected to have a poor long-term outcome and hence may be offered an augmentation or alternative treatment strategy. Participants who maintain abstinence during treatment are expected to have good long-term outcome and may benefit from minimal maintenance treatment or outside resources. Participants in the middle who fail to abstain but are drinking moderately without problems may benefit from continued treatment or periodic monitoring and the development of a plan to renew treatment if needed. As one approach, continued monitoring could be provided by the patient’s primary care provider (McKay & Hiller-Sturmhöfel, 2011).
Finally, our results showed relatively low predictive ability for both methods, possibly because of unmeasured variables that occur in the intervening period between the end of treatment and 1-year follow-up. Nonetheless, the finding that outcomes measured at the end of treatment are the most important predictors of long-term outcomes emphasizes the need to optimize initial treatment response to help patients achieve long-term success. In COMBINE, participants with shorter pre-treatment abstinence, especially those who were younger (Gueorguieva et al., 2014), and participants who were early noncompliers with treatment (Gueorguieva et al., 2013) had poor drinking outcomes during treatment. Other studies in substance users (McKay et al., 2013; Petry et al., 2012) have found that patients who were still using alcohol, compared with those who were abstinent, benefited from more intensive or extensive interventions. Thus, more intensive monitoring of these patients early in treatment with the option of providing alternative treatment may be needed to improve outcomes during treatment and follow-up.
Acknowledgment
Stephanie S. O’Malley, Ph.D., is a member of the American Society of Clinical Psychopharmacology work group. She participated in the Alcohol Clinical Trial Initiative, sponsored by Abbott Laboratories, Eli Lilly & Company, Lundbeck, Pfizer, and Ethypharma. She received medication donations from Pfizer Inc. She was involved in a clinical trial site for Eli Lilly & Company. She served on an Advisory Board of Alkermes and as a Scientific Panel Member for the Hazelden Betty Ford Foundation.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism Grants R01 AA017173, P50 AA012870, K05 AA014715, and K23 AA020000. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
References
- Abdi H., Valentin D., Edelman B. Neural networks. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Allen J. P., Moore C., Kuperminc G., Bell K. Attachment and adolescent psychosocial functioning. Child Development. 1998;69:1406–1419. doi:10.2307/1132274. [PMC free article] [PubMed] [Google Scholar]
- Anton R. F., O’Malley S. S., Ciraulo D. A., Cisler R. A., Couper D., Donovan D. M, Zweben A. the COMBINE Study Research Group. Combined pharmacotherapies and behavioral interventions for alcohol dependence: The COMBINE Study: A randomized controlled trial. JAMA. 2006;295:2003–2017. doi: 10.1001/jama.295.17.2003. doi:10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Bertholet N., Cheng D. M., Palfai T. P., Saitz R. Factors associated with favorable drinking outcome 12 months after hospitalization in a prospective cohort study of inpatients with unhealthy alcohol use. Journal of General Internal Medicine. 2010;25:1024–1029. doi: 10.1007/s11606-010-1382-1. doi:10.1007/s11606-010-1382-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodin M. C., Romelsjö A. Predictors of abstinence and nonproblem drinking after 12-step treatment in Sweden. Journal of Studies on Alcohol. 2006;67:139–146. doi: 10.15288/jsa.2006.67.139. doi:10.15288/jsa.2006.67.139. [DOI] [PubMed] [Google Scholar]
- Bond J., Kaskutas L. A., Weisner C. The persistent influence of social networks and Alcoholics Anonymous on abstinence. Journal of Studies on Alcohol. 2003;64:579–588. doi: 10.15288/jsa.2003.64.579. doi:10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- Bottlender M., Soyka M. Impact of craving on alcohol relapse during, and 12 months following, outpatient treatment. Alcohol and Alcoholism. 2004;39:357–361. doi: 10.1093/alcalc/agh073. doi:10.1093/alcalc/agh073. [DOI] [PubMed] [Google Scholar]
- Breiman L., Friedman J. H., Olshen R. A., Stone C. J. Classification and regression trees. Wadsworth, CA: Chapman & Hall/CRC; 1984. [Google Scholar]
- Breslin F. C., Sobell M. B., Sobell L. C., Buchan G., Cunningham J. A. Toward a stepped care approach to treating problem drinkers: The predictive utility of within-treatment variables and therapist prognostic ratings. Addiction. 1997;92:1479–1489. doi:10.1111/j.1360-0443.1997.tb02869.x. [PubMed] [Google Scholar]
- Carroll K. M., Rounsaville B. J., Nich C., Gordon L. T., Wirtz P. W., Gawin F. One-year follow-up of psychotherapy and pharmacotherapy for cocaine dependence: Delayed emergence of psychotherapy effects. Archives of General Psychiatry. 1994;51:989–997. doi: 10.1001/archpsyc.1994.03950120061010. doi:10.1001/archpsyc.1994.03950120061010. [DOI] [PubMed] [Google Scholar]
- Cisler R. A., Zweben A. Development of a composite measure for assessing alcohol treatment outcome: Operationalization and validation. Alcoholism: Clinical and Experimental Research. 1999;23:263–271. doi:10.1111/j.1530-0277.1999.tb04109.x. [PubMed] [Google Scholar]
- COMBINE Study Research Group. Testing combined pharmacotherapies and behavioral interventions in alcohol dependence: Rationale and methods. Alcoholism: Clinical and Experimental Research. 2003;27:1107–1122. doi: 10.1097/00000374-200307000-00011. doi:10.1111/j.1530-0277.2003.tb02873.x. [DOI] [PubMed] [Google Scholar]
- Falk D., Wang X. Q., Liu L., Fertig J., Mattson M., Ryan M., Litten R. Z. Percentage of subjects with no heavy drinking days: Evaluation as an efficacy endpoint for alcohol clinical trials. Alcoholism: Clinical and Experimental Research. 2010;34:2022–2034. doi: 10.1111/j.1530-0277.2010.01290.x. doi:10.1111/j.1530-0277.2010.01290.x. [DOI] [PubMed] [Google Scholar]
- Gueorguieva R., Wu R., Krystal J. H., Donovan D., O’Malley S. S. Temporal patterns of adherence to medications and behavioral treatment and their relationship to patient characteristics and treatment response. Addictive Behaviors. 2013;38:2119–2127. doi: 10.1016/j.addbeh.2013.01.024. doi:10.1016/j.addbeh.2013.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gueorguieva R., Wu R., O’Connor P. G., Weisner C., Fucito L. M., Hoffmann S., O’Malley S. S. Predictors of abstinence from heavy drinking during treatment in COMBINE and external validation in PREDICT. Alcoholism: Clinical and Experimental Research. 2014;38:2647–2656. doi: 10.1111/acer.12541. doi:10.1111/acer.12541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helland I. S. PLS regression and statistical models. Scandinavian Journal of Statistics. 1990;17:97–114. [Google Scholar]
- Jolliffe I. Principal component analysis. New York, NY: Springer-Verlag; 1986. [Google Scholar]
- LoCastro J. S., Youngblood M., Cisler R. A., Mattson M. E., Zweben A., Anton R. F., Donovan D. M. Alcohol treatment effects on secondary nondrinking outcomes and quality of life: The COMBINE Study. Journal of Studies on Alcohol and Drugs. 2009;70:186–197. doi: 10.15288/jsad.2009.70.186. doi:10.15288/jsad.2009.70.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludwig F., Tadayon-Manssuri E., Strik W., Moggi F. Self-efficacy as a predictor of outcome after residential treatment programs for alcohol dependence: Simply ask the patient one question! Alcoholism: Clinical and Experimental Research. 2013;37:663–667. doi: 10.1111/acer.12007. doi:10.1111/acer.12007. [DOI] [PubMed] [Google Scholar]
- Maisto S. A., McKay J. R., O’Farrell T. J. Twelve-month abstinence from alcohol and long-term drinking and marital outcomes in men with severe alcohol problems. Journal of Studies on Alcohol. 1998;59:591–598. doi: 10.15288/jsa.1998.59.591. doi:10.15288/jsa.1998.59.591. [DOI] [PubMed] [Google Scholar]
- Mann K., Lemenager T., Hoffmann S., Reinhard I., Hermann D., Batra A, Anton R. F. the PREDICT Study Team. Results of a double-blind, placebo-controlled pharmacotherapy trial in alcoholism conducted in Germany and comparison with the US COMBINE Study. Addiction Biology. 2013;18:937–946. doi: 10.1111/adb.12012. doi:10.1111/adb.12012. [DOI] [PubMed] [Google Scholar]
- McKay J. R., Hiller-Sturmhöfel S. Treating alcoholism as a chronic disease: Approaches to long-term continuing care. Alcohol Research & Health. 2011;33:356–370. [PMC free article] [PubMed] [Google Scholar]
- McKay J. R., Van Horn D. H., Lynch K. G., Ivey M., Cary M. S., Drapkin M. L., Plebani J. G. An adaptive approach for identifying cocaine dependent patients who benefit from extended continuing care. Journal of Consulting and Clinical Psychology. 2013;81:1063–1073. doi: 10.1037/a0034265. doi:10.1037/a0034265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W. R, editor. Combined Behavioral Intervention manual: A clinical research guide for therapists treating people with alcohol abuse and dependence, Vol. 1. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2004. [Google Scholar]
- Müller S. E., Weijers H. G., Böning J., Wiesbeck G. A. Personality traits predict treatment outcome in alcohol-dependent patients. Neuropsychobiology. 2008;57:159–164. doi: 10.1159/000147469. doi:10.1159/000147469. [DOI] [PubMed] [Google Scholar]
- Öjehagen A., Berglund M., Moberg A. L. A 6-year follow-up of alcoholics after long-term outpatient treatment. Alcoholism: Clinical and Experimental Research. 1994;18:720–725. doi: 10.1111/j.1530-0277.1994.tb00937.x. doi:10.1111/j.1530-0277.1994.tb00937.x. [DOI] [PubMed] [Google Scholar]
- O’Malley S. S., Rounsaville B. J., Farren C., Namkoong K., Wu R., Robinson J., O’Connor P. G. Initial and maintenance naltrexone treatment for alcohol dependence using primary care vs specialty care: A nested sequence of 3 randomized trials. Archives of Internal Medicine. 2003;163:1695–1704. doi: 10.1001/archinte.163.14.1695. doi:10.1001/archinte.163.14.1695. [DOI] [PubMed] [Google Scholar]
- Petry N. M., Barry D., Alessi S. M., Rounsaville B. J., Carroll K. M. A randomized trial adapting contingency management targets based on initial abstinence status of cocaine-dependent patients. Journal of Consulting and Clinical Psychology. 2012;80:276–285. doi: 10.1037/a0026883. doi:10.1037/a0026883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettinati H. M., Weiss R. D., Miller W. R., Donovan D. M., Ernst D. B., Rounsaville B. J. Medical management (MM) treatment manual: A clinical research guide for medically trained clinicians providing pharmacotherapy as part of the treatment for alcohol dependence, Vol. 2. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2004. [Google Scholar]
- Staines G., Magura S., Rosenblum A., Fong C., Kosanke N., Foote J., Deluca A. Predictors of drinking outcomes among alcoholics. American Journal of Drug and Alcohol Abuse. 2003;29:203–218. doi: 10.1081/ada-120018847. doi:10.1081/ADA-120018847. [DOI] [PubMed] [Google Scholar]
- Stout R. L., Kelly J. F., Magill M., Pagano M. E. Association between social influences and drinking outcomes across three years. Journal of Studies on Alcohol and Drugs. 2012;73:489–497. doi: 10.15288/jsad.2012.73.489. doi:10.15288/jsad.2012.73.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vik P. W., Cellucci T., Hedt J., Jorgensen M. Transition to college: A classification and regression tree (CART) analysis of natural reduction of binge drinking. International Journal of Adolescent Medicine and Health. 2006;18:171–180. doi: 10.1515/ijamh.2006.18.1.171. doi:10.1515/IJAMH.2006.18.1.171. [DOI] [PubMed] [Google Scholar]
- Weisner C., Ray G. T., Mertens J. R., Satre D. D., Moore C. Short-term alcohol and drug treatment outcomes predict long-term outcome. Drug and Alcohol Dependence. 2003;71:281–294. doi: 10.1016/s0376-8716(03)00167-4. doi:10.1016/S0376-8716(03)00167-4. [DOI] [PubMed] [Google Scholar]
- Ye Y., Zhong X., Zhang H. A genome-wide tree- and forest-based association analysis of comorbidity of alcoholism and smoking. BMC Genetics, 6, Supplement 1. 2005:S135. doi: 10.1186/1471-2156-6-S1-S135. doi:10.1186/1471-2156-6-S1-S135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Legro R. S., Zhang J., Zhang L., Chen X., Huang H, Eisenberg E the Reproductive Medicine Network. Decision trees for identifying predictors of treatment effectiveness in clinical trials and its application to ovulation in a study of women with polycystic ovary syndrome. Human Reproduction. 2010;25:2612–2621. doi: 10.1093/humrep/deq210. doi:10.1093/humrep/deq210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Singer B. Recursive partitioning and applications, 2nd ed. New York, NY: Springer; 2010. [Google Scholar]
- Zhang H., Wang M., Chen X. Willows: A memory efficient tree and forest construction package. BMC Bioinformatics. 2009;10:130. doi: 10.1186/1471-2105-10-130. doi:10.1186/1471-2105-10-130. [DOI] [PMC free article] [PubMed] [Google Scholar]