Abstract
The potentially harmful effects of short-term mechanical ventilation during surgery have been examined in recent years. An optimal strategy for mechanical ventilation of patients during non-laparoscopic abdominal surgery must be devised. A total of 63 patients undergoing elective open abdominal surgery with more than 2 h of ventilation time were selected for this randomized, open-label, clinical study. They were divided into three ventilation groups: high volume of 9 ml/kg IBW (ideal body weight) with ZEEP (zero end-expiratory pressure); low volume of 7 ml/kg IBW with 8 cm H2O PEEP (positive end expiratory pressure); and low volume of 7 ml/kg IBW with 8 cm H2O PEEP and recruitment. Intraoperative PaO2/FiO2 ratio and pulmonary compliance and postoperative pulmonary function were measured. There were no significant differences in intraoperative PaO2/FiO2 ratio among the three groups (P=0.31). The pulmonary compliance of three groups showed different changes over time (group effect over time P=0.0006). There were no significant differences in FEV1 or FVC among the three groups (P=0.32 and 0.09, respectively), but both of these measurements showed different changes over time (group effect over time P<0.001). On the first postoperative day, the low volume with high PEEP and recruitment group had significantly higher FEV1 than the other two groups (mean ± SD): 1.52±0.37 versus 0.95±0.38 (P<0.001) and 1.52±0.37 versus 0.95±0.34 (P<0.001), respectively. Low tidal volume with PEEP and recruitment showed advantages in maintaining the pulmonary compliance and expediting the recovery of the 1st postoperative day’s pulmonary function in patients undergoing non-laparoscopic abdominal surgery.
Keywords: Ventilation strategy, PaO2/FIO2 ratio, pulmonary compliance, pulmonary function
Introduction
There are more than 230 million patients who require general anesthesia and mechanical ventilation to undergo major surgery each year [1]. More than 30% of thoracic or abdominal surgery patients experience postoperative pulmonary complications [2]. The potentially harmful effects of short-term mechanical ventilation during surgery have been examined in recent years [3].
Mechanical ventilation can cause so-called ventilator-induced lung injury, which continually opens and closes atelectatic lung parts, distending the alveoli of the aerated lung tissue [4]. Fortunately, this injury can be lessened with low tidal volumes and high positive end expiratory pressure (PEEP) in critically ill patients with acute respiratory distress syndrome (ARDS) [5].
Various ventilation strategies to reduce ventilator-induced lung injury, promote early recovery, and reduce postoperative complications have been attempted in patients undergoing abdominal surgery [6-9]. In different clinical trials, traditional mechanical ventilation, using high tidal volumes with zero end-expiratory pressure (ZEEP), prevented atelectasis formation and hypoxemia in anesthetized patients [6]. However, high tidal volumes can lead to high inspiratory airway pressure, causing lung damage [7]. Futier [8] demonstrated the advantages of low tidal volumes (6-8 ml/kg of ideal body weight [IBW]) and 6-8 cm H2O PEEP in reducing health care utilization and improving clinical outcomes. Severgnini [9] suggested that a strategy of low tidal volumes (7 ml/kg IBW) and 10 cm H2O PEEP could improve postoperative pulmonary function more during general anesthesia. However, intraoperative oxygen index and dynamic pulmonary compliance are also important evaluative indicators. Partial pressure of oxygen/fraction of inspiration oxygen (PaO2/FiO2 ratio) has been used in a large number of experimental studies, to quantify pulmonary gas exchange [10,11] and to predict mortality during the early postoperative period after esophagectomy [12]. Research in animals and patients has confirmed that dynamic compliance could detect the onset of alveolar collapse and overdistention with greater sensitivity than PaO2 changes and functional residual capacity [13,14].
In our study, three primary ventilation strategies--high volume with ZEEP, low volume with 8 cm H2O PEEP, and low volume with 8 cm H2O PEEP and recruitment--were used to determine the influence of different ventilation strategies on three patient variables: intraoperative PaO2/FiO2 ratio, intraoperative pulmonary compliance and postoperative pulmonary function.
Methods
The present experiments were conducted in accordance with the Declaration of Helsinki. The protocol in this study was approved by the Ethics Committee of Harbin Medical University (No. 201314), and written informed consent was obtained from the patients prior to study enrollment.
Inclusion and exclusion criteria
The patients were screened and randomized by the clinical anesthesia service of our regional university hospital--the 1st Affiliated Hospital of Harbin Medical University, China-from patients planned to undergo abdominal major surgery under general anesthesia between March 2013 and June 2014.
Patients were included if they met the following conditions: their age was at least 60 years old; they were scheduled to undergo non-laparoscopic abdominal elective major surgery under general anesthesia and mechanical ventilation; their ventilation time was expected to last more than 2 h; and they did not have other serious systemic complications except for the digestive system. Patients were excluded if their body mass index (BMI) was greater than 35 kg/m2, they were receiving systemic corticosteroid therapy, intractable shock was considered, they had experienced acute lung injury or acute respiratory distress syndrome before surgery; they had received mechanical ventilation within the two previous weeks, their surgery was an emergency, their hemodynamic stability was not persistent, they were predicted to require prolonged mechanical ventilation post operation, they had any neuromuscular diseases or they had contraindications for positioning of an epidural catheter.
Standard procedures
The patients were pre-medicated with an intravenous injection of midazolam 0.05 mg/kg. Before the patients underwent general anesthesia, epidural, radial arterial and central venous catheters were inserted, an epidural catheter was placed at level T7-T12, and fluid infusion was administered at 10-15 ml/(kg·h) during surgery to stabilize hemodynamics.
All of the patients received routine anesthesia according to protocol, including intravenous sufentanil (0.25-0.5 μg/kg) and propofol (1-2 mg/kg) at induction; thereafter, anesthesia was maintained with sevoflurane to maintain a bispectral index (BIS) of 40-60; analgesia was provided with ropivacaine 0.5% (3-5) ml/h continuous infusion though the epidural catheter and a single intravenous injection of sufentanil 5 µg. The patients were intubated four minutes after administration of cisatracurium (0.03 mg/kg); cisatracurium was administered every 30 min, and the last administration occurred at least 30 min before the end of surgical suturing. All of the patients were pre-oxygenated to attain FiO2 greater than 0.85, and FiO2 was then maintained at approximately 0.5 during the whole anesthesia procedure with tracheal intubation. Routine intraoperative monitoring included invasive blood pressure, electrocardiography, pulse oximetry, end-tidal fraction of carbon dioxide (PETCO2), BIS and dynamic pressure-volume curve (Datex Ohmeda S/5 Avance; GE Healthcare, Helsinki, Finland).
The patients received a continuous infusion of ropivacaine 0.2% at 4 ml/2 h and morphine 0.04 mg/kg, as well as droperidol 0.75 mg per day postoperatively though the epidural catheter. The catheter was planned to be removed on the third day after surgery. Removal of the epidural catheter was scheduled at least 4 h before the next administration and 12 h after the last dose of low-molecular weight heparin.
Ventilation protocol
Randomization was performed with a computer-generated assignment sequence, and the results were inserted into the envelopes of different groups, which were then sealed to prevent revealing the allocations. The subjects were randomly divided into three groups: high volume with ZEEP group; the low volume with 8 cm H2O PEEP group; and the low volume with 8 cm H2O PEEP and recruitment group. High volume ventilation was a tidal volume of 9 ml/kg IBW and ZEEP and an inspiratory to expiratory ratio of 1:2; low volume ventilation was 7 ml/kg IBW and 8 cm H2O PEEP and an inspiratory to expiratory ratio of 1:1. All of the parameters were set by the same type of anesthesia machine (Drager Fa-bius GS, Lubeck, Germany). We changed plates to maintain PETCO2 at between 30 and 40 mmHg. IBW was calculated according to the following formulas: Men: 50 + 0.91 (height [cm] -152.4); or Women: 45.5 + 0.91 (height [cm] -152.4) [15].
Recruitment maneuvers were performed in volume-controlled ventilation every 30 min during tracheal intubation according to the standard as follows: the respiratory rate was 6 breaths/min, the inspiratory to expiratory ratio was 3:1, and PEEP was 8 cm H2O. The tidal volume was increased 4 ml/kg IBW once gradually until plateau pressure of 30 cm H2O was achieved three times [16].
Measurements
A D-lite sensor was used to measure the following variables every 15 min: tidal volume, PEEP, peak pressure, plateau pressure, airway resistance (Raw), and respiratory system dynamic compliance. Samples for arterial blood gases were drawn when the patients entered the operating room, 2 h after ventilation, 10 min after extubation, and when the patients left the operating room. Before and after surgery (on postoperative days 1, 3, 5 and 7), forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) were obtained at the bedside using a portable spirometer (Master-Screen GE, Care Fusion, America). The patient sat vertically at the bedside and breathed using the mouth though the tube while pinching his or her nose. Then, he or she was asked to inhale as deeply and exhale as forcefully and quickly as possible. We repeated the process 3-5 times to ensure that the highest value was only slightly better than the second highest value [9].
Postoperative observations
The following observations were acquired postoperatively: duration of hospitalization, postoperative pulmonary complications, acute heart failure, primary postoperative intensive care unit (ICU) admission, and in-hospital death. Postoperative pulmonary complications included dyspnea, pneumonia, pneumothorax, respiratory distress and chronic respiratory failure. All of the observations were diagnosed by the pneumology department or the ICU attending physicians.
Statistical analysis
The data are presented as the means ± SDs, medians and quartiles or percentages on an intention-to-treat basis. Comparisons of normally distributed variables were performed with one-way ANOVA, whereas non-parametric test was used for abnormal distributed variables, chi-square test was used for enumeration data. The vital outcome variables were tested with repeated measures ANOVA (group effects), while a mixed-effects model was used for the FEV1 and FVC data. All of the tests were two tailed, and statistical significance was accepted at P<0.05. All of the statistical analyses were performed with SAS software, version 9.13 (sequence retrieval system).
Results
A total of 66 patients were included and randomized into three groups, but 3 patients dropped out because of the use of laparoscopy during surgery. Finally, the number of patients in the high volume with ZEEP group was 22, the number in the low volume with PEEP group was 20, and the number in the low volume with PEEP and recruitment group was 21. One patient in the high volume group was extubated in the ICU on the first postoperative day, so we lost his extubation time. Otherwise, data obtained in the operating theater were available for all of the patients. Spirometry was performed in 58 patients 5 times with some patients abandoning it due to their lack of comfort. The three groups had similar baseline characteristics (Table 1).
Table 1.
Baseline characteristics
| High volume with ZEEP (n=22) | Low volume with 8 cm H2O PEEP (n=20) | Low volume with 8 cm H2O PEEP and recruitment (n=21) | P Value | |
|---|---|---|---|---|
| Age, (mean ± SD), yr | 67.41±5.13 | 66.10±5.46 | 69.67±8.37 | 0.21 |
| Sex, M/F | 15/7 | 10/10 | 13/8 | 0.48 |
| Height, median [IQR], cm | 168 [158-171] | 162.5 [157-169] | 166 [155-171] | 0.55 |
| Body weight, kg | ||||
| Actual, (mean ± SD) | 64.89±12.70 | 58.86±11.78 | 59.95±8.59 | 0.18 |
| Predicted, median [IQR] | 64.2 [54.24-66.93] | 56.94 [49.69-65.11] | 62.38 [47.87-66.93] | 0.48 |
| BMI, (mean ± SD), kg/m2 | 23.62±4.08 | 22.10±3.47 | 22.35±3.23 | 0.35 |
| Preoperative risk index, n (%) | ||||
| Risk class 1 | 2 (9.09) | 1 (5) | 1 (4.76) | 0.12 |
| Risk class 2 | 11 (50) | 9 (45) | 5 (23.81) | |
| Risk class 3 | 8 (36.36) | 10 (50) | 13 (61.90) | |
| Risk class 4 | 1 (4.55) | 0 (0) | 2 (9.52) | |
| Coexisting condition, n (%) | ||||
| Current smoking | 7 (31.82) | 7 (35) | 4 (19.05) | 0.48 |
| Chronic obstructive pulmonary disease | 4 (18.18) | 5 (25) | 4 (19.05) | 0.86 |
| Asthma | 0 (0) | 1 (5) | 0 (0) | 0.32 |
| Type of surgery, n (%) | ||||
| Gastrectomy | 2 (9.09) | 8 (40) | 6 (28.57) | 0.34 |
| Pancreaticoduodenectomy | 1 (4.55) | 1 (5) | 1 (4.76) | |
| Colorectal resection | 14 (63.64) | 9 (45) | 10 (47.62) | |
| Other procedure | 5 (22.73) | 2 (10) | 4 (19.05) |
IQR = interquartile range.
Intraoperative respiratory observation
Owing to the different mechanical ventilator settings, the data on tidal volume and PEEP were significant. Peak pressure, plateau pressure and PETCO2 were higher in the groups with low volume, and Raw was higher in the group with high volume. There were no statistically significant differences in the times of ventilation, surgery and extubation among the three groups (Table 2).
Table 2.
Intraoperative data
| High volume with ZEEP (n=22) | Low volume with 8 cm H2O PEEP (n=20) | Low volume with 8 cm H2O PEEP and recruitment (n=21) | P Value | |
|---|---|---|---|---|
| Tidal volume, median [IQR], ml | 580 [490-600] | 380 [330-460] | 440 [340-470] | <0.0001 |
| Tidal volume, median [IQR], ml/kg of predicted body weight | 9.19 [9.06-9.26] | 6.93 [6.65-7.07] | 7.01 [6.89-7.1] | <0.0001 |
| PEEP, median [IQR], cm H2O | ||||
| Baseline | 2 [2-2] | 8 [8-8] | 8 [8-8] | <0.0001 |
| End of surgery | 1.5 [1-2] | 8 [8-8] | 8 [8-9] | <0.0001 |
| Peak, median [IQR], cm H2O | ||||
| Baseline | 14 [13-17] | 16 [15-17] | 16 [16-17] | 0.03 |
| End of surgery | 14 [12-17] | 16 [16-17] | 15 [15-17] | 0.03 |
| Plateau pressure, median [IQR], cm H2O | ||||
| Baseline | 12.5 [11-15] | 14.5 [14-15.5] | 15 [15-16] | 0.003 |
| End of surgery | 13 [11-16] | 15 [15-16] | 14 [13-16] | 0.01 |
| Raw, cm H2O/(L·s) | ||||
| Baseline median [IQR], | 11.50 [9-14] | 9 [8-10.50] | 9 [7-12] | 0.04 |
| End of surgery, (mean ± SD) | 8.64±2.57 | 6.8±1.96 | 7.43±2.31 | 0.004 |
| PETCO2, mmHg | ||||
| Baseline, median [IQR] | 32.50 [30-37] | 35 [31.50-36.50] | 33 [32-35] | 0.65 |
| End of surgery, (mean ± SD) | 31.86±3.36 | 34.6±2.74 | 34.33±2.5 | 0.005 |
| Duration of mechanical ventilation, median [IQR], h | 2.87 [2.25-3.25] | 3.32 [2.67-3.77] | 3.45 [2.50-3.62] | 0.46 |
| Duration of surgery, median [IQR], h | 2.48 [2-3.25] | 3.09 [2.59-3.71] | 3 [2.15-3.47] | 0.22 |
| Duration of extubation, median [IQR], min | 15.50 [12-19] | 18.50 [14.50-22.50] | 20 [16-24] | 0.11 |
IQR = interquartile range.
Arterial blood gas analysis
There were no significant differences among the three groups before surgery. While intraoperative partial pressure of carbon dioxide (Pco2), postoperative PH and Pco2 were significantly different (P<0.05), intraoperative and postoperative hemoglobin and PaO2 showed no significant differences (Table 3). There were no significant differences in intraoperative PaO2/FiO2 ratio or different changes over time among the three groups (P=0.31, and group effect over time P=0.14). At 2 h after ventilation, the PaO2/FiO2 ratios of the three groups were 382.21±88.03, 450.10±70.29 and 442.08±93.46, respectively. The values were significantly greater in the two groups with low volume compared with the high volume group (P<0.05), but there was no significant difference between the two low volume groups (Figure 1; P=0.76).
Table 3.
Intraoperative artery blood gas analysis
| High volume with ZEEP (n=22) | Low volume with 8 cm H2O PEEP (n=20) | Low volume with 8 cm H2O PEEP and recruitment (n=21) | P Value | |
|---|---|---|---|---|
| Hemoglobin, (mean ± SD), g/L | ||||
| Preoperation | 128.59±22.65 | 126.70±23.82 | 125.33±20.17 | 0.89 |
| Intraoperation | 113.64±17.17 | 106.50±17.69 | 108.67±12.84 | 0.34 |
| Postoperation | 120.64±20.33 | 110.75±31.21 | 113.43±14.94 | 0.36 |
| PH, median [IQR] | ||||
| Preoperation | 7.44 [7.42-7.47] | 7.44 [7.43-7.45] | 7.43 [7.42-7.45] | 0.72 |
| Intraoperation | 7.40 [7.38-7.42] | 7.36 [7.32-7.4] | 7.37 [7.34-7.4] | 0.06 |
| Postoperation | 7.36 [7.33-7.38] | 7.33 [7.31-7.35] | 7.35 [7.34-7.38] | 0.02 |
| PcO2, mmHg | ||||
| Preoperation, median [IQR] | 35 [34-39] | 37 [35-39.50] | 35 [32-36] | 0.07 |
| Intraoperation, median [IQR] | 37.50 [35-40] | 40.50 [37.50-44] | 38 [36-40] | 0.04 |
| Postoperation, (mean ± SD) | 41.68±3.92 | 42.6±4.48 | 39.05±4.64 | 0.03 |
| PO2, mmHg | ||||
| Preoperation, median [IQR] | 87 [79-92] | 85 [79-100.50] | 93 [82-109] | 0.24 |
| Intraoperation, (mean ± SD) | 234±86.5 | 235.2±34.76 | 244.9±55.28 | 0.83 |
| Postoperation, median [IQR] | 81.50 [66-88] | 75.50 [69.50-88] | 84 [74-93] | 0.56 |
IQR = interquartile range.
Figure 1.
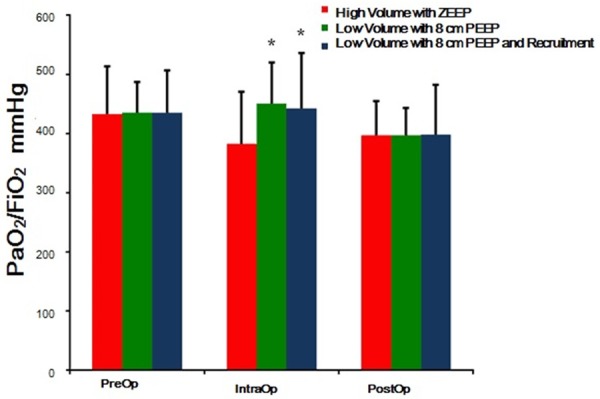
Pre-, intra- and postoperative PaO2/FiO2 ratio in three groups. *P<0.05 vevsus High volume with ZEEP group intra-operation.
Dynamic pulmonary compliance
During anesthesia, there was no significant differences in pulmonary compliance among the three groups (P=0.50), but different changes occurred over time (Figure 2; Group effect over time P<0.001). Compliance in the low volume with PEEP and recruitment group remained at the original level. However, compliance in the other two groups decreased over time.
Figure 2.
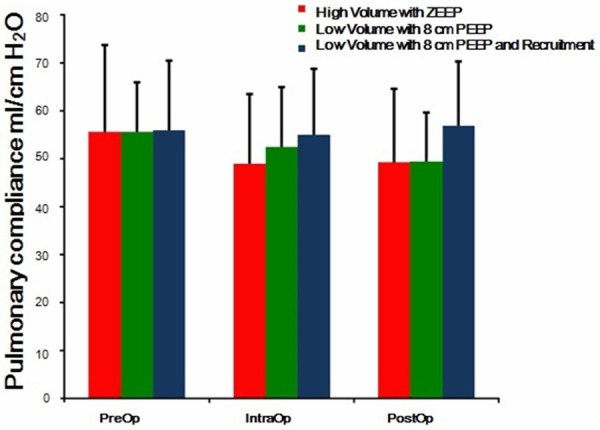
Pre-, intra- and postoperative Pulmonary compliance in three groups. Group effect over time P<0.001. The individual comparisons show no statistical significance.
Spirometry
There were no significant differences in FEV1 or FVC among the three groups (P=0.32 and 0.09, respectively), but both values underwent changes over time (Group effect over time P<0.001). On postoperative day 1, FEV1 in the low volume with PEEP and recruitment group was significantly higher than in the other two groups (mean ± SD): 1.52±0.37 versus 0.95±0.38 (P<0.001) and 1.52±0.37 versus 0.95±0.34 (P<0.001), respectively (Figure 3). The values of FVC on postoperative day1 in the three groups were 1.25±0.51, 1.25±0.44 and 1.77±0.6, respectively; the value in the low volume with PEEP and recruitment group was significantly higher than in the other two groups (P<0.05). The values of FVC on postoperative day3 in the three groups were 1.31±0.37, 1.58±0.4 and 1.95±0.68, and the value in the low volume with PEEP and recruitment group was significantly higher than in the other two groups (Figure 4; P<0.05). There were no significant differences between the high volume with ZEEP group and the low volume with PEEP group in FEV1 or FVC with simple effects.
Figure 3.
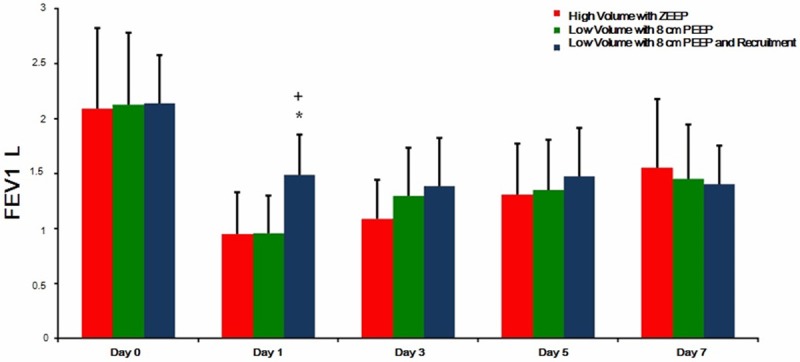
FEV1 in three groups pre-operation, on postoperative day 1, 3, 5 and 7. Group effect over time P<0.001, *P<0.05 vevsus High volume with ZEEP group on postoperative day 1, + P<0.05 vevsus Low volume with 8 cm H2O PEEP group on postoperative day 1.
Figure 4.

FVC in three groups pre-operation, on postoperative day 1, 3, 5 and 7. Group effect over time P<0.001, *P<0.05 vevsus High volume with ZEEP group on postoperative day 1, 3 and 5, + P<0.05 vevsus Low volume with 8 cm H2O PEEP group on postoperative day 1 and 3.
Postoperative observation
The results for length of hospital stay, postoperative pulmonary complications, primary postoperative ICU admissions, acute heart failure and in-hospital deaths showed no significant differences among the three groups (Table 4).
Table 4.
Postoperative observation
| High volume with ZEEP (n=22) | Low volume with 8 cm H2O PEEP (n=20) | Low volume with 8 cm H2O PEEP and recruitment (n=21) | P Value | |
|---|---|---|---|---|
| Duration of stay in hospital, median [IQR], days | 21.50 [20-31] | 18 [16-24] | 21 [19-30] | 0.09 |
| Pulmonary complication, n (%) | 2 (9.09) | 0 (0) | 1 (4.76) | 0.77 |
| Respiratory failure, n (%) | 1 (4.55) | 0 (0) | 1 (4.76) | 1.00 |
| Exintubation, n (%) | 1 (4.55) | 0 (0) | 1 (4.76) | 1.00 |
| Pneumonia, n (%) | 1 (4.55) | 0 (0) | 1 (4.76) | 1.00 |
| Pneumothorax, n (%) | 0 (0) | 0 (0) | 0 (0) | 1.00 |
| ICU admission, n (%) | 4 (18.18) | 0 (0) | 4 (19.05) | 0.11 |
| Acute cardiac failure, n (%) | 1 (4.55) | 0 (0) | 0 (0) | 1.00 |
| Death in hospital, n (%) | 1 (4.55) | 0 (0) | 0 (0) | 1.00 |
IQR = interquartile range.
Discussion
The low volume groups, with tidal volumes of 7 ml/kg IBW, showed some advantages during surgery regarding the PaO2/FiO2 ratio and pulmonary compliance, compared with the high volume group, with a tidal volume of 9 ml/kg IBW. The low volume with PEEP and recruitment group recovered the best over time with regard to postoperative FEV1 and FVC.
High tidal volume is one of the factors that induced ventilator-associated lung injury in healthy patients [17]. It led to overdistention, alveolar rupture and barotrauma. Nevertheless, low tidal volume can cause atelectasis, hypoxemia [18] and pulmonary inflammation [19]. However, it can be prevented by the incorporation of PEEP, and the alveoli can be stabilized with PEEP greater than 5 cm H2O. In another study, PEEP was found to decreasing the death rate of patients whose PaO2/FiO2 ratios were less than 200 mmHg [20]. In our study, at 2 hours after ventilation, the PaO2/FiO2 ratio was significantly higher in the groups with low volume, but there was no significant difference between the two low tidal volume groups. It seemed that PEEP might play a more important role in enhancing the intraoperative PaO2/FiO2 ratio than in recruitment. The strategy of low tidal volume, with PEEP and recruitment or not, might be better for the PaO2/FiO2 ratio during abdominal surgery.
Dynamic lung compliance was affected by the elasticity of lung tissue and Raw. During ventilation, the pulmonary alveoli were overdistented [21], resulting in atelectasis of nearby tissue and thus protein effusion; the activity of pulmonary surfactant decreased, and pulmonary compliance worsened. PEEP, in theory, could keep the alveoli expanding and prevent them from expanding and collapsing repeatedly [22], which would be good for the generation of pulmonary surfactant and the maintenance of lung compliance. Previous randomized, controlled trials have already discussed the influence of ventilation settings, and their conclusions conflicted because recruitment was seldom applied in them [5,23,24]. In our study, during anesthesia, pulmonary compliance in the low volume with PEEP and recruitment group remained the same, while in the high volume and low volume with PEEP groups, it decreased over time. This finding indicated that PEEP combined with recruitment could stop pulmonary compliance from decreasing. Because recruitment can increase the expansion of small airways and enhance the stability of the alveoli, it can successfully increase patients’ lung compliance.
Rothen [25] noted that sustained inspiratory pressure of more than 40 cm H2O was needed to reverse fully anesthesia-induced atelectasis in healthy patients. However, research has shown that recruitment can directly overdistend aerated alveoli, paradoxically resulting in increased ventilation-induced lung injury [26,27]. We paid attention to and controlled these parameters to within safe ranges. Our patients in this study did not have severe diseases of the respiratory system, and we did not detect any severe intraoperative complications in any of them.
Postoperative pulmonary function in abdominal surgery patients was restricted by decreased lung compliance, pain of incision, diaphragmatic dysfunction and ventilator muscle activity in an animal experiment [28]. Some research has reported that pain could decrease indices of pulmonary function [29,30]. To eliminate indeterminate factors, each patient received an epidural tube for three days after surgery to keep the VAS score for pain ≤3. In our study, FEV1 and FVC underwent different changes over time among the three groups. FEV1 and FVC in the low volume with PEEP and recruitment group were significantly higher than in the other groups on postoperative day 1, in accordance with the changes in pulmonary compliance over time. There were no significant differences between the high volume with ZEEP group and the low volume with PEEP group. Treschan [16] indicated that impaired lung function after major abdominal surgery was not improved by low tidal volume ventilation. It is particularly worth mentioning that recruitment maneuvers were excluded from the strategy of W. Kaisers. His results supported our outcomes as well.
In future studies, we will increase the simple size and conduct research in patients with severe diseases of the respiratory system.
Conclusion
Low tidal volume with PEEP and recruitment, which is a protective ventilation strategy, showed its advantages in maintaining the intraoperative pulmonary compliance and in expediting the recovery of the 1st postoperative day’s pulmonary function in patients who underwent major non-laparoscopic abdominal surgery.
Disclosure of conflict of interest
None.
References
- 1.Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, Gawande AA. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372:139–144. doi: 10.1016/S0140-6736(08)60878-8. [DOI] [PubMed] [Google Scholar]
- 2.Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242:326–341. doi: 10.1097/01.sla.0000179621.33268.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schultz MJ, Haitsma JJ, Slutsky AS, Gajic O. What tidal volumes should be used in patients without acute lung injury? Anesthesiology. 2007;106:1226–1231. doi: 10.1097/01.anes.0000267607.25011.e8. [DOI] [PubMed] [Google Scholar]
- 4.Serpa Neto A, Hemmes SN, de Abreu MG, Pelosi P, Schultz MJ. Protocol for stematic review and individual patient data meta-analysis of benefit of so-called lung-protective ventilation settings in patients under general anesthesia for surgery. Syst Rev. 2014;3:2. doi: 10.1186/2046-4053-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brower RG, Lanken PN, Maclntyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT. Higher versus Lower Positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J med. 2004;351:327–336. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 6.Futier E, Constantin JM, Jaber S. Protective lung ventilation in operating room: a systematic review. Minerva Anestesiol. 2014;80:726–735. [PubMed] [Google Scholar]
- 7.Chalhoub V, Yazigi A, Sleilaty G, Haddad F, Noun R, Madi-Jebara S, Yazbeck P. Effect of vital capacity manoeuvres on arterial oxygenation in morbidly obese patients undergoing open bariatric surgery. Eur J Anaesthesiol. 2007;24:283–288. doi: 10.1017/S0265021506001529. [DOI] [PubMed] [Google Scholar]
- 8.Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, Marret E, Beaussier M, Gutton C, Lefrant JY, Allaouchiche B, Verzilli D, Leone M, De Jong A, Bazin JE, Pereira B, Jaber S. A trial of intraoperative lowtidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–437. doi: 10.1056/NEJMoa1301082. [DOI] [PubMed] [Google Scholar]
- 9.Severgnini P, Selmo G, Lanza C, Chiesa A, Frigerio A, Bacuzzi A, Dionigi G, Novario F, Gregoretti C, de Abreu MG, Schultz MJ, Jaber S, Futier E, Chiaranda M, Pelosi P. Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology. 2013;118:1307–1321. doi: 10.1097/ALN.0b013e31829102de. [DOI] [PubMed] [Google Scholar]
- 10.Amato MB, Barbas CS, Medeiros DM, Schettino Gde P, Lorenzi Filho G, Kairalla RA, Deheinzelin D, Morais C, Fernandes Ede O, Takagaki TY. Beneficial effects of the “open lung approach” with low distending pressures in acute respiratory distress syndrome. A prospective randomized study on mechanical ventilation. Am J Respir Crit Care Med. 1995;152:1835–1846. doi: 10.1164/ajrccm.152.6.8520744. [DOI] [PubMed] [Google Scholar]
- 11.Piccinni P, Dan M, Barbacini S, Carraro R, Lieta E, Marafon S, Zamperetti N, Brendolan A, D'Intini V, Tetta C, Bellomo R, Ronco C. Early isovolaemic haemofiltration in oliguric patients with septic shock. Intensive Care Med. 2006;32:80–86. doi: 10.1007/s00134-005-2815-x. [DOI] [PubMed] [Google Scholar]
- 12.Szakmán T, Márton S, Molnár Z. Procalcitonin and PaO2/FiO2 ratio as predictors of mortality in the early postoperative period after esophagectomy. Magy Seb. 2002;55:16–23. [PubMed] [Google Scholar]
- 13.Suarez-Sipmann F, Bohm SH, Tusman G, Pesch T, Thamm O, Reissmann H, Reske A, Magnusson A, Hedenstierna G. Use of dynamic compliance for open lung positive end-expiratory pressure titration in an experimental study. Crit Care Med. 2007;18:214–221. doi: 10.1097/01.CCM.0000251131.40301.E2. [DOI] [PubMed] [Google Scholar]
- 14.Maisch S, Reissmann H, Fuellekrug B, Weismann D, Rutkowski T, Tusman G, Bohm SH. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth Analg. 2008;18:175–181. doi: 10.1213/01.ane.0000287684.74505.49. [DOI] [PubMed] [Google Scholar]
- 15.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 16.Treschan TA, Kaisers W, Schaefer MS, Bastin B, Schmalz U, Wania V, Eisenberger CF, Saleh A, Weiss M, Schmitz A, Kienbaum P, Sessler DL, Pannen B, Beiderlinden M. Ventilation with low tidal volumes during upper abdominal surgery does not improve postoperative lung function. Br J Anaesth. 2012;109:263–271. doi: 10.1093/bja/aes140. [DOI] [PubMed] [Google Scholar]
- 17.Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM, Rana R, St Sanver JL, Lymp JF, Afessa B, Hubmayr RD. Ventilatorassociated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med. 2003;32:1817–1824. doi: 10.1097/01.ccm.0000133019.52531.30. [DOI] [PubMed] [Google Scholar]
- 18.Hickling KG, Henderson SJ, Jackson R. Low mortality associated with low volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome. Intensive Care Med. 1990;16:372–377. doi: 10.1007/BF01735174. [DOI] [PubMed] [Google Scholar]
- 19.Chu EK, Whitehead T, Slutsky AS. Effects of cyclic opening and closing at low- and high-volume ventilation on bronchoalveolar lavage cytokines. Crit Care Med. 2004;32:168–174. doi: 10.1097/01.CCM.0000104203.20830.AE. [DOI] [PubMed] [Google Scholar]
- 20.Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, Slutsky AS, Pullenayegum E, Zhou Q, Cook D, Brochard L, Richard JC, Lamontagne F, Bhatnagar N, Stewart TE, Guyatt G. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303:865–873. doi: 10.1001/jama.2010.218. [DOI] [PubMed] [Google Scholar]
- 21.Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiment. Med. 1944;23:281–358. [Google Scholar]
- 22.Slutsky AS, Ranieri VM. Ventilator-Induced Lung Injury. N Engl J Med. 2013;369:2126–2136. doi: 10.1056/NEJMra1208707. [DOI] [PubMed] [Google Scholar]
- 23.Futier E, Constantin JM, Pelosi P, Chanques G, Massone A, Petit A, Kwiatkowski F, Bazin JE, Jaber S. Noninvasive ventilation and alveolar recruitment maneuver improve respiratory function during and after intubation of morbidly obese patients: a randomized controlled study. Anesthesiology. 2011;114:1354–1363. doi: 10.1097/ALN.0b013e31821811ba. [DOI] [PubMed] [Google Scholar]
- 24.Wolthuis EK, Choi G, Dessing MC, Bresser P, Lutter R, Dzoljic M, van der Poll T, Vroom MB, Hollmann M, Schultz MJ. Mechanical ventilation with lower tidal volumes and positive endexpiratory pressure prevents pulmonary in flammation in patients without preexisting lung injury. Anesthesiology. 2008;108:46–54. doi: 10.1097/01.anes.0000296068.80921.10. [DOI] [PubMed] [Google Scholar]
- 25.Rothen HU, Sporre B, Englberg G, Rothen HU, Sporre B, Engberg G, Wegenius G, Hedenstierna G. Reexpansion of atelectasis during general anaesthesia may have a prolonged effect. Acta Anaesthesiol Scand. 1995;39:118–125. doi: 10.1111/j.1399-6576.1995.tb05602.x. [DOI] [PubMed] [Google Scholar]
- 26.Fan E, Wilcox ME, Brower RG, Steawart TE, Mehta S, Lapinsky SE, Meade MO, Ferguson ND. Recruitment maneuvers for acute lung injury: a systematic review. Am J Respir Crit Care Med. 2008;178:1156–1163. doi: 10.1164/rccm.200802-335OC. [DOI] [PubMed] [Google Scholar]
- 27.Lapinsky SE, Mehta S. Bench-to-bedside review: recruitment and recruiting maneuvers. Crit Care. 2005;9:60–65. doi: 10.1186/cc2934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dureuil B, Cantineau JP, Desmonts JM. Effects of upper or lower abdominal surgery on diaphragmatic function. Br J Anaesth. 1987;59:1230–1235. doi: 10.1093/bja/59.10.1230. [DOI] [PubMed] [Google Scholar]
- 29.Michelet P, Guervilly C, Hélaine A, Avaro JP, Blayac D, Gaillat F, Dantin T, Thomas P, Kerbaul F. Adding ketamine to morphine for patientcontrolled analgesia after thoracic surgery: influence on morphine consumption, respiratory function, and nocturnal desaturation. Br J Anaesth. 2007;99:396–403. doi: 10.1093/bja/aem168. [DOI] [PubMed] [Google Scholar]
- 30.Josepha C, Gaillata F, Duponqa R, Lieven R, Baumstarckc K, Thomasd P, Penot-Ragone C, Kerbaul F. Is there any benefit to adding intravenous ketamineto patient-controlled epidural analgesia after thoracic surgery? A randomized double-blind study. Eur J Cardiothorac Surg. 2012;42:e58–65. doi: 10.1093/ejcts/ezs398. [DOI] [PubMed] [Google Scholar]


