Abstract
Objective:
Alcohol-impaired (AI) driving among college students remains a significant public health concern and may be the single most risky drinking outcome among young adults. Brief motivational interventions (BMIs) have been shown to reduce alcohol use and problems, but their specific efficacy for decreasing AI driving among college students is unknown. The present study analyzed data from three randomized controlled trials of BMI (Murphy et al., 2010: n = 74; Borsari et al., 2012: n = 530; and Martens et al., 2013: n = 365) to evaluate whether BMIs are associated with reductions in AI driving among college student drinkers.
Method:
Participants in all three studies were randomized to BMI or control conditions. Participants reported whether they had driven under the influence (yes/no) following the BMI over the follow-up period.
Results:
Separate binary logistic regression analyses were conducted for each study. For Studies 1 and 2, these analyses revealed that a BMI was significantly associated with reductions in AI driving at the final (6-month and 9-month, respectively) follow-up compared with the control condition. For Study 3, analyses revealed that a single-component BMI focused on the correction of misperceptions of descriptive norms was significantly associated with reductions in AI driving compared with the control group at the final (6-month) follow-up, whereas a single-component BMI focused on the use of protective behavioral strategies was not. Change in drinking level did not mediate the relationship between the condition and the change in AI driving.
Conclusions:
Counselor-administered BMIs that include descriptive normative feedback are associated with significant reductions in AI driving compared with control.
Despite years of prevention efforts, alcohol-impaired (AI) driving among college students remains a significant public health concern. Approximately 30% of college students report past-month AI driving, and 17% of college drinkers report driving after consuming five or more drinks (Hingson, 2009). Among the myriad consequences associated with drinking, AI driving is arguably the most immediately harmful; alcohol was involved in 50% of traffic-related deaths among 18- to 24-year-olds in 2009, and 74% of alcohol-related student deaths result from AI traffic accidents (Hingson et al., 2009; LaBrie et al., 2011). College students are more likely to drive after drinking than their same-aged peers who do not attend college (Paschall, 2003), and heavy episodic drinking (HED; defined as four/five drinks or more per occasion for women/men) is a strong predictor of AI driving among college students (Flowers et al., 2008). Compared with students who did not engage in HED over a 2-week period, students who engaged in three to four HED experiences were eight times more likely to drive after drinking (Paschall, 2003).
Although a variety of policy-based public health interventions (e.g., raising the legal drinking age, lowering the legal blood alcohol concentration driving limit, sobriety checkpoints, zero-tolerance laws, server training) have been implemented to decrease AI driving (Wechsler et al., 2003), the frequency of AI driving remains high, particularly among college students (Hingson et al., 2004). In addition, a number of media campaigns, school-based instructional programs, and peer organizations have been designed specifically to target AI driving among college students, but there is insufficient evidence that these approaches reduce AI driving (Elder et al., 2005). Moreover, the number of drinks students estimate they can consume and still be able to drive safely and legally within an hour is predictive of AI driving (Hingson, 2002). Thus, despite a variety of national and community interventions, many students perceive that there is a “safe” amount to drink before driving, and they may require more intensive, individual-based interventions to reduce AI driving.
The National Highway Traffic Safety Administration (2014) endorses screening and brief intervention as a useful tool for reducing impaired driving behaviors among college students. Brief motivational interventions (BMIs) have shown efficacy for reducing alcohol use and problems in college students and have been widely disseminated (Cronce & Larimer, 2011; Mun et al., 2015; Scott-Sheldon et al., 2014), but few published studies have examined the specific impact of BMIs on AI driving.
BMIs, including the popular Brief Alcohol Screening and Intervention for College Students (BASICS; Dimeff et al., 1999) model, typically consist of one or two individual therapeutic meetings (approximately 50 minutes per session; Carey et al., 2007) delivered in motivational interviewing (MI; Miller & Rollnick, 2012) style by a trained facilitator and include personalized feedback. Personalized feedback is created based on a series of questionnaires completed by students before their BMI session. In addition, although specific feedback components differ by study, a personalized drinking profile, information on social norms, prior alcohol-related consequences experienced by the student (including drinking and driving if endorsed), practical costs (e.g., money spent on alcohol and caloric intake from alcohol), and information on strategies to limit alcohol-related risk are typically included (see Miller et al., 2012). The feedback component is meant to guide a conversation that highlights the student’s risky drinking habits and explores ambivalence around changing drinking patterns. BMIs attempt to identify and correct faulty normative beliefs and highlight consequences of alcohol use (such as AI driving) to increase motivation to change.
Meta-analytic reviews provide evidence that BMIs succeed in reducing alcohol use (frequency, quantity, level of intoxication) and a variety of alcohol-related problems (see Carey et al., 2007, for a review). A specific target of BMIs is to reduce HED experiences, a key risk factor for AI driving, and previous research indicates that BMIs have shown efficacy in reducing the number of HED experiences (Cronce et al., 2012). Throughout the literature, the impact of BMIs on alcohol problems has been examined using an aggregate score of all alcohol problems endorsed. Although such results are useful when examining the impact of interventions on the total number of alcohol consequences experienced, the consequences include a wide range of outcomes, from relatively minor outcomes, such as feeling drowsy after a night out, to subjective reactions to drinking (feeling guilt, regret, or a desire to make a change), to highly significant (and specific) health risk behaviors such as unprotected sex and AI driving.
Only two published studies have examined whether BMIs effectively reduce AI driving among college-aged drinkers. Monti and colleagues (1999) examined whether the use of a BMI, compared with standard care, reduced specific alcohol-related consequences, including AI driving, among 94 adolescents (ages 18–19) treated in an emergency department. At 6-month follow-up, participants in the standard care condition were almost four times more likely to report AI driving than those in the BMI condition. However, less than half of the participants were currently enrolled in college, and the interventions took place in an emergency department following an alcohol-related event, rendering it difficult to determine whether a BMI would be effective when provided specifically to college student drinkers.
Subsequently, Schaus and colleagues (2009) conducted a randomized controlled trial to determine whether a BMI given to drinkers in a college health center significantly decreased drinking level and alcohol problems. Students who reported at least one HED experience in the past 2 weeks were randomized into either a control group (n = 182) or a BMI group (n = 181). Participants in the BMI group received two 20-minute BMI sessions delivered in MI style and a brochure on “alcohol prevention,” whereas participants in the control condition received only a brochure on alcohol prevention. A participant feedback document summarizing overall healthy lifestyle behaviors, personalized drinking information, social norms clarification, alcohol-related consequences (including AI driving), alcohol expectancies, and the use of protective behavioral strategies (PBS) was compiled and used as the source of normative feedback information during the two 20-minute BMI sessions. Participants provided data at baseline and completed follow-ups 3, 6, 9, and 12 months after the intervention. There was a statistically significant reduction in the intervention group in the number of times participants drove after three or more drinks at the 3-month follow-up. However, the intervention group and the control group did not differ significantly in the number of times AI driving occurred at any subsequent follow-up.
Given the dearth of studies examining the impact of BMIs on AI driving and the mixed findings of the prior two studies on the long-term impacts of BMIs on AI driving, it is important to determine the impact of AI driving at long-term follow-ups. The present study extended the existing studies by examining the impact of receiving a BMI on AI driving at the final follow-up of three unique randomized controlled trials.
Although few studies have examined the relative impact of specific feedback components, the results of recent research suggest that providing normative information and information on protective strategies to limit risk may be especially potent feedback elements (Miller et al., 2013). In addition, research has revealed that, when the BMI is highly personalized for the participant, having more BMI components generally improves drinking outcomes (Ray et al., 2014). BMIs typically promote harm-reduction strategies, often referred to as PBS, as a way to minimize or eliminate alcohol-related problems, such as reducing drinking quantity, spacing drinks to lower peak blood alcohol levels, avoiding specific high-risk situations, and planning ahead to arrange a designated driver or alternate transportation. Providing drinkers with personalized feedback on PBS may be particularly helpful in preventing AI driving. To date, no published studies have examined whether a single-component BMI that focuses on enhancing PBS reduces AI driving. In addition, multiple studies have found significant drinking reductions using solely a descriptive normative component (Lewis et al., 2007; Neighbors et al., 2010), suggesting that BMIs focusing specifically on social norms information may be enough to produce reliable changes in drinking. However, no published studies have investigated whether personalized, single-component descriptive social norms BMIs reduce AI driving. To provide the most efficacious alcohol interventions to college students, it is important to identify which specific BMI components are most effective in reducing AI driving among college student drinkers.
With the present study, the authors sought to extend the alcohol-intervention and impaired-driving literature by investigating whether receiving a BMI is associated with reductions in AI driving among college drinkers using data from three published randomized trials evaluating the efficacy of BMIs with college students (Borsari et al., 2012; Martens et al., 2013; Murphy et al., 2010). Although AI driving was examined in each study at baseline and at all follow-ups, the effect of the interventions delivered on this particularly important outcome was not examined, and it is possible that the interventions reduced AI driving even in the absence of an overall effect on drinking or alcohol problems. We hypothesized that, compared with the control groups, students in the active intervention conditions (BMI) would be significantly less likely to report AI driving at final follow-up. Furthermore, the present study sought to determine whether (a) single-component BMIs focused solely on the correction of misperceptions of descriptive norms or (b) use of PBS are associated with reductions in AI driving among college student drinkers.
Method
Description of parent trials
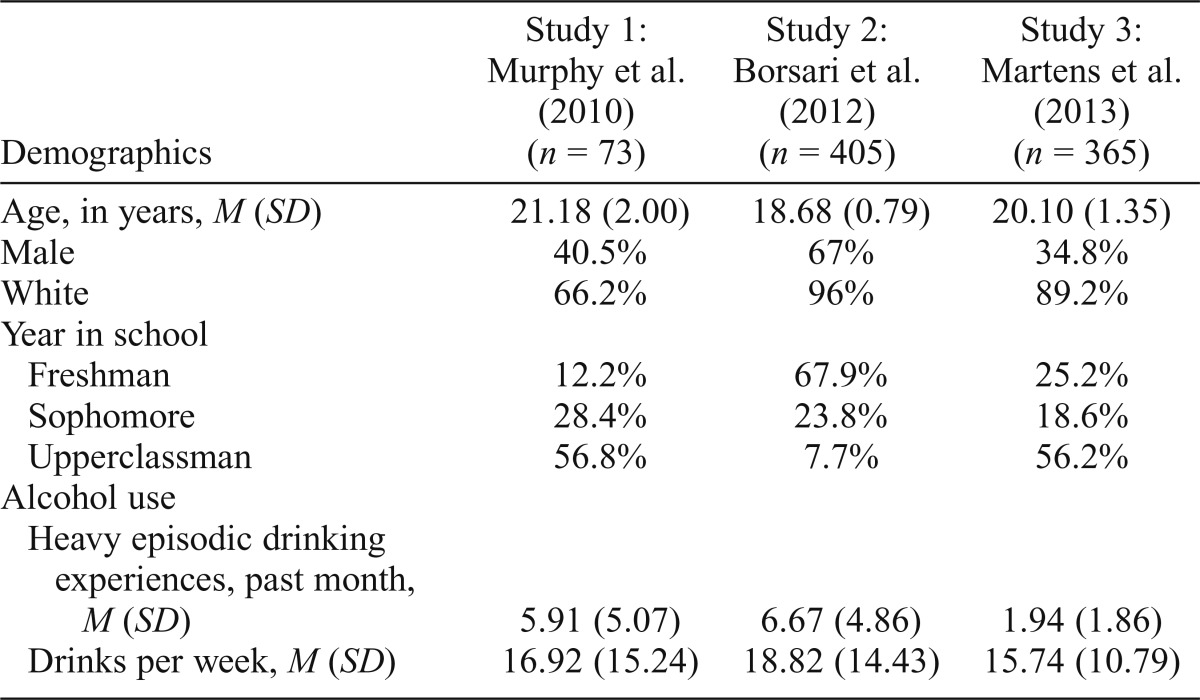
All three studies recruited undergraduate students, and participants received either course credit or monetary compensation for participating. Demographic information about each sample is provided in Table 1.
Table 1.
Descriptive data for each sample
| Demographics | Study 1: | Study 2: | Study 3: |
| Murphy et al. (2010) (n = 73) | Borsari et al. (2012) (n = 405) | Martens et al. (2013) (n = 365) | |
| Age, in years, M (SD) | 21.18 (2.00) | 18.68 (0.79) | 20.10 (1.35) |
| Male | 40.5% | 67% | 34.8% |
| White | 66.2% | 96% | 89.2% |
| Year in school | |||
| Freshman | 12.2% | 67.9% | 25.2% |
| Sophomore | 28.4% | 23.8% | 18.6% |
| Upperclassman | 56.8% | 7.7% | 56.2% |
| Alcohol use | |||
| Heavy episodic drinking experiences, past month, M (SD) | 5.91 (5.07) | 6.67 (4.86) | 1.94 (1.86) |
| Drinks per week, M (SD) | 16.92 (15.24) | 18.82 (14.43) | 15.74 (10.79) |
Study 1 (Murphy et al., 2010).
Participants reported having had at least one HED experience in the past month. Participants were randomized into one of two groups: BMI (n = 38) and Alcohol 101 Plus (n = 35). The groups did not differ on any demographic variables or on the outcome variable at baseline. Participants provided data at baseline and immediately after the intervention and completed follow-ups at 1 and 6 months after the intervention. Results revealed significant decreases in typical weekly drinking and frequency of heavy drinking among those receiving a BMI compared with those receiving a computerized intervention (Alcohol 101 Plus). Of note, only the 1-month follow-up outcomes have been previously published for this study (see Murphy et al., 2010). Because the drinking and driving item used as our outcome variable covered the past 6 months, we elected to focus on the 6-month rather than the 1-month outcomes.
Study 2 (Borsari et al., 2012).
This study evaluated a stepped-care approach with mandated students. Recruitment took place at the university’s Office of Health and Wellness with students who violated the campus alcohol policies. Using a stepped-care treatment approach, all participants who consented received peer-delivered, manualized brief advice and completed a 6-week follow-up (see Borsari et al., 2012). Students who reported four or more HED experiences and/or scored 5 or more on the Young Adult Alcohol Consequences Questionnaire (YAACQ) at the 6-week follow-up were identified as high-risk drinkers and were randomly assigned to either a BMI (n = 211) or assessment only (n = 194). Before the intervention, the two groups did not differ on any demographic variables. Participants provided data at baseline and at 6 weeks and completed follow-ups at 3, 6, and 9 months after the intervention. Results revealed that students who received a BMI significantly reduced their number of alcohol-related problems at the 6-month follow-up compared with students in the assessment-only condition.
Study 3 (Martens et al., 2013).
Students who reported having had at least one HED experience in the past 30 days were randomized into one of three groups: a single-component BMI focused on correcting misperceptions of descriptive norms (n =121), a single-component BMI focused on the use of PBS (n = 111), or Alcohol Education (AE; n = 133). In the single-component BMI focused on correcting misperceptions of descriptive norms condition, participants were provided with information on (a) self-reported alcohol use, (b) perceptions of the typical male and female student alcohol use, and (c) actual alcohol use of typical male and female students. In addition, participants were provided a percentile rank based on their average number of drinks per week. In the single-component BMI focused on the use of PBS condition, participants received feedback on PBS that they had used in the past 2 weeks as well as feedback on PBS that they used “rarely” or “never.” The groups did not differ on any demographic variables or on the outcome variable at baseline, and participants were assessed at baseline, 1 month, and 6 months after the intervention. Results revealed that students in the descriptive norms BMI condition significantly reduced drinking levels at the 6-month follow-up compared with those in the PBS BMI and control conditions.
Measures
AI driving was assessed in all three studies using an identical item from the Brief Young Adult Alcohol Consequences Questionnaire (BYAACQ; Kahler et al., 2005); participants either endorsed or denied “I have driven a car when I knew I had too much to drink to drive safely” in the past 2 (Study 2) or 6 (Studies 1 and 3) months. Single-item measures represent a common modality for assessing this behavior (e.g., Fairlie et al., 2010; Gustin & Simons, 2008; LaBrie et al., 2012; Teeters et al., 2014). The typical number of drinks per week and the change in the number of drinks per week from baseline to follow-up were assessed in all three studies by the Daily Drinking Questionnaire (Collins et al., 1985). Students were asked to estimate the total number of standard drinks they had consumed on each day during a typical week in the past month. The Daily Drinking Questionnaire is frequently used to assess alcohol consumption patterns among college students and is correlated with self-monitoring and retrospective drinking measures (Kivlahan et al., 1990). A separate item was included to assess HED. Students were asked to report how many times they had consumed four or more (if female) or five or more (if male) standard drinks on one occasion during the past month.
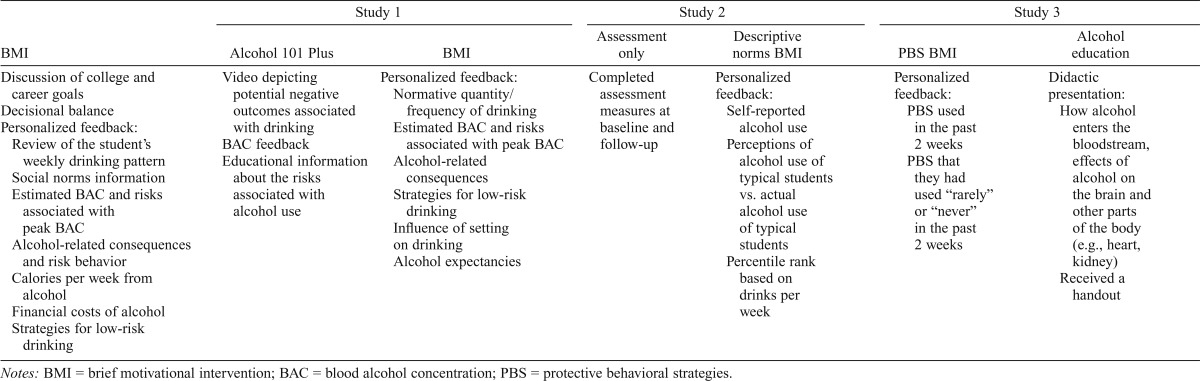
Brief motivational intervention
All three of the studies implemented a BMI conducted in MI style (Miller & Rollnick, 2012) and included a personalized feedback component (specific intervention elements used in each study by condition are provided in Table 2). Of note, AI driving was included as an alcohol-related consequence only if the student endorsed this behavior at baseline. Because BMIs are intended as preventive as well as treatment (reduction) focused, we chose to look at the outcomes of all study participants regardless of whether they endorsed AI driving at baseline. To identify the effect of specific BMI components on alcohol use and problems, the personalized feedback used in Study 3 included either (a) personalized normative information or (b) the use of PBS, both delivered in MI style. Graduate-level clinicians delivered the BMIs in all three studies.
Table 2.
Intervention elements by condition for each study
| BMI | Study 1 |
Study 2 |
Study 3 |
|||
| Alcohol 101 Plus | BMI | Assessment only | Descriptive norms BMI | PBS BMI | Alcohol education | |
| Discussion of college and career goals | Video depicting potential negative outcomes associated with drinking | Personalized feedback: | Completed assessment measures at baseline and follow-up | Personalized feedback: | Personalized feedback: | Didactic presentation: |
| Decisional balance | BAC feedback | Normative quantity/frequency of drinking | Self-reported alcohol use | PBS used in the past 2 weeks | How alcohol enters the bloodstream, effects of alcohol on the brain and other parts of the body (e.g., heart, kidney) | |
| Personalized feedback: | Educational information about the risks associated with alcohol use | Estimated BAC and risks associated with peak BAC | Perceptions of alcohol use of typical students vs. actual alcohol use of typical students | PBS that they had used “rarely” or “never” in the past 2 weeks | Received a handout | |
| Review of the student’s weekly drinking pattern | Alcohol-related consequences | Percentile rank based on drinks per week | ||||
| Social norms information | Strategies for low-risk drinking | |||||
| Estimated BAC and risks associated with peak BAC | Influence of setting on drinking Alcohol expectancies | |||||
| Alcohol-related consequences and risk behavior | ||||||
| Calories per week from alcohol | ||||||
| Financial costs of alcohol | ||||||
| Strategies for low-risk drinking | ||||||
Data analysis plan
Hierarchical logistic regression analyses were conducted separately for each study to determine whether AI driving differed significantly between the groups at the final follow-up (6 or 9 months after the intervention). The dependent variable was AI driving (yes/no). To control for baseline AI driving, AI driving (yes/no) at baseline was entered in Step 1. The treatment condition was entered in Step 2 to evaluate group differences.
To determine whether the change in AI driving was mediated by the change in drinking levels (the change in the average number of drinks per week) versus a more direct effect of the condition on AI driving, a mediational model using bootstrapping, which makes no assumptions about the sampling distribution of the indirect effect (Hayes, 2013), was conducted for each study. Following procedures outlined by Hayes (2013) using the PROCESS Macro, Model 4, analyses were conducted to determine whether the change in drinking level mediates the relationship between the intervention condition and the change in AI driving. A nonparametric bootstrap method of 5,000 samples using a confidence interval (CI) of 95% was used to test the indirect effect of the condition on the change in AI driving through the pathway of change in drinking levels. The change in drinking level was calculated by subtracting the average number of drinks per week at the final follow-up from the average number of drinks per week before the intervention. An alternative model was conducted for each analysis with gender and age as covariates. However, none of the primary findings was affected by these additions.
Results
Study 1 (Murphy et al., 2010)
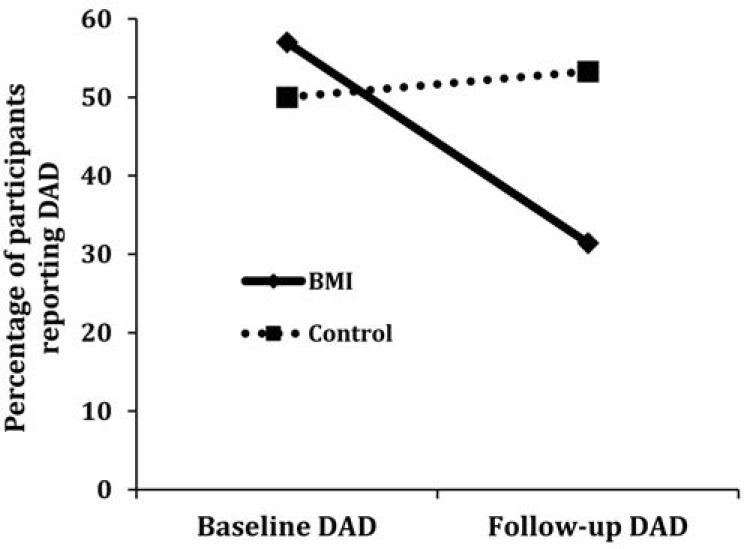
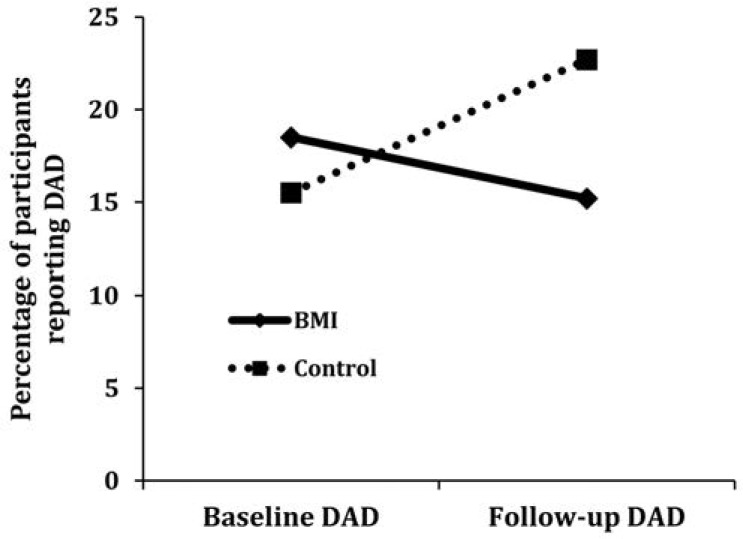
At the 6-month follow-up, the BMI group was significantly less likely to report AI driving (Table 3). In the BMI condition, 20 participants reported AI driving at baseline compared with 11 participants at the 6-month follow-up (45% reduction). In the education control condition, 15 participants reported AI driving at baseline compared with 16 participants at the 6-month follow-up (6.6% increase; Figure 1). Hierarchical logistic regression analyses revealed significant effects for group; participants in the BMI group were 3.71 times less likely to report AI driving at the 6-month follow-up (odds ratio [OR] = 3.71, 95% CI [1.12, 12.25]).
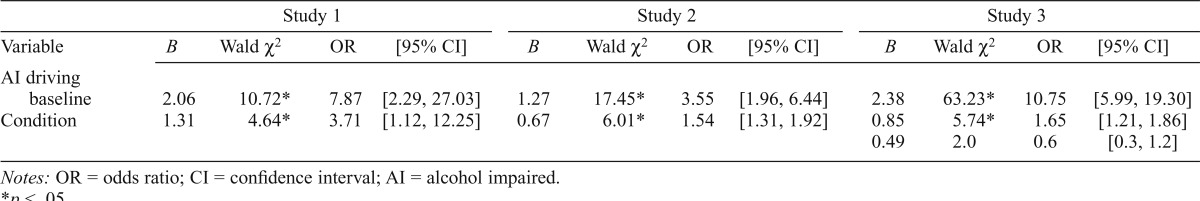
Table 3.
Logistic regression analyses
| Study 1 |
Study 2 |
Study 3 |
||||||||||
| Variable | B | Wald χ2 | OR | [95% CI] | B | Wald χ2 | OR | [95% CI] | B | Wald χ2 | OR | [95% CI] |
| AI driving baseline | 2.06 | 10.72* | 7.87 | [2.29, 27.03] | 1.27 | 17.45* | 3.55 | [1.96, 6.44] | 2.38 | 63.23* | 10.75 | [5.99, 19.30] |
| Condition | 1.31 | 4.64* | 3.71 | [1.12, 12.25] | 0.67 | 6.01* | 1.54 | [1.31, 1.92] | 0.85 | 5.74* | 1.65 | [1.21, 1.86] |
| 0.49 | 2.0 | 0.6 | [0.3, 1.2] | |||||||||
Notes: OR = odds ratio; CI = confidence interval; AI = alcohol impaired.
p < .05.
Figure 1.
Percentage of participants reporting alcohol-impaired driving by condition at baseline and 6-month follow-up in Study 1 (Murphy et al., 2010); DAD = driving after drinking; BMI = brief motivational intervention.
Study 2 (Borsari et al., 2012)
At the 9-month follow-up, the BMI group was significantly less likely to report AI driving (Table 3). In the BMI condition, 39 participants reported AI driving before the intervention compared with 32 participants at the 9-month follow-up (17.9% reduction). In the assessment-only condition, 30 participants reported AI driving before the assessment compared with 44 participants at the 9-month follow-up (46.6% increase; Figure 2). Hierarchical logistic regression analyses revealed significant effects for group; participants in the BMI group were more than 1.54 times less likely to report AI driving at the 9-month follow-up (OR = 1.54, 95% CI [1.31, 1.92]).
Figure 2.
Percentage of participants reporting alcohol-impaired driving by condition at baseline and 9-month follow-up in Study 2 (Borsari et al., 2012); DAD = driving after drinking; BMI = brief motivational intervention.
Study 3 (Martens et al., 2013)
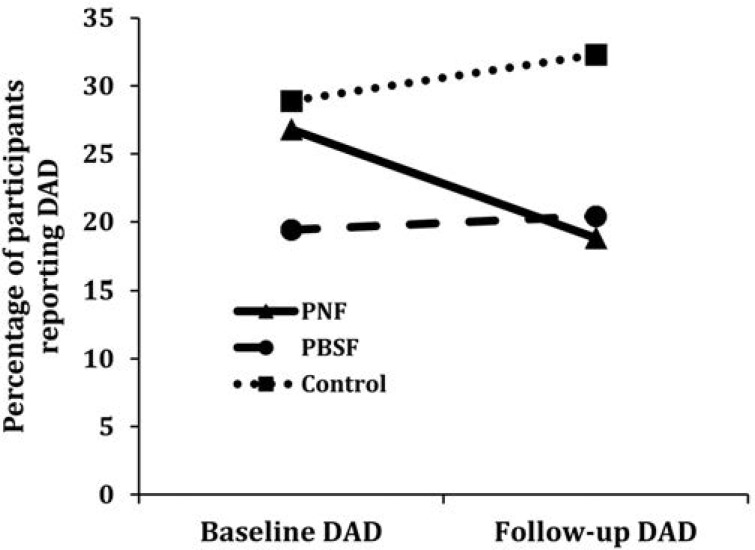
At the 6-month follow-up, the descriptive norms BMI group was significantly less likely than the control group to report AI driving (Table 3). In the descriptive norms condition, 30 participants reported AI driving at baseline compared with 21 participants at the 6-month follow-up (30% reduction). In the PBS BMI condition, 20 participants reported AI driving at baseline compared with 21 participants at the 6-month follow-up (5% increase). In the education control condition, 37 participants reported AI driving at baseline compared with 41 participants at the 6-month follow-up (10.8% increase; Figure 3). Hierarchical logistic regression analyses revealed significant effects for group; participants in the descriptive norms BMI group were 1.65 times less likely than the control group to report AI driving at the 6-month follow-up (OR = 1.65, 95% CI [1.21, 1.86]). No significant differences were found for those in the PBS BMI group compared with the control group.
Figure 3.
Percentage of participants reporting alcohol-impaired driving by condition at baseline and 6-month follow-up in Study 3 (Martens et al., 2013); DAD = driving after drinking; PNF = personalized normative feedback; PBSF = protective behavioral strategies feedback.
Change in typical drinking as a mediator of the relationship between condition and change in alcohol-impaired driving
The change in typical weekly drinking level was significantly associated with the change in AI driving at the final follow-up in Studies 1 and 2 but not in Study 3 (rs = .34, .09, .07 for Studies 1–3, respectively). Confidence intervals of the point estimates of indirect effects that do not include zero are considered significant. These analyses indicated that there was not an indirect effect of the condition on AI driving through the change in drinking level in any of the three studies. Thus, the change in drinking level did not mediate the relationship between the condition and the change in AI driving in Study 1, 95% CI [-.15, .05]; Study 2, 95% CI [-.01, .01]; or Study 3, 95% CI [-.01, 001]. We also tested exploratory models that evaluated the change in past-month HED experiences as a mediator of intervention effects. However, these mediation models were also not significant.
Discussion
Although many studies have examined the impact of BMIs on overall alcohol problems and drinking level, only one previously published study (Schaus et al., 2009) examined whether BMIs are associated with a reduction in AI driving among college student drinkers. Using data from three randomized controlled trials, the present study replicated and extended this research by examining whether BMIs reduce AI driving among three unique samples of college student drinkers at the final follow-up. The findings of Study 1 (Murphy et al., 2010) and Study 2 (Borsari et al., 2012) indicate that BMIs are associated with reductions in AI driving among college student drinkers. The results of Study 3 (Martens et al., 2013) reveal that a single-component BMI focused on correcting misperceptions of descriptive norms is associated with reductions in AI driving compared with an AE control, whereas a single-component BMI focused on the use of PBS is not. Of note, changes in drinking level did not mediate the relationship between the condition and the changes in AI driving, suggesting that BMIs’ effect on AI driving is not dependent on whether a student decreases his or her weekly drinking level.
Consistent with the findings of Schaus and colleagues (2009), results from the present study indicate that BMIs are associated with reductions in AI driving compared with control. However, in contrast to Schaus and colleagues’ (2009) findings, the reductions in AI driving in the present study persist for 6 months (Study 1 and Study 3) and 9 months (Study 2) after receipt of a BMI. It is possible that intervention differences accounted for the discrepancy in long-term intervention effects. Although an individual normative feedback document was compiled for each student in the Schaus et al. (2009) study, it is unclear how much of the BMI session focused on reviewing this feedback. In contrast, the personalized feedback information was reviewed extensively and served as the key element in the three studies described in this study. The findings of previous research indicate that motivational interventions that do not incorporate feedback are significantly less effective than BMIs that do incorporate feedback (Walters et al., 2009).
In addition, both sessions of the BMIs delivered by Schaus and colleagues (2009) focused on providing cognitive-behavioral skills training, whereas none of the sessions in the three studies analyzed in the present study contained cognitive-behavioral skills training modules. The PBS condition in Study 3 was most similar to cognitive-behavioral skills training and was not associated with reductions in AI driving. Although interventionists in the Schaus et al. (2009) study aimed to deliver the BMIs in an MI style, they suggest that the need to provide skills training at times required a more didactic, informational approach (Schaus et al., 2009). Further research is necessary to determine the characteristics of BMIs that lead to long-term intervention effects on AI driving.
Collectively, Studies 1 and 2 provide strong support for the association between counselor-administered BMIs modeled after the BASICS intervention and reductions in AI driving. Furthermore, results from these studies demonstrate that a full BMI appears to be more effective than a popular computerized education intervention used on many college campuses (Alcohol 101 Plus) or an alcohol assessment. Because both studies used the same basic feedback elements, we are not able to determine which elements of the BMI led to the changes in AI driving. Study 3 allowed us to directly compare two commonly used feedback components, descriptive social norms and PBS, both administered by counselors, to determine whether either of these single-component interventions was associated with reductions in AI driving.
The results of Study 3 indicate that a 20-minute, single-component BMI focused on correction of misperceptions of descriptive norms is associated with significant reductions in AI driving compared with an AE control, whereas a single-component BMI focused on the use of PBS is not. This finding is somewhat surprising, considering that strategies to avoid AI driving (e.g., preselecting a designated driver or arranging alternate forms of transportation) were explicitly addressed in the single-component BMI focused on the use of PBS, whereas AI driving was not addressed during the single-component BMI focused on correcting misperceptions of descriptive norms. Furthermore, PBS use has been shown to mediate the effects of several multicomponent brief alcohol interventions (Barnett et al., 2007; Larimer et al., 2007), and PBS use has been consistently associated with lower alcohol-related problems (Martens, 2007). Interventions that provide information on descriptive norms are theorized to increase motivation to change by identifying discrepancies between an individual’s behavior and perceived behavior among peers (Lewis & Neighbors, 2006). Although support for motivation to change as a mediator of outcomes is mixed (Apodaca & Longabaugh, 2009; Borsari et al., 2009), emphasizing discrepancies between perceived peer behavior and one’s own behavior may lead drinkers to rethink not only their consumption amount but also their drinking risks more generally. The PBS BMI focused on increasing specific protective behaviors that have been shown to be associated with less risky alcohol use but did not include a more general discussion of drinking level or norms.
Of note, reductions in AI driving did not occur as a result of changes in drinking level. This finding provides support for harm-reduction theory by showing that changes in high-risk behavior can be isolated from changes in drinking (Marlatt & Witkiewitz, 2002). Thus, college student drinkers who may be unwilling to cut back on the amount of alcohol consumed may still benefit from a BMI. After receiving a BMI, college students may decide to cut back on or cease engaging in risky alcohol-related behaviors, such as AI driving, even if they are not willing to cut back on overall alcohol consumption and the overall number of risky alcohol-related behaviors. Future research is necessary to determine the mechanisms of change associated with the impact of BMIs on AI driving.
Several limitations should be considered when interpreting these findings. A single-item measure of drinking and driving that asked participants whether they had driven after having had “too much to drink” was used for the outcome variable. Although this item was obtained from a reliable and valid measure of alcohol problems (Kahler et al., 2005), the results of previous research indicate that college students’ perceptions of their level of intoxication are often inaccurate (Mallett et al., 2009; White et al., 2003). Consequently, this measure may be confounded by individual differences in perceived intoxication. Participants in our sample may have driven with BACs over the legal limit but may not have felt that they had “too much to drive,” likely deflating the prevalence of impaired driving. Future research would benefit from the use of a more detailed measure of AI driving.
In addition, our samples were restricted to heavy episodic drinkers. Although this is a high-risk and relevant sample to determine BMI effectiveness for reducing AI driving, future research is necessary to determine whether BMIs reduce AI driving in a regular-drinking college student sample. In addition, it is possible that regression to the mean over time accounted for some of the group differences at the final follow-up in Study 3. Last, all alcohol use data were retrospective self-reports and may have been subject to self-presentation or social desirability bias. However, this concern is mitigated by the fact that retrospective self-report assessments of alcohol use and alcohol-related problems have been shown to be valid and reliable (Del Boca & Darkes, 2003).
Despite these limitations, this study has public health implications and extends the BMI and AI driving literatures. The present study’s findings provide support for the efficacy of BMIs for AI driving among college student drinkers. Because BMIs are individualized, based on assessment results, and counselor delivered, they necessarily accrue some costs; however, multiple cost-benefit analyses have revealed that these interventions are cost-effective (Bray et al., 2011). Future research should investigate the cost-effectiveness of BMIs specifically designed to reduce AI driving.
Furthermore, the results of the present study provide evidence that a brief, single-component personalized normative feedback intervention is associated with significant reductions in AI driving, whereas a brief, single-component BMI focused solely on the use of PBS on its own is not associated with reductions in AI driving among college student drinkers. Additional dismantling studies and future research on the effect of single-component interventions on AI driving are necessary. Another important direction for future research is to recruit college drinking drivers and determine whether a BMI aimed specifically at reducing AI driving would result in even greater reductions in AI driving.
Footnotes
This research was supported by a grant from the Alcohol Research Foundation (ABMRF; to James G. Murphy). Brian Borsari’s contribution to this article was supported by National Institute on Alcohol Abuse and Alcoholism Grant R01-AA015518 and VISN1 Career Development Award V1CDA2012-18. James G. Murphy’s contribution to this article was supported by National Institute on Alcohol Abuse and Alcoholism Grant R01-AA020829. The contents of this article are those of the authors and do not necessarily represent the views of the National Institute on Alcohol Abuse and Alcoholism, the Department of Veterans Affairs, or the United States government.
References
- Apodaca T. R., Longabaugh R.2009Mechanisms of change in motivational interviewing: A review and preliminary evaluation of the evidence Addiction 104705–715.doi:10.1111/j.1360-0443.2009.02527.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett N. P., Murphy J. G., Colby S. M., Monti P. M.2007Efficacy of counselor vs. computerized-delivered intervention with mandated college students Addictive Behaviors 322529–2548.doi:10.1016/j.addbeh.2007.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B., Hustad J. T. P., Mastroleo N. R., Tevyaw T. O., Barnett N. P., Kahler C. W., Monti P. M.2012Addressing alcohol use and problems in mandated college students: A randomized clinical trial using stepped care Journal of Consulting and Clinical Psychology 801062–1074.doi:10.1037/a0029902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B., Murphy J. G., Carey K. B.2009Readiness to change in brief motivational interventions: A requisite condition for drinking reductions? Addictive Behaviors 34232–235.doi:10.1016/j.addbeh.2008.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray J. W., Cowell A. J., Hinde J. M.2011A systematic review and meta-analysis of health care utilization outcomes in alcohol screening and brief intervention trials Medical Care 49287–294.doi:10.1097/MLR.0b013e318203624f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey K. B., Scott-Sheldon L. A. J., Carey M. P, DeMartini K. S.2007Individual-level interventions to reduce college student drinking: A meta-analytic review Addictive Behaviors 322469–2494.doi:10.1016/j.addbeh.2007.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins R. L., Parks G. A., Marlatt G. A.1985Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol Journal of Consulting and Clinical Psychology 53189–200.doi:10.1037/0022-006X.53.2.189 [DOI] [PubMed] [Google Scholar]
- Cronce J. M., Larimer M. E. Individual-focused approaches to the prevention of college student drinking. Alcohol Research & Health. 2011;34:210–221. [PMC free article] [PubMed] [Google Scholar]
- Cronce J. M., Larimer M. E., White H. R., Rabiner D. L. College student drinking and drug use: Multiple perspectives on a complex problem. Durham, NC: Guilford Press; 2012. Brief individual-focused alcohol interventions for college students. [Google Scholar]
- Del Boca F. K., Darkes J.2003The validity of self-reports of alcohol consumption: State of the science and challenges for research Addiction, 98, Supplement 21–12.doi:10.1046/j.1359-6357.2003.00586.x [DOI] [PubMed] [Google Scholar]
- Dimeff L. A., Baer J. S., Kivlahan D. R., Marlatt G. A. Brief Alcohol Screening and Intervention for College Students (BASICS): A harm reduction approach. New York, NY: Guilford Press; 1999. [Google Scholar]
- Elder R. W., Nichols J. L., Shults R. A., Sleet D. A., Barrios L. C., Compton Rthe Task Force on Community Preventive Services 2005Effectiveness of school-based programs for reducing drinking and driving and riding with drinking drivers: A systematic review. American Journal of Preventive Medicine, 28, Supplement 288–304.doi:10.1016/j.amepre.2005.02.015 [DOI] [PubMed] [Google Scholar]
- Fairlie A. M., Quinlan K. J., DeJong W., Wood M. D., Lawson D., Witt C. F.2010Sociodemographic, behavioral, and cognitive predictors of alcohol-impaired driving in a sample of U.S. college students Journal of Health Communication 15218–232.doi:10.1080/10810730903528074 [DOI] [PubMed] [Google Scholar]
- Flowers N. T., Naimi T. S., Brewer R. D., Elder R. W., Shults R. A., Jiles R.2008Patterns of alcohol consumption and alcohol-impaired driving in the United States Alcoholism: Clinical and Experimental Research 32639–644.doi:10.1111/j.1530-0277.2008.00622.x [DOI] [PubMed] [Google Scholar]
- Gustin J. L., Simons J. S.2008Perceptions of level of intoxication and risk related to drinking and driving Addictive Behaviors 33605–615.doi:10.1016/j.addbeh.2007.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A. F. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- Hingson R. W., Assailly J. P., Williams A. F.2004Underage drinking: Frequency, consequences, and interventions Traffic Injury Prevention 5228–236.doi:10.1080/15389580490465256 [DOI] [PubMed] [Google Scholar]
- Hingson R., Heeren T., Levenson S., Jamanka A., Voas R.2002Age of drinking onset, driving after drinking, and involvement in alcohol related motor-vehicle crashes Accident Analysis and Prevention 3485–92.doi:10.1016/S0001-4575(01)00002-1 [DOI] [PubMed] [Google Scholar]
- Hingson R. W., Zha W., Weitzman E. R.2009Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005 Journal of Studies on Alcohol and Drugs, Supplement 1612–20.doi:10.15288/jsads.2009.s16.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler C. W., Strong D. R., Read J. P.2005Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire Alcoholism: Clinical and Experimental Research 291180–1189.doi:10.1097/01.ALC.0000171940.95813.A5 [DOI] [PubMed] [Google Scholar]
- Kivlahan D. R., Marlatt G. A., Fromme K., Coppel D. B., Williams E.1990Secondary prevention with college drinkers: Evaluation of an alcohol skills training program Journal of Consulting and Clinical Psychology 58805–810.doi:10.1037/0022-006X.58.6.805 [DOI] [PubMed] [Google Scholar]
- LaBrie J. W., Kenney S. R., Mirza T., Lac A.2011Identifying factors that increase the likelihood of driving after drinking among college students Accident Analysis and Prevention 431371–1377.doi:10.1016/j. aap.2011.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie J. W., Napper L. E., Ghaidarov T. M.2012Predicting driving after drinking over time among college students: The emerging role of injunctive normative perceptions Journal of Studies on Alcohol and Drugs 73726–730.doi:10.15288/jsad.2012.73.726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer M. E., Lee C. M., Kilmer J. R., Fabiano P. M., Stark C. B., Geisner I. M., Neighbors C.2007Personalized mailed feedback for college drinking prevention: A randomized clinical trial Journal of Consulting and Clinical Psychology 75285–293.doi:10.1037/0022-006X.75.2.285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis M. A., Neighbors C.2006Social norms approaches using descriptive drinking norms education: A review of the research on personalized normative feedback Journal of American College Health 54213–218.doi:10.3200/JACH.54.4.213-218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis M. A., Neighbors C., Oster-Aaland L., Kirkeby B. S., Larimer M. E.2007Indicated prevention for incoming freshmen: Personalized normative feedback and high-risk drinking Addictive Behaviors 322495–2508.doi:10.1016/j.addbeh.2007.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallett K. A., Turrisi R., Larimer M. E., Mastroleo N. R.2009Have I had one drink too many? Assessing gender differences in misperceptions of intoxication among college students Journal of Studies on Alcohol and Drugs 70964–970.doi:10.15288/jsad.2009.70.964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt G. A., Witkiewitz K.2002Harm reduction approaches to alcohol use: Health promotion, prevention, and treatment Addictive Behaviors 27867–886.doi:10.1016/S0306-4603(02)00294-0 [DOI] [PubMed] [Google Scholar]
- Martens M. P., Pederson E. R., LaBrie J. W., Ferrier A. G., Cimini M. D.2007Measuring alcohol-related protective behavioral strategies among college students: Further examination of the Protective Behavioral Strategies Scale Psychology of Addictive Behaviors 21307–315.doi:10.1037/0893-164X.21.3.307 [DOI] [PubMed] [Google Scholar]
- Martens M. P., Smith A. E., Murphy J. G.2013The efficacy of single-component brief motivational interventions among at-risk college drinkers Journal of Consulting and Clinical Psychology 81691–701.doi:10.1037/a0032235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M. B., Leffingwell T., Claborn K., Meier E., Walters S., Neighbors C.2013Personalized feedback interventions for college alcohol misuse: An update of Walters & Neighbors (2005) Psychology of Addictive Behaviors 27909–920.doi:10.1037/a0031174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W. R., Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York, NY: Guilford Press; 2012. [Google Scholar]
- Monti P. M., Colby S. M., Barnett N. P., Spirito A., Rohsenow D. J., Myers M., Lewander W.1999Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department Journal of Consulting and Clinical Psychology 67989–994.doi:10.1037/0022-006X.67.6.989 [DOI] [PubMed] [Google Scholar]
- Mun E. Y., de la Torre J., Atkins D. C., White H. R., Ray A. E., Kim S. Y., Huh D.2015Project INTEGRATE: An integrative study of brief alcohol interventions for college students Psychology of Addictive Behaviors 2934–48.doi:10.1037/adb0000047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy J. G., Dennhardt A. A., Skidmore J. R., Martens M. P., McDevitt-Murphy M. E.2010Computerized versus motivational interviewing alcohol interventions: Impact on discrepancy, motivation, and drinking Psychology of Addictive Behaviors 24628–639.doi:10.1037/a0021347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Highway Traffic Safety Administration. Screening and brief intervention toolkit for college and university campuses. Washington, DC: Department of Transportation; 2014. http://www.nhtsa.gov/links/sid/3672Toolkit/pages/SupportingRes.html Retrieved from. [Google Scholar]
- Neighbors C., Lewis M. A., Atkins D. C., Jensen M. M., Walter T., Fossos N., Larimer M. E.2010Efficacy of web-based personalized normative feedback: A two-year randomized controlled trial Journal of Consulting and Clinical Psychology 78898–911.doi:10.1037/a0020766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paschall M. J.2003College attendance and risk-related driving behavior in a national sample of young adults Journal of Studies on Alcohol 6443–49.doi:10.15288/jsa.2003.64.43 [DOI] [PubMed] [Google Scholar]
- Ray A. E., Kim S.-Y., White H. R., Larimer M. E., Mun E.-Y., Clarke N., Huh D.the Project INTEGRATE Team 2014When less is more and more is less in brief motivational interventions: Characteristics of intervention content and their associations with drinking outcomes Psychology of Addictive Behaviors 281026–1040.doi:10.1037/a0036593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaus J. F, Sole M. L., McCoy T. P, Mullett N., O’Brien M. C.2009Alcohol screening and brief intervention in a college student health center: A randomized controlled trial Journal of Studies on Alcohol and Drugs, Supplement 16131–142.doi:10.15288/jsads.2009.s16.131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Sheldon L. A., Carey K. B., Elliott J. C., Garey L., Carey M. P.2014Efficacy of alcohol interventions for first-year college students: A meta-analytic review of randomized controlled trials Journal of Consulting and Clinical Psychology 82177–188.doi:10.1037/a0035192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeters J. B., Pickover A. M., Dennhardt A. A., Martens M. P., Murphy J. G.2014Elevated alcohol demand is associated with driving after drinking among college student binge drinkers Alcoholism: Clinical and Experimental Research 382066–2072.doi:10.1111/acer.12448 [DOI] [PubMed] [Google Scholar]
- Walters S. T., Vader A. M., Harris T. R., Field C. A., Jouriles E. N.2009Dismantling motivational interviewing and feedback for college drinkers: A randomized clinical trial Journal of Consulting and Clinical Psychology 7764–73.doi:10.1037/a0014472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H., Lee J. E., Nelson T. F., Lee H.2003Drinking and driving among college students: The influence of alcohol-control policies American Journal of Preventive Medicine 25212–218.doi:10.1016/S0749-3797(03)00199-5 [DOI] [PubMed] [Google Scholar]
- White A. M. What happened? Alcohol, memory blackouts, and the brain. Alcohol Research & Health. 2003;27:186–196. [PMC free article] [PubMed] [Google Scholar]