Abstract
[Purpose] To investigate the predictive value of maximum inspiratory pressure (MIP) and the rapid shallow breathing index (RSBI) in a ventilator weaning protocol and to evaluate the differences between clinical and surgical patients in the intensive care unit. [Subjects and Methods] Patients aged ≥15 years who underwent orotracheal intubation for mechanical ventilation and who met the criteria of the weaning protocol were included in the study. Receiver operating characteristic (ROC) curves were calculated for the analysis of each index. [Results] Logistic regression analysis was also performed. MIP showed greater sensitivity and specificity [area under the curve (AUC): 0.95 vs. 0.89] and likelihood ratios (LR) (positive(+): 20.85 vs. 9.45; negative(−): 0.07 vs. 0.17) than RSBI in the overall sample (OS) as well as in clinical patients (CP) (AUC: 0.99 vs. 0.90; LR+: 24.66 vs. 7.22; LR-: 0.01 vs. 0.15) and surgical patients (SP) (AUC: 0.99 vs. 0.87; LR+: 9.33 vs. 5.86; LR−: 0.07 vs. 0.14). The logistic regression analysis revealed that both parameters were significantly associated with the weaning success. The MIP showed greater accuracy than the RSBI (OS: 0.93 vs. 0.85; CP: 0.98 vs. 0.87; SP: 0.93 vs. 0.87). [Conclusion] Both parameters are good predictors of successful ventilator weaning.
Key words: Mechanical ventilation, Ventilator weaning, Physiological predictor indices
INTRODUCTION
After placing a patient on mechanical ventilation, the main goal is to define the best time to begin the weaning process1). Weaning is considered successful when a patient can stay off mechanical ventilation for more than 48 h2, 3). The greatest difficulty in the weaning process is the absence of one or more variables (mechanical, hemodynamic, neurological or exchange gas) and/or an adequate index for accurately predicting successful weaning4, 5).
Performing the transition process empirically prolongs the duration of mechanical ventilation, with consequent increases in treatment costs and the risk of death3, 6). It is therefore of extreme importance to establish adequate protocols to ensure the highest possible success rate for ventilator weaning. To date, there is no single index that can be used to determine weaning success7,8,9). However, maximum inspiratory pressure (MIP) and the rapid shallow breathing index (RSBI) are widely used owing to their ease of application in daily clinical practice10). MIP represents maximum pressure during inhalation against an obstructed airway11) and is used to assess inspiratory muscle strength12). In the intensive care unit (ICU), the MIP of patients on mechanical ventilation, even those with a low degree of cooperation for the execution of voluntary maneuvers, is used as a predictor of weaning success13). The RSBI is the ratio of respiratory rate and spontaneous tidal volume14, 15).
While MIP and RSBI are frequently used to predict weaning success, their predictive accuracy has not been well investigated. Thus, the aim of the present study was to investigate the ability of MIP and RSBI to predict weaning success in ventilated clinical and surgical patients.
SUBJECTS AND METHODS
A prospective cross-sectional study was carried out at the adult ICU of the Mandaqui Hospital Complex in the city of Sao Paulo, Brazil, between July 2011 and July 2013. This study was approved by the human research ethics committee of the institution, and written informed consent obtained from each subject or patient, or family.
The inclusion criteria were age ≥15 years, mechanical ventilation with orotracheal intubation, and hemodynamic stability. The exclusion criteria were progressive neuromuscular disease, a history of dependence on mechanical ventilation at home, interruption of mechanical ventilation prior to completing 24 h of respiratory support, and tracheostomy.
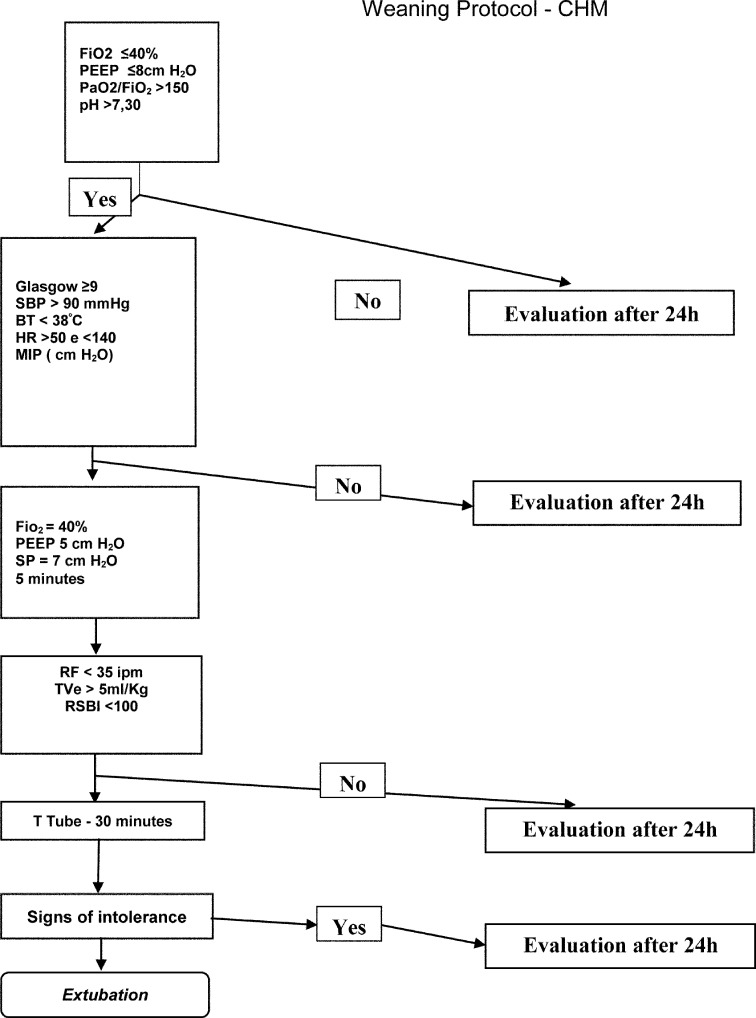
Following the preliminary analysis for inclusion, the ventilator weaning process was initiated using the following protocol: (1) Cause of need for mechanical ventilation resolved or controlled; (2) Score > 9 on the Glasgow coma scale, presence of respiratory drive; (3) Systolic blood pressure (SBP) > 90 mmHg; (4) At most a minimal need for vasoactive drugs; body temperature < 38 °C; (5) Inspired oxygen fraction (FiO2) < 40%, positive end-expiratory pressure (PEEP) < 8 cmH2O, pH > 7.30; and (6) Oxygen partial pressure/inspired oxygen fraction (PaO2/FiO2) ratio > 150 (Fig. 1). Patients failing to meet these criteria were continued on mechanical ventilation for at least 24 h, followed by further evaluation.
Fig. 1.
. Weaning protocol
FiO2: fraction of inspired oxygen; PEEP: positive end-expiratory pressure; PaO2/FiO2: ratio of arterial oxygen and fraction of inspired oxygen, pH: potential of hydrogen; Glasgow: coma scale; SBP: systolic blood pressure, HR: heart rate, Tax: axillary temperature; MIP: maximal inspiratory pressure, SP: pressure support, Rf: respiratory rate, TV: tidal volume, IRRS: index of rapid shallow breathing; T Tube: peace for oxygen therapy
During the next stage of the protocol, the enrolled subjects were placed on support pressure (SP) ventilation (SP = 7 cmH2O, PEEP = 5 cmH2O and FiO2 40%) for 5 min to evaluate respiratory mechanics which included: (1) Minute volume (MV); (2) Respiratory frequency (Rf); (3) Expiratory tidal volume (TVe); and (4) RSBI. If the RSBI was within the normal range (<100), the patient was placed on spontaneous breathing with a T tube for 30 min and received 5 L/min of oxygen. This flow could be increased to a maximum of 10 L/min if necessary to maintain an oxygen saturation (SpO2) >90%. Extubation was performed if the patient showed no signs of intolerance to the spontaneous breathing trial (SBT), such as tachypnea, desaturation, use of accessory respiratory muscles, or a diminished level of consciousness.
MIP was measured digitally as described by de Souza et al.13), who found no difference between digital and analog pressure gauges. The values were taken from the mechanical ventilation equipment (model 3010; manufacturer: TECME S.A., Argentina; distributor: Dixtal Biomédica®, Brazil) when the patient was on SP ventilation. The maneuver was performed following the manufacturer’s recommendations three times, with a 3-min interval between readings. The best value of the three readings was chosen.
The RSBI was calculated at two different moments: (1) after 5 min on SP ventilation and (2) immediately after 30 min of nebulization with the T tube. As no statistically significant difference was found between the two time periods, the decision was made to evaluate the RSBI obtained at 30 min.
The APACHE II index was used to determine the severity of the patients16, 17) and was calculated 24 h after admission to the ICU. All decisions regarding the time to initiate ventilator weaning and extubation were approved by the ICU medical, physiotherapeutic, and nursing teams.
Weaning success was defined as spontaneous breathing for more than 48 h. A weaning attempt was defined as the initiation of the SBT, followed by any sign of intolerance or physiological index below that established in the protocol. The following data were recorded for subsequent analysis: (1) Duration of mechanical ventilation; (2) Number of attempts at ventilator weaning and extubation; (3) Age of patient; (4) PaO2/FiO2 ratio; (5) RSBI; (6) MIP; (7) APACHE II index; (8) Death; and (8) Weaning success rate.
The Kolmogorov-Smirnov test was used to determine the distribution of the data. As a normal distribution was found, parametric analysis was performed and the data were expressed as mean ± standard deviation. The patients were grouped based on weaning success (successful vs. unsuccessful as previously defined). Analyses were carried out for the overall sample as well as with the separation of the sample into clinical and surgical patients. Logistic regression analysis was performed to calculate the contribution of each variable in the regression model. The area under the receiver operating characteristic (ROC) curve was calculated to predict the predictive performance of MIP and RSBI by using the method described by Hanley and McNeil18) and subsequently classified using the guidelines proposed by Swets19); (1) Area under the curve (AUC) ≤0.5 is considered non-informative; (2) AUC between 0.5 and 0.7 indicates a low degree of precision; (3) AUC between 0.7 and 0.9 indicates a moderate degree of precision; and (4) AUC between 0.9 and 1.0 is considered highly precise to perfect.
After the calculation of the positive likelihood ratio (LR+) and negative likelihood ratio (LR−), the values were interpreted as follows: (1) LR+ = 0.5 and LR− = 2.0 indicate that the index analyzed is associated with small changes in the likelihood of success or failure; (2) LR+ 2 to 5 and LR− 0.3 to 0.5 indicate that the index is associated with small, but potentially important changes in the likelihood of success or failure; (3) LR+ 5 to 10 and LR− 0.1 to 0.3 indicate that the index is associated with a clinically important likelihood of success or failure; and (4) LR+ > 10 and LR− < 0.1 indicate that the index is associated with a very large likelihood of success or failure20). The accuracy of the MIP and RSBI was defined by the following equation: (true positives + true negatives)/(true positives + true negatives + false positives + false negatives).
RESULTS
One hundred ninety-five patients were evaluated: 59 (30.3%) from general surgery, 36 (18.5%) from neurosurgery, 23 (11.8%) with lung disease, 15 (7.7%) with heart disease, 36 (18.5%) with neurological clinical conditions, 18 (9.2%) with general clinical conditions, and eight (4.1%) with other conditions. Ventilator weaning was successful in 150 patients (76.9%) and unsuccessful in 45 patients (23.1%). Table 1 displays the clinical and demographic characteristics of the patients. Both groups were similar with regard to gender and age distribution. The successful group had a significantly higher mean Glasgow score and MIP as well as a significantly lower mean RSBI, duration of MV, number of weaning attempts, and APACHE II score in comparison to the unsuccessful group.
Table 1. Demographic and clinical variables of the weaning protocol results.
| Success group n= 150 |
Failure group n= 45 |
|
|---|---|---|
| Age (years) | 53.6±20.6 | 58.2±18.1 |
| Gender M/F (%) | 58.66/40.66 | 48.88/53.33 |
| Glasgow | 10.64±0.5 | 9.22±0.5* |
| MIP (cmH2O) | 59.29±13.17 | 28.69±11.05* |
| Time of MV(days) | 4.5±3.5 | 8.71±4.1* |
| Number of trials | 1.06±0.3 | 2.24±0.5* |
| RSBI | 35.58±14.63 | 62.59±15.42* |
| PaO2/FiO2 | 349.8±105.6 | 304.1±73.3* |
| pH | 7.42±0.06 | 7.43±0.07* |
| APACHE II | 7.65±4.0 | 21.2±3.6* |
MIP: maximal inspiratory pressure; MV: mechanical ventilation; RSBI: rapid shallow breathing index; PaO2/FiO2: arterial oxygen pressure and fraction of inspired oxygen ratio; pH: potential of hydrogen; APACHE II: Acute Physiology and Chronic Health Evaluation II. *p<0.05
In the analysis of the predictive value of the indices analyzed regarding weaning success in the overall sample, the MIP showed greater sensitivity and specificity than the RSBI (Table 2). Likewise, the MIP showed greater sensitivity and specificity than the RSBI in the separate analyses of the clinical and surgical patients (Table 2). The logistic regression analysis revealed that both the MIP and RSBI contributed significantly to predicting ventilator weaning success. After adjusting for the RSBI, for each increase of 1 cmH2O, there is a 15 times greater chance of successful weaning, and after adjusting for MIP, for each 1 point decrease in RSBI, there is a 6 times greater chance of successful weaning (Table 3).
Table 2. Sensitivity, specificity, positive and negative predictive values, diagnostic accuracy, positive and negative Likelihood ratios.
| Index | SENS | SPE | PPV | NPV | DA (%) | LR+ | LR− |
|---|---|---|---|---|---|---|---|
| MIP | |||||||
| General Group | 0.93 | 0.95 | 0.98 | 0.79 | 0.93 | 20.85 | 0.07 |
| Clinics | 0.99 | 0.96 | 0.98 | 0.96 | 0.98 | 24.66 | 0.01 |
| Surgical | 0.93 | 0.90 | 0.97 | 0.78 | 0.93 | 9.33 | 0.07 |
| RSBI | |||||||
| General Group | 0.84 | 0.91 | 0.97 | 0.63 | 0.85 | 9.45 | 0.17 |
| Clinics | 0.89 | 0.88 | 0.95 | 0.68 | 0.87 | 7.22 | 0.15 |
| Surgical | 0.88 | 0.85 | 0.95 | 0.65 | 0.87 | 5.86 | 0.14 |
MIP: maximal inspiratory pressure; RSBI: rapid shallow breathing index; Sens: Sensitivity; Spe: specificity; PPV: positive predictive value; NPV: negative predictive value; DA: diagnostic accuracy; LR+: positive likelihood ratio; LR−: negative likelihood ratio
Table 3. Logistic regression (−2 log likelihood = 71.436a).
| Ods ratio | CI = 95% | ||
|---|---|---|---|
| MIP | 1.154 | 1.093 | 1.217* |
| RSBI | 0.943 | 0.097 | 0.981* |
MIP: maximal inspiratory pressure; RSBI: rapid shallow breathing index; CI: confidence interval; Ods ratio: after adjusting for RSBI, for each increase of 1 cmH2O, there is a 15 times greater chance of successful weaning, and after adjusting for MIP, for each 1 point decrease in RSBI, there is a 6 times greater chance of successful weaning, *p<0.05
DISCUSSION
The main finding of the present study was that both MIP and the RSBI of patients with ventilator weaning success differed significantly from those in the unsuccessful group. Moreover, in the analysis of sensitivity and specificity (area under the ROC curve), MIP demonstrated a greater precision in predicting weaning success than did RSBI.
There is a strong relationship between the MIP necessary to generate an adequate tidal volume and this relationship has been described as the main condition contributing to unsuccessful ventilator weaning21, 22). The fact that mechanical ventilation causes rapid diaphragm hypotrophy and weakness in humans23, 24) may explain why the MIP demonstrated a better predictive capacity regarding weaning success than RSBI in the present investigation. In previous studies, MIP has demonstrated considerable variation in its predictive capacity of weaning success11, 13). Nemer et al. and Souza et al.10, 13) reported AUC values of 0.52 and 0.79, respectively. In the present study however, MIP showed high predictive capacity in both clinical and surgical patients, with AUC values above 0.90 in the overall sample as well as in the separate analyses of these two groups of patients.
The RSBI is the most widely used index for predicting the success of ventilator weaning, as it reflects respiratory muscle endurance. However, respiratory muscle strength is not considered in the calculation of this index. A number of studies report AUC values ranging from 0.72 to 0.89 in the analysis of the predictive capacity of the RSBI regarding weaning success10, 20, 25,26,27, 28), which is in agreement with the values found in the present study. Nemer et al.10) recently proposed a new index that demonstrated better performance in predicting weaning success in comparison to the RSBI. This new index integrates variables of respiratory mechanics, such as respiratory compliance and gas exchange, but the calculation does not consider MIP.
In the present study, the logistic regression analysis showed that both the MIP and RSBI contributed significantly to explaining ventilator weaning success, with a greater odds ratio found for MIP. Another important finding in the present study was the non-difference in the PaO2/FiO2 ratio between the successful and unsuccessful groups. This suggests little importance of the variation in oxygen levels regarding the prediction of ventilation weaning success in the present sample. It is likely that since the patients underwent the SBT, they always had a PaO2/FiO2 ratio higher than 150, which characterizes the absence of a gas exchange disorder.
The MIP in our study was measured through mechanical ventilation, rather than by using an analog manometer, which is the gold standard for measuring such a variable. However, de Souza et al.13) showed that the values of MIP measured digitally on a mechanical ventilator are similar to those measured with the analog manometer. Another aspect to be considered in our study was the wide age range and types of diagnoses of individuals in our sample (clinical and surgical). However, we gathered the data in a general ICU and this has a better representation of the population seen in our service.
REFERENCES
- 1.Hess DR, MacIntyre NR: Ventilator discontinuation: why are we still weaning? Am J Respir Crit Care Med, 2011, 184: 392–394. [DOI] [PubMed] [Google Scholar]
- 2.Macintyre NR: Evidence-based assessments in the ventilator discontinuation process. Respir Care, 2012, 57: 1611–1618. [DOI] [PubMed] [Google Scholar]
- 3.Frutos-Vivar F, Ferguson ND, Esteban A, et al. : Risk factors for extubation failure in patients following a successful spontaneous breathing trial. Chest, 2006, 130: 1664–1671. [DOI] [PubMed] [Google Scholar]
- 4.Tobin MJ, Jubran A: Variable performance of weaning-predictor tests: role of Bayes’ theorem and spectrum and test-referral bias. Intensive Care Med, 2006, 32: 2002–2012. [DOI] [PubMed] [Google Scholar]
- 5.Frutos-Vivar F, Esteban A: Weaning from mechanical ventilation: why are we still looking for alternative methods? Med Intensiva, 2013, 37: 605–617. [DOI] [PubMed] [Google Scholar]
- 6.Vassilakopoulos T, Roussos C, Zakynthinos S: Weaning from mechanical ventilation. J Crit Care, 1999, 14: 39–62. [DOI] [PubMed] [Google Scholar]
- 7.Eskandar N, Apostolakos MJ: Weaning from mechanical ventilation. Crit Care Clin, 2007, 23: 263–274, x. [DOI] [PubMed] [Google Scholar]
- 8.Jubran A, Tobin MJ: Monitoring during mechanical ventilation. Clin Chest Med, 1996, 17: 453–473. [DOI] [PubMed] [Google Scholar]
- 9.Kollef MH, Shapiro SD, Silver P, et al. : A randomized, controlled trial of protocol-directed versus physician-directed weaning from mechanical ventilation. Crit Care Med, 1997, 25: 567–574. [DOI] [PubMed] [Google Scholar]
- 10.Nemer SN, Barbas CS, Caldeira JB, et al. : A new integrative weaning index of discontinuation from mechanical ventilation. Crit Care, 2009, 13: R152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nemer SN, Barbas CS, Caldeira JB, et al. : Evaluation of maximal inspiratory pressure, tracheal airway occlusion pressure, and its ratio in the weaning outcome. J Crit Care, 2009, 24: 441–446. [DOI] [PubMed] [Google Scholar]
- 12.Black LF, Hyatt RE: Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis, 1969, 99: 696–702. [DOI] [PubMed] [Google Scholar]
- 13.de Souza LC, da Silva CT, Jr, Almeida JR, et al. : Comparison of maximal inspiratory pressure, tracheal airway occlusion pressure, and its ratio in the prediction of weaning outcome: impact of the use of a digital vacuometer and the unidirectional valve. Respir Care, 2012, 57: 1285–1290. [DOI] [PubMed] [Google Scholar]
- 14.Verceles AC, Diaz-Abad M, Geiger-Brown J, et al. : Testing the prognostic value of the rapid shallow breathing index in predicting successful weaning in patients requiring prolonged mechanical ventilation. Heart Lung, 2012, 41: 546–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuo PH, Wu HD, Lu BY, et al. : Predictive value of rapid shallow breathing index measured at initiation and termination of a 2-hour spontaneous breathing trial for weaning outcome in ICU patients. J Formos Med Assoc, 2006, 105: 390–398. [DOI] [PubMed] [Google Scholar]
- 16.Knaus WA, Zimmerman JE, Wagner DP, et al. : APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med, 1981, 9: 591–597. [DOI] [PubMed] [Google Scholar]
- 17.Knaus WA, Draper EA, Wagner DP, et al. : APACHE II: a severity of disease classification system. Crit Care Med, 1985, 13: 818–829. [PubMed] [Google Scholar]
- 18.Hanley JA, McNeil BJ: A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology, 1983, 148: 839–843. [DOI] [PubMed] [Google Scholar]
- 19.Swets JA: Measuring the accuracy of diagnostic systems. Science, 1988, 240: 1285–1293. [DOI] [PubMed] [Google Scholar]
- 20.Conti G, Montini L, Pennisi MA, et al. : A prospective, blinded evaluation of indexes proposed to predict weaning from mechanical ventilation. Intensive Care Med, 2004, 30: 830–836. [DOI] [PubMed] [Google Scholar]
- 21.Vassilakopoulos T, Zakynthinos S, Roussos C: The tension-time index and the frequency/tidal volume ratio are the major pathophysiologic determinants of weaning failure and success. Am J Respir Crit Care Med, 1998, 158: 378–385. [DOI] [PubMed] [Google Scholar]
- 22.Carlucci A, Ceriana P, Prinianakis G, et al. : Determinants of weaning success in patients with prolonged mechanical ventilation. Crit Care, 2009, 13: R97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hermans G, Agten A, Testelmans D, et al. : Increased duration of mechanical ventilation is associated with decreased diaphragmatic force: a prospective observational study. Crit Care, 2010, 14: R127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levine S, Nguyen T, Taylor N, et al. : Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med, 2008, 358: 1327–1335. [DOI] [PubMed] [Google Scholar]
- 25.Yang KL, Tobin MJ: A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med, 1991, 324: 1445–1450. [DOI] [PubMed] [Google Scholar]
- 26.Sassoon CS, Mahutte CK: Airway occlusion pressure and breathing pattern as predictors of weaning outcome. Am Rev Respir Dis, 1993, 148: 860–866. [DOI] [PubMed] [Google Scholar]
- 27.Capdevila XJ, Perrigault PF, Perey PJ, et al. : Occlusion pressure and its ratio to maximum inspiratory pressure are useful predictors for successful extubation following T-piece weaning trial. Chest, 1995, 108: 482–489. [DOI] [PubMed] [Google Scholar]
- 28.Corbellini C, Trevisan CB, Villafañe JH, et al. : Weaning from mechanical ventilation: a cross-sectional study of reference values and the discriminative validity of aging. J Phys Ther Sci, 2015, 27: 1945–1950. [DOI] [PMC free article] [PubMed] [Google Scholar]