Abstract
IMPORTANCE
Acute traumatic spinal cord injury results in disability and use of health care resources, yet data on contemporary national trends of traumatic spinal cord injury incidence and etiology are limited.
OBJECTIVE
To assess trends in acute traumatic spinal cord injury incidence, etiology, mortality, and associated surgical procedures in the United States from 1993 to 2012.
DESIGN, SETTING, AND PARTICIPANTS
Analysis of survey data from the US Nationwide Inpatient Sample databases for 1993–2012, including a total of 63 109 patients with acute traumatic spinal cord injury.
MAIN OUTCOMES AND MEASURES
Age- and sex-stratified incidence of acute traumatic spinal cord injury; trends in etiology and in-hospital mortality of acute traumatic spinal cord injury.
RESULTS
In 1993, the estimated incidence of acute spinal cord injury was 53 cases (95% CI, 52–54 cases) per 1 million persons based on 2659 actual cases. In 2012, the estimated incidence was 54 cases (95% CI, 53–55 cases) per 1 million population based on 3393 cases (average annual percentage change, 0.2%; 95% CI, −0.5% to 0.9%). Incidence rates among the younger male population declined from 1993 to 2012: for age 16 to 24 years, from 144 cases/million (2405 cases) to 87 cases/million (1770 cases) (average annual percentage change, −2.5%; 95% CI, −3.3% to −1.8%); for age 25 to 44 years, from 96 cases/million (3959 cases) to 71 cases/million persons (2930 cases), (average annual percentage change, −1.2%; 95% CI, −2.1% to −0.3%). A high rate of increase was observed in men aged 65 to 74 years (from 84 cases/million in 1993 [695 cases] to 131 cases/million [1465 cases]; average annual percentage change, 2.7%; 95% CI, 2.0%–3.5%). The percentage of spinal cord injury associated with falls increased significantly from 28% (95% CI, 26%–30%) in 1997–2000 to 66% (95% CI, 64%–68%) in 2010–2012 in those aged 65 years or older (P < .001). Although overall in-hospital mortality increased from 6.6% (95% CI, 6.1%–7.0%) in 1993–1996 to 7.5% (95% CI, 7.0%–8.0%) in 2010–2012 (P < .001), mortality decreased significantly from 24.2% (95% CI, 19.7%–28.7%) in 1993–1996 to 20.1% (95% CI, 17.0%–23.2%) in 2010–2012 (P = .003) among persons aged 85 years or older.
CONCLUSIONS AND RELEVANCE
Between 1993 and 2012, the incidence rate of acute traumatic spinal cord injury remained relatively stable but, reflecting an increasing population, the total number of cases increased. The largest increase in incidence was observed in older patients, largely associated with an increase in falls, and in-hospital mortality remained high, especially among elderly persons.
Traumatic spinal cord injury leads to chronic impairment and disability. Despite the substantial effects of spinal cord injury on health-related quality of life and health care spending, data on trends in incidence, etiology, and medical care of acute traumatic spinal cord injury in the United States have limited availability from contemporary nationwide studies. Prior incidence rates, including from the Spinal Cord Injury Model Systems,1 have been calculated based on regional estimates from the 1980s.2–14 The quantification of acute spinal cord injury incidence is essential to understand its contribution to estimates on persons with disability in the United States. Knowing trends in etiology of acute spinal cord injury would also help identify specific population groups at risk and help target preventive measures.
The objective of this study was to assess trends in national incidence, etiology, health care utilization, and in-hospital mortality in acute traumatic spinal cord injury from 1993 to 2012.
Methods
Patient Population
We used the Nationwide Inpatient Sample (NIS) databases for the years 1993 through 2012. The NIS is part of the Healthcare Cost and Utilization Project sponsored by the Agency for Healthcare Research and Quality. It is the largest all-payer inpatient database available in the United States.15 The NIS has been extensively used to estimate population-based estimates and trends for a variety of medical conditions.16–18 The NIS survey uses sampling techniques to ensure national representation and provides sampling weights to enable calculation of national rates. The NIS has been validated by an independent contractor and against the National Hospital Discharge Survey.19,20 Further details about the database, sampling techniques, and validation can be found elsewhere.15,19,20 Institutional review board exemption was granted by Vanderbilt University Medical Center; institutional review board approval was obtained from VA Boston Healthcare System and a waiver of informed consent was granted.
Acute Spinal Cord Injury Admissions
The NIS has information on primary International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes and secondary diagnosis and procedure codes for each patient record. The Centers for Disease Control and Prevention has defined acute traumatic spinal cord injury based on a clinical and ICD-9-CM criterion.21 We used the ICD-9-CM criterion to define cases of acute traumatic spinal cord injury. Per this criterion, cases of acute traumatic spinal cord injury included (1) records with a primary diagnosis code of acute traumatic spinal cord injury (see list of codes in eAppendix 1 in the Supplement) or (2) records with a primary diagnosis code of any form of injury (see list of codes in eAppendix 1) and a secondary diagnosis code of acute traumatic spinal cord injury. The ICD-9-CM codes for acute traumatic spinal cord injury included injuries to the cauda equina but did not include injuries to spinal nerve roots and spinal plexus.10 Reliable information on degree of neurological deficits such as quadriplegia or paraplegia or extent of neurological function was not available.
We also designed a second comprehensive approach to define cases of acute traumatic spinal cord injury. This approach defined a case as existing if any of the ICD-9-CM diagnoses codes in the databases represented an acute traumatic spinal cord injury. Using this approach, an injury diagnosis code was not required if the record had an ICD-9-CM diagnosis code for acute traumatic spinal cord injury. The rationale for using the second approach was to capture patients with acute traumatic spinal cord injury who may have had other concomitant disorders such as brain injury, fractures, and shock that may have been coded as the primary ICD-9-CM code. Data extracted using the first, more conservative approach were used for subsequent analyses to assess age-stratified rates, etiology, complications, and procedures so as to not overestimate spinal cord injury incidence and because this approach has been previously reported.21 Spinal cord injury captured by ICD-9-CM codes in our study include cervical, thoracic, and lumbosacral injuries with or without vertebral fractures.
Etiology, Complications, and Procedures
The etiology of spinal cord injury was categorized based on ICD-9-CM E codes (external causes of injury) into unintentional falls (henceforth referred to as falls), motor vehicle crashes, and firearm injuries. This categorization was performed based on coding guidelines from the Centers for Disease Control and Prevention22 with minor modifications. The Healthcare Cost and Utilization Project inpatient databases have been reported to have a high level of completeness for E codes23. E codes were included as 1 of the 15 diagnosis codes in the NIS prior to 2003 and as separate variables with up to 4 E codes from 2003 onward. There were substantial changes to E codes in October 1994; hence, etiology was determined starting in the year 1997 for our study (1995–1996 were not used to determine etiology to allow for enough time to elapse after these substantial changes to the E codes). Within the E codes, in 2001, there were substantial changes to the E917 codes (striking against or struck accidentally [by objects or persons]). Moreover, prior to 2001, the E917 codes did not distinguish between an injury leading to a fall or not. Hence, E917 codes were not used to ascertain falls (only 1.1% of spinal cord injury records from 1993–2012 carried this code without another code for fall; see eAppendix 2 in the Supplement). We used ICD-9-CM codes for both traffic and nontraffic motor vehicle crashes.
ICD-9-CM procedure codes were used to identify commonly performed surgical procedures during inpatient admissions for acute spinal cord injury (see list of codes in eAppendix 2). In-hospital complication rates in acute spinal cord injury were determined using ICD-9-CM diagnosis codes for pulmonary embolism and infarction, deep venous thrombosis of lower extremity, and pressure ulcer (see list of codes in eAppendix 2).
Statistical Analysis
We estimated the population-based number of patients with acute traumatic spinal cord injury in the United States from 1993–2012 by using sampling weights provided in the NIS databases. Within each sampling stratum, the NIS defines sampling weights as the ratio of discharges in the American Hospital Association survey data for nonrehabilitation community hospitals to discharges in the sample.15 We used revised NIS sampling weights, released in 2014, for each of the years.24 We calculated standard deviations and 95% confidence intervals around the population-based point estimates using strata and cluster variables. We calculated overall and age-stratified spinal cord injury incidence rates per 1 million persons by using population estimates for a given age group and year from the US Census Bureau.25–27 Ninety-five percent confidence intervals around incidence rates were derived by dividing 95% confidence intervals of spinal cord injury point estimates by the total US population for each strata.28
We also calculated the unweighted proportion of patients by spinal cord injury etiology, in-hospital complications, in-hospital mortality, surgical procedures performed, and other clinical and demographic characteristics over blocks of 3 to 5 consecutive years. In-hospital mortality includes all-cause death that resulted during the index admission. The un-weighted calculations do not provide nationally representative estimates but provide percentages among the spinal cord injury patients who were sampled. Confidence intervals for proportions of events were determined using large sample approximation to the binomial distribution.
We used joinpoint regression analysis to assess changes in spinal cord injury incidence and population-based rates. Specialized software developed by the Surveillance Research Program of the National Cancer Institute was used for this purpose.29 Joinpoint regression summarizes the trend in rates over a period of time and assesses significant changes in slopes of linear trend using average annual percentage change (AAPC) estimated from the regression model.30 We also present 95% confidence intervals around AAPCs using the empirical quantile method.31 Trend analyses for unweighted proportions were made using the Armitage trend test or logistic regression. P<.05 was considered statistically significant for the trend tests.
Results
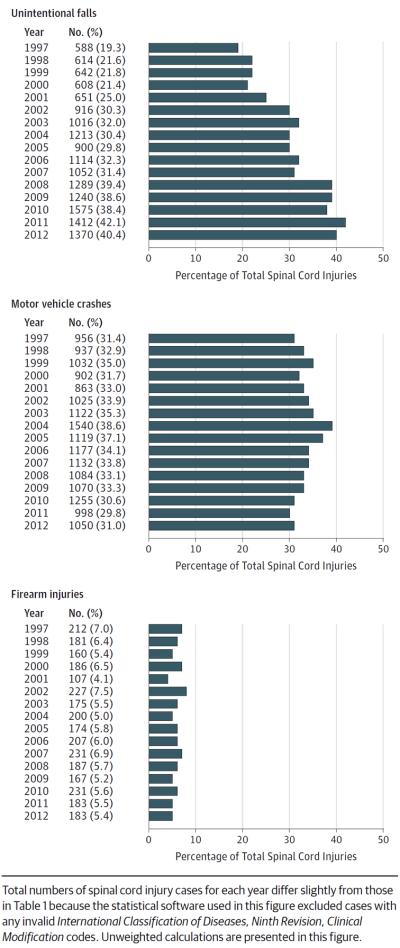
The total study sample consisted of 63 109 patients with acute traumatic spinal cord injury in 1993–2012. The actual number of cases with acute traumatic spinal cord injury in the NIS database increased from 2659 in 1993 to 3393 in 2012 (AAPC, 1.4%; 95% CI, 0.5%–2.3%) (Table 1). The estimated annual incidence rate was 53 cases (95% CI, 52–54 cases) per 1 million persons in 1993 and 54 cases (95% CI, 53–55 cases) per 1 million persons in 2012 (AAPC, 0.2%; 95% CI, −0.5% to 0.9%) (Figure 1 and eTable 1 in the Supplement). Age-stratified incidence rates showed a decreasing trend in younger age groups among the male population (a decrease from an estimated 144 cases/million [2405 cases] in 1993 to 87 cases/million [1770 cases] in 2012 for the 16- to 24-year-old age group [AAPC, −2.5%; 95% CI, −3.3% to −1.8%] and from 96 cases/million [3959 cases] in 1993 to 71 cases/million [2930 cases]in 2012 for the 25- to 44-year-old age group [AAPC, −1.2%; 95% CI, −2.1% to −0.3%]) (Table 2). Among the female population aged 16 to 24 years, the incidence rate decreased from 42 cases/million in 1993 to 27 cases/million in 2012 (AAPC, −1.8%; 95% CI, −3.1% to −0.5%). For both the male and female populations, a high rate of increase in spinal cord injury incidence from 1993 to 2012 was observed in elderly persons (for instance, from 84 cases/million [695 cases] to 131 cases/million [1465 cases] in men aged 65–74 years; AAPC, 2.7%; 95% CI, 2.0%–3.5%). Age- and sex-stratified numbers of cases in the databases and estimated numbers of age- and sex-stratified cases are provided in eTables 2 and 3 in the Supplement. Population estimates used to calculate incidence rates are provided in eTables 4 and 5 in the Supplement.
Table 1.
Number of Patients in Nationwide Inpatient Samples With Acute Traumatic Spinal Cord Injury in the United States, 1993–2012
| Spinal Cord Injury as Primary Diagnosis |
Spinal Cord Injury as Any Diagnoses |
|||
|---|---|---|---|---|
| Year | No. of Patients | Age, Mean, y | Male, % | No. of Patients |
| 1993 | 2659 | 40.5 | 73.5 | 3279 |
|
| ||||
| 1994 | 2680 | 40.5 | 75.5 | 3355 |
|
| ||||
| 1995 | 3112 | 40.9 | 72.1 | 3895 |
|
| ||||
| 1996 | 2983 | 42.0 | 73.2 | 3808 |
|
| ||||
| 1997 | 3048 | 41.8 | 72.4 | 4094 |
|
| ||||
| 1998 | 2848 | 42.5 | 73.2 | 3539 |
|
| ||||
| 1999 | 2946 | 42.1 | 72.8 | 3867 |
|
| ||||
| 2000 | 2849 | 43.3 | 74.7 | 3574 |
|
| ||||
| 2001 | 2611 | 44.7 | 73.6 | 3248 |
|
| ||||
| 2002 | 3025 | 44.8 | 72.8 | 3823 |
|
| ||||
| 2003 | 3180 | 45.1 | 71.2 | 4050 |
|
| ||||
| 2004 | 3993 | 44.2 | 71.3 | 4713 |
|
| ||||
| 2005 | 3021 | 44.8 | 71.3 | 3770 |
|
| ||||
| 2006 | 3453 | 46.3 | 72.5 | 4310 |
|
| ||||
| 2007 | 3357 | 46.8 | 72.3 | 4180 |
|
| ||||
| 2008 | 3274 | 48.8 | 70.0 | 4128 |
|
| ||||
| 2009 | 3217 | 49.3 | 69.7 | 4183 |
|
| ||||
| 2010 | 4106 | 48.6 | 71.1 | 5115 |
|
| ||||
| 2011 | 3354 | 51.1 | 70.1 | 4373 |
|
| ||||
| 2012 | 3393 | 50.5 | 70.7 | 4339 |
Figure 1.
Temporal Trends in Acute Traumatic Spinal Cord Injury Incidence Rate per 1 Million Persons in the United States, 1993–2012
Table 2.
Age- and Sex-Stratified Estimated Acute Traumatic Spinal Cord Injury Incidence Rates per 1 Million Persons in the United States
| Spinal Cord Injury Incidence Rate (95% CI) per Million |
||||||
|---|---|---|---|---|---|---|
| Year | Age 16–24 y | Age 25–44 y | Age 45–64 y | Age 65–74 y | Age 75–84 y | Age ≥85 y |
| Male | ||||||
|
| ||||||
| 1993 | 144 (112–177) | 96 (76–117) | 76 (61–91) | 84 (63–106) | 104 (74–134) | 204 (133–276) |
|
| ||||||
| 1994 | 151 (118–184) | 98 (75–120) | 86 (70–102) | 80 (61–100) | 126 (94–158) | 178 (119–238) |
|
| ||||||
| 1995 | 140 (106–174) | 99 (81–117) | 75 (63–87) | 81 (64–99) | 129 (101–158) | 200 (138–263) |
|
| ||||||
| 1996 | 134 (102–167) | 96 (76–115) | 80 (66–94) | 97 (76–117) | 108 (81–135) | 133 (71–194) |
|
| ||||||
| 1997 | 117 (87–147) | 87 (70–103) | 71 (57–85) | 78 (61–94) | 108 (85–131) | 154 (103–204) |
|
| ||||||
| 1998 | 130 (102–157) | 105 (83–126) | 77 (60–95) | 72 (56–89) | 150 (120–180) | 191 (127–254) |
|
| ||||||
| 1999 | 121 (97–144) | 90 (74–106) | 81 (68–95) | 83 (66–101) | 127 (100–155) | 221 (151–292) |
|
| ||||||
| 2000 | 113 (93–134) | 86 (70–101) | 76 (64–89) | 86 (69–103) | 122 (97–146) | 180 (128–232) |
|
| ||||||
| 2001 | 102 (80–123) | 75 (61–88) | 71 (61–82) | 88 (70–105) | 150 (122–178) | 196 (135–256) |
|
| ||||||
| 2002 | 103 (81–126) | 86 (69–102) | 80 (69–94) | 90 (73–106) | 138 (111–164) | 220 (165–275) |
|
| ||||||
| 2003 | 105 (83–126) | 81 (66–96) | 89 (74–104) | 91 (73–110) | 131 (106–155) | 220 (160–281) |
|
| ||||||
| 2004 | 139 (108–169) | 100 (80–120) | 111 (90–133) | 109 (85–132) | 147 (115–180) | 223 (160–286) |
|
| ||||||
| 2005 | 101 (80–122) | 73 (58–88) | 78 (65–92) | 87 (69–105) | 122 (97–148) | 192 (139–244) |
|
| ||||||
| 2006 | 107 (86–127) | 91 (75–107) | 92 (78–105) | 108 (89–127) | 155 (127–183) | 249 (192–307) |
|
| ||||||
| 2007 | 111 (87–134) | 83 (67–99) | 92 (76–109) | 104 (84–123) | 151 (121–181) | 244 (185–303) |
|
| ||||||
| 2008 | 90 (71–109) | 72 (58–86) | 86 (71–100) | 113 (93–133) | 160 (128–191) | 234 (172–296) |
|
| ||||||
| 2009 | 88 (71–106) | 66 (55–78) | 90 (76–104) | 119 (100–138) | 158 (128–188) | 218 (166–271) |
|
| ||||||
| 2010 | 108 (86–129) | 100 (82–119) | 112 (94–131) | 135 (110–160) | 196 (161–232) | 271 (206–336) |
|
| ||||||
| 2011 | 81 (63–99) | 67 (51–82) | 89 (72–105) | 122 (98–146) | 179 (149–209) | 238 (186–291) |
|
| ||||||
| 2012 | 87 (75–99) | 71 (62–79) | 105 (94–117) | 131 (113–149) | 151 (127–176) | 234 (183–285) |
|
| ||||||
| Female | ||||||
|
| ||||||
| 1993 | 42 (31–54) | 26 (19–32) | 27 (20–33) | 32 (24–41) | 65 (49–80) | 107 (71–142) |
|
| ||||||
| 1994 | 37 (27–48) | 26 (20–32) | 22 (17–28) | 32 (24–41) | 53 (40–66) | 91 (61–121) |
|
| ||||||
| 1995 | 34 (27–41) | 31 (25–37) | 25 (19–31) | 51 (40–63) | 84 (66–101) | 78 (54–102) |
|
| ||||||
| 1996 | 32 (25–40) | 29 (23–34) | 28 (22–33) | 38 (28–49) | 68 (53–83) | 111 (83–139) |
|
| ||||||
| 1997 | 32 (24,40) | 24 (20–29) | 21 (17–26) | 44 (34–54) | 64 (50–78) | 86 (59–113) |
|
| ||||||
| 1998 | 38 (28–48) | 24 (19–29) | 27 (22–32) | 39 (30–47) | 66 (52–81) | 100 (72–128) |
|
| ||||||
| 1999 | 38 (29–48) | 23 (19–27) | 25 (20–30) | 32 (24–41) | 63 (49–77) | 87 (61–113) |
|
| ||||||
| 2000 | 31 (22–39) | 23 (18–28) | 19 (14–23) | 33 (25–42) | 66 (53–79) | 117 (87–147) |
|
| ||||||
| 2001 | 26 (19–33) | 18 (14–23) | 22 (17–26) | 36 (27–45) | 80 (64–95) | 72 (50–93) |
|
| ||||||
| 2002 | 29 (22–36) | 24 (19–28) | 26 (20–32) | 36 (27–45) | 80 (64–96) | 93 (68–118) |
|
| ||||||
| 2003 | 33 (25–42) | 25 (19–31) | 27 (22–32) | 49 (39–59) | 77 (60–93) | 101 (76–126) |
|
| ||||||
| 2004 | 45 (33–58) | 33 (25–41) | 35 (27–42) | 54 (37–71) | 96 (79–113) | 109 (80–137) |
|
| ||||||
| 2005 | 30 (22–37) | 22 (17–27) | 23 (19–28) | 40 (31–49) | 84 (70–97) | 110 (83–136) |
|
| ||||||
| 2006 | 35 (27–44) | 23 (18–27) | 31 (25–36) | 43 (34–52) | 83 (68–98) | 122 (94–151) |
|
| ||||||
| 2007 | 32 (24–41) | 22 (18–27) | 28 (23–33) | 46 (36–56) | 97 (80–113) | 111 (82–139) |
|
| ||||||
| 2008 | 25 (17–32) | 24 (18–30) | 30 (24–35) | 54 (43–65) | 99 (81–117) | 123 (94–152) |
|
| ||||||
| 2009 | 25 (18–31) | 20 (16–25) | 30 (25–35) | 60 (47–72) | 99 (79–119) | 121 (95–148) |
|
| ||||||
| 2010 | 35 (26–44) | 28 (22–35) | 36 (30–42) | 63 (51–75) | 113 (92–133) | 156 (126–187) |
|
| ||||||
| 2011 | 21 (15–27) | 20 (15–24) | 30 (25–35) | 55 (44–67) | 100 (83–118) | 151 (123–180) |
|
| ||||||
| 2012 | 27 (21–33) | 21 (17–24) | 35 (30–39) | 53 (44–62) | 101 (84–118) | 134 (109–159) |
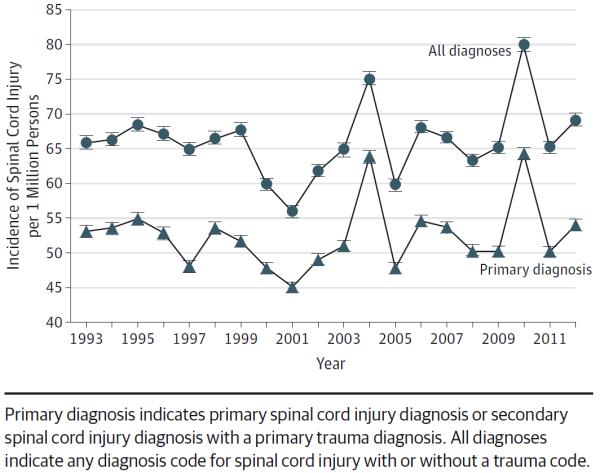
The etiology of spinal cord injury included falls, motor vehicle crashes, and firearm injuries in a majority of the cases from 1997 to 2012 (Figure 2). There was a significant increase in the proportion of traumatic spinal cord injuries resulting from falls between 1997 (19.3%; 95% CI, 17.9%–20.7%) and 2012 (40.4%; 95% CI, 38.7%–42.0%; P < .001) (eTable 6 in the Supplement). Age-stratified trends showed an increase in fall-related spinal cord injury as a proportion of total spinal cord injury cases among those aged 65 years or older between 1997–2000 (28%; 95% CI, 26%–30%) and 2010–2012 (66%; 95% CI, 64%–68%; P < .001) (eTable 7 in the Supplement). Spinal cord injury from firearms was one of the major contributors of spinal cord injury in the 16- to 24-year-old age group (14%–18% of cases). Motor vehicle crash was the etiology in 22.3% (95% CI, 19.7%–25.0%) of cases in 1997–2000 and in 17.9% (95% CI, 15.8%–19.9%) of cases in 2010–2012 in the 65- to 74-year-old age group, in 20.2% (95% CI, 17.5%–22.9%) of cases in 1997–2000 and in 15.4% (95% CI, 13.2%–17.6%) of cases in 2010–2012 in the 75-to 84-year-old age group, and in 11.5% (95% CI, 8.5%–14.6%) of cases in 1997–2000 and in 10.1% (95% CI, 7.8%–12.4%) of cases in 2010–2012 in those aged 85 years or older.
Figure 2.
Trends in Etiology of Acute Traumatic Spinal Cord Injury in the United States
Some of the most commonly performed surgical procedures showed a modest increase from 1993 to 2012: for inter-vertebral disk excision, from 11.2% (95% CI, 10.6%–11.7%) to 15.9% (95% CI, 15.2%–16.6%), and for spinal canal decompression, from 10.2% (95% CI, 9.6%–10.7%) to 15.9% (95% CI, 15.2%–16.6%). The percentage of patients with spinal cord injury undergoing vena cava filter placement showed a substantial increase from 4% (95% CI, 3.5%–4.2%) in 1993–1996 to 14.5% (95% CI, 13.9%–15.0%) in 2005–2009 (Table 3). During acute care inpatient stays in 2005–2009, 1.14% (95% CI, 0.98%–1.3%) of patients had a pulmonary embolism/infarction, 2.64% (95% CI, 2.39%–2.90%) had a deep venous thrombosis, and 4.84% (95% CI, 4.52%–5.17%) had a pressure ulcer. In 2010–2012, 1.5% (95% CI, 1.27%–1.73%) of patients had a pulmonary embolism/infarction, 2.93% (95% CI, 2.61%–3.25%) had a deep venous thrombosis, and 4.55% (95% CI, 4.16%–4.94%) had a pressure ulcer.
Table 3.
Surgical Procedures Performed for Acute Traumatic Spinal Cord Injury in the United Statesa
| No. With Procedure (%) [95% CI] |
|||||
|---|---|---|---|---|---|
| Procedures | 1993–1996 (n=11 425)b | 1997–2000 (n=11 684)b | 2001–2004 (n=12 796)b | 2005–2009 (n=16 315)b | 2010–2012 (n=10 849)b |
| Intervertebral disk excision | 1276 (11.2) [10.6–11.7] | 1617 (13.8) [13.2–14.5] | 1949 (15.2) [14.6–15.9] | 2544 (15.6) [15.0–16.1] | 1725 (15.9) [15.2–16.6] |
|
| |||||
| Spinal canal decompression | 1160 (10.2) [9.6–10.7] | 1343 (11.5) [10.9–12.1] | 1676 (13.1) [12.5–13.7] | 2467 (15.1) [14.6–15.7] | 1721 (15.9) [15.2–16.6] |
|
| |||||
| Spinal fusionc | 2019 (12.4) [11.9–12.9] | 1601 (14.8) [14.1–15.4] | |||
|
| |||||
| Vena cava filter | 441 (3.9) [3.5–4.2] | 745 (6.4) [5.9–6.8] | 1134 (8.9) [8.4–9.4] | 2359 (14.5) [13.9–15.0] | 1192 (11.0) [10.4–11.6] |
Unweighted calculations are presented.
Numbers of spinal cord injury cases are slightly different from those in Table 1 because statistical software used for this table excludes cases with any invalid International Classification of Diseases, Ninth Revision, Clinical Modification codes.
Calculated only for 2005–2012 because effective for discharges after October 1, 2004, the Centers for Medicare & Medicaid Services added payments for new spinal fusion devices.
Acute inpatient mortality was 6.6% (95% CI, 6.1%–7.0%) in 1993–1996 and 7.5% (95% CI, 7.0%–8.0%) in 2010–2012 (P<.001 for trend). However, mortality increased with increasing age but showed a decreasing trend over time among those aged 85 years or older from 24.2% (95% CI, 19.7%–28.7%) in 1993–1996 to 19.1% (95% CI, 16.4%–21.7%) in 2005–2009 and to 20.1% (95% CI, 17.0%–23.2%) in 2010–2012 (P = .003) (Table 4).
Table 4.
Temporal Trends in Outcomes of Acute Traumatic Spinal Cord Injury in the United Statesa
| Years |
P Value for Armitage Trend | |||||
|---|---|---|---|---|---|---|
| Characteristics | 1993–1996 | 1997–2000 | 2001–2004 | 2005–2009 | 2010–2012 | |
| Mortality | ||||||
|
| ||||||
| Age 16–24 y | .02 | |||||
|
| ||||||
| No. died/total | 90/2402 | 74/2254 | 88/2280 | 121/2664 | 70/1475 | |
|
| ||||||
| % (95% CI) | 3.8 (3.0–4.5) | 3.3 (2.5–4.0) | 3.9 (3.1–4.7) | 4.5 (3.8–5.3) | 4.8 (3.7–5.8) | |
|
| ||||||
| Age 25–44 y | .05 | |||||
|
| ||||||
| No. died/total | 172/4190 | 137/4101 | 149/3886 | 194/4393 | 121/2607 | |
|
| ||||||
| % (95% CI) | 4.1 (3.5–4.7) | 3.3 (2.8–3.9) | 3.8 (3.2–4.4) | 4.4 (3.8–5.0) | 4.6 (3.8–5.4) | |
|
| ||||||
| Age 45–64 y | .07 | |||||
|
| ||||||
| No. died/total | 99/2160 | 128/2438 | 193/3225 | 282/4619 | 189/3428 | |
|
| ||||||
| % (95% CI) | 4.6 (3.7–5.5) | 5.3 (4.4–6.1) | 6.0 (5.2–6.8) | 6.1 (5.4–6.8) | 5.5 (4.7–6.3) | |
|
| ||||||
| Age 65–74 y | .01 | |||||
|
| ||||||
| No. died/total | 120/970 | 112/949 | 140/1109 | 181/1680 | 130/1376 | |
|
| ||||||
| % (95% CI) | 12.4 (10.3–14.4) | 11.8 (9.7–13.9) | 12.6 (10.7–14.6) | 10.8 (9.3–12.3) | 9.5 (7.9–11.0) | |
|
| ||||||
| Age 75–84 y | .02 | |||||
|
| ||||||
| No. died/total | 140/731 | 168/851 | 190/1072 | 259/1462 | 153/1001 | |
|
| ||||||
| % (95% CI) | 19.2 (16.3–22.0) | 19.7 (17.1–22.4) | 17.7 (15.4–20.0) | 17.7 (15.8–19.7) | 15.3 (13.1–17.5) | |
|
| ||||||
| Age ≥85 y | .003 | |||||
|
| ||||||
| No. died/total | 84/347 | 109/424 | 143/494 | 160/840 | 129/643 | |
|
| ||||||
| % (95% CI) | 24.2 (19.7–28.7) | 25.7 (21.5–29.9) | 29.0 (24.9–32.9) | 19.1 (16.4–21.7) | 20.1 (17.0–23.2) | |
|
| ||||||
| Overall | <.001 | |||||
|
| ||||||
| No. died/total | 749/11 414 | 760/11 677 | 940/12 646 | 1227/16 302 | 811/10 837 | |
|
| ||||||
| % (95% CI) | 6.6 (6.1–7.0) | 6.5 (6.1–7.0) | 7.4 (7.0–7.9) | 7.5 (7.1–7.9) | 7.5 (7.0–8.0) | |
|
| ||||||
| Length of acute stay, median (interquartile range), d | 10 (4–20) | 8 (3–16) | 8 (4–16) | 8 (4–16) | 7 (4–15) | |
Unweighted calculations are presented. Excludes missing data (for mortality, n = 193 [0.31%]; for length of stay, n = 55 [0.09%]).
Discussion
We assessed national trends in incidence, etiology, surgical procedures performed, and mortality during inpatient admission for acute traumatic spinal cord injury in the United States from 1993 to 2012. Our data show that the overall absolute number of cases of acute traumatic spinal cord injury has modestly increased from 1993 to 2012, whereas the incidence rate has remained relatively stable (ie, 53 cases/million population in 1993 to 54 cases/million in 2012), with an estimated 13 706 cases in 1993 and an estimated 16 965 cases in 2012. There was a substantial increase in falls contributing to spinal cord injury incidence in those aged 65 to 84 years. There was substantial morbidity and mortality during acute inpatient hospital stays among patients with traumatic spinal cord injury. There were also increases in the proportion of cases undergoing procedures such as intervertebral disk excision and spinal canal decompression performed during inpatient acute spinal cord injury admissions.
Our findings on incidence rates of spinal cord injury are similar to findings from other studies. The Spinal Cord Injury Model Systems have for many years been the best source of data on the epidemiology of acute spinal cord injury.1 An incidence rate of 40 per 1 million persons is based on regional estimates from the 1980s.1 The most recent Model Systems estimate of 12 500 new cases per year was revised recently from 11 000 new cases per year based on the increase in the US population. A recent study based on the Nationwide Emergency Department Sample estimated the spinal cord injury incidence in 2007–2009 to be 56.4 per 1 million adults.32 State registries from the 1980s have been discontinued.33 Use of regional spinal cord injury incidence rates from the 1980s and extrapolation of those data to the current US population do not account for changes in seatbelt laws, vehicle safety, a rapidly increasing elderly population that is at a higher risk of falls, and advances in health care delivery that may lead to reduced motor vehicle crash mortality. In one of the first estimates of spinal cord injury incidence for 1970–1977,3 Bracken et al reported an overall incidence of 40.1 per 1 million with a male-female ratio of 2.4:1.
Because the incidence and etiology of spinal cord injury vary by age, we reported overall incidence and age-stratified incidence rates from 1993 to 2012. The overall incidence rate of spinal cord injury in the male population aged 16 to 24 years (144 cases/million in 1993 and 87 cases/million in 2012) and aged 25 to 44 years (96 cases/million in 1993 and 71 cases/million in 2012) substantially declined over time. Public education, improved motor vehicle safety features, stricter safety belt laws, and drunk driving laws and their enforcement may have contributed to this overall decline in spinal cord injury rates in these age groups.34 Price et al10 used data from the state of Oklahoma and reported that incidence rates of spinal cord injury were highest in the male 20- to 24-year-old population (annual rate, 144 cases/million) followed by the male 15- to 19-year-old population (annual rate, 136 cases/million). Our study does not account for those who died at the scene of the injury or those who may have died in the emergency department. We also found that spinal cord injury incidence rate was the highest (in most of the years) in those aged 85 years or older but that the rates showed a small increase over time. Conversely, spinal cord injury incidence rates have substantially increased over time in the 65- to 74-year-old and 75- to 84-year-old age groups and now account for a larger proportion of total spinal cord injury cases because of the increasing elderly population.
There was also an increase in the proportion of spinal cord injuries resulting from falls among elderly people. This is a major public health issue and it likely represents a more active 65- to 84-year-old US population currently compared with the 1990s, which increases the risk of falls in this age group. This issue may be further compounded in the future because of the aging population in the United States. Although spinal cord injury resulting from firearm injuries remained relatively stable over the duration of our study, firearm injury is a major preventable contributor of spinal cord injury, especially in the 16- to 24-year-old age group, in whom the rate of spinal cord injury attributable to firearm injury was higher. Surkin et al11 reported data from the state of Mississippi and found that vehicular causes followed by violence were the most common causes of spinal cord injury between 1992 and 1994.
The use of vena cava filters in acute spinal cord injury has also substantially increased from 1993–1996 to 2010–2012. This may represent the increased awareness of deep venus thrombosis as a serious complication and the increased use of retrievable vena cava filters since the early 2000s.35 It may also represent improved ICD-9-CM coding of these procedures in the databases over time. Other procedures performed during acute inpatient spinal cord injury admissions, such as intervertebral disk excision and spinal canal decompression, also increased during the period of this study.
Our study has several limitations. First, spinal cord injury incidence may be underestimated because the NIS does not include acute spinal cord injury cases from federal facilities, although most patients with acute spinal cord injury are transferred to nonfederal facilities. Second, there may be errors in coding of acute traumatic spinal cord injury, although the NIS has been extensively validated and reported to perform well for many estimates.19,20 The ICD-9-CM codes for patients with acute spinal cord injury vs patients with chronic spinal cord injury who are subsequently admitted to a hospital are different. It is possible that some patients were double counted or miscoded in the NIS, although there is no evidence to suggest that this coding bias was differential across the years of our study or between acute and chronic spinal cord injury. Third, the E codes for classification of falls has undergone some changes since October 1994.22 Most of these changes (such as adding a new fourth digit to some of the ICD-9-CM codes for falls) were made to classify falls into expanded categories and likely do not affect our overall estimates of the percentage of patients with falls. Moreover, most of these changes occurred in 1995 and our study determined the etiology of spinal cord injury starting in 1997. Fourth, the NIS database does not include information on variables such as degree of neurologic deficits and clinical functional outcomes.
Conclusions
Between 1993 and 2012, the incidence rate of acute traumatic spinal cord injury remained relatively stable but, reflecting an increasing population, the total number of cases increased. The largest increase in the incidence of spinal cord injury was observed among older patients, largely associated with an increase in falls, and in-hospital mortality remained high, especially among elderly persons.
Supplementary Material
Acknowledgments
Funding/Support: Dr Jain is supported by funding from National Institute of Arthritis and Musculoskeletal and Skin Diseases project 1K23AR059199 and the Foundation for Physical Medicine and Rehabilitation. Drs Morse and Garshick are supported by VA Rehabilitation Research and Development Merit Review grants B6618R and I01RX000792, National Institute of Health grant AR059270, and US Department of Education National Institute on Disability and Rehabilitation Research grant H133N110010.
Role of the Funders/Sponsors: The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Jain and Mr Ayers had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Jain, Harris, Morse, O'Connor.
Acquisition, analysis, or interpretation of data: Jain, Ayers, Peterson, Garshick.
Drafting of the manuscript: Jain, Ayers, Peterson, Harris, Garshick.
Critical revision of the manuscript for important intellectual content: Ayers, Peterson, Harris, Morse, O'Connor, Garshick.
Statistical analysis: Jain, Ayers, Peterson, Garshick.
Obtained funding: Garshick.
Administrative, technical, or material support: Peterson, Harris, Morse, O'Connor.
Study supervision: Harris, Morse, Garshick.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Garshick reports receipt of author royalty fees for UpToDate sections on respiratory physiology and respiratory health in chronic spinal cord injury. No other disclosures were reported.
Previous Presentation: An abstract of part of this work was presented at the Association of Academic Physiatrists' annual meeting; March 8, 2013; New Orleans, LA.
REFERENCES
- 1.National Spinal Cord Injury Statistical Center Spinal cord injury facts and figures at a glance. J Spinal Cord Med. 2013;36(1):1–2. doi: 10.1179/1079026813Z.000000000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.A comprehensive plan for spinal cord injury services in Pennsylvania. Pa Med. 1978;81(5):29–38. 43–54. [PubMed] [Google Scholar]
- 3.Bracken MB, Freeman DH, Jr, Hellenbrand K. Incidence of acute traumatic hospitalized spinal cord injury in the United States, 1970–1977. Am J Epidemiol. 1981;113(6):615–622. doi: 10.1093/oxfordjournals.aje.a113140. [DOI] [PubMed] [Google Scholar]
- 4.DeVivo MJ, Fine PR, Maetz HM, Stover SL. Prevalence of spinal cord injury: a reestimation employing life table techniques. Arch Neurol. 1980;37(11):707–708. doi: 10.1001/archneur.1980.00500600055011. [DOI] [PubMed] [Google Scholar]
- 5.Griffin MR, O'Fallon WM, Opitz JL, Kurland LT. Mortality, survival and prevalence: traumatic spinal cord injury in Olmsted County, Minnesota, 1935–1981. J Chronic Dis. 1985;38(8):643–653. doi: 10.1016/0021-9681(85)90018-9. [DOI] [PubMed] [Google Scholar]
- 6.Harvey C, Rothschild BB, Asmann AJ, Stripling T. New estimates of traumatic spinal cord injury prevalence: a survey-based approach. Paraplegia. 1990;28(9):537–544. doi: 10.1038/sc.1990.73. [DOI] [PubMed] [Google Scholar]
- 7.Kalsbeek WD, McLaurin RL, Harris BS, III, Miller JD. The National Head and Spinal Cord Injury Survey: major findings. J Neurosurg. 1980;(suppl):S19–S31. [PubMed] [Google Scholar]
- 8.Kirshblum SC, Groah SL, McKinley WO, Gittler MS, Stiens SA. Spinal cord injury medicine, I: etiology, classification, and acute medical management. Arch Phys Med Rehabil. 2002;83(3)(suppl 1):S50–S57. S90–S98. doi: 10.1053/apmr.2002.32156. [DOI] [PubMed] [Google Scholar]
- 9.Kraus JF, Franti CE, Riggins RS, Richards D, Borhani NO. Incidence of traumatic spinal cord lesions. J Chronic Dis. 1975;28(9):471–492. doi: 10.1016/0021-9681(75)90057-0. [DOI] [PubMed] [Google Scholar]
- 10.Price C, Makintubee S, Herndon W, Istre GR. Epidemiology of traumatic spinal cord injury and acute hospitalization and rehabilitation charges for spinal cord injuries in Oklahoma, 1988–1990. Am J Epidemiol. 1994;139(1):37–47. doi: 10.1093/oxfordjournals.aje.a116933. [DOI] [PubMed] [Google Scholar]
- 11.Surkin J, Gilbert BJ, Harkey HL, III, Sniezek J, Currier M. Spinal cord injury in Mississippi: findings and evaluation, 1992–1994. Spine (Phila Pa 1976) 2000;25(6):716–721. doi: 10.1097/00007632-200003150-00011. [DOI] [PubMed] [Google Scholar]
- 12.Thurman DJ, Burnett CL, Jeppson L, Beaudoin DE, Sniezek JE. Surveillance of spinal cord injuries in Utah, USA. Paraplegia. 1994;32(10):665–669. doi: 10.1038/sc.1994.107. [DOI] [PubMed] [Google Scholar]
- 13.Warren S, Moore M, Johnson MS. Traumatic head and spinal cord injuries in Alaska (1991–1993) Alaska Med. 1995;37(1):11–19. [PubMed] [Google Scholar]
- 14.Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord. 2006;44(9):523–529. doi: 10.1038/sj.sc.3101893. [DOI] [PubMed] [Google Scholar]
- 15.Healthcare Cost and Utilization Project [Accessed April 21, 2013];NIS database documentation. 2013 http://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp.
- 16.Healthcare Cost and Utilization Project [Accessed March 15, 2014];Research spotlights. 2014 Feb; http://www.hcup-us.ahrq.gov/reports/spotlights.jsp.
- 17.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 18.Jena AB, Sun EC, Romley JA. Mortality among high-risk patients with acute myocardial infarction admitted to US teaching-intensive hospitals in July: a retrospective observational study. Circulation. 2013;128(25):2754–2763. doi: 10.1161/CIRCULATIONAHA.113.004074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Healthcare Cost and Utilization Project [Accessed April 21, 2013];HCUP Quality Control Procedures. http://www.ahrq.gov/research/data/hcup/sasddocu/techsupp2.pdf.
- 20.Whalen D, Houchens R, Elixhauser A. [Accessed May 20, 2015]; (HCUP Methods Series Report 2003-1).Final 2000 NIS Comparison Report. http://www.hcup-us.ahrq.gov/reports/methods/2000NISComparisonReportFinal.pdf.
- 21.Centers for Disease Control and Prevention Trends in traumatic spinal cord injury–New York, 1982–1988. MMWR Morb Mortal Wkly Rep. 1991;40(31):535–537. 543. [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention [Accessed April 3, 2013];Recommended framework of E-code groupings for presenting injury mortality and morbidity data. http://www.cdc.gov/injury/wisqars/ecode_matrix.html.
- 23.Coben JH, Steiner CA, Barrett M, Merrill CT, Adamson D. Completeness of cause of injury coding in healthcare administrative databases in the United States, 2001. Inj Prev. 2006;12(3):199–201. doi: 10.1136/ip.2005.010512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Healthcare Cost and Utilization Project [Accessed December 24, 2014];Trend weights for 1993–2011 HCUP NIS data. 2014 Sep; http://www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp.
- 25.US Census Bureau [Accessed June 7, 2012];Resident population estimates of the United States by age and sex: April 1, 1990 to July 1, 1999. http://www.census.gov/popest/data/national/totals/1990s/tables/nat-agesex.txt.
- 26.US Census Bureau [Accessed June 7, 2012];Annual estimates of the resident population for the United States, regions, states, and Puerto Rico: April 1, 2000 to July 1, 2009. 2009 Dec; http://www.census.gov/popest/data/historical/2000s/vintage_2009/
- 27.US Census Bureau [Accessed December 27, 2014];Annual estimates of the resident population for selected age groups by sex: April 1, 2010 to July 1, 2012. 2013 Jun; https://www.census.gov/popest/data/historical/2010s/vintage_2012/national.html.
- 28.Barrett M, Lopez-Gonzalez L, Coffey R, Levit K. (HCUP Methods Series Report 2014-02).Population Denominator Data for Use With the HCUP Databases (Updated With 2013 Population Data) http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.
- 29.National Cancer Institute . Joinpoint Regression Program, Version 4.2.0. Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute; Bethesda, MD: Apr, 2015. [Google Scholar]
- 30.National Cancer Institute [Accessed December 12, 2013];Average annual percent change. 2013 http://surveillance.cancer.gov/joinpoint/webhelp/Executing_the_Joinpoint_Parameters/Statistical_Notes/Statistics_Related_to_the_k-joinpoint_Model/Average_Annual_Percent_Change.htm.
- 31.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 32.Selvarajah S, Hammond ER, Haider AH, et al. The burden of acute traumatic spinal cord injury among adults in the United States: an update. J Neurotrauma. 2014;31(3):228–238. doi: 10.1089/neu.2013.3098. [DOI] [PubMed] [Google Scholar]
- 33.Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50(5):365–372. doi: 10.1038/sc.2011.178. [DOI] [PubMed] [Google Scholar]
- 34.Insurance Institute for Highway Safety [Accessed April 18, 2013];Safety belt and child restraint laws. 2013 http://www.iihs.org/iihs/topics/laws/safetybeltuse?topicName=safety-belts.
- 35.Kaufman JA, Kinney TB, Streiff MB, et al. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. J Vasc Interv Radiol. 2006;17(3):449–459. doi: 10.1097/01.rvi.0000203418-39769.0d. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.