Abstract
A 47 year old lady with hyperthyroidism for past 1½ years was initially on Carbimazole 20 mg orally then changed to 30 mg (during Hysterectomy) but was taking 10 mg for last 1 year. She had intermittent fever with severe B/L bifrontal headache since 3 weeks. Routine investigations showed anaemia, neutropenia, leucopenia and CRP elevation. Peripheral smear showed normocytic normochromic anaemia with Rouleaux formation, leucopenia with 2% atypical cells and mild thrombocytosis. Widal test, RA factor (Rheumatoid factor) test, Ig M (Immunoglobulin M) dengue, Ig M Lepto, TORCH infections (Toxoplasmosis, Other (Syphilis, varicella-zoster, parvovirus B19), Cytomegalovirus and Herpes infections), ANA (Antinuclear antibody) screen cANCA (Cytoplasmic antineutrophil cytoplasmic antibodies) and pANCA (Perinuclear Anti-Neutrophil Cytoplasmic Antibodies) tests were negative. Bone marrow aspiration showed normo to hypercellular marrow with 15% atypical cells and plasma cells. Multiple myeloma workup was done. Carbimazole was withheld. Conclusion: Drug induced agranulocytosis occurs with in 1-2 months of taking the antithyroid medication but onset delayed by 1½ year. De-challenge resulted normalization of blood parameters.
Keywords: Agranulocytosis, carbimazole, hyperthyroidism
INTRODUCTION
Carbimazole, a prodrug which gets converted into the active form methimazole, is used alone or in combination with other medications for the treatment of hyperthyroidism. This therapy usually starts with two to three divided doses totaling 30–60 mg/day but the maximal blocking dose should be 120 mg/day. Usually within 4–8 weeks of initial therapy, symptoms will diminish and circulating thyroid hormone levels will return to normal. Typical range of daily maintenance dose is 5–30 mg/day.[1] Common side effects associated with this drug are minor but sometimes it can cause serious blood disorders. Higher doses of methimazole taken by the patient, greater than 30 mg/day and/or age of greater than 40 years has got higher chance for the development of agranulocytosis which can happen within 2 months of therapy.[2]
CASE REPORT
A 47-year-old lady presented with type II diabetes mellitus for the past 2 years on metformin, systemic hypertension for the past 1 year on telmisartan, hyperthyroidism for the past 1½ years was initially on T. carbimazole 20 mg once daily then changed to 30 mg once daily (at the time of hysterectomy) but was taking 10 mg once daily for the last 1 year. She presented with redness on both eyes 1 month ago, initially over left eye in late December 2013 which subsided next day, then followed by redness in the right eye which subsided after the application of eye drops within 5 days. There was no pain or discharge from either eye. She had on and off fever (100–101°F) since 3 weeks which was associated with severe B/L bifrontal headache initially but subsided within 1 week. She also had weight loss of 6 kg within 1 month (56–50 kg) as well as loss of appetite.
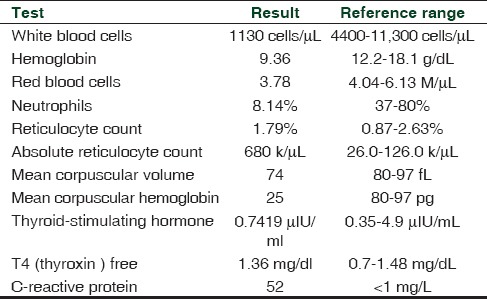
Routine investigations were done which showed anemia, neutropenia, leucopenia and high CRP (C reactive protein) [Table 1]. Peripheral smear showed normocytic normochromic anemia with Rouleaux formation, leucopenia with 2% atypical cells and mild thrombocytosis. She was empirically started on inj. Cefoperazone sulbactam 2 g IV (intravenously) twice daily in view of neutropenia, tachycardia and elevated CRP. Blood cultures, both aerobic and anaerobic, urine culture Widal test, RA factor (rheumatoid factor) test, Ig M (immunoglobulin M) dengue, Ig M Lepto, TORCH infections (Toxoplasmosis, Other (Syphilis, varicella-zoster, parvovirus B19), cytomegalovirus and herpes infections) and ANA (antinuclear antibody) screen all tests were found to be negative. Second option of bone marrow aspiration studies was sought from pathology department which showed normo to hypercellular marrow with 15% atypical cells and plasma cells, and advised correlation with flow cytometry. Carbimazole was withheld in view of leucopenia.
Table 1.
Laboratory investigations
Workup for multiple myeloma was done. Serum Ig G was 3196 mg/dL, Ig M 85.0 mg/dL, Serum beta 2 microglobulin 1.6 mg/dL, lambda freelite 102.93 mg/L, kappa freelite 63.88 mg/L but serum protein electrophoresis showed only polyclonal gammopathy. Bone marrow aspiration/biopsy as well as cultures was repeated. A bone marrow biopsy showed focally hypercellular marrow with increased plasma cells amidst trilineage maturation.
In this case, differential count showed reduced neutrophils (8%) and predominant lymphocytes. Bone marrow aspirate showed markedly reduced mature form of granulocytes. Bone marrow trephine also showed reduced myeloid series with increase in plasma cells. These findings are typically associated with agranulocytosis.
Endocrinology opinion was sought during the hospital stay for the modification of anti-thyroid medications as well as glycemic control since TFT (thyroid function test) done twice was within the normal range, anti-thyroid medications were not started for the time being. For glycemic control T. sitagliptin 50 mg once daily was added with metformin.
Since there was a possibility of autoimmune etiology for bicytopenia, rheumatology opinion was sought following which CANCA (cytoplasm antineutrophil cytoplasmic antibodies) and PANCA (perinuclear anti-neutrophil cytoplasmic antibodies) results showed negative results.
With the treatment she received her counts gradually showed an improving trend and she got discharged with T. folic acid 5 mg once daily. The WBC (white blood cells) count and neutrophil count became normal during the follow-up visit after 1 month.
COMMENT
Hyperthyroidism is a common endocrine disorder which affects mainly women with a prevalence of 2%.[3] Anti-thyroid drug therapy is the main treatment for this condition. A serious rare side effect of carbimazole is agranulocytosis. This drug-induced agranulocytosis is a lethal condition but reversible if recognized and treated accordingly[4]
The incidence of carbimazole induced agranulocytosis is 0.3–0.6%[5] and has got a mortality rate of 21.5%.[6] In 1983, a study conducted by Cooper et al. concluded that methimazole in higher doses of 30 mg/day age of 40 years or above caused greater risk for the development of agranulocytosis[2]
This diagnosis is still not applicable for patients who are on chemotherapy or patients with chronic neutropenia including congenital and chronic autoimmune neutropenia[4]
Drug-induced agranulocytosis occurs within 1–2 months of taking the anti-thyroid medication but the onset can get delayed. Usually the WBC count returns to normal over a period of 1–2 weeks after discontinuing the offending drug and the time taken can be ranged from 7 to 56 days[3,7]
Recovery of the neutrophil count depends upon the number of myeloid precursor cells present in the bone marrow and may get prolonged if there is granulocyte precursor aplasia[4]
The first mechanism for this agranulocytosis was explained by Sprikkelman et al. who explained four different possible immunological mechanisms.[8] Firstly, when the drug gets attached with granulocyte antibody production starts resulting in the destruction of granulocytes. Secondly, antibodies may target on the drug metabolite complex adsorbed on the neutrophil granulocyte in presence of plasma component. Thirdly, the drug may trigger auto antibodies. Finally, the interaction between the granulocyte antigen and the drug may induce the production of antibodies
Along with these mechanisms, idiosyncratic drug-induced agranulocytosis, which is a severe selective depression of myelopoiesis due to an unpredictable adverse reaction to a wide variety of drugs in hypertensive patients, has also been a postulated mechanism for agranulocytosis[4]
The prognosis of this event depends on variety of factors like age, co morbidity, duration of severe granulocytopenia and immediate antibiotic treatment[4]
Successful treatment of anti-thyroid drug-induced agranulocytosis by GCSF (granulocyte colony-stimulating factor) has been reported.[3,9] It enhances the recovery of the peripheral blood granulocyte lineage which results in the faster normalization of peripheral granulocyte count as well as reduction in chances of fatal complications like bacterial infections.[10]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM. 8th ed. United States of America: The McGraw Hill Companies; 2011. Pharmacotherapy: A Pathophysiologic Approach; pp. 1310–26. [Google Scholar]
- 2.Cooper DS, Goldminz D, Levin AA, Ladenson PW, Daniels GH, Molitch ME, et al. Agranulocytosis associated with antithyroid drugs. Effects of patient age and drug dose. Ann Intern Med. 1983;98:26–9. doi: 10.7326/0003-4819-98-1-26. [DOI] [PubMed] [Google Scholar]
- 3.Tavintharan S, Rajasoorya C, Chew LS. Carbimazole-induced agranulocytosis-a report of 2 recent cases. Singapore Med J. 1997;38:386–7. [PubMed] [Google Scholar]
- 4.Lee CH, Liang RH. Antithyroid drug-induced agranulocytosis. Hong Kong Med J. 1999;5:394–6. [PubMed] [Google Scholar]
- 5.Genet P, Pulik M, Lionnet F, Bremont C. Use of colonystimulating factors for the treatment of carbimazole-induced agranulocytosis. Am J Hematol. 1994;47:334–5. doi: 10.1002/ajh.2830470422. [DOI] [PubMed] [Google Scholar]
- 6.Juliá A, Olona M, Bueno J, Revilla E, Rosselló J, Petit J, et al. Drug-induced agranulocytosis: Prognostic factors in a series of 168 episodes. Br J Haematol. 1991;79:366–72. doi: 10.1111/j.1365-2141.1991.tb08042.x. [DOI] [PubMed] [Google Scholar]
- 7.Ng SC. Carbimazole-induced agranulocytosis treated with granulocyte-macrophage colony stimulating factor-a case report. Ann Acad Med Singapore. 1995;24:465–6. [PubMed] [Google Scholar]
- 8.Sprikkelman A, de Wolf JT, Vellenga E. The application of hematopoietic growth factors in drug-induced agranulocytosis: A review of 70 Cases. Leukemia. 1994;8:2031–6. [PubMed] [Google Scholar]
- 9.Gerl A, Gerhartz H, Wilmanns W. GM-CSF for agranulocytosis. J Intern Med. 1991;230:90–1. [PubMed] [Google Scholar]
- 10.Sheng WH, Hung CC, Chen YC, Fang CT, Hsieh SM, Chang SC, et al. Antithyroid-drug-induced agranulocytosis complicated by life-threatening infections. QJM. 1999;92:455–61. doi: 10.1093/qjmed/92.8.455. [DOI] [PubMed] [Google Scholar]


