Preamble
Keeping pace with the stream of new data and evolving evidence on which guideline recommendations are based is an ongoing challenge to timely development of clinical practice guidelines. In an effort to respond promptly to new evidence, the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) Task Force on Practice Guidelines (Task Force) has created a “focused update” process to revise the existing guideline recommendations that are affected by the evolving data or opinion. New evidence is reviewed in an ongoing fashion to more efficiently respond to important science and treatment trends that could have a major impact on patient outcomes and quality of care. Evidence is reviewed at least twice a year, and updates are initiated on an as-needed basis and completed as quickly as possible while maintaining the rigorous methodology that the ACCF and AHA have developed during their partnership of >20 years.
These updated guideline recommendations reflect a consensus of expert opinion after a thorough review primarily of late-breaking clinical trials identified through a broad-based vetting process as being important to the relevant patient population, as well as other new data deemed to have an impact on patient care (see Section 1.1, Methodology and Evidence Review, for details). This focused update is not intended to represent an update based on a complete literature review from the date of the previous guideline publication. Specific criteria/considerations for inclusion of new data include the following:
publication in a peer-reviewed journal;
large, randomized, placebo-controlled trial(s);
nonrandomized data deemed important on the basis of results affecting current safety and efficacy assumptions, including observational studies and meta-analyses;
strength/weakness of research methodology and findings;
likelihood of additional studies influencing current findings;
impact on current and/or likelihood of need to develop new performance measure(s);
request(s) and requirement(s) for review and update from the practice community, key stakeholders, and other sources free of relationships with industry or other potential bias;
number of previous trials showing consistent results; and
need for consistency with a new guideline or guideline updates or revisions.
Selected members of the previous writing committee as well as other experts in the subject under consideration are chosen by the ACCF and AHA to examine subject-specific data and to write guidelines in partnership with representatives from other medical organizations and specialty groups. Writing group members review the selected late-breaking clinical trials and other new data that have been vetted through the Task Force; weigh the strength of evidence for or against particular tests, treatments, or procedures; and include estimates of expected outcomes where such data exist. Patient-specific modifiers, comorbidities, and issues of patient preference that may influence the choice of tests or therapies are considered. When available, information from studies on cost is considered, but data on efficacy and outcomes constitute the primary basis for the recommendations contained herein.
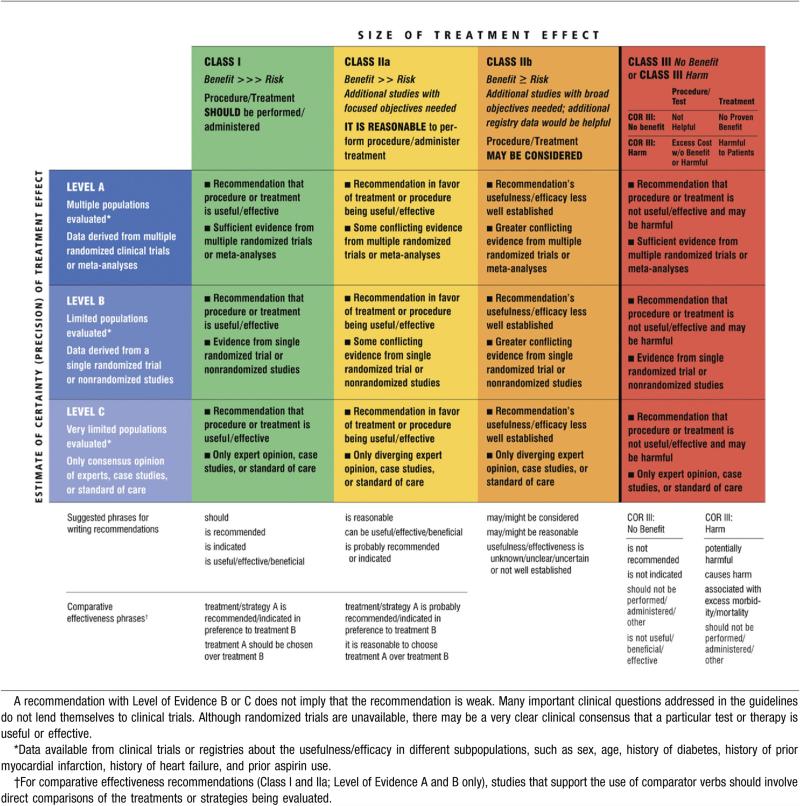
In analyzing the data and developing recommendations and supporting text, the writing group uses evidence-based methodologies developed by the Task Force (1). The Class of Recommendation (COR) is an estimate of the size of the treatment effect considering risks versus benefits in addition to evidence and/or agreement that a given treatment or procedure is or is not useful/effective or in some situations may cause harm. The Level of Evidence (LOE) is an estimate of the certainty or precision of the treatment effect. The writing group reviews and ranks evidence supporting each recommendation with the weight of evidence ranked as LOE A, B, or C according to specific definitions that are included in Table 1. Studies are identified as observational, retrospective, prospective, or randomized where appropriate. For certain conditions for which inadequate data are available, recommendations are based on expert consensus and clinical experience and are ranked as LOE C. When recommendations at LOE C are supported by historical clinical data, appropriate references (including clinical reviews) are cited if available. For issues for which sparse data are available, a survey of current practice among the clinicians on the writing group is the basis for LOE C recommendations, and no references are cited. The schema for COR and LOE is summarized in Table 1, which also provides suggested phrases for writing recommendations within each COR. A new addition to this methodology is a separation of the Class III recommendations to delineate whether the recommendation is determined to be of “no benefit” or is associated with “harm” to the patient. In addition, in view of the increasing number of comparative effectiveness studies, comparator verbs and suggested phrases for writing recommendations for the comparative effectiveness of one treatment or strategy versus another have been added for COR I and IIa, LOE A or B only.
Table 1.
Applying Classification of Recommendations and Level of Evidence
In view of the advances in medical therapy across the spectrum of cardiovascular diseases, the Task Force has designated the term guideline–directed medical therapy (GDMT) to represent optimal medical therapy as defined by ACCF/AHA guideline-recommended therapies (primarily Class I). This new term, GDMT, will be used herein and throughout all future guidelines.
Because the ACCF/AHA practice guidelines address patient populations (and healthcare providers) residing in North America, drugs that are not currently available in North America are discussed in the text without a specific COR. For studies performed in large numbers of subjects outside North America, each writing group reviews the potential influence of different practice patterns and patient populations on the treatment effect and relevance to the ACCF/AHA target population to determine whether the findings should inform a specific recommendation.
The ACCF/AHA practice guidelines are intended to assist healthcare providers in clinical decision making by describing a range of generally acceptable approaches to the diagnosis, management, and prevention of specific diseases or conditions. The guidelines attempt to define practices that meet the needs of most patients in most circumstances. The ultimate judgment regarding care of a particular patient must be made by the healthcare provider and patient in light of all the circumstances presented by that patient. As a result, situations may arise for which deviations from these guidelines may be appropriate. Clinical decision making should involve consideration of the quality and availability of expertise in the area where care is provided. When these guidelines are used as the basis for regulatory or payer decisions, the goal should be improvement in quality of care. The Task Force recognizes that situations arise in which additional data are needed to inform patient care more effectively; these areas will be identified within each respective guideline when appropriate.
Prescribed courses of treatment in accordance with these recommendations are effective only if followed. Because lack of patient understanding and adherence may adversely affect outcomes, physicians and other healthcare providers should make every effort to engage the patient's active participation in prescribed medical regimens and lifestyles. In addition, patients should be informed of the risks, benefits, and alternatives to a particular treatment and be involved in shared decision making whenever feasible, particularly for COR IIa and IIb, for which the benefit-to-risk ratio may be lower.
The Task Force makes every effort to avoid actual, potential, or perceived conflicts of interest that may arise as a result of industry relationships or personal interests among the members of the writing group. All writing group members and peer reviewers of the guideline are asked to disclose all such current relationships as well as those existing 12 months previously. In December 2009, the ACCF and AHA implemented a new policy for relationships with industry and other entities (RWI) that requires the writing group chair plus a minimum of 50% of the writing group to have no relevant RWI (Appendix 1 for the ACCF/AHA definition of relevance). These statements are reviewed by the Task Force and all members during each conference call and/or meeting of the writing group and are updated as changes occur. All guideline recommendations require a confidential vote by the writing group and must be approved by a consensus of the voting members. Members are not permitted to write, and must recuse themselves from voting on, any recommendation or section to which their RWI apply. Members who recused themselves from voting are indicated in the list of writing group members, and section recusals are noted in Appendix 1. Authors’ and peer reviewers’ RWI pertinent to this guideline are disclosed in Appendixes 1 and 2, respectively. Additionally, to ensure complete transparency, writing group members’ comprehensive disclosure information—including RWI not pertinent to this document—is available as an online supplement. Comprehensive disclosure information for the Task Force is also available online at www.cardiosource.org/ACC/About-ACC/Leadership/Guidelines-and-Documents-Task-Forces.cardiosource.org. The work of the writing group was supported exclusively by the ACCF and AHA without commercial support. Writing group members volunteered their time for this activity.
In an effort to maintain relevance at the point of care for practicing physicians, the Task Force continues to oversee an ongoing process improvement initiative. As a result, in response to pilot projects, several changes to these guidelines will be apparent, including limited narrative text and a focus on summary and evidence tables.
The recommendations in this focused update will be considered current until they are superseded by another focused update or the full-text guideline is revised. Guidelines are official policy of both the ACCF and AHA.
Alice K. Jacobs, MD, FACC, FAHA Chair, ACCF/AHA Task Force on Practice Guidelines
1. Introduction
1.1. Methodology and Evidence Review
The results of late-breaking clinical trials presented at the annual scientific meetings of the ACC, AHA, European Society of Cardiology, Society for Vascular Surgery, Society of Interventional Radiology, and Society for Vascular Medicine, as well as selected other data/articles published through December 2010, were reviewed by the 2005 guideline writing committee along with the Task Force and other experts to identify those trials and other key data that may impact guideline recommendations. On the basis of the criteria/considerations noted above, recent trial data and other clinical information were considered important enough to prompt a focused update of the “ACC/AHA 2005 Guidelines for the Management of Patients With Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic)” (2). Because clinical research and clinical care of vascular disease have a global investigative and international clinical care tradition, efforts were made to harmonize this update with the Trans-Atlantic Inter-Society Consensus document on Management of Peripheral Arterial Disease (TASC) and the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) Steering Committee guideline writing efforts (3).
To provide clinicians with a comprehensive set of data, whenever deemed appropriate or when published, the absolute risk difference and number needed to treat or harm are provided in the guideline, along with confidence intervals (CIs) and data related to the relative treatment effects, such as odds ratio, relative risk, hazard ratio (HR), or incidence rate ratio.
Consult the full-text version (2) or executive summary (4) of the “ACC/AHA 2005 Guidelines for the Management of Patients With Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic)” for policy on clinical areas not covered by the focused update. Individual recommendations modified in this focused update will be incorporated into future revisions and/or updates of the full-text guideline.
1.2. Organization of the Writing Group
For this focused update, all eligible members of the 2005 writing committee were invited to participate; those who agreed (referred to as the 2011 focused update writing group) were required to disclose all RWI relevant to the data under consideration. In addition, new members were invited in order to preserve the required RWI balance. The writing group included representatives from the ACCF, AHA, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society for Vascular Medicine, and Society for Vascular Surgery.
1.3. Document Review and Approval
This document was reviewed by 2 official reviewers each nominated by the ACCF and the AHA, as well as 2 reviewers each from the Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society for Vascular Medicine, and Society for Vascular Surgery; and 13 individual content reviewers (including members from the following groups: ACCF/AHA Task Force on Clinical Data Standards, ACCF Interventional Scientific Council, 2005 Peripheral Artery Disease Writing Committee, ACCF/AHA Task Force on Performance Measures, ACCF Prevention Committee, and ACCF Peripheral Vascular Disease Committee). All information on reviewers’ RWI was distributed to the writing group and is published in this document (Appendix 2).
This document was approved for publication by the governing bodies of the ACCF and AHA and endorsed by the Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society for Vascular Medicine, and Society for Vascular Surgery.
1.4. Scope of the Focused Update
Studies relevant to the management of patients with peripheral artery disease (PAD) (lower extremity, renal, mesenteric, and abdominal aortic) were identified and reviewed as described previously in Section 1.1. On the basis of these data, the writing group determined that updates to the 2005 recommendations were necessary for lower extremity and abdominal aortic disease but that the existing recommendations for renal and mesenteric disease remain valid (4). Although the specific recommendations for renal and mesenteric disease did not change, the following observations and clarifications were made:
Medical therapy for renal disease: No new pivotal trials or studies were identified.
Revascularization for renal disease: The writing group acknowledges that some new studies support a more limited role for renal revascularization. For example, the ASTRAL (Angioplasty and Stent for Renal Artery Lesions) investigators (5) concluded that there were substantial risks but no clinical benefit from revascularization in patients with atherosclerotic renovascular disease. The writing group concurred that the criteria for patient selection in this randomized controlled trial (RCT) potentially excluded many patients who might have benefitted from intervention. It is anticipated that ongoing studies such as the CORAL (Cardiovascular Outcomes in Renal Atherosclerotic Lesions) trial (6) will provide additional evidence relevant to these recommendations in the near future.
Methods of revascularization for renal disease: The 2005 recommendations remain current.
The 2011 focused update acknowledges the declining use of surgical revascularization and the increasing use of catheter-based revascularization for renal artery stenoses. The writing group determined that new data support the equivalency of surgical and endovascular treatment, with lower morbidity and mortality associated with endovascular treatment but higher patency rates with surgical treatment in those patients who survived for at least 2 years after randomization (5). The writing group also notes that new data suggest that: 1) the efficacy of revascularization may be reduced in patients with branch artery stenoses (7); and 2) patients undergoing renal artery bypass may do best when surgery is performed in high-volume centers (8).
2. Lower Extremity PAD
2.5. Diagnostic Methods
2.5.1. Recommendations for Ankle-Brachial Index, Toe-Brachial Index, and Segmental Pressure Examination
Table 2 contains recommendations for ankle-brachial index (ABI), toe-brachial index, and segmental pressure examination. See Appendix 3 for supplemental information.
Table 2.
Recommendations for Ankle-Brachial Index, Toe-Brachial Index, and Segmental Pressure Examination
| 2005 Recommendations | 2011 Focused Update Recommendations | Comments |
|---|---|---|
| Class I | ||
| The resting ABI should be used to establish the lower extremity PAD diagnosis in patients with suspected lower extremity PAD, defined as individuals with exertional leg symptoms, with nonhealing wounds, who are 70 years and older or who are 50 years and older with a history of smoking or diabetes. (Level of Evidence: C) | 1. The resting ABI should be used to establish the lower extremity PAD diagnosis in patients with suspected lower extremity PAD, defined as individuals with 1 or more of the following: exertional leg symptoms, nonhealing wounds, age 65 years and older, or 50 years and older with a history of smoking or diabetes (9–11). (Level of Evidence: B) | Modified recommendation (age modified and level of evidence changed from CtoB). |
| The ABI should be measured in both legs in all new patients with PAD of any severity to confirm the diagnosis of lower extremity PAD and establish a baseline (12–14). (Level of Evidence: B) | 2005 recommendation remains current in 2011 focused update. | |
| The toe-brachial index should be used to establish the lower extremity PAD diagnosis in patients in whom lower extremity PAD is clinically suspected but in whom the ABI test is not reliable due to noncompressible vessels (usually patients with long-standing diabetes or advanced age) (15–19). (Level of Evidence: B) | 2005 recommendation remains current in 2011 focused update. | |
| Leg segmental pressure measurements are useful to establish the lower extremity PAD diagnosis when anatomic localization of lower extremity PAD is required to create a therapeutic plan (20–23). (Level of Evidence: B) | 2005 recommendation remains current in 2011 focused update. | |
| 2. ABI results should be uniformly reported with noncompressible values defined as greater than 1.40, normal values 1.00 to 1.40, borderline 0.91 to 0.99, and abnormal 0.90 or less (24). (Level of Evidence: B) | New recommendation |
ABI indicates ankle-brachial index; and PAD, peripheral artery disease.
The German Epidemiologic Trial on Ankle Brachial Index Study Group included 6,880 patients ≥65 years of age and demonstrated that 21% of the cohort had either asymptomatic or symptomatic PAD (11). On the basis of this large epidemiologic study, the 2011 writing group modified the age for consideration of ABI diagnostic testing to ≥65 years. The writing group considered the potential impact of lowering the PAD detection age to 65 years, acknowledging that the ABI test would be used in an incrementally larger “at-risk” population. This reflects the intent of both the original evidence-based document and this focused update to blunt the profound ongoing underdiagnosis and undertreatment of individuals with PAD until limb ischemic symptoms have become severe. This ABI recommendation is intended for office-based and vascular laboratory diagnostic use and is not intended to serve as a population screening tool. The writing group noted with confidence that no other cardiovascular disease diagnostic test can be applied in an age-defined clinical population with such a high detection rate, low to no risk, and low cost. We encourage expansion of the evidence base by design and completion of ABI screening studies.
The definitions of normal and abnormal ABI values have been modified based on publication of the results of the Ankle Brachial Index Collaboration (24). This includes a normal ABI range of 1.00 to 1.40, and abnormal values continue to be defined as those ≤0.90. ABI values of 0.91 to 0.99 are considered “borderline” and values >1.40 indicate noncompressible arteries.
The 2005 recommendations stated that segmental pressure measurements are useful in the diagnosis and anatomic localization of lower extremity PAD. The 2011 writing group recognized that vascular diagnostic laboratories could use segmental pressures, Doppler waveform analysis, pulse volume recordings, or ABI with duplex ultrasonography (or some combination of these methods) to document the presence and location of PAD in the lower extremity.
2.6. Treatment
2.6.1.4. RECOMMENDATIONS FOR SMOKING CESSATION
Table 3 contains recommendations for smoking cessation. See Appendix 3 for supplemental information
Table 3.
Recommendations for Smoking Cessation
| 2005 Recommendation | 2011 Focused Update Recommendations | Comments |
|---|---|---|
| Class I | ||
| 1. Patients who are smokers or former smokers should be asked about status of tobacco use at every visit (25-28). (Level of Evidence: A) | New recommendation | |
| 2. Patients should be assisted with counseling and developing a plan for quitting that may include pharmacotherapy and/or referral to a smoking cessation program (26,29). (Level of Evidence: A) | New recommendation | |
| Individuals with lower extremity PAD who smoke cigarettes or use other forms of tobacco should be advised by each of their clinicians to stop smoking and should be offered comprehensive smoking cessation interventions, including behavior modification therapy, nicotine replacement therapy, or bupropion. (Level of Evidence: B) | 3. Individuals with lower extremity PAD who smoke cigarettes or use other forms of tobacco should be advised by each of their clinicians to stop smoking and offered behavioral and pharmacological treatment. (Level of Evidence: C) | Modified recommendation (wording clarified and level of evidence changed from B to C). |
| 4. In the absence of contraindication or other compelling clinical indication, 1 or more of the following pharmacological therapies should be offered: varenicline, bupropion, and nicotine replacement therapy (30-33). (Level of Evidence: A) | New recommendation |
PAD indicates peripheral artery disease.
No prospective RCTs have examined the effects of smoking cessation on cardiovascular events in patients with lower extremity PAD. Observational studies have found that the risk of death, myocardial infarction, and amputation is substantially greater, and lower extremity angioplasty and open surgical revascularization patency rates are lower in individuals with PAD who continue to smoke than in those who stop smoking (34–36). In some studies, exercise time is greater in patients who stop smoking than in current smokers (37,38). Efforts to achieve smoking cessation are recommended for patients with lower extremity PAD. Physician advice coupled with frequent follow-up achieves 1-year smoking cessation rates of approximately 5% compared with only 0.1% in individuals who try to quit smoking without a physician's intervention (39). With pharmacological interventions such as nicotine replacement therapy and bupropion, 1-year smoking cessation rates of approximately 16% and 30%, respectively, are achieved in a general population of smokers (33).
Varenicline, a nicotinic receptor partial agonist, has demonstrated superior quit rates when compared with nicotine replacement and bupropion in several RCTs (30–32). The superior smoking cessation may result from better reductions in craving and withdrawal symptoms (40). Despite its greater cost, varenicline is cost-effective because of its improved quit rates (41). In 2009, the US Food and Drug Administration released a Public Health Advisory noting that both bupropion and varenicline have been associated with reports of changes in behavior such as hostility, agitation, depressed mood, and suicidal thoughts or actions. In patients with PAD specifically, comprehensive smoking cessation programs that included individualized counseling and pharmacological support significantly increased the rate of smoking cessation at 6 months compared with verbal advice to quit smoking (21.3% versus 6.8%, p=0.02) (29). Tobacco cessation interventions are particularly critical in individuals with thromboangiitis obliterans, because it is presumed that components of tobacco may be causative in the pathogenesis of this syndrome, and continued use is associated with a particularly adverse outcome (42).
2.6.1.6. RECOMMENDATIONS FOR ANTIPLATELET AND ANTITHROMBOTIC DRUGS
Table 4 contains recommendations for antiplatelet and anti-thrombotic drugs. See Appendix 3 for supplemental information.
Table 4.
Recommendations for Antiplatelet and Antithrombotic Drugs
| 2005 Recommendations | 2011 Focused Update Recommendations | Comments |
|---|---|---|
| Class I | ||
| Antiplatelet therapy is indicated to reduce the risk of MI, stroke, or vascular death in individuals with atherosclerotic lower extremity PAD. (Level of Evidence: A) | 1. Antiplatelet therapy is indicated to reduce the risk of MI, stroke, and vascular death in individuals with symptomatic atherosclerotic lower extremity PAD, including those with intermittent claudication or critical limb ischemia, prior lower extremity revascularization (endovascular or surgical), or prior amputation for lower extremity ischemia (43–45). (Level of Evidence: A) | Modified recommendation (wording clarified). |
| Aspirin, in daily doses of 75 to 325 mg, is recommended as safe and effective antiplatelet therapy to reduce the risk of MI, stroke, or vascular death in individuals with atherosclerotic lower extremity PAD. (Level of Evidence: A) | 2. Aspirin, typically in daily doses of 75 to 325 mg, is recommended as safe and effective antiplatelet therapy to reduce the risk of MI, stroke, or vascular death in individuals with symptomatic atherosclerotic lower extremity PAD, including those with intermittent claudication or critical limb ischemia, prior lower extremity revascularization (endovascular or surgical), or prior amputation for lower extremity ischemia (44,45). (Level of Evidence: B) | Modified recommendation (wording clarified; and level of evidence changed from A to B). |
| Clopidogrel (75 mg per day) is recommended as an effective alternative antiplatelet therapy to aspirin to reduce the risk of MI, stroke, or vascular death in individuals with atherosclerotic lower extremity PAD. (Level of Evidence: B) | 3. Clopidogrel (75 mg per day) is recommended as a safe and effective alternative antiplatelet therapy to aspirin to reduce the risk of MI, ischemic stroke, or vascular death in individuals with symptomatic atherosclerotic lower extremity PAD, including those with intermittent claudication or critical limb ischemia, prior lower extremity revascularization (endovascular or surgical), or prior amputation for lower extremity ischemia (43). (Level of Evidence: B) | Modified recommendation (wording clarified). |
| Class IIa | ||
| 1. Antiplatelet therapy can be useful to reduce the risk of MI, stroke, or vascular death in asymptomatic individuals with an ABI less than or equal to 0.90 (45). (Level of Evidence: C) | New recommendation | |
| Class IIb | ||
| 1. The usefulness of antiplatelet therapy to reduce the risk of MI, stroke, or vascular death in asymptomatic individuals with borderline abnormal ABI, defined as 0.91 to 0.99, is not well established (46,47). (Level of Evidence: A) | New recommendation | |
| 2. The combination of aspirin and clopidogrel may be considered to reduce the risk of cardiovascular events in patients with symptomatic atherosclerotic lower extremity PAD, including those with intermittent claudication or critical limb ischemia, prior lower extremity revascularization (endovascular or surgical), or prior amputation for lower extremity ischemia and who are not at increased risk of bleeding and who are at high perceived cardiovascular risk (48,49). (Level of Evidence: B) | New recommendation | |
| Class III: No benefit | ||
| Oral anticoagulation therapy with warfarin is not indicated to reduce the risk of adverse cardiovascular ischemic events in individuals with atherosclerotic lower extremity PAD. (Level of Evidence: C) | 1. In the absence of any other proven indication for warfarin, its addition to antiplatelet therapy to reduce the risk of adverse cardiovascular ischemic events in individuals with atherosclerotic lower extremity PAD is of no benefit and is potentially harmful due to increased risk of major bleeding (50). (Level of Evidence: B) | Modified recommendation (level of evidence changed from C to B). |
ABI indicates ankle-brachial index; MI, myocardial infarction; and PAD, peripheral artery disease.
The writing group reviewed 5 RCTs and 1 meta-analysis related to antiplatelet therapy and PAD as part of this focused update (45–48,51). Although the 2002 Antithrombotic Trial-ists’ Collaboration meta-analysis demonstrated a significant reduction in cardiovascular events among symptomatic PAD patients randomized to antiplatelet therapy versus placebo, there was significant heterogeneity of enrollment criteria and antiplatelet dosing regimens among the trials (44). The results of 3 RCTs of aspirin use (100 mg daily) versus placebo for cardiovascular risk reduction among patients with PAD have been published since the 2005 guideline (45–47). These trials yielded mixed results, with the 2 larger trials with longer duration of follow-up demonstrating no benefit of aspirin (46,47). However, both of these studies enrolled only asymptomatic patients derived from population screening (not clinical populations) based on very mild decrements in ABI and thus represented relatively low-risk cohorts. The POPADAD (Prevention of Progression of Asymptomatic Diabetic Arterial Disease) study enrolled individuals with an ABI ≤0.99, whereas the Aspirin for Asymptomatic Atherosclerosis trial used a cutpoint of ABI ≤0.95 but calculated the ABI using the lower pedal pressure at the ankle. This method is in contrast to standard clinical practice (and this guideline) of using the higher pedal pressure at the ankle for determining ABI (46,47). These factors limit the generalizability of the results to patients with clinical PAD who are symptomatic and/or have lower ABI values and face a greater risk of ischemic events. The CLIPS (Critical Leg Ischemia Prevention Study) trial, which was the smallest of the 3 antiplatelet therapy trials reviewed, enrolled patients with more advanced PAD, defined by both symptoms and/or ABI values (ABI <0.85), and demonstrated a significant reduction in cardiovascular ischemic events among subjects randomized to aspirin (45). Of note, this trial was stopped early because of poor recruitment, with only 366 of a planned 2,000 patients enrolled. The 2009 meta-analysis of aspirin therapy for patients with PAD demonstrated a 34% risk reduction for nonfatal stroke among participants taking aspirin but no statistically significant reduction in overall cardiovascular events (51). This study included the CLIPS and POPADAD trials but not the Aspirin for Asymptomatic Atherosclerosis trial.
The recommended dose range of aspirin has been modified to 75 mg to 325 mg per day to reflect the doses studied in the aspirin clinical trials and in use in clinical practice. The 2005 recommendation of clopidogrel as an alternative to aspirin therapy is unchanged. No new clinical trials have directly compared aspirin monotherapy therapy with clopidogrel since the CAPRIE (Clopidogrel versus Aspirin in Patients at Risk of Ischemic Events) study demonstrated an incremental benefit of clopidogrel (43). On the basis of the findings of the CHARISMA (Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance) trial, it may be reasonable to consider combination antiplatelet therapy with aspirin plus clopidogrel for certain high-risk patients with PAD who are not considered at increased risk of bleeding (48,49,52). Selection of an antiplatelet regimen for the PAD patient should be individualized on the basis of tolerance and other clinical characteristics (i.e., bleeding risk) along with cost and guidance from regulatory agencies.
The WAVE (Warfarin Antiplatelet Vascular Evaluation) trial provided further evidence against the use of oral anticoagulation therapy in addition to antiplatelet therapy for prevention of cardiovascular events among patients with PAD, and the level of evidence is upgraded to B for this Class III recommendation (50).
The writing group emphasizes that selection of the optimal antiplatelet therapy and determination of optimum dosage in well-defined populations of patients with PAD are critical unanswered scientific questions. There is a need for additional data from large-scale RCTs and observational studies to investigate the efficacy and risk of antiplatelet medications across the spectrum of PAD defined according to symptom class (symptomatic versus asymptomatic) and objective measures of atherosclerosis severity (i.e., ABI value).
To date, no clinical trials have examined the efficacy of new antithrombotic medications such as prasugrel, ticagrelor, or vorapaxar to reduce ischemic events in patients with lower extremity PAD.
2.6.3. Recommendations for Critical Limb Ischemia: Endovascular and Open Surgical Treatment for Limb Salvage
Table 5 contains recommendations for endovascular and open surgical treatment for limb salvage in patients with critical limb ischemia. See Appendix 3 for supplemental information.
Table 5.
Recommendations for Critical Limb Ischemia: Endovascular and Open Surgical Treatment for Limb Salvage
| 2005 Recommendations | 2011 Focused Update Recommendations | Comments |
|---|---|---|
| Class I | ||
| For individuals with combined inflow and outflow disease with critical limb ischemia, inflow lesions should be addressed first. (Level of Evidence: C) | 2005 recommendation remains current in 2011 focused update. | |
| For individuals with combined inflow and outflow disease in whom symptoms of critical limb ischemia or infection persist after inflow revascularization, an outflow revascularization procedure should be performed (53). (Level of Evidence: B) | 2005 recommendation remains current in 2011 focused update. | |
| If it is unclear whether hemodynamically significant inflow disease exists, intraarterial pressure measurements across suprainguinal lesions should be measured before and after the administration of a vasodilator. (Level of Evidence: C) | 2005 recommendation remains current in 2011 focused update. | |
| Class IIa | ||
| 1. For patients with limb-threatening lower extremity ischemia and an estimated life expectancy of 2 years or less or in patients in whom an autogenous vein conduit is not available, balloon angioplasty is reasonable to perform when possible as the initial procedure to improve distal blood flow (54). (Level of Evidence: B) | New recommendation | |
| 2. For patients with limb-threatening ischemia and an estimated life expectancy of more than 2 years, bypass surgery, when possible and when an autogenous vein conduit is available, is reasonable to perform as the initial treatment to improve distal blood flow (54). (Level of Evidence: B) | New recommendation |
The writing group has reviewed the results of the multicenter BASIL (Bypass Versus Angioplasty in Severe Ischaemia of the Leg) trial funded by the United Kingdom National Institute of Health Research and Health Technology Assessment Programme (54). During a 5-year period, 452 patients with severe limb ischemia (characterized by rest/night pain and tissue loss, such as skin ulceration and gangrene, and thus including patients defined by this PAD guideline syndrome term critical limb ischemia) were randomly assigned to an initial treatment strategy of either open surgery or balloon angioplasty. Major clinical outcomes evaluated in this trial were amputation-free survival and overall survival. The initial results published in 2005 indicated that in patients with severe limb ischemia due to infrainguinal disease, the short-term clinical outcomes between bypass surgery–first and balloon angioplasty–first were similar (54,55). These initial results showed that bypass surgery–first was one third more expensive and was associated with higher morbidity than balloon angioplasty–first.
The trial also initially suggested that after 2 years, patients treated with balloon angioplasty–first had increased overall survival rates and fewer amputations. However, this early finding was based on a post hoc analysis of a relatively small number of outcome events. Thus, more prolonged follow-up was necessary to confirm or refute this finding. The results of a 2.5-year follow-up have been published (54) and confirm that there was no significant difference in amputation-free survival and overall survival between the 2 treatment strategies. However, a bypass surgery–first approach was associated with a significant increase in overall survival of 7.3 months (95% CI: 1.2 to 13.4 months; p=0.02) and a trend toward improved amputation-free survival of 5.9 months (95% CI: 0.2 to 12.0 months; p=0.06) for those patients who survived for at least 2 years after randomization. In summary, for all patients in the trial, there was no significant difference between the 2 treatment strategies in amputation-free survival or overall survival. However, these data suggest that it is reasonable for a bypass surgery–first approach to be considered for these carefully selected patients to prolong amputation-free survival and overall survival. This study has also confirmed that the outcomes following prosthetic bypass were extremely poor. Balloon angioplasty, when possible, may be preferable to prosthetic bypass even in patients with a life expectancy of >2 years (54).
5. Aneurysm of the Abdominal Aorta, Its Branch Vessels, and the Lower Extremities
5.2.8.1. RECOMMENDATIONS FOR MANAGEMENT OVERVIEW
Table 6 contains recommendations for management of abdominal aortic aneurysm (AAA). See Appendix 3 for supplemental information.
Table 6.
Recommendations for Management of Abdominal Aortic Aneurysm
| 2005 Recommendations | 2011 Focused Update Recommendations | Comments |
|---|---|---|
| Class I | ||
| Open repair of infrarenal AAA and/or common iliac aneurysms is indicated in patients who are good or average surgical candidates. (Level of Evidence: B) | 1. Open or endovascular repair of infrarenal AAAs and/or common iliac aneurysms is indicated in patients who are good surgical candidates (56,57). (Level of Evidence: A) | Modified recommendation (endovascular repair incorporated from 2005 Class IIb recommendation [see below*]; level of evidence changed from B to A). |
| Periodic long-term surveillance imaging should be performed to monitor for an endoleak, to document shrinkage or stability of the excluded aneurysm sac, and to determine the need for further intervention in patients who have undergone endovascular repair of infrarenal aortic and/or iliac aneurysms. (Level of Evidence: B) | 2. Periodic long-term surveillance imaging should be performed to monitor for endoleak, confirm graft position, document shrinkage or stability of the excluded aneurysm sac, and determine the need for further intervention in patients who have undergone endovascular repair of infrarenal aortic and/or iliac aneurysms (56,58). (Level of Evidence: A) | Modified recommendation (level of evidence changed from B to A). |
| Class IIa | ||
| Endovascular repair of infrarenal aortic and/or common iliac aneurysms is reasonable in patients at high risk of complications from open operations because of cardiopulmonary or other associated diseases. (Level of Evidence: B) | Deleted recommendation (no longer current). | |
| 1. Open aneurysm repair is reasonable to perform in patients who are good surgical candidates but who cannot comply with the periodic long-term surveillance required after endovascular repair. (Level of Evidence: C) | New recommendation | |
| Class IIb | ||
| Endovascular repair of infrarenal aortic and/or common iliac aneurysms may be considered in patients at low or average surgical risk. (Level of Evidence: B) | Deleted recommendation (endovascular repair incorporated into 2011 Class I, #1 [see above*]). | |
| 1. Endovascular repair of infrarenal aortic aneurysms in patients who are at high surgical or anesthetic risk as determined by the presence of coexisting severe cardiac, pulmonary, and/or renal disease is of uncertain effectiveness (59). (Level of Evidence: B) | New recommendation |
Indicates merging of deleted 2005 Class IIb recommendation with the modified 2011 Class I, #1 recommendation.
AAA indicates abdominal aortic aneurysm.
Although the methods of treatment for infrarenal abdominal aortic and iliac artery aneurysms have changed little over the past 5 years, a greater understanding of the appropriate application of these technologies and techniques has been gained. Overall, open and endovascular repair techniques have demonstrated clinical equivalence over time, with similar rates of overall and aneurysm-related mortality and morbidity.
For patients with an infrarenal AAA who are likely to live >2 years and who are good risk surgical candidates, open or endovascular intervention is indicated. There is no long-term advantage to either technique of aneurysm repair. This was clearly demonstrated in 2 large multicenter, randomized, prospective studies. The EVAR (United Kingdom Endovascular Aneurysm Repair) trial evaluated the outcomes of patients ≥60 years of age who were appropriate candidates for either endovascular or open repair of infrarenal AAAs that were at least 5.5 cm in diameter based on computed tomographic imaging (56). Over 5 years, 1,252 patients were enrolled and randomly assigned to either stent graft or open aneurysm repair. The primary outcomes measures were all-cause mortality and aneurysm-related mortality, and data were analyzed on an intention-to-treat basis. Follow-up was a minimum of 5 years or until death, with a median postprocedural follow-up of 6 years. The treatment groups, which were 90.7% male with a mean age of 74 years, were uniform with regard to comorbidities. There was a significant difference in procedural mortality between endovascular and open repair (1.8% endovascular repair versus 4.3% open repair, p=0.02, adjusted odds ratio: 0.39; 95% CI: 0.18 to 0.87). Over time, this initial benefit was not sustained. Over the period of observation, all-cause mortality in the endovascular group was 7.5 deaths per 100 person-years compared with 7.7 deaths per 100 person-years in the open-surgery group (p=0.72; adjusted HR: 1.03; 95% CI: 0.86 to 1.23). Aneurysm-related mortality was also similar, with 1.0 death per 100 person-years in the stent graft group compared with 1.2 deaths per 100 person-years in the open-surgery group (p=0.73; adjusted HR: 0.92; 95% CI: 0.57 to 1.49). Reintervention was required in 5.1% of patients treated with an endograft but in only 1.7% of those who underwent open surgery (p=0.001), underscoring the need for careful evaluation of the stent graft over time (56).
These findings were consistent with those reported in another multicenter, randomized, prospective trial (58). The DREAM (Dutch Randomized Endovascular Aneurysm Repair) trial evaluated the long-term outcomes of patients with infrarenal aortic aneurysms ≥5 cm who were randomized to either endovascular or open surgical treatment. The primary outcome measure was all-cause mortality. There were no differences in demographic characteristics or comorbidities between the 178 patients assigned to open surgery and the 173 patients assigned to endovascular intervention. Similar to the EVAR trial, the majority of patients in the DREAM trial were male (91.7%), with a mean age of 70 years. The minimum follow-up was 5 years, and the median was 6.4 years. Over this period of time the mortality rate of the 2 groups was not different. The overall survival rate was 69.9% in the open-surgery group and 68.9% among those undergoing stent graft repair (difference: 1.0%; 95% CI: −8.8 to 10.8; p=0.97). Although cardiovascular disease was the single most common cause of death, it accounted for only 33% of the deaths in the open-surgery group and 27.6% of the deaths in the endovascular treatment group. Deaths from noncardiovascular causes, such as cancer, were more common. During the follow-up period, freedom from secondary intervention was more common in the open-repair group compared with the endovascular treatment group (difference 11.5%; 95% CI: 2.0 to 21.0; p=0.03) (58).
More recently, a third trial has buttressed the results of the EVAR and DREAM trials. The OVER (Open Surgery Versus Endovascular Repair Veterans Affairs Cooperative Study) trial randomized 881 veterans with AAA ≥5 cm or an associated iliac artery aneurysm ≥3 cm or an AAA ≥4.5 cm with rapid enlargement to surgical or endovascular repair (60). The primary outcome was long-term, all-cause mortality. As with both the DREAM and EVAR trials, there were no differences in baseline demographic characteristics. The trial participants were overwhelmingly male (>99%), white (87%), and current or former smokers (95%). Over a mean follow-up of 1.8 years, there was no statistical difference in mortality, 7% versus 9.8% for endovascular and surgical repair, respectively (p=0.13). Interestingly, there were no differences in the rates of secondary therapeutic procedures or aneurysm-related hospitalizations between the groups, because increases in surgical complications offset the number of secondary endovascular repairs.
As with the EVAR trial, the DREAM and OVER trials confirmed that the early benefits of endovascular aneurysm repair, including a lower procedural mortality, are not sustained. Therefore, the method of aneurysm repair that is deemed to be most appropriate for each individual patient should be chosen (56,58,60). Endovascular treatment should not be used in patients who do not meet the established anatomical criteria or who cannot comply with the required follow-up imaging requirements. Patients require either computed tomography or magnetic resonance imaging of the engrafted segment of the aortoiliac segment at 1 month, 6 months, and then yearly to confirm that the graft has not moved and there are no endoleaks that have resulted in repressurization and/or growth of the aneurysm sac. If patients cannot be offered the indicated long-term follow-up evaluation and treatment because of the lack of access to required imaging modalities or inability to appropriately treat problematic endoleaks when identified, then endovascular repair should not be considered the optimal treatment method. Open surgical repair is indicated for those patients who do not meet the established criteria for endovascular treatment.
A patient whose general physical condition is deemed unsuitable for open aneurysm repair may not benefit from endovascular repair. This was suggested in a secondary protocol of the EVAR trial (56). The EVAR 2 trial randomized 404 patients with infrarenal aortic aneurysms of at least 5.5 cm with comorbidities that prevented open repair to receive either endovascular treatment or no intervention (61). One hundred ninety-seven patients were randomized to the endovascular treatment group and 179 actually underwent stent graft placement. Of 207 patients randomly assigned to the no-treatment group, 70 had aneurysm repair. The primary outcome was death from any cause. The patients were followed up for a minimum of 5 years or until death. The median follow-up period was 3.1 years. Thirty-day operative mortality was 7.3%. Although a significant difference in aneurysm-related mortality between the 2 groups was identified (3.6 deaths per 100 person-years for endovascular therapy versus 7.3 deaths per 100 person-years without treatment, adjusted HR: 0.53; 95% CI: 0.32 to 0.89; p=0.02), this was not associated with longer survival. During follow-up there was no significant difference in overall mortality between the 2 groups (21.0 deaths per 100 person-years in the endovascular group versus 22.1 deaths per 100 person-years in the no-treatment group; HR for endovascular repair: 0.99; CI: 0.78 to 1.27; p=0.97). Although there was no observed benefit to the endovascular treatment of infrarenal AAAs in patients whose physical health was considered too poor to withstand open aneurysm repair in this trial, optimal management of this challenging patient population has not been definitively established. Additional studies are required to better define the role of endovascular aneurysm repair in patients with significantly impaired physical health who are considered to be at high surgical or anesthetic risk (61). d to better define the role of endovascular aneurysm repair in patients with significantly impaired physical health who are considered to be at high surgical or anesthetic risk (61).
Supplementary Material
Appendix
Appendix 1.
Author Relationships With Industry and Other Entities (Relevant)—2011 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Peripheral Artery Disease
| Writing Group Member |
Employment | Consultant | Speakers’ Bureau |
Ownership/ Partnership/ Principal |
Personal Research | Institutional, Organizational, or Other Financial Benefit |
Expert Witness | Voting Recusal (by Section)* |
|---|---|---|---|---|---|---|---|---|
| Thom W. Rooke, Chair | Mayo Clinic—Professor of Medicine | None | None | None | None | None | None | None |
| Alan T. Hirsch, Vice Chair | University of Minnesota Medical School: Cardiovascular Division—Vascular Medicine Program: Director; Professor of Medicine: Epidemiology and Community Health | • eV3 | None | None | • Abbott
Vasculart • BMS/sanofi-aventist • Cytokinetics • Sanofi-aventist • ViroMed (PI) |
None | None | 2.5.1 2.6.1.6 2.6.3 |
| Sanjay Misra, Vice Chair | Mayo Clinic: Division of Vascular and Interventional Radiology—Associate Professor of Radiology | • Johnson & Johnson | None | None | None | None | None | 2.6.3 |
| Anton N. Sidawy, Vice Chair | George Washington University—Professor and Chairman, Department of Surgery | None | None | None | None | None | None | None |
| Joshua A. Beckman | Brigham and Women's Hospital Cardiovascular Division: Cardiovascular Fellowship Program—Director | • Bristol-Myers
Squibb† • Sanofi-aventis† |
None | None | None | None | None | 2.6.1.6 |
| Laura K. Findeiss | University of California, Irvine:
Chief, Division of Vascular and
Interventional Radiology—Associate Professor of Radiology and Surgery |
None | None | None | None | None | None | None |
| Jafar Golzarian | University of Minnesota Medical School—Professor of Radiology and Surgery | None | None | None | None | None | None | None |
| Heather L. Gornik | Cleveland Clinic Foundation Cardiovascular Medicine: Noninvasive Vascular Laboratory—Medical Director | None | None | None | • Summit Doppler Systems† | • Summit Doppler Systems† | None | 2.5.1 |
| Jonathan L. Halperin | Mount Sinai Medical Center—Professor of Medicine | • Bayer
HealthCare • Boehringer Ingelheim† • Daiichi-Sankyo • Johnson & Johnson • Portola Pharmaceuticals • Sanofi-aventis† |
None | None | • NIH-NHLBI (DSMB) | None | None | 2.6.1.6 |
| Michael R. Jaff | Harvard Medical School—Associate Professor of Medicine | • Abbott Vascular‡ • Boston Scientific‡ • Medtronic Vascular‡ |
None | None | None | None | None | 2.6.3 |
| Gregory L. Moneta | Oregon Health & Science University—Chief and Professor of Vascular Surgery | None | None | None | None | None | None | None |
| Jeffrey W. Olin | Mount Sinai School of Medicine—Professor of Medicine and Director of the Vascular Medicine Program | • Genzyme | None | None | •
BMS/sanofi-aventis • Colorado Prevention Center (DSMB) • Merck |
None | • Defendant; pulmonary embolism; 2009 | 2.6.1.6 |
| James C. Stanley | University of Michigan, Division of Vascular Surgery, University Hospital—Handleman Professor of Surgery | None | None | None | None | None | None | None |
| Christopher J. White | Ochsner Clinic Foundation: Department of Cardiology—Chairman | None | None | None | • Boston Scientific‡ • Neovasc‡ • St. Jude Medical‡ |
None | None | 2.6.3 5.2.6 |
| John V. White | Advocate Lutheran General Hospital—Chief of Surgery | None | None | None | None | None | None | None |
| R. Eugene Zierler | University of Washington—Professor of Surgery | None | None | None | None | None | None | None |
This table represents the relationships of writing group members with industry and other entities that were determined to be relevant to this document. These relationships were reviewed and updated in conjunction with all meetings and/or conference calls of the writing group during the document development process. The table does not necessarily reflect relationships with industry at the time of publication. A person is deemed to have a significant interest in a business if the interest represents ownership of ≥5% of the voting stock or share of the business entity, or ownership of ≥$10,000 of the fair market value of the business entity; or if funds received by the person from the business entity exceed 5% of the person's gross income for the previous year. Relationships that exist with no financial benefit are also included for the purpose of transparency. Relationships in this table are modest unless otherwise noted.
According to the ACCF/AHA, a person has a relevant relationship IF: (a) The relationship or interest relates to the same or similar subject matter, intellectual property or asset, topic, or issue addressed in the document; or (b) the company/entity (with whom the relationship exists) makes a drug, drug class, or device addressed in the document, or makes a competing drug or device addressed in the document; or (c) the person or a member of the person's household, has a reasonable potential for financial, professional or other personal gain or loss as a result of the issues/content addressed in the document.
Writing group members are required to recuse themselves from voting on sections to which their specific relationships with industry and other entities may apply.
Significant relationship.
No financial benefit.
DSMB indicates Data and Safety Monitoring Board; NHLBI, National Heart, Lung, and Blood Institute; NIH, National Institutes of Health; and PI, principal investigator.
Appendix 2.
Reviewer Relationships With Industry and Other Entities (Relevant)—2011 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Peripheral Artery Disease
| Peer Reviewer | Representation | Consultant | Speakers’ Bureau | Ownership/ Partnership/ Principal |
Personal Research | Institutional, Organizational, or Other Financial Benefit |
Expert Witness |
|---|---|---|---|---|---|---|---|
| Eric R. Bates | Official Reviewer—Board of Trustees | • Bristol-Myers
Squibb • Daiichi-Sankyo • Merck • Sanofi-aventis |
None | None | None | None | None |
| Mark A. Creager | Official Reviewer—ACCF/AHA Task Force on Practice Guidelines | • Genzyme | None | None | None | None | None |
| William R. Hiatt | Official Reviewer—AHA | None | None | None | • BMS/sanofi-aventis | None | None |
| Hani Jneid | Official Reviewer—AHA | None | None | None | None | None | None |
| Krishnaswami Vijayaraghavan | Official Reviewer—Board of Governors | • Daiichi-Sankyo | •
Sanofi-aventis • Novartis |
None | None | • Johnson &
Johnson* • Merck |
None |
| Gary Ansel | Organizational Reviewer—SCAI | • Bard • Boston Scientific* • Cordis/Johnson & Johnson* • ev3 |
• Cordis/Johnson & Johnson* | None | • Abbott/Guidant
Vascular • Boston Scientific* • Cook Medical* |
None | None |
| Yung-wei Chi | Organizational Reviewer—SVM | None | None | None | None | None | None |
| Michael Conte | Organizational Reviewer—SVS | None | None | None | None | None | None |
| Tony Das | Organizational Reviewer—SCAI | • Abbott Vascular* • Bard* • Boston Scientific • Cordis* |
None | None | None | None | None |
| Thomas Huber | Organizational Reviewer—SVS | None | None | None | None | • Abbott Vascular† • Cook† • Medtronic† |
None |
| John P. Reilly | Organizational Reviewer—SVM | None | • Cordis • Johnson & Johnson • Lilly/Daiichi-Sankyo* |
None | None | None | |
| Wael A. Saad | Organizational Reviewer—SIR | None | None | None | None | None | None |
| T. Gregory Walker | Organizational Reviewer—SIR | • Medtronic Endovascular | None | None | None | None | None |
| J. Dawn Abbott | Content Reviewer—ACCF PVD Committee | • Medtronic Endovascular | None | None | None | None | None |
| Jeffrey L. Anderson | Content Reviewer—ACCF/AHA Task Force on Practice Guidelines | None | None | None | None | None | None |
| Herbert D. Aronow | Content Reviewer—ACCF PVD Committee | • Medtronic Endovascular | None | None | None | None | None |
| Jeffrey Berger | Content Reviewer | None | None | None | None | None | None |
| Lee A. Green | Content Reviewer—ACCF/AHA Task Force on Performance Measures | None | None | None | None | None | None |
| John Gordon | Content Reviewer—Board of Governors | None | None | None | None | None | None |
| Norman R. Hertzer | Content Reviewer—2005 PAD Writing Committee | None | None | None | None | None | None |
| Courtney O. Jordan | Content Reviewer—ACCF Prevention Committee | None | None | None | None | None | None |
| Prakash Krishnan | Content Reviewer | None | None | None | None | None | None |
| Michael Mansour | Content Reviewer—Board of Governors | None | None | None | None | None | None |
| Issam D. Moussa | Content Reviewer—ACCF Interventional Scientific Council | None | None | None | None | None | None |
| Rahul Patel | Content Reviewer—2005 PAD Writing Committee | None | None | None | None | None | None |
| Pam N. Peterson | Content Reviewer—ACCF/AHA Task Force on Clinical Data Standards | None | None | None | None | None | None |
| John Rundback | Content Reviewer—2005 PAD Writing Committee | • ev3 | • Boston Scientific | None | None | None | None |
This table represents the relationships of reviewers with industry and other entities that were disclosed at the time of peer review and determined to be relevant. It does not necessarily reflect relationships with industry at the time of publication. A person is deemed to have a significant interest in a business if the interest represents ownership of ≥5% of the voting stock or share of the business entity, or ownership of ≥$10,000 of the fair market value of the business entity; or if funds received by the person from the business entity exceed 5% of the person's gross income for the previous year. A relationship is considered to be modest if it is less than significant under the preceding definition. Relationships that exist with no financial benefit are also included for the purpose of transparency. Relationships in this table are modest unless otherwise noted. Names are listed in alphabetical order within each category of review.
According to the ACCF/AHA, a person has a relevant relationship IF: (a) The relationship or interest relates to the same or similar subject matter, intellectual property or asset, topic, or issue addressed in the document; or (b) the company/entity (with whom the relationship exists) makes a drug, drug class, or device addressed in the document, or makes a competing drug or device addressed in the document; or (c) the person or a member of the person's household, has a reasonable potential for financial, professional or other personal gain or loss as a result of the issues/content addressed in the document.
Significant relationship.
No financial benefit.
ACCF indicates American College of Cardiology Foundation; AHA, American Heart Association; PAD, peripheral artery disease; PVD, peripheral vascular disease; SCAI, Society for Cardiovascular Angiography and Interventions; SIR, Society of Interventional Radiology; SVM, Society for Vascular Medicine; and SVS, Society for Vascular Surgery.
Appendix 3.
2011 Peripheral Artery Disease Focused Update Summary Table
| Patient
Population/Inclusion and Exclusion Criteria |
Endpoints |
Study Conclusion (as Reported in Study Article) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study Title | Aim of Study | Study Type | Study Size | Inclusion | Exclusion | Primary | Secondary | Statistical Analysis (Results) | p (95% CI) | OR/HR/RR | Other Information | |
| Revascularization
versus medical therapy for RAS: the ASTRAL Investigators (5) |
To review the clinical benefit of percutaneous revascularization of the renal arteries to improve patency in atherosclerotic renovascular disease |
Randomized, unblinded trial |
806 | Patients who had
substantial anatomical atherosclerotic stenosis in ≥1 renal artery that was considered potentially suitable for endovascular revascularization and whose physician was uncertain that the patient would definitely receive a worthwhile clinical benefit from revascularization, taking into account the available evidence |
Patients who
required surgical revascularization or were considered to have a high likelihood of requiring revascularization within 6 mo, if they had nonatheromatous CV disease, or if they had undergone previous revascularization for RAS |
Renal function, measured by the reciprocal of the serum creatinine level |
Blood pressure, time to renal and major CV events, and mortality |
During a 5-y period, rate of
progression of renal impairment (as shown by the slope of the reciprocal of the serum creatinine level) was −0.07×10−3 L/micromole/y in the revascularization group, compared with −0.13×10−3 L/micromole/y in the medical therapy group, a difference favoring revascularization of 0.06×10−3 L/micromole/y (95% CI: −0.002 to 0.13; p=0.06). Over the same time, mean serum creatinine level was 1.6 mmol/L (95% CI: −8.4 to 5.2 [0.02 mg/dL; 95% CI: −0.10 to 0.06]) lower in the revascularization group than in the medical therapy group. There was no significance between-groups difference in systolic blood pressure; decrease in diastolic blood pressure was smaller in the revascularization group than in the medical-therapy group. |
Revascularization
group: p=0.88; 95% CI: 1.40; 0.67 to 1.40 Major CVevents: p=0.61; 95% CI: 0.75 to 1.1 Death: p= 0.46; 95% CI: 0.69 to 1.18 |
The 2 study groups had
similar rates of renal events. Revascularization group: HR: 0.97; 95% CI: 0.67 to 1.40; p=0.88 Major CV events: HR: 0.94; 95% CI: 0.75 to 1.19; p=0.61 Death: HR: 0.90; 95% CI: 0.69 to 1.18; p=0.46 |
There are substantial risks but
no evidence of a worthwhile clinical benefit from revascularization in patients with atherosclerotic renovascular disease. |
Power=80%, ITT analysis |
| ABI combined with FRS
to predict CV events and mortality: a meta-analysis ABI collaboration (24) |
To determine if ABI provides information on risk of CV events and mortality independent of FRS and can improve risk prediction |
Meta-analysis | 24,955 men and 23 339 women with 480,325 person- years of follow-up. Studies included 16 population cohort studies. |
Studies whose participants were derived from a general population, measured ABI at baseline, and individual followed up to detect total and CV mortality |
N/A | Risk of death by ABI had a reverse
J- shaped distribution with a normal (low- risk) ABI of 1.11 to 1.40.10-y CV mortality in men with low ABI (0.90) was 18.7% (95% CI: 13.3% to 24.1%) and with normal ABI (1.11 to 1.40) was 4.4% (95% CI: 3.2% to 5.7%). Corresponding mortalities in women were 12.6% (95% CI: 6.2% to 19.0%) and 4.1% (95% CI: 2.2% to 6.1%). Low ABI (0.90) was associated with approximately twice the 10-y total mortality, CV mortality, and major coronary event rate compared with the overall rate in each FRS category. Inclusion of ABI in CV risk stratification using the FRS would result in reclassification of risk category and modification of treatment recommendations in ~19% of men and 36% of women. |
10-y CVmortality: Men: HR: 4.2; 95% CI: 3.3to 5.4 Women: HR: 3.5; 95% CI: 2.4to 5.1 |
Measurement of ABI may
improve accuracy of CV risk prediction beyond FRS. |
Relevant studies were
identified. Asearch of MEDLINE (1950 to February 2008) and EMBASE (1980 to February2008) was conducted using common text words for the term ABI combined with text words and medical subject headings to capture prospective cohort designs. |
|||
| Outcomes following endovascular vs. open repair of AAA: a randomized trial (60) |
To
compare postoperative outcomes up to 2 y after endovascular or open repair of AAA (interim report of a 9-y trial) |
Randomized, multicenter clinical trial; elective endovascular (n=444) or open (n=437) repair of AAA |
881 | Veterans (49 y old) from 42 VA Medical Centers with eligible AAA who were candidates for both elective endovascular repair and open repair of AAA |
N/A | Long-term (5 to 9 y) all-cause mortality |
2° outcomes
included: 1)procedure failure, 2)short-term major morbidity, 3)in-hospital and ICUs associated with initial repair, 4)other procedure- related morbidities such as incisional hernia or new or worsened claudication, 5)HRQOL, and 6)erectile dysfunction. 2° outcomes cover short-term perioperative period |
Perioperative mortality (30-d or
inpatient) was lower for endovascular repair (0.5% vs. 3.0%; p=0.004); no significant difference in mortality at 2 y (7.0% vs. 9.8%; p=0.13). Patients in endovascular repair group had reduced median procedure time (2.9 vs. 3.7 h), blood loss (200 vs. 1,000 mL), transfusion requirement (0 vs. 1.0 units), duration of mechanical ventilation (3.6 vs. 5.0 h), hospital stay (3 vs. 7 d), and ICU stay (1 vs. 4 d), but required substantial exposure to fluoroscopy and contrast. No differences between the 2 groups in major morbidity, procedure failure, 2° therapeutic procedures, aneurysm- related hospitalizations, HRQOL, or erectile function. |
Perioperative mortality: p= 0.004; Mortality at 2 y: p=0.13 |
HR: 0.7; 95% CI: 0.4 to 1.1 | Short-term outcomes
after elective AAA repair, perioperative mortality was low for both procedures and lower for endovascular than open repair. Early advantage of endovascular repair was not offset by increased morbidity or mortality in the first 2 y after repair. Long-term outcome data are needed. |
Analysis by ITT. Trial is
ongoing, and report covers October 15, 2002 through October 15, 2008. |
| Aspirin for prevention of CV events in patients with PAD: a meta- analysis of randomized trials (51) |
To investigate the effect of ASA on CV event rates in patients with PAD | Meta-analysis (18 trials involving 5,269 persons were identified) |
N=5,269; 2,823 patients taking ASA (alone or with dipyridamole) and 2,446 in control group |
Inclusion criteria:
1) prospective, RCTs either open-label or blinded; 2) assignment of PAD participants to ASA treatment or placebo or control group; and 3) available data on all- cause mortality, CV death, MI, stroke, and major bleeding |
N/A | CV events (nonfatal MI, nonfatal stroke, and CV death) |
All-cause mortality, major bleeding, and individual components of the 1° outcome measure |
5,000 patient meta-analysis with
~88% power to detect a 25% difference (from 10% to 7.5%) and 70% power to detect a 20% difference (from 10% to 8%) in RR of CV death, MI, or stroke in the ASA group vs. placebo or control groups. Patient characteristics, ASA dosages, and length of follow-up differed across studies, so RR for each study was assumed to have a random offset from the population mean RR (i.e., a random- effects model). The Cochran Q statistic and I2 statistic were calculated by study authors to assess degree of heterogeneity among the trials. |
Effect of any ASA on
prevention of composite CV endpoints, p=0.13. Effect of any ASA on prevention of nonfatal MI, nonfatal stroke, and CV death p=0.81; Nonfatal stroke, p=0.02; CV death, p= 0.59 Effect of any ASA on prevention of any death and major bleeding: Any death, p=0.85 Major bleeding, p=0.98. Effect of ASA monotherapy on prevention of adverse outcomes composite CV endpoints, p=0.21 |
Effect of any ASA on
prevention of composite CV endpoints: RR: 0.88; 95% CI: 0.76 to 1.04 Effect of any ASA on prevention of nonfatal MI, nonfatal stroke, and CV death: Nonfatal MI: RR: 1.04; 95% CI: 0.78 to 1.39 Nonfatal stroke: RR: 0.66; 95% CI: 0.47 to 0.94 CV death: RR: 0.94; 95% CI: 0.74 to 1.19 ASA effect on prevention of any death and major bleeding: Any death RR: 0.98; 95% CI: 0.83 to 1.17 Major bleeding: RR: 0.99; 95% CI: 0.66 to 1.50 Effect of ASA monotherapy on prevention of adverse outcomes: Composite CV endpoints: RR: 0.75; 95% CI: 0.48 to 1.18 Nonfatal stroke: RR: 0.64; 95% CI: 0.42 to 0.99 |
In patients with PAD,
treatment with ASA alone or with dipyridamole resulted in a statistically nonsignificant decrease in the 1° endpoint of CV events and a significant reduction in nonfatal stroke. Results for the 1° endpoint may reflect limited statistical power. Additional RCTs are needed to establish a net benefit and bleeding risks in PAD. |
Outcome measures: 1° outcome was RR reduction of ASA therapy on composite endpoint of nonfatal MI, nonfatal stroke, and CV death in the population of patients who received any ASA therapy (with or without dipyridamole). 2° outcomes were all-cause mortality with each component of the 1° endpoint. The 1° safety outcome evaluated occurrence of major bleeding as defined by each study. ITT analysis used. |
| Aspirin for prevention of CV events in a general population screened for a low ABI: an RCT (47) |
To determine effectiveness of ASA in preventing events in people with a low ABI identified on screening of the general population |
ITT, double-blind RCT |
28,980 men and women 50 to 75 y old |
N/A | N/A | Composite of initial fatal or nonfatal coronary event or stroke or revascularization |
All initial vascular events, defined as a composite of a 1° endpoint event or angina, intermittent claudication, or TIA; and all-cause mortality |
1° endpoint event: 13.5 per
1,000 person-years; 95% CI: 12.2 to 15.0. No statistically significant difference was found between groups (13.7 events per 1,000 person-years in the ASA group vs. 13.3 in the placebo group; HR: 1.03; 95% CI: 0.84 to 1.27). 2° endpoint (vascular event): 22.8 per 1,000 person-years; 95% CI: 21.0 to 24.8, and no statistically significant difference was found between groups (22.8 events per 1,000 person-years in the ASA group vs. 22.9 in the placebo group; HR: 1.00; 95% CI: 0.85 to 1.17). No significant difference in all-cause mortality between groups, 176 vs. 186 deaths, respectively; HR: 0.95; 95% CI: 0.77 to 1.16. An initial event of major hemorrhage requiring admission to hospital occurred in 34 participants (2.5 per 1,000 person- years) in the ASA group and 20 (1.5 per 1,000 person-years) in the placebo group (HR: 1.71; 95% CI: 0.99 to 2.97). |
1° endpoint: No
statistically significant difference was found between groups. HR: 1.03; 95% CI: 0.84 to 1.27 2° endpoint (vascular event): No statistically significant difference between groups, HR: 1.00; 95% CI: 0.85 to 1.17 All-cause mortality: HR: 0.95; 95% CI: 0.77 to 1.16 An initial event of major hemorrhage requiring admission: HR: 1.71; 95% CI: 0.99 to 2.97 |
Among participants
without clinical CV disease, identified with a low ABI based on screening a general population, administration of ASA compared with placebo did not result in a significant reduction in vascular events. |
Interventions: Once-daily 100
mg ASA (enteric coated) or placebo. Statistics: The trial was powered to detect a 25% proportional risk reduction in major vascular events. Predicted risk reduction evidence from 1) event rates in asymptomatic participants with a low ABI were similar to those with symptomatic PAD, suggesting that the risk reduction could be comparable with patients who have clinical disease (~25% to 15%), and 2) in stable angina, unlike ACS with thrombosis complicating atherosclerotic plaque, risk reduction could reach 33%. Study termination: Subsequently, DSMB stopped the trial 14 mo early due to the improbability of finding a difference in the 1° endpoint by the end date and an increase in major bleeding (p= 0.05) in the ASA group. Even though the trial was stopped early, the required number of events was achieved. |
|
| Prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomized placebo-controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic PAD (46) |
To determine whether ASA and antioxidant therapy, combined or alone, are more effective than placebo in reducing development of CV events in patients with diabetes mellitus and asymptomatic PAD |
Multicenter, randomized, double-blind, 2×2 factorial, placebo- controlled trial |
1,276 | Adults of either sex, >40
y old, with type 1 or type 2 diabetes who were determined to have asymptomatic PAD as detected by lower-than- normal ABI (≤0.99). The trial used a higher cut-off point (0.99 vs. 0.9) because it is recognized that calcification in the vessels of people with diabetes can produce a normal or high ABI, even in the presence of arterial disease. |
People with evidence of symptomatic CV disease; those who use ASA or antioxidant therapy on a regular basis; those with peptic ulceration, severe dyspepsia, a bleeding disorder, or intolerance to ASA; those with suspected serious physical illness (such as cancer), which might have been expected to curtail life expectancy; those with psychiatric illness (reported by their general practitioner); those with congenital heart disease; and those unable to give informed consent |
2 hierarchical composite 1° endpoints of death from CAD or stroke, nonfatal MI or stroke, or amputation above the ankle for CLI; and death from CAD or stroke |
N/A | Overall, 116 of 638 1° events
occurred in the ASA groups compared with 117 of 638 in the no-ASA groups (18.2% vs. 18.3%); 43 deaths from CAD or stroke in the ASA groups compared with 35 in the no-ASA groups (6.7% vs. 5.5%). Among the antioxidant groups, 117 of 640 (18.3%) 1° events occurred compared with 116 of 636 (18.2%) in the no-antioxidant groups. There were 42 deaths (6.6%) from CAD or stroke in the antioxidant groups compared with 36 deaths (5.7%) in the no-antioxidant groups. |
Comparison of ASA and
no-ASA groups—Composite endpoint: p=0.86 Death from CAD or stroke: p=0.36 Comparison of antioxidant and no-antioxidant groups—Composite endpoint: p= 0.85 Death from CAD or stroke: p= 0.40 |
ASA groups 1° events:
HR: 0.98; 95% CI: 0.76 to 1.26 ASA groups deaths from CAD or stroke HR: 1.23 (0.79 to 1.93) Antioxidant groups 1° events: HR: 1.03; 95% CI: 0.79 to 1.33 Antioxidant groups deaths from CAD or stroke: HR: 1.21; 95% CI: 0.78 to 1.89 |
This trial does not
provide evidence to support the use of ASA or antioxidants in primary prevention of CV events and mortality in the population with diabetes studied. |
Power: 1,276 patients
were recruited, and final power calculations, undertaken in 2003, projected that if follow-up continued until June 2006, then 256 events would be expected to occur during the trial. This would give 73% power to detect a 25% relative reduction in event rate and 89% power to detect a 30% reduction in event rate if only 1 treatment was effective. Interventions were daily ASA 100 mg or placebo tablet, plus antioxidant or placebo capsule. The antioxidant capsule contained α-tocopherol 200 mg, ascorbic acid 100 mg, pyridoxine hydrochloride 25 mg, zinc sulphate 10 mg, nicotinamide 10 mg, lecithin 9.4 mg, and sodium selenite 0.8 mg. |
| Endovascular vs. open repair of AAA: the United Kingdom EVAR Trial Investigators (56) |
To investigate the long-term outcome of endovascular repair of AAA compared with open repair |
Randomized trial | 1,252 | N/A (published in
previous reports) (61) |
N/A (published in previous reports) (61) | Death from any cause. Also assessed: aneurysm- related death, graft-related complications, and graft-related reinterventions |
N/A | 30-d operative mortality was 1.8%
in the endovascular repair group and 4.3% in the open-repair group. |
30-d operative mortality
(for endovascular repair compared with open repair): p= 0.02 Aneurysm-related mortality: p=0.73 Rate of death from any cause: p=0.72 |
30-d operative mortality
(for endovascular repair compared with open repair): adjusted OR: 0.39; 95% CI: 0.18 to 0.87 Aneurysm-related mortality: adjusted HR: 0.92; 95% CI: 0.57 to 1.49 Rate of death from any cause: adjusted HR: 1.03; 95% CI: 0.86 to 1.23 |
Endovascular repair of AAA
was associated with a significantly lower operative mortality than open surgical repair. However, no differences were seen in total mortality or aneurysm-related mortality in the long term. Endovascular repair was associated with increased rates of graft-related complications and reinterventions and was more costly. |
Rates of
graft-related complications and reinterventions were higher with endovascular repair, and new complications occurred up to 8 y after randomization, contributing to higher overall costs. Per-protocol analysis yielded results very similar to those of ITT analysis. |
| Endovascular repair of aortic aneurysm in patients physically ineligible for open repair: the United Kingdom EVAR Trial Investigators (59) |
To investigate
whether endovascular repair reduces the rate of death among patients who were considered physically ineligible for open surgical repair |
Randomized trial | 404 | N/A (see original study [61]) | N/A (see original study [61]) | Death from any cause. Also assessed: aneurysm- related death, graft-related complications, and graft-related reinterventions |
N/A | 30-d operative mortality was 7.3%
in the endovascular repair group. The overall rate of aneurysm rupture in the no-intervention group was 12.4 (95% CI: 9.6 to 16.2) per 100 person-years. A total of 48% of patients who survived endovascular repair had graft-related complications, and 27% required reintervention within the first 6 y. |
Aneurysm-related
mortality: p=0.02 Total mortality: p=0.97 |
Aneurysm-related mortality
was lower in the endovascular repair group. Adjusted HR: 0.53; 95% CI: 0.32 to 0.89. Total mortality: adjusted HR: 0.99; 95% CI: 0.78 to 1.27 |
This RCT involved patients
who were physically ineligible for open repair; endovascular repair of AAA was associated with a significantly lower rate of aneurysm-related mortality than no repair. However, endovascular repair was not associated with reduction in the rate of death from any cause. Rates of graft- related complications and reinterventions were higher with endovascular repair, and it was more costly. |
During 8 y of
follow-up, endovascular repair was considerably more expensive than no repair (cost difference, £9,826 [US $14,867]; 95% CI: £7,638 to £12,013 [$11,556 to $18,176]). |
| BASIL (54) | An ITT analysis of AFS and OS in patients randomized to a BSX- first or a BAP-first revascularization strategy |
Randomized trial | 452 | BASIL trial methods have
been published in detail elsewhere (55). |
BASIL trial methods have been published in detail elsewhere (55). |
1°
aim: determine whether a BSX- first or a BAP- first revascularization strategy was associated with better clinical outcome for patients. Defined better as improved AFS; used this as 1° endpoint for power calculation and prespecified statistical plan design. |
2° outcomes
included postprocedural morbidity, reinterventions, HRQOL, and use of hospital resources. |
For those patients who survived for 2
y after randomization: initial randomization to a BSX-first revascularization strategy was associated with an increase in subsequent restricted mean overall survival of 7.3 mo (95% CI: 1.2 to 13.4 mo) and an increase in restricted mean AFS of 5.9 mo (95% CI: 0.2 to 12.0 mo) during the subsequent mean follow-up of 3.1 y (range: 1 to 5.7 y). |
For those patients surviving 2
y from randomization: BSX-first revascularization was associated with subsequent AFS of p= 0.108 and subsequent OS of p=0.009. For those patients who survived for 2 y after randomization: initial randomization to a BSX- first revascularization strategy was associated with an increase in subsequent restricted mean overall survival, p=0.02, and an increase in restricted mean AFS, p= 0.06. |
For those patients surviving 2
y from randomization: BSX-first revascularization was associated with reduced HR for subsequent AFS of 0.85 (95% CI: 0.5 to 1.07) in an adjusted, time- dependent Cox proportional hazards model and subsequent OS of 0.61 (95% CI: 0.50 to 0.75) in an adjusted, time- dependent Cox proportional hazards model. |
Overall there was no
significant difference in AFS or OS between the 2 strategies. However, for those patients who survived for ≥2 y after randomization, a BSX- first revascularization strategy was associated with a significant increase in subsequent OS and a trend toward improved AFS. |
The sample size
calculations proposed that 223 patients per treatment would be needed for 90% power to detect a 15% difference in 3-y AFS at the 5% significance level. This calculation was based on the assumption that the 3-y survival value might be 50% in 1 group and 65% in the others). |
| Statins are
independently associated with reduced mortality in patients undergoing IBG surgery for CLI (PREVENT III) (62) |
To determine efficacy of edifoligide for prevention of graft failure |
Multicenter, randomized, prospective trial |
1,404 patients with CLI |
Patients ≥18 y old
who underwent IBG with autogenous vein for CLI, defined as gangrene, nonhealing ischemic ulcer, or ischemic rest pain. See primary trial report for further information (63). |
Claudication as an indication for IBG surgery or use of a nonautogenous conduit. See primary trial report for further information (63). |
Major adverse CV events <30 d, vein graft patency, and 1-y survival assessed by Kaplan-Meier method |
N/A | Patient treatment breakdown:
636 patients (45%) were taking statins, 835 (59%) were taking beta blockers, and 1,121 (80%) were taking antiplatelet drugs. Perioperative major adverse CV events (7.8%) and early mortality(2.7%) were not measurably affected by use of any drug class. Use of beta blockers and antiplatelet drugs had no appreciable impact on survival. None of the drug classes were associated with graft patency measures at 1 y. Statin use was associated with a significant survival advantage at 1 y of 86% vs. 81% by analysis of both unweighted and propensity score-weighted data. |
Statin use associated
with significant survival advantage at 1y:p=0.03 Significant predictors of 1-y mortality by Cox regression modeling were: Statin use p=0.001 Age >75 y, p=0.001 CAD, p= 0.001 CKD stage 4, p=0.001 CKD stage 5, p<0.001 Tissue loss, p=0.003 |
Statin use associated with
a significant survival advantage at 1 y: HR: 0.71; 95% CI: 0.52 to 0.98 Significant predictors of 1-y mortality by Cox regression modeling were: Statin use HR: 0.67; 95% CI: 0.51 to 0.90 Age >75 yHR: 2.1; 95% CI: 1.60 to 2.82 CAD HR: 1.5; 95% CI: 1.15 to 2.01 CKD stage 4 HR: 2.0; 95% CI: 1.17 to 3.55 CKD stage 5 HR: 3.4; 95% CI: 2.39 to 4.73 Tissue loss HR: 1.9; 95% CI: 1.23 to 2.80 |
Statin use was associated
with improved survival in CLI patients 1 y after surgical revascularization. Further studies are indicated to determine optimal dosing in this population and to definitively address the question of relationship to graft patency. These data add to the growing literature supporting statin use in patients with advanced PAD. |
Propensity scores used
to evaluate the influence of statins, beta blockers, and antiplatelet agents on outcomes while adjusting for demographics, comorbidities, medications, and surgical variables that may influence drug use. |
| Mortality and
vascular morbidity in older adults with asymptomatic vs. symptomatic PAD (getABI) (11) |
To assess risk of mortality and vascular morbidity in elderly persons with asymptomatic vs. symptomatic PAD in the primary care setting |
Prospective cohort study |
6880 representative unselected patients 65 y of age: 5,392 patients had no PAD, 836 had asymptomatic PAD (ABI: 0.9 without symptoms), and 593 had symptomatic PAD (lower extremity peripheral revascularization, amputation as a result of PAD, or intermittent claudication symptoms regardless of ABI) |
Age 65 y, legally
competent, and able to cooperate appropriately and provide written informed consent (64) |
Life expectancy of 6 mo as judged by the general practitioner (64) |
1°
outcomes and identification of CV events during follow- up: severe vascular events were defined as follows: CV, including MI or coronary revascularization; cerebrovascular, including stroke or carotid revascularization; and lower extremity peripheral vascular, including peripheral revascularization or amputation because of PAD during follow-up. |
N/A | Lower ABI categories were
associated with increased risk. PAD was a strong factor for prediction of the composite endpoint in an adjusted model. |
Risk of symptomatic
compared with asymptomatic PAD patients: Composite of all-cause death or severe vascular event HR: 1.48; 95% CI: 1.21 to 1.80 All-cause death alone HR: 0.13, 95% CI: 0.89 to 1.43 All-cause death/MI/stroke (excluding lower extremity peripheral vascular events and any revascularizations) HR: 1.18; 95% CI: 0.92 to 1.52 CV events alone HR: 1.20; 95% CI: 0.89 to 1.60 Cerebrovascular events alone HR: 1.33; 95% CI: 0.80 to 2.20 |
Asymptomatic PAD
diagnosed through routine screening in offices of PCPs has a high and/or vascular event risk. Notably, risk of mortality was similar in symptomatic and asymptomatic patients with PAD and was significantly higher than in those without PAD. In the primary care setting, the diagnosis of PAD has important prognostic value. |
Incidence rates and 95%
CIs were calculated as events per 1,000 person-years. The composite endpoint of all-cause mortality or severe vascular events occurred in 27.2 (no PAD), 60.4 (asymptomatic PAD), and 104.7 (symptomatic PAD) cases per 1,000 patient-years. In analysis by ABI category, patients with an ABI of 1.1 to 1.5 had the lowest event rate per 1,000 patient-years (24.3 events), whereas event rates increased substantially with decreasing ABI. In patients with an ABI of 0.5, lower extremity peripheral revascularization, or amputation resulting from PAD, event rates were increased 6- fold (146.3), and the corresponding adjusted risk was increased 4.65-fold (95% CI: 3.57 to 6.05). |
|
| Effectiveness of a
smoking cessation program for PAD patients (65) |
To test the effectiveness of a smoking cessation program designed for patients with PAD |
RCT | 124 | Diagnosis of lower
extremity PAD, defined as at least 1 of the following: ABI <0.90 in at least 1 lower extremity; toe brachial index <0.60; objective evidence of arterial occlusive disease in 1 lower extremity by duplex ultrasound, MRA, or CTA; prior leg arterial revascularization or amputation due to PAD, and current smoking (defined as smoking at least 1 cigarette/ d, at least 6 d/wk). Additional inclusion criteria: desire to quit smoking in the next 30 d, age >18 y, ability to speak and write English, no participation in a smoking cessation program in the past 30 d, and consumption of < 21 alcoholic drinks per wk. |
N/A | Tobacco use 7-d point prevalence of smoking (i.e., “Have you smoked a cigarette, even a puff, in the past 7 d?”), at the 3- and 6- mo follow-ups |
N/A | Participants randomized to the
intensive intervention group were significantly more likely to be confirmed abstinent at 6-mo follow-up: 21.3% vs. 6.8% in the minimal intervention group: chi- squared=5.21. |
Members of the
intensive intervention group were significantly more likely to be confirmed abstinent at 6-mo follow-up: p=0.023. |
N/A | Many long-term smokers with PAD are willing to initiate a serious quit attempt and to engage in an intensive smoking cessation program. Intensive intervention for tobacco dependence is a more effective smoking cessation intervention than minimal care. Studies should be conducted to examine the long-term effectiveness of intensive smoking cessation programs in this population in order to examine the effect of this intervention on clinical outcomes related to PAD. |
|
| Prevention of serious vascular events by aspirin among patients with PAD: randomized, double-blind trial: CLIPS Group (45) |
To assess the prophylactic efficacy of ASA and a high- dose antioxidant vitamin combination in patients with PAD in terms of reduction of risk of a first vascular event (MI, stroke, vascular death) and CLI |
RCT, double-blind clinical trial with 2X2 factorial design |
366 outpatients with stage I to II PAD documented by angiography or ultrasound, with ABI <0.85 or toe index <0.6 |
Study involved outpatients with symptomatic (claudicant) or asymptomatic PAD documented by angiography or ultrasound, who had 1 ABI <0.85 or 1 toe index <0.6. Patients were referred either by the GP or ER physician for a diagnostic workup. Diabetic persons could be included, provided metabolic control was stable (HbA1c). Only patients who accepted randomization (i.e., continuation after run-in period) were included in the study. |
Exclusion criteria: Fontaine stage III or IV PVD; life expectancy <24 mo; vascular surgery or angioplasty in the last 3 mo; pregnancy or lactation; contraindication to ASA; major CV events requiring antiplatelet therapy; participation in another clinical trial; uncooperative patients; treatment with drugs that interfere with hemostasis, such as anticoagulants, antiplatelet agents, and prostanoids, peripheral vasodilators, ASA and/or supplementary vitamins that could not be discontinued or had to be introduced |
Major vascular events: CV death, MI, or stroke and CLI |
N/A | 7 of 185 patients who were allocated
to ASA and 20 of 181 patients who were allocated to placebo suffered a major vascular event (risk reduction 64%). 5 and 8 patients, respectively, suffered CLI (total 12 vs. 28). There was no evidence that antioxidant vitamins were beneficial (16/185 vs. 11/181 vascular events). Neither treatment was associated with any significant increase in adverse events. |
Major vascular event:
p=0.022; CLI: p=0.014 |
N/A | For the first time direct
evidence shows that low-dose ASA should routinely be considered for patients with PAD, including those with concomitant type 2 diabetes. |
The safety endpoint
was incidence of bleeding. Inclusion of this trial in a meta-analysis of other RCTs of antiplatelet therapy in PAD makes the overall results highly significant (p<0.001) and suggests that low-dose ASA reduces the incidence of vascular events by 26%. |
| Patients with PAD in
the CHARISMA trial (49) |
To determine
whether clopidogrel plus ASA provides greater protection against major CV events than ASA alone in patients with PAD |
Prospective, multicenter, randomized, double-blind, placebo-controlled study |
3,096 patients with symptomatic (2,838) or asymptomatic (258) PAD |
To fulfill the symptomatic PAD inclusion criterion, patients had to have either current intermittent claudication together with an ABI of 0.85 or a history of intermittent claudication together with a previous related intervention (amputation, surgical or catheter-based peripheral revascularization). Asymptomatic patients with an ABI of 0.90 were identified among those with multiple risk factors. |
The details of the trial design have been published previously (66) |
1° efficacy endpoint: first occurrence of MI, stroke (of any cause), or death from CV causes (including hemorrhage). 1° safety endpoint: severe bleeding according to the GUSTO definition |
Principal 2°
efficacy endpoints: first occurrence of MI, stroke, death from CV causes, hospitalization for UA, TIA, or a revascularization procedure (coronary, cerebral, or peripheral) |
Post hoc analysis of the 3,096
patients with symptomatic (2,838) or asymptomatic (258) PAD from the CHARISMA trial. CV death, MI, or stroke rates (1° endpoint) were higher in PAD patients than in those without PAD: 8.2% vs. 6.8%. Severe, fatal, or moderate bleeding rates did not differ between groups, whereas minor bleeding was increased with clopidogrel: 34.4% vs. 20.8%. Among patients with PAD: The 1° endpoint occurred in 7.6% in the clopidogrel plus ASA group and 8.9% in the placebo plus ASA group. The rate of MI was lower in the dual antiplatelet arm than the ASA-alone arm: 2.3% vs. 3.7%. The rate of hospitalization for ischemic events: 16.5% vs. 20.1%. |
Rates of minor bleeding:
OR: 1.99; 95% CI: 1.69 to 2.34. Among the patients with PAD: 1° endpoint: HR: 0.85; 95% CI: 0.66 to 1.08 Rate of MI: HR: 0.63; 95% CI: 0.42 to 0.96 Rate of hospitalization: HR: 0.81; 95% CI: 0.68 to 0.95 Rate of hospitalization for ischemic events: HR: 0.81; 95% CI: 0.68 to 0.95 |
Dual therapy provided
some benefit over ASA alone in PAD patients for the rate of MI and the rate of hospitalization for ischemic events, at cost of an increase in minor bleeding. |
N/A | |
| CHARISMA (48) | To view dual antiplatelet therapy with clopidogrel plus low-dose ASA in a broad population of patients at high risk for atherothrombotic events |
Prospective, multicenter, randomized, double-blind, placebo-controlled study |
15,603 | See study for the
inclusion criteria for those with multiple risk factors and those with established vascular disease. |
Patients were excluded from the trial if they were taking oral antithrombotic medications or NSAIDs on a long-term basis (although COX-2 inhibitors were permitted). Patients were also excluded if, in the judgment of the investigator, they had established indications for clopidogrel therapy (such as recent ACS). Patients who were scheduled to undergo revascularization were not allowed to enroll until the procedure had been completed; such patients were excluded if they were considered to require clopidogrel after revascularization. |
1°
efficacy endpoint: composite of MI, stroke, or death from CV causes. 1° safety endpoint: severe bleeding, according to the GUSTO definition |
Principal 2°
efficacy endpoint: first occurrence of MI, stroke, death from CV causes, or hospitalization for UA, TIA, or a revascularization procedure (coronary, cerebral, or peripheral) |
1° efficacy rate endpoint: 6.8%
with clopidogrel plus ASA and 7.3% with placebo plus ASA. Principal 2° efficacy rate endpoint, including hospitalizations for ischemic events, was 16.7% and 17.9%. Principal 2° efficacy endpoint, including the rate of severe bleeding, 1.7% and 1.3%. 1° endpoint rate among patients with multiple risk factors was 6.6% with clopidogrel and 5.5% with placebo. The rate of death from CV causes also was higher with clopidogrel (3.9% vs. 2.2%). In the subgroup with clinically evident atherothrombosis, the rate was 6.9% with clopidogrel and 7.9% with placebo. |
1° endpoint rate among
patients with multiple risk factors: p=0.20 1° endpoint rate in the subgroup with clinically evident atherothrombosis: p=0.046 Rate of death from CV causes: p=0.01 1° efficacy endpoint rate: p= 0.22 Principal 2° efficacy rate endpoint, including rate of severe bleeding: p= 0.09 Principal 2° efficacy rate endpoint, including hospitalizations for ischemic events: p= 0.04 |
1° efficacy endpoint rate:
RR 0.93; 95% CI: 0.83 to 1.05 1° endpoint rate in subgroup with clinically evident atherothrombosis: RR: 0.88; 95% CI: 0.77 to 0.998 1° endpoint rate among patients with multiple risk factors: RR: 1.2; 95% CI: 0.91 to 1.59 Principal 2° efficacy endpoint, including the rate of severe bleeding: RR: 1.25, 95% CI: 0.97 to 1.61. Principal 2° efficacy rate endpoint, including hospitalizations for ischemic events: RR: 0.92; 95% CI: 0.86 to 0.995 |
There was a suggestion of
benefit with clopidogrel treatment in patients with symptomatic atherothrombosis and a suggestion of harm in patients with multiple risk factors. Overall, clopidogrel plus ASA was not significantly more effective than ASA alone in reducing rate of MI, stroke, or death from CV causes. |
Other efficacy endpoints
included death from any cause and death from CV causes, as well as MI, ischemic stroke, any stroke, and hospitalization for UA, TIA, or revascularization considered separately. |
| Oral anticoagulant
and antiplatelet therapy and PAD: the WAVE trial Investigators (50) |
To view the role of oral anticoagulants in prevention of CV complications in patients with PAD |
Randomized, open-label, clinical trial |
2,161 patients | Men and women who were 35 to 85 y old and had PAD |
Patients who had an indication for oral anticoagulant treatment, were actively bleeding or at high risk for bleeding, had had a stroke within 6 mo before enrollment, or required dialysis |
First coprimary outcome: MI, stroke, or death from CV causes. Second coprimary outcome: MI, stroke, severe ischemia of the peripheral or coronary arteries leading to urgent intervention, or death from CV causes |
N/A | MI, stroke, or death from CV
causes occurred in 132 of 1,080 patients receiving combination therapy (12.2%) and in 144 of 1,081 patients receiving antiplatelet therapy alone (13.3%). MI, stroke, severe ischemia, or death from CV causes occurred in 172 patients receiving combination therapy (15.9%) compared with 188 patients receiving antiplatelet therapy alone (17.4%). Life- threatening bleeding occurred in 43 patients receiving combination therapy (4.0%) compared with 13 patients receiving antiplatelet therapy alone (1.2%). |
MI, stroke, or death from
CV causes: p=0.48 MI, stroke, severe ischemia, or death from CV causes: p=0.37 Life-threatening bleeding: p<0.001 |
MI, stroke, or death from
CV causes: RR: 0.92; 95% CI: 0.73 to 1.16 MI, stroke, severe ischemia, or death from CV causes: RR: 0.91; 95% CI: 0.74 to 1.12 Life-threatening bleeding: RR: 3.41; 95% CI: 1.84 to 6.35 |
The combination of an
oral anticoagulant and antiplatelet therapy was no more effective than antiplatelet therapy alone in preventing major CV complications and was associated with an increase in life- threatening bleeding. |
Safety outcomes were
life- threatening, moderate, or minor bleeding episodes |
AAA indicates Abdominal Aortic and Iliac Aneurysms; ABI, ankle brachial index; ACS, acute coronary syndrome; AFS, amputation-free survival; ASA, aspirin; ASTRAL, Angioplasty and Stent for Renal Artery Lesions trial; BAP, balloon angioplasty; BASIL, Bypass versus Angioplasty in Severe Ischaemia of the Leg trial; BSX-first, bypass surgery; CAD, coronary artery disease; CHARISMA, Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance; CI, confidence interval; CKD, chronic kidney disease; CLI, critical limb ischemia; CLIPS, Critical Leg Ischemia Prevention Study; COX-2, cyclooxygenase; CTA, computed tomographic angiography; CV, cardiovascular; DSMB, data safety monitoring board; Embase, Excerpta Medica Database; ER, emergency room; EVAR, endovascular aneurysm repair; FRS, Framingham Risk Score; GP, general practitioner; GUSTO, Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries; HbA1c, hemoglobin A1c; HR; hazard ratio; HRQOL, health-related quality of life; IBG, infrainguinal bypass graft; ICU, intensive care unit; ITT, intention-to-treat; MEDLINE, Medical Literature Analysis and Retrieval System Online; MI, myocardial infarction; N/A, not available; NSAIDs, nonsteroidal anti-inflammatory drugs; OR, odds radio; OS, overall survival; MRA, magnetic resonance angiography; PAD, peripheral artery disease; PCP, primary care physician; POPADAD, prevention of progression of arterial disease and diabetes; PREVENT III, The Project of Ex-Vivo Vein Graft Engineering via Transfection III; PVD, peripheral vascular disease; RAS, renal artery stenosis; RCT, randomized controlled trial; RR, relative risk; SLI, severe leg ischemia; TIA, transient ischemic attack; UA, unstable angina; VA, Department of Veterans Affairs; WAVE, Warfarin Antiplatelet Vascular Evaluation trial; 1°, primary; and 2°, secondary.
Footnotes
2011 WRITING GROUP MEMBERS*
Thom W. Rooke, MD, FACC, Chair†; Alan T. Hirsch, MD, FACC, Vice Chair*; Sanjay Misra, MD, Vice Chair*‡; Anton N. Sidawy, MD, MPH, FACS, Vice Chair§; Joshua A. Beckman, MD, FACC, FAHA*∥; Laura K. Findeiss, MD‡; Jafar Golzarian, MD†; Heather L. Gornik, MD, FACC, FAHA*†; Jonathan L. Halperin, MD, FACC, FAHA*¶; Michael R. Jaff, DO, FACC*†; Gregory L. Moneta, MD, FACS†; Jeffrey W. Olin, DO, FACC, FAHA*#; James C. Stanley, MD, FACS†; Christopher J. White, MD, FACC, FAHA, FSCAI***; John V. White, MD, FACS†; R. Eugene Zierler, MD, FACS†
2005 WRITING COMMITTEE MEMBERS
Alan T. Hirsch, MD, FACC, Chair; Ziv J. Haskal, MD, FAHA, FSIR, Co-Chair; Norman R. Hertzer, MD, FACS, Co-Chair; Curtis W. Bakal, MD, MPH, FAHA; Mark A. Creager, MD, FACC, FAHA; Jonathan L. Halperin, MD, FACC, FAHA§; Loren F. Hiratzka, MD, FACC, FAHA, FACS; William R. C. Murphy, MD, FACC, FACS; Jeffrey W. Olin, DO, FACC; Jules B. Puschett, MD, FAHA; Kenneth A. Rosenfield, MD, FACC; David Sacks, MD, FSIR‡; James C. Stanley, MD, FACS§; Lloyd M. Taylor, Jr, MD, FACS§; Christopher J. White, MD, FACC, FAHA, FSCAI**; John V. White, MD, FACS§; Rodney A. White, MD, FACS§
ACCF/AHA TASK FORCE MEMBERS
Alice K. Jacobs, MD, FACC, FAHA, Chair; Jeffrey L. Anderson, MD, FACC, FAHA, Chair-Elect; Nancy Albert, PhD, CCNS, CCRN, FAHA; Mark A. Creager, MD, FACC, FAHA; Steven M. Ettinger, MD, FACC; Robert A. Guyton, MD, FACC; Jonathan L. Halperin, MD, FACC, FAHA; Judith S. Hochman, MD, FACC, FAHA; Frederick G. Kushner, MD, FACC, FAHA; E. Magnus Ohman, MD, FACC; William Stevenson, MD, FACC, FAHA; Clyde W. Yancy, MD, FACC, FAHA
Writing group members are required to recuse themselves from voting on sections to which their specific relationships with industry and other entities may apply; see Appendix 1 for recusal information. † ACCF/AHA Representative. ‡ Society of Interventional Radiology Representative. § Society for Vascular Surgery Representative. ∥ Society for Vascular Medicine Representative. ¶ ACCF/AHA Task Force on Practice Guidelines Liaison. # ACCF/AHA Task Force on Performance Measures Liaison. ** Society for Cardiovascular Angiography and Interventions Representative.
This document was approved by the American College of Cardiology Foundation Board of Trustees and the American Heart Association Science Advisory and Coordinating Committee in July 2011.
The American College of Cardiology requests that this document be cited as follows: Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK, Golzarian J, Gornik HL, Halperin JL, Jaff MR, Moneta GL, Olin JW, Stanley JC, White CJ, White JV, Zierler RE. 2011 ACCF/AHA focused update of the guideline for the management of patients with peripheral artery disease (updating the 2005 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2011;58:2020–45.
This article is copublished in Circulation, Catheterization and Cardiovascular Interventions, the Journal of Vascular Surgery, and Vascular Medicine.
Copies: This document is available on the World Wide Web sites of the American College of Cardiology (www.cardiosource.org) and the American Heart Association (my.americanheart.org). For copies of this document, please contact Elsevier Inc. Reprint Department, fax (212) 633-3820, reprints@elsevier.com.
Staff
American College of Cardiology Foundation
David R. Holmes, Jr., MD, FACC, President
John C. Lewin, MD, Chief Executive Officer
Janet Wright, MD, FACC, Senior Vice President, Science and Quality
Charlene May, Senior Director, Science and Clinical Policy
American College of Cardiology Foundation/American Heart Association
Lisa Bradfield, CAE, Director, Science and Clinical Policy Debjani Mukherjee, MPH, Associate Director, Evidence-Based Medicine
Maria Koinis, Specialist, Science and Clinical Policy
American Heart Association
Ralph L. Sacco, MS, MD, FAAN, FAHA, President
Nancy Brown, Chief Executive Officer
Rose Marie Robertson, MD, FAHA, Chief Science Officer
Gayle R. Whitman, PhD, RN, FAHA, FAAN, Senior Vice President, Office of Science Operations
Nereida A. Parks, MPH, Science and Medicine Advisor, Office of Science Operations
Jody Hundley, Production Manager, Scientific Publications, Office of Science Operations
References
- 1.ACCF/AHA Task Force on Practice Guidelines. [July 1, 2011];Methodologies and Policies from the ACCF/AHA Task Force on Practice Guideline. Available at http://assets.cardiosource.com/Methodology_Manual_for_ACC_AHA_Writing_Committees.pdf and http://circ.ahajournals.org/site/manual/index.xhtml.
- 2.Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary: a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) J Am Coll Cardiol. 2006;47:1239–312. doi: 10.1016/j.jacc.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Norgren L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) Eur J Vasc Endovasc Surg. 2007;33(Suppl 1):S1–75. doi: 10.1016/j.ejvs.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 4.Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) J Am Coll Cardiol. 2006;47:e1–192. [Google Scholar]
- 5.Wheatley K, Ives N, Gray R, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med. 2009;361:1953–62. doi: 10.1056/NEJMoa0905368. [DOI] [PubMed] [Google Scholar]
- 6.Cooper CJ, Murphy TP, Matsumoto A, et al. Stent revascularization for the prevention of cardiovascular and renal events among patients with renal artery stenosis and systolic hypertension: rationale and design of the CORAL trial. Am Heart J. 2006;152:59–66. doi: 10.1016/j.ahj.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 7.Alhadad A, Mattiasson I, Ivancev K, et al. Revascularisation of renal artery stenosis caused by fibromuscular dysplasia: effects on blood pressure during 7-year follow-up are influenced by duration of hypertension and branch artery stenosis. J Hum Hypertens. 2005;19:761–7. doi: 10.1038/sj.jhh.1001893. [DOI] [PubMed] [Google Scholar]
- 8.Modrall JG, Rosero EB, Smith ST, et al. Operative mortality for renal artery bypass in the United States: results from the National Inpatient Sample. J Vasc Surg. 2008;48:317–22. doi: 10.1016/j.jvs.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 9.Criqui MH, Denenberg JO, Bird CE, et al. The correlation between symptoms and non-invasive test results in patients referred for peripheral arterial disease testing. Vasc Med. 1996;1:65–71. doi: 10.1177/1358863X9600100112. [DOI] [PubMed] [Google Scholar]
- 10.Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286:1317–24. doi: 10.1001/jama.286.11.1317. [DOI] [PubMed] [Google Scholar]
- 11.Diehm C, Allenberg JR, Pittrow D, et al. Mortality and vascular morbidity in older adults with asymptomatic versus symptomatic peripheral artery disease. Circulation. 2009;120:2053–61. doi: 10.1161/CIRCULATIONAHA.109.865600. [DOI] [PubMed] [Google Scholar]
- 12.Fowkes FG. The measurement of atherosclerotic peripheral arterial disease in epidemiological surveys. Int J Epidemiol. 1988;17:248–54. doi: 10.1093/ije/17.2.248. [DOI] [PubMed] [Google Scholar]
- 13.Feigelson HS, Criqui MH, Fronek A, et al. Screening for peripheral arterial disease: the sensitivity, specificity, and predictive value of noninvasive tests in a defined population. Am J Epidemiol. 1994;140:526–34. doi: 10.1093/oxfordjournals.aje.a117279. [DOI] [PubMed] [Google Scholar]
- 14.Nassoura ZE, Ivatury RR, Simon RJ, et al. A reassessment of Doppler pressure indices in the detection of arterial lesions in proximity penetrating injuries of extremities: a prospective study. Am J Emerg Med. 1996;14:151–6. doi: 10.1016/S0735-6757(96)90122-9. [DOI] [PubMed] [Google Scholar]
- 15.Carter SA. Clinical measurement of systolic pressures in limbs with arterial occlusive disease. JAMA. 1969;207:1869–74. [PubMed] [Google Scholar]
- 16.Carter SA, Tate RB. Value of toe pulse waves in addition to systolic pressures in the assessment of the severity of peripheral arterial disease and critical limb ischemia. J Vasc Surg. 1996;24:258–65. doi: 10.1016/s0741-5214(96)70101-5. [DOI] [PubMed] [Google Scholar]
- 17.Carter SA, Tate RB. The value of toe pulse waves in determination of risks for limb amputation and death in patients with peripheral arterial disease and skin ulcers or gangrene. J Vasc Surg. 2001;33:708–14. doi: 10.1067/mva.2001.112329. [DOI] [PubMed] [Google Scholar]
- 18.Brooks B, Dean R, Patel S, et al. TBI or not TBI: that is the question: is it better to measure toe pressure than ankle pressure in diabetic patients? Diabet Med. 2001;18:528–32. doi: 10.1046/j.1464-5491.2001.00493.x. [DOI] [PubMed] [Google Scholar]
- 19.Ramsey DE, Manke DA, Sumner DS. Toe blood pressure: a valuable adjunct to ankle pressure measurement for assessing peripheral arterial disease. J Cardiovasc Surg (Torino) 1983;24:43–8. [PubMed] [Google Scholar]
- 20.Belcaro G, Nicolaides AN, Bull ML, et al. The value of segmental pressure measurement in the assessment of peripheral vascular disease. Int Angiol. 1986;5:7–12. [PubMed] [Google Scholar]
- 21.Gundersen J. Segmental measurements of systolic blood pressure in the extremities including the thumb and the great toe. Acta Chir Scand Suppl. 1972;426:1–90. [PubMed] [Google Scholar]
- 22.Johnston KW, Hosang MY, Andrews DF. Reproducibility of noninvasive vascular laboratory measurements of the peripheral circulation. J Vasc Surg. 1987;6:147–51. doi: 10.1067/mva.1987.avs0060147. [DOI] [PubMed] [Google Scholar]
- 23.Kupinski A. Segmental pressure measurement and plethysmography. J Vasc Technol. 2002;1:32–8. [Google Scholar]
- 24.Fowkes FG, Murray GD, Butcher I, et al. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA. 2008;300:197–208. doi: 10.1001/jama.300.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nides MA, Rakos RF, Gonzales D, et al. Predictors of initial smoking cessation and relapse through the first 2 years of the Lung Health Study. J Consult Clin Psychol. 1995;63:60–9. doi: 10.1037//0022-006x.63.1.60. [DOI] [PubMed] [Google Scholar]
- 26.Mohiuddin SM, Mooss AN, Hunter CB, et al. Intensive smoking cessation intervention reduces mortality in high-risk smokers with cardiovascular disease. Chest. 2007;131:446–52. doi: 10.1378/chest.06-1587. [DOI] [PubMed] [Google Scholar]
- 27.Lancaster T, Stead LF. Mecamylamine (a nicotine antagonist) for smoking cessation. Cochrane Database Syst Rev. 2000:CD001009. doi: 10.1002/14651858.CD001009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rothemich SF, Woolf SH, Johnson RE, et al. Effect on cessation counseling of documenting smoking status as a routine vital sign: an ACORN study. Ann Fam Med. 2008;6:60–8. doi: 10.1370/afm.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hennrikus D, Joseph A, Lando H, et al. Effectiveness of a smoking cessation program for peripheral artery disease patients: a randomized controlled trial. J Am Coll Cardiol. 2010;25:2105–12. doi: 10.1016/j.jacc.2010.07.031. [DOI] [PubMed] [Google Scholar]
- 30.Gonzales D, Rennard SI, Nides M, et al. Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs sustained-release bupropion and placebo for smoking cessation: a randomized controlled trial. JAMA. 2006;296:47–55. doi: 10.1001/jama.296.1.47. [DOI] [PubMed] [Google Scholar]
- 31.Jorenby DE, Hays JT, Rigotti NA, et al. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA. 2006;296:56–63. doi: 10.1001/jama.296.1.56. [DOI] [PubMed] [Google Scholar]
- 32.Nides M, Oncken C, Gonzales D, et al. Smoking cessation with varenicline, a selective alpha4beta2 nicotinic receptor partial agonist: results from a 7-week, randomized, placebo- and bupropion-controlled trial with 1-year follow-up. Arch Intern Med. 2006;166:1561–8. doi: 10.1001/archinte.166.15.1561. [DOI] [PubMed] [Google Scholar]
- 33.Jorenby DE, Leischow SJ, Nides MA, et al. A controlled trial of sustained-release bupropion, a nicotine patch, or both for smoking cessation. N Engl J Med. 1999;340:685–91. doi: 10.1056/NEJM199903043400903. [DOI] [PubMed] [Google Scholar]
- 34.Faulkner KW, House AK, Castleden WM. The effect of cessation of smoking on the accumulative survival rates of patients with symptomatic peripheral vascular disease. Med J Aust. 1983;1:217–9. doi: 10.5694/j.1326-5377.1983.tb99395.x. [DOI] [PubMed] [Google Scholar]
- 35.Jonason T, Bergstrom R. Cessation of smoking in patients with intermittent claudication: effects on the risk of peripheral vascular complications, myocardial infarction and mortality. Acta Med Scand. 1987;221:253–60. [PubMed] [Google Scholar]
- 36.Lassila R, Lepantalo M. Cigarette smoking and the outcome after lower limb arterial surgery. Acta Chir Scand. 1988;154:635–40. [PubMed] [Google Scholar]
- 37.Quick CR, Cotton LT. The measured effect of stopping smoking on intermittent claudication. Br J Surg. 1982;69(Suppl):S24–6. doi: 10.1002/bjs.1800691309. [DOI] [PubMed] [Google Scholar]
- 38.Gardner AW. The effect of cigarette smoking on exercise capacity in patients with intermittent claudication. Vasc Med. 1996;1:181–6. doi: 10.1177/1358863X9600100302. [DOI] [PubMed] [Google Scholar]
- 39.Law M, Tang JL. An analysis of the effectiveness of interventions intended to help people stop smoking. Arch Intern Med. 1995;155:1933–41. [PubMed] [Google Scholar]
- 40.West R, Baker CL, Cappelleri JC, et al. Effect of varenicline and bupropion SR on craving, nicotine withdrawal symptoms, and rewarding effects of smoking during a quit attempt. Psychopharmacology (Berl) 2008;197:371–7. doi: 10.1007/s00213-007-1041-3. [DOI] [PubMed] [Google Scholar]
- 41.Knight C, Howard P, Baker CL, et al. The cost-effectiveness of an extended course (12+12 weeks) of varenicline compared with other available smoking cessation strategies in the United States: an extension and update to the BENESCO model. Value Health. 2010;13:209–14. doi: 10.1111/j.1524-4733.2009.00672.x. [DOI] [PubMed] [Google Scholar]
- 42.Olin JW. Thromboangiitis obliterans (Buerger's disease) N Engl J Med. 2000;343:864–9. doi: 10.1056/NEJM200009213431207. [DOI] [PubMed] [Google Scholar]
- 43.CAPRIE Steering Committee A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE) Lancet. 1996;348:1329–39. doi: 10.1016/s0140-6736(96)09457-3. [DOI] [PubMed] [Google Scholar]
- 44.Antithrombotic Trialists’ Collaboration Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324:71–86. doi: 10.1136/bmj.324.7329.71. [published correction appears in BMJ. 2002;324:141] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Catalano M, Born G, Peto R. Prevention of serious vascular events by aspirin amongst patients with peripheral arterial disease: randomized, double-blind trial. J Intern Med. 2007;261:276–84. doi: 10.1111/j.1365-2796.2006.01763.x. [DOI] [PubMed] [Google Scholar]
- 46.Belch J, MacCuish A, Campbell I, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ. 2008;337:a1840. doi: 10.1136/bmj.a1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fowkes FG, Price JF, Stewart MC, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA. 2010;303:841–8. doi: 10.1001/jama.2010.221. [DOI] [PubMed] [Google Scholar]
- 48.Bhatt DL, Fox KA, Hacke W, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006;354:1706–17. doi: 10.1056/NEJMoa060989. [DOI] [PubMed] [Google Scholar]
- 49.Cacoub PP, Bhatt DL, Steg PG, et al. Patients with peripheral arterial disease in the CHARISMA trial. Eur Heart J. 2009;30:192–201. doi: 10.1093/eurheartj/ehn534. [DOI] [PubMed] [Google Scholar]
- 50.Anand S, Yusuf S, Xie C, et al. Oral anticoagulant and antiplatelet therapy and peripheral arterial disease. N Engl J Med. 2007;357:217–27. doi: 10.1056/NEJMoa065959. [DOI] [PubMed] [Google Scholar]
- 51.Berger JS, Krantz MJ, Kittelson JM, et al. Aspirin for the prevention of cardiovascular events in patients with peripheral artery disease: a meta-analysis of randomized trials. JAMA. 2009;301:1909–19. doi: 10.1001/jama.2009.623. [DOI] [PubMed] [Google Scholar]
- 52.Bhatt DL, Flather MD, Hacke W, et al. Patients with prior myocardial infarction, stroke, or symptomatic peripheral arterial disease in the CHARISMA trial. J Am Coll Cardiol. 2007;49:1982–8. doi: 10.1016/j.jacc.2007.03.025. [DOI] [PubMed] [Google Scholar]
- 53.Bernstein EF, Rhodes GA, Stuart SH, et al. Toe pulse reappearance time in prediction of aortofemoral bypass success. Ann Surg. 1981;193:201–5. doi: 10.1097/00000658-198102000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bradbury AW, Adam DJ, Bell J, et al. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: an intention-to-treat analysis of amputation-free and overall survival in patients randomized to a bypass surgery-first or a balloon angioplasty-first revascularization strategy. J Vasc Surg. 2010;51:5S–17S. doi: 10.1016/j.jvs.2010.01.073. [DOI] [PubMed] [Google Scholar]
- 55.Adam DJ, Beard JD, Cleveland T, et al. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005;366:1925–34. doi: 10.1016/S0140-6736(05)67704-5. [DOI] [PubMed] [Google Scholar]
- 56.Greenhalgh RM, Brown LC, Powell JT, et al. Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med. 2010;362:1863–71. doi: 10.1056/NEJMoa0909305. [DOI] [PubMed] [Google Scholar]
- 57.Blankensteijn JD, de Jong SE, Prinssen M, et al. Two-year outcomes after conventional or endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2005;352:2398–405. doi: 10.1056/NEJMoa051255. [DOI] [PubMed] [Google Scholar]
- 58.De Bruin JL, Baas AF, Buth J, et al. Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. N Engl J Med. 2010;362:1881–9. doi: 10.1056/NEJMoa0909499. [DOI] [PubMed] [Google Scholar]
- 59.Greenhalgh RM, Brown LC, Powell JT, et al. Endovascular repair of aortic aneurysm in patients physically ineligible for open repair. N Engl J Med. 2010;362:1872–80. doi: 10.1056/NEJMoa0911056. [DOI] [PubMed] [Google Scholar]
- 60.Lederle FA, Freischlag JA, Kyriakides TC, et al. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA. 2009;302:1535–42. doi: 10.1001/jama.2009.1426. [DOI] [PubMed] [Google Scholar]
- 61.Brown LC, Epstein D, Manca A, et al. The UK Endovascular Aneurysm Repair (EVAR) trials: design, methodology and progress. Eur J Vasc Endovasc Surg. 2004;27:372–81. doi: 10.1016/j.ejvs.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 62.Schanzer A, Hevelone N, Owens CD, et al. Statins are independently associated with reduced mortality in patients undergoing infrainguinal bypass graft surgery for critical limb ischemia. J Vasc Surg. 2008;47:774–81. doi: 10.1016/j.jvs.2007.11.056. [DOI] [PubMed] [Google Scholar]
- 63.Conte MS, Bandyk DF, Clowes AW, et al. Results of PREVENT III: a multicenter, randomized trial of edifoligide for the prevention of vein graft failure in lower extremity bypass surgery. J Vasc Surg. 2006;43:742–51. doi: 10.1016/j.jvs.2005.12.058. [DOI] [PubMed] [Google Scholar]
- 64.Diehm C, Schuster A, Allenberg JR, et al. High prevalence of peripheral arterial disease and co-morbidity in 6,880 primary care patients: cross-sectional study. Atherosclerosis. 2004;172:95–105. doi: 10.1016/s0021-9150(03)00204-1. [DOI] [PubMed] [Google Scholar]
- 65.Hennrikus D, Joseph AM, Lando HA, et al. Effectiveness of a smoking cessation program for peripheral artery disease patients: a randomized controlled trial. J Am Coll Cardiol. 2010;56:2105–12. doi: 10.1016/j.jacc.2010.07.031. [DOI] [PubMed] [Google Scholar]
- 66.Bhatt DL, Topol EJ. Clopidogrel added to aspirin versus aspirin alone in secondary prevention and high-risk primary prevention: rationale and design of the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) trial. Am Heart J. 2004;148:263–8. doi: 10.1016/j.ahj.2004.03.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.