Abstract
Objective:
The relationship between experiencing trauma and increased alcohol consumption has been well established. Exposure to childhood trauma has been linked to both early onset of drinking and problematic substance use. However, the mechanisms underlying this relationship remain unclear. The results of early work suggested that drinking to relieve negative affect (i.e., drinking to cope) was driving this connection. However, the findings of more recent work suggest that drinking might be used to enhance positive affect as a way of addressing the aftereffects of early trauma. The current study looked at these two drinking expectancies as indirect pathways between the experience in early childhood of living in a home with parental violence and peak alcohol use in emerging adulthood.
Method:
Participants were 1,064 children and their parents involved in a longitudinal community study of children at high risk for the development of alcoholism and a community contrast group of those at lower risk. Baseline assessment was at age 3–5 years, self-reports of internalizing behavior and drinking expectancies were obtained at age 12–14, and drinking measures were assessed at age 18–20.
Results:
Results indicated that coping expectancy was a mediator of the relationship between early childhood trauma and later peak alcohol use, whereas enhancement expectancy was not.
Conclusions:
Children living in homes with parental violence were more likely to develop ineffective coping strategies, such as using alcohol to decrease negative affect. These results support the self-medication theory. They also demonstrate the long-term effects of early life experience on drinking behavior in early adulthood.
Exposure to trauma in early childhood leads to a host of enduring adverse consequences, including dysregulated affect, disordered behavior, and risks for self-harm. Children with early exposure have higher rates of posttraumatic stress disorder (PTSD), depression, and behavioral problems (Polusny & Follette, 1995). In addition, they are more likely to engage in risky sexual behavior, have an eating disorder, or attempt suicide (Castillo Mezzich et al., 1997; Kendler et al., 2000; Polusny & Follette, 1995; Rodriguez-Srednicki, 2002). Problematic substance use and early onset of drinking are also associated with early childhood trauma (Douglas et al., 2010; Dube et al., 2006; Epstein et al., 1998; Grayson & Nolen-Hoeksema, 2005; Lo and Cheng, 2007; Polusny & Follette, 1995; Shin et al., 2009; Simpson & Miller, 2002). In one study of 1,411 female adult twins, those who reported childhood sexual assault (30.4%) were at a threefold increased risk of becoming dependent on alcohol or other drugs (Kendler et al., 2000).
Children exposed to violence between their parents suffer similar long-term effects as do children who experience other traumas, including increased levels of PTSD, internalizing and externalizing problems, and increased likelihood of substance use disorders (Caetano et al., 2003; Graham-Bermann & Perkins, 2010; Moretti et al., 2006; Wood & Sommers, 2011). Hamburger and colleagues (2008) assessed the history of child maltreatment in 3,559 students between grades 7 and 12 in a high-risk community. They found that adolescents who witnessed violence between their parents were as likely as those who had experienced more direct forms of child maltreatment (e.g., sexual or physical abuse) to report an early age at initiation of drinking. Furthermore, Fuller et al. (2003) found that marital aggression was more important than direct aggression to the child for preschool children’s aggressive behavior, a predictor of later substance misuse.
Exposure to parental violence has been assessed in a variety of ways. Definitions of exposure to parental violence have ranged from direct involvement in the conflict to being “ostensibly unaware” (Holden, 2003). Often, exposure to violence is measured using mothers’ reports of children seeing or hearing violence. However, it is typical for parents to underreport and underestimate the amount of violence to which their children were exposed (Edleson, 1999; Stephens, 1999). For the purposes of this study, we defined exposure to parental violence as living in a home with parental violence. Previous research has shown that the majority of children living in households with parental violence are aware of it. For example, Hughes (1988) found that all of the abused women in his sample reported that their children were at home during the assaults. Similarly, Smith et al. (1997) found that 89% of abused mothers in their study reported that their children witnessed more than 20% of the violence in the home. In addition, the researchers estimated that 39% of the children witnessed between 80% and 100% of the violence that occurred. Young children are especially at risk for witnessing parental violence (Fantuzzo et al., 1997; McDonald et al., 2007). Because we measured violence at ages 3–8, a time when children are especially dependent on their caregivers, it is likely that they were exposed to a large percentage of the violence that occurred.
There are many explanations for the association between early childhood trauma and later substance misuse. Trauma can contribute both to an intensification of intrusive negative emotions and to a dulling of positive affect. It follows then that trauma survivors may be motivated to use alcohol problematically for a variety of reasons. Wills and Shiffman (1985) produced a model positing that individuals may use alcohol to regulate emotions of positive and negative valence. They explained that people will use alcohol to decrease negative affect when they are overaroused or to enhance positive emotions when they are hypoaroused. Because trauma can lead to both overwhelming and numbing symptoms, children exposed to trauma may be especially vulnerable to substance use disorders.
Motives are reasons that a subject endorses for drinking (Cooper, 1994; Leigh, 1990); this necessitates having already initiated drinking. In contrast, expectancies are beliefs about the effects of alcohol and are in evidence even before the onset of alcohol use (Jester et al., 2015). Both motives and expectancies have been linked to alcohol use, involving both frequency and consumption (Agrawal et al., 2008). In this study, we measured alcohol expectancies because, at ages 12–14, many of our participants had not yet initiated alcohol use.
There have been mixed findings in the literature regarding which drinking motives and expectancies mediate the relationship between trauma and alcohol problems. Initially investigators focused on the coping motive to explain that people consume alcohol to alleviate distress associated with trauma (Lindgren et al., 2012; Miranda et al., 2002; Ullman et al., 2005). This work was initiated to find support for the self-medication theory that posits that individuals with a trauma history will use substances to decrease negative affect (Khantzian, 1985). Although using substances may be an effective, yet damaging, method for coping with the distressing symptoms of trauma, the authors of recent studies have argued that alcohol may also be a means to increase positive emotion (Goldstein et al., 2010; Grayson and Nolen-Hoeksema, 2005; Nugent et al., 2012; Simpson, 2003; Simpson et al., 2014). For example, Simpson and colleagues (2014) found that both coping motives for dealing with negative affect and enhancement motives to increase positive affect moderated the relationship between same-day alcohol use and PTSD symptoms as well as increased drinking in those men and women with comorbid PTSD and alcohol dependence.
In addition, Grayson and Nolen-Hoeksema (2005) proposed a model that child sexual abuse survivors use alcohol to regulate both negative and positive emotions. In their study, using a sample of 697 adult women, they compared two different models: a “distress coping” model and an “emotion regulation” model. The distress coping model posits that the relationship between childhood sexual assault and alcohol problems in adulthood would be mediated by distress and a motive to drink to cope with negative emotions. The emotion regulation model added seeking positive emotions as an additional mediator. The researchers concluded that their emotion regulation model, which included both positive and negative reasons for drinking, had more explanatory power than a model including only drinking to cope with the negative emotions associated with early trauma. In a college sample, Goldstein and colleagues (2010) found that, for men, enhancement motives mediated the relationship between child maltreatment and drinking, but for women, coping motives mediated the relationship.
Similarly, Lindgren and colleagues (2012) looked at enhancement and coping motives as mediators of the relationship between sexual assault and drinking outcomes in a longitudinal study of 131 female undergraduates. They found evidence for mediation of the relationship between sexual assault and problem drinking by the coping motive. However, although the enhancement motive was correlated with both sexual assault and later drinking outcomes, it did not mediate the relationship. The authors concluded that their findings were in support of the self-medication theory (Khantzian, 1985). However, they did not explicitly measure psychological distress in relation to sexual victimization.
The current study sought to further elucidate the role of drinking expectancies as mediators of the relationship between early trauma and later alcohol use with a longitudinal design including both males and females. Earlier trauma studies have mostly concentrated on childhood sexual assault (Grayson & Nolen-Hoeksema, 2005; Lindgren et al., 2012; Simpson, 2003) or childhood maltreatment (Goldstein et al., 2010). Here we extend the base of potential applicability by examining children in homes with parental violence. No other study to our knowledge has examined the possible expectancies for drinking in young adults who grew up in homes with parental violence.
Method
Participants
This sample included data from 1,064 children (31% female) and their parents (413 mothers and 407 fathers from 491 families). The majority of the participants were White (85%), along with 7% African American, 4% Hispanic, 3% biracial, and 0.4% Native American. Written informed consent was provided by all study participants, and the protocol was approved by the University of Michigan School of Medicine Institutional Review Board. Participants in the current project were part of the ongoing Michigan Longitudinal Study, a prospective, multiwave study that has been collecting data on families with high levels of parental alcohol use disorder, along with control families drawn from the same neighborhood, since 1985 (Zucker et al., 1996, 2000). At the time of enrollment, families had to have at least one 3- to 5-year-old male child. Enrollment in the study was based on the father’s alcohol use disorder. Control subjects had no parental history of alcohol use disorder. For the current sample, 73% of fathers and 35% of mothers had a lifetime diagnosis of alcohol abuse or dependence according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994), at baseline. See Zucker and colleagues (2000) for a more detailed description of the study.
Measures
Measures were administered every 3 years over six periods starting at ages 3–5 and were completed by the children and their parents.
Demographics.
Race/ethnicity, sex, age, education, and family monthly income were ascertained from each participant.
Parental violence.
The Conflict Tactics Scales (Straus, 1979) are the most widely used measures to evaluate intimate partner violence. They evaluate three ways to handle conflict: reasoning, verbal aggression, and physical aggression. Techniques for handling conflict were assessed over the last year through 15 items ranging from “discussed the issue calmly” to “threatened with a knife or gun.” The biological mother and the biological father reported how frequently each incident happened, from never to daily. The questionnaire was administered to the parents when their child was 3–5 years old and again when the child was 6–8 years old to gauge the amount of violence in the home that each child may have been exposed to in early childhood. Responses from the two assessments were averaged. We defined a “violent” act as threatening or using physical force against a partner (e.g., “Threatened to throw something at or threatened to hit the other person”; “Pushed, grabbed, shoved, slapped, hit, or spanked the other person”). A latent variable was created based on the reported violence that the mother and father suffered and perpetrated. Specifically, we looked at four variables: violence to the father reported by the father, violence to the mother reported by the mother, violence to the mother reported by the father, and violence to the father reported by the mother. Exposure to parental violence was defined as living in a home with parental violence.
Distress.
We used the total internalizing behavior score on the Youth Self-Report of the Achenbach Child Behavior Checklist (Achenbach, 1991) as a measure of distress. The broadband internalizing scale comprises the narrow band scales Withdrawn (7 items, e.g., “I would rather be alone than with others”), Somatic complaints (8 items, e.g., “Physical problems without known medical cause: Headaches”), and Anxious/Depressed (16 items, e.g., “I feel that no one loves me” and “I am nervous or tense”). The children rated each item using a 3-point Likert scale when they were between ages 12 and 14. Test–retest reliability of item scores on the Youth Self-Report range from .95 at a 1-week interval to .84 at a 3-month interval (Achenbach, 1991).
Alcohol expectancies.
The Alcohol Expectancy Questionnaire (Brown et al., 1987) was administered at ages 12–14. The scale consists of 69 questions about alcohol expectancies, and participants rate each statement as true or false. We created two subscales, “Drinking to Enhance Positive Mood” (“enhancement expectancy”) and “Drinking to Cope with Distress” (“coping expectancy”), to match as closely as possible the drinking motives scales created by Cooper and colleagues (1992) and used by Grayson and Nolen-Hoeksema (2005) and Lindgren and colleagues (2012). The enhancement subscale included five expectancy statements that drinking creates a positive mood (e.g., “drinking makes me feel good”), and the coping subscale included nine beliefs that drinking alcohol lessens distress (e.g., “drinking helps get me out of a depressed mood”).
Alcohol measures.
Two heavy alcohol use measures were used, based on the Drinking and Drug History questionnaire (Zucker et al., 1990). Participants reported “peak alcohol use,” the maximum number of drinks in a 24-hour period in the last 3 years, when they were within ages 18–20, using 10 response categories: 0, 1–2, 3–4, 5–6, 7–9, 10–14, 15–19, 20–24, 25–29, and more than 30 drinks. In addition, we derived a measure of the number of heavy episodic drinking days in the last year based on questions regarding frequency and quantity of consumption of beer, wine and wine drinks, and distilled spirits. Heavy episodic drinking was defined as having five or more drinks at a time.
Data analysis
Structural equation models were estimated using the Mplus program (Muthén and Muthén, 1998–2007). The possible covariates of age at the time of assessment, race, parental education, and family income were examined for inclusion. When correlations between the possible confound and any variable in the structural equation model were found to be significant, the covariate was included in the model. For example, family income at age 6–8 was significantly correlated with each of the violence measures; therefore, it was added as a covariate of the violence latent variable. Full information maximum likelihood was used to account for missing data. This estimation technique uses all of the available data.
The distress coping structural equation model was also estimated taking into account the fact that the violence variables are count data, using the exponential link function and the maximum-likelihood estimator with robust standard errors. This resulted in very similar path weights and mediation results; however, model fit was unavailable for the exponential link function. Therefore, the model assuming normal distributions for the violence variables was reported.
Results
Table 1 shows the correlations between all the variables in the structural equation model. Parental violence in early childhood was related to increased levels of maximum drinking in early adulthood. Coping expectancy was related to internalizing behavior, whereas enhancement expectancy was not.
Table 1.
Correlations among parental violence, distress, coping expectancy, enhancement, and peak alcohol consumption
| Variable | Vio-dad | Vio-mom | Vio-mo2 | Vio-da2 | Distress | Enhance | Cope | Max. drink | Episodic |
| Violence to father reported by father | - | .41*** | .66*** | .46*** | .06 | .03 | .03 | .13** | .03 |
| Violence to mother reported by mother | - | .56** | .64** | .17** | -.02 | .03 | .14*** | .02 | |
| Violence to mother reported by the father | - | .37** | .11** | .01 | .03 | .1 5*** | .04 | ||
| Violence to father reported by the mother | - | .06 | -.02 | -.01 | .08 | .01 | |||
| Distress | - | .06 | .14** | .06 | .04 | ||||
| Enhancement expectancy | - | .73** | .44*** | .40*** | |||||
| Coping expectancy | - | .42*** | .44*** | ||||||
| Maximum number of drinks | - | .57*** |
Notes: N = 1,064. Vio-dad = violence to the father reported by the father; vio-mom = violence to the mother reported by the mother; vio-mo2 = violence to the mother reported by the father; vio-da2 = violence to the father reported by the mother; distress = internalizing symptoms; enhance = enhancement expectancy; cope = coping expectancy; max. drink = maximum number of drinks; episodic = heavy episodic drinking frequency.
p < .01;
p < .001.
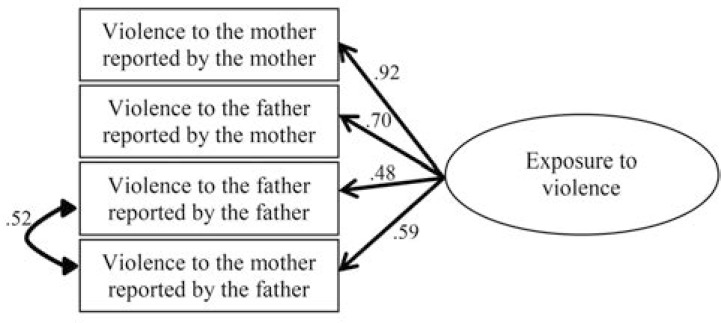
Parental violence
To assess the amount of violence the child was exposed to between ages 3 and 8, self-reports of violence perpetrated and received were obtained from both parents. Depending on reporter and victim, between 43% and 45% of the sample reported at least one incident of violent behavior, and between 6% and 11% reported three or more incidents of violent behavior in the past year. We developed a latent variable for exposure to violence by combining the four reports of violence: the mother’s reports of violence that she perpetrated against her partner, the mother’s reports of violence her partner inflicted on her, the father’s reports of violence that he perpetrated against the mother, and the father’s reports of violence that the mother inflicted on him. To increase the fit of the model, we included a correlated residual variance between violence to the father reported by the father and violence to the mother reported by the father. All factor loadings were significant (Figure 1); however, the model fit indices were mixed (comparative fit index [CFI] = .94, root mean square error of approximation [RMSEA] = .31) because of high levels of correlation between the indicator residuals. For the measurement model in Figure 1, addition of another correlated residual would have resulted in 0 degrees of freedom for the model, and therefore it could not provide fit statistics. For the structural models, we included correlated residuals between other indicators of violence (not shown).
Figure 1.
Latent variable for exposure to violence. Standardized factor loadings and standardized residual covariance are shown.
Heavy alcohol use
For maximum use over the last 3 years at age 18–20, 71% reported some alcohol use. Only 4% reported 1 to 4 drinks as maximum, 14% reported 5 to 9 drinks as their peak drinking, 22% reported 10 to 14 drinks as peak drinking, and 31% reported peak drinking of 15 or more drinks. With regard to heavy episodic drinking (five or more drinks at a time) in the last year, 64% reported at least one heavy drinking episode. The median number of heavy episodic drinking days reported was 10, and the average for those who reported any heavy episodic drinking was 14.7 days.
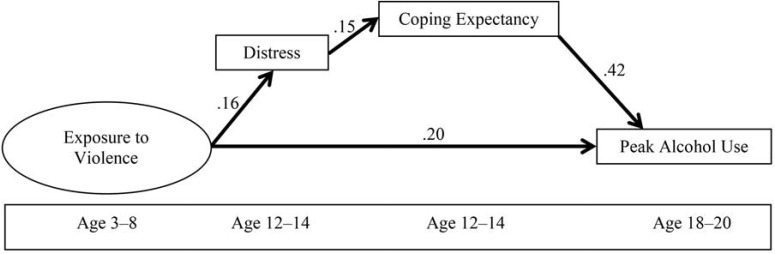
Distress coping model
We estimated the model shown in Figure 2, in which distress and coping expectancy mediate the relationship between exposure to parental violence and peak alcohol use. The model fit was very good (CFI = 1.0, RMSEA = .005). The relationship between parental violence in the home and maximum drinking was mediated by internalizing behavior and coping expectancy (standardized sum of indirect = .010, p = .034). We added covariates into the model to test for possible confounding of the results. When race, age at assessment, family income, parental alcoholism, and parental education were accounted for, the model fit was good (CFI = .99, RMSEA = .019), and the results indicated significant mediation by coping expectancy and internalizing behavior (standardized sum of indirect = .013, p = .024). The model with covariates had a reduced sample size because of missing values on the covariates (n = 776).
Figure 2.
Distress coping model. Structural equation model in which the relationship between exposure to violence in early childhood and young adulthood alcohol consumption is mediated by distress and coping expectancy. Solid paths are significant at p < .05.
To test for gender effects, two-group modeling was used. First, the model was estimated for males and females separately, and similar results were found in each group. Next, the groups were modeled simultaneously, fixing beta weights in each group to be equal, χ2(24) = 143.7. Finally, the two-group model was estimated with the beta weights free to vary across groups, χ2(20) = 141.5. The two models did not differ significantly, Δχ2(4) = 2.2, n.s. This indicates that the loadings in the models for males and females did not differ significantly. The nonindependence of siblings was also taken into account, using maximum likelihood with robust standard errors. Support for mediation by the distressing and coping expectancy model was slightly decreased in this model (sum of indirect = .013, p = .059).
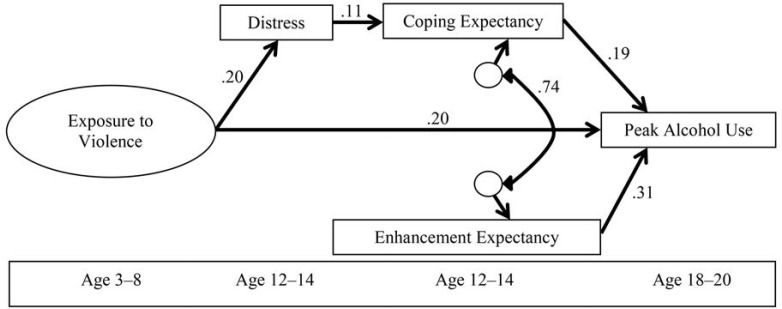
Emotion regulation model
Recall that the only difference between the distress coping model and the emotion regulation model was that the emotion regulation model included an enhancement expectancy pathway in addition to the distress coping pathway (Figure 3). The model fit well (CFI = .96, RMSEA = .08). The emotion regulation model hypothesizes that parental violence in the home and later peak alcohol use would be mediated by increased enhancement expectancy in addition to increased distress and coping expectancy. We did not find support for the emotion regulation model. The pathway from exposure to parental violence to peak alcohol use was not mediated by the enhancement expectancy in this model (standardized sum of indirect = -.004, p = .80). We also checked models with only enhancement expectancy (not coping expectancy). Again, there was no support for mediation from parental violence to alcohol consumption (standardized sum of indirect = -.005, p = .84). Finally, we added internalizing as part of the pathway (replacing coping expectancy with enhancement expectancy in Figure 2) and again found no support for mediation (standardized sum of indirect = .006, p = .24).
Figure 3.
Emotion regulation model. Structural equation model in which the relationship between exposure to violence in early childhood and young adulthood alcohol consumption is mediated by enhancement expectancy as well as by distress and coping expectancy. Solid paths are significant at p < .05.
Heavy episodic drinking
We repeated the models using the alcohol measure of heavy episodic drinking, quantified as the number of heavy drinking days in the past year. Model results were consistent with the previous results, and a significant mediation effect was found from exposure to parental violence through the coping expectancy and internalizing behavior (unstandardized indirect effect = 1.191, p = .027). Results from the model in Figure 3 (with the outcome variable now being heavy episodic drinking) also showed results consistent with our previous findings. Enhancement expectancy and coping expectancy both predicted heavy episodic drinking, the mediation effect through coping and internalizing behavior was significant (unstandardized indirect effect = 0.806, p = .033), and the mediation effect through enhancement expectancy was not significant (unstandardized indirect effect = 0.335, p = .72).
Discussion
This study provides further insight into the relationship between early childhood trauma and alcohol use in adolescence by comparing two models that examine different potential pathways to alcohol consumption in children growing up in homes with parental violence. This type of violence is particularly traumatic for young children, because they may be witnessing the two people who are most likely their main sources of support in serious conflict and unable to control their emotions. We found a direct relationship between exposure to parental violence as young children and increased peak alcohol use as young adults. We also found that the distress coping model was a significantly better fit for the data than the emotion regulation model. In the distress coping model, the relationship between exposure to parental violence as children and peak alcohol use in young adulthood was mediated by the coping expectancy pathway through increased distress and increased coping expectancy. Thus, it appears that a child who grew up in a home with parental violence is likely to experience increased distress and will then be motivated to use alcohol to cope with the resulting negative affect. The enhancement expectancy, believing that drinking will increase positive affect, was related to the mother’s report of intimate partner violence and to later peak alcohol use. However, the enhancement expectancy did not mediate the relationship between exposure to parental violence and peak alcohol use. Our results did not change when we accounted for parental alcoholism.
This work extends the findings of Fuller et al. (2003), using the same sample of children at an earlier age. They found that, in the preschool period, parents’ aggression toward each other was a more important predictor of child aggression than direct aggression to the child. Child aggression is an aspect of behavioral undercontrol that is related to later substance use problems (Zucker et al., 2011), and it also involves a significant amount of negative emotional arousal. Experiences of living in a home with parental violence appear to set the stage for later negative emotional experience.
Our findings suggest that children in homes with parental violence will develop a desire to decrease negative affect and will be motivated to use alcohol to alleviate this psychological distress. This finding extends previous research that proposed that traumatized youth may drink to decrease distress (Polusny & Follette, 1995) and is consistent with the self-medication theory (Khantzian, 1985). These findings differ from those of Grayson and Nolen-Hoeksema (2005) and Goldstein and colleagues (2010), as they found support for an emotion regulation model that includes drinking not only to decrease negative emotions but also to increase positive emotions.
Our results are similar to those of Lindgren and colleagues (2012), who also found support for the self-medication theory (Khantzian, 1985). This may be because of the longitudinal design of the two studies, which may have elucidated the temporal pathways more clearly than the cross-sectional design used by Grayson and Nolen-Hoeksema (2005) and Goldstein and colleagues (2010). However, Lindgren and colleagues used a retrospective longitudinal design, with the first assessment taking place after the sexual assault had occurred. Thus, they cannot disentangle whether the high drinking motives and problems predated the sexual assault or were a result of the negative affect associated with sexual assault. Our study used prospective data starting in early childhood. Therefore, we can see the direct association between exposure to parental violence at ages 3–8, distress and coping expectancies at ages 12–14, and then peak alcohol use at ages 18–20. We also extended the findings of Lindgren and colleagues (2012), as we included a measure of psychological distress to directly show the pathway from trauma to increased distress to coping expectancies to increases in peak alcohol use in adolescents who grew up in homes with parental violence.
Furthermore, we demonstrated that the findings on childhood trauma could generalize to a sample of children who grew up in homes with parental violence and to a sample that included males. This is not surprising because children who are exposed to parental violence experience similar long-term effects as children who experience other traumas, including increased levels of PTSD, dysregulated affect, earlier initiation of drinking, and increased likelihood of substance use disorders (Caetano et al., 2003; Moretti et al., 2006; Wood & Sommers, 2011).
We did not find support for increased enhancement expectancy as a pathway from childhood trauma to peak alcohol use. Our results differ from those of many studies that have observed such a pathway (Goldstein et al., 2010; Grayson & Nolen-Hoeksema, 2005; Nugent et al., 2012; Simpson, 2003; Simpson et al., 2014). In addition, we did not find any gender differences when the model was tested separately for males and females. This differs from the findings of Goldstein and colleagues (2010), who showed that enhancement motives mediated the relationship between child maltreatment and drinking for men, but coping motives mediated the relationship for women. These discrepancies may be attributable to differences of the current sample, which is specifically at high risk for alcohol consumption.
Because of the high levels of parental alcoholism, the children in this study experienced a great deal of adversity in addition to the trauma reported here. For instance, they were likely to have been exposed to pathological levels of drinking and the associated stresses of living with an alcoholic parent (Sher et al., 1997). This high level of adversity may result in greater amounts or intensity of negative affect. Children of alcoholic parents have also been found to have impaired mood regulation (Sorocco et al., 2015) and higher levels of negative affect (Kuperman et al., 1999; Reich et al., 1993; Rubio-Stipec et al., 1991; Sorocco et al., 2015). The combination of higher negative affect and difficulty regulating mood may render the desire to increase positive affect to be less salient in these children.
Another reason there might be divergent findings is that the age at time of the trauma, the type of trauma, and the severity of the trauma differed across all studies. For example, many of the studies measured childhood abuse or neglect any time before age 18 (Goldstein et al., 2010; Grayson & Nolen-Hoeksema, 2005; Nugent et al., 2012; Simpson, 2003; Simpson et al., 2014), whereas we measured trauma occurring much earlier. The earlier exposure to trauma would be expected to have a greater effect on developing emotion regulation.
The way in which we operationalized our variables may have also contributed to the divergent results. We measured drinking expectancies, whereas the majority of the other studies measured drinking motives. We measured expectancies because they could be assessed in children who had not yet started drinking, whereas motives cannot be measured until after drinking initiation. Although there is significant overlap between motives and expectancies, and both predict drinking behavior, there are also differences (Cooper, 1994; Leigh, 1990). Kuntsche et al. (2010) found a distinction between motives (I drink to achieve X) and expectancies (after drinking, I expect X), even when using identical items for motives and expectancies.
This study has several strengths. The longitudinal design allowed us to use prospective data to see a clear temporal order of events. Another strength is that we measured both mothers’ and fathers’ reports of violence. Typically, only the mothers’ reports of violence are measured. Also, these findings add to a limited body of empirical research on the pathways that underlie the association between exposure to parental violence and later alcohol use.
However, our results also have some limitations. We used the reported violence from the biological parents to gauge the amount of violence between the parents without the parents’ direct report of how much violence their children witnessed. Although these amounts are undoubtedly correlated, not all parental violence occurs in the presence of their children.
Children who are exposed to violence between their parents may be more likely to develop ineffective coping strategies, such as using alcohol to decrease negative affect. Interventions for these children may include teaching coping skills to reduce the link between exposure to parental violence as children and later alcohol consumption in adolescence. Because early trauma may lead to increased risk for substance misuse in adolescence, and heavy substance users with a trauma history may be at a higher risk for more severe alcohol and psychiatric problems (Zlotnick et al., 1997), screening for trauma histories in patients seeking treatment for substance misuse is recommended.
Footnotes
This research was supported by National Institutes of Health Grant R01 AA07065 (to Robert A. Zucker and Mary Heitzeg).
References
- Achenbach T. M. Integrative guide for the 1991 CBCL/4-18, YSR, and TRF profiles. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Agrawal A., Dick D. M., Bucholz K. K., Madden P. A., Cooper M. L., Sher K. J., Heath A. C. Drinking expectancies and motives: A genetic study of young adult women. Addiction. 2008;103:194–204. doi: 10.1111/j.1360-0443.2007.02074.x. doi:10.1111/j.1360-0443.2007.02074.x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed.) Washington, DC: Author; 1994. [Google Scholar]
- Brown S. A., Christiansen B. A., Goldman M. S. The Alcohol Expectancy Questionnaire: An instrument for the assessment of adolescent and adult alcohol expectancies. Journal of Studies on Alcohol. 1987;48:483–491. doi: 10.15288/jsa.1987.48.483. doi:10.15288/jsa.1987.48.483. [DOI] [PubMed] [Google Scholar]
- Caetano R., Field C. A., Nelson S. Association between childhood physical abuse, exposure to parental violence, and alcohol problems in adulthood. Journal of Interpersonal Violence. 2003;18:240–257. doi:10.1177/0886260502250074. [Google Scholar]
- Castillo Mezzich A., Tarter R. E., Giancola P. R., Lu S., Kirisci L., Parks S. Substance use and risky sexual behavior in female adolescents. Drug and Alcohol Dependence. 1997;44:157–166. doi: 10.1016/s0376-8716(96)01333-6. doi:10.1016/S0376-8716(96)01333-6. [DOI] [PubMed] [Google Scholar]
- Cooper M. L. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. doi:10.1037/1040-3590.6.2.117. [Google Scholar]
- Cooper M. L., Russell M., Skinner J. B., Windle M. Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment. 1992;4:123–132. doi:10.1037/1040-3590.4.2.123. [Google Scholar]
- Douglas K. R., Chan G., Gelernter J., Arias A. J., Anton R. F., Weiss R. D., Kranzler H. R. Adverse childhood events as risk factors for substance dependence: Partial mediation by mood and anxiety disorders. Addictive Behaviors. 2010;35:7–13. doi: 10.1016/j.addbeh.2009.07.004. doi:10.1016/j.addbeh.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube S. R., Miller J. W., Brown D. W., Giles W. H., Felitti V. J., Dong M., Anda R. F. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. Journal of Adolescent Health. 2006;38 doi: 10.1016/j.jadohealth.2005.06.006. 444 e441–410. doi:10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Edleson J. L. Children’s witnessing of adult domestic violence. Journal of Interpersonal Violence. 1999;14:839–870. doi:10.1177/088626099014008004. [Google Scholar]
- Epstein J. N., Saunders B. E., Kilpatrick D. G., Resnick H. S. PTSD as a mediator between childhood rape and alcohol use in adult women. Child Abuse & Neglect. 1998;22:223–234. doi: 10.1016/s0145-2134(97)00133-6. doi:10.1016/S0145-2134(97)00133-6. [DOI] [PubMed] [Google Scholar]
- Fantuzzo J., Boruch R., Beriama A., Atkins M., Marcus S. Domestic violence and children: Prevalence and risk in five major U.S. cities. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:116–122. doi: 10.1097/00004583-199701000-00025. doi:10.1097/00004583-199701000-00025. [DOI] [PubMed] [Google Scholar]
- Fuller B. E., Chermack S. T., Cruise K. A., Kirsch E., Fitzgerald H. E., Zucker R. A. Predictors of aggression across three generations among sons of alcoholics: Relationships involving grandparental and parental alcoholism, child aggression, marital aggression and parenting practices. Journal of Studies on Alcohol. 2003;64:472–483. doi: 10.15288/jsa.2003.64.472. doi:10.15288/jsa.2003.64.472. [DOI] [PubMed] [Google Scholar]
- Goldstein A. L., Flett G. L., Wekerle C. Child maltreatment, alcohol use and drinking consequences among male and female college students: An examination of drinking motives as mediators. Addictive Behaviors. 2010;35:636–639. doi: 10.1016/j.addbeh.2010.02.002. doi:10.1016/j.addbeh.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Graham-Bermann S. A., Perkins S. Effects of early exposure and lifetime exposure to intimate partner violence (IPV) on child adjustment. Violence and Victims. 2010;25:427–439. doi: 10.1891/0886-6708.25.4.427. doi:10.1891/0886-6708.25.4.427. [DOI] [PubMed] [Google Scholar]
- Grayson C. E., Nolen-Hoeksema S. Motives to drink as mediators between childhood sexual assault and alcohol problems in adult women. Journal of Traumatic Stress. 2005;18:137–145. doi: 10.1002/jts.20021. doi:10.1002/jts.20021. [DOI] [PubMed] [Google Scholar]
- Hamburger M. E., Leeb R. T., Swahn M. H. Childhood maltreatment and early alcohol use among high-risk adolescents. Journal of Studies on Alcohol and Drugs. 2008;69:291–295. doi: 10.15288/jsad.2008.69.291. doi:10.15288/jsad.2008.69.291. [DOI] [PubMed] [Google Scholar]
- Holden G. W. Children exposed to domestic violence and child abuse: Terminology and taxonomy. Clinical Child and Family Psychology Review. 2003;6:151–160. doi: 10.1023/a:1024906315255. doi:10.1023/A:1024906315255. [DOI] [PubMed] [Google Scholar]
- Hughes H. M. Psychological and behavioral correlates of family violence in child witnesses and victims. American Journal of Orthopsychiatry. 1988;58:77–90. doi: 10.1111/j.1939-0025.1988.tb01568.x. doi:10.1111/j.1939-0025.1988.tb01568.x. [DOI] [PubMed] [Google Scholar]
- Jester J. M., Wong M. M., Cranford J. A., Buu A., Fitzgerald H. E., Zucker R. A. Alcohol expectancies in childhood: Change with the onset of drinking and ability to predict adolescent drunkenness and binge drinking. Addiction. 2015;110:71–79. doi: 10.1111/add.12704. doi:10.1111/add.12704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K. S., Bulik C. M., Silberg J., Hettema J. M., Myers J., Prescott C. A. Childhood sexual abuse and adult psychiatric and substance use disorders in women: An epidemiological and cotwin control analysis. Archives of General Psychiatry. 2000;57:953–959. doi: 10.1001/archpsyc.57.10.953. doi:10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Khantzian E. J. The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Journal of Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. doi:10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- Kuntsche E., Wiers R. W., Janssen T., Gmel G. Same wording, distinct concepts? Testing differences between expectancies and motives in a mediation model of alcohol outcomes. Experimental and Clinical Psychopharmacology. 2010;18:436–444. doi: 10.1037/a0019724. doi:10.1037/a0019724. [DOI] [PubMed] [Google Scholar]
- Kuperman S., Schlosser S. S., Lidral J., Reich W. Relationship of child psychopathology to parental alcoholism and antisocial personality disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:686–692. doi: 10.1097/00004583-199906000-00015. doi:10.1097/00004583-199906000-00015. [DOI] [PubMed] [Google Scholar]
- Leigh B. C. Alcohol expectancies and reasons for drinking: Comments from a study of sexuality. Psychology of Addictive Behaviors. 1990;4:91–96. doi:10.1037/h0080578. [Google Scholar]
- Lindgren K. P., Neighbors C., Blayney J. A., Mullins P. M., Kaysen D. Do drinking motives mediate the association between sexual assault and problem drinking? Addictive Behaviors. 2012;37:323–326. doi: 10.1016/j.addbeh.2011.10.009. doi:10.1016/j.addbeh.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo C. C., Cheng T. C. The impact of childhood maltreatment on young adults’ substance abuse. American Journal of Drug and Alcohol Abuse. 2007;33:139–146. doi: 10.1080/00952990601091119. doi:10.1080/00952990601091119. [DOI] [PubMed] [Google Scholar]
- McDonald R., Jouriles E. N., Briggs-Gowan M. J., Rosenfield D., Carter A. S. Violence toward a family member, angry adult conflict, and child adjustment difficulties: Relations in families with 1- to 3-year-old children. Journal of Family Psychology. 2007;21:176–184. doi: 10.1037/0893-3200.21.2.176. doi:10.1037/0893-3200.21.2.176. [DOI] [PubMed] [Google Scholar]
- Miranda R., Jr., Meyerson L. A., Long P. J., Marx B. P., Simpson S. M. Sexual assault and alcohol use: Exploring the selfmedication hypothesis. Violence and Victims. 2002;17:205–217. doi: 10.1891/vivi.17.2.205.33650. doi:10.1891/vivi.17.2.205.33650. [DOI] [PubMed] [Google Scholar]
- Moretti M. M., Obsuth I., Odgers C. L., Reebye P. Exposure to maternal vs. paternal partner violence, PTSD, and aggression in adolescent girls and boys. Aggressive Behavior. 2006;32:385–395. doi:10.1002/ab.20137. [Google Scholar]
- Muthén L., Muthén B. Mplus user's guide (5th ed.) Los Angeles, CA: Authors; 1998–2007. [Google Scholar]
- Nugent N. R., Lally M. A., Brown L., Knopik V. S., McGeary J. E. OPRM1 and diagnosis-related posttraumatic stress disorder in binge-drinking patients living with HIV. AIDS and Behavior. 2012;16:2171–2180. doi: 10.1007/s10461-011-0095-8. doi:10.1007/s10461-011-0095-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polusny M. A., Follette V. M. Long-term correlates of child sexual abuse: Theory and review of the empirical literature. Applied & Preventive Psychology. 1995;4:143–166. doi:10.1016/S0962-1849(05)80055-1. [Google Scholar]
- Reich W., Earls F., Frankel O., Shayka J. J. Psychopathology in children of alcoholics. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:995–1002. doi: 10.1097/00004583-199309000-00017. doi:10.1097/00004583-199309000-00017. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Srednicki O.2002Childhood sexual abuse, dissociation, and adult self-destructive behavior Journal of Child Sexual Abuse 1075–89.doi:10.1300/J070v10n03_05 [DOI] [PubMed] [Google Scholar]
- Rubio-Stipec M., Bird H., Canino G., Bravo M., Alegria M. Children of alcoholic parents in the community. Journal of Studies on Alcohol. 1991;52:78–88. doi: 10.15288/jsa.1991.52.78. doi:10.15288/jsa.1991.52.78. [DOI] [PubMed] [Google Scholar]
- Sher K. J., Gershuny B. S., Peterson L., Raskin G. The role of childhood stressors in the intergenerational transmission of alcohol use disorders. Journal of Studies on Alcohol. 1997;58:414–427. doi: 10.15288/jsa.1997.58.414. doi:10.15288/jsa.1997.58.414. [DOI] [PubMed] [Google Scholar]
- Shin S. H., Edwards E. M., Heeren T. Child abuse and neglect: Relations to adolescent binge drinking in the national longitudinal study of Adolescent Health (AddHealth) Study. Addictive Behaviors. 2009;34:277–280. doi: 10.1016/j.addbeh.2008.10.023. doi:10.1016/j.addbeh.2008.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson T. L. Childhood sexual abuse, PTSD, and the functional roles of alcohol use among women drinkers. Substance Use & Misuse. 2003;38:249–270. doi: 10.1081/ja-120017248. doi:10.1081/JA-120017248. [DOI] [PubMed] [Google Scholar]
- Simpson T. L., Miller W. R. Concomitance between childhood sexual and physical abuse and substance use problems. A review. Clinical Psychology Review. 2002;22:27–77. doi: 10.1016/s0272-7358(00)00088-x. doi:10.1016/S0272-7358(00)00088-X. [DOI] [PubMed] [Google Scholar]
- Simpson T. L., Stappenbeck C. A., Luterek J. A., Lehavot K., Kaysen D. L. Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology. 2014;123:237–247. doi: 10.1037/a0035193. doi:10.1037/a0035193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J., Berthelsen D., O’Connor I. Child adjustment in high conflict families. Child: Care, Health and Development. 1997;23:113–133. doi: 10.1111/j.1365-2214.1997.tb00888.x. doi:10.1111/j.1365-2214.1997.tb00888.x. [DOI] [PubMed] [Google Scholar]
- Sorocco K. H., Carnes N. C., Cohoon A. J., Vincent A. S., Lovallo W. R. Risk factors for alcoholism in the Oklahoma Family Health Patterns project: Impact of early life adversity and family history on affect regulation and personality. Drug and Alcohol Dependence. 2015;150:38–45. doi: 10.1016/j.drugalcdep.2015.02.001. doi:10.1016/j.drugalcdep.2015.02.001. [DOI] [PubMed] [Google Scholar]
- Stephens D. L. Battered women’s views of their children. Journal of Interpersonal Violence. 1999;14:731–746. doi:10.1177/088626099014007004. [Google Scholar]
- Straus M. A. Measuring intrafamily conflict and violence: The Conflict Tactics (CT) Scales. Journal of Marriage and the Family. 1979;41:75–88. doi:10.2307/351733. [Google Scholar]
- Ullman S. E., Filipas H. H., Townsend S. M., Starzynski L. L. Trauma exposure, posttraumatic stress disorder and problem drinking in sexual assault survivors. Journal of Studies on Alcohol. 2005;66:610–619. doi: 10.15288/jsa.2005.66.610. doi:10.15288/jsa.2005.66.610. [DOI] [PubMed] [Google Scholar]
- Wills T. A., Shiffman S. Coping behavior and its relation to substance use: A conceptual framework. In: Shiffman S., Wills T. A., editors. Coping and substance use (pp. 3–24) New York, NY: Academic Press; 1985. [Google Scholar]
- Wood S. L., Sommers M. S. Consequences of intimate partner violence on child witnesses: A systematic review of the literature. Journal of Child and Adolescent Psychiatric Nursing. 2011;24:223–236. doi: 10.1111/j.1744-6171.2011.00302.x. doi:10.1111/j.1744-6171.2011.00302.x. [DOI] [PubMed] [Google Scholar]
- Zlotnick C., Shea M. T., Recupero P., Bidadi K., Pearlstein T., Brown P. Trauma, dissociation, impulsivity, and self-mutilation among substance abuse patients. American Journal of Orthopsychiatry. 1997;67:650–654. doi: 10.1037/h0080263. doi:10.1037/h0080263. [DOI] [PubMed] [Google Scholar]
- Zucker R. A., Ellis D. A., Fitzgerald H. E., Bingham C. R., Sanford K. Other evidence for at least two alcoholisms II: Life course variation in antisociality and heterogeneity of alcoholic outcome. Development and Psychopathology. 1996;8:831–848. doi:10.1017/S0954579400007458. [Google Scholar]
- Zucker R. A., Fitzgerald H. E., Noll R. B. Drinking and drug history (Unpublished instrument) Michigan State University; East Lansing, MI: 1990. [Google Scholar]
- Zucker R. A., Fitzgerald H. E., Refior S. K., Puttler L. I., Pallas D. M., Ellis D. A. The clinical and social ecology of childhood for children of alcoholics: Description of a study and implications for a differentiated social policy. In: Fitzgerald H. E., Lester B. M., Zuckerman B. S., editors. Children of addiction: Research, health and policy issues (pp. 109–141) New York, NY: Routledge Falmer; 2000. [Google Scholar]
- Zucker R. A., Heitzeg M. M., Nigg J. T. Parsing the under-control–disinhibition pathway to substance use disorders: A multilevel developmental problem. Child Development Perspectives. 2011;5:248–255. doi: 10.1111/j.1750-8606.2011.00172.x. doi:10.1111/j.1750-8606.2011.00172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]