Abstract
Drawing on cross-sectional data collected in three Kansas City jails, our objective was to describe the social, neighborhood-based context of sexual health risk prior to incarceration for 290 women. Half of the participants were clustered in Kansas City's urban core before their incarceration. Women who lived in these neighborhoods, which had the highest density of our incarcerated participants, were three times as likely to report a history of trading sex for money, drugs, or life necessities, compared to women who lived elsewhere in the city. Living in a neighborhood that was perceived to have low social capital was also associated with sexually transmitted infection history. Gaining an understanding of these social influences in women's lives—particularly at the neighborhood level—provides key insights that will allow future interventions to change the health outcomes of women who move between disadvantaged communities and local jails.
Keywords: sexual health, jail, incarcerated women, neighborhood disadvantage
Introduction
Each year, about 12 million people pass through jails in the United States – one-tenth of whom are women.1 The ‘war on drugs’ policies, in particular, have led to a 600% increase in the number of women who have passed through the justice system over the last twenty-five years and a disproportionate criminalization of women of color.2,3 Black women make up half the population of women in U.S. prisons and are seven times as likely to have been incarcerated than White women.4,5 Eighty-five percent of women in jail are incarcerated for non-violent offenses.6 These offenses—often tied to their histories of abuse, addiction, and poverty—include drug possession and property crimes, which account for between 60-80% of women's charges.7,8 Seventy percent of incarcerated women leave children under the age of 18 behind, for whom they are often the primary caregivers. Prior to incarceration, 30% have children under age five living with them.9,10
Sexual health risk, in particular, is high for women with ongoing criminal justice involvement. Up to 83% of incarcerated women have unintended pregnancy histories, and both birth control and condom use are inconsistent.11 Up to 50% of women in jails and prisons have had an STI or history of trading sex for money or drugs.11 Sexual health risk is exacerbated by patterns of violence and abuse, drug use, and mental health problems, all of which are present in as many as 60-90% of women in correctional facilities.12,13,14 In one study, 67% of women in a county jail reported a history of sexual abuse, and 79% reported a history of physical abuse.12 Another study found 63.6% of women in a Chicago jail to have a lifetime prevalence of drug abuse/dependence—and on top of that, 33.5% were dealing with post-traumatic stress disorder.14 Other studies have found close to half of women in jails reporting depression or anxiety in the year before their incarceration, or throughout their lifetimes.8,10
Though we know much about the individual-level correlates of sexual health risk, little is known about how the community context prior to incarceration affects women's health. Because of women's short-term stays and rapid turnover in jails—typically in close proximity to their daily lives, and therefore their sexual partners—women's communities, both pre- and post-incarceration, may have a strong influence on their sexual health risk. The objective of this study was to describe the social, neighborhood-based context of sexual health risk prior to incarceration for a sample of urban, Midwestern women in local jails.
These women overwhelmingly come from urban communities, where they experience high rates of poverty, low rates of health insurance, and inadequate health and social service infrastructures.15 Following release from jail, women return to these communities to navigate a series of daunting challenges—personal relationships put on hold, limited resources, and complex community networks that are constantly changing—while confronting multiple, competing needs to generate income, find housing, and reunify with families and partners.8,16,17 Housing opportunities that were in place in the three, six, or nine months before release often no longer exist. Women must collect their children from relatives or the foster care system and enroll them in new schools. But perhaps most urgent is the need to address children's emotional responses to the abrupt departure and reappearance of their mother.
Importantly, the communities to which women come from and return to after release are already disadvantaged, characterized by high rates of violence, to which women are particularly susceptible.18 While the association between poverty and violence has been generally acknowledged, the impact on health at the community level has been minimally studied.19 In addition to violence, these communities have been weakened by the reality of having many members cycling in and out of jails and prisons, thus reducing individual and community levels of social capital (that is, social continuity that builds networks and reciprocity). Taxman refers to this reality as “churning,” or the process of incarcerating, releasing, and re-incarcerating large numbers of individuals in any community.20 This process undermines positive social norms, facilitates disorganization, disrupts family and social networks, and contributes to reduced social cohesion. Neighborhoods that experience high rates of churning disproportionately suffer the burden and unintended consequences of incarceration.21
This burden of community incarceration may also be related to sexual health in particular, though few studies have actually explored this. For example, Thomas & Torrone found that in North Carolina, community-wide rates of sexually transmitted infections (STIs) and teen pregnancies strongly correlated with increasing incarceration rates.22 Similarly, using publicly available data, Johnson and Raphael suggested that the high incarceration rates of Black males are a significant cause of racial/ethnic disparities in HIV infection rates among non-incarcerated Black men and women.23 But a gap in the literature is how this neighborhood context—including the burden of community incarceration—affects the most vulnerable women, who actually experience criminal justice involvement firsthand.
In this study, we focused on the interplay between women's personal health histories and the context of the communities in which they lived immediately before their incarceration. Specifically, we wanted to understand how social, neighborhood-based context explains health outcomes among women with criminal justice involvement. Previous research hasn't fully fleshed out the relationship between incarcerated women's perception of their social environment and how that environment is related to health. Women's perceptions of their communities are important, since we hypothesize that fears and insecurities at the community level reflect the reality of disadvantage, serving as barriers to preventive health care that can minimize risk. This hypothesis is based on the theoretical foundations of the social determinants of health,24 which suggest that social- and community-level variables are the base cause of the majority of health conditions. Using an urban Midwestern area as a lab for sexual health risk, we examined the research question: “To what extent do neighborhood violence, social capital, trust, and incarceration density contribute to the sexual health of women incarcerated in local jails?” Understanding social, neighborhood-level influences in these vulnerable women's lives can provide a focus for future interventions and change these outcomes.
Methods
Design, Sample, and Procedures
Over a six-month study period in 2010, we conducted a cross-sectional survey of health needs and service usage with a convenience sample of 290 women in three urban jails in the greater Kansas City metropolitan area (one facility on the Missouri side of the state line, and two on the Kansas side).25 Kansas City provided an interesting “lab,” given its location across two state lines and two million people living in an 8,000 square mile region. This metropolitan area is home to one of the wealthiest counties in the state of Kansas, as well as one of the poorest (Johnson and Wyandotte Counties). In addition to this economic inequality, the urban core of Jackson County, Missouri is also known for its school district woes, as well as its racial/ethnic segregation. As is common within similar jurisdictions in other states, people in the local justice system of Kansas City tend to come from the poorest neighborhoods,14 making this an ideal location for studying the relationship between community disadvantage and health risks among this unique population of women incarcerated in short-term correctional facilities.
On any given day, about 1,900 men and women in total were housed in the three facilities where we conducted the research. Over 90% of these men and women resided in local communities prior to incarceration, and about 10% of the average daily population was female. We estimate that we interviewed approximately half of all women housed in the facilities, given the study period, average daily population, and turnover at the jails. Participants were recruited with flyers posted at the three jails and through word of mouth in each housing unit by the special programs coordinators. All women in the facilities were eligible and invited to participate, although only those who volunteered were included as potential participants. Reasons for the women not wanting to participate are unknown. Recruitment of this convenience sample occurred on an ongoing basis over the six-month data collection period and depended on the number of willing participants (for example, those not making court appearances). Our sample was similar to the overall population of women at the three jails in terms of age, race, and ethnic characteristics.
Interviewers read a standardized recruitment script and consent form to each potential participant, a consent form that was approved jointly by the authors’ university institutional review boards. We also assessed general cognitive impairment at this time by observing the interactions between potential participants and the researcher. No participants were turned away for this reason. After signing a consent form and having any questions answered, the women were administered a face-to-face survey by the interviewer. All interviews were conducted in semi-private spaces at the jail. Each participant was given a $5 credit to her commissary account or gift basket with hygiene products as compensation for participation.
Variables
For this study, we used three primary outcome measures for sexual health: 1) History of unintended pregnancy, which was assessed with the question, “Did you ever have a pregnancy that was unplanned, unintended, or a surprise?” 2) Lifetime history of STIs, which was assessed by asking participants if a doctor had ever told them that they had HIV/AIDS, syphilis, gonorrhea, or chlamydia. 3) History of trading sex, which was assessed by the question, “Have you ever exchanged sex for money, drugs, or life necessities?”
Based on the conceptual framework of Brunner and Marmot,24 we used three constructs to measure community disadvantage: Neighborhood violence, perception of neighborhood social capital and trust, and neighborhood incarceration density. We used three proxy measures of neighborhood violence: Fear of one's neighborhood was assessed with the question, “In the neighborhood where you lived before being incarcerated, were you afraid you would be hurt by violence?” There were four possible responses: None of the time, a little bit of the time, most of the time, all of the time.26 Level of neighborhood violence in the six months prior to incarceration was assessed by asking if participants had heard about a fight in which a weapon was used, a violent argument between neighbors or friends, a gang fight, a robbery or mugging, or a murder, with possible yes/no responses for each item.26,27 We computed a summary score of all types of violence, with higher scores indicating a greater level of neighborhood violence. Victimization by neighborhood violence was assessed with the question, “In the neighborhood where you lived before being incarcerated, did anyone ever use violence, such as a fight (hitting, pushing, and shoving), against you or any member of your family?”26 Though perception of violence and victimization by neighborhood violence may be related, we wanted to understand the differing contributions of perception and experience.
To understand participants’ perception of neighborhood social capital and trust, we used two measures. First, a ten-item social capital measure asked participants about their level of trust in neighbors, the feeling that neighbors would help them, that the neighborhood had prospered, and an overall assessment of neighborhood safety. Items included, “Most people in my neighborhood are basically honest and can be trusted,” or “Most people in my neighborhood are willing to help if you need it”.28 Responses were on a four-point Likert scale of strongly disagree, disagree, agree, or strongly agree. A mean scale score was computed for these 10 questions, with higher scores indicating greater social capital within a neighborhood (Cronbach's alpha = 0.86). Trust in institutions was measured by asking how much confidence participants had in the legal system, the police, and the government, with possible responses on a four-point Likert scale of no confidence at all, not very much, quite a lot, or a great deal.28,29 A mean scale score was computed for these three questions with higher scores indicating greater trust in institutions (Cronbach's alpha = 0.85).
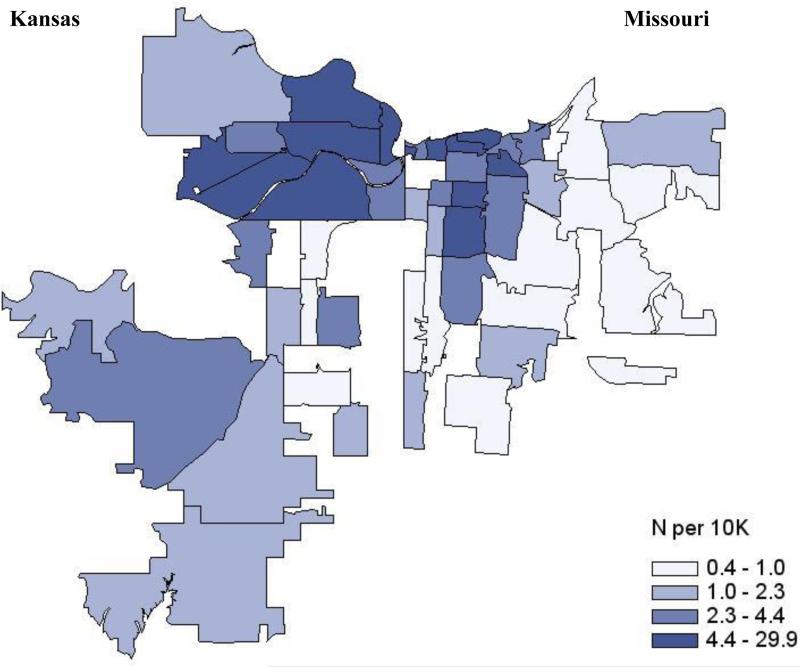
To calculate neighborhood incarceration density, we collected zip codes to generate a map of where participants lived immediately prior to their incarceration. Though not a precise measure of residential location, we felt this was the most sensitive measure available, given the need to protect the confidentiality of incarcerated participants. We then split the sample according to the Figure 1 map: Those women in the highest incarceration areas represented by the darkest blue were in one group (N=135, 48.2%), and those in all other areas were assigned to the other group (N=145, 51.8%) for comparison.
Figure 1. Density of Female Incarcerated Participants per Population, Kansas City Metropolitan Area, N=290.
Shaded areas represent the frequency of our participants’ zip codes per 10,000 residents. For example, the darkest shaded areas indicate that for every 10,000 people in that zip, at least 4.4 women were surveyed by us, but we could have surveyed anywhere between 4.4 – 29.9.
We also included variables—demographic, behavioral, and personal background variables known to be associated with both women's criminal justice experience and their sexual health risk as possible analytic covariates. Demographic items included age, race/ethnicity, and education level.10,30,31 Women's criminal justice history was assessed with three measures: How many times women had been arrested, how many months they had spent in prison or jail during their lifetime, and how many days they were incarcerated in the past year.
Mental health was assessed by asking participants if they were ever told by a clinician that they had depression, anxiety, schizophrenia, or bipolar disease. The drug dependence assessment was based on DSM IV criteria. For example, participants were asked six questions about drug use in the year before incarceration. This included questions such as, “Did you need to use more drugs to get the same high as when you first started using?” If participants answered “yes” to three out of six criteria, they were classified as “drug-dependent” (Cronbach's alpha=0.89).32 Abuse history before age 16 was measured by documenting frequency of sexual abuse before age 16 with the following question: “Did anyone ever do any of the following things when you didn't want them to: Touch the private parts of your body, make you touch their private parts, threaten or try to have sex with you, or sexually force themselves on you? Did it happen 0 times, 1-2 times, 3-5, 6-10, or more than ten times?”33 To assess physical abuse before age 16, we asked participants to answer three questions about how often they had been hit, pushed or shoved, or kicked or punched (Cronbach's alpha = 0.82 for sexual abuse and physical abuse questions).33 Because frequency varied across physical and sexual abuse questions, we coded abuse as answering “yes” one or more times to any of these questions. We assessed intimate partner violence in the year prior to incarceration by asking participants if a sex partner had physically hurt, insulted, or screamed at the participant on a regular basis or fairly often.34 Because we condensed all types of intimate partner violence into one question and treated this as a dichotomous variable, the psychometric properties of this question are unknown.
Analyses
Using SAS version 9.2, we mapped participants’ zip codes prior to incarceration. For all other variables, we computed group sizes and percentages, or means and standard deviations, using SPSS version 18. We first conducted a series of bivariate tests to assess the relationship between independent and dependent variables, where selection of variables was guided by our conceptual framework (that is, studying the social determinants of health with a particular focus on the social, neighborhood-based context of sexual health risk). To assess the relationship between key independent variables (neighborhood-level violence, social capital and trust, and incarceration density) and our selected sexual health outcomes, we ran logistic regression models, also using SPSS. We computed odds ratios (the exponentiated β coefficients) and confidence intervals to assess statistical significance of the models.35
Results
The mean age of the 290 women in our study was 33.9 (SD=9.8). Most of the women were White (43.0%) or Black (40.6%), reflecting the makeup of jails in Kansas City. Two-thirds of our sample (70.1%) had graduated from high school or received a GED, 62% had a lifetime history of mental health problem diagnosis, and over half (55.2%) were drug dependent in the year before incarceration. Many (64.5%) participants reported a history of physical or sexual abuse before age 16. Nearly half (46.4) of the women had experienced intimate partner violence in the year prior to incarceration. These results are shown in Table 1.
Table 1.
Characteristics of Women in Kansas City Jails, N=290
| N | % | |
|---|---|---|
| Age, mean (sd) | 33.93 | (9.76) |
| Race/Ethnicity | ||
| Black | 116 | 40.6 |
| White | 123 | 43.0 |
| Latino | 24 | 8.4 |
| Bi-racial | 9 | 3.1 |
| Other | 14 | 4.9 |
| Graduated from high school/GED | 202 | 70.1 |
| Lifetime history of mental health problem diagnosis | 178 | 62.0 |
| Drug dependence in year before incarceration | 128 | 55.2 |
| History of physical or sexual abuse before age 16 | 187 | 64.5 |
| Intimate partner violence in year before incarceration | 127 | 46.4 |
| History of unintended pregnancy | 155 | 53.8 |
| Lifetime history of STDs | 58 | 20.4 |
| Has ever exchanged sex for drugs or money | 68 | 24.5 |
| Afraid of being hurt by violence in neighborhood, mean (sd)1 | 1.49 | (0.90) |
| Level of neighborhood violence, mean (sd)2 | 1.24 | (1.55) |
| Victim or family member a victim of neighborhood violence | 61 | 21.7 |
| Perceived neighborhood social capital, mean (sd)3 | 2.54 | (0.50) |
| Level of trust in institutions, mean (sd)4 | 2.09 | (0.81) |
| Months lived in neighborhood prior to incarceration, mean (sd) | 71.89 | (108.20) |
| Number of days in jail in past year, mean (sd) | 82.98 | (96.56) |
| Lifetime number of arrests, mean (sd) | 7.51 | (7.71) |
| Lifetime months in jail or prison, mean (sd) | 17.90 | (31.31) |
“In the neighborhood where you lived before being incarcerated, were you afraid you would be hurt by violence?” 1=None of the time, 2=A little bit of the time, 3=Most of the time, 4=All of the time
Level of neighborhood violence in past six months, high summary score = greater perceived neighborhood violence
High scale score, on scale of 1 to 4 = greater neighborhood social capital
High scale score, on scale of 1 to 4 = greater trust in institutions
As for sexual health risk, 53.8% of the women reported a lifetime history of unintended pregnancy; 20.4% reported a lifetime history of STIs; and 24.5% reported ever having traded sex for money, drugs, or life necessities.
Half of female participants were clustered in Kansas City's urban core, in 13 of the most disadvantaged zip codes on either side of the state line. This cluster is represented by the darkest blue shading in Figure 1. These neighborhoods are characterized by high rates of poverty, racial/ethnic segregation, violence, and crime.36 One of the zip codes in this cluster was infamously dubbed ‘Murder Factory’ by a local journalist, spurring a series of articles profiling the social life and tragedies in this Kansas City neighborhood.37
Participants’ perceptions of community disadvantage mirrored the neighborhoods’ reputations. Women who lived in neighborhoods with the highest rates of incarceration for our participants feared violence more than participants who lived in other areas (fear of violence score of 1.59 vs. 1.34 on a scale 1 to 4, p<0.05). These women also had lower social capital scores (2.45 vs. 2.63 on a scale of 1 to 4, p<0.01).
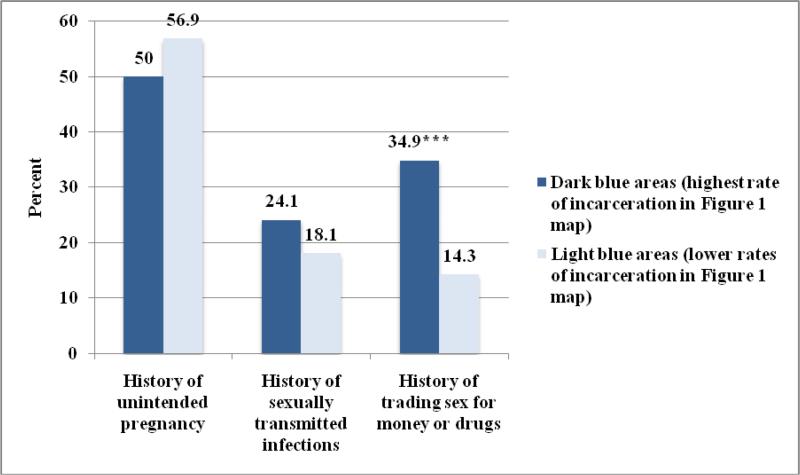
When exploring the differences in sexual health outcomes between women who lived in this cluster of neighborhoods (48.2% of the sample) versus those living elsewhere (51.8%), more women in the disadvantaged neighborhoods had a history of trading sex for money, drugs, or life necessities (34.9% vs. 14.3%, p<0.001) (Figure 2). When exploring the relationship between sexual health and neighborhoods where both men and women lived prior to incarceration (data not shown in Figure), we also found a statistically significant difference in STI histories for those women living in high incarceration areas (24.7% with history of STIs) compared to low incarceration areas (15.0%, p<0.05). People living in neighborhoods with high rates of incarceration also reported higher rates of trading sex in exchange for money, drugs, or life necessities (32.0% vs. 15.3%, p<0.001).
Figure 2. Frequency of Women's Sexual Health Outcomes by Neighborhood Incarceration Density, N=290.
We split the sample according to the Figure 1 map: those women in the highest incarceration areas represented by the darkest blue were in one group (N=135, 48.2%), and those in all other areas were assigned to the other group (N=145, 51.8%) for comparison.
*p≤0.05, **p≤0.01, ***p≤0.001
The relationship between perception and experience of neighborhood-level violence, social capital and trust, incarceration density, and selected sexual health outcomes is shown in Table 2, where both unadjusted and adjusted odds ratios are presented. After adjusting for lifetime history of mental health diagnosis, history of physical or sexual abuse before age 16, and intimate partner violence in the year prior to incarceration (associated with history of STIs, p<0.05), only perceived neighborhood social capital was inversely and independently associated with history of STIs (B = −0.74, OR = 0.48, Wald χ2 = 5.06, d.f. = 1, p = 0.024). Living in neighborhoods with the highest density of our incarcerated participants was positively associated with a history of trading sex (B = 1.18, OR = 3.25, Wald χ2 = 7.47, d.f. = 1, p = 0.006) after controlling for other factors independently associated with the dependent variable, p<0.05: Age, race, drug dependence in the year prior to incarceration, history of physical or sexual abuse before age 16, intimate partner violence in the year prior to incarceration, and lifetime number of months spent in jail or prison.
Table 2.
Neighborhood Correlates of Women's Lifetime Sexual Health Risk, N=290
| History of unintended pregnancy | History of sexually transmitted infections | History of trading sex for money or drugs | ||||
|---|---|---|---|---|---|---|
| OR1 (95% CI) | AOR2 (95% CI) | OR (95% CI) | AOR3 (95% CI) | OR (95% CI) | AOR4,5 (95% CI) | |
| Level of neighborhood violence6 | 1.00 (0.86, 1.17) | 0.97 (0.81, 1.14) | 1.27* (1.06, 1.52) | 1.11 (0.92, 1.36) | 1.37** (1.14, 1.66) | 1.04 (0.82, 1.31) |
| Victim of neighborhood violence | 1.91* (1.04, 3.51) | 1.67 (0.87, 3.20) | 2.41** (1.23, 4.70) | 1.50 (0.74, 3.06) | 1.97* (1.01, 3.84) | 1.01 (0.43, 2.36) |
| Perceived neighborhood social capital | 0.85 (0.53, 1.37) | 0.95 (0.58, 1.55) | 0.37** (0.20, 0.69) | 0.48* (0.25, 0.91) | 0.77 (0.43, 1.41) | 1.26 (0.58, 2.70) |
| Level of trust in institutions | 0.92 (0.68, 1.26) | 0.96 (0.70, 1.31) | 0.70 (0.46, 1.06) | 0.74 (0.48, 1.14) | 1.15 (0.79, 1.68) | 1.23 (0.76, 1.99) |
| Neighborhood incarceration density | 0.70 (0.43, 1.14) | 0.78 (0.46, 1.30) | 1.35 (0.75, 2.45) | 1.62 (0.85, 3.07) | 3.88*** (1.98, 7.63) | 3.25** (1.40, 7.57) |
Unadjusted odds ratios (OR) and adjusted odds ratios (AOR) are presented with 95% confidence intervals above.
Adjusted models for history of unintended pregnancy included the following variables as covariates, based on their association with the dependent variable at the p≤0.05 level in bivariate analysis: White race, lifetime history of mental health problem diagnosis, and intimate partner violence in the year prior to incarceration.
Adjusted models for history of sexually transmitted infections included the following covariates: lifetime history of mental health problem diagnosis, history of physical or sexual abuse before age 16, and intimate partner violence in the year prior to incarceration.
Adjusted models for history of trading sex for money or drugs included the following covariates: age, White race, drug dependence in the year prior to incarceration, history of physical or sexual abuse before age 16, intimate partner violence in the year prior to incarceration, and lifetime number of months spent in jail or prison.
We constructed a correlation matrix to test for multicolinearity among variables of interest prior to running each of the regression models. Any statistically significant correlations between independent variables and covariates were weak with a Pearson's Correlation < 0.3.
We did not include the “fear” of violence variable in the regression analysis since it was correlated with the level of neighborhood violence scale, had similar magnitude of association with dependent variables as the level of neighborhood violence scale, and was less robust than the neighborhood violence scale, since it was a single item measure.
p≤0.05
p≤0.01
p≤0.001
Discussion
Our results suggest that while community disadvantage is an important factor affecting the health of incarcerated women, it's more likely the additive effect of both individual and neighborhood disadvantages that leads to negative health outcomes. Like many others, our study showed high levels of disadvantage for incarcerated women: The concentration of racial/ethnic minorities in jail, high levels of mental health problems, drug dependence, and childhood and intimate partner abuse histories.5,12,13,14 These factors were coupled with the burden of unintended pregnancy, STIs, and the trading of sex for money, drugs, or life necessities. Our contribution here was to demonstrate how neighborhood-level disadvantages, measured primarily through the women's perception of social capital and their neighborhood's actual incarceration burden, were associated with health outcomes.
In the general population, perceptions of a neighborhood's condition—measured through the use of a “broken windows” index and other indicators of social cohesion—have been associated with STI rates.38,39 Indeed, the conceptual orientation of this study was to understand how social- and community-level variables are related to health conditions.24 For example we found that women's perceptions of low social capital in a neighborhood were associated with their STI histories. It's hard to know what this means for women on the ground. Do they feel less comfortable seeking health care? Are there other, more pressing STI risks in disadvantaged communities? Fleshing out these issues qualitatively might help inform the types of neighborhood and individual interventions needed to address STI risk. We also don't fully understand to what extent the intersection of neighborhood disadvantage and incarceration history plays a role in the women's sexual health risk. Certainly, jails and prisons house a disproportionate number of sex workers and drug users—those women at greatest risk of STI transmission. But this study sought to understand in a very exploratory manner, whether neighborhood incarceration density also played a role in sexual health risk.
Other researchers have also found that for the general population, as incarceration rates go up among a neighborhood's residents, so does sexual health vulnerability.22,23 These researchers and others have thoughtfully outlined the relationship between the burden of incarceration on communities and the rupturing of social fabric—breakdown in family, community, economy, and political processes.21 This burden of incarceration on communities has broader health outcomes for its members, whether incarcerated or not.21,40 We used a slightly different methodological approach in this exploratory study and examined the effect of neighborhood incarceration density based on where our own participants lived. Using zip code-based maps, we found that the neighborhoods with the highest density of our incarcerated participants were located in the urban core of Kansas City, where there are high rates of violence and crime. The women living in these areas had greater fear of neighborhood violence and lower perception of neighborhood social capital. These women were also significantly more likely to have exchanged sex for money, drugs, or life necessities, signifying the intersection of violence, crime, and sexual health risk at the individual and community levels.41 Ultimately, we attempted to demonstrate that the most vulnerable members of a community are often concentrated in disadvantaged communities to begin with, reducing the chance that they'll avoid health risks and experience long-term success.
Our study had several limitations, one of which was the problem of measurement. We chose to focus on the STIs most routinely screened for in samples of incarcerated men and women.42,43,44 But this means our study didn't include information on other important viral infectious diseases, such as hepatitis C. In this exploratory study, where data collection was ultimately part of a local needs assessment,25 we also failed to include robust, standardized measures of mental health status and intimate partner violence. Larger studies, in which these variables serve as key outcomes, would include more nuanced measures of these domains. Other limitations of this study include its cross-sectional design, our selection of a relatively small convenience sample, and the lack of citywide data included in the comparison. Although we have acknowledged these limitations elsewhere, we note that our study is one of the first to collect individual-level data about perceptions of neighborhood disadvantage among an incarcerated sample.25 The future direction of this research would be to simultaneously analyze the contribution of individual experiences—including criminal justice history and perception of disadvantages—and actual community-wide disadvantage in relation to health outcomes. Doing so would make for a robust empirical analysis of the impact of incarceration on public health. Studying the complex intersection of individual and social forces holds significant implications for intervention in jails, upon release for women, and at the broader community level.
Conclusions
What our work points to is the need for interventions that simultaneously address the health needs of incarcerated women and their broader experiences of disadvantage in their communities. Local experience with reentry services could be more effective if located directly in the communities that suffer the greatest incarceration burden. Services would ideally include a specific health care access component, perhaps using a patient navigator model45 that helps women deal with the neighborhood conditions that might serve as barriers to seeking health care or preventive care. The second focus of effective interventions would be to get to the root of violence and powerlessness in vulnerable women's lives. This is based both on the findings of the current study, in which women had long trauma histories, and those of other researchers, including Zaitrow and Thomas,46 Bloom, Owen and Covington, 7 and Chesney-Lind.47 Such interventions borrow from feminist models of substance abuse, acknowledge past and current trauma and abuse, focus on physical and social power imbalances in women's health care, and take into account women's personal and social resources. 48,49,50 Ideally, these interventions would focus on developing women's abilities to organize their lives and successfully engage within their social networks and communities.
Though we propose two important components of intervention, specifically targeted at women who move between local jails and disadvantaged communities, many others could focus on organizing at the community level51 and implementing broader efforts to improve the economic, political, and health care infrastructure in the most disadvantaged communities.
Contributor Information
Megha Ramaswamy, Preventive Medicine and Public Health, University of Kansas School of Medicine.
Patricia J. Kelly, School of Nursing, University of Missouri-Kansas City, kellypj@umkc.edu, Fax 816-235-1701.
References
- 1.Minton TD. Jail inmates at midyear 2010: Statistical tables. Bureau of Justice Statistics. 2011 Available at: http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&iid=2375.
- 2.Mauer M. Race to Incarcerate. The New Press; New York: 2006. [Google Scholar]
- 3.Solovitch S. Women are silent casualties of war on drugs. North County Times; Dec 24, 2006. [Google Scholar]
- 4.Amnesty International Women in prison: A fact sheet. In “Not Part of My Sentence: Violations of the Human Rights Of Women in Custody.”. 1999 Available at: http://www.prisonpolicy.org/scans/women_prison.pdf.
- 5.Freudenberg N. Adverse effects of US jail and prison policies on the health and well-being of women of color. Am J Public Health. 2002;92(12):1895–1899. doi: 10.2105/ajph.92.12.1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harlow CW. Profile of Jail Inmates, 1996. Bureau of Justice Statistics. 1998 Available at: http://bjs.ojp.usdoj.gov/content/pub/pdf/pji96.pdf.
- 7.Bloom B, Owen B, Covington S. Gender-responsive strategies for women offenders. US Department of Justice. National Institute of Corrections; 2005. Available at: http://www.idoc.idaho.gov/sites/default/files/webfm/documents/education_and_treatment/program_services/Gender%20responsivity.pdf. [Google Scholar]
- 8.Freudenberg N, Moseley J, Labriola M, Daniels J, Murrill C. Characteristics of people leaving New York City jails by age, gender, and race/ethnicity: implications for public health interventions. Pub Health Rep. 2007;122:733–743. doi: 10.1177/003335490712200605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beck AJ. The importance of successful reentry to jail population growth.. Presented at The Jail Reentry Roundtable; Washington, DC. June 27, 2006; The Urban Institute; 2006. Available at: http://www.urban.org/projects/reentry-roundtable/round-table9.cfm. [Google Scholar]
- 10.Kelly PJ, Peralez-Dieckmann E, Cheng A, Collins C. Profile of women in a county jail. J Psycosoc Nurs. 2010;48(4):38–45. doi: 10.3928/02793695-20100302-02. [DOI] [PubMed] [Google Scholar]
- 11.Clarke J, Hebert M, Rosengard C, Rose J, DaSilva K, Stein M. Reproductive health care and family planning needs among incarcerated women. Am J Public Health. 2006;96(5):834–839. doi: 10.2105/AJPH.2004.060236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fickenscher A, Lapidus J, Silk-Walker P, Becker T. Women behind bars: health needs of inmates in a county jail. Pub Health Rep. 2001;116(3):191–196. doi: 10.1093/phr/116.3.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richie B, Johnsen C. Abuse histories among newly incarcerated women in a New York City jail. J Am Med Wom Assoc. 1996;51(3):111–114. [PubMed] [Google Scholar]
- 14.Teplin L, Abram K, McClelland G. Prevalence of psychiatric disorders among incarcerated women. Arch Gen Psych. 1996;53:505–512. doi: 10.1001/archpsyc.1996.01830060047007. [DOI] [PubMed] [Google Scholar]
- 15.Urban Institute Communities and re-entry. 2010 Available at: http://www.urban.org/projects/reentry-portfolio/communities.cfm.
- 16.James D. Bureau of Justice Statistics Publication No. NCJ 201932. US Department of Justice; 2004. Profile of jail inmates, 2002. [Google Scholar]
- 17.Richie B. Challenges incarcerated women face as they return to their communities: findings from life history interviews. Crime Delinq. 2001;47(3):368–389. [Google Scholar]
- 18.Johnson S, Solomon B, Shields W, McDonald E, McKenzie L, Gielen A. Neighborhood violence and its association with mother's health: Assessing the relative importance of perceived safety and exposure to violence. Journal of Urban Health. 2009;86(4):538–50. doi: 10.1007/s11524-009-9345-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Short J. Poverty, Ethnicity, and Violent Crime. Westview Press; Boulder, CO: 1997. [Google Scholar]
- 20.Taxman FS, Byrne JM, Pattavina A. Racial disparity and the legitimacy of the criminal justice system: exploring consequences for deterrence. J Health Care Poor Underserved. 2005;16(4 Suppl B):57–77. doi: 10.1353/hpu.2005.0119. [DOI] [PubMed] [Google Scholar]
- 21.Clear TR. Imprisoning Communities: How Mass Incarceration Makes Disadvantaged Neighborhoods Worse. Oxford University Press, Inc; New York, NY: 2007. [Google Scholar]
- 22.Thomas JC, Torrone E. Incarceration as forced migration: effects on selected community health outcomes. Am J Public Health. 2006;96:1762–1765. doi: 10.2105/AJPH.2005.081760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson RC, Raphael S. The effects of male incarceration on dynamics of AIDS infection rates among African-American women and men. Presented to the incarceration study group of the Russell Sage Foundation. 2005 Jul; [Google Scholar]
- 24.Brunner E, Marmot M. Social organization, stress, and health. In: Marmot M, Wilkinson R, editors. Social Determinants of Health. Oxford University Press; Oxford: 2006. pp. 6–30. [Google Scholar]
- 25.Ramaswamy M, Kelly PJ, Koblitz A, Kimminau KS, Engelman KK. Understanding the role of violence in incarcerated women's cervical cancer screening and history. Women Health. 2001;51:423–441. doi: 10.1080/03630242.2011.590875. [DOI] [PubMed] [Google Scholar]
- 26.Wright R, Mitchell H, Visness C, Cohen S, Stout J, Evans R, Gold DR. Community violence and asthma morbidity: The inner-city asthma study. Am J Public Health. 2004;94(4):625–632. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 28.Hjollund L, Tinggaard Svendsen G. Social capital: A standard method of measurement. 2000 Available at: http://www.hha.dk/nat/WPER/00-9_gts.pdf.
- 29.Inglehart R, Basañez M, Moreno A. Findings from the 1990-93 World Values Survey. University of Michigan Press; Ann Arbor, MI: 1998. Human values and beliefs: A cross-cultural sourcebook. Political, religious, sexual, and economic norms in 43 societies. [Google Scholar]
- 30.Kim A, Page-Shafer K, Reyes L, Delgado V, Klausner J, Molitor F, Katz M, McFarland W. Vulnerability to HIV among women formerly incarcerated and women with incarcerated sexual partners. AIDS Behav. 2002;6(4):331–338. [Google Scholar]
- 31.McClelland G, Teplin L, Abram K, Jacobs N. HIV and AIDS risk behaviors among female jail detainees: Implications for public health policy. Am J Public Health. 2002;92(5):818–825. doi: 10.2105/ajph.92.5.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Compton W, Grant B, Colliver J, Glanz MD, Stinson FS. Prevalence of marijuana disorders in the United States: 1991-1992 and 2002-2002. J Am Med Assoc. 2004;291(17):2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- 33.Walsh C, MacMillan H, Trocme N, Jamieson E, Boyle M. Measurement of victimization in adolescence: Development and validation of the Childhood Experiences of Violence Questionnaire. Child Abuse Neglect. 2008;32(11):1037–57. doi: 10.1016/j.chiabu.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Sherin K, Sinacore J M, Li XQ, Zitter RE, Shakil A. HITS: A short domestic violence screening tool for use in a family practice setting. Fam Med. 1998;30(7):508–512. [PubMed] [Google Scholar]
- 35.Morgan SP, Teachman JD. Logistic regression: Description, examples, and comparisons. J Marriage Fam. 1998;50(4):929–36. [Google Scholar]
- 36.Kansas City Police Department . KCPD statement on 2008 homicides. Vol. 31. Crime Scene KC. Kansas City Star; Dec, 2008. [Google Scholar]
- 37.Rizzo T. Murder Factory, Part 1: 64130, the ZIP code of notoriety in Missouri. Kansas City Star; Jan 24, 2009. [Google Scholar]
- 38.Cohen D, Spear S, Scribner R, Kissinger P, Mason K, Wildgen J. “Broken windows” and the risk of gonorrhea. Am J Public Health. 2000;90(2):230–6. doi: 10.2105/ajph.90.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ellen JM, Jennings JM, Meyers T, Chung SE, Taylor R. Perceived social cohesion and prevalence of sexually transmitted diseases. Sex Transm Dis. 2004;31(2):117–22. doi: 10.1097/01.OLQ.0000110467.64222.61. [DOI] [PubMed] [Google Scholar]
- 40.Thomas JC, Levandowski BA, Roman Isler M, Torrone E, Wilson G. Incarceration and sexually transmitted infections: A neighborhood perspective. J Urban Health. 2007;85(1):90–99. doi: 10.1007/s11524-007-9231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thomas JC, Torrone EA, Browning CR. Neighborhood factors affecting rates of sexually transmitted diseases in Chicago. J Urban Health. 2010;87(1):102–12. doi: 10.1007/s11524-009-9410-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Javanbakht M, Boudov M, Anderson LJ, Malek M, Smith LV, Chien M, Guerry S. Sexually transmitted infections among incarcerated women: findings from a decade of screening in a Los Angeles County Jail, 2002-2012. Am J Public Health. 2014;104(11):e103–9. doi: 10.2105/AJPH.2014.302186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wiehe SE, Barai N, Rosenman MB, Aalsma MC, Scanlon ML, Fortenberry JD. Test positivity for Chlamydia, gonorrhea, and syphilis infection among a cohort of individuals released from jail in Marion County, Indiana. Sex Transm Dis. 2015;42(1):30–6. doi: 10.1097/OLQ.0000000000000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spaulding AC, Miller J, Trigg BG, Braverman P, Lincoln T, Reams PN, Staples-Horne M, Sumbry A, Rice D, Satterwhite CL. Screening for sexually transmitted diseases in short-term correctional institutions: summary of evidence reviewed for the 2010 Centers for Disease Control and Prevention Sexually Transmitted Diseases Treatment Guidelines. Sex Transm Dis. 2013;40(9):679–84. doi: 10.1097/01.olq.0000431353.88464.ab. [DOI] [PubMed] [Google Scholar]
- 45.Dembosky A. Clinic workers to include ex-inmates in health care's embrace. New York Times; Feb 4, 2010. [Google Scholar]
- 46.Zaitrow B, Thomas J. Women in Prison: Gender and Social Control. Lynne Rienner Publishers; Boulder, CO: 2003. [Google Scholar]
- 47.Chesney-Lind M. The Female Offender: Girls, Women and Crime. Sage; Thousand Oaks, CA: 1997. [Google Scholar]
- 48.Abbott AA. A feminist approach to substance abuse treatment and service delivery. Soc Work Health Care. 1994;19(3-4):67–83. doi: 10.1300/J010v19n03_04. [DOI] [PubMed] [Google Scholar]
- 49.Kelly PJ, Bobo T, Avery S, McLachlan K. Feminist perspectives and practice with young women. Issues Comp Ped Nurs. 2004;27(2):121–33. doi: 10.1080/01460860490451831. [DOI] [PubMed] [Google Scholar]
- 50.Kelly PJ, Blacksin B, Mason E. Factors affecting substance abuse treatment completion for women. Issues Ment Health Nurs. 2001;22(3):287–304. doi: 10.1080/01612840152053110. [DOI] [PubMed] [Google Scholar]
- 51.Draine J, McTighe L, Bourgois P. Education, empowerment and community based structural reinforcement: an HIV prevention response to mass incarceration and removal. Int J Law Psychiatry. 2011;34(4):295–302. doi: 10.1016/j.ijlp.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]