Lipodystrophy is a disorder afflicting subcutaneous fat and can result in lipoatrophy or lipohypertrophy. Before the advent of recombinant human insulin, insulin-induced lipoatrophy was a common problem among insulin users. Lipoatrophy is a clinical condition characterized by localized loss of subcutaneous fat. The prevalence of lipoatrophy was reported to be as high as 24–55% with animal insulins (1). Fortunately, with the use of human insulin, lipoatrophy has become a rare complication (2). Lipohypertrophy is characterized by increased localized adipose tissue mass. Its prevalence is reported to be as high as 20–30% in people with type 1 diabetes using human insulin products (3).
Lipodystrophy resulting from insulin use is localized to insulin injection sites, and its presence might affect insulin absorption. The pathophysiological mechanism of insulin-induced lipodystrophy remains to be determined. Although various mechanisms have been proposed, presence of high-titer anti-insulin antibodies and individual susceptibility to these conditions point toward an immune-mediated mechanism. Concurrent occurrence of lipoatrophy and lipohypertrophy in the same patient is uncommon and, to the best of our knowledge, has not been reported previously.
Case 1 Presentation
A 12-year-old girl with type 1 diabetes for the past 3 years presented with inadequate glycemic control and significant unexplained glycemic variability. She was taking human regular insulin three times per day before meals and human NPH insulin before breakfast and dinner. She had localized lipoatrophy on the abdomen (noted for the past 3 months). Her weight, height, and BMI were 26.3 kg, 130.2 cm, and 15.56 kg/m2, respectively. On examination, she had a localized area of depression on the right side of the abdomen (lipoatrophy), as well as lipohypertrophy on the left side (Figure. 1). Her A1C was 8.8%, and her anti-insulin antibody level was >100 U/mL (normal <10 U/mL). MRI of the affected part of the abdomen showed subtle lipoatrophic and lipohypertrophic changes. After changing the injection site, her blood glucose levels and glycemic variability improved. After 3 months, her A1C was 7.6%.
FIGURE 1.

Lipoatrophy and lipohypertrophy on the abdomen in case 1. Red arrow, lipoatrophy; blue arrow, lipohypertrophy.
Case 2 Presentation
An 8-year-old girl with type 1 diabetes for the past 2 years presented to our clinic. She stated that she had been suffering from recurrent episodes of unexplained hypoglycemia. She was taking human regular insulin twice daily and premixed human insulin (regular 30/NPH 70) once daily. Home capillary blood glucose readings showed erratic and variable glycemic control. There was no history suggestive of fever, infection, foot ulcer, organ dysfunction, or endocrinopathy. On examination, her weight, height, and BMI were 19.2 kg, 114.7 cm, and 14.41 kg/m2, respectively. There was localized loss of fat (lipoatrophy) and lipohypertrophy on the abdomen (Figure 2). Her A1C was 10.4%, and her anti-insulin antibody titer was >100 U/mL. MRI of the affected part of the abdomen showed significant loss of subcutaneous fat in one area and lipohypertrophy elsewhere (Figure 3). A punch biopsy from the lipoatrophic area showed absence of subcutaneous fat and inflammatory cells (Figure 4). We advised her to take insulin in her unaffected thigh and also to rotate her injection sites. Over the next few weeks, her home blood glucose readings improved significantly, with far fewer episodes of hypoglycaemia. After 3 months, her A1C had decreased to 9.6%, with improvement in the lipodistrophy.
FIGURE 2.

Lipoatrophy and lipohypertrophy on the abdomen in case 2. Red arrow, lipoatrophy; blue arrow, lipohypertrophy.
FIGURE 3.
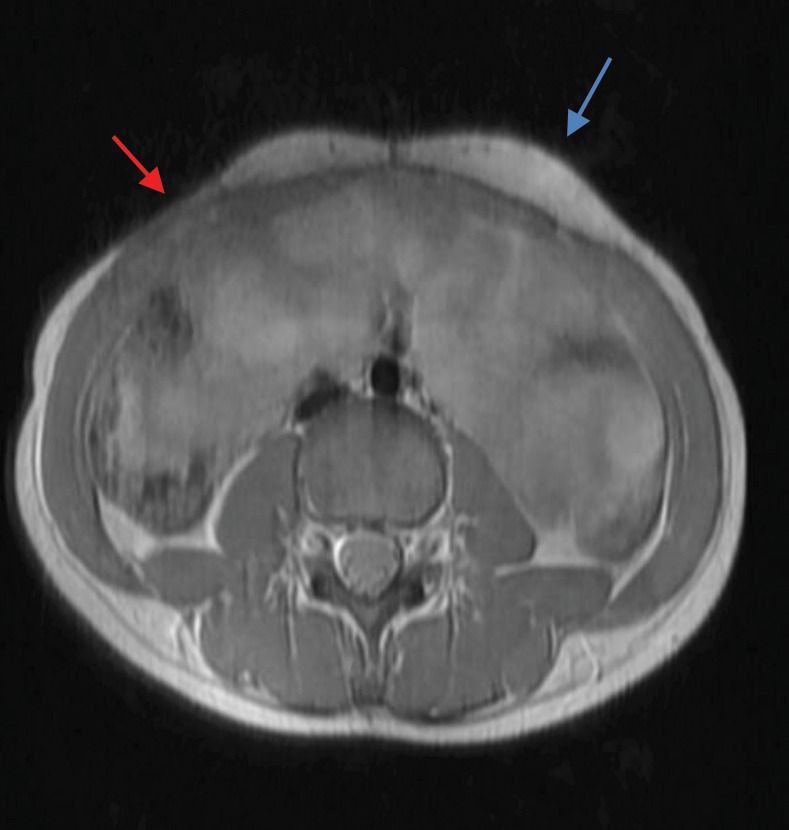
MRI of abdomen showing lipoatrophic and lipohypertrophic areas in case 2. Red arrow, lipoatrophy; blue arrow, lipohypertrophy.
FIGURE 4.
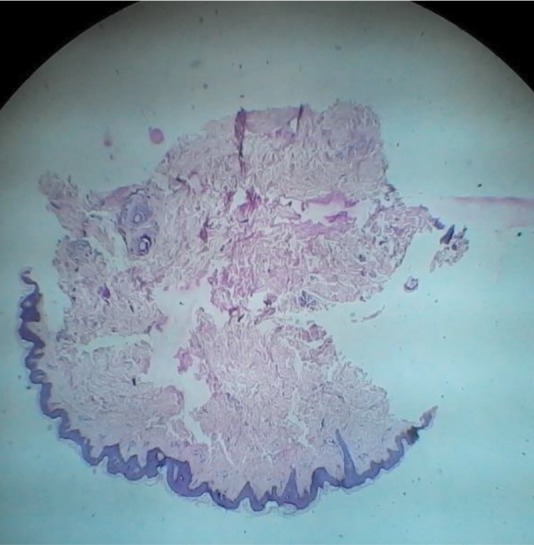
Histopathological examination (high power field, hematoxylin-eosin stain) of the lipoatrophic area shows loss of subcutaneous fat and absence of inflammatory cells in case 2.
Questions
Can lipoatrophy and lipohypertrophy occur in same patient?
What are the possible underlying mechanisms?
Do these conditions affect glycemic status?
Commentary
The pathogenesis of insulin-induced lipodystrophy remains obscure. Among various proposed mechanisms, immune complex–mediated tissue damage is the most important. It has been previously reported that there is infiltration of inflammatory cells, presence of antigen-antibody complex, and deposition of immunoglobulin M with complement component 3 or fibrin-fibrinogen in the walls of dermal blood vessels in affected areas (1). There is also increased local production of inflammatory cytokines such as tumor necrosis factor α and interleukin-6 by T cells and monocytes. De-differentiation of adipocytes in the subcutaneous tissue occurs, resulting in lipoatrophy (4). Improvement of lipoatrophy with local dexamethasone injection further substantiates this hypothesis (5). Some investigators have reported that lipoatrophic areas are infiltrated by an increased number of mast cells. Degranulation of mast cells mediates the local inflammatory process. Mast cell stabilizer cromolyn sodium, when given topically, resulted in significant improvement (2).
Lipohypertrophy may be the result of local anabolic action of insulin on adipocytes, promoting fat and protein synthesis. However, other mechanisms such as reuse of needles and trauma from frequent injections at the same site have also been postulated (6).
Anti-insulin antibodies have an important role in insulin pharmacokinetics and immune-mediated adverse effects such as lipodystrophy. Antibody production is influenced by several factors such as genetics, degree of purity of the insulin, species of insulin origin, and mode of insulin administration. The antibodies are usually of immunoglobulin G– or immunoglobulin E– class antibodies. Although animal insulin has been associated with higher titers of antibody production, it has been observed that highly purified human recombinant insulin can also produce anti-insulin antibodies. It is hypothesized that lipoatrophy is the result of antigen antibody complex formation (7). It is also important to note that anti-insulin antibody levels are positively correlated with lipohypertrophy (8).
Apart from related cosmetic concerns, the importance of insulin-induced lipodystrophy lies in alteration of insulin absorption and glycemic variability. Abnormal absorption kinetics from dystrophic areas produce erratic blood glucose levels, leading to unpredictable hypo- and hyperglycemia. Evidence suggests that clearance of insulin from lipohypertrophic areas is significantly delayed (9).
Specific treatment of lipohypertrophy and lipoatrophy is still unavailable. As described above, dexamethasone and cromolyn sodium have been tried in a few patients with variable results. Liposuction has been tried in lipohypertrophy (6). Although a specific susceptibility to insulin-induced lipodystrophy has yet to be uncovered, proper insulin administration technique and rotation of injection sites would be a prudent option to decrease the chances of these complications.
Both of the patients described here had lipoatrophy and lipohypertrophy in different injection sites. After ensuring proper injection technique, including rotation of sites, both had improvement in A1C and glycemic variability. We could not explain the mechanism behind the occurrence of both lipoatrophy and lipohypertrophy in the same patient. However, high-titer anti-insulin antibodies may be responsible. The presence of both lipoatrophy and lipohypertrophy in the same patient using recombinant human insulin is extremely rare and, to the best of our knowledge, has not been reported previously.
Clinical Pearls
Insulin injection sites should be examined in every patient, particularly those who have variable glycemic status.
Proper injection technique and rotation method should be advised to every patient taking insulin.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Reeves WG, Allen BR, Tattersall RB. Insulin-induced lipoatrophy: evidence for an immune pathogenesis. BMJ 1980;280:1500–1503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lopez X, Castells M, Ricker A, Velazquez EF, Mun E, Goldfine AB. Human insulin analog–induced lipoatrophy. Diabetes Care 2008;31:442–444 [DOI] [PubMed] [Google Scholar]
- 3.Hauner H, Stockhamp B, Haastert B. Prevalence of lipohypertrophy in insulin treated diabetic patients and predisposing factors. Exp Clin Endocrinol Diabetes 1996;104:106–110 [DOI] [PubMed] [Google Scholar]
- 4.Gepner CA, Bongrand P, Farnarier C. Insulin-induced lipoatrophy in type I diabetes: a possible tumor necrosis factor- α-mediated dedifferentiation of adipocytes. Diabetes Care 1996;19:1283–1285 [DOI] [PubMed] [Google Scholar]
- 5.Kumar D, Miller LV, Mehatalia SD. Use of dexamethasone in treatment of insulin lipoatrophy. Diabetes 1977;26:296–299 [DOI] [PubMed] [Google Scholar]
- 6.Chowdhury TA, Escudier V. Poor glycaemic control caused by insulin induced lipohypertrophy. BMJ 2003;327:383–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Haeften TW. Clinical significance of insulin antibodies in insulin-treated diabetic patients. Diabetes Care 1989;12:641–648 [DOI] [PubMed] [Google Scholar]
- 8.Raile K, Noelle V, Landgraf R, Schwarz HP. Insulin antibodies are associated with lipoatrophy but also with lipohypertrophy in children and adolescents with type 1 diabetes. Exp Clin Endocrinol Diabetes 2001;109:393–396 [DOI] [PubMed] [Google Scholar]
- 9.Young RJ, Hannan WJ, Frier BM, Steel JM, Duncan LJ. Diabetic lipohypertrophy delays insulin absorption. Diabetes Care 1984;7:479–480 [DOI] [PubMed] [Google Scholar]


