Abstract
Background
End-tidal CO2 (ETCO2), partial pressure of exhaled CO2 (PECO2), and volume of expired CO2 (VCO2) can be continuously monitored non-invasively to reflect pulmonary ventilation and perfusion status. Although ETCO2 ≥14mmHg has been shown to be associated with return of an adequate heart rate in neonatal resuscitation and quantifying the PECO2 has the potential to serve as an indicator of resuscitation quality, there is little information regarding capnometric measurement of PECO2 and ETCO2 in detecting return of spontaneous circulation (ROSC) and survivability in asphyxiated neonates receiving cardiopulmonary resuscitation (CPR).
Methods
Seventeen newborn piglets were anesthetized, intubated, instrumented, and exposed to 45-minute normocapnic hypoxia followed by apnea to induce asphyxia. Protocolized resuscitation was initiated when heart rate decreased to 25% of baseline. Respiratory and hemodynamic parameters including ETCO2, PECO2, VCO2, heart rate, cardiac output, and carotid artery flow were continuously measured and analyzed.
Results
There were no differences in respiratory and hemodynamic parameters between surviving and non-surviving piglets prior to CPR. Surviving piglets had significantly higher ETCO2, PECO2, VCO2, cardiac index, and carotid artery flow values during CPR compared to non-surviving piglets.
Conclusion
Surviving piglets had significantly better respiratory and hemodynamic parameters during resuscitation compared to non-surviving piglets. In addition to optimizing resuscitation efforts, capnometry can assist by predicting outcomes of newborns requiring chest compressions.
Introduction
Neonatal asphyxia is a common cause of mortality and morbidity and worldwide contributes to approximately 1 million deaths annually. It has been reported that 0.08% of term-born neonates required cardiopulmonary resuscitation (CPR) [1]. In the latest guidelines on neonatal resuscitation, the American Heart Association states that if the heart rate remains undetected after 10 minutes in asystolic neonates, discontinuing the resuscitation efforts is justified [2]. However, the decision to discontinue resuscitation may be influenced by issues such as the presumed aetiology of the arrest, gestation of the baby, potential reversibility of the situation, and parents’ previously expressed feelings about the acceptable risk of morbidity. Thus, an objective method to assess recovery or to predict success of resuscitation may help decision-making.
End-tidal CO2 (ETCO2) is the level of CO2 at the end of an exhaled breath and is mainly determined by alveolar ventilation, pulmonary perfusion (right ventricular output), and total body CO2 production due to metabolism [3]. During acutely low cardiac output states, such as cardiac arrest, decreased pulmonary flow becomes the primary determinant of ETCO2, resulting in low ETCO2 values [4,5]. Observing changing levels of ETCO2, which reflect changes in pulmonary blood flow, while delivering chest compressions (CC) and ventilations has proven to be useful in determining circulatory status during cardiac arrest and resuscitation in human adults [6]. In theory, if all steps of CPR are performed adequately (e.g. delivering adequate ventilation (breathing), and performing CC (circulation)), ETCO2 values should be normal. Thus, low ETCO2 could be an indicator of ineffective CC and/or ventilation, which potentially could be used to improve the efficacy of the resuscitation in real time.
Partial pressure of exhaled CO2 (PECO2), which can be monitored non-invasively, reflects ventilation-perfusion matching. Other methods commonly used to measure ventilation-perfusion matching involve invasive or isotopic techniques that are not feasible in the neonatal population. To our knowledge, no studies regarding monitoring PECO2 have been done during CPR or within the neonatal population.
Using a swine model of neonatal hypoxia and asphyxia, we aimed to examine the temporal changes of ETCO2, volume of expired CO2 (VCO2), PECO2 and their relationship with survivability and hemodynamic changes during CPR. Based on the principle of animal experimentation, we reviewed the data collected in our previous experiments [7,8] in an attempt to discover an objective approach to evaluate recovery or predict the outcome of resuscitation. We hypothesized that ETCO2 and PECO2 during CPR correlated with hemodynamic changes and preceded the return of spontaneous circulation (ROSC) in asphyxiated newborn piglets.
Methods
Respiratory data was recorded for twenty newborn mixed breed piglets (1–4 days of age, weighing 1.6–2.3 kg), which were obtained on the day of experimentation from the University Swine Research Technology Centre. All experiments were conducted in accordance with the guidelines and approval of the Animal Care and Use Committee (Health Sciences), University of Alberta and presented according to the ARRIVE guidelines [9]. The piglets were instrumented as previously described [7,8]. A graphical display of the study protocol is presented in Fig 1. Animal ethics protocol number: AUP00000237.
Fig 1. Study protocol.
Respiratory parameters
A respiratory function monitor (NM3, Respironics, Philips, Andover, MA) was used to continuously measure tidal volume (VT), airway pressures, gas flow, ETCO2, VCO2, and PECO2. The combined gas flow and ETCO2 pneumotachometer was placed between the endotracheal tube and the ventilation device. Gas flow and airway pressures were measured using a fixed orifice flow pneumotachometer. VT was calculated by integrating the flow signal. ETCO2 was measured with a mainstream sensor using non-dispersive infrared absorption.
Experimental protocol
We reviewed data from our previous experiments [7,8], where piglets were randomized to receive either coordinated CPR with 3:1 compression:ventilation ratio vs. continuous CC during sustained inflations (SI) [7] or 3:1 compression:ventilation ratio vs. continuous CC with non-synchronized ventilation (CCaV) [8]. Briefly, all piglets were exposed to 45 minutes of normocapnic hypoxia. Hypoxia was followed by asphyxia until heart rate decreased to 25% of baseline, which was achieved by disconnecting the ventilator and clamping the endotracheal tube. Fifteen seconds after heart rate reached 25% of baseline, positive pressure ventilation was conducted for 30 seconds prior to the initiation of CC. ROSC was defined as an increase in heart rate >150/min for 15 seconds (Fig 1).
Technique of Resuscitation: Positive pressure ventilation was provided with a Neopuff T-Piece (Fisher & Paykel, Auckland, New Zealand); default settings were a peak inflating pressure of 30 cmH2O, a positive end expiratory pressure of 5 cmH2O, and a gas flow of 8 L/min. CC were performed using the two-thumb encircling technique by a single operator (GMS) in all piglets. A metronome was used to achieve the targeted CC rate. After 30 seconds of CC, oxygen was increased from 21% to 100%. Epinephrine was administered if no increase in heart rate or ROSC was observed despite adequate ventilation and CC. One minute after CC were commenced, epinephrine (0.01 mg/kg per dose) was given intravenously and then every minute as needed to a maximum of four doses. CPR in the 3:1 group was performed according to the current resuscitation guidelines with 90 CC and 30 inflations per minute [2]. Piglets randomized to the SI group received a SI with a peak inflating pressure of 30 cmH2O for 30 seconds. During SI, CC with a rate of 120 per minute was provided. SI was interrupted after 30 seconds for one second before a further 30 seconds of SI was provided. CC was delivered continuously until ROSC was achieved. Piglets randomized to CCaV received continuous CC at a rate of 90 CC/minute and asynchronous ventilations at a rate of 30 ventilations/minute. After ROSC, piglets were allowed to recover for four hours, and were then euthanized with an intravenous overdose of phenobarbital (100 mg/kg).
Data collection and analysis
Demographics of study piglets were recorded. Transonic flow probes, heart rate, and pressure transducer outputs were digitized and recorded with custom Asyst programming software (Data Translation, Ontario, Canada). Peak inflating pressure, VT, ETCO2, PECO2, and VCO2 were measured and analyzed using Flow Tool Physiologic Waveform Viewer (Philips Healthcare, Wallingford, CT). Respiratory function data were available for a total of 17 asphyxiated piglets, due to a malfunction of the respiratory function monitor [7,8]. Cardiac index (CI) was calculated using pulmonary artery blood flow (PABF)/body weight. The maximum duration of CC was 300 seconds; for analysis, we grouped the data into 5-second epochs. The data are presented as mean ± standard deviation (SD) for normally distributed continuous variables and median (interquartile range—IQR) when distribution was skewed. For all respiratory parameters, continuous values during CPR were analyzed. The data was tested for normality and compared using Student’s t-test for parametric and the Mann-Whitney U-test for nonparametric comparisons of continuous variables; χ2 was used for categorical variables. P-values are 2-sided and p<0.05 was considered statistically significant. Statistical analyses were performed with Stata (Intercooled 10, Statacorp Tx).
Results
Seventeen piglets were exposed to normocapnic hypoxia and asphyxia prior to receiving CPR. Baseline characteristics are presented in Table 1. The heart rate prior to commencement of CPR was similar between survivors and non-survivors (Table 1). The period of asphyxia was also similar between survivors and non-survivors (Table 1).
Table 1. Characteristics at baseline and prior to commencement of Cardio-Pulmonary Resuscitation (CPR).
| Survivors (n = 10) | Non-survivors (n = 7) | p-value | |
|---|---|---|---|
| Baseline characteristics | |||
| Age (days) | 2 (1) | 3(1) | 0.10 |
| Weight (g) | 1830 (141) | 1800 (141) | 0.67 |
| Male/female | 7/2 | 7 | 0.21 |
| Heart rate (bpm) | 229 (22) | 252 (26) | 0.08 |
| Arterial pH | 7.37 (0.05) | 7.33 (0.05) | 0.25 |
| Arterial PCO2 (mm Hg) | 45 (4) | 47 (3) | 0.40 |
| Plasma lactate (mmol/L) | 3.9 (0.6) | 4.2 (1.3) | 0.46 |
| Arterial hemoglobin (g/L) | 83 (10) | 80 (12) | 0.54 |
| Characteristics at commencement of CPR | |||
| Asphyxia time (sec)# | 87 (55–120) | 102 (72–135) | 0.26 |
| Heart rate prior CPR (bpm)# | 33 (0–49) | 58 (38–63) | 0.13 |
| Arterial pH | 6.96 (0.1) | 6.89 (0.1) | 0.21 |
| Arterial PCO2 (mm Hg) | 79 (20) | 84 (24) | 0.65 |
| Plasma lactate (mmol/L) | 11 (4) | 12 (4) | 0.87 |
Data presented as mean (SD) unless indicated #median (IQR)
Resuscitation
Overall, nine piglets achieved ROSC compared to eight who did not. Oxygen use was similar between groups (Table 2). Swine in both groups required epinephrine; however, the number of administered doses of epinephrine was significantly higher in the non-survivor group compared to the survivor group (Table 2).
Table 2. Characteristics during Cardio-Pulmonary Resuscitation (CPR).
| Survivors (n = 10) | Non-survivors (n = 7) | p-value | |
|---|---|---|---|
| Oxygen use | 8/2 | 6/1 | 0.76 |
| Epinephrine use | 5/5 | 6/1 | 0.13 |
| Doses of epinephrine+ | 1 (0–4) | 3 (0–4) | 0.042 |
| Mean arterial pressure (mm Hg) | 40 (16) | 34 (4) | 0.25 |
| Pulmonary arterial pressure (mm Hg) | 36 (11) | 30 (6) | 0.13 |
| Central venous pressure (mm Hg) | 26 (9) | 26 (9) | 0.99 |
Data presented as mean (SD) unless indicated +mean (range)
Respiratory parameters
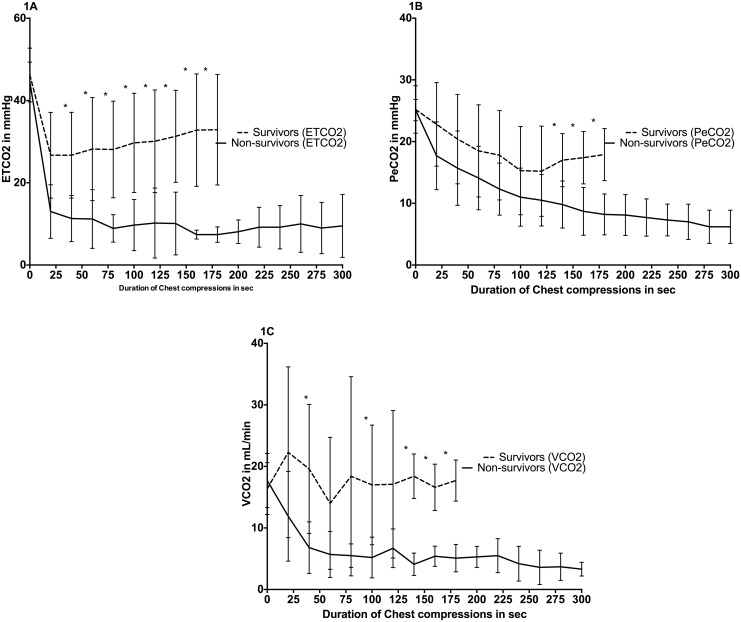
ETCO2 values were significantly higher in survivors compared to non-survivors during CPR (Fig 2A). PECO2 values were also significantly higher in survivors compared to non-survivors after 32 seconds of CC (Fig 2B). VCO2 values were observed to be significantly higher in survivors compared to non-survivors during CPR (Fig 2C).
Fig 2. ETCO2 (1A), PeCO2 (1B), VCO2 (1C) for survivors vs. non-survivors.
Baseline (at “0”, PPV until “30sec”, and CPR thereafter). Data are presented in mean (middle of line) with standard deviation (error bars), (* indicates p<0.05 survivors vs. non-survivors).
Median (IQR) VT delivery and peak inflation pressure were similar between survivors and non-survivors; 14.8 (12.7–18.7) mL/kg and 30 (29–31) cmH2O compared to 14.5 (12.5–17.8) mL/kg, and 30 (30–30) cmH2O, respectively.
Hemodynamic parameters
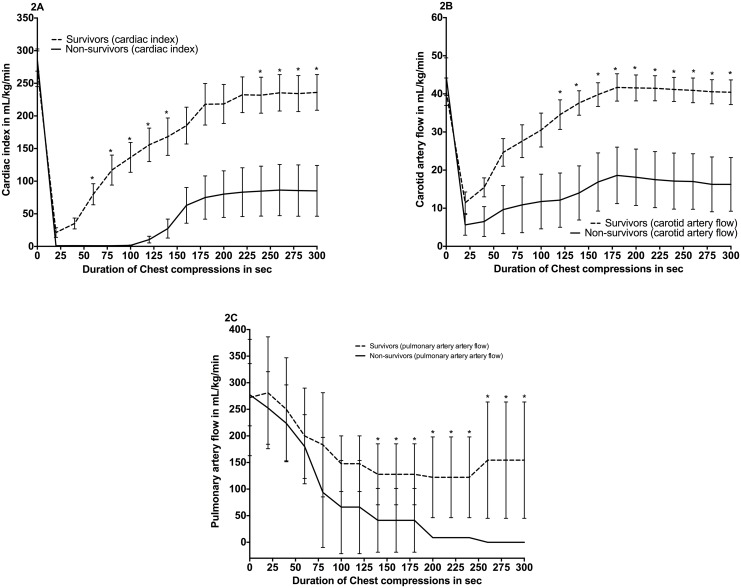
Piglets in the survivor group had a significantly increased median (IQR) carotid artery blood flow (CABF) from 120 seconds of CC onwards and significantly increased CI for the entire duration of CC compared to non-survivors (Fig 3A–3C). PABF was significantly increased in the latter part of resuscitation between survivors and non-survivors (Fig 3C). No differences between groups regarding mean arterial blood pressure, pulmonary artery blood pressure, and central venous pressure were observed (Table 2).
Fig 3. Cardiac index (2A), carotid artery flow (2B), pulmonary artery flow (2C) for survivors vs. non-survivors.
Baseline (at “0”, PPV until “30sec”, and CPR thereafter). Data are presented in mean (middle of line) with standard deviation (error bars), (* indicates p<0.05 survivors vs. non-survivors).
Discussion
In this study, we analyzed data from our experiments using an established swine model of neonatal asphyxia and resuscitation [10] to assess hemodynamic and respiratory parameters, which could potentially provide a clinical indicator to achieve ROSC. Our results indicated that surviving piglets had significantly higher values of ETCO2, VCO2, and PECO2 values during CPR compared to non-surviving piglets (Fig 2A–2C). In addition, we observed significantly higher CABF and CI during CPR in surviving piglets (Fig 3A and 3B). Surviving piglets also required significantly less epinephrine administration. Our data suggests that continuously monitoring ETCO2, VCO2, and PECO2 during CC has the potential to be a non-invasive measurement to indicate ROSC, support prediction of outcomes in newborns requiring CC, and determine whether resuscitation efforts could be discontinued.
In the adult population, changes in ETCO2 are used to evaluate ventilation and cardiac output during situations such as CPR [6]. A study using the same porcine model of hypoxia and asphyxia reported that even in low cardiac output states, positive CO2-detector results are observed [10]. In addition, ETCO2 has been detected during bradycardia (heart rate <50 beats/min) in an extremely preterm newborn [11]. Observing changing levels of ETCO2, which reflect changes in pulmonary blood flow, while delivering CC and ventilations has proven to be useful in determining circulatory status during cardiac arrest and resuscitation in human adults [6]. Furthermore, ETCO2 is good indicators of adequate establishment of the three components of CPR: airway, breathing, and circulation. In our study, piglets that achieved ROSC had significantly higher ETCO2 levels throughout the duration of CPR compared to piglets that did not achieve ROSC (Fig 2A). Chalak et al reported similar results by predicting ROSC using capnometry in a neonatal porcine model [3]. Using an ETCO2 of 14 mmHg was the most reliable indicator for ROSC with 92% sensitivity and 81% specificity. Chalak et al suggested that monitoring ETCO2 trends during resuscitation would allow uninterrupted CC and could provide a better indicator of the effectiveness of perfusion during CC [3]. This hypothesis was confirmed in an extremely preterm newborn where an increase in ETCO2 preceded and successfully predicted ROSC [11]. ETCO2 monitoring is a non-invasive tool that has been shown to predict and demonstrate ROSC during both animal and human adult cardiac arrest [6, 12–15]. Guidelines currently do not have any recommendations for the use of qualitative colorimetric CO2-detector during CPR; however, it may be useful to implement qualitative colorimetric CO2-detector or quantitative detectors measuring ETCO2, VCO2, and PeCO2 as a means to guide resuscitation efforts during CPR, and also serve as a predictor for ROSC.
VCO2, or the volume of expired CO2, reflects changes in both ventilation and perfusion, and therefore V/Q matching. Palme-Kilander et al reported that low VCO2 values recorded in preterm infants could originate from a number of factors, including deficient aeration due to residual lung fluid, very low tone, and deficient perfusion of the lungs [16]. Furthermore, a recent study showed that higher VCO2 levels are associated with lung aeration and successful establishment of a functional residual capacity [17]. Survivors in our study had significantly higher VCO2 during some portions of CPR (Fig 2C). Increased levels of VCO2 in the survivors reflected adequate ventilation, perfusion, and lung aeration. Thus, VCO2 has the potential to be a useful respiratory parameter that provides valuable information during neonatal resuscitation.
PECO2 is the partial pressure of exhaled CO2 and is a continuous, non-invasive measurement. Since the physiological dead space/tidal volume (VD/VT) ratio is never zero [18], PECO2 is always lower than the ETCO2 [19]. With poor ventilation to perfusion matching, VD/VT increases, regardless of whether mismatching is due to uneven perfusion, uneven ventilation, or a mixture of uneven perfusion and uneven ventilation, causing a lower PECO2. Thus, PECO2 is reduced under all conditions of uneven ventilation/perfusion [18]. In the case of ventilation mismatch, PECO2 is dilute relative to ETCO2, and the PECO2/ETCO2 ratio is reduced [18]. In the case of reduced or maldistributed pulmonary blood flow without airway defects, both PECO2 and ETCO2 would be reduced, resulting in a near normal PECO2/ETCO2 ratio [18]. To our knowledge, no studies regarding monitoring PECO2 have been done during CPR or within the neonatal population. Piglets in the current study that successfully achieved ROSC had significantly higher PECO2 levels in the latter portion of CPR (Fig 2B), indicating sufficient gas exchange was occurring. Low levels of PECO2 can only be attributed to poor or low quality of ventilation during CPR, while depressed levels of both PECO2 and ETCO2 may signify inadequate pulmonary perfusion due to poor circulation. These findings may have important clinical use; by continuously analyzing PECO2 and ETCO2 during CPR, resuscitators can determine changes in ventilation or perfusion and adjust ventilation to improve in this context.
In the delivery room pulse oximetry is used to measure oxygen saturation (SpO2) to titrate oxygen delivery and monitor heart rate [2]. Pulse oximetry can be used to immediately after birth and, in the majority of cases, heart rate and oxygen saturation are displayed within 90 seconds [19–21]. However, in situations of poor peripheral perfusion (e.g. cardiac arrest or severe bradycardia) reliable signals are not always achieved and therefore relying on pulse oximetry to asses the adequacy of CC can be misleading [18]. Therefore measurements of ETCO2, PECO2, and VCO2 allow resuscitators to assess the quality of their resuscitation and assess changes in ventilation or perfusion [3,22]. Low SpO2 values cannot differentiate between poor ventilation and poor perfusion. In addition, no study in newborns has assessed if changes in pulse oximetry waveforms can be used to predict ROSC. In summary, correctly applied pulse oximetry together with capnometry will aid the resuscitator to improve resuscitation performance.
The blood flow at the common carotid artery can serve as a good surrogate of cerebral blood flow in feto-neonatal animals [23]. It has been well documented that cerebral blood flow is related to the arterial partial pressure of CO2 (PaCO2) [24]. In fact, an increase in cerebral blood flow is caused by an increase in PaCO2 [24]. We measured a significantly higher CABF and CI in the surviving group, which demonstrates increased PaCO2 and augmented antegrade blood flow just 40 seconds after CC was initiated. This is of clinical importance; by combining this information with capnometry, we can start to assess the quality of CC, attempt to enhance resuscitation efforts to improve ETCO2 and PECO2 levels, and increase the probability of achieving ROSC within the first minute of resuscitation. If prolonged CPR efforts are given and there is no evidence that ROSC could be attained, it may be appropriate to cease resuscitation after considering all other factors.
Limitations
All piglets had already undergone fetal to neonatal transition, which limits the applicability to delivery room resuscitation. However, recent studies demonstrated that exhaled CO2 could be measured during neonatal transition to guide ventilation [16,22,25]. All piglets were anesthetized and sedated, which differs from delivery room resuscitations. Piglets were intubated using a tightly sealed endotracheal tube to prevent any endotracheal tube leak, which allowed accurate assessment of gas flow for the purpose of this study, but is not a precise replication of the clinical setting where mask ventilation is normally used. In addition, the ductus arteriosus was ligated in all piglets in order to ensure cardiac output could be accurately assessed by PABF. Despite these limitations, the findings are still relevant because the distribution of cardiac output in the fetus and the post-translational neonate during asphyxia episodes are qualitatively similar [26–28]. Piglets were also given different CC techniques, which may have contributed to overall survival and results [7,8]. Since manual ventilations and CC could cause ETCO2 to fluctuate with the effort of compression and rate of ventilation [15,29], uniform CC and a constant rate of ventilation needs to be delivered to use ETCO2 as a predictor of ROSC [3]. Of note, to reduce the use of animals, the study population came from different experimental series with different CPR strategies. Additionally, acute and chronic illnesses with comorbidities can result in a ventilation/perfusion mismatch, which can limit the accuracy of ETCO2 [30] and may be resolved by using PECO2 as a marker of ventilation/perfusion mismatch in future studies. Of note, our protocol of giving 100% oxygen after 30 seconds of CC and then administrating epinephrine 60 seconds after commencement of CC and thereafter every minute, is not in line with the current resuscitation guidelines for asphyxiated newborn infants.
Conclusion
The secondary outcomes of a swine model of neonatal resuscitation demonstrate that continuously monitoring ETCO2, VCO2, and PECO2 during CC has the potential to be a continuous, non-invasive measurement to indicate ROSC, support prediction of outcomes in newborns requiring CC, and determine whether resuscitation efforts should be discontinued. Furthermore, capnometry during CPR can assist in optimizing resuscitation efforts. Further investigation is required to confirm if PECO2 is a viable indicator of ventilation/perfusion mismatch for the neonatal population.
Supporting Information
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
The authors would like to thank the Laerdal Foundation for Acute Medicine, Norway, (http://www.laerdalfoundation.org) for their support of the current study. ESL was supported in part by the Northern Alberta Clinical Trials and Research Centre, Faculty of Medicine and Dentistry, University of Alberta, and Neonatal Research Fund, Northern Alberta Neonatal Program, Alberta Health Services. MOR is supported by a Fellowship of Molly Towell Perinatal Research Foundation, Edmonton, Alberta, Canada. GMS is a recipient of the Heart and Stroke Foundation/University of Alberta Professorship of Neonatal Resuscitation and a Heart and Stroke Foundation Canada Research Scholarship. No relation with industry exists. Respironics (Philips, Wallingford, CT) and Fisher & Paykel (Auckland, New Zealand) provided a respiratory function monitor and Neopuff T-pieces for the study, respectively. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Wyckoff M, Perlman J, Finer NN, Horbar JD. Cardiopulmonary Resuscitation in Very Low Birth Weight Infants. Pediatrics 2000; 106:618–620. [DOI] [PubMed] [Google Scholar]
- 2.Perlman J, Wyllie J, Kattwinkel J, Atkins DL, Chameides L, Goldsmith JP, et al. Part 11: Neonatal resuscitation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2010; 122(16 Suppl 2):S516–538. 10.1161/CIRCULATIONAHA.110.971127 [DOI] [PubMed] [Google Scholar]
- 3.Chalak L, Barber C, Hynan L, Garcia D, Christie L, Wyckoff M. End-tidal CO2 detection of an audible heart rate during neonatal cardiopulmonary resuscitation after asystole in asphyxiated piglets. Pediatr Res 2011; 69:401–405. 10.1203/PDR.0b013e3182125f7f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callaham M, Barton C. Prediction of outcome of cardiopulmonary resuscitation from end-tidal carbon dioxide concentration. Crit Care Med 1990; 18:358–362. [DOI] [PubMed] [Google Scholar]
- 5.Domsky M, Wilson RF, Heins J. Intraoperative end-tidal carbon dioxide valuesand derived calculations correlated with outcome: prognosis and capnography. Crit Care Med 1995; 23:1497–1503. [DOI] [PubMed] [Google Scholar]
- 6.Falk JL, Rackow EC, Weil MH. End-tidal carbon dioxide concentration during cardiopulmonary resuscitation. N Engl J Med 1988; 318:607–611. [DOI] [PubMed] [Google Scholar]
- 7.Schmölzer GM, O'Reilly M, Labossiere J, Lee TF, Cowan S, Nicoll J, et al. Cardiopulmonary resuscitation with chest compressions during sustained inflations: a new technique of neonatal resuscitation that improves recovery and survival in a neonatal porcine model. Circulation 2013;128:2495–2450. 10.1161/CIRCULATIONAHA.113.002289 [DOI] [PubMed] [Google Scholar]
- 8.Schmölzer GM, O’Reilly M, LaBossiere J, Lee TF, Cowan S, Qin S, et al. 3: 1 Compression to ventilation ratio versus continuous chest compression with asynchronous ventilation in a porcine model of neonatal resuscitation. Resuscitation 2014;85:270–275. 10.1016/j.resuscitation.2013.10.011 [DOI] [PubMed] [Google Scholar]
- 9.Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 2010;8:e1000412 10.1371/journal.pbio.1000412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nicoll J, O’Reilly M, Labossiere J, Lee TF, Cowan S, Bigam DL, et al. Effect of cardiac output changes on exhaled carbon dioxide in newborn piglets. Resuscitation 2013;84:1439–1442. 10.1016/j.resuscitation.2013.05.004 [DOI] [PubMed] [Google Scholar]
- 11.Li ES, Cheung PY, Pichler G, Aziz K, Schmölzer GM. Respiratory function and near infrared spectroscopy recording during cardiopulmonary resuscitation in an extremely preterm newborn. Neonatology 2014;105:200–204. 10.1159/000357609 [DOI] [PubMed] [Google Scholar]
- 12.Weil MH, Bisera J, Trevino RP, Rackow EC. Cardiac output and end-tidal carbon dioxide. Crit Care Med 1985; 13:907–909. [DOI] [PubMed] [Google Scholar]
- 13.Trevino RP, Bisera J, Weil MH, Rackow EC, Grundler WG. End-tidal CO2 as a guide to successful cardiopulmonary resuscitation: a preliminary report. Crit Care Med 1985; 13:910–911. [DOI] [PubMed] [Google Scholar]
- 14.Garnett AR, Ornato JP, Gonzalez ER, Johnson EB. End-tidal carbon dioxide monitoring during cardiopulmonary resuscitation. JAMA 1987; 257:512–515. [PubMed] [Google Scholar]
- 15.Kern KB, Sanders AB, Voorhees WD, Babbs CF, Tacker WA, Ewy GA. Changes in expired end-tidal carbon dioxide during cardiopulmonary resuscitation in dogs: a prognostic guide for resuscitation efforts. J Am Coll Cardiol 1989; 13:1184–1189. [DOI] [PubMed] [Google Scholar]
- 16.Palme-Kilander C, Tunell R. Pulmonary gas exchange during facemask ventilation immediately after birth. Arch Dis Child 1993;68:11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kang L, Cheung PY, Pichler G, O’Reilly M, Aziz K, Schmölzer GM. Monitoring lung aeration during respiratory support in preterm infants at birth. PLOS ONE 2014; 9:e102729 10.1371/journal.pone.0102729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hansen J, Ulubay G, Chow B, Sun X-G, Wasserman K. Mixed-expired and end-tidal CO2 distinguish between ventilation and perfusion defects during exercise testing in patients with lung and heart diseases. Chest 2007; 132:977–983. [DOI] [PubMed] [Google Scholar]
- 19.Rabi Y, Dawson JA. Oxygen therapy and oximetry in the delivery room. Semin Fetal Neonatal Med 2013;18:330–5. 10.1016/j.siny.2013.08.007 [DOI] [PubMed] [Google Scholar]
- 20.Dawson JA, Kamlin COF, Wong C, Pas te A, Vento M, Cole TJ, et al. Changes in heart rate in the first minutes after birth. Arch Dis Child Fetal Neonatal 2010;95:F177–81. [DOI] [PubMed] [Google Scholar]
- 21.Dawson JA, Kamlin COF, Vento M, Wong C, Cole TJ, Donath S, et al. Defining the reference range for oxygen saturation for infants after birth. Pediatrics 2010;125:e1340–7. 10.1542/peds.2009-1510 [DOI] [PubMed] [Google Scholar]
- 22.Van Os S, Cheung PY, Pichler G, Aziz K, OReilly M, Schmölzer GM. Exhaled carbon dioxide can be used to guide respiratory support in the delivery room. Acta Paediatr 2014;103:796–806 10.1111/apa.12650 [DOI] [PubMed] [Google Scholar]
- 23.Gratton R, Carmichael L, Homan J, Richardson B. Carotid arterial blood flow in the ovine fetus as a continuous measure of cerebral blood flow. J Soc Gynecol Investig 1996;3:60–65. [DOI] [PubMed] [Google Scholar]
- 24.Grubb RL, Raichle ME, Eichling JO, Ter-Pogossian MM. The effects of changes in PaCO2 cerebral blood volume, blood flow, and vascular mean transit time. Stroke 1974;5:630–639. [DOI] [PubMed] [Google Scholar]
- 25.Hooper SB, Fouras A, Siew ML, Wallace MJ, Kitchen MJ, te Pas AB, et al. Expired CO2 levels indicate degree of lung aeration at birth. PLoS One 2013;8:e70895 10.1371/journal.pone.0070895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Behrman RE, Lees MH, Peterson EN, De Lannoy CW, Seeds AE. Distribution of the circulation in the normal and asphyxiated fetal primate. Am J Obstet Gynecol 1970; 108:956–969. [DOI] [PubMed] [Google Scholar]
- 27.Cohn HE, Sacks EJ, Heymann MA, Rudolph AM. Cardiovascular responses to hypoxemia and acidemia in fetal lambs. Am J Obstet Gynecol 1974; 120:817–824. [DOI] [PubMed] [Google Scholar]
- 28.Leffler CW, Busija DW, Beasley DG, Fletcher AM, Green RS. Effects of indomethacin on cardiac output distribution in normal and asphyxiated piglets. Prostaglandins 1986; 31:183–190. [DOI] [PubMed] [Google Scholar]
- 29.Steedman DJ, Robertson CE. Measurement of end-tidal carbon dioxide concentration during cardiopulmonary resuscitation. Arch Emerg Med 1990; 7:129–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LaValle TL, Perry AG. Capnography: assessing end-tidal CO2 levels. Dimens Crit Care Nurs 1995; 14:70–77. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.