Abstract
PURPOSE
The aim of this study was to determine the incidence of invasive breast carcinoma in patients with preoperative diagnosis of ductal carcinoma in situ (DCIS) by stereotactic vacuum-assisted biopsy (SVAB) performed for microcalcification-only lesions, and to identify the predictive factors of invasion.
METHODS
From 2000 to 2010, the records of 353 DCIS patients presenting with microcalcification-only lesions who underwent SVAB were retrospectively reviewed. The mammographic size of microcalcification cluster, presence of microinvasion within the cores, the total number of calcium specks, and the number of calcium specks within the retrieved core biopsy specimen were recorded. Patients were grouped as those with or without invasion in the final pathologic report, and variables were compared between the two groups.
RESULTS
The median age was 58 years (range, 34–88 years). At histopathologic examination of the surgical specimen, 63 of 353 patients (17.8%) were found to have an invasive component, although SVAB cores had only shown DCIS preoperatively. The rate of underestimation was significantly higher in patients with microcalcification covering an area of 40 mm or more, in the presence of microinvasion at biopsy, and in cases where less than 40% of the calcium specks were removed from the lesion.
CONCLUSION
Invasion might be underestimated in DCIS cases diagnosed with SVAB performed for microcalcification-only lesions, especially when the mammographic size of calcification is equal to or more than 40 mm or if microinvasion is found within the biopsy specimen and less than 40% of the calcifications are removed. At least 40% of microcalcification specks should be removed from the lesion to decrease the rate of underestimation with SVAB.
Because of the widespread use of breast screening mammography, the number of women diagnosed with ductal carcinoma in situ (DCIS) has increased dramatically in recent years. DCIS is a noninvasive form of breast cancer, accounting for up to 30% of breast cancers in screening populations and approximately 5% of breast carcinomas in symptomatic patients (1–3). DCIS has a variety of mammographic presentations, but the most common mammographic feature is microcalcification (4). Indeed 80%–90% of DCIS lesions present with microcalcifications only, without any accompanying mass lesions (4). Other findings such as masses, nodular abnormalities, dilated retroareolar ducts, architectural distortions, and developing densities have also been reported (5).
Ultrasound-guided biopsy is often the method of choice for sonographically visible breast lesions as it provides easy access for biopsy. However, in cases when the abnormality seen on mammography is not visible on ultrasonography, stereotactic biopsy is the recommended sampling method. For microcalcification-only lesions with no accompanying mass, ultrasonography often fails to identify the site of the lesion; hence, stereotactic biopsy is used more frequently.
In most breast units, stereotactic 14-gauge automated core biopsy has been replaced by stereotactic vacuum-assisted biopsy (SVAB) using 8- to 11-gauge needles (6). Large core SVAB allows larger samples to be obtained in a shorter period of time compared with samples obtained using automated core biopsy devices (7). Moreover, this technique has the advantage of a single insertion in the area of interest compared with automated core biopsy devices, which require repeated insertions. Several published articles have shown that SVAB decreased the rate of cancer underestimation and the rate of failure to retrieve breast microcalcifications (8).
The management of noninvasive and invasive breast cancers is different and therefore, an accurate preoperative diagnosis is crucial for adequate surgical planning. Underestimation of DCIS lesions occurs when an invasive component is found after surgery, which had been missed at the initial preoperative sampling. The underestimation rate of stereotactic 14-gauge automated core biopsy in DCIS was reported as 16%–35% (9–11), while that of SVAB was 5%–29% (6, 9, 11–13).
The purpose of this study was to determine the rate, causes, and predictive factors of underestimation of invasive carcinoma in patients diagnosed with DCIS following SVAB of microcalcification-only lesions.
Methods
From February 2000 to December 2010, 1480 SVAB procedures were performed for lesions detected on mammography. Our department policy is to perform stereotactic biopsy when US shows no abnormality. The stereotactic breast biopsy database was retrospectively reviewed. Of 1480 biopsies, 385 (26%) were reported as DCIS lesions. Of 385 biopsies, 376 (97.6%) were for microcalcification-only lesions. The remaining nine biopsies were for architectural distortions (n=3), masses (n=4), and asymmetric densities (n=2), all of which were excluded from this study. In addition, 23 of 376 microcalcification-only lesions were also excluded because postoperative surgical data was unavailable. Thus, 353 lesions were included in this study. In line with our Trust’s policy, ethics committee approval was not required as it was a retrospective study.
Biopsy procedure
All SVABs were performed on a digital prone table (Fischer Imaging) using 11-gauge vacuum probes (Mammotome, Ethicon Endo-Surgery). The target lesion was identified following the scout and two 15° stereotactic images. After local anesthetic infiltration of 10 mL 2% lidocaine, the needle was inserted in the center of the lesion. A second set of stereotactic images was obtained to confirm the accuracy of the position of the needle. Needle-tip location was modified, if required, to ensure its vicinity to the target. In cases where more than one lesion was targeted, a different device was used. Among 353 SVABs, there was only one patient where post-biopsy hematoma formation required a surgical drainage. For any given biopsy procedure, when subsequent examination of the biopsy site was deemed necessary for whatever reason, a radiopaque biopsy marking clip was inserted into the biopsy site after completion of the biopsy. Post-biopsy mammograms were obtained to confirm clip placement and to check for residual calcifications.
Radiography of specimen
The core specimens were visualized in a digital imaging machine (Faxitron X-ray Corporation) incorporating the ability to magnify four times. The exposure factors of 16 kV and 10 mAs were used to confirm that the lesion was obtained within the specimen. The specimen radiograph was assessed while the patient was still in position. If the specimen radiograph showed no calcification in the cores, further sets of biopsies were obtained with further specimen radiography until adequate calcium retrieval was obtained. The specimens were separated into two categories as with and without calcification before being sent for histopathologic examination The tissue specimens were then placed in formalin to be processed at pathology. Total number of calcium specks retrieved was recorded at the time of biopsy from the magnification views.
Pathology of specimen
Pathologic handling of specimen was performed in line with the NHSBSP guideline and the Royal College of Pathologists guidelines (14).
Data collection and analysis
The mammographic findings were recorded using a coding system from 1 to 5 according to the NHSBSP and the Royal College of Radiologists guidelines. M1, normal; M2, benign; M3, indeterminate/probably benign; M4, suspicious of malignancy; M5, highly suspicious of malignancy. Royal College of Radiologists Breast Group (RCRBG) scores can be equated with Breast Imaging Reporting and Data System (BI-RADS) scores as follows: RCRBG score 1 with BI-RADS 1/2, RCRBG score 2 with BI-RADS 3, RCRBG score 3 with BI-RADS 4a/b, RCRBG score 4 with BI-RADS 4c, and RCRBG score 5 with BI-RADS 5 (15).
The patient type (screening or symptomatic), lesion size, mammographic code, percent of the retrieved calcification (number of removed specks of microcalcification versus all visible microcalcification specks on initial magnification mammography), breast composition (entirely fat, scattered density, heterogeneously dense, extremely dense), number of core specimens obtained, the nuclear grade of tumor, and the presence or absence of necrosis, and the presence or absence of microinvasion were recorded. The number of microcalcification specks were recorded precisely when the speck number was less than or equal to 20; in cases where number of specks were more, the counting was approximated in group of tens (i.e., 21–30). Surgery was performed in all 353 patients. The final histopathologic diagnosis from the postoperative specimen was compared with the preoperative SVAB diagnosis. The study population was divided in two groups based on the presence (Group 1) or absence (Group 2) of invasion in the final histopathologic examination of the surgical specimens.
Statistical analysis
Statistical analyses were performed by SPSS version 13.0 (SPSS, Inc.). Data are presented as the mean and standard deviation or n (%). One-sample Kolmogorov-Smirnov test was used to evaluate the distribution of data. The differences between the subgroups were analyzed by chi-square or Fisher’s exact, and Mann-Whitney U tests. A P < 0.05 was considered significant.
The cutoff values for lesion sizes (30 mm and 40 mm) were obtained from previous publications (6, 16). In order to find the cutoff value for percent of microcalcification specks removed, we tested different percentages to determine a statistically significant cutoff value for the underestimation of invasion, and reached the minimum statistically significant percent at 40%.
Results
Of 353 patients with microcalcification-only lesions (mean age, 57.6±9.0 years), 209 (59%) were detected by screen ing mammography, and the remaining 144 (41%) were symptomatic. At final surgical pathology, 63 of 353 DCIS lesions (underestimation ratio, 18%) had an invasive component, which had been missed at the initial biopsy.
The median size of the cluster of microcalcification in the underestimated cases was 17 mm (2–125 mm) and the median size in accurately diagnosed cases was 15 mm (2–125 mm) (P = 0.150). However, the rate of underestimation increased with larger lesions and this was statistically significant for those lesions with a cluster of microcalcification equal to or greater than 40 mm in size (28% vs. 16%, P = 0.025). Indeed, among 292 patients in whom the microcalcification size was smaller than 40 mm, there was an upgrade to invasive disease in 46 cases (16%), whereas among 61 patients with larger lesions (≥ 40 mm), invasive carcinoma was found in 17 cases (28%) (Table 1). There was no statistically significant difference when the cutoff value was taken as 30 mm (P = 0.263). The rate of underestimation was significantly higher in lesions where less than 40% of microcalcification specks were removed during the biopsy (P = 0.030). In 13 of 44 cases (29.5%) where less than 40% of calcification was retrieved, the initial DCIS diagnosis was upgraded to invasion. However, among 309 cases where more than 40% of calcium specks were removed, an upgrade occurred only in 50 patients (16.2%) (Table 1).
Table 1.
Variables that were statistically significant in the comparison of accurately diagnosed and underestimated DCIS lesions at SVAB
| Variables | Accurately diagnosed (n=290) | Underestimated (n=63) | P |
|---|---|---|---|
| Size (mm) | 0.025 | ||
| <40 | 246 (84.2) | 46 (15.8) | |
| 0–20 | 188 | 35 | |
| 20–40 | 58 | 11 | |
| ≥40 | 44 (72.1) | 17 (27.9) | |
| 40–60 | 25 | 9 | |
| >60 | 19 | 8 | |
|
| |||
| Percentage of microcalcification removed | 0.030 | ||
| <40% | 259 (83.8) | 50 (16.2) | |
| ≥40% | 31 (70.5) | 13 (29.5) | |
|
| |||
| Presence of microinvasion | 0.004 | ||
| Absent | 281 (83.6) | 55 (16.4) | |
| Present | 9 (52.9) | 8 (47.1) | |
Data are presented as n or n (%).
The presence of microinvasion at initial biopsy was also highly significant (P = 0.001) in the underestimation of invasion. Of 63 underestimated DCIS cases, eight (13%) were reported to have microinvasion at SVAB (Fig.). In comparison, nine of 290 accurately diagnosed DCIS cases (3%) were reported to have microinvasion at SVAB. Of 17 cases where microinvasion was reported at SVAB specimen, histopathology after subsequent surgery revealed invasive carcinoma in eight (47%) (Table 1).
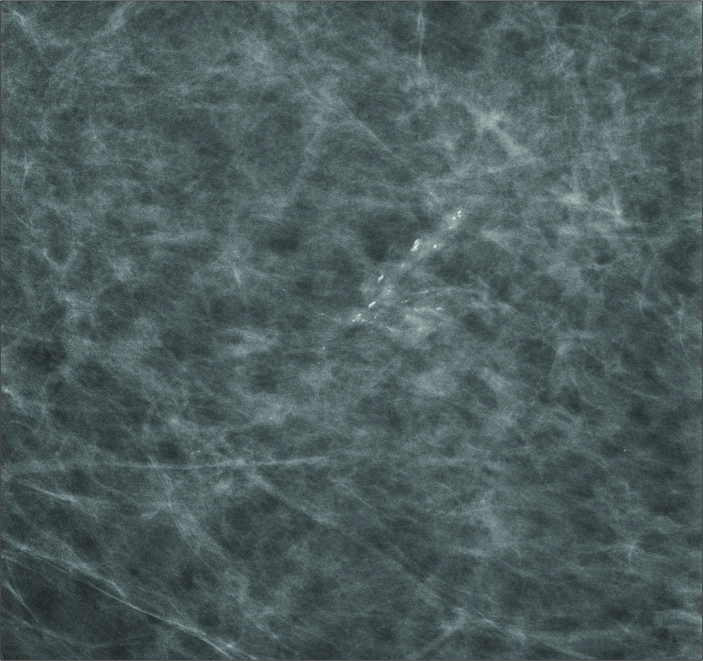
Figure.
A 61-year-old woman with breast cancer detected at routine mammography screening. Magnification view shows microcalcifications in the left breast. Case was reported to have DCIS with microinvasion at initial SVAB biopsy; histopathology after subsequent surgery revealed invasive carcinoma.
The median number of cores taken at biopsy in the underestimated cases was 12 (range, 5–40) and the median number in accurately diagnosed cases was 13 (range, 5–40). There was no statistically significant difference in the number of core specimens obtained between the two groups (Table 2).
Table 2.
Variables that were not statistically significant in the comparison of accurately diagnosed and underestimated DCIS lesions at SVAB
| Variables | Accurately diagnosed (n=290) n (%) |
Underestimated (n=63) n (%) |
P |
|---|---|---|---|
| Patient type | 0.224 | ||
| Screen | 176 (84.2) | 33 (15.8) | |
| Symptomatic | 114 (79.2) | 30 (20.8) | |
|
| |||
| Breast composition | 0.474 | ||
| Entirely fat | 44 (84.6) | 8 (15.4) | |
| Scattered density | 162 (80.6) | 39 (19.4) | |
| Heterogeneously dense | 75 (82.4) | 16 (17.6) | |
| Extremely dense | 9 (100) | 0 (0) | |
|
| |||
| Mammography code | 0.477 | ||
| M3 | 105 (84.7) | 19 (15.3) | |
| M4 | 133 (82.1) | 29 (17.9) | |
| M5 | 52 (77.6) | 15 (22.4) | |
|
| |||
| Number of specimen | 0.805 | ||
| <12 | 65 (80.2) | 16 (19.8) | |
| 12–23 | 214 (82.9) | 44 (17.1) | |
| ≥24 | 11 (78.6) | 3 (21.4) | |
|
| |||
| The nuclear grade of tumor | 0.719 | ||
| Low grade | 42 (85.7) | 7 (14.3) | |
| Intermediate grade | 99 (80.5) | 24 (19.5) | |
| High grade | 149 (82.3) | 32 (17.7) | |
|
| |||
| Presence of necrosis | 0.436 | ||
| Absent | 109 (80.1) | 27 (19.9) | |
| Present | 181 (83.4) | 36 (16.6) | |
M3, indeterminate/probably benign; M4, suspicious of malignancy; M5, highly suspicious of malignancy.
There was also no statistically significant difference for underestimation of invasion between screening and symptomatic patients, mammographic code, breast composition, the nuclear grade of tumor, and the presence or absence of necrosis (Table 2).
Discussion
In our series 17.8% of DCIS lesions diagnosed by SVAB were found to have invasion at subsequent surgery. Factors increasing the underestimation of invasion in DCIS lesions were lesions ≥40 mm on mammogram, the presence of microinvasion at initial biopsy, and cases where less than 40% of microcalcification specks were removed at biopsy.
In diagnosis of breast lesions, surgical excisional biopsy has now been replaced by automated core needle biopsy and vacuum-assisted biopsies. Microcalcification-only lesions without any accompanying mass are usually difficult to identify on sonographic examinations, and stereotactic biopsy in such cases is the method of choice. Because calcifications are specifically targeted during the stereotactic procedure, an invasive component —if present— may be missed, particularly if it is small or eccentrically located. Although removing a greater volume of tissue may improve concordance between core specimen and final histopathologic results, it is doubtful that this will entirely eliminate underestimation (12). Several published articles have shown a higher underestimation rate with the automated core-needle biopsy compared to SVAB (9–11). Sim et al. (17) reported that the underestimation rate of DCIS (26%) was significantly higher when preoperative biopsies were performed using core biopsy needles, compared with the lower underestimation rate of DCIS (19.9%) in biopsies obtained using VAB devices. Although SVAB allows more accurate histopathologic results, underestimation still occurs (7, 10, 18). Some investigators have found rates of underestimation ranging from 5% to 29% for DCIS at SVAB (6, 9, 11–13). In this study, the underestimation rate of DCIS was 18%.
Philpotts et al. (19) reported a trend for increased size among the underestimated cases, but this was not statistically significant. However Laurenco et al. (13) found a statistically significant relation between the increasing size and underestimation rates. Brem et al. (6) found the underestimation rates to be significantly higher in lesions 30 mm or larger. Orsaria et al. (16) reported that lesions larger than 40 mm have a greater probability of having invasive components than others. Van Nuys prognostic classification uses 40 mm as a cutoff value for a score of 3. In our series there was no statistically significant difference when the cutoff point was taken as 30 mm. However, a cutoff point of 40 mm appeared to be statistically significant.
It is predictable that the accuracy of biopsy increases for smaller lesions. SVAB enables retrieval of a large volume of tissue. It is not uncommon that all or nearly all of the targeted lesion is removed. Several studies have shown that underestimation is less frequent in such cases (19–22). Liberman et al. (23) showed a trend toward a lower incidence of DCIS underestimation in cases when the mammographic target had been completely excised using 11-gauge SVAB. To the best of our knowledge, there has been no study investigating the percentage of retrieved microcalcification required to decrease the underestimation rate, up to date. In our series the percentage of calcification specks retrieved was found to be statistically significant at a cutoff value of 40%.
In DCIS lesions microinvasion is described when an invasive component smaller than 2 mm is found (24). DCIS with microinvasion accounts for less than 1% of all breast cancers, and 13.5% of all DCIS lesions have been shown to have a microinvasive component (25). In our series, 17 of 353 cases (5%) demonstrated microinvasion. The rate of underestimation was statistically significant in these cases. Philpotts et al. (19) also showed, in a smaller series, a higher underestimation rate in cases with microinvasion.
Jackman et al. (8) reported that they tried to obtain at least 12 specimens per lesion upon vacuum biopsy. We could not find any significant correlation between the number of retrieved cores and correct diagnosis. To the best of our knowledge, there is no minimum number needed in the literature. We determined that obtaining at least 40% microcalcification specks decreases the underestimation rate on SVAB. In general, SVAB removes larger number of cores compared with automated core biopsy devices. It has been shown that the underestimation rate is lower with increased number of cores (9, 21). When more than 10 specimens per lesion are obtained, the underestimation rate of DCIS reduces significantly (9). On the other hand, Liberman et al. (20) showed that, for larger lesions, underestimation inevitably occurs even when more that 40 core specimens were retrieved. In our series the number of retrieved cores had no effect on the underestimation rates. In line with our results, other studies have also reported no statistically significant relationship between the mean number of core specimens obtained in the DCIS-only and the underestimated invasive groups (10, 12, 19, 26). In this study, there was no difference in the underestimation rates with increasing number of retrieved cores, i.e., <12, 12–23, and ≥24. It appeared that the number of cores containing calcification was more important in avoiding the upgrading than the total number of retrieved cores.
In our study the mammographic code, the grade of DCIS, or the presence of necrosis had no effect on underestimation rates. This was also consistent with the findings of Lee et al. (12). The BI-RADS scoring system is a more commonly used system than the UK RCRBG scoring system because many radiologists are not familiar with the RCRBG scoring system. Unlike the BI-RADS scoring system, the RCRBG scoring system does not specify the percent probability of each category (16). There are different philosophical acceptances of both scoring systems; for example, BI-RADS 3 and 4a lesions with low risk of malignancy undergo short-term follow-up in the United States but, if palpable, would be subject to biopsy in the UK (27).
There are some drawbacks and limitations to our study. The count of the number of microcalcification specks was done as accurately as possible and this had to be approximated for larger lesions. Also, the NHSBSP coding system (M1–M5) was used in this study, which is the accepted system in the United Kingdom. As the lesion coding was performed at the time of biopsy prospectively, we inclined to keep the codes as they were, instead of translating these into BI-RADS, although it is a more commonly used system. Another limitation is that, instead of performing ROC analyses, we used predetermined cutoff values in published manuscript or tested different values to find the most significant cutoff values.
In conclusion, we found that 18% of DCIS lesions diagnosed by SVAB had invasion at subsequent surgery. Since presence of invasion can change patient management in some situations, we should take into account factors increasing the rate of underestimation of invasion in DCIS lesions, such as lesions greater than or equal to 40 mm on mammography and the presence of microinvasion at initial biopsy. At least 40% of the microcalcification specks should be removed at biopsy in order to decrease the underestimation rate.
Main points.
The surgical management of DCIS and invasive tumors differs; hence, accurate preoperative diagnosis is important.
As much as 18% of the lesions diagnosed as DCIS preoperatively may be underestimated even when SVAB is used.
Lesions greater than or equal to 40 mm on mammogram and the presence of microinvasion at initial biopsy should be considered as possible factors for upgrading to invasive disease.
In order to decrease the underestimation rate, at least 40% of the microcalcification specks should be removed.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Yang WT, Tse GM. Sonographic, mammographic, and histopathologic correlation of symptomatic ductal carcinoma in situ. AJR Am J Roentgenol. 2004;182:101–110. doi: 10.2214/ajr.182.1.1820101. http://dx.doi.org/10.2214/ajr.182.1.1820101. [DOI] [PubMed] [Google Scholar]
- 2.Evans AJ, Pinder S, Ellis IO, et al. Screening-detected and symptomatic ductal carcinoma in situ: mammographic features with pathologic correlation. Radiology. 1994;191:237–240. doi: 10.1148/radiology.191.1.8134579. http://dx.doi.org/10.1148/radiology.191.1.8134579. [DOI] [PubMed] [Google Scholar]
- 3.Shin HJ, Kim HH, Kim SM, Kwon GY, Gong G, Cho OK. Screening-detected and symptomatic ductal carcinoma in situ: Differences in the sonographic and pathologic features. AJR Am J Roentgenol. 2008;190:516–525. doi: 10.2214/AJR.07.2206. http://dx.doi.org/10.2214/AJR.07.2206. [DOI] [PubMed] [Google Scholar]
- 4.Evans A, Pinder S, Wilson R, et al. Ductal carcinoma in situ of the breast: correlation between mammographic and pathologic findings. AJR Am J Roentgenol. 1994;162:1307–1311. doi: 10.2214/ajr.162.6.8191988. http://dx.doi.org/10.2214/ajr.162.6.8191988. [DOI] [PubMed] [Google Scholar]
- 5.Ikeda DM, Andersson I. Ductal carcinoma in situ: atypical mammographic appearances. Radiology. 1989;172:661–666. doi: 10.1148/radiology.172.3.2549563. http://dx.doi.org/10.1148/radiology.172.3.2549563. [DOI] [PubMed] [Google Scholar]
- 6.Brem RF, Schoonjans JM, Goodman SN, Nolten A, Askin FB, Gatewood OM. Nonpalpable breast cancer: percutaneous diagnosis with 11- and 8-gauge stereotactic vacuum-assisted biopsy devices. Radiology. 2001;219:793–796. doi: 10.1148/radiology.219.3.r01jn34793. http://dx.doi.org/10.1148/radiology.219.3.r01jn34793. [DOI] [PubMed] [Google Scholar]
- 7.Berg WA, Krebs TL, Campassi C, Magder LS, Sun CC. Evaluation of 14- and 11- gauge directional, vacuum-assisted biopsy probes and 14-gauge biopsy guns in a breast parenchymal model. Radiology. 1997;205:203–208. doi: 10.1148/radiology.205.1.9314986. http://dx.doi.org/10.1148/radiology.205.1.9314986. [DOI] [PubMed] [Google Scholar]
- 8.Jackman RJ, Rodriguez-Soto J. Breast microcalcifications: retrieval failure at prone stereotactic core and vacuum breast biopsy--frequency, causes, and outcome. Radiology. 2006;239:61–70. doi: 10.1148/radiol.2383041953. http://dx.doi.org/10.1148/radiol.2383041953. [DOI] [PubMed] [Google Scholar]
- 9.Jackman RJ, Burbank F, Parker SH, et al. Stereotactic breast biopsy of nonpalpable lesions: determinants of ductal carcinoma in situ underestimation rates. Radiology. 2001;218:497–502. doi: 10.1148/radiology.218.2.r01fe35497. http://dx.doi.org/10.1148/radiology.218.2.r01fe35497. [DOI] [PubMed] [Google Scholar]
- 10.Won B, Reynolds HE, Lazaridis CL, Jackson VP. Stereotactic biopsy of ductal carcinoma in situ of the breast using an 11-gauge vacuum-assisted device: persistent underestimation of disease. AJR Am J Roentgenol. 1999;173:227–229. doi: 10.2214/ajr.173.1.10397131. http://dx.doi.org/10.2214/ajr.173.1.10397131. [DOI] [PubMed] [Google Scholar]
- 11.Darling MLR, Smith DN, Lester SC, et al. Atypical ductal hyperplasia and ductal carcinoma in situ as revealed by large core needle breast biopsy: results of surgical excision. AJR Am J Roentgenol. 2000;175:1341–1346. doi: 10.2214/ajr.175.5.1751341. http://dx.doi.org/10.2214/ajr.175.5.1751341. [DOI] [PubMed] [Google Scholar]
- 12.Lee CH, Carter D, Philpotts LE, et al. Ductal carcinoma in situ diagnosed with stereotactic core needle biopsy: can invasion be predicted? Radiology. 2000;217:466–470. doi: 10.1148/radiology.217.2.r00nv08466. http://dx.doi.org/10.1148/radiology.217.2.r00nv08466. [DOI] [PubMed] [Google Scholar]
- 13.Lourenco AP, Mainiero MB, Lazarus E, Giri D, Schepps B. Stereotactic breast biopsy: comparison of histologic underestimation rates with 11- and 9-gauge vacuum-assisted breast biopsy. AJR Am J Roentgenol. 2007;189:275–279. doi: 10.2214/AJR.07.2165. http://dx.doi.org/10.2214/AJR.07.2165. [DOI] [PubMed] [Google Scholar]
- 14.Pathology reporting of breast disease. NHSBSP; 2001. NHS Cancer Screening Programmes and the Royal College of Pathologists. Publication no 50. [Google Scholar]
- 15.Taylor K, Britton P, O’Keeffe S, Wallis MG. Quantification of the UK 5-point breast imaging classification and mapping to BI-RADS to facilitate comparison with international literature. Br J Radiol. 2011;84:1005–1010. doi: 10.1259/bjr/48490964. http://dx.doi.org/10.1259/bjr/48490964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Orsaria P, Granai AV, Venditti D, Petrella G, Buonomo O. Investigational paradigms in downscoring and upscoring DCIS: surgical management review. Int J Surg Oncol. 2012;2012:560493. doi: 10.1155/2012/560493. http://dx.doi.org/10.1016/j.crad.2014.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sim YT, Litherland J, Lindsay E, et al. Upgrade of ductal carcinoma in situ on core biopsies to invasive disease at final surgery: a retrospective review across the Scottish Breast Screening Programme. Clin Radiol. 2015;70:502–506. doi: 10.1016/j.crad.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 18.Jackman RJ, Nowels KW, Rodriguez-Soto J, Marzoni FA, Finkelstein SI, Shepard MJ. Stereotactic, automated, large-core needle biopsy of nonpalpable breast lesions: false-negative and histologic underestimation rates after long-term follow-up. Radiology. 1999;210:799–805. doi: 10.1148/radiology.210.3.r99mr19799. http://dx.doi.org/10.1148/radiology.210.3.r99mr19799. [DOI] [PubMed] [Google Scholar]
- 19.Philpotts LE, Lee CH, Horvath LJ, Lange RC, Carter D, Tocino I. Underestimation of breast cancer with 11-gauge vacuum suction biopsy. AJR Am J Roentgenol. 2000;175:1047–1050. doi: 10.2214/ajr.175.4.1751047. http://dx.doi.org/10.2214/ajr.175.4.1751047. [DOI] [PubMed] [Google Scholar]
- 20.Liberman L, Smolkin JH, Dershaw DD, Morris EA, Abramson AF, Rosen PP. Calcification retrieval at stereotactic 11-G directional vacuum-assisted breast biopsy. Radiology. 1998;208:251–260. doi: 10.1148/radiology.208.1.9646821. http://dx.doi.org/10.1148/radiology.208.1.9646821. [DOI] [PubMed] [Google Scholar]
- 21.Lomoschitz FM, Helbich TH, Rudas M, et al. Stereotactic 11-gauge vacuum-assisted breast biopsy: influence of number of specimens on diagnostic accuracy. Radiology. 2004;232:897–903. doi: 10.1148/radiol.2323031224. http://dx.doi.org/10.1148/radiol.2323031224. [DOI] [PubMed] [Google Scholar]
- 22.Liberman L, Dershaw DD, Rosen PP, Morris EA, Abramson AF, Borgen PI. Percutaneous removal of malignant mammographic lesions at stereotactic vacuum-assisted biopsy. Radiology. 1998;206:711–715. doi: 10.1148/radiology.206.3.9494489. http://dx.doi.org/10.1148/radiology.206.3.9494489. [DOI] [PubMed] [Google Scholar]
- 23.Liberman L, Kaplan JB, Morris EA, Abramson AF, Menell JH, Dershaw DD. To excise or to sample the mammographic target: what is the goal of stereotactic 11-gauge vacuum-assisted breast biopsy? AJR Am J Roentgenol. 2002;179:679–683. doi: 10.2214/ajr.179.3.1790679. http://dx.doi.org/10.2214/ajr.179.3.1790679. [DOI] [PubMed] [Google Scholar]
- 24.Silver SA, Tavassoli FA. Mammary ductal carcinoma in situ with microinvasion. Cancer. 1998;82:2382–2390. doi: 10.1002/(sici)1097-0142(19980615)82:12<2382::aid-cncr12>3.0.co;2-l. http://dx.doi.org/10.1002/(SICI)1097-0142(19980615)82:12<2382::AID-CNCR12>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 25.Silverstein MJ, Waisman JR, Gamagani P, et al. Intraductal carcinoma of the breast (208 cases). Clinical factors influencing treatment of choice. Cancer. 1990;66:102–108. doi: 10.1002/1097-0142(19900701)66:1<102::aid-cncr2820660119>3.0.co;2-5. http://dx.doi.org/10.1002/1097-0142(19900701)66:1<102::AID-CNCR2820660119>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 26.Houssami N, Ciatto S, Ellis I, Ambrogetti D. Underestimation of malignancy of breast core-needle biopsy: concepts and precise overall and category-specific estimates. Cancer. 2007;109:487–495. doi: 10.1002/cncr.22435. http://dx.doi.org/10.1002/cncr.22435. [DOI] [PubMed] [Google Scholar]
- 27.Wilkinson LS, Ridley NT. The practical application of the UK 5-point scoring system for breast imaging: how standardisation of reporting supports the multidisciplinary team. Br J Radiol. 2011;84:965–966. doi: 10.1259/bjr/51580547. http://dx.doi.org/10.1259/bjr/51580547. [DOI] [PMC free article] [PubMed] [Google Scholar]