Abstract
[Purpose] Stroke and other cerebrovascular diseases are major causes of adult mobility problems. Because stroke immobilizes the affected body part, balance training uses the healthy body part to complete the target movement. The muscle utilization rate on the stroke affected side is often reduced which further hinders affected side functional recovery in rehabilitation. [Subjects and Methods] This study tested a newly-developed interactive device with two force plates to measuring right and left side centers of pressure, to establish its efficacy in the improvement of the static standing ability of patients with hemiplegia. An interactive virtual reality game with different side reaction ratios was used to improve patient balance. The feasibility of the proposed approach was experimentally demonstrated. [Results] Although the non-affected-side is usually used to support the body weight in the standing position, under certain circumstances the patients could switch to using the affected side. A dramatic improvement in static standing balance control was achieved in the eyes open condition. [Conclusion] The proposed dual force plate technique used in this study separately measured the affected and non-affected-side centers of pressure. Based on this approach, different side ratio integration was achieved using an interactive game that helped stroke patients improve balance on the affected side. Only the patient who had suffered stroke relatively recently benefited significantly. The proposed technique is of little benefit for patients whose mobility has stagnated to a certain level.
Key words: Stroke, Standing balance, Affected side
INTRODUCTION
Stroke and other cerebrovascular diseases caused by cerebral vascular blockage or bleeding cause loss of normal blood circulation in the affected area and anoxia, resulting in irreversible brain damage which manifests as functional impairments in consciousness, movement, senses, recognition, comprehension, and language. Common mobility impairments include: lateral muscle weakness, abnormal lateral muscle tension, abnormal postural control, abnormal coordination, abnormal movement sequencing and loss of joint coordination. These are all factors which contribute to problems with postural control, thereby affecting standing balance ability1). Standing balance ability in turn is strongly associated with walking speed2). Postural control evaluation and training are important contributors to the rehabilitation of balance, walking ability and other daily living activities performed by stroke patients3, 4).
The modern theory of movement control and movement learning holds that in humans all intentional movements are task-specific5), i.e. the response is specific to the environment or situation. Traditional rehabilitation focuses on practicing specific movements without reference to a meaningful task. However, rehabilitation therapies involving task-specific actions often have better effects than traditional non-task-specific rehabilitation therapies6). According to Barclay-Goddard, Stevenson, Poluha, et al.7), through traditional treatment, stroke patients can increase standing symmetry when using a force plate for treatment. Van Peppen, Kortsmit, Lindeman, et al.8) concluded that stroke patients using visual feedback with traditional treatments showed greater improvements than patients receiving standard treatment only in standing symmetry, postural sway movement with the eyes open and closed, and walking speed9). Dynamic balance ability is the ability to change postural without losing one’s balance10). Limits of stability (LOS: the maximum center of gravity displacement possible without loss of balance) are also reduced in stroke patients. Damage to the central nervous system function directly affects posture, movement, and thus, balance ability. Reduced muscle strength and mobility will also result in deficits in postural control and balance ability11). The hemiparesis that often results from stroke tends to force patients to complete movements using a compensation strategy, e.g. fixing the affected part and using the healthy part to complete the target movement. This behavior will decrease the free movement factors in the central nervous system and reduce the complexity of movement choice, making it easier to complete the intended action. However, this behavior does not require postural control, so nervous impulses to the affected side reduce, which further hinders functional recovery of the affected side in rehabilitation12,13,14). This means that techniques which oblige stroke patients to practice centralized postural and balance control on the affected side will have considerable impact on the stroke patients’ recovery of balance, walking and other mobility-related functions.
In this study, a device to enable stroke patients to learn better movement control during rehabilitation than relying on traditional rehabilitation therapies was tested. The device uses two force plates to measure right and left side centers of foot pressure (COP), and visual feedback with different side reaction ratios to prompt movements of the affected side while the non-affected support base remains in a fixed position.
SUBJECTS AND METHODS
A schematic diagram of the device and task used in this study is shown in Fig. 1. Patients stand on the signal capture device (dual force plate), and are prompted with a task from the interactive game through a monitor. The patient then changes the body center to move an object as prompted by a task shown on the monitor. All of these physical actions are used to execute balance training and task assessment.
Fig. 1.
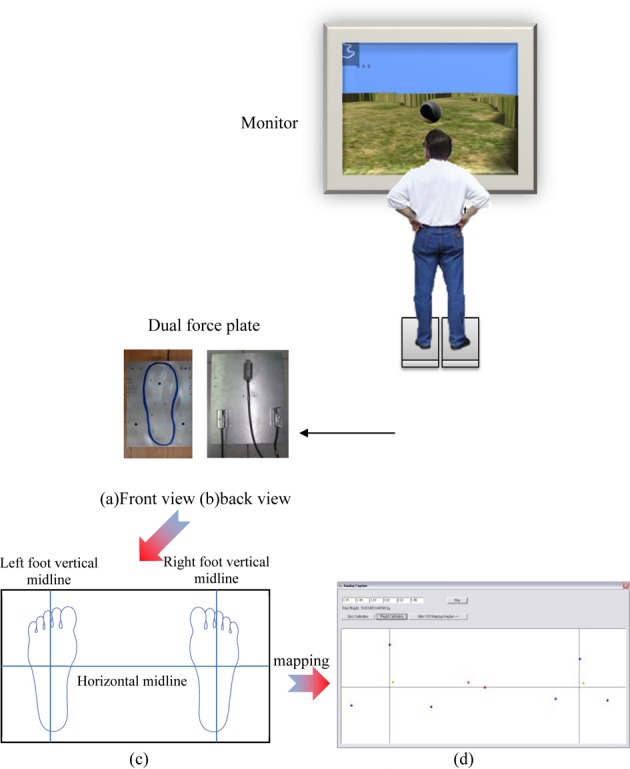
System schematic diagram
This study used a COP capture device consisting of a load cell, signal transmitter and an analog/digital converter with a Universal Serial Bus (USB) interface. Weight distribution data collected from the foot plantar stress center are displayed in a two-dimensional plane and entered into the game for coordination.
Figure 1a shows the COP capture device which consists of two plates (30 × 245 × 10 mm, 304 stainless steel), one for each foot. The bottom displays an equilateral triangle (width 165mm) consisting of three load cells acting as a unit (Fig. 1b). The center of this equilateral triangle is the geometric center of the stepping zone. The user needs to step on the center of the stepping zone to align the geometric center of the plantar area and the center of the load cell as closely as possible. Figure 1c and 1d show how movements are captured when the COP capture device has been set up. The load cell retrieves signals from the right and left feet of the user, and the movements of foot pressure center are post-processed to construct the center distribution figure.
If the region D is located in the two-dimensional coordinate system, which is the density function ρ(x, y), region D is further divided into left and right sides, sub-regions DL and DR. The overall weight of the system is the subject’s weight on both feet, which is calculated using the formula:
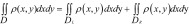 |
The center of gravity of the system is calculated using the formula:
 |
The three vertices of a subject’s plantar force on the region DL(DR), have force and moment arm values Li (Ri) and XLi, YLi (XRi, YRi); for i = 1–3, respectively. Figure 2 shows the relationship between the force and the moment arm diagram, and the center of gravity is be derived as follows:
 |
Fig. 2.
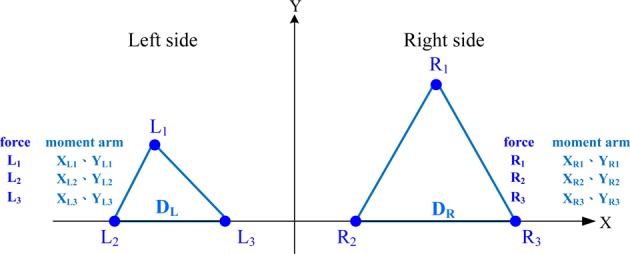
The relationship between the force and the moment arm
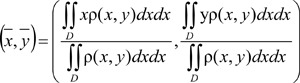
Figure 3 provides a diagram of this capture device. A signal transmitter is used to provide the operational voltage to the load cell and amplify the signal for transmission to the analog/digital converter. The device was designed for periodic sampling. The sampling frequency used in this study was 100 Hz. Converted data is saved in a buffer zone and transmitted when the software requests it. After acquisition by the analysis software, data is processed by a finite impulse response filter (to a low-pass filter, 10 Hz) and organized in chronological sequence. The software was written in Microsoft Visual C#, for (1) setting the function of the analog/digital converter with the USB interface; (2) processing load cell data tables; (3) processing vector parameters; (4) center distribution plots after vector processing; (5) a graphic user interface to display raw data and center distribution plots after vector processing; and (6) a graphic user interface to set vector processing and system parameters.
Fig. 3.
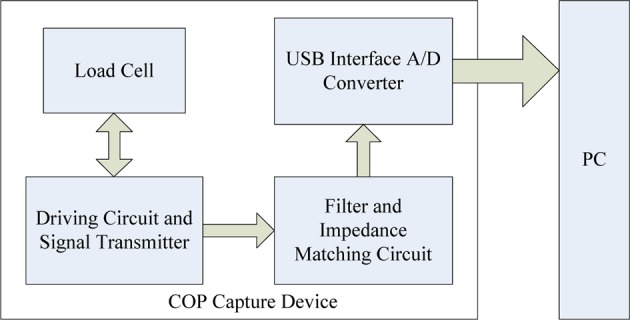
Schematic diagram of the capture device
The game engine was developed using the Microsoft .NET Framework. Microsoft Visual C# with XNA Game Studio was used to build this engine with (1) an event processing queue (2) a graphic engine (3) a user interface (4) a database interface (Fig. 4).
Fig. 4.
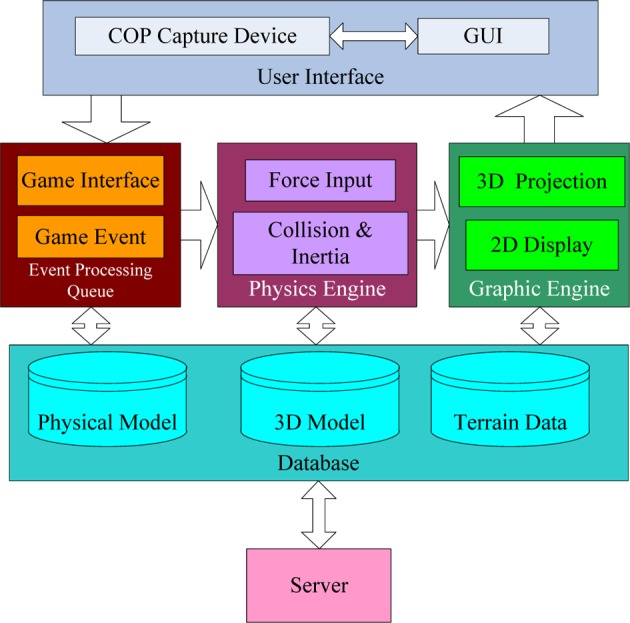
Architecture of the game engine
The COP capture device of this system used the proportion, single load cell value: whole load cell value = single foot center point distribution value: single foot center point reflect plane boundary, to reflect the collected weight distribution in the virtual plane. The six distribution values are then merged to become the pressure centers of the right and left feet and the whole COP in the virtual plane of the game engine using this rule: healthy side: affected side = 1: n (n is decided by the medical staff based on the patient’s diagnosed medical condition: n=1.5 for case A, and 4 for case B in this study).
If the COP values are over the boundary the display is locked to that boundary. In this study the task for patients was to use COP to aim an arrow and to shoot it at a target, When the sum value of the healthy side load cell is less than 20% of the value for the load cell unit as a whole, red warnings were displayed on the monitor to tell the patient to move their COP to the other side.
A randomly moving target was displayed in the virtual plane of the game display. The formula controlling movement of the target is given by:
Horizontal boundary Bh= Vertical boundary Bv=1,000 (unit)Moving velocity v: ±1≤v≤±10 (unit/fps) Moving velocity changing rate n: 10≤n≤100 (fps)
The target moved randomly throughout the game. The patients had to move their COP to the target. The user was considered to have located the target when the angle formed by the target and the monitor center (the location of the camera) and the difference was less than 5°. At this point, the arrow was shot at the target. The time taken to locate the target was recorded and transmitted to a server via the internet.
The experiments in this study were approved by the Human Ethics Committee, Taipei Medical University Hospital, Taiwan. All subjects provided their written informed consent to participation in this study. Inclusion criteria were stroke with hemiplegia, and an age between 25 to 60 years. Exclusion criteria were inability to stand unaided or with an assistive device.
This study reports the results of two subjects who used the device for movement control training of the affected side. Training consisted of three thirty-minute sessions a week for three weeks. Training sessions consisted of following the randomly moving target as described above, with one five-minute break in the middle of the session. The training was the same for both patients. A test re-test repeated measures design was used to evaluate performance. Baseline performance was measured before the start of training, and performance was measured again at the end of the training period.
The tools used to evaluate performance were: the Berg Balance Scale (BBS)15, 16), 14 balance tasks scored on a five-point (0–4) scale with 0 representing the poorest performance; the Motor Assessment Scale (MAS)17) which evaluates motor function on a seven-point (0–6) scale, in this study, only items relevant to standing balance were used; and the newly-developed device was used to evaluate the COP distribution. The evaluation included the COP motion distribution of the left and right feet and whole body while standing with the eyes open for one minute, and standing with the eyes closed for one minute.
RESULTS
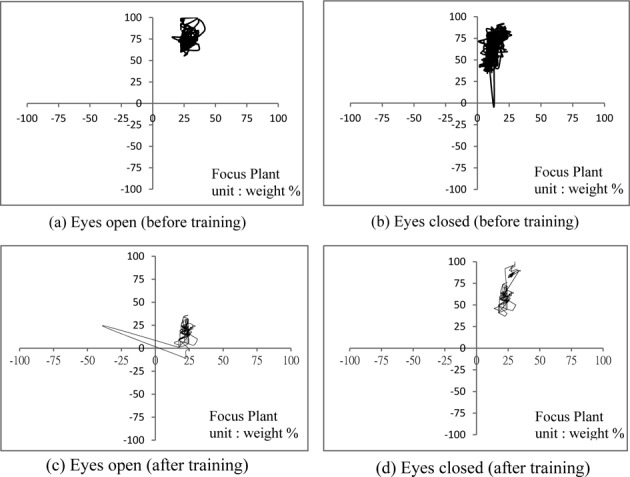
The effect on balance performance training using the device was assessed using two patients. The side ratio n was 1.5 for case A (the reaction in the game was 60% on the affected side and 40% on the non-affect-side), and 4 for case B (affected-side 80%, non-affected-side 20%). COP distribution was measured before and after training. Table 1 summarizes patient data. Figure 5 shows the COP distribution for patient A: before training in the eyes open condition (Fig. 5a); before training, eyes closed (Fig. 5b); after training, eyes open (Fig. 5c); after training, eyes closed (Fig. 5d). COP distributions for patient B are shown in Fig. 6: before training, eyes open (Fig. 6a); before training, eyes closed (Fig. 6b); after training, eyes open (Fig. 6c); after training, eyes closed (Fig. 6d). The COP numerical distribution is shown in Fig. 7: patient A, eyes open (Fig. 7a) and eyes closed (Fig. 7b); patient B, eyes open (Fig. 7c) and eyes closed (Fig. 7d).
Table 1. Basic information the two cases in this study.
| subject | A | B |
|---|---|---|
| Gender | Male | Male |
| Age (years) | 49 | 39 |
| Height (cm) | 167 | 168 |
| Weight (kg) | 82 | 72 |
| BMI | 29.4 | 25.51 |
| Main symptoms | Stroke | Stroke |
| Onset period | 6 months | 11 months |
| Dominant side / affected side | right/ right | right / right |
| Other illnesses | Asthma, hypertension, aphasia | No |
| Habits and customs | Stopped drinking and smoking (about a year) Exercise at least one hour a day |
Stopped smoking (8 months) Exercise one to two hours a day |
Fig. 5.
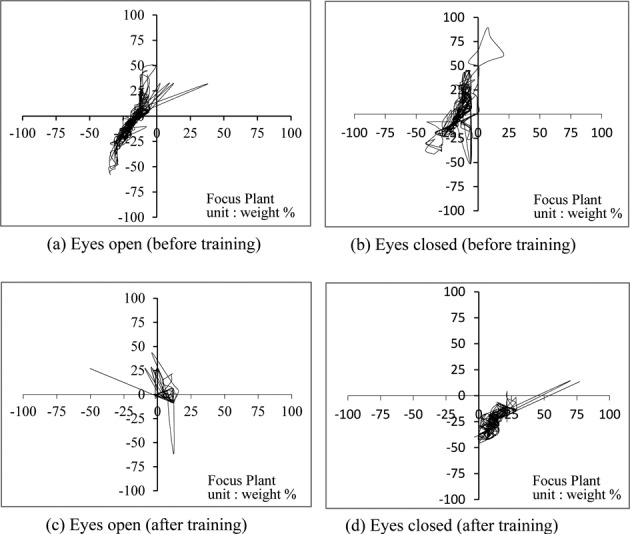
The COP distribution of case A
Fig. 6.
The COP distribution of case B
Fig. 7.
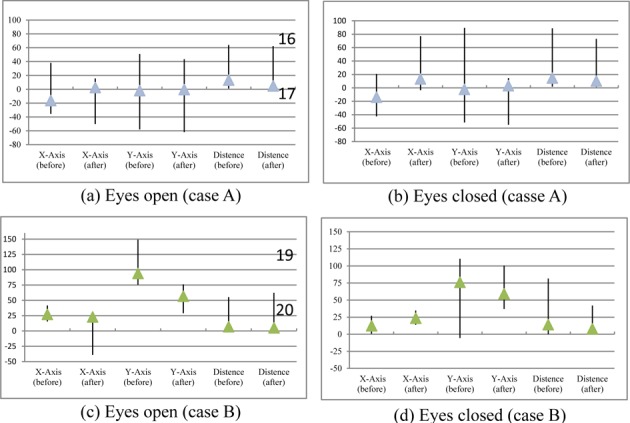
COP distribution before and after training
Baseline and post-training balance assessments using the BBS showed that neither patient A nor patient B regressed on the items for which performance at baseline was already at a ceiling. The BBS improvement of case A was 19.44% and that of case B was 11.9%, showing that the interactive game used in this study can help stroke patients improve their balancing ability on the stroke affected side. Detailed results are presented in Table 2.
Table 2. Balance ability assessment with BBS.
| Subject | BBS sub task | Before training | After training | Progress | ||
|---|---|---|---|---|---|---|
| A | Sit to Stand | With hand assistance | Without hand assistance | Significant | ||
| Standing unsupported with eyes closed | Unstable | More stable | Significant | |||
| Stand unsupported with feet together | With hand assistance | Without hand assistance and longer standing time | Average | |||
| Reaching forward with outstretched arm | Some reach | Longer reach | Average | |||
| Pick up object from the floor from a standing position | No change | Non | ||||
| Turn to look behind over left and right shoulders while standing | Can’t look behind over affected side | Can look behind over affected side | Significant | |||
| Turn 360° | Low speed | Faster speed (but the score not enough to next level) | Weak | |||
| Place alternate foot on bench or stool while standing unsupported | Could not step on a stool | Stepped on the stool twice without any support | Significant | |||
| Stand unsupported with one foot in front | Not able to stand | Unsupported with one foot in front for 8 s | Significant | |||
| Standing on one leg | Could not stand on the affected side, short term on the healthy side | Still could not stand on the affected side, but more time on the healthy side | Average | |||
| B | Stand unsupported with feet together | stand for a long time, but need assistance to drew the feet | drew the feet by himself | Significant | ||
| Place alternate foot on bench or stool while standing unsupported | Took 24 s | Only took 12 s | Significant | |||
| Stand unsupported with one foot in front | Not able to stand | Stood for 20 s | Significant | |||
| Reaching forward with outstretched arm | 18 cm | 19 cm | Weak | |||
| Pick up object from the floor from a standing position | No change | Non | ||||
| Turn to look behind over left and right shoulders while standing | No change | Non | ||||
| Turn 360° | Took 13 s | Took 12 s | Weak | |||
| BBS score | Case A | Case B | ||||
| Before/After/Rate of progress | 36 point / 43point /19.44% | 42 point / 47 point /11.9% | ||||
Table 2 shows that the progress of patient A was not sufficient on some of the BBS items to elicit an improvement in score, although there was some evidence of progress. We speculate that additional training time would have elicited larger gains in performance. On items such as “Reaching forward with an outstretched arm,” and “Picking up an object from the floor from a standing position,” there were no obvious changes in performance, presumably because these items involve upper limb movement.
Patient B was tested after a longer recovery period and was in better physical condition, and his baseline balance performance was better than that of patient A. Among the items which were worst at baseline, items involving upper limb movement showed little change after the training, but items related to standing balance showed obvious improvement.
Table 3 gives detailed data on the MAS scores of both patients. The test program included seated balance and transitions from sitting to standing and walking.
Table 3. Balance ability assessment with MAS.
| Subject | MAS sub task | Before training | After training | Progress | |
|---|---|---|---|---|---|
| A | Balance sitting | Could maintain sitting, but the weight of two body side was uneven | Improved. Could look around and touch the side floor but not the front floor. | Average | |
| Sitting to standing | Could complete independ- ently, but the weight was uneven. | The uneven situation was improved but the speed was rather slow. | Average | ||
| Walking | Had to have assistance all the time for walking. | Could walk steadily without assistance device but still slow. | Average | ||
| B | Balance sitting | Normal performance | Some progress | Weak | |
| Sitting to standing | Good performance | Better performance | Significant | ||
| Walking | Good performance | Walking speed was obviously faster | Significant | ||
| MAS score | Case A | Case B | |||
| Before/after/Rate of progress | 6 point/12 point /100% | 16 point /17 point /6.25 % | |||
The COP distribution data is shown in Table 4. After training, the COP distribution of patient A shifted towards the right (affected side); presumably because the patient habitually supported standing with the healthy side. The affected side showed smaller effort during the game, so the patients were forced to use their healthy side to finish the game. Over time they became used to having their affected side absorb the weight when standing on the force plate. The data of the center point drift and the average value of the center point of the average distance showed that there was considerable improvement in the eyes open condition. This may be because the patients knew they could find a datum point and maintain that datum point. There was no obvious improvement in the eyes closed condition. In fact, the average value for the center position distance in the eyes closed condition indicated a slight deterioration in performance. Both patients showed considerable improvement in terms of the center point drift area.
Table 4. COP distribution.
| Subject | Center point average position | Average value of the center point drifting position and the center point of the average distance |
|||
|---|---|---|---|---|---|
| OE (before/after) | CE (before/after) | OE (before/after) | CE (before/after) | ||
| A | (−16.20, −1.97) / (2.55, −0.36) | (−13.80, 3.35) / (13.48, −22.41) | 13.39 / 4.92 | 14.78 / 10.39 | |
| COP distribution change: position moved to right side (affected side) from left side (healthy side). | Progress: OE: 63.25%, CE: 29.70% drift area of center point (before/after): OE: 1,284.90 / 543.50 (progress 57.70%) CE: 1,673.30 / 1,238.10 (progress 26%) | ||||
| B | (27.10, 93.99)/ (22.89, 56.71) | (12.23, 76.06) / (23.42, 59.19) | 6.92 / 5.12 | 14.03 / 14.82 | |
| COP distribution change: moved from the upper side to the center (the virtual center of the center point on mapping plane) | Progress: OE: 26.01%, CE: −5.63% drift area of center point (before/after): OE: 767.20 / 574.30 (progress 25.14%) CE: 1599.90 / 873.20 (progress 45.42%) | ||||
DISCUSSION
Patient A showed a 19.44% improvement in performance on the BBS and 100% improvement in performance on the MAS following training using the device and interactive game. Although patient A used his healthy side to support his body weight in a standing position, under certain circumstances he could switch to using the affected side. Patient A showed considerable improvement in static standing balance control with his eyes open. Patient B showed much smaller improvements in performance: an 11.9% improvement in performance on the BBS, and a 6.25% performance on the MAS. In center point plane performance, there was no significant change in the center point position; and there was no detectable change in average drift extent, even though the center point drift area was smaller.
It is our opinion, that the difference in the effectiveness of the training for the two patients was due to differences in the length of recovery. Case B was tested after an 11 month recovery period and had already achieved considerable gains in mobility, most of which were persistent. This persistence was derived from functional use of the movements in the course of daily life. The patients had not received static standing balance in daily living activities. This accounts for the pattern of improvements seen following training. The training produced a considerable improvement in static center point drift but no obvious improvement in center point position. It is our opinion, that patient A made significant progress in all aspects of balance because testing occurred after a shorter recovery period, and patient A had not recovered as much mobility as patient B, leading to larger training effects.
In summary, an interactive game with dual force and different side ratio developed for this study can help stroke patients train their balance on their stroke affected side, but this method is only effective for patients who have recently experienced stroke and offers little benefit to patients who have recovered a significant degree of mobility. We were unable to determine the level of baseline mobility at which training ceases to be effective as this study assessed only two cases. Future research should investigate the effects of our rehabilitation protocol in stroke patients with hemiplegia with varying recovery periods, e.g. 6 to 11 months, BBS score below a certain threshold, e.g. 42, or MAS scores below a certain threshold, e.g. 16 to provide further evidence regarding its efficacy.
REFERENCES
- 1.Geurts AC, de Haart M, van Nes IJ, et al. : A review of standing balance recovery from stroke. Gait Posture, 2005, 22: 267–281. [DOI] [PubMed] [Google Scholar]
- 2.Bohannon RW: Gait performance of hemiparetic stroke patients: selected variables. Arch Phys Med Rehabil, 1987, 68: 777–781. [PubMed] [Google Scholar]
- 3.Bonita R, Beaglehole R: Recovery of motor function after stroke. Stroke, 1988, 19: 1497–1500. [DOI] [PubMed] [Google Scholar]
- 4.J C and R S, Neurological Rehabilitation: Optimizing Motor Performance, 2nd ed. 2000.
- 5.Hu MH: Motor Control and Motor Learning, 4th ed. Taipei, 2003. [Google Scholar]
- 6.Weiss A, Suzuki T, Bean J, et al. : High intensity strength training improves strength and functional performance after stroke. Am J Phys Med Rehabil, 2000, 79: 369–376, quiz 391–394. [DOI] [PubMed] [Google Scholar]
- 7.Barclay-Goddard R, Stevenson T, Poluha W, et al. : Force platform feedback for standing balance training after stroke. Cochrane Database Syst Rev, 2004, (4): CD004129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Peppen RP, Kortsmit M, Lindeman E, et al. : Effects of visual feedback therapy on postural control in bilateral standing after stroke: a systematic review. J Rehabil Med, 2006, 38: 3–9. [DOI] [PubMed] [Google Scholar]
- 9.Ko Y, Ha H, Bae YH, et al. : Effect of space balance 3D training using visual feedback on balance and mobility in acute stroke patients. J Phys Ther Sci, 2015, 27: 1593–1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nichols DS: Balance retraining after stroke using force platform biofeedback. Phys Ther, 1997, 77: 553–558. [DOI] [PubMed] [Google Scholar]
- 11.Juneja G, Czyrny JJ, Linn RT: Admission balance and outcomes of patients admitted for acute inpatient rehabilitation. Am J Phys Med Rehabil, 1998, 77: 388–393. [DOI] [PubMed] [Google Scholar]
- 12.Burdea G, Popescu V, Hentz V, et al. : Virtual reality-based orthopedic telerehabilitation. IEEE Trans Rehabil Eng, 2000, 8: 430–432. [DOI] [PubMed] [Google Scholar]
- 13.Tarr MJ, Warren WH: Virtual reality in behavioral neuroscience and beyond. Nat Neurosci, 2002, 5: 1089–1092. [DOI] [PubMed] [Google Scholar]
- 14.Seo K, Kim H, Han J: Effects of dual-task balance exercise on stroke patients’ balance performance. J Phys Ther Sci, 2012, 24: 593–595. [Google Scholar]
- 15.Berg K, Wood-Dauphine S, Williams JI, et al. : Measuring balance in the elderly: preliminary development of an instrument. Physiother Can, 1989, 41: 304–311. [Google Scholar]
- 16.Bennie S, Bruner K, Dizon A, et al. : Measurements of balance: comparison of the timed “up and go” test and functional reach test with the berg balance scale. J Phys Ther Sci, 2003, 15: 93–97. [Google Scholar]
- 17.Poole JL, Whitney SL: Motor assessment scale for stroke patients: concurrent validity and interrater reliability. Arch Phys Med Rehabil, 1988, 69: 195–197. [PubMed] [Google Scholar]


