Abstract
Objective:
This study considered the processes linking functional limitation and pain with depressive symptoms and two alcohol-related outcomes (past-month drinking and problematic drinking) over a 3-year period.
Method:
Data were drawn from a two-wave Miami-Dade County community study of people with physical disabilities (N = 559). Structural equation modeling was used to assess whether depressive symptoms mediated the associations among functional limitation, bodily pain, and the alcohol-related outcomes considered, and whether these associations were moderated by gender.
Results:
When the effects of the sociodemographic control variables were controlled for, depressive symptoms partly explained the effects of Wave 1 functional limitation and bodily pain on problematic drinking at Wave 2. The mediating effects of depressive symptoms on problematic drinking were significantly greater for men than for women.
Conclusions:
The findings demonstrate clear linkages between two physical health indicators, depressive symptoms and drinking, and highlight the circumstances in which gender matters most for understanding these associations.
The aging of the population in the United States has been accompanied by a sizable increase in the prevalence of physical disability, which is defined as a restriction of or inability to perform activities of daily living and instrumental activities (Verbrugge & Patrick, 1995). Although prevalence rates vary depending on the definition of disability applied, the U.S. Census estimates that 18% of the population now experiences some form of physical disability (Brault, 2012).
These estimates in the U.S. population raise concern because physical disability is associated with a host of negative mental health outcomes (Brown & Turner, 2010; Hughes et al., 2001; Mirowsky & Ross, 1999; Turner et al., 2006). Although the majority of research on the mental health consequences of physical disability has been devoted to understanding the linkages between disability and psychological distress (Brown & Turner, 2010; Mirowsky & Ross, 1999; Nosek & Hughes, 2003), there is growing recognition that disability is also directly linked with alcohol use and alcohol use disorders (Brown et al., 2014; Corrigan & Bogner, 2007; Ebener & Smedema, 2011; Turner et al., 2006). Indeed, given the host of negative consequences associated with comorbid physical health and alcohol-related problems, including greater poverty, the loss of self-care abilities, and an increase in medical complications (Bombardier & Rimmele, 1998; Heinemann & Hawkins, 1995; Tate et al., 2004), further understanding of the linkages between physical disability and alcohol use seems crucial.
To this end, the present study applies a tension-reduction model of drinking to further explore the associations among physical disability, depressive symptoms, and two alcohol-related outcomes (i.e., past-month drinking and problematic drinking patterns) among a community sample (N = 559) in Miami-Dade County, Florida. Given that men are consistently found to drink more than women and experience more alcohol-related problems (Brown & Richman, 2012; Horwitz & White, 1987; Palfai et al., 2007; Richman et al., 2002) and because there is some indication that physical health complaints are associated with a greater prevalence of alcohol-related difficulties among men (Corrigan & Bogner, 2007; Ebener & Smedema, 2011; Turner et al., 2006), particular attention is paid to whether—or to what extent—any observed associations among the indicators of physical disability, depressive symptoms, and alcohol-related outcomes vary by gender. Tests of the indirect and conditional effects of physical disability and depressive symptoms on alcohol-related outcomes are integrated into a parsimonious structural equation model.
Drinking as a tension-reduction strategy
Tension-reduction models of drinking maintain that alcohol is used as a form of self-medication to reduce the negative effects of various forms of stressor exposure (Brown et al., 2014; Richman et al., 1997, 2002; Steele & Josephs, 1990). Psychological distress is thought to influence alcohol use partly because alcohol can reduce or alleviate feelings of tension or distress brought about by stressor exposure (Baumeister et al., 1994; Conger, 1956; Hull & Young, 1983; Hull et al., 1986). Tension-reduction theories further suggest that any stressor or stressful event that increases psychological distress also has the capacity to increase alcohol consumption patterns and related difficulties (Cooper et al., 1992; Cox & Klinger, 1988).
This investigation examines two correlates of physical disability—functional limitation and bodily pain—that have long been conceptualized as chronic or acute stressors in the stress and coping literature. Functional limitation is described as a source of chronic or enduring strain because it tends to be associated with limits on social involvement and can challenge the performance of key and valued social roles (Brown & Turner, 2010; Koenig et al., 1995; Turner & Noh, 1988). Bodily pain, which varies considerably in its magnitude and chronicity, is described as a form of stressor exposure because it may present an obstacle to one’s ability or motivation to engage in activities that are conducive to well-being (Gayman et al., 2011). Functional limitation and bodily pain are also both consistently linked with depressive symptoms (Baune et al., 2008; Breslin et al. 2006; Brown & Turner, 2010; Gayman et al., 2011; Yang, 2006), which provides grounds for anticipating that they may be linked with alcohol use vis-à-vis its tension-reducing functions.
Gender as a moderator
Prior research additionally provides some support for the hypothesis that the associations among functional limitation, bodily pain, depressive symptoms, and alcohol-related outcomes may vary by gender (Turner et al., 2006). For example, Turner and colleagues (2006) report that men with physical disabilities are more prone to problematic drinking patterns than both women and their nondisabled counterparts, whereas women with physical disabilities are more likely to experience a depressive disorder than both men and nondisabled women. These findings raise the possibility that the mediating effects of depressive symptoms for the associations among functional limitation, bodily pain, and alcohol-related outcomes may vary systematically by gender. However, these potential mediating effects have not been formally investigated.
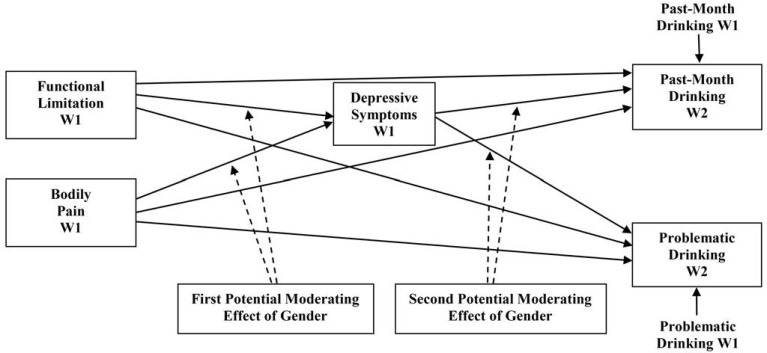
A moderated mediation approach (Preacher et al., 2007) can provide information on whether the mediating effects of depressive symptoms are contingent on gender and clarify why this is so. One possibility is that the effect of depressive symptoms on past-month drinking patterns or problematic drinking varies fundamentally by gender. This potential linkage is represented as the first potential moderating effect of gender in Figure 1. Available evidence indicating that men tend to drink more—and more problematically—compared with women, when the effects of psychological distress are accounted for (Brown & Richman, 2012; Peirce et al., 1994; Richman et al., 2002), suggests that the mediating effects of depressive symptoms for the associations among functional limitation, bodily pain, and the alcohol-related outcomes may be more pronounced among men than among women.
Figure 1.
Potential moderating effects of gender on the associations among functional limitation, bodily pain, psychological distress, and alcohol-related outcomes. W = wave.
Another possibility is that the effects of functional limitation and/or bodily pain on depressive symptoms may vary by gender, as indicated by the second potential moderating effect of gender in Figure 1. Supporting this possibility, there is some evidence that women with physical disabilities appear to be particularly prone to depressive symptomatology (Coyle & Roberge, 1992; Hughes et al., 2001; Nosek et al., 2008). For example, in the general population, women are found to be more than twice as likely as men to experience depressive symptoms (Henderson et al., 1998; Nolen-Hoeksema et al., 1999), but women with physical disabilities are estimated to be as much as 13 times more likely to experience clinically significant levels of depressive symptoms than women in the general population (Hughes et al., 2001). It is less clear, however, whether this pattern derives from gender differences in the effects of functional limitation or the effects of bodily pain. Some evidence, for example, indicates that activity limitations are more strongly associated with depressive symptoms among men, whereas chronic pain is more strongly associated with depressive symptoms among women (Beekman et al., 1995; Haley et al., 1985).
In summary, previous research provides grounds for anticipating that depressive symptoms may mediate the associations among functional limitation, bodily pain, and the alcohol-related outcomes of past-month drinking and problematic drinking (Hypothesis 1). In addition, given evidence suggesting that any mediating effects observed may be conditioned by gender, two more hypotheses are tested: (a) The effects of functional limitation and/or bodily pain on depressive symptoms are moderated by gender (Hypothesis 2), and (b) the effect of depressive symptoms on past-month drinking patterns or problematic drinking is moderated by gender (Hypothesis 3). The evaluation of these hypotheses controls for the sociodemographic characteristics of age, socioeconomic status, and race/ethnicity, which are linked with psychological well-being and alcohol-related outcomes among people with physical disabilities. Specifically, age and socioeconomic status are found to be inversely associated with depressive symptoms and the prevalence of alcohol misuse among people with physical disabilities (Bruce, 2001; Turner et al., 2006; Yang, 2006), and there is some evidence that Latinos with physical disabilities report higher levels of depressive symptoms and lower rates of alcohol-related disorders than their non-Hispanic White and African American counterparts (Brown & Turner, 2010; Turner et al., 2006).
Method
Study procedures and sample
Data are derived from a two-wave panel study of Miami-Dade County, Florida, residents that was undertaken to examine the social determinants of mental health problems among individuals with and without physical disabilities. Based on national age-, gender-, and race/ethnicity-specific rates of disability and on the Miami-Dade County demographic structure, approximately 10,000 households were randomly screened to develop a sampling frame within which physically disabled persons were significantly over represented (Turner et al., 2006). Stratified random samples were drawn so that women and men were equally represented within the study and so that the racial/ethnic composition of study participants would reflect that of the Miami-Dade County community. Additional details regarding the sampling procedure are presented by Turner and colleagues (2006).
From 2000 to 2001, 1,986 first-wave interviews were completed, with a success rate of 82%. Respondents were reinterviewed 3 years later. Excluding the 100 Wave 1 participants who died in the interim and 59 Wave 1 participants who were too ill to be interviewed, the second wave of interviews achieved a success rate of 82.5%. Of this total sample, 559 respondents indicated that they experience a physically disabling health condition and provided complete responses during both interviews. The working sample for this study is limited to these 559 respondents because respondents without physical disabilities were not asked questions concerning the presence or severity of various functional limitations.
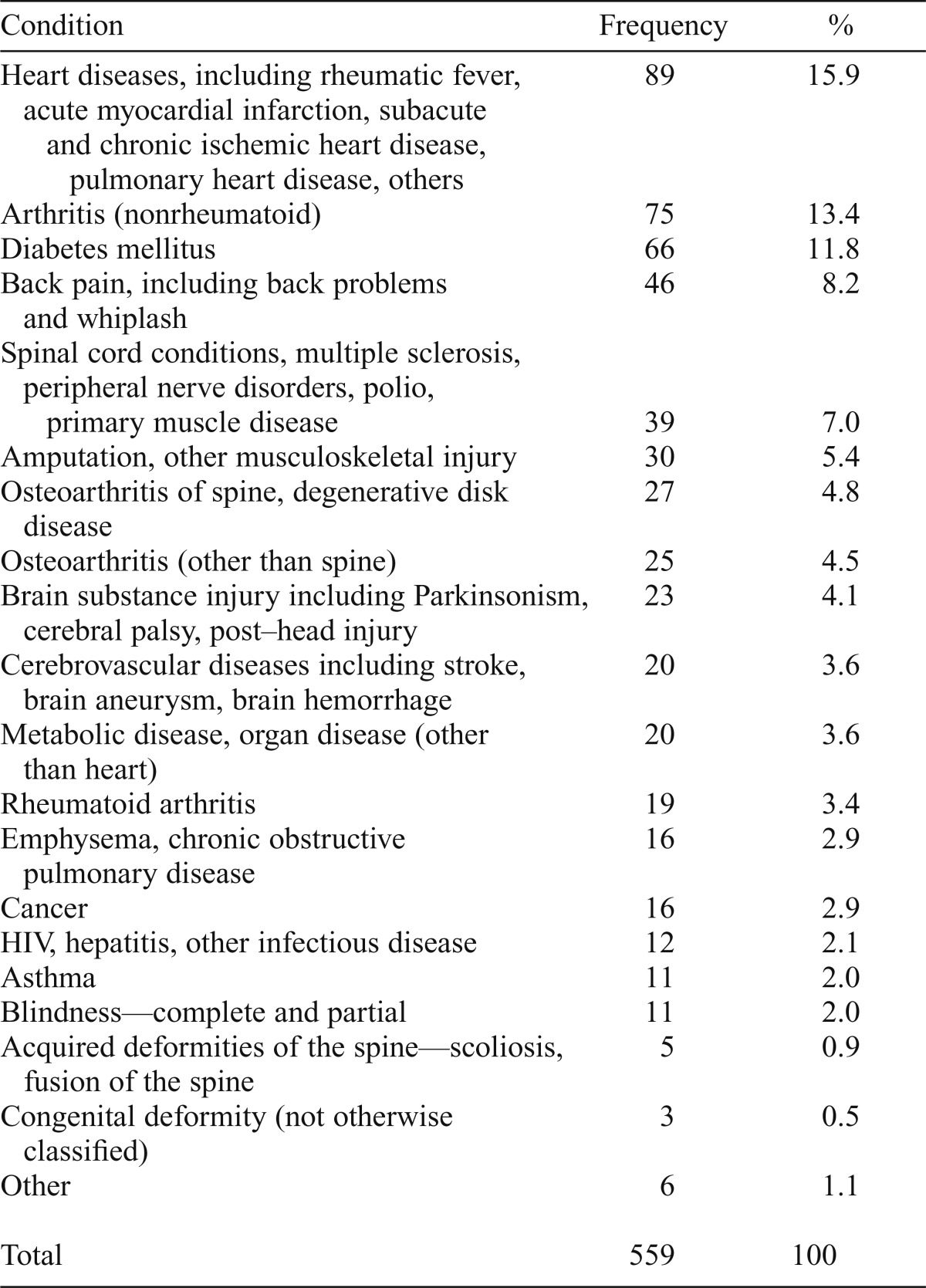
The oversampling of individuals with a disability and the fact that the nondisabled participants were matched by age resulted in a greater proportion of older respondents than in the general population. Ages in the sample ranged from 20 to 93 years with a median of 59, whereas the median age of the general population of Miami-Dade County in 2000 was 35.6 years (U.S. Census Bureau, 2000). Given this discrepancy in ages and the dramatic oversampling of individuals with physical disabilities, it is inaccurate to suggest that this sample is representative of the Miami-Dade County population. However, the sample is generally representative of people with physical disabilities in Miami-Dade County. Because this sample was drawn to broadly represent people with physical disabilities in this community, it is heterogeneous with respect to the types of disabilities reported and the age at disability onset. The distribution of types of conditions giving rise to physical limitation among this sample, as reported during the initial interview, is presented in Table 1. The mean age at onset of a physical disability reported during the first interview is 45 years, although the sample includes people born with a disability and those who did not experience physical limitation until after age 80.
Table 1.
Distribution of primary disabling conditions
| Condition | Frequency | % |
| Heart diseases, including rheumatic fever, acute myocardial infarction, subacute and chronic ischemic heart disease, pulmonary heart disease, others | 89 | 15.9 |
| Arthritis (nonrheumatoid) | 75 | 13.4 |
| Diabetes mellitus | 66 | 11.8 |
| Back pain, including back problems and whiplash | 46 | 8.2 |
| Spinal cord conditions, multiple sclerosis, peripheral nerve disorders, polio, primary muscle disease | 39 | 7.0 |
| Amputation, other musculoskeletal injury | 30 | 5.4 |
| Osteoarthritis of spine, degenerative disk disease | 27 | 4.8 |
| Osteoarthritis (other than spine) | 25 | 4.5 |
| Brain substance injury including Parkinsonism, cerebral palsy, post–head injury | 23 | 4.1 |
| Cerebrovascular diseases including stroke, brain aneurysm, brain hemorrhage | 20 | 3.6 |
| Metabolic disease, organ disease (other than heart) | 20 | 3.6 |
| Rheumatoid arthritis | 19 | 3.4 |
| Emphysema, chronic obstructive pulmonary disease | 16 | 2.9 |
| Cancer | 16 | 2.9 |
| HIV, hepatitis, other infectious disease | 12 | 2.1 |
| Asthma | 11 | 2.0 |
| Blindness—complete and partial | 11 | 2.0 |
| Acquired deformities of the spine—scoliosis, fusion of the spine | 5 | 0.9 |
| Congenital deformity (not otherwise classified) | 3 | 0.5 |
| Other | 6 | 1.1 |
| Total | 559 | 100 |
Measures
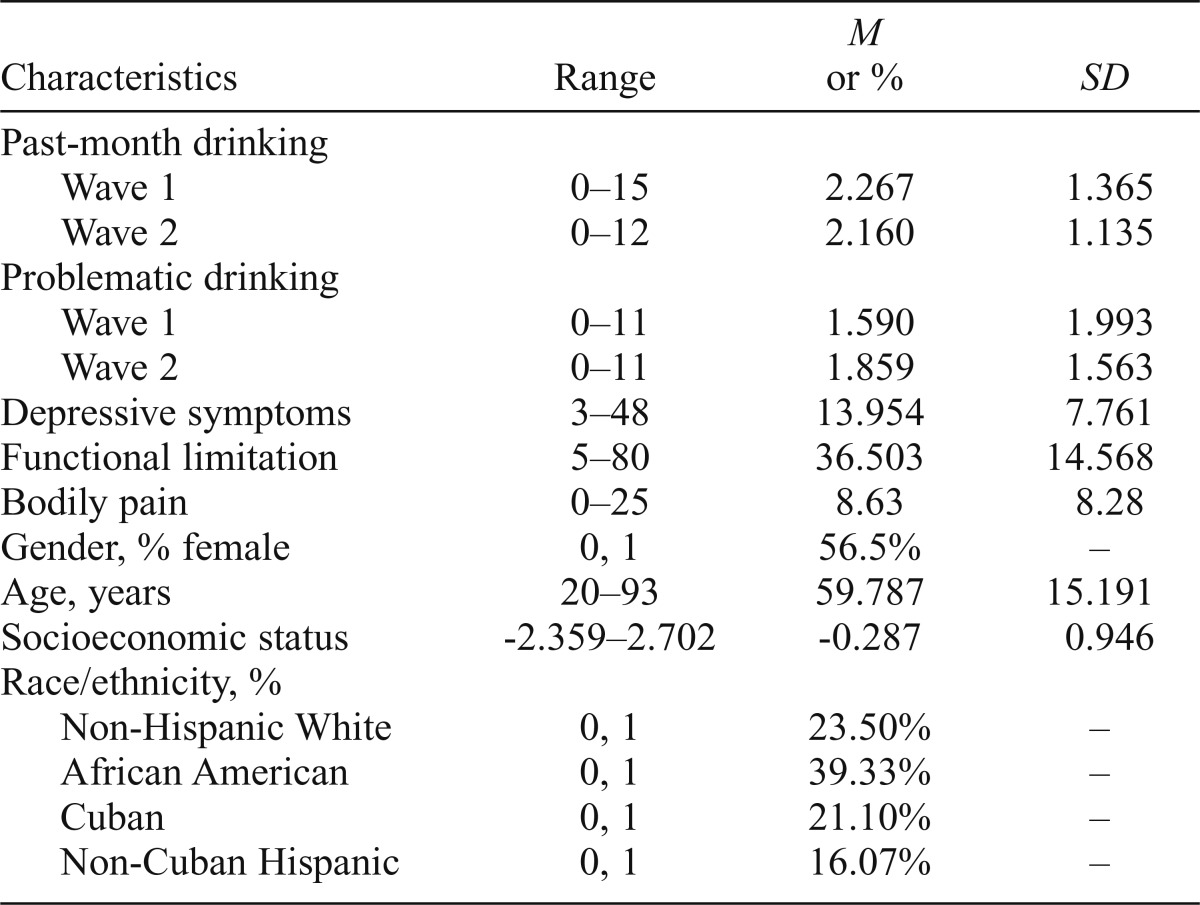
Summary statistics for all study variables are found in Table 2. Two alcohol-related outcomes were considered at Wave 2: (a) quantity and variability of past-month drinking (b) and problematic drinking patterns. Predictor variables were depressive symptoms, functional limitation, bodily pain, and gender, measured at Wave 1. The sociodemographic characteristics of age, socioeconomic status, and race/ethnicity (measured at Wave 1) were included as covariates in all analyses. Wave 1 levels of past-month drinking and problematic drinking were also controlled to assess changes in drinking patterns across the two waves of the study.
Table 2.
Means and standard deviations of variables (N = 559)
| Characteristics | Range | M or % | SD |
| Past-month drinking | |||
| Wave 1 | 0–15 | 2.267 | 1.365 |
| Wave 2 | 0–12 | 2.160 | 1.135 |
| Problematic drinking | |||
| Wave 1 | 0–11 | 1.590 | 1.993 |
| Wave 2 | 0–11 | 1.859 | 1.563 |
| Depressive symptoms | 3–48 | 13.954 | 7.761 |
| Functional limitation | 5–80 | 36.503 | 14.568 |
| Bodily pain | 0–25 | 8.63 | 8.28 |
| Gender, % female | 0, 1 | 56.5% | – |
| Age, years | 20–93 | 59.787 | 15.191 |
| Socioeconomic status | -2.359–2.702 | -0.287 | 0.946 |
| Race/ethnicity, % | |||
| Non-Hispanic White | 0, 1 | 23.50% | – |
| African American | 0, 1 | 39.33% | – |
| Cuban | 0, 1 | 21.10% | – |
| Non-Cuban Hispanic | 0, 1 | 16.07% | – |
Past-month drinking patterns.
This study used one of the most widely used methods of assessing alcohol consumption (Keyes et al., 2009; Rote & Brown, 2013), which is based on the multiplicative function of how often a respondent drank alcohol in the past month and the amount of alcohol consumed when one did drink alcohol.
Problematic drinking.
The measure of problematic drinking was an abbreviated, six-item version of the Brief Michigan Alcohol Screening Test inventory (α = .79), which is used as a screening tool for alcohol dependence and problems among current drinkers based on alcohol consumption over the past year (Maisto et al., 1995).
Depressive symptoms.
The occurrence of depressive symptoms was estimated using a modified version of the 20-item Center for Epidemiological Studies Depression Scale (Radloff, 1977), for which there is ample evidence of reliability and validity. This abbreviated 14-item measure excludes somatic complaints to avoid potential confounding of mental and physical health status. The omitted items include problems with eating, keeping your mind on what you are doing, effort, restlessness, talking, and getting going. The summated measure has high reliability (α = .83) and produces results similar to the full scale (Brown & Turner, 2010).
Functional limitation.
The measure of level of functional limitation was an adaptation of the models of disability proposed by the World Health Organization (2001). Degree of limitation was assessed by considering activities or abilities that are compromised and the extent to which they are compromised. Pooling from several previously used measures (Fries et al., 1980; Jette, 1980; Jette & Deniston, 1978; Katz et al., 1970; Lawton & Brody, 1969; Nagi, 1976; Rosow & Breslau, 1966), this 19-item index assesses difficulties related to the performance of activities of daily living (e.g., personal hygiene, eating), instrumental activities of daily living (e.g., housework, shopping), and physical mobility (e.g., walking without aid, ability to stand from sitting) (full list of items available on request). This standardized measure yields an alpha coefficient of .91.
Bodily pain.
Bodily pain was assessed by asking respondents whether they had experienced any bodily pain over the preceding 4 weeks. Those who answered affirmatively were questioned on the frequency and average intensity of pain experienced. Response categories for the intensity item ranged from 1 (very mild) to 5 (very severe). Those for frequency ranged from 1 (once or twice) to 5 (every day or almost every day). Respondents who reported no pain over the past 4 weeks were coded as 0 (none) for intensity of pain and 0 (never) for frequency of pain. Both items were coded so that higher values indicate greater intensity and frequency of pain. As used in prior research (e.g., Gayman et al., 2011), the pain measure is derived by multiplying scores on the two dimensions as an indicator of pain severity (range: 0-25).
Gender.
Gender was coded 1 for females and 0 for males.
Sociodemographic control variables.
Age in years was used as a continuous measure. Socioeconomic status was estimated in terms of three components—income, education, and occupational prestige level (Hollingshead, 1957). Such an approach provides a general assessment of socioeconomic status while reducing sample loss associated with missing data. This approach was selected because information on household income could not be obtained for 15%. Scores on these three dimensions were standardized, summed, and divided by the number of measures on which each respondent provided data. Race/ethnicity was a set of dummy variables including non-Hispanic Whites, African Americans, and Latinos. The “Latino” designation primarily represented individuals from Central America. In all regression analyses, non-Hispanic Whites represented the reference category.
Analytic strategy
Structural equation modeling using Mplus software (Version 6.11; Muthén & Muthén, 1998-2010) was used to examine the predictive significance of functional limitation and bodily pain for depressive symptoms at Wave 1 and the two drinking outcomes considered at Wave 2 (i.e., past-month drinking and problematic drinking), controlling for Wave 1 levels of the drinking outcomes, as well as gender and the sociodemographic control variables. The first stage in the analysis considered the potential for depressive symptoms to mediate the associations between the indicators of physical disability and each of the drinking outcomes assessed (Hypothesis 1). Formal mediation tests using the procedures described by Muthén and Muthén (1998-2010) for Mplus software were used.
The next step in the analysis examined whether any significant indirect paths from Wave 1 functional limitation or bodily pain to the drinking outcomes considered at Wave 2 were conditionally based on gender. The moderated mediation procedures for Mplus software described by Preacher et al. (2007) were used for these tests. These procedures determined whether any indirect effects observed were conditional because the effect of functional limitation or bodily pain on depressive symptoms was moderated by gender (Hypothesis 2), or the effect of depressive symptoms on past-month drinking patterns or problematic drinking was moderated by gender (Hypothesis 3).
Results
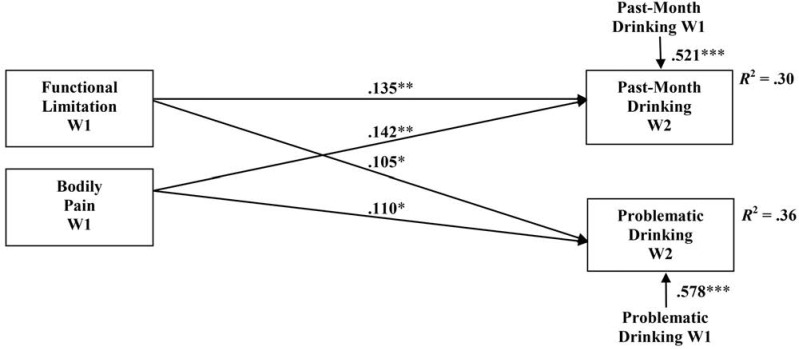
The hypothesized associations among gender, functional limitation, bodily pain, depressive symptoms, and the alcohol-related outcomes were elaborated on in the structural equation modeling analysis in three steps. As a precursor to the full model, Preacher and colleagues (2007) emphasize the importance of first establishing a connection between that which is to be mediated and the outcome of interest. Estimation of this preliminary model (Figure 2), including only functional limitation, bodily pain, past-month drinking, problematic drinking, and the sociodemographic covariates, produced a just identified model, and, as such, meaningful fit statistics are not provided.
Figure 2.
The direct effects of functional limitation and bodily pain on past-month drinking and problematic drinking (N = 559). Notes: Model controlled for age, gender, socioeconomic status, and race/ethnicity. Standardized regression coefficient reported. W = wave.
*significant at .05; **significant at .01; ***significant at .001.
The standardized path coefficients from functional limitation to past-month drinking and problematic drinking demonstrated that greater limitation was associated with a tendency to drink more in the past month (β = .135, p < .01) and a greater incidence of problematic drinking (β = .105, p < .05), net of the sociodemographic covariates. Bodily pain was also predictive of a tendency to both drink more (β = .142, p < .01) and drink more problematically (β = .110, p < .05) over time.
In this baseline model, it should additionally be noted that significant differences by gender were observed, such that women drank less in the past month (β = -.104, p < .01) and less problematically (β = -.233, p < .001). Variation in the drinking outcomes was not observed by the other social statuses included in this investigation.
With the addition of depressive symptoms to the model, the model remained just identified. When the combined effects of functional limitation, bodily pain, and depressive symptoms were considered, the coefficients for the paths from functional limitation and bodily pain to each of the drinking outcomes no longer approached significance. However, depressive symptoms were associated with a tendency to drink more problematically (β = .189, p < .001). This pattern of findings was partly consistent with the prediction of Hypothesis 1, that depressive symptoms would mediate the association between functional limitation or bodily pain and the alcohol-related outcomes.
Formal mediation tests revealed that greater depressive symptoms accounted for a substantial portion of the effects of functional limitation and bodily pain on problematic drinking. The total effect of functional limitation on problematic drinking in this model was .121, of which .036 was explained by its indirect effect via depressive symptoms. The total effect of bodily pain on problematic drinking was .109, of which .028 was explained by the indirect effect of depressive symptoms.
Moderation tests next assessed whether the mediating effects of depressive symptoms varied by gender (Hypotheses 2 and 3). The first stage in this test examined whether the pattern of findings might have varied for men and women because of gender differences in the associations of functional limitation and bodily pain with depressive symptoms (Hypothesis 2). No significant effects were observed for this pathway.
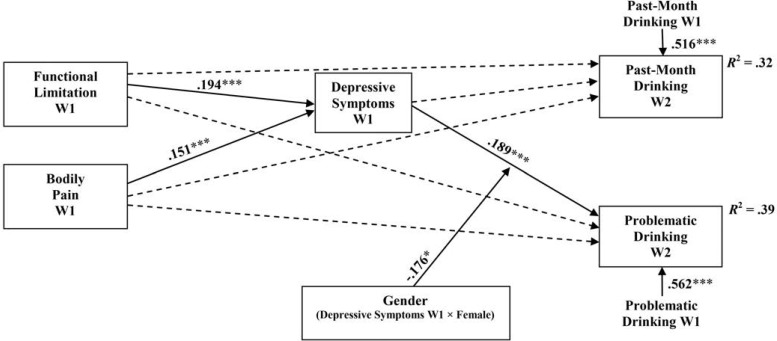
The next stage in this test considered whether the pattern of findings varied for women and men because of gender differences in the effects of depressive symptoms (Hypothesis 3). A significant interaction of depressive symptoms and gender in the prediction on problematic drinking was observed (β = -.176, p < .05), as illustrated in Figure 3. This interaction effect indicated that the mediating effects of depressive symptoms differed for men and women because the relationship between depressive symptoms and problematic drinking was significantly less strong for women than for men, net of the remaining variables.
Figure 3.
Structural equation model relating functional limitation and bodily pain to depressive symptoms and the alcohol-related outcomes (N = 559). Notes: Standardized regression coefficients reported. Model controls for age, gender, socioeconomic status, and race/ethnicity. A solid arrow indicates a significant effect; a dashed arrow indicates a nonsignificant effect. W = wave.
*significant at .05; ***significant at .001.
Discussion
The present study adds to a growing literature on the linkage of physical disability with alcohol-related outcomes (Brown et al., 2014; Corrigan & Bogner, 2007; Ebener &
Smedema, 2011; Turner et al., 2006), specifying that both greater functional limitation and bodily pain are associated with a tendency to drink more—and more problematically—over time. Further, this investigation addressed the mechanisms through which these physical health indicators and alcohol-related outcomes are linked by addressing two questions: The first is the question of whether or to what extent depressive symptoms mediate the associations among functional limitation, bodily pain, and the alcohol-related outcomes of past-month drinking and problematic drinking (Hypothesis 1). The second question concerns whether any mediating effects observed are conditional based on gender (Hypotheses 2 and 3).
With respect to the first question (Hypothesis 1), this examination provides strong support for a tension-reduction model (Brown et al., 2014; Richman et al., 1997, 2002; Steele & Josephs, 1990) for understanding the association between physical health and alcohol-related outcomes by demonstrating that depressive symptoms substantially mediate the association between functional limitation and problematic drinking over the 3-year study period. Moreover, this examination extends previous applications of this tension-reduction framework to the experience of pain, illustrating that the connection between bodily pain and problematic drinking substantially derives from the linkage between pain and depressive symptoms.
The latter observation may be of particular relevance to the pain management literature. Dependence on prescription drugs is often cited as a challenge in the clinical treatment of chronic pain conditions (see Glajchen, 2001, for a review), and understanding the circumstances in which pain self-medication is most likely to occur seems crucial in addressing this issue. Within this context, the use of various drugs may also be implicated in the linkages examined or as alternative substance-related outcomes. These possibilities warrant further investigation.
The similarity in the pattern of findings across both indicators of health status (i.e., functional limitation and bodily pain) also raises questions concerning whether certain dimensions of health are particularly salient for alcohol-related problems. For example, it seems plausible that increases in pain may compel one to drink more as an attempt to self-medicate pain symptoms, or that certain forms of functional limitation may influence alcohol use more than others in the extent to which they restrict one’s ability to carry out selfcare tasks or perform key social roles. Further study over a longer period may help resolve these issues. Additional research might also consider the potential for bi-directional relationships between depressive symptoms and alcohol-related outcomes across multiple points of time. It seems plausible, for instance, that increases in problematic drinking could lead to declines in psychological well-being, thus further exacerbating the pattern of findings reported in this analysis.
This investigation also demonstrates gender differences in the mediating framework assessed. Although no support was found for the hypothesis of gender differences in the associations of functional limitation and bodily pain with depressive symptoms (Hypothesis 2), gender differences were found in the linkage between depressive symptoms and problematic drinking, supporting Hypothesis 3. Findings revealed that, because men were significantly more likely than women to exhibit a problematic pattern of drinking as a function of greater depressive symptoms, they were more likely to drink problematically in the context of greater functional limitation and bodily pain.
These observations are consistent with prior evidence that tension-reduction models of drinking are more salient for understanding alcohol consumption patterns among men than among women (Brown & Richman, 2012; Peirce et al., 1994; Richman et al., 2002). They are also concerning in view of other evidence that men are less likely than women to seek professional help for physical and emotional health problems (Galdas et al., 2005; Kessler et al., 1981). These considerations, taken together, highlight the need for further study on self-medication as an alternative to professional help seeking among people with physical disabilities.
Another interpretation of the gender-based findings is that poor physical health may be more restrictive against alcohol use for women with physical disabilities compared with their male counterparts. This is supported by indications that alcohol consumption is more stigmatized among women than men (Cunningham et al., 1993; Schober & Annis, 1996) and that more emphasis is placed on social desirability among women with disabilities than among men with disabilities (Nosek & Hughes, 2003; Nosek et al., 2008). Evidence that, nationally, women report greater functional limitation than men (National Center for Health Statistics, 2002) further highlights the need for consideration of the risk and protective factors underlying the associations among physical health, psychological distress, and alcohol-related outcomes for women and men. It should also be noted that this study included only one indicator of psychological distress—depressive symptoms; anxiety is an additional mood state of interest in applications of the tension-reduction perspective and might be addressed as an additional mediator in future studies.
Several additional limitations of the present investigation merit comment. First, it is important to acknowledge that this sample is unique in two ways. The first is that it was drawn to represent the community-dwelling population of people with physical disabilities who, as such, are older than the general population. This circumstance may account for the lack of significant age variation observed in the drinking measures, and additional analyses provided no evidence of age variation in the pattern of findings reported when age was assessed as both a continuous and categorical variable. This pattern is inconsistent with some prior work (e.g., Turner et al., 2006).
The second unique feature of this sample is its Miami-Dade County context, in which the two largest Latino populations in the United States (Mexicans and Puerto Ricans) are virtually unrepresented. Although the pattern of findings was not found to vary across the racial/ethnic groups included in this sample, further study is needed to determine whether the findings are generalizable to Latinos living in other areas as well as the U.S. population as a whole.
In addition, the bodily pain measure is limited to the multiplicative function of two indicators. Although studies using different measures of pain were found to produce results similar to those using the measure employed here (Bair et al., 2003), further analysis using more sophisticated measures is suggested.
Finally, the effects observed may vary depending on the type of health condition involved, its duration and severity, and whether one’s limitations are visible to others (Crocker & Quinn, 2000; Nosek & Hughes, 2003; Rohmer & Louvet, 2009). Because this sample was heterogeneous with respect to health conditions included, individual categories included too few cases to examine these issues. Further study of variation in alcohol-related outcomes based on these aspects of physical disability may broaden our understanding of its behavioral and psychological consequences and the ways in which they are gendered.
Footnotes
This research was supported by National Institute on Drug Abuse Grants RO1 DA13292 and RO1 DA016429 (to R. Jay Turner).
References
- Bair M. J., Robinson R. L., Katon W., Kroenke K. Depression and pain comorbidity: A literature review. Archives of Internal Medicine. 2003;163:2433–2445. doi: 10.1001/archinte.163.20.2433. doi:10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- Baumeister R. F., Heatherton T. F., Tice D. M. Losing control: How and why people fail at self-regulation. San Diego, CA: Academic Press; 1994. [Google Scholar]
- Baune B. T., Caniato R. N., Garcia-Alcaraz M. A., Berger K. Combined effects of major depression, pain and somatic disorders on general functioning in the general adult population. Pain. 2008;138:310–317. doi: 10.1016/j.pain.2008.01.002. doi:10.1016/j.pain.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Beekman A. T. F., Kriegsman D. M. W., Deeg D. J. H., van Tilburg W. The association of physical health and depressive symptoms in the older population: Age and sex differences. Social Psychiatry and Psychiatric Epidemiology. 1995;30:32–38. doi: 10.1007/BF00784432. doi:10.1007/BF00784432. [DOI] [PubMed] [Google Scholar]
- Bombardier C. H., Rimmele C. T. Alcohol use and readiness to change after spinal cord injury. Archives of Physical Medicine and Rehabilitation. 1998;79:1110–1115. doi: 10.1016/s0003-9993(98)90180-0. doi:10.1016/S0003-9993(98)90180-0. [DOI] [PubMed] [Google Scholar]
- Brault M. W. Americans with disabilities: 2010. Current population reports. Washington, DC: U.S. Census Bureau; 2012. [Google Scholar]
- Breslin F. C., Gnam W., Franche R.-L., Mustard C., Lin E. Depression and activity limitations: Examining gender differences in the general population. Social Psychiatry and Psychiatric Epidemiology. 2006;41:648–655. doi: 10.1007/s00127-006-0079-6. doi:10.1007/s00127-006-0079-6. [DOI] [PubMed] [Google Scholar]
- Brown R. L., Richman J. A. Sex differences in mediating and moderating processes linking economic stressors, psychological distress, and drinking. Journal of Studies on Alcohol and Drugs. 2012;73:811–819. doi: 10.15288/jsad.2012.73.811. doi:10.15288/jsad.2012.73.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R. L., Richman J. A., Rospenda K. M. Economic stressors and alcohol-related outcomes: Exploring gender differences in the mediating role of somatic complaints. Journal of Addictive Diseases. 2014;33:303–313. doi: 10.1080/10550887.2014.969604. doi:10.1080/10550887.2014.969604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R. L., Turner R. J. Physical disability and depression: Clarifying racial/ethnic contrasts. Journal of Aging and Health. 2010;22:977–1000. doi: 10.1177/0898264309360573. doi:10.1177/0898264309360573. [DOI] [PubMed] [Google Scholar]
- Bruce M. L. Depression and disability in late life: Directions for future research. American Journal of Geriatric Psychiatry. 2001;9:102–112. doi:10.1176/appi.ajgp.9.2.102. [PubMed] [Google Scholar]
- Conger J. J. Alcoholism: Theory, problem and challenge. II. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Cooper M. L., Russell M., Skinner J. B., Frone M. R., Mudar P. Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology. 1992;101:139–152. doi: 10.1037//0021-843x.101.1.139. doi:10.1037/0021-843X.101.1.139. [DOI] [PubMed] [Google Scholar]
- Corrigan J. D., Bogner J. Interventions to promote retention in substance abuse treatment. Brain Injury. 2007;21:343–356. doi: 10.1080/02699050701253103. doi:10.1080/02699050701253103. [DOI] [PubMed] [Google Scholar]
- Cox W. M., Klinger E. A motivational model of alcohol use. Journal of Abnormal Psychology. 1988;97:168–180. doi: 10.1037//0021-843x.97.2.168. doi:10.1037/0021-843X.97.2.168. [DOI] [PubMed] [Google Scholar]
- Coyle C. P., Roberge J. J. The psychometric properties of the Center for Epidemiological Studies-Depression Scale (CES-D) when used with adults with physical disabilities. Psychology & Health. 1992;7:69–81. doi:10.1080/08870449208404296. [Google Scholar]
- Crocker J., Quinn D. M. Social stigma and the self: Meanings, situations, and self-esteem. In: Heatherton T. F., Kleck R. E., Hebl M. R., Hull J. G., editors. The social psychology of stigma. New York, NY: Guilford Press; 2000. pp. 153–183. [Google Scholar]
- Cunningham J. A., Sobell L. C., Chow V. M. What’s in a label? The effects of substance types and labels on treatment considerations and stigma. Journal of Studies on Alcohol. 1993;54:693–699. doi: 10.15288/jsa.1993.54.693. doi:10.15288/jsa.1993.54.693. [DOI] [PubMed] [Google Scholar]
- Ebener D. J., Smedema S. M. Physical disability and substance use disorders: A convergence of adaptation and recovery. Rehabilitation Counseling Bulletin. 2011;54:131–141. doi:10.1177/0034355210394873. [Google Scholar]
- Fries J. F., Spitz P., Kraines R. G., Holman H. R. Measurement of patient outcome in arthritis. Arthritis and Rheumatism. 1980;23:137–145. doi: 10.1002/art.1780230202. doi:10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- Galdas P. M., Cheater F., Marshall P. Men and health helpseeking behaviour: Literature review. Journal of Advanced Nursing. 2005;49:616–623. doi: 10.1111/j.1365-2648.2004.03331.x. doi:10.1111/j.1365-2648.2004.03331.x. [DOI] [PubMed] [Google Scholar]
- Gayman M. D., Brown R. L., Cui M. Depressive symptoms and bodily pain: The role of physical disability and social stress. Stress & Health. 2011;27:52–63. doi: 10.1002/smi.1319. doi:10.1002/smi.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glajchen M. Chronic pain: Treatment barriers and strategies for clinical practice. Journal of the American Board of Family Practice. 2001;14:211–218. [PubMed] [Google Scholar]
- Haley W. E., Turner J. A., Romano J. M. Depression in chronic pain patients: Relation to pain, activity, and sex differences. Pain. 1985;23:337–343. doi: 10.1016/0304-3959(85)90003-X. doi:10.1016/0304-3959(85)90003-X. [DOI] [PubMed] [Google Scholar]
- Heinemann A. W., Hawkins D. Substance abuse and medical complications following spinal cord injury. Rehabilitation Psychology. 1995;40:125–140. doi:10.1037/0090-5550.40.2.125. [Google Scholar]
- Henderson A. S., Jorm A. F., Korten A. E., Jacomb P., Christensen H., Rodgers B. Symptoms of depression and anxiety during adult life: Evidence for a decline in prevalence with age. Psychological Medicine. 1998;28:1321–1328. doi: 10.1017/s0033291798007570. doi:10.1017/S0033291798007570. [DOI] [PubMed] [Google Scholar]
- Hollingshead A. B. Two factor index of social position. New Haven, CT: A. B. Hollingshead; 1957. [Google Scholar]
- Horwitz A. V., White H. R. Gender role orientation and styles of pathology among adolescents. Journal of Health and Social Behavior. 1987;28:158–170. doi:10.2307/2137129. [PubMed] [Google Scholar]
- Hughes R., Swedlund N., Petersen N., Nosek M. Depression and women with spinal cord injury. Topics in Spinal Cord Injury Rehabilitation. 2001;7:16–24. doi: 10.1310/sci2001-23. doi:10.1310/HPKX-D0PV-MNFV-N349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull J. G., Young R. D. Self-consciousness, self-esteem, and success-failure as determinants of alcohol consumption in male social drinkers. Journal of Personality and Social Psychology. 1983;44:1097–1109. doi: 10.1037//0022-3514.44.6.1097. doi:10.1037/0022-3514.44.6.1097. [DOI] [PubMed] [Google Scholar]
- Hull J. G., Young R. D., Jouriles E. Applications of the self-awareness model of alcohol consumption: Predicting patterns of use and abuse. Journal of Personality and Social Psychology. 1986;51:790–796. doi: 10.1037//0022-3514.51.4.790. doi:10.1037/0022-3514.51.4.790. [DOI] [PubMed] [Google Scholar]
- Jette A. M. Functional Status Index: Reliability of a chronic disease evaluation instrument. Archives of Physical Medicine and Rehabilitation. 1980;61:395–401. [PubMed] [Google Scholar]
- Jette A. M., Deniston O. L. Inter-observer reliability of a functional status assessment instrument. Journal of Chronic Diseases. 1978;31:573–580. doi: 10.1016/0021-9681(78)90017-6. doi:10.1016/0021-9681(78)90017-6. [DOI] [PubMed] [Google Scholar]
- Katz S., Downs T. D., Cash H. R., Grotz R. C.1970Progress in development of the index of ADL The Gerontologist 1020–30.doi:10.1093/geront/10.1_Part_1.20. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Brown R. L., Broman C. L. Sex differences in psychiatric help-seeking: Evidence from four large-scale surveys. Journal of Health and Social Behavior. 1981;22:49–64. doi:10.2307/2136367. [PubMed] [Google Scholar]
- Keyes K. M., Geier T., Grant B. F, Hasin D. S. Influence of a drinking quantity and frequency measure on the prevalence and demographic correlates of DSM-IV alcohol dependence. Alcoholism: Clinical and Experimental Research. 2009;33:761–771. doi: 10.1111/j.1530-0277.2009.00894.x. doi:10.1111/j.1530-0277.2009.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig H. G., Pappas P., Holsinger T., Bachar J. R. Assessing diagnostic approaches to depression in medically ill older adults: How reliably can mental health professionals make judgments about the cause of symptoms? Journal of the American Geriatrics Society. 1995;43:472–478. doi: 10.1111/j.1532-5415.1995.tb06091.x. doi:10.1111/j.1532-5415.1995.tb06091.x. [DOI] [PubMed] [Google Scholar]
- Lawton M. P., Brody E. M. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. doi:10.1093/geront/9.3_Part_1.179. [PubMed] [Google Scholar]
- Maisto S. A., Connors G. J., Allen J. P. Contrasting self-report screens for alcohol problems: A review. Alcoholism: Clinical and Experimental Research. 1995;19:1510–1516. doi: 10.1111/j.1530-0277.1995.tb01015.x. doi:10.1111/j.1530-0277.1995.tb01015.x. [DOI] [PubMed] [Google Scholar]
- Mirowsky J., Ross C. E. Well-being across the life course. In: Horwitz A. V., Scheid T. L., editors. Handbook for the study of mental health: Social contexts, theories, and systems. Cambridge, England: Cambridge University Press; 1999. pp. 328–347. [Google Scholar]
- Muthén L. K., Muthén B. O. Mplus user’s guide: Statistical analysis with latent variables. 6th ed. Los Angeles, CA: Authors; 1998–2010. [Google Scholar]
- Nagi S. Z. An epidemiology of disability among adults in the United States. The Milbank Memorial Fund Quarterly. Health and Society. 1976;54:439–467. doi:10.2307/3349677. [PubMed] [Google Scholar]
- National Center for Health Statistics. Healthy women with disabilities: Analysis of the 1994–1995 National Health Interview Survey: Series 10 Report. Hyattsville, MD: National Center for Health Statistics; 2002. [Google Scholar]
- Nolen-Hoeksema S., Larson J., Grayson C. Explaining the gender difference in depressive symptoms. Journal of Personality and Social Psychology. 1999;77:1061–1072. doi: 10.1037//0022-3514.77.5.1061. doi:10.1037/0022-3514.77.5.1061. [DOI] [PubMed] [Google Scholar]
- Nosek M. A., Hughes R. B. Psychosocial issues of women with physical disabilities: The continuing gender debate. Rehabilitation Counseling Bulletin. 2003;46:224–233. doi:10.1177/003435520304600403. [Google Scholar]
- Nosek M. A., Hughes R. B., Robinson-Whelen S. The complex array of antecedents of depression in women with physical disabilities: Implications for clinicians. Disability and Rehabilitation. 2008;30:174–183. doi: 10.1080/09638280701532219. doi:10.1080/09638280701532219. [DOI] [PubMed] [Google Scholar]
- Palfai T. P., Cheng D. M., Samet J. H., Kraemer K. L., Roberts M. S., Saitz R. Depressive symptoms and subsequent alcohol use and problems: A prospective study of medical inpatients with unhealthy alcohol use. Journal of Studies on Alcohol and Drugs. 2007;68:673–680. doi: 10.15288/jsad.2007.68.673. doi:10.15288/jsad.2007.68.673. [DOI] [PubMed] [Google Scholar]
- Peirce R. S., Frone M. R., Russell M., Cooper M. L. Relationship of financial strain and psychosocial resources to alcohol use and abuse: The mediating role of negative affect and drinking motives. Journal of Health and Social Behavior. 1994;35:291–308. doi:10.2307/2137211. [PubMed] [Google Scholar]
- Preacher K. J., Rucker D. D., Hayes A. F. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. doi:10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Radloff L. S. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi:10.1177/014662167700100306. [Google Scholar]
- Richman J. A., Rospenda K. M., Nawyn S. J., Flaherty J. A. Workplace harassment and the self-medication of distress: A conceptual model and case illustrations. Contemporary Drug Problems. 1997;24:179–200. [Google Scholar]
- Richman J. A., Shinsako S. A., Rospenda K. M., Flaherty J. A., Freels S. Workplace harassment/abuse and alcohol-related outcomes: The mediating role of psychological distress. Journal of Studies on Alcohol. 2002;63:412–419. doi: 10.15288/jsa.2002.63.412. doi:10.15288/jsa.2002.63.412. [DOI] [PubMed] [Google Scholar]
- Rohmer O., Louvet E. Describing persons with disability: Salience of disability, gender, and ethnicity. Rehabilitation Psychology. 2009;54:76–82. doi: 10.1037/a0014445. doi:10.1037/a0014445. [DOI] [PubMed] [Google Scholar]
- Rosow I., Breslau N. A Guttman health scale for the aged. Journal of Gerontology. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. doi:10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- Rote S. M., Brown R. L. Gender differences in alcohol and drug use among Hispanic adults: The influence of family processes and acculturation. Journal of Addictive Diseases. 2013;32:354–364. doi: 10.1080/10550887.2013.859452. doi:10.1080/10550887.2013.859452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schober R., Annis H. M. Barriers to help-seeking for change in drinking: A gender-focused review of the literature. Addictive Behaviors. 1996;21:81–92. doi: 10.1016/0306-4603(95)00041-0. doi:10.1016/0306-4603(95)00041-0. [DOI] [PubMed] [Google Scholar]
- Steele C. M., Josephs R. A. Alcohol myopia. Its prized and dangerous effects. American Psychologist. 1990;45:921–933. doi: 10.1037//0003-066x.45.8.921. doi:10.1037/0003-066X.45.8.921. [DOI] [PubMed] [Google Scholar]
- Tate D. G., Forchheimer M. B., Krause J. S., Meade M. A., Bombardier C. H. Patterns of alcohol and substance use and abuse in persons with spinal cord injury: Risk factors and correlates. Archives of Physical Medicine and Rehabilitation. 2004;85:1837–1847. doi: 10.1016/j.apmr.2004.02.022. doi:10.1016/j.apmr.2004.02.022. [DOI] [PubMed] [Google Scholar]
- Turner R. J., Lloyd D. A., Taylor J. Physical disability and mental health: An epidemiology of psychiatric and substance disorders. Rehabilitation Psychology. 2006;51:214–223. doi:10.1037/0090-5550.51.3.214. [Google Scholar]
- Turner R. J., Noh S. Physical disability and depression: A longitudinal analysis. Journal of Health and Social Behavior. 1988;29:23–37. doi:10.2307/2137178. [PubMed] [Google Scholar]
- Verbrugge L. M., Patrick D. L. Seven chronic conditions: Their impact on US adults’ activity levels and use of medical services. American Journal of Public Health. 1995;85:173–182. doi: 10.2105/ajph.85.2.173. doi:10.2105/AJPH.85.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. International classification of functioning, disability, and health. Geneva: World Health Organization; 2001. [Google Scholar]
- Yang Y. How does functional disability affect depressive symptoms in late life? The role of perceived social support and psychological resources. Journal of Health and Social Behavior. 2006;47:355–372. doi: 10.1177/002214650604700404. doi:10.1177/002214650604700404. [DOI] [PubMed] [Google Scholar]