To the Editor
Hypoplastic metatarsals, or idiopathic brachymetatarsia, is a relatively frequent diagnosis in podiatric practice. Patients with this abnormality typically seek surgery because of cosmetic concerns, difficulty wearing shoes, or foot discomfort. Hypoplastic metatarsals may be accompanied by other physical features, most often related to Albright’s hereditary osteodystrophy. When findings indicative of Albright’s hereditary osteodystrophy are present in conjunction with laboratory abnormalities, pseudohypoparathyroidism type 1a is the likely diagnosis. However, the case we describe here shows that isolated hypoplastic metatarsals can be the initial presentation of pseudohypoparathyroidism type 1b.
Pseudohypoparathyroidism type 1b has been considered distinct from type 1a. Patients with either form of pseudohypoparathyroidism present with parathyroid hormone (PTH)–resistant hypocalcemia and hyperphosphatemia and may have resistance to other hormones. Both disorders are caused by genetic or epigenetic defects that involve the GNAS complex, which encodes the alpha subunit of the stimulatory G protein and splice variants thereof.1–3 Pseudohypoparathyroidism type 1a is caused by maternal inactivating mutations affecting GNAS exons 1 through 13, and type 1b is caused by maternal GNAS or STX16 deletions, paternal uniparental disomy involving chromosome 20q, or as-yet-undefined genetic mutations that alter GNAS methylation imprints. Despite the fact that the two types of pseudohypoparathyroidism are caused by distinct genetic defects, growing evidence indicates that there is considerable overlap between the two disorders, as shown by the case we describe here.
An otherwise healthy 16-year-old girl visited an emergency department because of palpitations, tingling and numbness of the arms and hands, and hand spasms. Six months earlier, postoperative osteomyelitis had developed after an elective distraction osteosynthesis to lengthen the left fourth metatarsal; the right fourth metatarsal had been successfully elongated 9 months earlier. The physical examination revealed Trousseau’s sign and a short left fourth toe (Fig. 1).
Figure 1. Images of the Toes before and after Surgery.
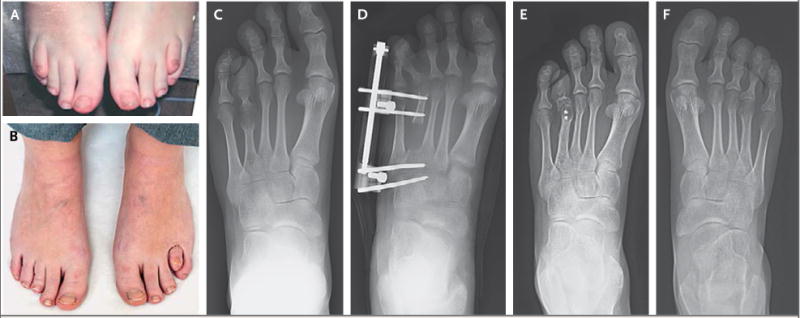
The patient’s shortened fourth toes before distraction osteogenesis are shown in Panel A. Panel B shows the toes after the procedure; the right toe appears normal, whereas the left toe is not completely corrected, because of an infection that required removal of the external fixators. Radiographs of the shortened left fourth metatarsal before surgical intervention are shown in Panel C. Panel D shows the left foot after osteotomy, with external fixation in place and overcorrection of the metatarsal. Panel E shows the foot after removal of the external fixation device and shortening osteotomy to relocate the joint, leaving only two screws in place. Panel F shows a normal-appearing right fourth metatarsal 9 years after distraction osteogenesis.
The laboratory results included an ionized calcium level of 3.5 mg per deciliter (0.88 mmol per liter), a total calcium level of 6.5 mg per deciliter (1.6 mmol per liter), a serum phosphate level of 4.1 mg per deciliter, a PTH level of 1027 pg per milliliter, and a thyroid-stimulating hormone level of 2.7 mIU per liter. Radiography revealed a short left fourth metatarsal with screws from the earlier distraction osteogenesis procedure; the right fourth metatarsal had a normal appearance after elongation, and all other metatarsals were also normal. No mutation was identified in exons 1 through 13 of GNAS (DNA Diagnostic Laboratory, Johns Hopkins University), which indicated that pseudohypoparathyroidism type 1a was unlikely. Epigenetic changes were identified at four differentially methylated GNAS regions (see the Supplementary Appendix, available with the full text of this letter at NEJM.org); there was no evidence of allelic loss or paternal uniparental isodisomy involving chromosome 20q.
This case shows that isolated shortening of the metatarsals may be the initial evidence for pseudohypoparathyroidism type 1b, a disorder that can go unrecognized for extended periods but that often causes severe hypocalcemia. Because such patients typically remain normocalcemic through PTH-dependent bone resorption, preoperative testing of patients who present to lengthen an isolated fourth metatarsal or metacarpal4,5 should include a PTH measurement, even in the absence of other features of Albright’s hereditary osteodystrophy.
Supplementary Material
Acknowledgments
Supported by grants (R01DK46718-20 and PO1DK11794 [subproject IV], to Dr. Jüppner) from the National Institute of Diabetes and Digestive and Kidney Diseases.
Footnotes
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
Contributor Information
Amita Sharma, Email: asharma5@partners.org, Massachusetts General Hospital, Boston, MA.
Alfred J. Phillips, St. Elizabeth Medical Center, Brighton, MA
Harald Jüppner, Massachusetts General Hospital, Boston, MA
References
- 1.Weinstein LS. The stimulatory G protein alpha-subunit gene: mutations and imprinting lead to complex phenotypes. J Clin Endocrinol Metab. 2001;86:4622–6. doi: 10.1210/jcem.86.10.8007. [DOI] [PubMed] [Google Scholar]
- 2.Mantovani G. Clinical review: pseudohypoparathyroidism: diagnosis and treatment. J Clin Endocrinol Metab. 2011;96:3020–30. doi: 10.1210/jc.2011-1048. [DOI] [PubMed] [Google Scholar]
- 3.Bastepe M, Jüppner H. Pseudohypoparathyroidism, Albright’s hereditary osteodystrophy, and progressive osseous heteroplasia: disorders caused by inactivating GNAS mutations. In: DeGroot LJ, Jameson JL, editors. Endocrinology. 7th. Philadelphia: W.B. Saunders; 2015. pp. 1147–59. [Google Scholar]
- 4.Fox IM. Treatment of brachymetatarsia by the callus distraction method. J Foot Ankle Surg. 1998;37:391–5. doi: 10.1016/s1067-2516(98)80047-1. [DOI] [PubMed] [Google Scholar]
- 5.Wada A, Bensahel H, Takamura K, Fujii T, Yanagida H, Nakamura T. Metatarsal lengthening by callus distraction for brachymetatarsia. J Pediatr Orthop B. 2004;13:206–10. doi: 10.1097/00009957-200405000-00012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


