Abstract
Introduction
The Helicopter Emergency Medical Service (HEMS) was established for the prehospital trauma care of patients. Improved rescue times and increased coverage areas are discussed as specific advantages of HEMS. We recently found evidence that HEMS exerts beneficial effects on outcomes for severely injured patients. However, it still remains unknown which group of trauma patients might benefit most from HEMS rescue. Consequently, the unique aim of this study was to reveal which patients might benefit most from HEMS rescue.
Methods
Trauma patients (ISS ≥9) primarily treated by HEMS or ground emergency medical services (GEMS) between 2002 and 2012 were analysed using the TraumaRegister DGU. A multivariate regression analysis was used to reveal the survival benefit between different trauma populations.
Results
The study included 52 281 trauma patients. Of these, 68.8% (35 974) were rescued by GEMS and 31.2% (16 307) by HEMS. HEMS patients were more severely injured compared to GEMS patients (ISS: HEMS 24.8±13.5 vs. GEMS 21.7±18.0) and more frequently suffered traumatic shock (SBP sys <90mmHg: HEMS 18.3% vs. GEMS 14.8%). However, logistic regression analysis revealed that HEMS rescues resulted in an overall survival benefit compared to GEMS (OR 0.81, 95% CI [0.75–0.87], p<0.001, Nagelkerke's R squared 0.526, area under the ROC curve 0.922, 95% CI [0.919–0.925]). Analysis of specific subgroups demonstrated that patients aged older than 55 years (OR 0.62, 95% CI [0.50–0.77]) had the highest survival benefit after HEMS treatment. Furthermore, HEMS rescue had the most significant impact after ‘low falls’ (OR 0.68, 95% CI [0.55–0.84]) and in the case of minor severity injuries (ISS 9–15) (OR 0.66, 95% CI [0.49–0.88]).
Conclusions
In general, trauma patients benefit from HEMS rescue with in-hospital survival as the main outcome parameter. Focusing on special subgroups, middle aged and older patients, low-energy trauma, and minor severity injuries had the highest survival benefit when rescued by HEMS. Further studies are required to determine the potential reasons of this benefit.
Introduction
Helicopter emergency medical service (HEMS) has been implemented in the preclinical treatment of trauma patients in diverse countries [1,2]. In some countries (e.g. Germany), HEMS rescue has been incorporated in a dense nationwide network of emergency medical services [1–5]. Nevertheless, the potentially beneficial effects of HEMS on patients' outcomes and cost efficiency are still controversial [1,3,6,7]. In this context, several disadvantages of HEMS such as the high financial burden [8] and the limited availability of HEMS, due to weather conditions or darkness have been reported [1,3,9]. However, presumable advantages compared to ground emergency medical services (GEMS) have also been described. In this context, HEMS is expected to facilitate rapid transport due to an increased transportation velocity [10]. Furthermore, HEMS medical crew members are supposed to be more experienced in trauma management, improving preclinical treatment of trauma patients [10,11] which might also result in improved triage and transportation to a specialist trauma centre thereby minimising inter-hospital transfers [12]. Also, the HEMS-related effects on posttraumatic mortality have been discussed controversially. While no significant effects of HEMS on mortality were found in some analyses [11,13,14], recent studies partly based on huge nationwide databases reported an independent benefit towards survival [1,6,15–18]. According to a current Cochrane Database analysis, these divergent results might be due to methodological issues, the considerable heterogeneity of health care systems (e.g. physician-staffed HEMS) and differences in the included study populations. In this context, it might be postulated that factors like demographic data and trauma mechanisms as well as injury severity or distribution might also affect the potential merits of HEMS rescue [7]. Two previous studies discussing these issues have been published using the German trauma registry [1,5]. As we have already demonstrated a significant benefit of HEMS rescue in Germany by these studies, the purpose of the current investigation was to examine whether age, gender, mode of injury, or injury severity could be used to determine specific trauma patient populations who might benefit explicitly from HEMS rescue.
Materials and Methods
The TraumaRegister DGU
The TraumaRegister DGU of the German Trauma Society (Deutsche Gesellschaft für Unfallchirurgie, DGU) was founded in 1993. The aim of this multi-centre database is anonymous and standardised documentation of severely injured patients.
Data are collected prospectively in four consecutive time phases from the site of the accident until discharge from hospital: A) Pre-hospital phase, B) Emergency room and initial surgery, C) Intensive care unit and D) Discharge. The documentation includes detailed information on demographics (age, gender), injury pattern, comorbidities, pre- and in-hospital management, course in the intensive care unit, relevant laboratory findings including data on transfusions and outcomes for each individual. The inclusion criteria are admission to hospital via emergency room with subsequent ICU/ICM care or reach the hospital with vital signs and die before admission to ICU. The infrastructure for documentation, data management, and data analysis is provided by AUC–Academy for Trauma Surgery (AUC–Akademie der Unfallchirurgie GmbH), a company affiliated to the German Trauma Society. The scientific leadership is provided by the Committee on Emergency Medicine, Intensive Care and Trauma Management (Sektion NIS) of the German Trauma Society. The participating hospitals submit their data anonymously into a central database via a web-based application. Scientific data analysis is approved according to a peer review procedure established by Sektion NIS. The participating hospitals are primarily located in Germany (90%), but a rising number of hospitals in other countries contribute data as well (at the moment from Austria, Belgium, China, Finland, Luxembourg, Slovenia, Switzerland, The Netherlands, and the United Arab Emirates). Currently, approximately 25 000 cases from more than 600 hospitals are entered into the database per year.
Participation in the TraumaRegister DGU is voluntary. For hospitals associated with TraumaNetzwerk DGU, however, the entry of at least a basic data set is obligatory for reasons of quality assurance. Actually, 58% of patients were treated in Level I trauma centres, 33% in Level II centres, and 9% in Level III centres.
This study followed the guidelines of the revised UN declaration of Helsinki in 1975 and its latest amendment in 1996 (42nd general meeting). The study was approved by the internal review board of the Sektion NIS (Sektion Notfall, Intensivmedizin und Schwerverletztenversorgung) of the German Trauma Society (DGU). The present study is in line with the publication guidelines of the TraumaRegister DGU and registered as TR-DGU project ID 2013–033. Furthermore, this study was approved by the institutional ethical review board of the University Hospital Aachen, Pauwelsstraße 30, 52074 Aachen, Germany (No. EK 225/15). There was no need for written informed consent from the participants.
Inclusion criteria
The present study included the following patients from the TR-DGU:
-
-
Treated in a German Level I or II trauma centre
-
-
Date of admission from January 2002 until December 2012
-
-
Transportation to hospital either by physician staffed helicopter (HEMS) or physician staffed ground emergency medical services (GEMS)
-
-
Primary admission from the scene of injury (inter-hospital transfers excluded)
-
-
Early transfer out (<48h) excluded since final outcome not available
-
-
Injury Severity Score (ISS) ≥ 9 points
Injury severity and clinical outcome
The injury distribution was determined according to the Abbreviated Injury Scale (AIS, version 2005) and the overall injury severity was summarised by the Injury Severity Score (ISS) [19]. Furthermore, the New Injury Severity Score (NISS) was determined [20]. In order to assess the severity of traumatic brain injury (TBI), the first pre-hospital Glasgow Coma Scale (GCS) was used in addition to the AIS score [21]. Presence of a severe TBI was assumed if the AIS head score was ≥ 3 points and/ or GCS was ≤ 8 points.
The incidence of haemorrhagic shock in the preclinical setting was defined by a systolic blood pressure (SBP) ≤90mmHg.
The clinical course included the duration of mechanical ventilation as well as the length of intensive care unit and overall hospital stay [1]. Complications during hospital treatment included sepsis and organ failure [1]. The diagnosis of sepsis was made according to the criteria of the ACCP/SCCM consensus conference committee [22,23]. Organ function status was evaluated according to the Sequential Organ Failure Assessment (SOFA) score [24]. With three or more points an organ function was considered as failure while multiple organ dysfunction syndrome (MODS) was defined as simultaneous failure of at least two organs.
On-scene treatment and mission times
Six different procedures of on-scene treatment were documented in the TR-DGU and analysed in order to evaluate potential differences in management between HEMS and GEMS. These procedures were intubation, insertion of a chest tube, application of vasopressors or sedatives, volume infusion, and cardio-pulmonary resuscitation (CPR). As HEMS and GEMS physicians are trained standardly in ATLS (Advanced Trauma Life Support) and PHTLS (Prehospital Trauma Life Support) in Germany, HEMS and GEMS physicians can be argued as comparably trained in these on-scene procedures and the prehospital management of trauma patients in general.
In addition, mission duration was defined as the time from accident until arrival at the emergency room.
Statistics
Incidences are presented with counts and percentages while continuous values are presented as mean, standard deviation (SD) and median (MD). Due to the large sample size, even minor differences between the groups would become statistically significant, formal statistical testing was largely avoided. Selected differences were evaluated using the Chi-squared test for counts, and Mann-Whitney’s U-test for continuous variables. The interpretation of results, however, should focus on clinically relevant differences rather than on significant p-values.
Multivariate logistic regression analysis with in-hospital mortality as the dependent variable was performed in order to adjust for confounding variables. Besides the mode of transportation, the following variables were included as confounders in the statistical model: Time of treatment, ISS, age, gender, unconsciousness (GCS ≤ 8), AIS head (four and five points), shock (prehospital systolic blood pressure ≤ 90 mmHg), intubation, type of injury (blunt/ penetrating), mechanism of injury, level of care of the target hospital, and time of day (daytime/night). Results were reported as odds ratios with 95% confidence intervals (95% CI).
Subsequently, the logistic regression analysis was repeated in subgroups of patients using only the significant confounders identified in the first model as confounding independent predictor variables. From these subgroup analyses only the odds ratio (OR) of the HEMS (relative to GEMS) was reported, with 95% CI.
The data were analysed using the Statistical Package for the Social Sciences (SPSS; version 22; IBM Inc., Somers, NY, USA).
Results
Demographic data
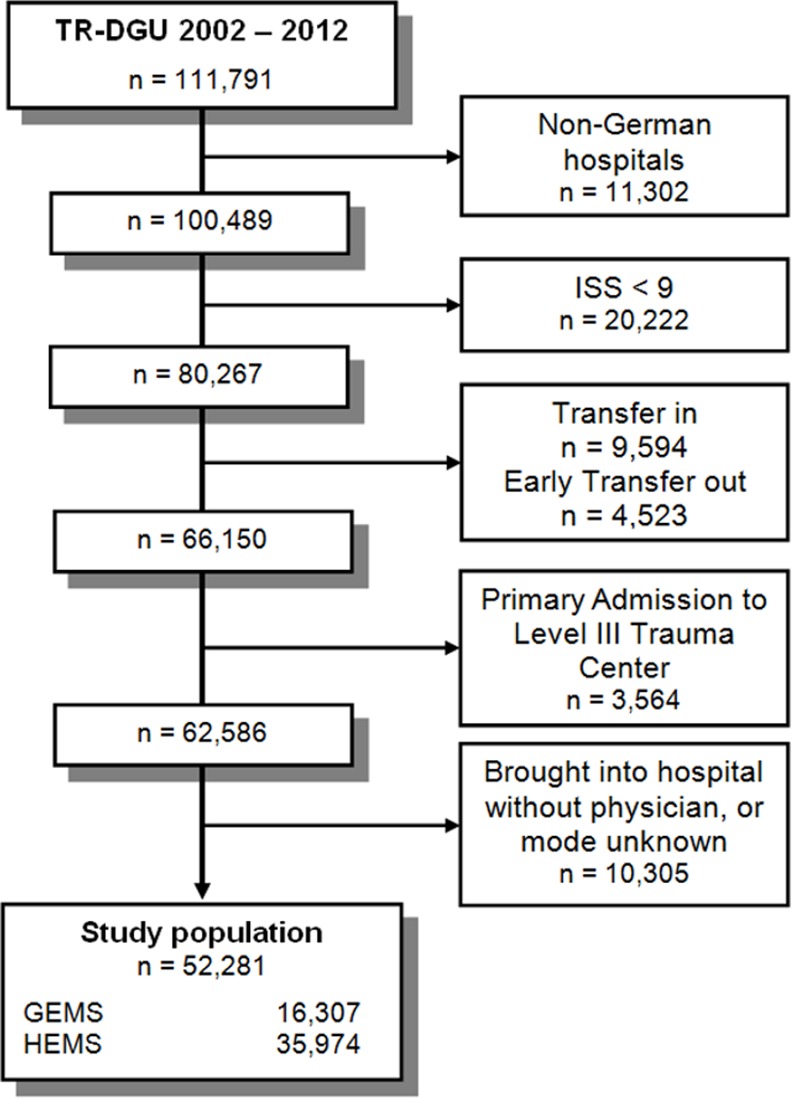
A total of 52 281 trauma patients were included in the present study (Fig 1). Of these, 68.8% (n = 35 974) were rescued by GEMS and 31.2% (n = 16 307) by HEMS. The mean age for all patients was 46.6 ± 21.4 years, and 72.2% were males. Patients transported by HEMS were younger (HEMS: 43.9 ± 20.3 years; GEMS: 47.8 ± 21.8) and more often of male gender (HEMS: 75.0%; GEMS: 70.9%). Overall, 69.3% (n = 36 212) of patients were transported to a Level I trauma centre, 30.7% (n = 16 069) to a Level II trauma centre.
Fig 1. Study flow chart illustrating the selection of patients.
Cause of injury, injury distribution and on-scene treatment
Overall, 60.1% of included patients suffered from traffic accidents. HEMS patients suffered more often from high energy trauma, mainly road traffic accidents by car and motorcycle (Table 1). A total of 67.9% (n = 35 476) of all patients had an ISS ≥16 points. Patients rescued by HEMS sustained a higher injury severity (Table 2) associated with an increased incidence of on-scene traumatic shock (HEMS: 18.3% vs. GEMS: 14.8%).
Table 1. Trauma mechanism.
| All patients | HEMS | GEMS | |
|---|---|---|---|
| Traffic—Car | 13,811 | 33.4% | 25.3% |
| Traffic—Motorbike | 7,525 | 21.4% | 12.3% |
| Traffic—Bicycle | 4,053 | 7.5% | 8.5% |
| Traffic—Pedestrian | 4,000 | 4.4% | 9.7% |
| High fall > 3m | 8,828 | 16.8% | 18.2% |
| Low fall < 3m | 7,351 | 8.6% | 17.6% |
| Others | 4,064 | 7.9% | 8.3% |
Table 2. Demographics, injury distribution and injury severity.
| HEMS | GEMS | |
|---|---|---|
| Age (years) | 43.9 ± 20.3 | 47.8 ± 21.8 |
| Gender (male) | 75.0% | 70.9% |
| Head | 45.6% | 41.7% |
| Chest | 52.3% | 45.2% |
| Abdomen | 16.0% | 13.5% |
| Extremities | 37.8% | 31.5% |
| ISS (mean ± SD) [median] | 24.8 ± 13.5 [22.0] | 21.7 ± 13.3 [18.0] |
| NISS (mean ± SD) [median] | 30.5 ± 15.7 [27.0] | 27.1 ± 14.9 [22.0] |
| ISS ≥ 16 | 74.5% | 64.8% |
| 24-hours mortality | 7.6% | 7.0% |
| Overall mortality | 14.2% | 13.3% |
Patients treated by GEMS more often had isolated traumatic brain injuries (TBI) (HEMS: 9.6% vs. GEMS: 13.7%), while the incidence of TBI in severe trauma patients was higher in HEMS rescues (HEMS: 45.9% vs. GEMS: 40.0%).
Helicopter rescue teams performed more on-scene interventions (Table 3). Furthermore, a prolonged overall mission duration (HEMS: 76.6 ± 28.2 min. vs. GEMS: 60.7 ± 26.7 min.) and a longer on-scene time (HEMS: 37.0 ± 20.4 min. vs. GEMS: 28.0 ± 16.0 min.) compared to GEMS was observed with HEMS treatment.
Table 3. On-scene interventions.
| On-scene management | HEMS | GEMS |
|---|---|---|
| Intubation | 61.5% | 31.6% |
| Chest tube insertion | 9.0% | 2.8% |
| Application of vasopressors | 11.3% | 7.3% |
| Application of sedatives | 87.2% | 71.5% |
| Volume infusion | 95.6% | 91.5% |
| Cardio-pulmonary resuscitation | 3.0% | 3.2% |
Posttraumatic complications, clinical treatment and outcomes
Evaluating the in-hospital clinical course, an increased incidence of multiple organ dysfunction syndrome (MODS) (HEMS: 30.1% vs. GEMS: 23.1%) and sepsis (HEMS 8.3% vs. GEMS 6.1%) was revealed for HEMS patients. In these patients, the duration of mechanical ventilation (HEMS: 6.4 ± 10.8 days vs. GEMS: 4.0 ± 8.7 days), ICU treatment (HEMS: 10.3 ± 13.2 days vs. GEMS: 7.5 ± 11.2 days) and overall length of stay (HEMS: 25.2 ± 26.6 days vs. GEMS: 19.6 ± 19.2 days) were also increased. Overall in-hospital mortality was 13.5% (n = 7 084), with 14.2% patients deceased after HEMS rescue and 13.3% after GEMS rescue.
Outcome measurement and subgroup analysis
According to the logistic regression model, HEMS rescues resulted in a significant overall mean survival benefit compared to GEMS (OR 0.81, 95% CI [0.75–0.87], p<0.001), Nagelkerke's R squared 0.526, area under the ROC curve 0.922, 95% CI [0.919–0.925]). This result is adjusted for other independent predictors of survival such as injury severity, the presence of a severe TBI, a shock in the preclinical setting, penetrating trauma, and the level of care of the treating hospital (Table 4).
Table 4. HEMS rescue as independent survival predictor (n = 52,006). Only significant factors are presented.
| Predictor towards mortality | Regression coefficient | Odds Ratio | 95% CI | p-value |
|---|---|---|---|---|
| HEMS | -0.217 | 0.805 | 0.746–0.868 | <0.001 |
| Injury Severity (NISS, per point) | 0.053 | 1.054 | 1.051–1.057 | <0.001 |
| Severe Traumatic Brain Injury (AIS ≥ 5) | 0.864 | 2.372 | 2.159–2.606 | <0.001 |
| Penetrating trauma | 0.375 | 1.455 | 1.240–1.707 | <0.001 |
| Shock (SBP ≤ 90mmHg) | 0.740 | 2.097 | 1.933–2.274 | <0.001 |
| Hospital Level of Care (Level II) | 0.112 | 1.118 | 1.034–1.209 | 0.005 |
The impact of HEMS in different subgroups, compared to the overall survival benefit of HEMS (OR 0.81), should identify trauma patients which benefit most from HEMS rescue in Germany. With respect to demographic aspects, elderly patients aged 55 years and above revealed the strongest survival benefit (Table 5). Regarding the trauma mechanism, HEMS rescue had the most benefit following ‘low falls’ while the outcome in traffic injuries was comparable with GEMS. With respect to the injury severity, major benefits were identified in patients with minor polytrauma (ISS less than 25) (Table 5).
Table 5. Multivariate analysis of HEMS versus GEMS in subgroups of patients.
Instead of the full model only the OR for HEMS is reported which was 0.81 in the whole patient group (Table 4).
| Subgroup | n | Odds Ratio for HEMS | 95% CI |
|---|---|---|---|
| 1–15 years | 1,919 | 1.07 | 0.63–1.81 |
| 16–54 years | 31,577 | 0.90 | 0.80–1.00 |
| 55–64 years | 6,177 | 0.62 | 0.50–0.77 |
| 65–74 years | 5,843 | 0.74 | 0.62–0.89 |
| >74 years | 6,490 | 0.72 | 0.61–0.85 |
| Car accident | 13,744 | 0.93 | 0.80–1.08 |
| Motorcycle accident | 7,489 | 0.95 | 0.74–1.20 |
| Bicycle accident | 4,030 | 1.08 | 0.83–1.42 |
| Pedestrian accident | 3,984 | 0.77 | 0.58–1.03 |
| High fall | 8,772 | 0.82 | 0.68–1.00 |
| Low falls | 7,317 | 0.68 | 0.55–0.84 |
| ISS 9–15 | 16,732 | 0.66 | 0.49–0.88 |
| ISS 16–24 | 15,950 | 0.73 | 0.61–0.88 |
| ISS 25–33 | 10,208 | 0.78 | 0.68–0.89 |
| ISS ≥34 | 9,116 | 0.90 | 0.80–1.01 |
| Traumatic brain injury (AIS ≥3) | 22,322 | 0.83 | 0.76–0.90 |
| Chest trauma (AIS ≥3) | 24,665 | 0.83 | 0.75–0.92 |
| Abdomen trauma (AIS ≥3) | 7,413 | 0.90 | 0.76–1.07 |
| Pelvic trauma (AIS ≥3) | 9,695 | 0.82 | 0.70–0.97 |
| On-scene CPR | 1,639 | 0.84 | 0.63–1.13 |
Discussion
Since its introduction, the outcome benefit of HEMS rescue in trauma patients has been discussed controversially. Decisions for initiation of preclinical treatment and transportation of trauma patients by HEMS rescue are still not evidence based [7]. Furthermore, the significance of potential risks and benefits of HEMS treatment remain unclear [25]. The partly divergent results might be caused by the methodological weakness of some studies, the considerable heterogeneity of health care systems (e.g. physician-staffed HEMS), and different study methodologies [7]. Based on the beneficial effects of HEMS rescue observed in our previous study [1], we aimed to identify specific subgroups of trauma patients which might particularly benefit from HEMS rescue. This analysis was again based on one of the largest databases of trauma patients (TraumaRegister DGU). The main results might be summarised as follows:
In general, almost all subgroups of trauma patients benefit from HEMS rescue with in-hospital survival as the main outcome parameter (OR 0.81, 95% CI [0.75–0.87], p<0.001).
Patients treated by HEMS differed significantly in terms of age, trauma mechanism, injury distribution, injury severity, and on-scene trauma management compared to GEMS patients.
Elderly patients with low energy trauma had the greatest benefit from HEMS compared to GEMS.
In-hospital mortality has uniformly been suggested to represent the most important end-point outcome when analysing the impact of HEMS-associated preclinical care for multiple trauma patients [1,3,6,7,11–13]. In accordance with various other investigations based on large databases [6,16,26], we also found a beneficial effect of HEMS on posttraumatic mortality. This is in line with the results of Abe et al. who analysed the Japanese Trauma Databank [26]. The authors found an adjusted survival benefit of physician staffed HEMS with an odds ratio of 1.23. Furthermore, patients treated by helicopter differed from GEMS patients in terms of age, trauma mechanism, injury distribution and injury severity, and on-scene trauma management comparable to results of the present study. In 2010, Brown et al. analysed the National Trauma Databank comparing 41 987 HEMS and 216 400 GEMS patients [16]. The authors adjusted for injury severity, age, gender, injury mechanism, vital signs, level of trauma centre, and urgency of operation. Again, HEMS was associated with an improved survival similar to the effect reported in this study. The largest registry study with a study population of approximately 230 000 patients was currently performed by Galvagno et al. [6]. After adjustment for several confounding factors and a variance calculation to control for clustering by trauma centre, helicopter transport was associated with a lower mortality in Level I (OR 0.88) and Level II trauma centres (OR 0.86). Although this statistical aspect was argued to represent more valid data compared to previous studies [6], the comparison of differently trained rescue teams represents a potential limitation which has also previously been discussed [1,3,13,14]. In the present study, the presumable confounding factor of different rescue teams can be neglected due to the fact that exclusively physician staffed rescue teams were compared. However, other studies did not find a positive impact of HEMS transportation on outcomes in trauma patients [11,13,14,27]. In a current Cochrane Review, these divergent results led to the conclusion that the relevance of potentially beneficial effects of HEMS need further clarification. It has been suggested that the considerable heterogeneity of study populations and study methodologies in the current literature might be significant reasons for this diversity of study results [7].
We therefore performed an analysis of specific subgroups based on demographic data, injury mechanism as well as injury severity and distribution. Beside the overall benefit of HEMS rescue in almost all subgroups of trauma patients, we particularly found the most pronounced survival benefit in the group of elderly patients, in patients with low-energy trauma and in the group with a lower injury severity. This aspect demands a critical reflection due to the steadily increasing average age of trauma patients. As geriatric trauma patients have been identified as the fastest growing population in trauma centres with an estimation of 40% by the year 2050 [28–30], the challenge to prevent mortality in this trauma population will also involve the prehospital management in HEMS and GEMS rescue. Analysing potential trauma mechanisms in young and older patients, low-level falls as the major cause for low-energy trauma have been identified as the predominant cause of injury in patients aged over 65 years [30,31]. In this respect, Sterling et al. demonstrated that almost 50% of patients older than 65 years suffered from falls compared to only 7% in the younger generation [32]. Nevertheless, road traffic accidents represent the second most common mechanism of injury of elderly patients [33,34]. In accordance with the different trauma mechanisms between young and older patients, differences towards the treatment strategies were revealed [35,36]. Peschman et al. demonstrated that patients older than 65 years were more likely to be admitted to hospital compared to younger patients [35]. Despite this increased rate of hospital admission, older patients were more frequently triaged to non-trauma centres despite a proven favourable outcome in specialist trauma centres [31,33,36]. In this context, it was demonstrated that elderly trauma patients injured in traffic accidents had a lower mortality compared to those after low-energy trauma even when adjusted for injury severity and comorbidities [31,34]. This was explained by a longer delay in triage, and a longer time between the assessment and admission after falls when compared to traffic accidents [31,34]. Focusing on the presented survival rates in helicopter rescue in this study, the preferred admission to Level I trauma centres in HEMS rescue could be argued to be one potential reason for the improved survival in older patients. Furthermore, direct admission to hospital was guaranteed due to the inclusion criteria of this study.
Beside the impact of trauma care levels, further independent mortality risk factors in older trauma patients have been evaluated. Hranjek et al. found that the injury severity, blood pressure and mechanical ventilation were independent predictors of mortality in older trauma patients [37]. Even a minor injury severity between 16 and 19 ISS points had an odds ratio towards mortality of 2.4 in these patients [37]. Furthermore, hypotension has been observed in 20% of elderly trauma patients, and was associated with an increase of the mortality risk from 12% to 35% [36]. Consequently, an early and aggressive treatment strategy for older trauma patients has been noted by several studies [31,36,38]. In conclusion, the demonstrated improved survival in HEMS rescue might have been determined by the extended on-scene treatment by HEMS compared to GEMS and the direct hospital admission in this study.
In summary, elderly patients benefit from both, aggressive on-scene treatment and resuscitation as well as an early admission to a trauma centre with geriatric trauma experience regardless of the trauma mechanism. We suggest in this study that these aspects were guaranteed in HEMS rescue, influencing the impact of HEMS. Beside the HEMS rescue as a transportation platform, on-scene management and preferred admission to Level I trauma centres might have improved the survival in consequence.
The present study has limitations that need to be recognised. Although databank analyses include a large number of patients, their validity might be restricted due to detection of minor statistical differences without mandatory clinical relevance [1]. We therefore decided to present the descriptive variables of our study populations without statistical significances. Furthermore, we had to exclude approximately 9% of all patients due to missing data regarding the transportation mode. Although this might have influenced our results, we expect this bias to be of minor effect. In comparison, Galvagno excluded 40% due to missing disposition information [6]. Another bias could be expected by factors not evaluated by the databank (weather conditions, transportation distances, etc.). Further criticism could be mentioned regarding the inclusion criterion of an ISS ≥9 points. We decided to use the inclusion criterion of ISS ≥9 because many patients with an ISS between 9 and 15 were transported by helicopter. Little information is available regarding minor polytrauma treated by HEMS [39]. In addition, including patients with an ISS <16 has previously been established [1,40]. This study did not intend to evaluate the potential reason for the outcome benefit in HEMS rescue. Therefore, we did not analyse the influence of on-scene treatment procedures and mission times towards outcome although we provided these data in order to guarantee comparability to further studies in this field. In this respect, intubation especially as an on-scene procedure should be argued critically considering the reasons (Traumatic Brain Injury and unconsciousness, analgesia, etc.). Another important aspect should be considered. In general, patients under CPR are not transported by HEMS due to the small space that is available during HEMS transport. Patients transported by HEMS must have already returned to spontaneous circulation.
Conclusions
In summary, trauma patients benefit from HEMS rescue with in-hospital survival as a main outcome parameter. Analysing different subgroups, older patients, low-energy trauma, and minor injury severity had the most pronounced survival benefit when rescued by HEMS. An aggressive on-scene treatment, a direct and early hospital admission, and preferred admission to Level I trauma centres might have influenced the survival in older patients in the case of HEMS rescue. Nevertheless, further studies are required to determine the potential reasons for this benefit.
Acknowledgments
This manuscript is part of the doctoral thesis of Mr. Magnus Frey.
Abbreviations
- AIS
Abbreviated Injury Scale
- AUC
AUC—Akademie der Unfallchirurgie GmbH / AUC—Academy for Trauma Surgery
- CI
Confidence interval
- CPR
Cardiopulmonary resuscitation
- DGU
German Trauma Society
- GCS
Glasgow Coma Scale
- GEMS
Ground emergency medical services
- HEMS
Helicopter emergency medical services
- ICU
Intensive Care Unit
- ISS
Injury Severity Score
- m
Meter (unit)
- min.
Minute (unit)
- MODS
Multiple Organ Dysfunction Syndrome
- OR
Odds ratio
- SBP
Systolic blood pressure
- SD
Standard deviation
- SOFA
Sequential Organ Failure Assessment
- SPSS
Statistical Package for the Social Sciences
- TR-DGU
TraumaRegister DGU
Data Availability
Data is provided by the TraumaRegister DGU. Data are available from the TraumaRegister DGU for researchers who meet the criteria for access to confidential data.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Andruszkow H, Lefering R, Frink M, Mommsen P, Zeckey C, Rahe K, et al. (2013) Survival benefit of helicopter emergency medical services compared to ground emergency medical services in traumatized patients. Crit Care 17: R124 10.1186/cc12796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sturm JA, Pape HC, Dienstknecht T (2013) Trauma care in Germany: an inclusive system. Clin Orthop Relat Res 471: 2912–2923. 10.1007/s11999-013-2967-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andruszkow H, Frink M, Zeckey C, Krettek C, Hildebrand F, Mommsen P (2012) Merits and capabilities of helicopter emergency medical service (HEMS) in traumatized patients. Technology and health care: official journal of the European Society for Engineering and Medicine 20: 435–444. [DOI] [PubMed] [Google Scholar]
- 4.Schweigkofler U, Reimertz C, Lefering R, Hoffmann R, TraumaRegister DGU (2014) [Importance of air ambulances for the care of the severely injured.]. Unfallchirurg. [DOI] [PubMed] [Google Scholar]
- 5.Andruszkow H, Hildebrand F, Lefering R, Pape HC, Hoffmann R, Schweigkofler U (2014) Ten years of helicopter emergency medical services in Germany: Do we still need the helicopter rescue in multiple traumatised patients? Injury 45 Suppl 3: S53–58. 10.1016/j.injury.2014.08.018 [DOI] [PubMed] [Google Scholar]
- 6.Galvagno SM Jr., Haut ER, Zafar SN, Millin MG, Efron DT, Koenig GJ Jr., et al. (2012) Association between helicopter vs ground emergency medical services and survival for adults with major trauma. JAMA: the journal of the American Medical Association 307: 1602–1610. 10.1001/jama.2012.467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galvagno SM Jr., Thomas S, Stephens C, Haut ER, Hirshon JM, Floccare D, et al. (2013) Helicopter emergency medical services for adults with major trauma. Cochrane Database Syst Rev 3: CD009228 10.1002/14651858.CD009228.pub2 [DOI] [PubMed] [Google Scholar]
- 8.Taylor C, Jan S, Curtis K, Tzannes A, Li Q, Palmer C, et al. (2012) The cost-effectiveness of physician staffed Helicopter Emergency Medical Service (HEMS) transport to a major trauma centre in NSW, Australia. Injury 43: 1843–1849. 10.1016/j.injury.2012.07.184 [DOI] [PubMed] [Google Scholar]
- 9.Westhoff J, Hildebrand F, Grotz M, Richter M, Pape HC, Krettek C (2003) Trauma care in Germany. Injury 34: 674–683. [DOI] [PubMed] [Google Scholar]
- 10.Butler DP, Anwar I, Willett K (2010) Is it the H or the EMS in HEMS that has an impact on trauma patient mortality? A systematic review of the evidence. Emergency medicine journal: EMJ 27: 692–701. 10.1136/emj.2009.087486 [DOI] [PubMed] [Google Scholar]
- 11.Biewener A, Aschenbrenner U, Rammelt S, Grass R, Zwipp H (2004) Impact of helicopter transport and hospital level on mortality of polytrauma patients. The Journal of trauma 56: 94–98. [DOI] [PubMed] [Google Scholar]
- 12.Plevin RE, Evans HL (2011) Helicopter transport: help or hindrance? Current opinion in critical care. [DOI] [PubMed] [Google Scholar]
- 13.Bulger EM, Guffey D, Guyette FX, MacDonald RD, Brasel K, Kerby JD, et al. (2012) Impact of prehospital mode of transport after severe injury: a multicenter evaluation from the Resuscitation Outcomes Consortium. The journal of trauma and acute care surgery 72: 567–573; discussion 573–565; quiz 803. 10.1097/TA.0b013e31824baddf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Jongh MA, van Stel HF, Schrijvers AJ, Leenen LP, Verhofstad MH (2012) The effect of Helicopter Emergency Medical Services on trauma patient mortality in the Netherlands. Injury 43: 1362–1367. 10.1016/j.injury.2012.01.009 [DOI] [PubMed] [Google Scholar]
- 15.Thomas SH, Cheema F, Wedel SK, Thomson D (2002) Trauma helicopter emergency medical services transport: annotated review of selected outcomes-related literature. Prehosp Emerg Care 6: 359–371. [DOI] [PubMed] [Google Scholar]
- 16.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML (2010) Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. The Journal of trauma 69: 1030–1034; discussion 1034–1036. 10.1097/TA.0b013e3181f6f450 [DOI] [PubMed] [Google Scholar]
- 17.Stewart KE, Cowan LD, Thompson DM, Sacra JC, Albrecht R (2011) Association of direct helicopter versus ground transport and in-hospital mortality in trauma patients: a propensity score analysis. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine 18: 1208–1216. [DOI] [PubMed] [Google Scholar]
- 18.Sullivent EE, Faul M, Wald MM (2011) Reduced mortality in injured adults transported by helicopter emergency medical services. Prehosp Emerg Care 15: 295–302. 10.3109/10903127.2011.569849 [DOI] [PubMed] [Google Scholar]
- 19.Baker SP, O'Neill B, Haddon W Jr., Long WB (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. The Journal of trauma 14: 187–196. [PubMed] [Google Scholar]
- 20.Lavoie A, Moore L, LeSage N, Liberman M, Sampalis JS (2004) The New Injury Severity Score: a more accurate predictor of in-hospital mortality than the Injury Severity Score. The Journal of trauma 56: 1312–1320. [DOI] [PubMed] [Google Scholar]
- 21.Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. A practical scale. Lancet 2: 81–84. [DOI] [PubMed] [Google Scholar]
- 22.Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101: 1644–1655. [DOI] [PubMed] [Google Scholar]
- 23.Bone RC, Sprung CL, Sibbald WJ (1992) Definitions for sepsis and organ failure. Critical care medicine 20: 724–726. [DOI] [PubMed] [Google Scholar]
- 24.Vincent JL, de Mendonca A, Cantraine F, Moreno R, Takala J, Suter PM, et al. (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on "sepsis-related problems" of the European Society of Intensive Care Medicine. Critical care medicine 26: 1793–1800. [DOI] [PubMed] [Google Scholar]
- 25.Thomas SH, Brown KM, Oliver ZJ, Spaite DW, Lawner BJ, Sahni R, et al. (2014) An Evidence-based Guideline for the air medical transportation of prehospital trauma patients. Prehosp Emerg Care 18 Suppl 1: 35–44. 10.3109/10903127.2013.844872 [DOI] [PubMed] [Google Scholar]
- 26.Abe T, Takahashi O, Saitoh D, Tokuda Y (2014) Association between helicopter with physician versus ground emergency medical services and survival for adults with major trauma in Japan. Crit Care 18: R146 10.1186/cc13981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Talving P, Teixeira PG, Barmparas G, DuBose J, Inaba K, Lam L, et al. (2009) Helicopter evacuation of trauma victims in Los Angeles: does it improve survival? World journal of surgery 33: 2469–2476. 10.1007/s00268-009-0185-1 [DOI] [PubMed] [Google Scholar]
- 28.Richmond TS, Kauder D, Strumpf N, Meredith T (2002) Characteristics and outcomes of serious traumatic injury in older adults. J Am Geriatr Soc 50: 215–222. [DOI] [PubMed] [Google Scholar]
- 29.Adams SD, Cotton BA, McGuire MF, Dipasupil E, Podbielski JM, Zaharia A, et al. (2012) Unique pattern of complications in elderly trauma patients at a Level I trauma center. J Trauma Acute Care Surg 72: 112–118. 10.1097/TA.0b013e318241f073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hannan EL, Waller CH, Farrell LS, Rosati C (2004) Elderly trauma inpatients in New York state: 1994–1998. J Trauma 56: 1297–1304. [DOI] [PubMed] [Google Scholar]
- 31.Sampalis JS, Nathanson R, Vaillancourt J, Nikolis A, Liberman M, Angelopoulos J, et al. (2009) Assessment of mortality in older trauma patients sustaining injuries from falls or motor vehicle collisions treated in regional level I trauma centers. Ann Surg 249: 488–495. 10.1097/SLA.0b013e31819a8b4f [DOI] [PubMed] [Google Scholar]
- 32.Sterling DA, O'Connor JA, Bonadies J (2001) Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma 50: 116–119. [DOI] [PubMed] [Google Scholar]
- 33.Pandya SR, Yelon JA, Sullivan TS, Risucci DA (2011) Geriatric motor vehicle collision survival: the role of institutional trauma volume. J Trauma 70: 1326–1330. 10.1097/TA.0b013e31820e327c [DOI] [PubMed] [Google Scholar]
- 34.Spaniolas K, Cheng JD, Gestring ML, Sangosanya A, Stassen NA, Bankey PE (2010) Ground level falls are associated with significant mortality in elderly patients. J Trauma 69: 821–825. 10.1097/TA.0b013e3181efc6c6 [DOI] [PubMed] [Google Scholar]
- 35.Peschman J, Neideen T, Brasel K (2011) The impact of discharging minimally injured trauma patient: does age play a role in trauma admission? J Trauma 70: 1331–1336. 10.1097/TA.0b013e31821693e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Salottolo KM, Mains CW, Offner PJ, Bourg PW, Bar-Or D (2013) A retrospective analysis of geriatric trauma patients: venous lactate is a better predictor of mortality than traditional vital signs. Scand J Trauma Resusc Emerg Med 21: 7 10.1186/1757-7241-21-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hranjec T, Sawyer RG, Young JS, Swenson BR, Calland JF (2012) Mortality factors in geriatric blunt trauma patients: creation of a highly predictive statistical model for mortality using 50,765 consecutive elderly trauma admissions from the National Sample Project. Am Surg 78: 1369–1375. [PMC free article] [PubMed] [Google Scholar]
- 38.Bala M, Willner D, Klauzni D, Bdolah-Abram T, Rivkind AI, Gazala MA, et al. (2013) Pre-hospital and admission parameters predict in-hospital mortality among patients 60 years and older following severe trauma. Scand J Trauma Resusc Emerg Med 21: 91 10.1186/1757-7241-21-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taylor CB, Curtis K, Jan S, Newcombe M (2013) Helicopter emergency medical services (HEMS) over-triage and the financial implications for major trauma centres in NSW, Australia. BMC Emerg Med 13: 11 10.1186/1471-227X-13-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brathwaite CE, Rosko M, McDowell R, Gallagher J, Proenca J, Spott MA (1998) A critical analysis of on-scene helicopter transport on survival in a statewide trauma system. The Journal of trauma 45: 140–144; discussion 144–146. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is provided by the TraumaRegister DGU. Data are available from the TraumaRegister DGU for researchers who meet the criteria for access to confidential data.


