Abstract
Context:
This study is a continuation of the earlier studies and has been extended to investigate the potential forensic markers of elder abuse.
Aims:
To determine the prevalence of elder abuse in various outpatient departments (OPDs). To study the associated parameters related to the abuser and the abused. To determine the existence of potential forensic markers of elder abuse.
Settings and Design:
The subjects were randomly selected from the medical and the dental OPDs of the university.
Materials and Methods:
Eight hundred and thirty two elderly subjects in the age range 40-60 years were interviewed using a questionnaire to determine the existence of elder abuse. The subjects were investigated and examined for weight, nutrition and hydration, vital signs, habits, existing visual and auditory capabilities, medications, disclosure of wills/deeds, signs of depression, and documented cleanliness. The mini-mental state examination, the Geriatric Depression Scale, the Clock drawing test, and the Brief Psychiatric Rating Scale were used to determine the potential forensic markers.
Statistical Analysis Used:
Mean values in percentage were determined by dividing the number of determined subjects by the total number of subjects for that parameter.
Results:
About 37% in medical and 41% in dental OPDs were found to have suffered from abuse, mostly in the age group 60-70 years. Females received more abuse and a combination of son and daughter-in-law constituted most abusers. Various potential markers of elder abuse and neglect investigated among the elder abuse victims included depression (89%), signs of improper feeding (83%), changes in personal hygiene (69%), need for medical/dental treatment (78%), medication misuse (67%), changes in wills/deeds (26%), decubiti (10%), bruises (17%), skin tears (27%), and confusion (23%).
Conclusions:
Elder abuse exists in one or more forms in both medical and dental OPDs among both males and females in all age groups.
Keywords: Deed, depression, neglect, personal hygiene, domestic violence
Introduction
While preparing a presentation on an earlier study for a national forensic conference, the authors of the present study came across incidents of extreme elder abuse in India reported in the electronic media over the past 5 years that inspired this study to be continued further. Extreme cases, where an elderly person was either killed by his/her son or money was paid to contract killers to get a parent killed, have come to the limelight in the world of crime.[1,2,3,4,5,6] Whatever might be the case, the fact is that many elderly might be dying because their children might be depriving them of adequate nutrition, medical and general health care, or subjecting them to extreme physical abuse. Forensic science needs to encompass this subject comprehensively. Researchers who are associated with elder abuse and neglect believe that the state of medical knowledge and forensic science regarding elder abuse and neglect is approximately equivalent to that of child abuse and neglect three decades ago and domestic violence 10-15 years ago.[7] The difference has been that though children and young victims of domestic violence are generally healthy and are not expected to die, older people suffer from medical problems and are functionally dependant that makes them vulnerable and potential victims of stressors causing death. Medical conditions and aging bring attributes that mimic or mask the markers of elder abuse and neglect, which if critically scrutinized can simplify analysis and detection.
Developing countries like India not only lack primary data relating to forensic markers, but many of them are still in a mode of denial because of culture and traditions.[8] Nevertheless, the evidence is enough, which is apparent and striking but deceptive and blunt when refused. Elder abuse affects every social stratum and shows no regard for race, creed, or color. It is well documented that elder abuse has a direct influence on the quality of life of the person who is being abused. The mortality associated with elder abuse has been studied and it has been found that elder abuse victims have poorer survival rates than those of self-neglect.[9,10] Extreme cases of abuse, for example, gunshot wounds, knife wounds, burns, large decubiti, starvation, or bite marks are not diagnostic dilemmas; most cases fall into an area where abuse and neglect are not clear-cut as there are minute distinctions.[11] Resolution of these difficult distinctions, though, is beyond the scope of this study. However, whether elder abuse and neglect have occurred is a conclusion that is drawn from a constellation of factors, which are both medical and legal. The present study is a continuation of its first study and is aimed to determine the prevalence of elder abuse subjects in dental and medical hospital outpatient departments (OPDs), along with their parameters. More significantly, this study will also evaluate the presence or absence of various clinical and forensic markers in the subjects that indicate neglect.
Materials and Methods
After obtaining ethical clearance from the Ethics Committee of the university, which is in accordance with the Declaration of Helsinki on human experimentation, informed consent was taken from the subjects. The study was conducted on 832 elderly subjects whose age ranged 40-80 years. About 512 subjects were interviewed in the medical OPD and 320 in the dental OPD of the university in the western part of the state of Uttar Pradesh (India). Subject selection was random and constituted diverse communities with 349 females, 480 males, and 3 subjects belonging to the other sex. Selection criteria required the subjects to be living with their existing family, seeking treatment in various specialties, to be cooperative for any protocol that was needed for the study, and not have any impairment of thinking, memory, functional ability, or decision-making capacity. The subjects were screened for diagnosis of elder abuse of one or more forms with the help of a questionnaire.[12] All the subjects were investigated and examined for weight, evaluation of nutrition and hydration, vital signs, habits, existing visual and auditory capabilities, medications including written prescriptions, disclosure of wills/deeds, general physical examination, including a detailed oral examination, signs of depression, documented cleanliness, and a detailed social history including that of the existing family members. Examination of each subject was done by experts in the field of medicine, surgery, psychiatry, ophthalmology, orthopedics, oral practice, oral pathology, prosthodontics, and physiotherapy. The methodology to determine the forensic markers included the mini-mental state examination (MMSE),[13] the Geriatric Depression Scale (GDS),[14,15] the Clock drawing test,[16,17] and the Brief Psychiatric Rating Scale (BPRS).[18] The MMSE or Folstein test was used to exclude subjects with cognitive impairment, especially cases of dementia, the GDS identified depression and its associated levels, the clock drawing test identified subjects who could be suffering from spatial neglect and the BPRS was used to measure psychiatric symptoms such as depression, anxiety, hallucinations and unusual social behavior. The data collected was entered into an SPSS (Statistical Package for Social sciences) (IBM version 20) and various properties of the variables were defined. Means for each variable were tabulated and represented in graphic form. Prevalence of elder abuse subjects was determined by calculating the number of abused and non-abused subjects from the total number of subjects surveyed. Abuse prevalence in relation to age and sex was determined by calculating the number of abused subjects of a particular age/sex group from the total number of subjects belonging to the same age group of the total sample. Potential forensic markers were determined by a combination of relevant clinical history, clinical examination, pertinent investigation, and laboratory/psychological tests.
Results
Among the total number of subjects included in the survey, 39.85% were suffering from some form of elder abuse. This constituted about 41.9% of abused subjects in the dental OPD and about 37.8% in the m edical OPD [Graph 1]. Abuses in one form or the other were seen to be less prevalent in the fourth and seventh decades of life, whereas they were most prevalent in the fifth decade [Graph 2]. Among the sexes, it was observed that the male subjects were affected in all ages with the exception between 60 years and 70 years during which time the females received more abuse [Graph 3].
Graph 1.
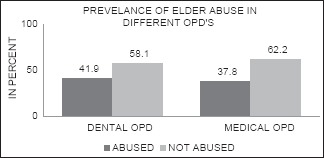
Distribution of elder abuse subjects in various OPD
Graph 2.
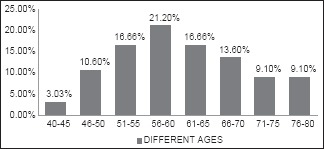
Prevalence of abuse among different age groups in both categories (OPDs)
Graph 3.
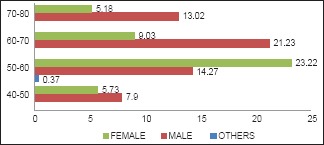
Relationship between various sexes with respect to different age groups
Among the different types of elder abuse, the combination type of more than one abuse was more prevalent (38.9% of dental patients and 13.6% of medical patients), followed by psychological abuse (29.3% of dental patients and 27.4% of medical patients) and neglect (20.3% of dental patients and 24.1% of medical patients) [Graph 4]. Within the various combination types, results showed that the psychological type of abuse was more prevalent than any individual type. Psychological abuse was present in more than 74% of dental OPD and 86% of medical OPD subjects. About 25% of dental patients and 23% of medical patients were found to suffer from more than two types of abuse [Graph 5]. The relationship between the different types of abuse and the abuser as depicted in Graph 6 shows that physical abuse, neglect, and financial abuse were committed mostly by sons, whereas psychological abuse mostly by daughters-in-law. Abuse by spouse was also prevalent, especially in females. Those subjects who were suffering from more than one abuse (combined) were also mostly done so by a combination of the son and the daughter-in-law (54.54% of dental patients and 48.12% of medical patients) [Graph 7]. Various potential markers of elder abuse and neglect investigated among the elder abuse victims included depression (89%), signs of improper feeding (83%), changes in personal hygiene (69%), need for medical/dental treatment (78%), medication misuse (67%), changes in wills/deeds (26%), decubiti (10%), bruises (17%), skin tears (27%), and confusion (23%) [Graph 8].
Graph 4.
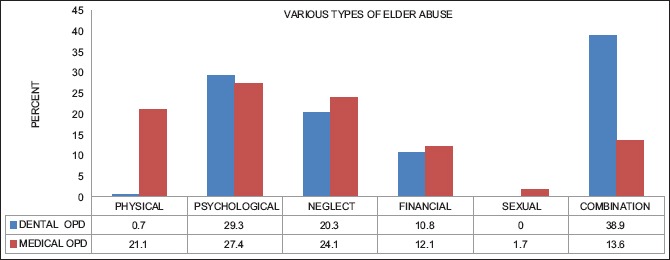
Distribution of different types of abuse in respective OPDs
Graph 5.
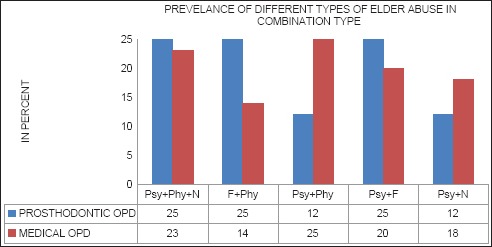
Combination of various types of elder abuse
Graph 6.
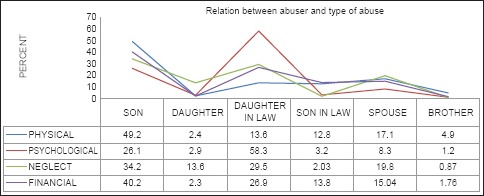
Association between the different types of abuser and the type of abuse
Graph 7.
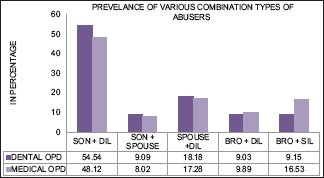
Distribution of different types of abusers
Graph 8.
Distribution of potential forensic markers in the study subjects (in percentage)
Discussion
Older people not only constitute the fastest growing segment of the population but also the largest consumers of health-care facilities.[19] Projections suggest that by 2025, the elderly will constitute 12-13%,[19] which by 2050 will further rise to 17% of the entire population.[20] Although it has been said that an issue like elder abuse is not a problem for countries like India because a value-based joint family system prevails, studies done in various parts of India reveal a different picture [Graph 9].[21,22,23,24,25,26,27] Worldwide, it is evident that elder abuse is on the rise and it may be due to many factors that need to be understood to find solutions. The present study shows that patients visiting hospitals for either medical or dental treatment do suffer from some type of abuse and it may affect the patient's compliance with any treatment. Majority of the abused subjects were found in the age group 50-60 years, especially females (23%), with a combination type of elder abuse being the most prevalent (38%) and psychological type associated with other abuses being the most common.
Graph 9.
Various studies on elder abuse conducted in India
Forensic aspects of elder abuse and neglect are not only undocumented but unexplored and uncharted too. As primary data related to forensic markers of elder abuse are scant, this study investigated the presence or absence of abrasions, lacerations, bruises, fractures, restraints, decubiti, weight loss, dehydration, medication use, burns, cognitive and mental health problems, personal hygiene, and sexual abuse by integrating every possible data available from the subjects. About 26% of the elders abused revealed that they had already made and declared their will and that their main assets had been transferred. The subjects especially most of the widows seemed to be under high risk of financial exploitation, which is in accordance with Parveza et al.[28] The subjects who had changed or were forced to change their will were suffering from multiple types of abuse. Three subjects who had suddenly transferred their personal belongings like vehicle, land, and house had no explanation that raised suspicions of elder abuse as mentioned by Fulmer[29] and Tueth.[30] Gauging of a forensic marker like personal hygiene can be difficult at times as poor personal care is a matter of lifestyle or choice. In order to consider hygiene as a forensic marker, only those (69%) out of the total number of subjects were considered who had exhibited a definite and significant decline in their overall hygiene compared to the past, in spite of not suffering from any form of dementia or psychotic illness.[31,32] Age-related changes have no impact on one's hygiene; therefore, any decline in personal hygiene demonstrates neglect.[33,34] Dirty clothes and footwear, dirt-laden nails, bad odor emanating from clothes, and skin infections like scabies were some of the signs found during examination of the abused subjects.
Cognitive and mental health disorders like depression, dementia, alcohol abuse, psychosis (not related to age),[35,36] and self-neglect though affecting a large number of aging individuals, have been considered as potential forensic markers. A large majority of the elder abused subjects in this study were found to be depressed (89%) and some were abusing alcohol (5%), which is in accordance with the studies done earlier.[37,38] Individuals with dementia and depression are likely to be more prone to further abuse and neglect because such patients tend to exceed the threshold of tolerance of the caregivers.[39] The results of the present study showed that about 67% of the abused subjects gave a history indicative of misuse of medication by withholding necessary medication, delaying the purchase of medicines, administering medicines not mentioned by the doctors, altering the dose of medicines, and not being monitored when any new medicine was prescribed. As mentioned in the literature, geriatric patients consuming adult dose itself indicates drug abuse.[40,41] Forensic markers in the form of unusually located skin tears[42,43,44] (27%) especially in the physically abused subjects, bruises[45,46] (17%), history of avulsed teeth, and existing decubiti[47,48,49] (10%) were also seen, which indicated abuse and neglect on the part of the caregivers. Unusual locations of skin tears in the study were found in the head region, especially the left side, and on the subject's back, neck, and face. The bruised individuals showed retention of shape of causative agents, parallel marks, and bruised hands. Perhaps the most important forensic marker that was highlighted during the study was related to malnutrition. Loss of weight in some individuals over the last 3-5 years ranged 8-15 kg. A large percentage of the subjects required partial and complete dentures, which most of them had never made, whereas 83% were not fed the food of their choice and 65% were inappropriately fed (isolated feeding, cold food, previous day's food, leftover food, and food that would harm like excessive sweet, salty, oily, spicy, and partially cooked food). Malnutrition can be an important predisposing factor for other illnesses or death as it can lead to rapid loss of weight (40% loss of body weight can result in death).[49]
Summary and Conclusion
Elder abuse exists among those patients who visit medical and dental hospitals. Elder abuse affects the quality of life of a person and could be an important factor in such subjects showing poor compliance with medical or dental treatment. Health care workers, especially those who rely on the patient's cooperation for better treatment results, should not rule out the possibility of existing elder abuse. It is also important that evidence-based forensic markers of elder abuse and neglect are further studied for various parameters related to both the abuser and the abused. Scant data in the field demand comprehensive research programs that will enhance the forensic detection of those cases where death might be due to elder abuse or neglect.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Drunkard son kills father. The Times of India. 2011. Oct, [Last accessed on 2011 Oct 11]. Available from: http://www.timesofindia.indiatimes.com/india/drunkard-son-killsfather/articleshow/10522821.cms .
- 2.Drunkard son kills father in Uttar Pradesh. [Last accessed on 2012 Jun 09]. Available from: http://www.ibnlive.in.com/news/drunkard- son-kills-father-in-uttar- pradesh/265208-44.html .
- 3.Horrifying case of son killed his father rocked the Rae bareli. [Last accessed on 2013 May 07]. Available from: http://www.dailypioneer.com/state-editions/lucknow/horrifying-case-of-son-killed-his-father-rocked-the-rae-bareli.html .
- 4.Sons hire contract killer for murdering 70-year-old father. [Last accessed on 2014 Mar 03]. Available from: http://www.news18.com/news/uttar-pradesh/sons-hire-contract-killer-for-murdering-70-year-old-father-379359.html .
- 5.Man kills father, step-brother, wife over property dispute. The Times of India. [Last accessed on 2014 Mar 07]. Available from: http://www.article.wn.com/view/2013/12/30/Man_kills_father_stepbrother_wife_over_property_dispute/
- 6.Inebriated son kills father over trivial issue. [Last accessed on 2012 Jul 13]. Available from: http://timesofindia.indiatimes.com/city/nagpur/Inebriated-son-kills-father-over-trivial-issue-arrested/articleshow/14856652.cms .
- 7.Washington, DC: [Last accessed on 2000 Oct 18]. Elder Justice Roundtable Report: Medical Forensic Issues Concerning Abuse and Neglect. The Department of Justice medical forensic roundtable discussion. Available from: http://www.ojp.usdoj.gov/nij/elderjust . [Google Scholar]
- 8.Shankardass MK. Combating elder abuse in India: An emerging social, legal and public health concern, symposists’ papers, invited symposia on elder abuse, executive editor, Toshio Tatara, Tokyo International Forum, Japan. Indian J Gerontol. 2008;22:422–46. [Google Scholar]
- 9.Dyer CB, Goodwin JS, Pickens-Pace S, Burnett J, Kelly PA. Self-neglect among the elderly: A model based on more than 500 patients seen by a geriatric medicine team. Am J Public Health. 2007;97:1671–6. doi: 10.2105/AJPH.2006.097113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lachs MS, Williams CS, O’Brien S, Pillemer KA, Charlson ME. The mortality of elder mistreatment. JAMA. 1998;280:428–32. doi: 10.1001/jama.280.5.428. [DOI] [PubMed] [Google Scholar]
- 11.Rawson RD, Ommen RK, Kinard G, Johnson J, Yfantis A. Statistical evidence for the individuality of the human dentition. J Forensic Sci. 1984;29:245–53. [PubMed] [Google Scholar]
- 12.Mattoo KA, Shalabh K, Khan A. Geriatric forensics: A dentist's perspective and contribution to identify existence of elder abuse among his patients. J Forensic Dent Sci. 2010;2:81–5. doi: 10.4103/0975-1475.81287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 14.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clin Gerontol. 1986;5:165–73. [Google Scholar]
- 15.Yesavage JA, Brink TL, Rose TL. Development and validation of a geriatric depression screening scale: A preliminary report. J Psychiatr Res. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 16.Agrell B, Dehlin O. The clock-drawing test. Age Ageing. 1998;27:399–403. doi: 10.1093/ageing/afs149. [DOI] [PubMed] [Google Scholar]
- 17.Bartolomeo P. Visual neglect. Curr Opin Neurol. 2007;20:381–6. doi: 10.1097/WCO.0b013e32816aa3a3. [DOI] [PubMed] [Google Scholar]
- 18.Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812. [Google Scholar]
- 19.Active ageing: A policy framework. Geneva, World Health Organization, 2002 (WHO/NMH/NPH/02.8) [Last accessed on 2012 July 13]. Available from http://www.whqlibdoc.who.int/hq/2002/WHO_NMH_NPH_02.8.pdf .
- 20.Hudson M. Analyses of the concepts of elder mistreatment: Abuse and neglect. J Elder Abuse Negl. 1988;1:5–26. [Google Scholar]
- 21.Madrid, Spain: 2002. Second World Assembly on Ageing. Plan of Action and Political Declaration. [Google Scholar]
- 22.Soneja S. Elder abuse in India. Country report for World Health Organization. HelpAge-India. [Last accessed on 2015 Feb 6]. Available from: http://www.who.int/ageing/projects/elder_abuse/alc_ea_ind.pdf .
- 23.Chokkanathan S, Lee AE. Elder mistreatment in urban India: A community based study. J Elder Abuse Negl. 2005;17:45–61. doi: 10.1300/j084v17n02_03. [DOI] [PubMed] [Google Scholar]
- 24.Mattoo KA, Shalabh K, Khan A. Prevalence of elder abuse among completely edentulous patients seeking complete denture prosthesis: A survey. J Indian Acad Geriatr. 2009;5:177–80. [Google Scholar]
- 25.Help Age India. Help Age India's ‘Report on Elder Abuse in India’ brings out some startling facts. [Last accessed on 2013 July 10]. Available from: http://www.orissadiary.com/ShowOriyaColumn.asp?i=19158 .
- 26.The Hindu. Chennai ranks lowest in elder abuse [internet]. Chennai. 2011. Jun 16, [Last accessed on 2012 July 13]. Available from http://www.thehindu.com/news/cities/Chennai/article2107897.ece .
- 27.Times of Bangalore. Bangalore tops elder abuse cases: Survey. 2011 [Google Scholar]
- 28.Parveza GJ, Vande Weerd C, Hughes-Harrison V. Financial exploitation of the elderly: A descriptive study of victims and abusers in an urban area. Paper presented at the 50th Annual Scientific Meeting of the Gerontological Society of America; Cincinnati, Ohio. 1997 [Google Scholar]
- 29.Fulmer T, Birkenhauer D. Elder mistreatment assessment as a part of everyday practice. J Gerontol Nurs. 1992;18:42–5. doi: 10.3928/0098-9134-19920301-10. [DOI] [PubMed] [Google Scholar]
- 30.Tueth MJ. Exposing financial exploitation of impaired elderly persons. Am J Geriatr Psychiatry. 2000;8:104–11. [PubMed] [Google Scholar]
- 31.Aravanis SC, Adelman RD, Breckman R, Fulmer TT, Holder E, Lachs M, et al. Diagnostic and treatment guidelines on elder abuse and neglect. Arch Fam Med. 1993;2:371–88. doi: 10.1001/archfami.2.4.371. [DOI] [PubMed] [Google Scholar]
- 32.Butler RN. Warning signs of elder abuse: The family physician may be the patient's only protection from family violence. Geriatrics. 1999;54:3–4. [PubMed] [Google Scholar]
- 33.Lachs MS. Washington, DC: National Institute of Justice; [Last accessed on 2000 Oct 18]. Elder justice roundtable: Medical forensic issues concerning abuse and neglect. Paper presented at the department of justice medical forensic roundtable discussion. Available from: http://www.ojp.usdoj.gov/nij/elderjust . [Google Scholar]
- 34.Lachs MS, Pillemer K. Abuse and neglect of elderly persons. N Engl J Med. 1995;332:437–43. doi: 10.1056/NEJM199502163320706. [DOI] [PubMed] [Google Scholar]
- 35.Coyne AC, Reichman WE, Berbig LJ. The relationship between dementia and elder abuse. Am J Psychiatry. 1993;150:643–46. doi: 10.1176/ajp.150.4.643. [DOI] [PubMed] [Google Scholar]
- 36.Ghodousi A, Maghsoodloo S, Hoseini SMS. Forensic aspect of elder abuse: Risk factors and characteristics. J Res Med Sci. 2011;16:1598–604. [PMC free article] [PubMed] [Google Scholar]
- 37.Dyer CB, Pavlik VN, Murphy KP, Hyman DJ. The high prevalence of depression and dementia in elder abuse and neglect. J Am Geriatr Soc. 2000;48:205–8. doi: 10.1111/j.1532-5415.2000.tb03913.x. [DOI] [PubMed] [Google Scholar]
- 38.Dyer CB, Pavlik VN, Festa NA. Elder mistreatment: Analysis of allegation types and variables associated with multiple allegations from a state wide database. The annual meeting of the American Geriatrics Society. 2000 May 20; [Google Scholar]
- 39.Benton D, Marshall C. Elder abuse. Clin Geriatr Med. 1991;7:831–45. [PubMed] [Google Scholar]
- 40.Monane M, Monane S, Semla T. Optimal medication use in elders. Key to successful aging. West J Med. 1997;167:233–7. [PMC free article] [PubMed] [Google Scholar]
- 41.Zubenko GS, Sunderland T. Geriatric psychopharmacology: Why does age matter? Harv Rev Psychiatry. 2000;7:311–33. [PubMed] [Google Scholar]
- 42.Malone M, Rozario N, Gavinski M, Goodwin J. The epidemiology of skin tears in the institutionalized elderly. J Am Geriatr Soc. 1991;39:591–5. doi: 10.1111/j.1532-5415.1991.tb03599.x. [DOI] [PubMed] [Google Scholar]
- 43.Crane J. Injury interpretation. In: Stark MM, editor. Forensic Science: A Physician's Guide to Clinical Forensic Medicine. Totowa, NJ: Humana Press; 2000. pp. 23–25. [Google Scholar]
- 44.Knight B. 11th ed. New York: Oxford University Press Inc; 1997. Simpson's Forensic Medicine; pp. 122–24. [Google Scholar]
- 45.Langlois NE, Gresham GA. The ageing of bruises: A review and study of the colour changes with time. Forensic Sci Int. 1991;50:227–38. doi: 10.1016/0379-0738(91)90154-b. [DOI] [PubMed] [Google Scholar]
- 46.Fanslow JL, Norton RN, Spinola CG. Indicators of assault-related injuries among women presenting to the emergency department. Ann Emerg Med. 1998;32:341–8. doi: 10.1016/s0196-0644(98)70011-3. [DOI] [PubMed] [Google Scholar]
- 47.Barton A, Barton M. London: Faber and Faber; 1981. The Management and Prevention of Pressure Sores; pp. 88–90. [Google Scholar]
- 48.Bennett GC, Bliss MR. Pressure sores: Etiology and prevalence. In: Tallis R, Fillit H, Brocklehurst JC, editors. Brocklehurst's Textbook of Geriatric Medicine and Gerontology. 5th ed. London: Harcourt Brace and Co; 1998. pp. 178–80. [Google Scholar]
- 49.Schor JD, Selby A, Bertone CA. Geriatric assessment in the diagnosis and treatment of elder abuse. N J Med. 1995;92:108–10. [PubMed] [Google Scholar]