Abstract
Metastatic spread of differentiated thyroid cancer to genitourinary organs is rare. Synchronous presentation of renal and adrenal thyroid metastasis is even less common, this case being only the 3rd reported. We describe a case of a 60-year-old male with oligometastatic thyroid cancer, where adrenal and renal metastases were the only extracervical sites of disease and triggered the patient's presentation.
Keywords: Thyroid cancer, Adrenal mass, Renal tumor, Oligometastasis
Introduction
Spread of metastatic thyroid cancer to genitourinary organs is rare with less than 25 cases reported in English publications. We present a unique case of a 60-year-old male with oligometastatic thyroid cancer with renal and adrenal involvement.
Case presentation
A 60-year-old male with hypertension and hypercholesterolemia presented with a 3-month history of left flank discomfort without associated constitutional or urologic complaints. Initial physical exam and laboratory work-up failed to reveal any significant abnormalities. CT of the abdomen and pelvis with and without contrast demonstrated a 12.8 × 7.7 × 9.1 cm left adrenal mass that appeared cystic and contained calcifications (Fig. 1). The mass displaced the left kidney and extended superiorly along the aorta to the level of the celiac arterial plexus. Small, bilateral, non-enhancing simple renal cysts were also observed. Amongst them was a 1.1 cm well-circumscribed non-enhancing left upper pole hyperdense renal lesion (24HU pre-, 26HU post-contrast) (Fig. 2). Incidentally noted was a mass in the descending colon. On colonoscopy, a 5 cm descending colon polypoid lesion was noted at 50 cm from the anal verge. No other abnormalities were noted on CT scan of the abdomen and pelvis.
Figure 1.

Left adrenal mass.
Figure 2.
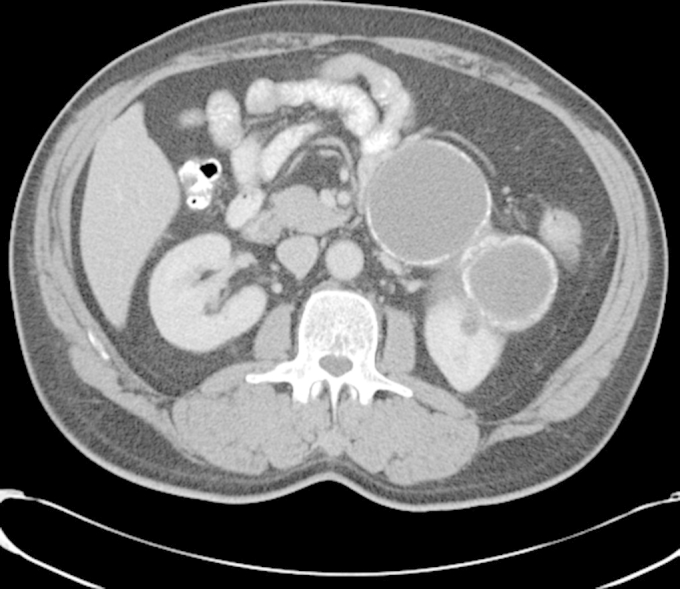
Left upper pole hyperdense renal cyst.
The patient was referred to our institution for further work-up of the adrenal mass and the colon polyp. He underwent an adrenal functional work-up, which was within normal limits. Intra-operatively, left upper pole hyperdense renal cyst was exposed and its appearance was heterogeneous and suspicious for a cystic neoplasm. An off-clamp partial nephrectomy was performed, along with the planned left adrenalectomy and left hemicolectomy. Patient had an uneventful post-operative course. Surgical pathology revealed the colon mass to be a 2.5 cm Grade II invasive adenocarcinoma of the colon arising in a villous adenoma. Muscularis propria invasion was observed and 24 adjacent lymph nodes were tumor-free (pT2N0Mx, Stage 1). Both, the adrenal and the renal lesions stained positive for CAM 5.2, CK7, vimentin, thyroglobulin, TTF-1 and negative for CK20 and inhibin on immunohistochemical analyses, consistent with metastatic papillary thyroid carcinoma.
Imaging demonstrated cervical lymphadenopathy and a 2.3 cm right thyroid lobe mass consistent with thyroid cancer. Enlarged nodes suspicious for malignancy were noted in the right jugular chain. The patient underwent a total thyroidectomy with central compartment and superior mediastinal lymphadenectomy, transcervical partial thymectomy and right modified radical neck dissection. Final pathology revealed a 2.5 cm papillary thyroid carcinoma with extrathyroid extension, and 13 of 43 positive lymph nodes, pT3bN1bM1, Stage 4. Whole body radioiodine scan demonstrated a focus in central neck with no evidence of additional metastatic disease. Patient received 180 mCi of adjuvant radioiodine-131 5 weeks after the procedure. A post-therapy scan demonstrated an uptake in the right maxillary periorbital sinus, consistent with sinusitis. The patient remains disease-free 25 months after his initial surgical therapy.
Discussion
Thyroid cancer is a heterogeneous disease with incidence on the rise.1 The majority of thyroid neoplasms are well-differentiated and 79% are of papillary type.2 These lesions are generally indolent with a 10 year mortality of less than 7%.3 Distant metastases are seen in only 2% of patients with papillary thyroid carcinoma and most commonly affect the lungs and bone.4 For patients who present with metastases, 50% 10-year survival is reported.5
Metastatic spread of differentiated thyroid cancer to genitourinary organs is rare. Kidney involvement has been reported in approximately 25 cases, all except two in a setting of widely metastatic disease.6 Synchronous presentation of renal and adrenal thyroid metastasis is even less common, this case being the 3rd reported. To our knowledge, this is the first case where adrenal and renal metastases were the only extracervical sites of disease and triggered the patient's presentation.7, 8
Conclusion
Thyroid gland should be considered as a potential albeit rare source of metastases in a setting of genitourinary masses.
Conflicts of interest
There is no conflict of interest for any of the authors involved.
References
- 1.Chen A.Y., Jemal A., Ward E.M. Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer. 2009;115:3801–3807. doi: 10.1002/cncr.24416. [DOI] [PubMed] [Google Scholar]
- 2.Hundahl S.A., Fleming I.D., Fremgen A.M. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985–1995 [see comments] Cancer. 1998;83:2638–2648. doi: 10.1002/(sici)1097-0142(19981215)83:12<2638::aid-cncr31>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 3.Donohue J.H., Goldfien S.D., Miller T.R. Do the prognoses of papillary and follicular thyroid carcinomas differ? Am J Surg. 1984;148:168–173. doi: 10.1016/0002-9610(84)90306-4. [DOI] [PubMed] [Google Scholar]
- 4.Shaha A.R., Shah J.P., Loree T.R. Differentiated thyroid cancer presenting initially with distant metastasis. Am J Surg. 1997;174:474–476. doi: 10.1016/s0002-9610(97)00158-x. [DOI] [PubMed] [Google Scholar]
- 5.Elisei R., Molinaro E., Agate L. Are the clinical and pathological features of differentiated thyroid carcinoma really changed over the last 35 years? Study on 4187 patients from a single Italian institution to answer this question. J Clin Endocrinol Metab. 2010;95:1516–1527. doi: 10.1210/jc.2009-1536. [DOI] [PubMed] [Google Scholar]
- 6.Song H.J., Xue Y.L., Xu Y.H. Rare metastases of differentiated thyroid carcinoma: pictorial review. Endocr Relat Cancer. 2011;18:R165–174. doi: 10.1530/ERC-11-0068. [DOI] [PubMed] [Google Scholar]
- 7.Malhotra G., Upadhye T.S., Sridhar E. Unusual case of adrenal and renal metastases from papillary carcinoma of thyroid. Clin Nucl Med. 2010;35:731–736. doi: 10.1097/RLU.0b013e3181ea342b. [DOI] [PubMed] [Google Scholar]
- 8.Kumar A., Nadig M., Patra V. Adrenal and renal metastases from follicular thyroid cancer. Br J Radiol. 2005;78:1038–1041. doi: 10.1259/bjr/24024066. [DOI] [PubMed] [Google Scholar]


