Abstract
Eosinophilic cystitis is a rare inflammatory disease of the bladder which origin and pathogenesis are unknown. Since the first description in 1960, hundreds of cases have been reported, 20 Pseudotumor forms. We report a case of cystitis eosinophils in tumor-form, a patient of 72 years without urological or allergic history. The patient was treated with endoscopic resection alone. The outcome was favorable with disappearance symptoms and no recurrence at 1, 3 and 6 months controls. We carry a literature review of cystitis eosinophils on the different clinical manifestations, the means diagnostic and therapeutic modalities.
Keywords: Eosinophilic cystitis, Bladder tumor, Diagnosis, Treatment
Introduction
Eosinophilic cystitis is a rare inflammatory pathology of the bladder wall whose origin and physiopathology are still unknown.1, 2 Since the first description in 1960, one hundred cases have been reported, 20 of which a pseudotumor forms.1 Clinical symptoms, as well as the radiological endoscopic appearance are nonspecific. The diagnosis is based solely on histological examination.1, 2
The therapeutic management is usually based on corticosteroids or nonsteroidal anti-inflammatory drugs, sometimes on the endoscopic resection of lesions, exceptionally on surgery.1, 2
We report the observation of pseudotumoral eosinophilic cystitis treated with endoscopic resection with favorable outcome.
Case report
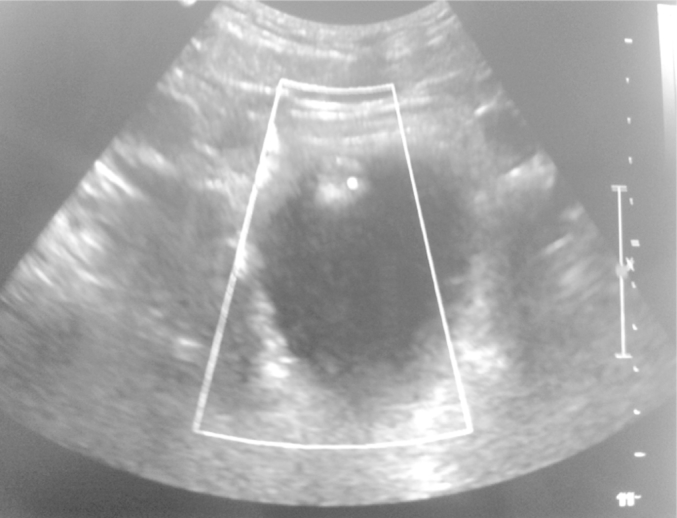
A 72 year old man, smoker, without any special occupational exposure consults for irritative urinary symptoms with terminal hematuria since 2 months. His physical examination was normal. An ultrasonography (Figure 1, Figure 2) shows a bud of 14 mm at the bladder dome and is vascularized in doppler. We performed a cystoscopy which shows a budding lesion measuring 1.5 cm below the bottom which has been resectioned. The adjacent mucosa is slightly inflammatory. Pathological examination concluded at an edematous and congestive shuffle with a rich inflammatory infiltrate composed predominantly of eosinophils in the lamina propria without signs of malignancy. The outcome was favorable with no symptoms at 1, 3 and 6 months postoperatively controls.
Figure 1.

Sonographic appearance of pseudotumor of the bladder dome.
Figure 2.
This pseudotumor is vascularized at Doppler.
Discussion
Eosinophilic cystitis has two main presentations, affecting two types of distinct populations. On the one hand for children and the young woman, the surface shape and diffuse is the most common and found in 30% of cases atopy.3
The other type of population affected is that of middle-aged men, often on a pre-existing uropathy field.4, 5 It is in these frameworks that are found most often eosinophilic cystitis pseudo tumor shape.
The onset of symptoms is often brutal. Clinical signs of superficial forms are dominated by an irritative syndrome: intense urinary frequency, pelvic pain, hematuria. The tumor forms more readily cause dysuria or urinary retention.5 A case of spontaneous bladder perforation has been reported.2
In cystoscopy, the mucosa is inflammatory, edematous or necrotic and ulcerated. Sometimes there are polypoid areas or real tumors making discuss a malignant epithelial tumor.5, 6
The imagery contributes little to the diagnosis. It can at best bring out the tumor syndrome without prejudging its nature.1, 2
The formal diagnosis is histological: infiltration of layers of the bladder wall by inflammatory cells in which predominantly eosinophils, together with high levels of IgE and IgA in cells infiltrating the wall1 (Figure 3, Figure 4). The pseudotumoral forms are marked by the discreet nature of the superficial infiltrate contrasting with the frequency of lesions necrosis and fibrosis of the deeper layers. These lesions, whose development is focal and willingly changeable, require profound and multiple biopsies.1
Figure 3.
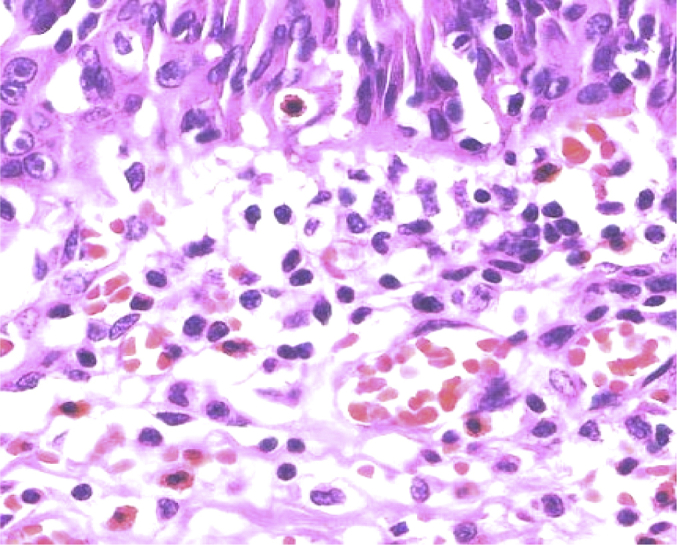
Many eosinophils in the blood vessels and in chorion at the urothelial mucosa.
Figure 4.
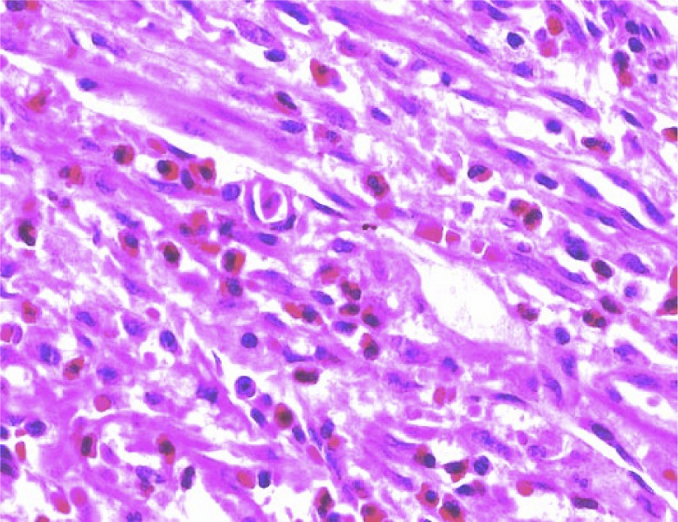
Inflammatory infiltrates composed predominantly of eosinophils in the lamina propria.
In biology, a peripheral eosinophilia is present in about 30% of cases1, 6 and is more common in case of allergic terrain, diffuse form or in children.1, 4 Increased serum IgE and IgA is sometimes found.3 In pseudotumoral forms, the entire laboratory tests may be normal.
The disease progresses to the extension of the lesions, the invasion of adjacent structures, recurrence and chronicity.1, 3, 5 In pseudotumoral forms, the spontaneous evolution is never favorable, unlike some diffuse forms and especially childhood forms.7
The treatment of eosinophilic cystitis is mainly based on corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs),1, 2 optionally in combination with antihistamines or azathioprine.1
The pseudotumoral forms, however, seem to respond poorly to these treatments. This is why other types of protocols have been proposed: cotrimoxazole,1, 5 cyclophosphamide, and actinomycin D,8 azathioprine and DMSO instillations.9 In case of proven allergy, the eviction of the allergen responsible is required.7
In case of failure of medical treatment or to the impact of the lesions (bladder retraction, ureteral obstruction) the surgery is inevitable. Resection (or electrocautery) endoscopic lesions often provide good results.2
In case of failure, partial cystectomy with bladder expansion must be avoided as possible.5 Indeed, a surgical aggression on an inflammatory bladder could be the cause of a hyperacute evolution. Cystectomy appears as an effective alternative.9
Conclusion
Pseudotumoral eosinophilic cystitis is an exceptional pathology that falls within the scope of the differential diagnosis of bladder cancer. His presentation is misleading and the differential diagnosis is possible only after histological examination. It occurs most often in older men with multiple pathologies history of lower urinary tract.
The development is done toward the extension of the lesions to the whole of the bladder but also to the adjacent structures. The frequency of recurrence and the tendency to chronicity require close monitoring.
Medical treatment is the first line (corticosteroids, NSAIDs, cotrimoxazole, DMSO or immunosuppressants), combined with transurethral resection of the lesions. In case of failure, cystectomy seems a preferable alternative to partial surgery.
Conflict of interest
The authors declare that they have no conflicts of interest related to this article.
Footnotes
Available online 26 February 2015
References
- 1.Chaffange P., Valignat C., Ruffion A., Archimbaud J.P. Cystite à éosinophiles pseudo tumorale d'évolution suraiguë. A propos d'un cas. Prog Urol. 1999;9:1113–1116. [PubMed] [Google Scholar]
- 2.Ficarra V., Beltrami P., Giusti G., Tontodonati M., Zanon G., Malossini G. Perforation vésicale spontanée due à une cystite à éosinophiles: à propos d'une observation. Prog Urol. 1997;7:1012–1014. [PubMed] [Google Scholar]
- 3.Kessler W.O., Clark P.L., Kaplan G.W. Eosinophilic cystitis. Urology. 1975;6:499–501. doi: 10.1016/0090-4295(75)90640-8. [DOI] [PubMed] [Google Scholar]
- 4.Castillo J., Jr., Cartagena R., Montes M. Eosinophilic cystitis: a therapeutic challenge. Urology. 1988;32:535–537. doi: 10.1016/s0090-4295(98)90037-1. [DOI] [PubMed] [Google Scholar]
- 5.Popert R.J., Ramsay J.W., Owen R.A., Fisher C., Hendry W.F. Eosinophilic cystitis mimicking invasive bladder tumour: discussion paper. J R Soc Med. 1990;83:776–778. doi: 10.1177/014107689008301209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kopf A., Boue F., Delfraissy J.F. Eosinophilic cystitis of allergic origin. Presse Med. 1984;13:83–86. [PubMed] [Google Scholar]
- 7.Sujka S.K., Fisher J.E., Greenfield S.P. Eosinophilic cystitis in children. Urology. 1992;40:262–264. doi: 10.1016/0090-4295(92)90488-i. [DOI] [PubMed] [Google Scholar]
- 8.Nkposong E.O., Attah E.B. Eosinophilic cystitis. Eur Urol. 1978;4:274–278. doi: 10.1159/000473970. [DOI] [PubMed] [Google Scholar]
- 9.Chantepie G., Duquesne G., Saout J. Cystite à éosinophiles: à propos de 2 cas. Chirurgie. 1985;111:43–46. [PubMed] [Google Scholar]


