Abstract
Objective: To study the potential protective effects of gastrodin on reducing tissue oxidative stress and attenuating cognitive deficits in vascular dementia induced by cerebral chronic hyperfusion. To explore the detailed molecular mechanisms. Methods: 6 to 8 week old male Wistar rats were adopted as experimental animals. Animals were divided into the following groups: Group 1 (sham group with no occlusion), Group 2 (control group with 2VO procedure), Group 3 (sham group with gastrodin administration), Group 4 (2VO group with gastrodin administration). Morris water maze (MWM) test was adopted to test the learning and memory function of rats within different groups. MDA, glutathione peroxidase and total thiol assessment was done to reflect the oxidative stress in the brain tissue. Cell counting kit-8 (CCK8) and flow cytometry (FCM) were performed to examine the cell viability and apoptosis rate of SH-SY5Y cells induced by hydrogen peroxide and rescued by gastrodin treatments. Reactive oxygen species (ROS) generation was determined by the 2’, 7’-dichlorofluorescein diacetate (DCFH-DA) assay. qPCR and Western blot (WB) were adopted to detect the molecular mechanisms related to the anti-apoptosis and ROS scavenging effects of gastrodin. Results: Our results indicated an obvious protective effect of gastrodin on vascular dementia induced brain ischemia. Administration of gastrodin could improve the impaired learning and memory function induced by 2VO procedure in rats. The levels of MDA were partially decreased by the administration of gastrodin. The levels of glutathione peroxidase and total thiol were partially restored by the administration of gastrodin. Cell viability was improved by gastrodin in a dose-dependent pattern on SH-SY5Y cells induced by hydrogen peroxide (P < 0.05). Cell apoptosis rate was reduced by gastrodin in a dose-dependent pattern on SH-SY5Y cells induced by hydrogen peroxide (P < 0.05). Gastrodin could scavenge ROS generation induced by pre-treatment of hydrogen peroxide. Both qPCR and WB results showed significant enhancements on the expression levels of NFE2L2, ADH7, GPX2 and GPX3 (P < 0.05). Conclusion: Gastrodin administration is protective on the learning and memory functions that might be affected by vascular dementia induced oxidative stress due to brain ischemia. On the molecular level, NFE2L2, ADH7, GPX2 and GPX3 were up regulated by gastrodin.
Keywords: Vascular dementia, gastrodin, oxidative stress, cognitive dysfunction, NFE2L2
Introduction
Chronic cerebral hypoperfusion (CCH) is a pathological condition that can be caused by diseases such as Alzheimer’s diseases, vascular dementia, etc [1,2]. It has already been reported that CCH is closely related with learning and memory dysfunction, especially in vascular dementia [3,4]. CCH animal model (2VO rats) is generated by disrupting of the bilateral common carotid arteries. The process is much like the pathological change occurred in vascular dementia. Cerebral chronic hypoperfusion in the cortex and white matter was caused by cerebral blood flow disruption in the 2VO rats. Neuronal injury was caused symbolized by the cognitive dysfunction and suboptimal metabolism. The renin-angiotensin system (RAS) was regarded as potential target since it was reported to be important regulatory systems in the circulatory homeostasis [5,6].
Overexpression of reactive oxygen species (ROS) stimulated by the disruption of cerebral blood flow is one of the main causes of vascular dementia induced cognitive deficits and behavioral dysfunction [7]. Accumulation of excessive ROS usually initiates the initiation of tissue oxidative stress and breaks the balance between ROS and the antioxidants interaction. DNA fragmentation and damage, protein damage and lipid peroxidation can be caused by over generation of ROS and free radicals [8]. ROS generation and its harmful effects were not only discovered in vascular dementia but also other CNS diseases with ischemic, hemorrhage and reperfusion conditions [9-12]. In the brain, over generation of ROS can cause cell death and apoptosis of neurons and astrocytes leading to permanent neuronal damage. In this regard, ROS removing compounds were intensively studied in the past decades.
Gastrodin, one form of natural phenol, can be found in a number of plants and herbs. Gastrodin is also commonly used in traditional Chinese medicine for symptoms like fever and diarrhea. It has been proved that gastrodin has the ability of scavenging ROS and reducing lipid perioxidation. Gastrodin was also proved to be neuroprotective in different kinds of neurological diseases like Alzheimer’s disease, Parkinson’s disease and brain ischemia [13-15]. The ROS scavenging ability of gastrodin was emphasized in most of the studies referring the protective effects of gastrodin. Several studies also focused on the anti-apoptosis activity of gastrodin on particular cell types [16,17]. However, no study has yet been done considering the protective effects of gastrodin on CCH.
In the present study, we reported that gastrodin has protective effects on the chronic ischemia caused by vascular dementia through 2VO rat model. Gastrodin was proved alleviative on the cognitive and behavioral dysfunction caused by vascular dementia. Gastrodin could also reduce oxidative stress by scavenging ROS in the 2VO rats.
Methods and materials
Reagents
Dulbecco’s Modified Eagle Media (DMEM) and fetal bovine serum (FBS) was purchased from Gibco (life technologies, USA). Penicillin-streptomycin solution was obtained from Hyclone (Thermo Scientific, USA). 2’, 7’-dichlorofluorescein diacetate (DCFH-DA) was obtained from Molecular Probes (Eugene, OR, USA). Gastrodin was obtained from Sigma-Aldrich (NY, USA).
Animals
6 to 8 week old male Wistar rats were purchased from Shanghai Experimental Animal Center (Shanghai, China). Experimental procedures were approved and performed according to guidelines of laboratory animal care and use. All efforts were made to reduce the number of animals tested and their suffering.
Surgical procedures
Permanent cerebral hypoperfusion was realized by disruption of bilateral common carotid arteries (2VO rats). The detailed surgical procedures were as follows: Rats were first anesthetized with ketamine/xylazine (45/6 mg/kg). After anesthetization, a ventral cervical incision was performed and the bilateral common carotid arteries were carefully exposed. Vessels were then separated from the sheath and sympathetic nerves. The vessels were ligated with surgical suture for ischemia simulation. The whole surgery was performed on heating device to maintain the body temperature of rats.
Morris water maze test
Morris water maze was adopted to test the alterations of cognitive and behavioral performance within different groups. Animals were divided into the following groups: Group 1 (Sham group with no occlusion), Group 2 (Control group with 2VO procedure), Group 3 (Sham group with gastrodin administration), Group 4 (2VO group with gastrodin administration). The maze device contains a circular water pool with diameter of 1.5 m and height of 0.6 m. Rats in different groups were put in the pool at the starting points in the four different corners. One black platform was placed below the water surface and rats were aimed to locate the platform. Rats will be placed onto the platform if they cannot find the platform by themselves. The escape latency and swim speed were recorded for the analysis of the total performances.
Cell culture
SH-SY5Y cells were obtained from the Shanghai Experimental Cell Bank (Shanghai, China). The cells were cultured in DMEM medium with 10% FBS and 1% penicillin and streptomycin. Cells were seeded with a density of 106 cells/flasks and then cultured for 2 weeks under the condition of 5% CO2, 95% humidity incubator at 37°C.
MDA, glutathione peroxidase and total thiol assessment
Lipid peroxidation (LPO) was evaluated by testing the level of MDA. Thiobarbituric acid can react with MDA producing a red colored compound with an absorbance light wave of 532 nm. In the experimental procedure, phosphoric acid (2 mL, 1%) and TBA (1 mL 0.5%) were mixed and centrifuge and heated to boiling. 5 mL butanol was then added after cooling and then mixed together. After centrifugation, the red colored layer was transferred to a new 96-well plate to test the absorbance at 532 nm. The standard curve was calculated and made at the dosage of 0 μM to 10 μM according to previous studies. Glutathione peroxidase (GSH-Px) concentration was determined by GSH peroxidase kit obtained from Sigma-Aldrich (NY, USA). The procedures followed the manufacturer’s instructions. Thiol concentration was evaluated by DTNB assay. DTNB reacts with thiol and produce yellow color at an absorbance of 412 nm. Thiol concentration was determined by equations explained in previous studies [18].
CCK-8 cell proliferation and viability assay
SH-SY5Y cells were seeded (2 × 103 per well) into 96-well plates and were cultured overnight. Cells were stressed with hydrogen peroxide and then with or without treatments of gastrodin. Culture medium was removed the next day and fresh medium was added. Cell proliferation and viability were evaluated by Cell Counting Kit-8 (CCK8, Dojindo, Japan) reagent at 12 h, 24 h, and 48 h according to the manufacturers’ instructions. The absorbency of cells was measured using a 96-well plate reader at 450 nm.
Flow cytometry cell apoptosis assay
SH-SY5Y cells apoptosis rate was detected by FCM with Annexin V-FITC Apoptosis Detection Kit (KeyGEN) following to the manufacturer’s instructions. 100 mL of 105 cells in suspension were stained with kit solution (Annexin-V-FITC and PI) in dark for 15 min. The apoptosis rate was assayed by using FACSCalibur Flow Cytometry (BD, USA) at 488 nm.
Reactive oxygen species (ROS) assay
SH-SY5Y cells (5 × 103 cells/well in 96 well plates) were cultured in DMEM medium (10% FBS, 1% antibiotics) containing hydrogen peroxide for 24 h as stress stimulation and each well was replaced with DMEM medium (10% FBS, 1% antibiotics). Cells were then treated with different concentrations of gastrodin and control group was set as blank. Intracellular ROS level was measured by 2’, 7’-dichlorofluorescein diacetate (DCFH), which can be oxidized into fluorescent DCF. After fixing, the cells were washed in 1 × PBS and then incubated in the dark for 30 min with 10 μM DCFH-DA. Images were taken using the fluorescence of DCF by fluorescence microscopy.
qPCR
Total RNA was isolated using Trizol reagent (Life Technologies). Reverse transcriptase and oligo’dT primer were used to prepare cDNA from 1 μg of RNA according the manufacturer’s instructions (Takara, Japan). Two microlitres of each cDNA was then used for PCR amplification using primers for NFE2L2, ADH7, GPX2 and GPX3. The detailed information of primers was shown in Table 1.
Table 1.
Primer sequences for qPCR
| primers | Forward | Reverse | Tm (°C) |
|---|---|---|---|
| NFE2L2 | 5’-GCGTCGCATTACCAACAT-3’ | 5’-CTGGAAGCTCACCAACGA-3’ | 57 |
| ADH7 | 5’-ACCCGAAGCGGACATT-3’ | 5’-GGCATCTCCCTGAACG-3’ | 58 |
| GPX2 | 5’-TACCCACCTCAGACACC-3’ | 5’-ATCCCCAATCAGAAACAC-3’ | 59 |
| GPX3 | 5’-AGCAAAGAAGACGAG-3’ | 5’-CAGCGTCTCAAACAGG-3’ | 61 |
| β-actin | 5’-TCCCTGTATGCCTCTG-3’ | 5’-ATGTCACGCACGATTT-3’ | 61 |
Western blot
Cells were first lysed in prepared buffer containing 10 mM Tris, 0.1% SDS, 5 mM EDTA. The pH was regulated to 7.2. 20 μg of protein samples were loaded to SDS-PAGE. PVDF membranes were chosen for transfer. After blocking in 5% skim milk in PBS, membranes were incubated with antibodies against NFE2L2 (1:1000), ADH7 (1:1000), GPX2 (1:1000), GPX3 (1:1000) and β-actin (1:1000) overnight at 4°C followed by 1 h-incubation with secondary antibody (1:2000). Blots against β-actin served as loading control.
Statistical analysis
All data were analyzed by SPSS (ver. 13.0) software and the results were showed by mean ± SD. Student’s t-test and two-way analysis of variance (ANOVA) were used to assess statistical significance, with P ≤ 0.05 being regarded as significant.
Results
Gastrodin attenuates learning and memory impairments in 2VO rats
A training trial lasts for four days was performed using the MWM devices aiming to evaluate the learning and memory function of gastrodin treatment. Escape latency time was recorded in the four groups. The results showed that animals in 2VO group presented significant high latency time than the sham group (P < 0.05). These results were confirmed of the impairment of the learning and memory function representing a vascular dementia model. The results also revealed that long-term administration of Gastrodin improved the performances of 2VO group animals. Learning and memory function were partially restored in 2VO + Gastrodin groups with significant alterations (P < 0.05). (Figure 1A). We also find that sham animals administered with gastrodin was not associated with the change of learning and memory functions. We then focused on the spending time in the target quadrant to test the memory. Results showed that mice underwent 2VO procedure presented worse memory ability with shorter average spending time on a particular target quadrant (P < 0.05). In 2VO groups administered with gastrodin, the memory ability was improved indicated by an extension of the spending time in the target quadrant (P < 0.05). The results were consistent with the learning ability that sham group treated with gastrodin didn’t show any change on consolidation of memories. An additional thing we noticed was that the swimming speed of the four groups showed no significant differences. This observation excluded the possibility that the learning and memory differences were caused by mobility disorders (Figure 1C).
Figure 1.

Gastrodin attenuates learning and memory impairments in 2VO rats. Animals were divided into the following groups: Group 1 (Sham group with no occlusion), Group 2 (Control group with 2VO procedure), Group 3 (Sham group with gastrodin administration), Group 4 (2VO group with gastrodin administration). A. Swimming speed of the four different groups. B. Average time spending proportion in the target quadrant. C. Escape latency to find the hidden platform. Data in the figures represent average ± SD (n = 3). *P < 0.05, compared to 2VO group. #P < 0.05, compared to sham group.
Gastrodin reduces MDA, GSH-Px and thiol levels in the hippocampus and frontal cortex
Oxidative stress is one of the main damage occurs after 2VO procedure. To test the degree of the free radical induced tissue damage, MDA, GA and thiol levels were detected with different methods. The results presented that the MDA levels were significantly elevated in the 2VO groups in both hippocampus and the frontal cortex compare to the sham groups (P < 0.05). In accordant with the previous results, administration of gastrodin can significantly down-regulate the elevated MDA levels in the hippocampus and the frontal cortex (Figure 2A) (P < 0.05). As expected, administration of gastrodin to sham rats did not show any change of MDA levels in the sham + gastrodin groups. GSH-Px concentration was determined to estimate the antioxidant enzyme activity in cells against the free radicals and ROS generation. As shown in Figure 2, 2VO groups showed much less GSH-Px concentration compare with the sham group (Figure 2B). Administration of gastrodin was not fully but partially restored the GSH-Px concentration in the 2VO + Gastrodin groups (P < 0.05). Administration of gastrodin in the sham + gastrodin group showed no difference compare with the sham group. Total thiol concentration was then tested by DTNB assay aiming to evaluate the non-enzymatic defense against the free radicals and ROS generation. Similarly with the GSH-Px concentration examination, 2VO rats showed a significant decrease in the level of total thiol compare to the sham group (P < 0.05). Administration of gastrodin in 2VO rats could partially improve the total thiol level decreased by 2VO procedure (Figure 2C). Administration of gastrodin in the sham + gastrodin did not show statistical meaningful changes on the thiol level.
Figure 2.
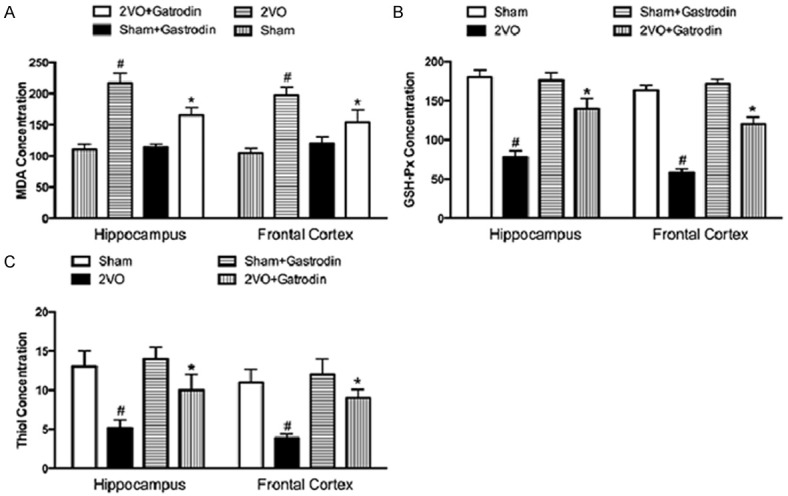
Gastrodin reduces MDA, GSH-Px and thiol levels in the hippocampus and frontal cortex. Animals were divided into four groups described as previous. A. Effects of Gastrodin on the levels of MDA in the hippocampus and frontal cortex of 2VO rats and sham rats. B. Effects of Gastrodin on the levels of GSH-Px in the hippocampus and frontal cortex of 2VO rats and sham rats. C. Effects of Gastrodin on the levels of thiol in the hippocampus and frontal cortex of 2VO rats and sham rats. Data in the figures represent average ± SD (n = 3). *P < 0.05, compared to 2VO group. #P < 0.05, compared to sham group.
Gastrodin increases cell viability of SH-SY5Y cells treated with hydrogen peroxide
To simulate the in vivo situation of vascular dementia and 2VO models, we stimulated the SH-SY5Y cells with hydrogen peroxide for oxidative stress. Cell viability was evaluated with or without treatments of gastrodin. Gastrodin was treated under three different concentrations: 0.1 µM, 0.5 µM and 1 µM. Cell viability was measured at 12 h, 24 h and 48 h respectively. The results showed that oxidative stress induced by hydrogen peroxide could significantly down-regulate the cell viability at the three time points (Figure 3A-C). The cell viability of SH-SY5Y cells was improved by gastrodin treatments in a dose-dependent way. 1 µM of gastrodin showed the best improving effects that almost reached to the same level of the control groups. We then tested the cell apoptosis rate induced by oxidative stress. The results went an opposite pattern showing that pueararin could decrease the apoptosis rate induced by hydrogen peroxide in a dose-dependent way (Figure 3D-F). 1 µM of gastrodin showed the best anti-apoptosis effects compare to the other gastrodin treatments groups.
Figure 3.

Gastrodin increases cell viability of SH-SY5Y cells treated with hydrogen peroxide. SH-SY5Y cells were culture stimulated by hydrogen peroxide with or without treatments of different dosages of gastrodin. A. Cell viability evaluation of in different groups at 12 h by CCK-8. B. FCM analysis of cell apoptosis rate of SH-SY5Y cells at 12 h. C. Cell viability evaluation of in different groups at 24 h by CCK-8. D. FCM analysis of cell apoptosis rate of SH-SY5Y cells at 24 h. E. Cell viability evaluation of in different groups at 48 h by CCK-8. F. FCM analysis of cell apoptosis rate of SH-SY5Y cells at 48 h. Data in the figures represent average ± SD (n = 3). *P < 0.05, compared to control group. #P < 0.05, compared to positive control group.
Gastrodin scavenges ROS production of SH-SY5Y cells under hydrogen peroxide stress
To further explore the ROS scavenging ability of gastrodin, we performed ROS scavenging assay by DCFH-DA on SH-SY5Y cells. Intracellular ROS levels were analyzed by DCFH-DA, which is cell permeable and oxidation sensitive within cells. After 24 h’s induction of hydrogen peroxide, culture medium was replaced with different dosages of gastrodin. After 12 h or 24 h of gastrodin treatment, intracellular ROS levels were then analyzed by DCFH-DA. The results remarkably showed that gastrodin decrease the intensity of DCF fluorescence within SH-SY5Y cells in a dose-dependent way (Figure 4A). Quantitative analysis of DCF fluorescence intensity showed that groups induced with hydrogen peroxide and no treatment of gastrodin showed the highest fluorescence level. The ROS positive cell number was significantly down regulated by gastrodin treatments at both 12 h and 24 h. 1 µM of gastrodin showed the best ROS scavenging ability compare to other groups (P < 0.05).
Figure 4.

Gastrodin scavenges ROS production of SH-SY5Y cells under hydrogen peroxide stress. A. ROS positive SH-SY5Y cells at 12 h. B. ROS positive SH-SY5Y cells at 24 h. Data in the figures represent average ± SD (n = 3). *P < 0.05, compared to control group. #P < 0.05, compared to positive control group.
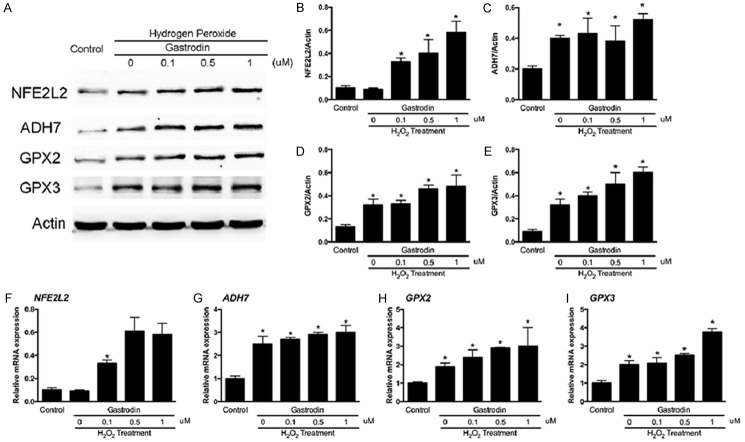
Gastrodin increases expression of NFE2L2, ADH7, GPX2 and GPX3 expression in SH-SY5Y cells
We previously proved that gastrodin could effectively scavenge intracellular ROS generation induced by hydrogen peroxide. To explore the underlying mechanisms, we hypothesized that the antioxidant activity of gastrodin might be related with alterations of gene expressions. We then investigated several crucial genes related with antioxidant protein expression namely NFE2L2, ADH7, GPX2 and GPX3. qPCR and western blot were performed to test the expression changes of these genes (Figure 5). From the results, we found that hydrogen peroxide is not affective on the mRNA level of NFE2L2, while gastrodin treatments could significantly improve the expression of NFE2L2 (Figure 5A). As for the FoxO family, both ADH7, GPX2 and GPX3 were improved by hydrogen peroxide induction on the mRNA levels. Gastrodin treatments could enhance the improving effects of hydrogen peroxide (Figure 5B-D) (P < 0.05). The results were consistent on the protein levels proved by WB (Figure 5E). The quantitative analysis of WB images showed that these anti oxidative stress genes expressions were up regulated in different patterns according to the mRNA level alterations (Figure 5F-I).
Figure 5.
Gastrodin increases expression of NFE2L2, ADH7, GPX2 and GPX3 expression in SH-SY5Y cells. A. Representative WB images of NFE2L2, ADH7, GPX2 and GPX3. B. Quantitative analysis of NFE2L2 intensity against actin. C. Quantitative analysis of ADH7 intensity against actin. D. Quantitative analysis of GPX2 intensity against actin. E. Quantitative analysis of GPX3 intensity against actin. F. Relative mRNA expression of NFE2L2. G. Relative mRNA expression of ADH7. H. Relative mRNA expression of GPX2. I. Relative mRNA expression of GPX3. Data in the figures represent average ± SD (n = 3). *P < 0.05, compared to control group. #P < 0.05, compared to positive control group.
Discussion
2VO rat models were chosen as the in vivo animal model in our study. Two target areas were mostly affected from this ischemia namely hippocampus and frontal cortex in which hippocampus is in charge of the learning and memory function. The ligation of the bilateral common arteries could cause global ischemia of the brain. Morris Water Maze test was then performed for the evaluation of learning and memory function in each group. All the results indicated protective effects of gastrodin on the impaired function of learning and memory abilities in 2VO rats. In the previous studies, it was also reported that the cholinergic system could also be affected by chronic ischemia [19,20]. It was interesting to find that stimulation of the cholinergic system could improve the impaired spatial memory in the experimental animal model. Another report demonstrated that release of glutamate in the CNS could be regarded as a symbolic event under the ischemic condition [21]. As one of the functional neurotransmitter, glutamate was reported capable of generating ROS that is inductive of neuronal apoptosis and cell death [22]. In this regard, drugs were investigated targeting neurotransmitters like glutamate and acetylcholine treating patients with diseases such as VD. Besides, different kinds of medications were invented treating VD such as antioxidants, free radicals scavengers and calcium ion antagonists [23].
Our results demonstrated that gastrodin administration both in vivo and in vitro could significantly reverse the oxidative stress induced by ischemic conditions or hydrogen peroxide. Gastrodin administration could also improve the learning ability and consolidate the memory condition in 2VO rats. We found that the protective effects of gastrodin on the chronic ischemia and oxidative stress induced by hydrogen peroxide in vitro are closely related with its ROS scavenging ability, which also explained the anti-apoptosis activity of gastrodin in vitro. On the molecular level, we discovered that treatments of gastrodin were associated with the up regulation of several antioxidant protein expressions. The mRNA level and protein levels of NFE2L2, ADH7, GPX2 and GPX3 were significantly up regulated by treatments of gastrodin. It was also interesting to find that hydrogen peroxide treatment alone could also up regulate the expression of NFE2L2 (Figure 5E).
It has already been proved that oxidative stress plays a crucial role in the ischemic and hypoxic brain damage. Oxidative stress is also related with over expression of inflammatory cytokines and cognitive dysfunction caused by vessels impairments [24-27]. ROS is capable of oxidize membranous lipids, cell proteins and nuclear acids within the nuclei that eventually lead to cellular dysfunction. In this consideration, we focused on the ROS over generation and free radicals production in the brain tissue of 2VO rats. We measured the levels of MDA, which is a marker of lipid peroxidation [28,29]. GSH-Px and thiol levels were measured as enzymatic and non-enzymatic defense of ROS generation in vitro respectively. To further explain the ROS scavenging ability of gastrodin in vitro, SH-SY5Y cells were selected to be cultured in vitro and stimulated with hydrogen peroxide as simulation of ischemic induced oxidative stress in vivo. In our results, it was indicated that gastrodin treatments were capable of reducing the hydrogen peroxide induced cell apoptosis. We found that gastrodin treatments partially reversed the adverse effects of oxidative stress induced by hydrogen peroxide in a dose-dependent way.
To explore the underlying mechanisms, we focused on the forkhead box O (FoxO) family and NFE2L2 expression. The FoxO family reduces ROS production by increasing the expression of several antioxidant enzymes of redox signaling. FoxO family proteins are also transcription factors regulating cell proliferation, differentiation, apoptosis, cell cycle arrest and autophagy [30,31]. Another gene we focused on is NFE2L2, which also regulate antioxidant proteins protective on oxidative damages [32]. Both FoxO family and NFE2L2 have important roles in the physiological function and pathological conditions in the CNS [33-35]. For the first time we reported that gastrodin treatments is associated with the up regulation of both these genes in the ischemic brain.
In conclusion, we hypothesized that gastrodin is protective on the vascular dementia induced chronic brain ischemia by reducing the oxidative stress and facilitating the cognitive functions.
Disclosure of conflict of interest
None.
References
- 1.Austin BP, Nair VA, Meier TB, Xu G, Rowley HA, Carlsson CM, Johnson SC, Prabhakaran V. Effects of hypoperfusion in Alzheimer’s disease. J Alzheimers Dis. 2011;26(Suppl 3):123–133. doi: 10.3233/JAD-2011-0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ciobica A, Bild W, Hritcu L, Haulica I. Brain renin-angiotensin system in cognitive function: pre-clinical findings and implications for prevention and treatment of dementia. Acta Neurol Belg. 2009;109:171–180. [PubMed] [Google Scholar]
- 3.Annahazi A, Mracsko E, Sule Z, Karg E, Penke B, Bari F, Farkas E. Pre-treatment and posttreatment with alpha-tocopherol attenuates hippocampal neuronal damage in experimental cerebral hypoperfusion. Eur J Pharmacol. 2007;571:120–128. doi: 10.1016/j.ejphar.2007.05.048. [DOI] [PubMed] [Google Scholar]
- 4.Farkas E, Luiten PG, Bari F. Permanent, bilateral common carotid artery occlusion in the rat: a model for chronic cerebral hypoperfusion-related neurodegenerative diseases. Brain Res Rev. 2007;54:162–180. doi: 10.1016/j.brainresrev.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Wright JW, Harding JW. The brain renin-angiotensin system: a diversity of functions and implications for CNS diseases. Pflugers Arch. 2013;465:133–151. doi: 10.1007/s00424-012-1102-2. [DOI] [PubMed] [Google Scholar]
- 6.Mogi M, Iwanami J, Horiuchi M. Roles of Brain Angiotensin II in Cognitive Function and Dementia. Int J Hypertens. 2012;2012:169649. doi: 10.1155/2012/169649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Z, Wang Y, Xie Y, Yang Z, Zhang T. Protective effects of exogenous hydrogen sulfide on neurons of hippocampus in a rat model of brain ischemia. Neurochem Res. 2011;36:1840–1849. doi: 10.1007/s11064-011-0502-6. [DOI] [PubMed] [Google Scholar]
- 8.Floyd RA. Antioxidants, oxidative stress and degenerative neurological disorders. Proc Soc Exp Biol Med. 1999;222:236–245. doi: 10.1046/j.1525-1373.1999.d01-140.x. [DOI] [PubMed] [Google Scholar]
- 9.Nowak JZ. Oxidative stress, polyunsaturated fatty acids-derived oxidation products and bisretinoids as potential inducers of CNS diseases: focus on age-related macular degeneration. Pharmacol Rep. 2013;65:288–304. doi: 10.1016/s1734-1140(13)71005-3. [DOI] [PubMed] [Google Scholar]
- 10.Sorce S, Krause KH, Jaquet V. Targeting NOX enzymes in the central nervous system: therapeutic opportunities. Cell Mol Life Sci. 2012;69:2387–2407. doi: 10.1007/s00018-012-1014-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsieh HL, Yang CM. Role of redox signaling in neuroinflammation and neurodegenerative diseases. Biomed Res Int. 2013;2013:484613. doi: 10.1155/2013/484613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li J, O W, Li W, Jiang ZG, Ghanbari HA. Oxidative stress and neurodegenerative disorders. Int J Mol Sci. 2013;14:24438–24475. doi: 10.3390/ijms141224438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen PZ, Jiang HH, Wen B, Ren SC, Chen Y, Ji WG, Hu B, Zhang J, Xu F, Zhu ZR. Gastrodin suppresses the amyloid beta-induced increase of spontaneous discharge in the entorhinal cortex of rats. Neural Plast. 2014;2014:320937. doi: 10.1155/2014/320937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang XL, Xing GH, Hong B, Li XM, Zou Y, Zhang XJ, Dong MX. Gastrodin prevents motor deficits and oxidative stress in the MPTP mouse model of Parkinson’s disease: involvement of ERK1/2-Nrf2 signaling pathway. Life Sci. 2014;114:77–85. doi: 10.1016/j.lfs.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 15.Wang Y, Wu Z, Liu X, Fu Q. Gastrodin ameliorates Parkinson’s disease by downregulating connexin 43. Mol Med Rep. 2013;8:585–590. doi: 10.3892/mmr.2013.1535. [DOI] [PubMed] [Google Scholar]
- 16.Huang Q, Shi J, Gao B, Zhang HY, Fan J, Li XJ, Fan JZ, Han YH, Zhang JK, Yang L, Luo ZJ, Liu J. Gastrodin: an ancient Chinese herbal medicine as a source for anti-osteoporosis agents via reducing reactive oxygen species. Bone. 2015;73:132–144. doi: 10.1016/j.bone.2014.12.059. [DOI] [PubMed] [Google Scholar]
- 17.Shu C, Chen C, Zhang DP, Guo H, Zhou H, Zong J, Bian Z, Dong X, Dai J, Zhang Y, Tang Q. Gastrodin protects against cardiac hypertrophy and fibrosis. Mol Cell Biochem. 2012;359:9–16. doi: 10.1007/s11010-011-0992-1. [DOI] [PubMed] [Google Scholar]
- 18.Korani MS, Farbood Y, Sarkaki A, Fathi Moghaddam H, Taghi Mansouri M. Protective effects of gallic acid against chronic cerebral hypoperfusion-induced cognitive deficit and brain oxidative damage in rats. Eur J Pharmacol. 2014;733:62–67. doi: 10.1016/j.ejphar.2014.03.044. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka K, Ogawa N, Asanuma M, Kondo Y, Nomura M. Relationship between cholinergic dysfunction and discrimination learning disabilities in Wistar rats following chronic cerebral hypoperfusion. Brain Res. 1996;729:55–65. [PubMed] [Google Scholar]
- 20.Ni JW, Matsumoto K, Li HB, Murakami Y, Watanabe H. Neuronal damage and decrease of central acetylcholine level following permanent occlusion of bilateral common carotid arteries in rat. Brain Res. 1995;673:290–296. doi: 10.1016/0006-8993(94)01436-l. [DOI] [PubMed] [Google Scholar]
- 21.Davalos A, Shuaib A, Wahlgren NG. Neurotransmitters and pathophysiology of stroke: evidence for the release of glutamate and other transmitters/mediators in animals and humans. J Stroke Cerebrovasc Dis. 2000;9:2–8. doi: 10.1053/jscd.2000.18908. [DOI] [PubMed] [Google Scholar]
- 22.Novelli A, Reilly JA, Lysko PG, Henneberry RC. Glutamate becomes neurotoxic via the N-methyl-D-aspartate receptor when intracellular energy levels are reduced. Brain Res. 1988;451:205–212. doi: 10.1016/0006-8993(88)90765-2. [DOI] [PubMed] [Google Scholar]
- 23.Itil TM, Eralp E, Ahmed I, Kunitz A, Itil KZ. The pharmacological effects of ginkgo biloba, a plant extract, on the brain of dementia patients in comparison with tacrine. Psychopharmacol Bull. 1998;34:391–397. [PubMed] [Google Scholar]
- 24.Sanderson TH, Reynolds CA, Kumar R, Przyklenk K, Huttemann M. Molecular mechanisms of ischemia-reperfusion injury in brain: pivotal role of the mitochondrial membrane potential in reactive oxygen species generation. Mol Neurobiol. 2013;47:9–23. doi: 10.1007/s12035-012-8344-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Godinez-Rubi M, Rojas-Mayorquin AE, Ortuno-Sahagun D. Nitric oxide donors as neuroprotective agents after an ischemic strokerelated inflammatory reaction. Oxid Med Cell Longev. 2013;2013:297357. doi: 10.1155/2013/297357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kahles T, Brandes RP. NADPH oxidases as therapeutic targets in ischemic stroke. Cell Mol Life Sci. 2012;69:2345–2363. doi: 10.1007/s00018-012-1011-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olmez I, Ozyurt H. Reactive oxygen species and ischemic cerebrovascular disease. Neurochem Int. 2012;60:208–212. doi: 10.1016/j.neuint.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 28.Bilenko MV, Tel’pukhov VI, Churakova TD, Komarov PG. [Effect of ischemia and reperfusion of the rat brain on lipid peroxidation and the protective effect of antioxidants] . Biull Eksp Biol Med. 1988;105:394–397. [PubMed] [Google Scholar]
- 29.Akdag MZ, Dasdag S, Ulukaya E, Uzunlar AK, Kurt MA, Taskin A. Effects of extremely lowfrequency magnetic field on caspase activities and oxidative stress values in rat brain. Biol Trace Elem Res. 2010;138:238–249. doi: 10.1007/s12011-010-8615-3. [DOI] [PubMed] [Google Scholar]
- 30.Xie Q, Chen J, Yuan Z. Post-translational regulation of FOXO. Acta Biochim Biophys Sin (Shanghai) 2012;44:897–901. doi: 10.1093/abbs/gms067. [DOI] [PubMed] [Google Scholar]
- 31.Oellerich MF, Potente M. FOXOs and sirtuins in vascular growth, maintenance, and aging. Circ Res. 2012;110:1238–1251. doi: 10.1161/CIRCRESAHA.111.246488. [DOI] [PubMed] [Google Scholar]
- 32.Sandberg M, Patil J, D’Angelo B, Weber SG, Mallard C. NRF2-regulation in brain health and disease: implication of cerebral inflammation. Neuropharmacology. 2014;79:298–306. doi: 10.1016/j.neuropharm.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang M, An C, Gao Y, Leak RK, Chen J, Zhang F. Emerging roles of Nrf2 and phase II antioxidant enzymes in neuroprotection. Prog Neurobiol. 2013;100:30–47. doi: 10.1016/j.pneurobio.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Popa-Wagner A, Mitran S, Sivanesan S, Chang E, Buga AM. ROS and brain diseases: the good, the bad, and the ugly. Oxid Med Cell Longev. 2013;2013:963520. doi: 10.1155/2013/963520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Salminen A, Kaarniranta K, Kauppinen A, Ojala J, Haapasalo A, Soininen H, Hiltunen M. Impaired autophagy and APP processing in Alzheimer’s disease: The potential role of Beclin 1 interactome. Prog Neurobiol. 2013;106-107:33–54. doi: 10.1016/j.pneurobio.2013.06.002. [DOI] [PubMed] [Google Scholar]