Abstract
Purpose: A growing body of research has begun to examine wellness behaviors in sexual minority women. While a number of constructs have been associated with wellness behaviors in this population, including outness, social support, and mental health, no research has attempted to forge the specific and unique connections among them. The aim of the current study was to construct a theoretical chain among these variables leading to wellness behaviors among an ethnically diverse sample of sexual minority women.
Methods: A sample of 150 ethnically diverse, cisgender women identifying as lesbian, bisexual, queer, or an “other” non-heterosexual sexual orientation completed a web-administered national survey. Scales assessed participants' outness, social support, mental health, and wellness behaviors.
Results: In a series of simultaneous, multiple regressions, outness to one's family was positively associated with wellness behavior and social support; social support from one's family and friends was positively associated with mental health; and depression was negatively associated with wellness behaviors. Two multiple mediational models generally suggested a cascading influence of outness to one's family on wellness behaviors through social support from one's family and depression.
Conclusion: The study is one of the first to find potentially cascading links among personal, social, and mental health variables with health behaviors in a sample of diverse lesbian, bisexual, and queer (LBQ) women. It thereby illuminates a number of potential targets for health promotion interventions in this population.
Key words: : access to care, bisexual mental health needs, lesbian
Introduction
Lesbian, bisexual, and queer (LBQ) women face significant disparities in health behaviors and outcomes.1 Compared to heterosexual women, lesbian and bisexual women have fewer mammograms, pap smears, gynecological cancer screenings,2–5 and general preventive health screenings.6 This lower preventive healthcare utilization has been connected with a range of health outcomes, as bisexual women face higher rates of back problems, digestive symptoms, fatigue, and other functional health concerns than heterosexual women.7,8 Recent research examining health maintenance behaviors has found that lesbian women may also be at increased risk for cervical and breast cancers,2,9,10 though definitively higher risk of both conditions in LBQ women has yet to be established. Lesbian women also share the same risk of polycystic ovarian syndrome (PCOS) as heterosexual women,11 that may often go undiagnosed due to lack of preventive healthcare utilization. Additionally, sexual minority women are at a heightened risk for cigarette smoking, alcohol abuse, obesity, and chronic physical health problems.2,10,12,13 Despite these disparities, only 85 National Institutes of Health-funded studies have involved sexual minority women.14 Most included only a lesbian sample (n=63), half included bisexual women (n=41), and very few included any other sexual minority identification (n=3). Patterns of wellness behaviors in lesbian, bisexual, and other sexual minority women are a critical area for research.
One potentially important predictor of health or wellness behaviors in LBQ women is outness—the disclosure of sexual orientation—which has been linked to increased mental health and reduced risky sexual behaviors in sexual minorities.15 Outness can manifest in many different ways, and the manner by which an individual discloses sexual orientation can differ greatly. LBQ women may be selectively “out” (i.e., they have disclosed their sexual orientation to peers and family, but are not out at work or school). In other cases, an LBQ woman may openly disclose her sexual orientation.15 Other research has found that outness among sexual minority women is associated with less anxiety, more positive affect, greater self-esteem,16 less psychological distress,17 higher self-efficacy, and more lifestyle satisfaction.18 Additionally, disclosure of sexual orientation to health care providers has been associated with greater health care utilization.6,9,19 Among lesbian and bisexual women, nondisclosure of sexual orientation to parents has been associated with greater drug abuse and depression, as well as poorer wellness behaviors in comparison to lesbian and bisexual women who have disclosed.20
A second important predictor of wellness behaviors among LBQ women is social support, which has also been positively associated with outness among lesbian women.16 Social support may be an important resource for lesbian and bisexual women,21,22 as greater social support has been associated with lower depression and anxiety,16,23,24 as well as higher life satisfaction and self-esteem.23,25 Family support in particular has been robustly related to psychosocial and physical health in the lesbian, gay, bisexual, transgender, and queer (LGBTQ community).20,26–33
A third important predictor of wellness behaviors among LBQ women is mental health: Multiple studies have found that anxiety and depression are high among lesbian and bisexual women.34–37 Primary mental health concerns reported by lesbian women include depression, anxiety and panic disorders, alcoholism, eating disorders, and suicide attempts.38 Among LGBT individuals, poor mental health has been associated with poor health behaviors such as illicit drug use,39,40 tobacco use,41–43 and alcohol abuse.12 Additionally, among sexual minority women, higher depression and anxiety have been associated with poor health-related quality of life,44 lack of exercise,12 obesity, and poor general health.12,45
The Current Study
Although research has generally examined the constructs of outness, social support, mental health, and wellness behaviors in sexual minority women, no research to date has linked these separate constructs into a theoretical chain. The purpose of the current study is to integrate the most important subcomponents of these larger constructs into a path model with data from a national sample of ethnically diverse sexual minority women. It is hypothesized that greater outness will lead to greater social support, which will increase mental health and eventually wellness behaviors.
Method
Participants
The sample included 150 cisgender women who identified as lesbian, bisexual, queer, or an “other” non-heterosexual orientation and were at least 18 years of age. Sexual orientation was self-reported and participants had the option of selecting from the categories of heterosexual, bisexual, lesbian, queer, or “other” which included writing in their sexual orientation label (“pansexual,” “Kinsey 5,” etc.). All participants selected a non-heterosexual orientation, as this was part of the inclusion criteria specified for participation in the informed consent. Recruitment was conducted via a web-administered national survey. To prevent the analyses from being impacted by false or fabricated responses, any data that showed an indication of being produced from an automated computer program (e.g., unreasonably short or long completion time), containing impossible response patterns (e.g., selecting the first or last item of every scale), or containing incorrect responses to randomly inserted accuracy check items (e.g., “Please select ‘Strongly Disagree’ for this item”) were automatically deleted from the survey software. Due to the presence of participant incentives, this method of automatic response deletion was necessary to reduce the chance of obtaining false responses. Because this was an automatic process, the total number of deleted data entries is unknown. The mean age of participants was 31.9 (SD=11.95), and the range was 18–66 (Table 1).
Table 1.
Demographics of Study Sample
| Variable | n | % |
|---|---|---|
| Sexual Orientation | ||
| Lesbian | 58 | 38.7 |
| Bisexual | 49 | 32.7 |
| Queer | 38 | 25.3 |
| Other | 5 | 3.3 |
| Race | ||
| White/European American | 44 | 29.3 |
| Black/African American | 39 | 26 |
| Asian/Asian American/Pacific Islander | 25 | 16.7 |
| Latino/Hispanic | 17 | 11.3 |
| American Indian/Native American | 4 | 2.7 |
| Multiracial/Multiethnic | 19 | 12.7 |
| Other | 2 | 1.3 |
| Employment | ||
| Full-time | 66 | 44 |
| Part-time | 18 | 12 |
| College enrollment | 24 | 16 |
| College enrollment & part-time | 27 | 18 |
| Unemployed | 15 | 10 |
| Education | ||
| Completed high school/received GED | 9 | 6 |
| Completed some college | 37 | 24.7 |
| 2-year technical degree | 14 | 9.3 |
| 4-year degree | 45 | 30 |
| Master's degree | 33 | 22 |
| Doctoral degree | 12 | 8 |
| Social Class | ||
| Upper Class ($200K+) | 5 | 3.3 |
| Upper Middle Class ($60K–199K) | 62 | 41.3 |
| Lower Middle Class ($30K–59K) | 44 | 29.3 |
| Working Class ($15K–29K) | 22 | 14.7 |
| Lower Class ($7K–14K) | 17 | 11.3 |
| Age (years) | ||
| 18–25 | 61 | 40.7 |
| 26–33 | 37 | 24.7 |
| 34–41 | 22 | 14.7 |
| 42–49 | 10 | 6.7 |
| 50–57 | 12 | 8 |
| 58–66 | 8 | 5.5 |
Measures
Outness Inventory (OI)
The OI46 is an 11-item scale that assesses the degree to which sexual minorities disclose their sexual orientation to others across three dimensions: Out to Family, World, and Religion. Higher scores indicate greater levels of outness. Because many participants did not identify as having a religious community, that subscale was omitted. The OI has adequate internal consistency.46
Multidimensional Scale of Perceived Social Support (MSPSS)
The MSPSS47 is a 12-item measure of social support across three dimensions: Social Support from Family, Friends, and a Significant Other. Higher scores indicate greater social support. The MSPSS has strong internal consistency (α=.88) for the overall scale and subscales (.85–.91), as well as good construct validity.47
Hopkins Symptoms Checklist 25 (HSCL)
The HSCL-2548 is the short-version of the 58-item Hopkins Symptom Checklist. It is a 25-item assessment of anxiety and depression, and higher scores indicate greater symptoms with a clinical cutoff at 1.75.49
Rosenberg Self-Esteem (RSES)
The RSES50 is a 10-item measure of self-esteem with higher scores reflecting better self-esteem. The scale has high internal consistency (α=.89).51
Health Behavior Checklist (HBC)
The HBC52 is comprised of 40 items assessing health behaviors across three dimensions: Wellness, Traffic-Risk, and Accident Control Behaviors, although only the 10-item Wellness Behaviors subscale is used in the current study, and higher scores indicate better wellness behaviors. The Wellness Behaviors subscale includes items that assess exercise, health information consumption and communication, primary care utilization, nutrition habits, and weight maintenance. The Wellness Behaviors subscale has adequate internal consistency (α=.77).52 To the best of our knowledge, this is the first instance that this measure has been used with sexual minority women sample.
Procedure
Participants were recruited through online forums and groups in national/regional LGBTQ organizations and online community groups via listservs and message boards, with an emphasis on groups catering to women of color. Participants interested in the study emailed the study coordinator who screened participants across eligibility criteria. Eligible individuals were emailed a survey link and unique access code. After the survey, participants input an email address to receive a $15 Amazon.com electronic gift card.
Data Analyses
Simultaneous multiple regressions were run in order to identify the largest pattern of connections between indices of outness, social support, mental health, and wellness behavior. The first regression included the two subscales of the OI (Out to World and Out to Family) as predictors and the Wellness Behavior subscale of the Vicker's HBC as the criterion. The second regression included the two subscales of the OI as predictors and the total score of the MSPSS as the criterion. The third regression included the three MSPSS subscales (Social Support from Family, Social Support from Friends, and Social Support from Significant Other) as predictors and the total score of the Hopkins Symptom Checklist-25 (HSCL-25) as the criterion. The fourth regression included the two subscales of the HSCL-25 (Depression and Anxiety) as the predictors and the Wellness Behavior subscale of the HBC as the criterion. The purpose of this series of regressions was to isolate the most significant patterns of connections among individual indices (subscales) of the larger constructs (outness, social support, mental health, and wellness behaviors). Based on the connections between variables identified in the series of regressions, two path models were constructed in order to examine possible direct and indirect effects among the variables most consistently associated with each other in the regressions. A significant indirect effect (or mediational effect) would indicate that the relationship between two variables in the path model could be statistically explained by the mediator.
Results
Exploratory multiple regressions
The first regression with Out to World and Family as predictors explained 9.4% of the variance in Wellness Behavior (F[2, 147]=7.58, P=.001). Out to Family was independently associated (β=.33, P<.001), such that more outness to one's family was associated with greater wellness behavior. Out to World was not uniquely associated (β=−.13, P=.134).
The second regression with Out to World and Family as predictors explained 5.7% of the variance in social support (F[2, 147]=4.43, P=.014). Out to Family was independently associated with social support (β=.19, P=.033), such that more outness to one's family was associated with greater social support. Out to World was not significant (β=.10, P=.274).
The third regression including Social Support from Family, Friends, and Significant Other as predictors explained 25.1% of the variance in mental health (F[3, 146]=16.31, P<.001). Social Support from Family (β=−.17, P=.039) and Social Support from Friends (β=−.31, P<.001) were positively associated with mental health, but Social Support from Significant Other (β=−.16, P=.050) was only marginally related.
The fourth regression included the Depression and Anxiety as predictors and Wellness Behavior as the criterion. These variables explained 9.0% of the variance in Wellness Behavior (F[2, 147]=7.26, p=.001). Depression was independently and negatively associated with Wellness Behavior (β=−.31, P=.010), while Anxiety was not (β=.01, P=.929).
Mediational models
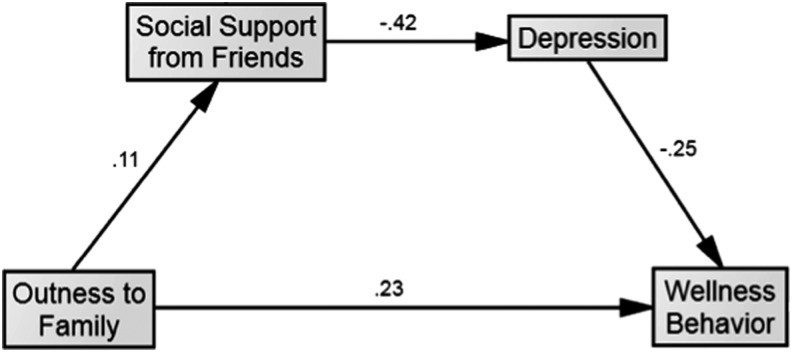
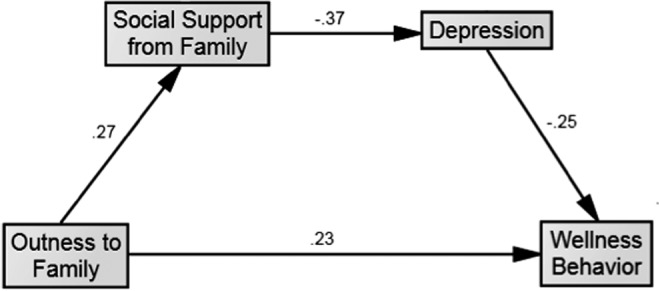
In the first model, Outness to Family was specified to lead to the ultimate outcome, Wellness Behavior. Two successive mediators, Social Support from Family and Depression, were included in this model (Figure 1). A second model included the same series of variables and direct and indirect effects with the substitution of Social Support from Friends for Social Support from Family (Figure 2). Because the sample size in the current study was lower than the 200 recommended by Boomsma and Hoogland,53 fit indices were omitted as they would likely be more obscuring than illuminating. Instead, the focus was on direct and indirect effects.
FIG. 1.
Mediation Model of Outness to Family, Social Support from Family, Depression, and Wellness Behavior.
FIG. 2.
Mediation Model of Outness to Family, Social Support from Friends, Depression, and Wellness Behavior.
In the first model, Outness to Family positively predicted Wellness Behavior (β=.23, P=.004) and Social Support from Family (β=.27, P<.001), Social Support from Family inversely predicted Depression (β=−.37, P<.001), and Depression inversely predicted Wellness Behavior (β=−.25, P=.002). The indirect effect of Outness to Family on Depression through Social Support from Family was statistically significant (β=−.10, P<.001), as was the indirect effect of Social Support from Family on Wellness Behavior through Depression (β=.09, P<.001). These findings suggest a multiple mediation effect.
In the second model, Outness to Family positively predicted Wellness Behavior (β=.23, P=.004), but did not significantly predict Social Support from Friends (β=.11, P=.183), Social Support from Friends inversely predicted Depression (β=−.42, p<.001), and Depression inversely predicted Wellness Behavior (β=−.25, P=.002). The indirect effect of Outness to Family on Depression through Social Support from Friends was not statistically significant (β=−.05, P=.152), although the indirect effect of Social Support from Friends on Wellness Behavior through Depression was (β=.11, P<.001). These findings suggest a single mediational effect.
Exploratory analyses
In order to examine demographic differences in Wellness Behavior, a number of exploratory analyses were conducted: Greater Wellness Behavior was positively associated with age (r=.33, P<.001) and education (r=.30, P<.001), but not with family social class (r=−.15, P=.064). Participants differed in Wellness Behavior as a function of sexual orientation, F(3, 146)=6.65, P<.001. Queer participants (M=28.29, SD=6.65) reported less Wellness Behavior than bisexual (M=32.73, SD=6.92), P=.003, and lesbian participants (M=34.53, SD=7.09), P<.001. Participants also differed in Wellness Behavior as a function of race/ethnicity, F(6, 143)=2.85, P=.012. Black/African-American participants (M=28.69, SD=7.85) reported less Wellness Behavior than White (M=34.36, SD=6.13), P<.001, and Multiracial/Multiethnic participants (M=34.79, SD=5.66), P=.002.
Discussion
A growing body of research has begun to examine wellness behavior in sexual minority women.14 While a number of constructs have been associated with wellness behavior in this population including outness, social support, and mental health, no research has attempted to forge the specific and unique connections among them. The aim of the current study was to construct a theoretical chain among these variables leading to wellness behavior among an ethnically diverse sample of sexual minority women. In a series of simultaneous multiple regressions, outness to one's family was positively associated with wellness behaviors and social support; social support from one's family and friends were positively associated with mental health; and depression was negatively associated with wellness behaviors. Two multiple mediational models generally suggested a cascading influence of outness to one's family on wellness behavior through social support from one's family and depression.
In the first two regressions, with indices of outness as the predictors and wellness behavior and social support as the criteria, Outness to Family was a unique predictor of both. These findings are consistent with previous studies, which have found that greater outness is associated with greater social support and better physical health in sexual minority women.16,20,54 Disclosure of deeply personal issues more generally has been associated with an array of physical health benefits,55 and among sexual minorities, coming out has been positively associated with wellness behavior including regular health care use and decreased substance use.19,20 Additionally, greater disclosure of one's sexual orientation has been associated with a greater sense of belonging to the LGBT community,54,56 suggesting that connecting with people who experience similar social challenges may provide social support for coping with minority stressors. Outness to one's family may be of particular importance for LBQ women, as disclosing one's sexual orientation to one's parents has been associated with parent-child relationship quality through increased closeness and honesty.57 Disclosure may also increase future social support, which has a strong association with health promotion.58
In the third regression with social support regressed onto mental health, social support from family and friends were each independently associated with mental health. These results are congruent with prior research showing that greater social support is related to lower depression in sexual minority women24,59,60 and greater life satisfaction.23,25,61 Additionally, lesbian and bisexual women with unsupportive parents have been shown to have more days of depression in the previous month.20 Taken together, the results suggest that various forms of social support may prove beneficial for promoting good mental health in sexual minority women.
In the final regression, depression was uniquely associated with wellness behavior, which is also in line with previous research. Poor mental health of LGBT individuals has been associated with illicit drug use,39 sexually transmitted infections,40,62 tobacco use,41–43 and alcohol abuse.12 Most of these associations have been identified in LGBT adolescents, although research on sexual minority women has found reduced mental health to be associated with poor health-related quality of life,44 lack of exercise,12 and poor general health.45,12
Mediational models and clinical implications
A major goal of this study was to create a path model linking outness through social support and mental health to wellness behavior. Consistent with the hypothesis, in the first model the indirect effects of outness to family and wellness behaviors through social support from family and depression were significant. To test whether social support from friends was a key part of the theoretical chain, the second model examined if outness to family was linked to wellness behavior through social support from friends and depression. The direct effect of outness to family on social support from friends was not significant, and neither was the indirect effect of social support from friends on the relationship between outness to family and mental health. The lack of a direct effect of outness to family on social support from friends, as well as only one significant mediational effect, in comparison to all significant direct and indirect effects in the first model, suggests the retention of the first model over the second. An interpretation could be that LBQ women who were more out to their family received greater social support from their family, which in turn decreased depression and increased wellness behavior. This is in line with past research identifying social support mediating the relationship between outness and mental health in lesbian and gay individuals.25
These results have a number of health promotion implications. Health promotion specialists or healthcare providers taking a prevention approach may be able to work with LBQ women struggling with disclosure by assisting them to decide whether to come out to the right people and under what contexts, as doing so could create a stronger sense of identity as well as expand social support. Additionally, interventions may be helpful in encouraging LBQ women to build healthier relationships with their families and re-forge connections between potentially estranged family members to address conflicting emotions and generate a greater sense of empathy for each other.57 By creating healthy relationships, families of LBQ women could be better able to empathize with LBQ women and subsequently provide social support as these women navigate the effects of greater disclosure. Cognitive behavioral therapy may also prove useful in helping eliminate cognitive distortions surrounding being a sexual minority woman and reduce depression.63 Having a greater understanding and awareness of internalized heterosexism could encourage greater self-acceptance, reduce depression, and promote overall greater wellness behavior.
Limitations and future directions
This study has several limitations, and as a result, directions for future research. Though this was a national sample, participants were recruited through online forums and community groups. Participants may have been more “out” and subsequently more connected to support communities than LBQ women in the general population. Additionally, participants had a fairly high level of education, with the majority having completed at least some college. Given that a higher level of education may be associated with less psychological distress, it will be important in future studies to recruit participants with less education. Furthermore, the process by which participants initiated the survey (emailing the study coordinator personally) may have generated a sample that was highly motivated to complete the study. Additionally, the small sample size precludes the provision of fit indices of the path models. Future research should recruit larger samples as well as one that is more representative of the spectrum of outness among LBQ women. Since structural equation modeling with a sample size of 150 cannot easily control for the demographic differences in wellness behaviors found in the exploratory analyses, future research with larger sample sizes would also be able to remove the effects of these demographics or to determine whether these demographics moderate the relationships among key components of the model. Finally, because the data are correlational in nature, true causation cannot be proved from the path analysis. Indeed, greater social support could lead to greater outness, or improved mental health could make it easier to have better social support. Longitudinal designs employing cross-lagged panel techniques in future research could better parse out causality.
Conclusion
Despite these limitations, the current study modeled potential links between outness and wellness behaviors in sexual minority women, with mediating roles of social support and mental health. The study is one of the first to link personal, social, and mental health variables with health behaviors in this population. As a result, it illuminates a number of potential targets for health promotion interventions in LBQ women.
Acknowledgments
The survey software for this study was funded by award number UL1TR000058 from the National Center for Research Resources.
Author Disclosure Statement
No conflicting financial interests exist.
References
- 1.Hutchinson MK, Thompson AC, Cederbaum JA: Multisystem factors contributing to disparities in preventive health care among lesbian women. J Obstet Gynecol Neonatal Nurs 2006;35:393–402 [DOI] [PubMed] [Google Scholar]
- 2.Valanis BG, Bowen DJ, Bassford T, et al. : Sexual orientation and health: Comparisons in the women's health initiative sample. Arch Fam Med 2000;9:843–853 [DOI] [PubMed] [Google Scholar]
- 3.Moegelin L, Nilsson B, Helström : Reproductive health in lesbian and bisexual women in Sweden. Acta Obstet Gynecol Scand 2010;89:205–209 [DOI] [PubMed] [Google Scholar]
- 4.Fish J, Anthony D: UK national lesbians and health care survey. Women Health 2005;41:27–45 [DOI] [PubMed] [Google Scholar]
- 5.Matthews AK, Bradenburg DL, Johnson TP, Hughes TL: Correlates of underutilization of gynecological cancer screening among lesbian and heterosexual women. Prev Med 2004;38:105–113 [DOI] [PubMed] [Google Scholar]
- 6.Bergeron S, Senn CY: Health care utilization in a sample of Canadian lesbian women: Predictors of risk and resilience. Women Health 2003;37:19–35 [DOI] [PubMed] [Google Scholar]
- 7.Cochran SD, Mays VM: Physical health complaints among lesbians, gay men, and bisexual and homosexually experienced heterosexuals: Results from the California Quality of Life Survey. Am J Public Health 2007;97:2048–2055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cochran SD, Mays VM, Bowen D, et al. : Cancer-related risk indicators and preventive screening behaviors among lesbians and bisexual women. Am J Public Health 2001;91:591–597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tracy JK, Schluterman N, Greenberg D: Understanding cervical cancer screening among lesbians: A national survey. BMC Public Health 2013;13:442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steele LS, Ross LE, Dobinson C, et al. : Women's sexual orientation and health: Results from a Canadian population-based survey. Women Health 2009;49:353–367 [DOI] [PubMed] [Google Scholar]
- 11.Smith HA, Markovic N, Matthews AK, et al. : comparison of polycystic ovary syndrome and related factors between lesbian and heterosexual women. Womens Health Issues 2011;21:191–198 [DOI] [PubMed] [Google Scholar]
- 12.Austin EL, Irwin JA: Health behaviors and health care utilization of southern lesbians. Womens Health Issues 2010;20:178–184 [DOI] [PubMed] [Google Scholar]
- 13.Gruskin EP, Hart S, Gordon N, Ackerson L: Patterns of cigarette smoking and alcohol use among lesbians and bisexual women enrolled in a large health maintenance organization. Am J Public Health 2001;91:976–979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coulter R, Kenset K, Bowen D, Scout D: Research funded by the national institutes of health on the health of lesbian, gay, bisexual, and transgender populations. Am J Public Health 2014;104:105–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosario M: The coming-out process and its adaptational and health-related associations among gay, lesbian, and bisexual youth: Stipulation and exploration of a mode. Am J Community Psychol 2001;29:133–160 [DOI] [PubMed] [Google Scholar]
- 16.Jordan KM, Deluty RH: Coming out for lesbian women: Its relation to anxiety, positive affectivity, self-esteem, and social support. J Homosex 1998;35:41–63 [DOI] [PubMed] [Google Scholar]
- 17.Morris JF, Waldo CR, Rothblum RD: A model of predictors and outcomes of outness among lesbian and bisexual women. Am J Orthopsychiatry 2001;71:61–71 [DOI] [PubMed] [Google Scholar]
- 18.Anderson M, Mavis B: Sources of coming out self-efficacy for lesbians. J Homosex 1997;32:37–52 [DOI] [PubMed] [Google Scholar]
- 19.Steele LS, Tinmouth JM, Lu A: Regular health care use by lesbians: A path analysis of predictive factors. Fam Pract 2006;23:631–636 [DOI] [PubMed] [Google Scholar]
- 20.Rothman E, Sullivan M, Keyes S, Boehmer U: Parents' supportive reactions to sexual orientation disclosure associated with better health: Results from a population-based survey of LGB adults in Massachusetts. J Homosex 2012;59:186–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kwon P: Resilience in lesbian, gay, and bisexual individuals. Per Soc Psychol Rev 2013;17:371–383 [DOI] [PubMed] [Google Scholar]
- 22.Kaminski E: Lesbian health: Social context, sexual identity, and well-being. J Lesbian Stud 2000;4:87–10124802686 [Google Scholar]
- 23.Keleher K, Wei M, Liao KY: Attachment, positive feelings about being a lesbian, perceived general support, and well-being. J Soc Clin Psychol 2010;29:847–873 [Google Scholar]
- 24.Ayala J, Coleman H: Predictors of depression among lesbian women. J Lesbian Stud 2008;4:71–86 [Google Scholar]
- 25.Beals KP, Peplau LA, Gable SL: Stigma management and wellbeing: The role of perceived social support, emotional processing, and suppression. Pers Soc Psychol Bull 2009;35:867–879 [DOI] [PubMed] [Google Scholar]
- 26.Bouris A, Guilamo-Ramos V, Pickard A, et al. : A systematic review of parental influences on the health and well-being of lesbian, gay, and bisexual youth: Time for a new public health research and practice agenda. J Prim Prev 2010;31:273–309 [DOI] [PubMed] [Google Scholar]
- 27.Needham BL, Austin EL: Sexual orientation, parental support, and health during the transition to young adulthood. J Youth Adolesc 2010;39:1189–1198 [DOI] [PubMed] [Google Scholar]
- 28.Teasdale B, Bradley-Engen MS: Adolescent same-sex attraction and mental health: The role of stress and support. J Homosex 2010;57:287–309 [DOI] [PubMed] [Google Scholar]
- 29.Sheets RL, Mohr JJ: Perceived social support from friends and family and psychosocial functioning in bisexual young adult college students. J Couns Psychol 2009;56:152–163 [Google Scholar]
- 30.Homma Y, Saewyc EM: The emotional wellbeing of Asian-American sexual minority youth in school. J LGBT Health Res 2007;3:67–78 [DOI] [PubMed] [Google Scholar]
- 31.Ueno K: Sexual orientation and psychological distress in adolescence. Examining interpersonal stressors and social support processes. Soc Psychol Q 2005;68:258–277 [Google Scholar]
- 32.Floyd F, Stein TS, Harter K, et al. : Gay, lesbian, and bisexual youths: Separation-individuation, parental attitudes, identity consolidation, and wellbeing. J Youth Adolesc 1999;28:719–739 [Google Scholar]
- 33.D'augelli A, Grossman A, Starks M: Parents' awareness of lesbian, gay, and bisexual youths' sexual orientation. J Marriage Fam 2005;67:474–482 [Google Scholar]
- 34.Kerr DL, Santurri L, Peters P: A comparison of lesbian, bisexual, and college undergraduate women on selected mental health issues. J Am Coll Health 2013;61:185–194 [DOI] [PubMed] [Google Scholar]
- 35.Hughes TL, Haas AP, Razzano L, et al. : Comparing lesbians' and heterosexual women's mental health: A multi-site survey. J Gay Lesbian Soc Serv 2000;11:57–76 [Google Scholar]
- 36.Kerr SK, Emerson AM: A review of lesbian depression and anxiety. J Psychol Human Sex 2004;15:143–162 [Google Scholar]
- 37.Cochran SD, Sullivan JG, Mays VS: Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. J Consult Clin Psychol 2003;71:53–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roberts SJ, Grindel CG, Patsdaughter CA, et al. : Mental health problems and use of services of lesbians: Results of the Boston Lesbian Health Project II. J Gay Les Soc Serv 2004;17:1–16 [Google Scholar]
- 39.Hughes T, Szalacha LA, McNair R: Substance abuse and mental health disparities: Comparisons across sexual identity groups in a national sample of young Australian women. Soc Sci Med 2010;71:824–831 [DOI] [PubMed] [Google Scholar]
- 40.Lehavot K, Simoni M: The impact of minority stress on mental health and substance use among sexual minority women. J Consult Clin Psychol 2011;79:159–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sivadon A, Matthews AK, David KM: Social integration, psychological distress, and smoking behaviors in a Midwest LGBT community. J Am Psychiatr Nurses Assoc 2014;20:307–314 [DOI] [PubMed] [Google Scholar]
- 42.Blosnich J, Lee JG, Horn K: A systematic review of the aetiology of tobacco disparities for sexual minorities. Tob Control 2013;22:66–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Balsam KF, Beadnell B, Riggs KR: Understanding sexual orientation health disparities in smoking: A population-based analysis. Am J Orthopsychiatry 2012;82:482–493 [DOI] [PubMed] [Google Scholar]
- 44.Dibble SL, Eliason MJ, Crawford B: Correlates of wellbeing among African American lesbians. J Homosex 2012;59:820–838 [DOI] [PubMed] [Google Scholar]
- 45.Frederiksen-Goldsen K, Kim H, Barkan SE, et al. : Disparities in health-related quality of life: A comparison of lesbians and bisexual women. Am J Public Health 2010;100:2255–2261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mohr JJ, Fassinger R: Measuring dimensions of lesbian and gay male experience. Meas Eval Couns Dev 2000;33:66–90 [Google Scholar]
- 47.Zimet GD, Dahlem NW, Zimet SG, Farley GK: The multidimensional scale of perceived social support. J Pers Assess 1988;52:30–41 [DOI] [PubMed] [Google Scholar]
- 48.Derogatis LR, Lipman RS, Rickels K, et al. : The Hopkins Symptom Checklist (HSCL): A self-report inventory. Behav Sci 1974;19:1–15 [DOI] [PubMed] [Google Scholar]
- 49.Winokur A, Winokur DF, Rickels K, Cox DS: Symptoms of emotional distress in a family planning service: Stability over a four-week period. Br J Psychiatry 1984;144:395–399 [DOI] [PubMed] [Google Scholar]
- 50.Rosenberg M: Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press, 1965 [Google Scholar]
- 51.Bosker MJ: Assessing level of outness among gay, lesbian, and bisexual individuals and its relation to depression, anxiety, and self-esteem. DAI 2002;64:1482B [Google Scholar]
- 52.Vickers RR, Conway TL, Hervig LK: Demonstration of replicable dimensions of health behaviors. Prev Med 1990;19:377–401 [DOI] [PubMed] [Google Scholar]
- 53.Boomsma A, Hoogland JJ: The robustness of LISREL modeling revisited. In: Structural Equation Modeling: Present and Future. Cudeck R, du Toit S, Sörbom D, eds. Chicago, IL: Scientific Software International, 2001, pp 139–168 [Google Scholar]
- 54.Bradford J, Ryan C, Rothblum ED: National lesbian health care survey: Implications for mental health care. J Consult Clin Psychol 1994;62:228–242 [DOI] [PubMed] [Google Scholar]
- 55.Pennebaker JW, Chung CK: Expressive writing, emotional upheavals, and health. In: Oxford Handbook of Health Psychology. Edited by Friedman H. New York, NY: Oxford University Press, 2011 [Google Scholar]
- 56.Boatwright KJ, Gilbert MS, Forrest L, Ketzenberger K: Impact of identity development upon career trajectory: Listening to the voices of lesbian women. J Vocat Behav 1996;48:210–228 [Google Scholar]
- 57.LaSala MC: Lesbians, gay men, and their parents: Family therapy for the coming-out crisis. Fam Process 2000;39:67–81 [DOI] [PubMed] [Google Scholar]
- 58.Sarason BR, Sarason IG, Gurgung RAR: Close personal relationships and health outcomes: A key to the role of social support. In: Personal Relationships: Implications for Clinical and Community Psychology. Sarason B, Duck S, eds. Chichester, UK: Wiley, 2001, pp 15–41 [Google Scholar]
- 59.Szymanski DM, Kashubeck-West S: Mediators of the relationship between internalized oppressions and lesbian and bisexual women's psychological distress. Counsel Psychol 2008;36:575–594 [Google Scholar]
- 60.Oetjen H, Rothblum ED: Lesbians aren't gay: Factors affecting depressing among lesbians. J Homosex 2000;39:49–73 [DOI] [PubMed] [Google Scholar]
- 61.Sheets RL, Mohr JJ: Perceived social support from friends and family and psychosocial functioning in bisexual young adult college students. J Counsel Psychol 2009;56:152–163 [Google Scholar]
- 62.Frost DM, Parsons JT, Nanín JE: Stigma, concealment, and symptoms of depression as explanations for sexually transmitted infections among gay men. J Health Psychol 2007;12:636–640 [DOI] [PubMed] [Google Scholar]
- 63.Ross LE, Doctor F, Dimito A, et al. : Can talking about oppression reduce depression? J Gay Lesbian Soc Serv 2008;19:1–15 [Google Scholar]