Abstract
Previous research has identified several individual-level factors that modify the risk of childhood trauma on adult psychiatric symptoms, including symptoms of major depression (MD) and posttraumatic stress (PTS). Neighborhood-level factors also influence the impact of individual-level exposures on adult psychopathology. However, no prior studies to our knowledge have explored cross-level interactions between childhood trauma and neighborhood-level factors on MD and PTS symptoms. The purpose of this study was therefore to explore cross-level interactions between a neighborhood-level factor – neighborhood-level crime – and childhood trauma on MD and PTS symptoms. Participants in this study (N = 3,192) were recruited from a large public hospital, and completed self-report inventories of childhood trauma and MD and PTS symptoms. Participant addresses were mapped onto 2010 census tracts, and data on crime within each tract was collected. Multilevel models found a significant cross-level interaction between childhood trauma and neighborhood crime on MD symptoms, such that the influence of high levels of childhood trauma on MD symptoms was enhanced for participants living in high-crime neighborhoods. Supplementary analyses found variation in the strength of cross-level interaction terms by types of childhood trauma and crime, with the strongest associations including emotional neglect paired with personal and property crime. The results provide preliminary support for interventions that help childhood trauma survivors find housing in less vulnerable neighborhoods and build skills to cope with neighborhood crime.
Keywords: Childhood trauma, major depression, posttraumatic stress, neighborhood crime, cross-level interaction, multilevel modeling
Exposure to childhood trauma is a robust predictor of psychiatric disorders in adulthood (e.g., Fergusson, Boden, & Horwood, 2008; Heim, Shugart, Craighead, & Nemeroff, 2010). For example, a recent review of 44 articles published from 2001 to 2011 found that five forms of childhood trauma (physical, sexual, and emotional abuse, and emotional and physical neglect) have each been associated with a range of adult psychiatric disorders, among them major depressive disorder (MDD) and posttraumatic stress disorder (PTSD) (Carr, Martins, Stingel, Lemgruber, & Juruena, 2013). Childhood trauma has also shown a dose-response effect relationship with psychiatric symptoms in adulthood, such that persons who experienced more severe childhood trauma and multiple forms of childhood trauma are at increased risk for more severe symptoms (Clemmons, Walsh, DiLillo, & Messman-Moore, 2007).
Not all childhood trauma survivors experience psychiatric disorders in adulthood, however. A longitudinal, epidemiologic study, for example, found that although child abuse survivors were at increased risk of having at least one Axis I psychiatric disorder in adulthood relative to other participants, 45.5% of survivors did not meet criteria for any disorder (Collishaw et al., 2007). Efforts to identify factors that enhance or attenuate the risk associated with exposure to childhood trauma could yield important implications for efforts to reduce its mental health burden. Several individual-level moderating factors have been identified to date, including genetic variants and recent stressful life events as risk-enhancing factors (McLaughlin, Conron, Koenen, & Gilman, 2010; Nugent, Tyrka, Carpenter, & Price, 2011), and social support, attachment, and a resilient coping style as risk-attenuating factors (Aspelmeier, Elliott, & Smith, 2007; Roy, Carli, & Sarchiapone, 2011; Sperry & Widom, 2013).
In addition to these individual-level factors, it is likely that characteristics of neighborhoods modify the risk associated with childhood trauma. This is consistent with an ecological perspective on mental health, which posits that mental health is influenced by factors at multiple levels, from individual characteristics and experiences to characteristics of broader sociocultural context, as well as interactions been them (e.g., Bronfenbrenner, 1979; Glass & McAtee, 2006). A large body of research indicates a host of neighborhood-level factors, such as concentrated disadvantage, residential instability, and crime, increase the risk for both childhood trauma exposure and adverse mental health outcomes across the lifespan (e.g., Coulton, Crampton, Irwin, Spilsbury, & Korbin, 2007; Garbarino & Sherman, 1980; Klebanov, Brooks-Gunn, & Duncan, 1994; Leventhal & Brooks-Gunn, 2000). In addition, several studies to date have documented interactions between contemporaneous individual- and neighborhood-level factors in shaping risk for adult psychopathology (Rajaratnam, O'Campo, Caughy, & Mutaner, 2008; Wind & Komproe, 2012). For example, a large study of community-dwelling adults found that the impact of individual-level violence exposure on the likelihood of suffering a depressive or anxiety disorder was enhanced for participants living in high-crime neighborhoods (Stockdale et al., 2007). No published study to our knowledge has explored interactions between individual-level childhood trauma exposure and neighborhood-level factors, including neighborhood-level crime.
Although this issue has not been explored empirically, the presence of cross-level interactions between childhood trauma exposure and neighborhood-level crime could depend in part on both the type of childhood trauma and the nature of the crime. In this vein, the same study of community-dwelling adults found that the impact of lower individual-level social support on the probability of disorder was greater among participants living in communities with higher social isolation, as indicated by lower household occupancy (Stockdale et al., 2007). In contrast, the cross-level interactions between individual-level violence exposure and neighborhood-level social isolation, and between individual-level support and neighborhood-level crime were non-significant, providing preliminary evidence that cross-level interactions might be limited to scenarios wherein the individual- and neighborhood-level exposures are similar in nature.
Current Study
The primary purpose of the current study was to explore cross-level interactions between individual-level childhood trauma and neighborhood-level crime on major depression (MD) and posttraumatic stress (PTS) symptoms among a sample of adults recruited from a large, urban public hospital. Since no prior studies have explored this topic empirically, these analyses were best conceptualized as exploratory. Nonetheless, we hypothesized that the impact of childhood trauma on MD and PTS symptoms would be enhanced for participants living in higher-crime neighborhoods. Secondarily, we examined variation in patterns of significance for cross-level interactions by the type of childhood trauma (physical, sexual, and emotional abuse, and emotional and physical neglect) and type of crime (personal and property crime) in predicting MD and PTS symptoms. These analyses were, again, exploratory, but we hypothesized that the trends in the data would suggest stronger interactions when the childhood trauma and crime were more similar in nature. For example, we suspect that the interaction would be stronger when individual-level physical abuse was paired with personal crime than with property crime.
Method
Participants and Procedures
Participants in this study were part of a large ongoing study of patients at a public hospital in Atlanta, Georgia, and were recruited from waiting rooms in the primary care and obstetrics gynecology clinics. Participants completed a battery of survey instruments, including measures of childhood trauma, and MD and PTS symptoms. The survey was administered verbally due to the relatively high rates of impaired literacy in the study community. The battery took between 30 and 90 minutes to complete, participants were paid $15 for their participation, and participant home addresses were collected. As reported elsewhere [masked for blind review], the lifetime prevalence of childhood trauma, MDD and PTSD among participants in the larger study are elevated compared to estimates from nationally representative studies. The initial sample for the current study included the first 4,000 participants who provided home addresses. The [masked for blind review] Institutional Review Boards approved the study, and participants provided written informed consent.
The 4,000 addresses were fully de-identified, cleaned and parsed to facilitate geocoding using either the Navteq Address Points and Address Range databases, or the US Census Tiger 2010 Street Address Range database. Of these, 174 addresses were dropped from the current study due to being (a) incomplete or invalid (n = 146), (b) located outside of the 20-county study area (n = 12), or (c) identified as a duplicate case (n = 17). This resulted in a total of 3,826 participants with valid addresses. Of these 3,826 participants, 634 were dropped due to missing data on one or more of the variables included in the study. The final sample consisted of 3,192 participants residing in 413 census tracts.
Measures
Childhood trauma history
Childhood trauma history with assessed with the Childhood Trauma Questionnaire-Short Form (CTQ-SF; Bernstein et al., 2003). The CTQ-SF consists of 25 items, with five items assessing five different subtypes of childhood trauma experienced prior to age 11: physical abuse (e.g., “people in my family hit me so hard that it left me with bruises and marks”), sexual abuse (e.g., “someone molested me”), emotional abuse (e.g., “people in my family said hurtful or insulting things to me”), emotional neglect (e.g., “there was someone in my family that helped me feel that I was important or special,” reverse coded) and physical neglect (e.g., “I had to wear dirty clothes”). Participants rated items on a scale from 1 (never true) to 5 (very often true), and subscale and full-scale scores were calculated as the sum of responses. The CTQ-SF is a commonly used measure for retrospective assessment of childhood trauma and has been shown to have good internal consistency across diverse samples (Bernstein et al., 2003). In the current study, Cronbach's alpha reliability for the CTQ-SF full scale was .93, and ranged from .67 to .94 for the five CTQ-SF subscales.
Neighborhood-level crime
Data on neighborhood-level crime were collected from CrimeRisk 2010 (Applied Geographic Solutions, 2010). Data on the total levels of crime, as well as levels of the two subtypes that comprise total crime (personal crime – e.g., murder, rape; and property crime – e.g., larceny, motor vehicle theft) were collected for the 413 census tracts (year 2010) in which the participants lived. Crime levels are relative to the national average, which is set at 100. For example, a value of 200 would mean that the tract had twice the amount of crime as the national average, and a value of 50 would mean that the tract had half the amount of crime as the national average. To facilitate interpretation of the main and interactive effects of neighborhood-level crime, we divided this variable by its interquartile range (IQR = 308) for the 413 census tracts represented in the study.
Posttraumatic stress symptoms
PTS symptoms were assessed via the Posttraumatic Symptom Scale-Interview Version (PSS-I; Foa, Riggs, Dancu, & Rothbaum, 1993). The PSS consists of 17 items corresponding to the symptoms of PTSD as specified in the Diagnostic and Statistical Manual of Mental Disorders (4th edition, text revision; DSM-IV-TR; American Psychiatric Association, 2000). Participants rated the extent to which they experienced each symptom (e.g., “Have you been having recurrent bad dreams or nightmares about the trauma?”) over the prior two weeks from 0 (not at all) to 3 (5 or more times per week), and a symptom severity score was computed as the sum of all ratings. The PSS-I has been shown to have high internal consistency, inter-rater reliability, and validity (Foa & Tolin, 2000). Cronbach's alpha in the current study was .92.
Major depression symptoms
The Beck Depression Inventory-II (BDI; Beck, Steer, & Brown, 1996) was used to assess MD symptoms. The BDI consists of 21 items corresponding to DSM-IV symptoms of major depression. For each item, participants indicate which of four statements best describes the way they have been feeling over the past two weeks. Each statement has a corresponding score, ranging from 0 (e.g., “I do not feel sad”) to 3 (e.g., “I am so sad or unhappy that I can't stand it”). A symptom severity score was computed as the sum of all ratings. The BDI-II has had evidence of reliability, internal consistency, and validity across a wide variety of samples, including primary care medical patients (Arnau, Meagher, Norris, & Bramson, 2001). Cronbach's alpha in the current study was .93.
Statistical Analysis
Data management and descriptive analysis was performed in SPSS 20.0 (IBM Corp., 2011). We first assessed differences on all variables included in the study between complete cases and cases that were dropped due to missing data using Bonferroni-corrected one-way analyses of variance (ANOVAs) and chi-square analyses of the individual-level data file. For descriptive purposes, we also constructed a series of maps in ArcGIS (ESRI, 2011) to illustrate the geographic study area and distribution of key variables across census tracts. Maps displaying levels of key variables were constructed for tracts with five or more participants both to protect participants’ privacy and ensure adequate representation. Bivariate relationships between all variables in the main analysis were then computed as correlations for factors at the same level (i.e, between two individual-level factors), and as multilevel regression weights for factors at different levels (i.e., between one individual-level and one neighborhood-level factor).
Multilevel multivariable models to fulfill the primary study aim were then conducted in Mplus 7.1 (Muthén & Muthén, 1998-2012). First, main effects of individual-level childhood trauma and neighborhood-level crime on PTS and MD symptoms were tested (Model 1). Second, the cross-level interaction between childhood trauma and crime was entered (Model 2). All models controlled for demographic characteristics (age, gender, non-Hispanic Black race), as well as comorbid symptoms (PTS symptoms for the models predicting MD symptoms, and MD symptoms for the models predicting PTS symptoms). Unstandardized coefficients are presented in results, as standardized values are unavailable for multilevel models in Mplus 7.1. To fulfill the secondary aim of the study, we conducted supplementary analyses assessing the significance levels of the cross-level interactions between each childhood trauma subscale and each type of crime in predicting MD and PTS symptoms, again controlling for demographic characteristics, comorbid symptoms, and main effects of childhood trauma and crime. Significance levels of the cross-level interaction terms are presented, and the full set of these results is available upon request.
Results
Descriptive and Bivariate Analyses
Table 1 presents individual- and neighborhood-level descriptive data. For the CTQ-SF subscales, we noted that participants on average had the highest scores for emotional neglect, and the lowest scores for physical neglect. For the neighborhood-level crime data, we noted that the levels of total, personal, and property crime were higher than the national average, ranging from 2.12 times the national average for personal crime to 2.38 times the national average for total crime. However, there was substantial variation around each of the means.
Table 1.
Descriptive Data for Study Variables
| M (SD) or % | Range | |
|---|---|---|
| Individual-level (N = 3192) | ||
| Age | 39.98 (13.82) | 18-75 |
| Female gender | 70.4% | -- |
| Non-Hispanic Black | 94.1% | -- |
| Childhood trauma – Total | 40.39 (17.09) | 25-121 |
| Childhood trauma – Sexual abuse | 7.63 (4.97) | 5-25 |
| Childhood trauma – Physical abuse | 8.00 (3.88) | 5-25 |
| Childhood trauma – Emotional abuse | 8.80 (4.75) | 5-25 |
| Childhood trauma – Emotional neglect | 9.01 (4.87) | 5-25 |
| Childhood trauma – Physical neglect | 6.95 (3.09) | 5-24 |
| PTS symptoms | 12.51 (12.28) | 0-51 |
| MD symptoms | 14.05 (11.99) | 0-59 |
| Neighborhood-level (N = 413) | ||
| Total crime | 238.25 (229.12) | 2-892 |
| Personal crime | 212.06 (236.35) | 3-980 |
| Property crime | 233.06 (222.95) | 1-974 |
Note. M = Mean; SD = Standard Deviation; PTS = Posttraumatic Stress; MD = Major Depression.
Bonferroni-corrected independent-samples t-tests and chi-square tests found that participants dropped due to missing data lived in neighborhoods with significantly higher levels of total, personal, and property crime.
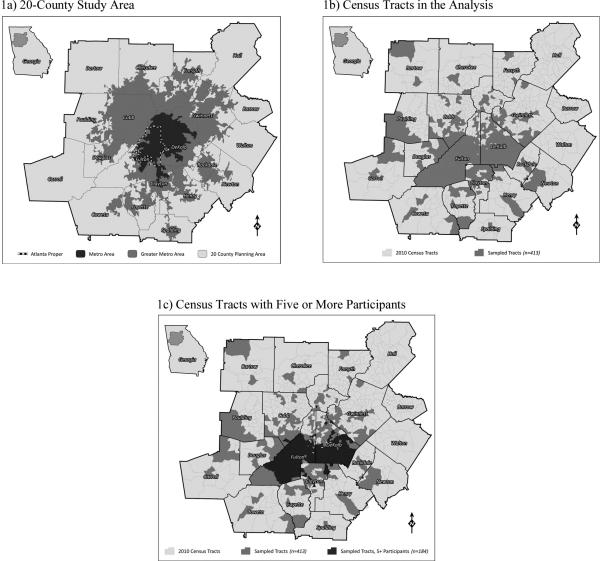
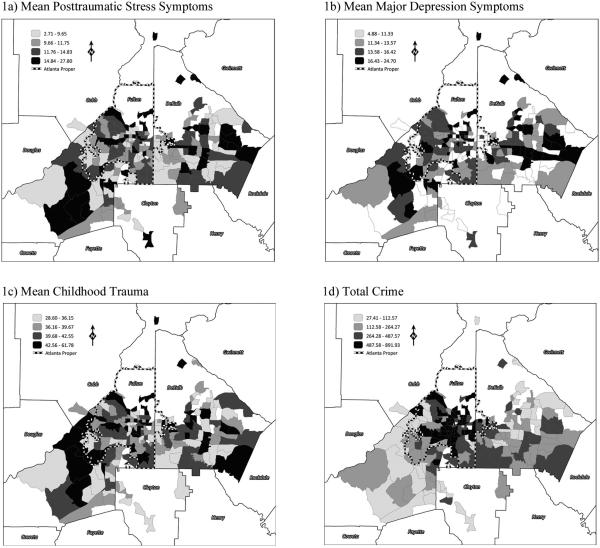
Figure 1 shows (a) the 20-county study area within Georgia, (b) the 413 census tracts represented in the analysis, and (c) the 184 census tracts with five or more participants included in the analysis. In Figure 2, we show levels of (a) mean PTS symptoms, (b) mean MD symptoms, (c) mean childhood trauma, and (d) total crime within each of the 184 tracts. Quartiles were used to define four levels for each factor across the 184 tracts. Lighter shading on the maps was used to represent tracts with lower levels of each factor, and darker shading to represent tracts with higher levels. In reviewing these maps, we noted that there was substantial overlap in levels of mean PTS symptoms (Figure 2a), mean MD symptoms (Figure 2b), and mean childhood trauma (Figure 2c), and that overall the patterns of shading across these maps were very similar. For example, tracts with the highest levels of mean PTS symptoms also tended to have the highest levels of mean MD symptoms and mean childhood trauma – that is, the tracts with the darkest shading for one factor tended to have the darkest shading for the other two factors. In contrast, we observed that the geographic distribution of total crime did not seem to align with those of the other three outcomes, and the tracts with the highest levels of total crime (represented by the darkest shading) were concentrated in Atlanta proper.
Figure 1. Maps showing study area.
Maps of (a) the 20-county study area, (b) the 413 census tracts represented in the analysis, and (c) 184 census tracts with five or more participants.
Figure 2. Maps showing study variables.
Levels of (a) mean posttraumatic stress (PTS) symptoms, (b) mean major depression (MD) symptoms, (c) mean childhood trauma, and (d) total crime for the 184 census tracts with five or more study participants. For each factor, four levels were defined by quartiles for the 184 census tracts. Lighter shading is used to represent lower levels of each factor, and darker shading to represent higher levels. PTS symptoms were assessed via the Posttraumatic Symptom Scale-Interview Version (PSS-I; Foa, Riggs, Dancu, & Rothbaum, 1993), with possible scale scores ranging from 0 to 51. MD symptoms were assessed via the Beck Depression Inventory-II (BDI; Beck, Steer, & Brown, 1996), with possible scale scores ranging from 0 to 63. Childhood trauma was assessed with the Childhood Trauma Questionnaire-Short Form (CTQ-SF; Bernstein et al., 2003), with possible scale scores ranging from 25 to 125. Data on total crime was collected from CrimeRisk 2010 (Applied Geographic Solutions, 2010) and are relative to the national average (set at 100).
Bivariate relationships between all variables in the study are shown in Table 2. At the bivariate level, childhood trauma was significantly associated with PTS and MD symptoms, whereas total crime was not.
Table 2.
Bivariate Relationships between Variables Included in the Main Analysis
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Age | -- | ||||||
| 2. Female gender | −.23*** | -- | |||||
| 3. Non-Hispanic Black | −.02 | .05 | -- | ||||
| 4. Childhood trauma – Total | > − .01 | .10*** | −.08*** | -- | |||
| 5. PTS symptoms | .01 | .02 | −.07*** | .47*** | -- | ||
| 6. MD symptoms | .05** | .06** | −.05** | .45*** | .69*** | -- | |
| 7. Total crime | .19 | −.15 | .02 | .27 | .26 | .16 | -- |
Note. N = 3,192 participants nested in 413 census tracts. PTS = Posttraumatic Stress; MD = Major Depression. Bivariate relationships between individual-level variables (1-6) were assessed using correlation analysis. Bivariate relationships between individual-level variables (1-6) and the neighborhood-level variable (7) assessed through multilevel regression models, and standardized estimates are presented.
p < .01
p < .001.
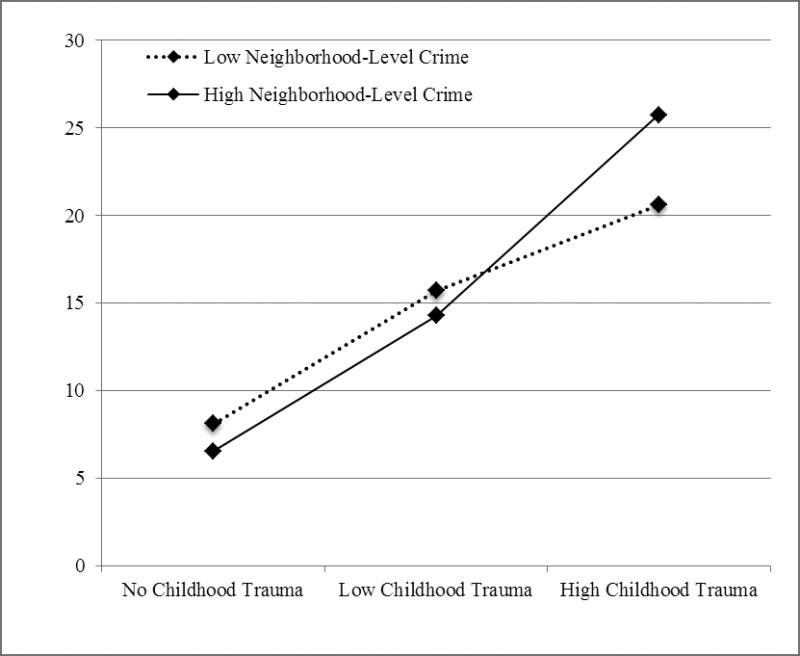
Multilevel Multivariable Models
Table 3 shows the results of the multilevel multivariable models. In Model 1 for MD symptoms, significant predictors of higher symptoms were female gender, older age, higher PTS symptoms, and higher childhood trauma at the individual-level, whereas neighborhood-level total crime was non-significant. In Model 2 for MD symptoms, the cross-level interaction between individual-level childhood trauma and neighborhood-level crime was significant (p = .04). To illustrate the interaction, mean levels of MD symptoms were computed in the individual-level data file for participants with high levels of childhood trauma (defined as one standard deviation or more above the mean), low levels of childhood trauma (defined as within one-half standard deviation of the mean), and no childhood trauma (defined as a CTQ-total score of 25, the lowest score possible), living in neighborhoods with high versus low levels of crime (defined as one standard deviation or more above or below the mean, respectively). As shown in Figure 3, for participants with no and low childhood trauma, there were similar levels of MD symptoms among participants living in high- versus low-crime neighborhoods. In contrast, for participants with high levels of childhood trauma, those living in high-crime neighborhoods had higher MD symptoms than those living in low-crime neighborhoods.
Table 3.
Results of Multilevel Regression Analyses Predicting Posttraumatic Stress and Major Depression Symptoms
| MD Symptoms |
PTS Symptoms |
|||
|---|---|---|---|---|
| Model 1 Est. (SE) | Model 2 Est. (SE) | Model 1 Est. (SE) | Model 2 Est. (SE) | |
| Individual-level | ||||
| Female gender | 1.05 (.35)** | .76 (.34)* | −1.48 (.36)*** | −1.33 (.36)*** |
| Age | .05 (.01)*** | .03 (.01)** | −.06 (.01)*** | −.05 (.01)*** |
| Non-Hispanic Black | .39 (.63) | −.71 (.66) | −3.36 (.73)*** | −2.55 (.71)*** |
| Comorbid symptomsa | .59 (.02)*** | .59 (.02)*** | .61 (.02)*** | .61 (.02)*** |
| Childhood trauma – Total | .11 (.01)*** | .08 (.02)*** | .13 (.01)*** | .17 (.02)*** |
| Neighborhood-level | ||||
| Total Crime | .04 (.21) | −.01 (.22) | −.08 (.19) | −.05 (.19) |
| Cross-level | ||||
| Childhood trauma – Total × Total Crime | -- | .06 (.03)* | -- | −.02 (.01) |
Note. N = 3,192 participants nested in 413 census tracts. PTS = Posttraumatic Stress; MD = Major Depression; Est. = Estimate; SE = Standard Error.
Comorbid symptoms were PTS symptoms in the models predicting MD symptoms, and MD symptoms in the models predicting PTS symptoms.
p < .05
p < .01
p < .001.
Figure 3. Illustration of the cross-level interaction between childhood trauma and neighborhood-level crime on Major Depression symptoms.
High levels of childhood trauma, and high and low levels of crime were defined as one standard deviation or more above or below the mean, respectively. Low levels of childhood trauma were defined as being within one-half standard deviation of the mean. The figure presents mean levels of Major Depression symptoms computed with individual-level data. Subsample sizes: No Childhood Trauma-Low Neighborhood-level Crime, n = 65; Low Childhood Trauma-Low Neighborhood-Level Crime, n = 201; High Childhood Trauma-Low Neighborhood-level Crime, n = 78; No Childhood Trauma-High Neighborhood-level Crime, n = 68; Low Childhood Trauma-High Neighborhood-Level Crime, n = 169; High Childhood Trauma-High Neighborhood-level Crime, n = 90.
In Model 1 for PTS symptoms of the multilevel results (Table 3), male gender, younger age, higher MD symptoms, and higher childhood trauma were significantly associated with higher PTS symptoms, and non-Hispanic Black race was significantly associated with lower PTS symptoms. At the neighborhood-level total crime was not significantly associated with PTS symptoms. In Model 2, the cross-level interaction was a non-significant predictor of PTS symptoms.
Supplementary Analysis: Childhood Trauma and and Crime Subtypes
The significance levels of the interaction terms for analyses with different combinations of childhood trauma and crime subtypes are listed in Table 4. For MD symptoms, the significant interaction including total childhood trauma was significant with personal crime, and the significant interaction including total crime was significant with the emotional neglect subscale. The interaction including the emotional neglect subscale was also a significant predictor of MD symptoms with personal and property crime. All other cross-level interaction terms were non-significant.
Table 4.
Significance levels of Interaction between Childhood Trauma and Neighborhood-Level Crime Subtypes in Secondary Analyses
| Total Crime | Personal Crime | Property Crime | |
|---|---|---|---|
| Major Depression Symptoms | |||
| Childhood trauma – Total | .04 | .04 | .05a |
| Childhood trauma – Sexual abuse | .45 | .30 | .73 |
| Childhood trauma – Physical abuse | .12 | .13 | .16 |
| Childhood trauma – Emotional abuse | .08 | .08 | .12 |
| Childhood trauma – Emotional neglect | .01 | .01 | .01 |
| Childhood trauma – Physical neglect | .25 | .39 | .17 |
| Posttraumatic Stress Symptoms | |||
| Childhood trauma – Total | .14 | .19 | .12 |
| Childhood trauma – Sexual abuse | .94 | .90 | .98 |
| Childhood trauma – Physical abuse | .35 | .41 | .34 |
| Childhood trauma – Emotional abuse | .37 | .46 | .32 |
| Childhood trauma – Emotional neglect | .02 | .03 | .02 |
| Childhood trauma – Physical neglect | .06 | .15 | .03 |
Note. N = 3,192 participants nested in 413 census tracts. Analyses controlled for age, female gender, non-Hispanic Black race, comorbid symptoms, and main effects of childhood trauma and crime. For clarity, significance levels below .05 are shown in boldface.
p = .053.
For PTS symptoms, the interaction including total childhood trauma was non-significant with personal and property crime, whereas the interaction including total crime was significant with the emotional neglect subscale. The emotional neglect subscale was also significant with personal and property crime, and the physical neglect subscale was significant with property crime. Supplementary analyses (not shown) indicated the same pattern of results for all significant interactions – that is, that the impact of high childhood trauma on symptoms was enhanced for participants living in neighborhoods with high levels of crime.
Discussion
This study explored whether neighborhood-level crime modified the risk for MD and PTS symptoms associated with childhood trauma among a large sample of urban adults. Through multilevel modeling, we found a significant cross-level interaction for MD symptoms, such that the influence of high levels of childhood trauma on MD symptoms was enhanced for participants living in neighborhoods with high levels of total crime. Secondary analyses found variation in significance levels for different combinations of childhood trauma and crime subtypes, with statistically significant cross-level interactions when emotional neglect was paired with total, personal, and property crime. In addition, although the cross-level interaction between total childhood trauma and total crime was a non-significant predictor of PTS symptoms, the cross-level interactions when emotional neglect was paired with total, personal, and property crime, and when physical neglect was paired with property crime reached statistical significance. Taken together, the results suggest that living in a high-crime neighborhood can increase childhood trauma survivors’ risk for MD and PTS symptoms, depending upon the type of childhood trauma experienced and nature of the crime.
The results align with prior research showing childhood trauma as a robust predictor of adult mental health (e.g., Carr et al., 2013). Indeed, although the significant cross-level interaction showed that living in a high-crime neighborhood enhanced the risk associated with higher childhood trauma, the main effects of childhood trauma on PTS and MD symptoms across neighborhoods remained evident. Nonetheless, this study adds neighborhood-level crime to the growing list of factors that modify the association between childhood trauma and adult mental health (e.g., McLaughlin et al., 2009; Sperry & Widom, 2013), and moreover, shows that such factors are not limited to the individual-level.
The results are also consistent with prior research showing that neighborhood-level factors modify the risk associated with individual-level exposures (e.g., Rajaratnam et al., 2008), and the previous study showing a cross-level interaction specifically with neighborhood-level crime (Stockdale et al., 2007). Notably, this is the first study to our knowledge to document a cross-level interaction with childhood trauma as the individual-level exposure. Future research is needed to understand the mechanisms underlying this finding – that is, why living in a neighborhood with high crime would enhance high childhood trauma survivors’ risk for MD symptoms. One possibility could be that living in a high-crime neighborhood enhances survivors’ sense of hopelessness, triggering negative core beliefs about oneself, other people and the world and thereby augmenting MD symptoms (Cukor & McGinn, 2006). Another possibility is that persons living in high-crime neighborhoods face a general increased risk for assaultive violence and other traumatic events and stressors, and that these individual-level experiences trigger the negative mental health impact of high childhood trauma. This explanation would also be consistent with the concept of stress sensitization, wherein persons who have experienced childhood trauma are at higher risk of psychopathology after exposure to further traumatic events (McLaughlin et al., 2010). Finally, the cross-level interaction could be influenced in part by selection effects – that is, persons who have experienced high levels of childhood trauma are more likely to reside in high-crime neighborhoods, perhaps due in part to the socioeconomic difficulties that childhood trauma survivors are more likely to encounter (Zielinski, 2009). Notably, however, in our bivariate analysis, we found that the cross-level association between childhood trauma and neighborhood crime was non-significant.
Future research is also needed to understand why the mental health of high childhood trauma survivors might be more sensitive to neighborhood-level crime than that of their counterparts. In this vein, studies using Adverse Childhood Experiences Scale (ACES; Dube et al., 2003) suggest that childhood trauma could alter neurobiological mechanisms involved in later stress responses, such as amygdala activity and daily cortisol rhythms (Bublitz & Stroud, 2013; Teicher & Samson, 2013), and accelerated cell aging (Chen et al., 2014). Further research has indicated that the biological correlates of childhood trauma in adulthood might be even more pronounced in the context of current stress, demonstrating the importance of assessing both childhood trauma and current environments in studies of adult psychopathology (Bubliz, Parade, & Stroud, 2014). Our finding that the cross-level interaction was significant for MD, but not PTS, symptoms suggests that the impact of neighborhood crime could have a more general impact on survivors’ mental health, rather than an effect on symptoms tied to a specific traumatic event.
The significant cross-level interaction between neighborhood-level crime and childhood trauma predicting MD symptoms should be interpreted in light of our secondary analyses, which explored variation in significance levels for different combinations of crime and childhood trauma subtypes in predicting MD and PTS symptoms. These results were counter to our expectation that the strongest associations would be for more closely related combinations, such that, for example, the interaction including child sexual abuse would be stronger when paired with personal versus property crimes. Instead, we found that the only interaction terms predicting MD symptoms that remained significant included emotional neglect, paired with total, personal, and property crime. The stronger interactive effect for emotional neglect could be due in part to the greater frequency of its occurrence, reflected by higher CTQ-SF subscale scores, relative to all other subscales. On the other hand, the significant interaction terms for PTS symptoms were not limited to emotional neglect, but rather also included physical neglect, which was the least commonly reported type of childhood trauma. It is therefore possible that emotional neglect specifically increases sensitivity for MD symptoms in response to neighborhood crime, whereas neglect more generally – that is, either emotional or physical neglect – increases sensitivity for PTS symptoms.
Future research could explore whether these trends apply to other neighborhood- and individual-level exposures, as well as the biological and psychosocial mechanisms underlying them. Additional research could also investigate why some types of crime might be more likely to enhance the negative mental health impact of childhood trauma, with potential explanations being variation in rates of different crimes, the extent to which different crimes are reported, community members’ knowledge of different criminal activities in their neighborhood, and effects of such knowledge on perceptions of safety. More generally, further research on cross-level interactions is needed to provide a deeper understanding of the contexts that enhance the long-term psychological effects of childhood trauma and other individual-level exposures. Such findings could potentially yield important insights for clinical and public health interventions, for example by identifying neighborhoods that would be most conducive to childhood trauma survivors’ psychological functioning and coping strategies that could offset the negative impact of living in a high-risk neighborhood.
Several limitations of this study are worth noting. First, childhood trauma was assessed retrospectively and neither prospective nor archival data were available to validate participants’ reports. However, it is worth noting that childhood trauma is most often assessed retrospectively and that a recent study found no difference in the extent to which prospective and retrospective reports of childhood trauma were associated with adult psychopathology (Scott, McLaughlin, Smith, & Ellis, 2012). Second, the reliability of one of the childhood trauma subscales (physical neglect) was low, which could have obscured relationships with MD and PTS symptoms, as well as the strength of interaction terms. Third, MD and PTS symptoms were assessed via self-report measures and in reference to the prior two weeks, and it is possible that the results would not hold if symptoms were assessed via a clinical interview or in reference to a longer period of time. Fourth, the study relied on cross-sectional data, and therefore we were unable to explore such issues as whether cross-level interactions were predictive of changes in symptoms over time. We similarly lacked data on participants’ tenure in their current neighborhoods, as well as the characteristics of other neighborhoods in which they had previously lived. Longitudinal data on neighborhoods could be used in future studies to explore such issues as whether there are dose-response effects of neighborhood-level crime, and whether exposure to neighborhood-level crime in childhood influences reactions to exposure to the same in adulthood. Fifth, neighborhoods were defined by census tracts, which perhaps do not reflect how participants perceive their neighborhoods. The use of census tracts posed some advantages, however, including the availability of data at the census tract level, and greater stability of tract boundaries, versus those of locally defined neighborhoods, over time (Osypuk & Galea, 2007). Finally, the study was conducted in a unique geographic context, the sample was not representative of the study area, and all participants were seeking primary care or obstetrics gynecology services at a public hospital – factors that limit the external validity of the study.
Despite these limitations, the results of the study provide further evidence that neighborhood characteristics can modify the influence of individual-level exposures on psychopathology. In particular, they suggest that living in a high-crime neighborhood can enhance the risk for higher MD and PTS symptoms among childhood trauma survivors, depending in part on the types of neighborhood crime and childhood trauma experienced. The findings provide insight into some of the variability in psychological functioning among childhood trauma survivors, and support for interventions that help survivors identify housing in low-crime neighborhoods and build skills to cope with neighborhood crime.
Acknowledgments
We would like to thank the participants of the Grady Trauma Project as well as the volunteer and staff who have made this important work possible. This work was primarily supported by the National Institutes of Mental Health (T32 MH013043l, R01 MH071537, R01 MH096764, and R01 HD071982). Support was also received from Emory and Grady Memorial Hospital General Clinical Research Center, NIH National Centers for Research Resources (M01RR00039), and Howard Hughes Medical Institute. The contents of this manuscript do not reflect the views of the Department of Veterans Affairs or the United States Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sarah R. Lowe, Department of Psychology, Montclair State University
James W. Quinn, Department of Epidemiology, Columbia University, Mailman School of Public Health
Catherine A. Richards, Hutchinson Institute for Cancer Outcomes Research, Fred Hutchinson Research Center
John Pothen, MD/PhD Program, Emory School of Medicine.
Andrew Rundle, Department of Epidemiology, Columbia University, Mailman School of Public Health.
Sandro Galea, Department of Epidemiology, Boston University School of Public Health.
Kerry J. Ressler, Department of Psychiatry, Emory School of Medicine
Karestan C. Koenen, Department of Society, Human Development, and Health, Harvard T. H. Chan School of Public Health
Bekh Bradley, Atlanta VA Medical Center, Mental Health Service Line, and Department of Psychiatry, Emory School of Medicine..
References
- American Psychological Association . Diagnostic and statistical manual of mental disorders. 4th edition, text revision Author; Washington, DC: 2000. [Google Scholar]
- Applied Geographic Solutions Database methodology guide, 2010A update. 2010 Retrieved from http://www.appliedgeographic.com/ags_2010%20web%20pdf%20files/ags2010amethod ologyguide.pdf.
- Arnau RC, Meagher MW, Norris MP, Bramson R. Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychology. 2001;20:112–119. doi: 10.1037//0278-6133.20.2.112. doi:10.1037/0278-6133.20.2.112. [DOI] [PubMed] [Google Scholar]
- Aspelmeier JE, Elliott AN, Smith CH. Childhood sexual abuse, attachment, and trauma symptoms in college females: The moderating role of attachment. Child Abuse & Neglect. 2007;31:549–566. doi: 10.1016/j.chiabu.2006.12.002. doi: 0.1016/j.chiabu.2006.12.002. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown G. Manual for the Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Zulle W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. doi:10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- Bublitz MH, Parade S, Stroud LR. The effects of childhood sexual abuse on cortisol trajectories in pregnancy are moderated by current family functioning. Biological Psychology. 2014;103:152–157. doi: 10.1016/j.biopsycho.2014.08.014. doi:10.1016/j.biopsycho.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bublitz MH, Stroud LR. Maternal history of child abuse moderates the association between daily stress and diurnal cortisol in pregnancy: A pilot study. Stress. 2013;16:706–710. doi: 10.3109/10253890.2013.825768. doi: 10.3109/10253890.2013.825768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr C, Martins CMS, Stingel AM, Lemgruber VB, Juruena MF. The role of early life stress in adult psychiatric disorders: A systematic review according to childhood trauma subtypes. Journal of Nervous and Mental Disease. 2013;201:1007–1020. doi: 10.1097/NMD.0000000000000049. doi:10.1097/NMD.0000000000000049. [DOI] [PubMed] [Google Scholar]
- Chen SH, Epel ES, Mellon SH, Lin J, Reus VI, Rosser R, Wollkowitz OM. Adverse childhood experiences and leukocyte telomere maintenance in depressed and healthy adults. Journal of Affective Disorders. 2014;169:86–90. doi: 10.1016/j.jad.2014.07.035. doi:10.1176/appi.ajp.2013.12070957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemmons JC, Walsh K, DiLillo D, Messman-Moore TL. Unique and combined contributions of multiple child abuse types and abuse severity to adult trauma symptomatology. Child Maltreatment. 2007;12:172–181. doi: 10.1177/1077559506298248. doi:10.1177/1077559506298248. [DOI] [PubMed] [Google Scholar]
- Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B. Resilience to adult psychopathology following childhood maltreatment: Evidence from a community sample. Child Abuse & Neglect. 2007;31:211–229. doi: 10.1016/j.chiabu.2007.02.004. doi: 0.1016/j.chiabu.2007.02.004. [DOI] [PubMed] [Google Scholar]
- Coulton CJ, Crampton DS, Irwin M, Spilsbury JC, Korbin JE. How neighborhoods influence childhood maltreatment: A review of the literature and alternative pathways. Child Abuse & Neglect. 2007;31:1117–1142. doi: 10.1016/j.chiabu.2007.03.023. doi:10.1016/j.chiabu.2007.03.023. [DOI] [PubMed] [Google Scholar]
- Cukor D, McGinn LK. History of child abuse and severity of adult depression: The mediating role of cognitive schema. Journal of Child Sexual Abuse. 2006;15:19–34. doi: 10.1300/J070v15n03_02. doi: 10.1300/J070v15n03_02. [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111:564–72. doi: 10.1542/peds.111.3.564. doi:10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- ESRI. ArcGIS Desktop: Release 10. Environmental Systems Research Institute; Redlands, CA: 2011. [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse & Neglect. 2008;32:607–619. doi: 10.1016/j.chiabu.2006.12.018. doi:10.1016/j.chiabu.2006.12.018. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–463. doi:10.1002/jts.2490060405. [Google Scholar]
- Foa EB, Tolin DF. A comparison of the PTSD Symptom Scale-Interview Version and the Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 2000;13:181–191. doi: 10.1023/A:1007781909213. doi:10.1023/A:1007781909213. [DOI] [PubMed] [Google Scholar]
- Garbarino J, Sherman D. High-risk neighborhoods and high-risk families: The human ecology of maltreatment. Child Development. 1980;51:188–198. doi:10.1111/j.1467-8624.1980.tb02525.x. [PubMed] [Google Scholar]
- Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: Extending horizons, envisioning the future. Social Science & Medicine. 2006;62:1650–1671. doi: 10.1016/j.socscimed.2005.08.044. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- Heim C, Shugart M, Craighead WE, Nemeroff CB. Neurobiological and psychiatric consequences of child abuse and neglect. Developmental Psychobiology. 2010;52:671–690. doi: 10.1002/dev.20494. doi:10.1002/dev.20494. [DOI] [PubMed] [Google Scholar]
- IBM Corp. Released . IBM SPSS Statistics for Windows. Version 20.0. IBM Corp; Armonk, NY: 2011. [Google Scholar]
- Klebanov PK, Brooks-Gunn J, Duncan GJ. Does neighborhood and family poverty affect mothers’ parenting, mental health, and social support. Journal of Marriage and Family. 1994;56:441–445. doi:10.2307/353111. [Google Scholar]
- Leventhal T, Brooks-Gunn J. The neighborhoods they live in: The effects of neighborhood residence on child and adolescent outcomes. Psychological Bulletin. 2000;126:309–337. doi: 10.1037/0033-2909.126.2.309. doi:10.1037//0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychological Medicine. 2010;40:1647–1658. doi: 10.1017/S0033291709992121. doi:10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. Muthén & Muthén; Seventh Edition. Los Angeles, CA: 1998-2012. [Google Scholar]
- Nugent NR, Tyrka AR, Carpenter LL, Price LH. Gene-environment interactions: Early life stress and risk for depressive and anxiety disorders. Psychopharmacology. 2011;214:175–196. doi: 10.1007/s00213-010-2151-x. doi:10.1007/s00213-010-2151-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osypuk TL, Galea S. What level macro? Choosing appropriate levels to assess how place influences population health. In: Galea S, editor. Macrosocial determinants of population health. Springer; New York, NY: 2007. pp. 399–435. [Google Scholar]
- Rajaratnam JK, O'Campo P, Caughy MO, Mutaner C. The effect of social isolation on depressive symptoms varies by neighborhood characteristics: A study of an urban sample of women with pre-school aged children. International Journal of Mental Health and Addiction. 2008;6:464–475. doi:10.1007/s11469-007-9115-3. [Google Scholar]
- Roy A, Carli V, Sarchiapone M. Resilience mitigates the suicide risk associated with childhood trauma. Journal of Affective Disorders. 2011;133:591–594. doi: 10.1016/j.jad.2011.05.006. doi:10.1016/j.jad.2011.05.006. [DOI] [PubMed] [Google Scholar]
- Scott KM, McLaughlin KA, Smith DA, Ellis PM. Childhood maltreatment and DSM-IV adult mental disorders: a comparison of prospective and retrospective findings. British Journal of Psychiatry. 2012;200:469–475. doi: 10.1192/bjp.bp.111.103267. doi:10.1192/bjp.bp.111.103267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperry DM, Widom CS. Child abuse and neglect, social support, and psychopathology in adulthood: A prospective investigation. Child Abuse & Neglect. 2013;37:415–425. doi: 10.1016/j.chiabu.2013.02.006. doi: 10.1016/j.chiabu.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockdale SE, Wells KB, Tang L, Belin TR, Zhang L, Sherbourne CD. The importance of social context: Neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Social Science & Medicine. 2007;65:1867–1881. doi: 10.1016/j.socscimed.2007.05.045. doi:10.1016/j.socscimed.2007.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Samson JA. Childhood maltreatment and psychopathology: A case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. American Journal of Psychiatry. 2013;170:1114–1133. doi: 10.1176/appi.ajp.2013.12070957. doi:10.1176/appi.ajp.2013.12070957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wind TR, Komproe IH. The mechanisms that associate community social capital with post-disaster mental health: A multilevel model. Social Science & Medicine. 2012;75:1715–1720. doi: 10.1016/j.socscimed.2012.06.032. doi:10.1016/j.socscimed.2012.06.032. [DOI] [PubMed] [Google Scholar]
- Zielinski DS. Child maltreatment and adult socioeconomic well- being. Child Abuse & Neglect. 2009;33:666–678. doi: 10.1016/j.chiabu.2009.09.001. doi:10.1016/j.chiabu.2009 .09.001. [DOI] [PubMed] [Google Scholar]