Abstract
Objectives
To examine the relationship between nonmedical use of prescription opioids and heroin initiation from childhood to young adulthood, and to test whether certain ages, racial/ethnic, and income groups were at higher risk for this transition.
Study design
Among a nationally representative sample of US adolescents assessed in the 2004-2011 National Surveys on Drug Use and Health cross-sectional surveys (n = 223 534 respondents aged 12-21 years), discrete-time hazard models were used to estimate the age-specific hazards of heroin initiation associated with prior history of nonmedical use of prescription opioids. Interactions were estimated between prior history of nonmedical use of prescription opioids and age of nonmedical use of prescription opioid initiation, race/ethnicity, and income.
Results
A prior history of nonmedical use of prescription opioids was strongly associated with heroin initiation (hazard ratio 13.12, 95% CI 10.73, 16.04). Those initiating nonmedical use of prescription opioids at ages 10-12 years had the highest risk of transitioning to heroin use; the association did not vary by race/ethnicity or income group.
Conclusions
Prior use of nonmedical use of prescription opioids is a strong predictor of heroin use onset in adolescence and young adulthood, regardless of the user's race/ethnicity or income group. Primary prevention of nonmedical use of prescription opioids in late childhood may prevent the onset of more severe types of drug use such as heroin at later ages. Moreover, because the peak period of heroin initiation occurs at ages 17-18 years, secondary efforts to prevent heroin use may be most effective if they focus on young adolescents who already initiated nonmedical use of prescription opioids.
Adolescence and young adulthood are particularly vulnerable ages for heroin initiation and use. In the US, in 2013,18- to 25-year-olds had the highest rates of heroin use.1 Further, the number of adolescents (aged 12-17 years) with past-year heroin dependence increased from 8000 in 2002-2005 to 13 000 in 2009-2011; among young adults (aged 18-25 years) heroin dependence increased from 137 000 to 216 000 in these same periods.2
Such an increase in heroin use and dependence may be partly driven by the transition to heroin use among the growing population of youth with a history of nonmedical use of prescription opioids.3,4 “Nonmedical prescription opioid use refers to use of prescription opioids under physician care at quantities that exceed those prescribed, or use without a prescription. Nonmedical use of prescription opioids is the second most frequent type of illicit drug use among adolescents and young adults, after marijuana1: youth tend to obtain prescription opioids from friends or relatives for free.5,6 Among young adults in 2008-2010, frequent users of nonmedical use of prescription opioids experienced a 95% increase in heroin use from 2002-2004 to 2008-2010.7 Prescription opioids have a similar chemical structure as heroin and, thus, have similar pharmacological effects.8-10 Given the high prevalence of nonmedical use of prescription opioids among adolescents and young adults,11 if there were a strong relationship between nonmedical use of prescription opioids and heroin initiation in this age group, a small shift in the prevalence of nonmedical use of prescription opioids could have an important population-level impact on heroin use.7
As a first step to informing focused primary prevention efforts, research is needed to identify age periods when nonmedical use of prescription opioids initiation may pose a particularly high risk for later heroin use and to identify sociodemographic groups that may be at considerable risk for experiencing this transition. The link between nonmedical use of prescription opioid onset in early adolescence and later development of prescription opioid abuse/dependence, as well as evidence suggesting that adolescents have increased biological vulnerability to addiction, suggest that early initiation of nonmedical use of prescription opioids may also pose a particular risk for future related drug use problems such as heroin initiation.12,13 The risk of transition from nonmedical use of prescription opioids to heroin use may also be stronger among racial/ethnic minorities and lower-income groups, who, once prescription drugs became more expensive and difficult to obtain following the introduction of an abuse-deterrent formulation of Oxycontin (Purdue Pharma LP, Stamford, Connecticut), may have started to use heroin as a less expensive alternative to prescription opioids.4,14,15 To our knowledge, no studies have yet examined heterogeneity in the relationship between nonmedical use of prescription opioids and heroin initiation by age or social group.
We focus our study on adolescents and young adults, and build on the prior literature by: (1) examining whether the risk of heroin initiation in adolescence and young adulthood is associated with a prior history of nonmedical use of prescription opioids; and (2) testing whether the relationship between nonmedical use of prescription opioids and heroin initiation in adolescence and young adulthood varies by age on nonmedical use of prescription opioid initiation, race/ethnicity, or family income.
Methods
We used data from the 223 534 adolescents and young adults aged 12-21 years who were included in the 2004-2011 National Survey on Drug Use and Health (NSDUH) public use files. This study was approved by the Columbia University Mailman School of Public Health Institutional Review Board. The NSDUH is the primary source of information on the prevalence of drug use in the US population among those aged 12 years and older.2 It is an annual cross-sectional survey that collects annual data from residents of households and noninstitutional group quarters and from civilians living on military bases.2 As such, the NSDUH is representative of the noninstitutionalized, civilian population in the US, and it excludes institutionalized individuals including those in residential drug use treatment centers. Individuals who do not speak English or Spanish are not interviewed and, therefore, not included in the sample.2
The survey uses a multistage area probability sample for each state and the District of Columbia and oversamples younger age groups (aged 12-25 years) and Blacks and Hispanics. In-person interviews were conducted by a trained interviewer using computer-assisted personal interviewing. Questions about sensitive behaviors such as drug use were administered more privately using audio computer-assisted self-interviewing to increase the level of honest reporting of illegal drug use and other sensitive behaviors.16
Respondents were offered a $30 incentive for participation in the survey.
Weighting techniques were used to account for the complex survey design (see Statistical Analyses section below). Response rates, in years 2002-2011, varied between 87% and 91% and 74% and 77% for household screening and completed interviews, respectively. Adolescent and young adult completed interviews weighted response rates varied similarly (84% and 90% and 80% and 85%, respectively). Detailed information about the sample design and survey methods of NSDUH are found in the NSDUH annual reports from the Substance Abuse and Mental Health Services Administration.2
Retrospective reports of nonmedical use of prescription opioids and heroin initiation were used to construct a person-time dataset, recording respondents' drug use initiation patterns from age 7 years (the earliest age at which respondents reported nonmedical use of prescription opioids) until age of censoring (defined as age of heroin initiation or age of interview). Initiation of heroin use (n = 7) or nonmedical use of prescription opioids (n = 656) earlier than age 8 years was not considered because of concerns about validity of reports of opioid use in early childhood.
Measures
Our outcome of interest was age of initiation of heroin use among adolescent and young adults (ages 12-21 years at date of interview). Individuals were asked: How old were you the first time you used heroin?
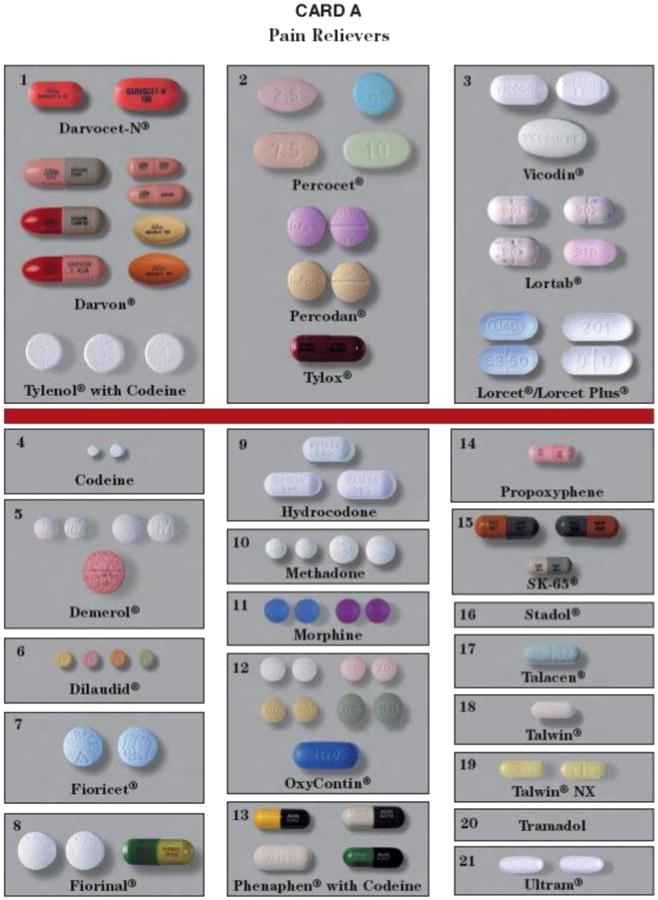
Our main exposure was prior nonmedical use of prescription opioids history. In NSDUH, “nonmedical use” refers to situations in which a subject used a drug that was not prescribed for him/her, or he/she took the drug only for the experience or feeling it caused.2 The following information was provided to participants as an attempt to reduce false positive responses: “These questions are about prescription pain reliever use. We are not interested in your use of over-the-counter pain relievers that can be bought in stores without a doctor's prescription.” To improve the identification of pain relievers used in the past, cards with pictures of multiple types of prescription opioids were handed to participants (Appendices 1 and 2; available at www.jpeds.com). Respondents were asked to identify the type used and provide the frequency of use. Initiation of drug use was defined based on the response to the following question: “How old were you the first time you used any prescription pain reliever that was not prescribed for you that or that you took only for the experience or feeling it caused?”
For the purpose of our study, we created a time-variant predictor variable that indicated whether the previous exposure to nonmedical use of prescription opioids occurred before the initiation of heroin use. This variable was coded at each specific period as 0 if a person had not used nonmedical use of prescription opioids up to that age and was coded as 1 if the person started using nonmedical use of prescription opioids at that age or before.
Categories of age at initiation of nonmedical use of prescription opioid use were also generated to account for differences in the risk of heroin use across ages at initiation of nonmedical use of prescription opioids (initiation at age 8-9, 10-12, 13-15, 16-18, and 19-21 years).
Models were adjusted for other types of substance use prior to heroin use. This was defined as the initiation of any substance use (ie, cocaine, marijuana, tranquilizers, sedatives, stimulant, hallucinogens, methamphetamines, inhalants, crack cocaine, lysergic acid diethylamide, and 3,4-methylenedioxy-methamphetamine [ecstasy]), different from nonmedical use of prescription opioids, before the initiation of heroin use. We also adjusted for prior use of alcohol.
Demographic covariates included the following: (1) age (age round number values from 7-21 years); (2) sex (male/female); race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, and Asian/NativeAmerican); (3)past-year family income (<$20 000, $20 000-$49 999, $50 000-$74 999, and $75 000+); (4) metropolitan statistical area (MSA; MSA with more than 1 million persons, MSA with less than1 million persons, or not in a MSA); and (5) calendar year of interview (2004-2011). MSA was included to account for potential confounding because of the urban-rural differences in both nonmedical use of prescription opioid and heroin use.
Statistical Analyses
Exploratory and descriptive analyses using NSDUH weighting were conducted to identify proportions of individuals with previous nonmedical use of prescription opioid and heroin use and their sociodemographic characteristics. The association between nonmedical use of prescription opioid status and the initiation of heroin use was estimated using discrete-time hazard models. To select the best-fitting method to model the shape of the baseline hazard function, we evaluated the goodness-of-fit of a series of models with different time-ordered sets of polynomials.17 The cubic order polynomial was chosen to model the baseline hazard, as it showed lower deviance (indicative of better fit) and also a lower Akaike information criterion value, compared with the linear and quadratic models. A lower Akaike information criterion represents a smaller distance between the unknown true likelihood function of the data and the fitted likelihood function of the model.
We used the following modeling strategy. First, we tested whether prior nonmedical use of prescription opioid use was associated with the risk of heroin initiation. To test this, model 1 included the following covariates: nonmedical use of prescription opioid status, time (modeled as a cubic order polynomial), race/ethnicity, previous initiation of any substance use (other than nonmedical use of prescription opioid and heroin), previous initiation of alcohol use, sex, age, income, MSA, and year of survey. Second, we tested whether the association between prior use of nonmedical use of prescription opioid and heroin initiation varied by age of nonmedical use of prescription opioid initiation.
Therefore, model 2 also included an interaction term between prior use of nonmedical use of prescription opioids and categories of age of initiation of nonmedical use of prescription opioids. Third, we tested if the risk of heroin initiation by nonmedical use of prescription opioid status differed by race/ethnicity. Model 3 included an interaction term between prior use of nonmedical use of prescription opioids and race/ethnicity (eg, Hispanic vs White). Fourth, we tested whether the risk of heroin initiation associated with nonmedical use of prescription opioid status differed by income. Model 4 thus included an interaction term between prior use of nonmedical use of prescription opioids and income category. A Wald test of linear hypothesis18 was used to compare model fit between model 1 and models 2-4. It tested the null hypothesis that the coefficients of new variables introduced in models 2-4 were equal to zero (eg, coefficients of the interaction term between prior use of nonmedical use of prescription opioids and categories of age of initiation of nonmedical use of prescription opioids were equal to zero).
To take into account the complex sampling design, all analyses were based on Taylor series approximations using “svy” commands of Stata 13.0 (StataCorp, College Station, Texas).19 In order to obtain unbiased estimates, analyses were weighted using the provided person-level analysis weights that account for the selection probability at specific stages or for adjustment factors. As multiple NSDUH survey years were used, we divided the person-level analysis weights by the number of years of NSDUH data used in analyses (8 years).20 The final weight can be interpreted as the total number of people in the target population represented by each record in the sample. Predictive mean neighborhood methods with unweighted hot-deck imputation were used to replace missing values with appropriate response codes.2
Result
Sociodemographic characteristics of the study population are presented in Table I. The most frequently reported initiation age of nonmedical use of prescription opioids was 16-18 years of age (45%) followed by 13-15 years (33%). Among the 1385 respondents (0.66% of sample; 95% CI 0.62, 0.70) who reported heroin use, 1045 (76%) also reported a history of nonmedical use of prescription opioids (Table I). The incidence of heroin initiation was 67 per 100 000 person-years.
Table I. Demographic characteristics of individuals in NSDUH (2004-2011) aged 12-21 years by prior history of nonmedical prescription opioid use*.
| Total population | Prior history of nonmedical prescription opioid use (N = 31803) | No prior history of nonmedical prescription opioid use (N = 191 731) | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n | % | n | % | n | % | |
| Sex | ||||||
| Male | 112 152 | 51 | 15 836 | 52 | 96 316 | 51 |
| Female | 111 382 | 49 | 15 967 | 48 | 95 415 | 49 |
| Age (y) | ||||||
| 12-13 | 46 179 | 19 | 1818 | 5 | 44 361 | 21 |
| 14-15 | 49 382 | 20 | 4566 | 12 | 44 816 | 22 |
| 16-17 | 50 294 | 20 | 7840 | 20 | 42 454 | 20 |
| 18-19 | 40 558 | 21 | 8459 | 30 | 32 099 | 20 |
| 20-21 | 37 121 | 20 | 9120 | 33 | 28 001 | 17 |
| Race/ethnicity | ||||||
| White | 37 823 | 19 | 21 442 | 69 | 113 603 | 58 |
| Hispanic | 135 045 | 60 | 4645 | 16 | 33 178 | 19 |
| Black | 30 625 | 15 | 3014 | 10 | 27 611 | 16 |
| Other | 20 041 | 7 | 2702 | 5 | 17 339 | 7 |
| Heroin use (ever in lifetime) | ||||||
| No | 222 149 | 99 | 30 758 | 97 | 191 391 | 100 |
| Yes | 1385 | 1 | 1045 | 3 | 340 | 0 |
| Age at initiation of nonmedical use of prescription opioids (y) | ||||||
| 8-9 | 544 | 2 | 544 | 2 | ||
| 10-12 | 3908 | 11 | 3908 | 11 | ||
| 13-15 | 11 452 | 33 | 11 452 | 33 | ||
| 16-18 | 13 205 | 45 | 13 205 | 45 | ||
| 19-21 | 2694 | 9 | 2694 | 9 | ||
| Prior use of other drugs/alcohol | ||||||
| No | 146 216 | 64 | 5993 | 18 | 140 249 | 72 |
| Yes | 77 318 | 36 | 25 810 | 82 | 51 482 | 28 |
| Household income categories ($) | ||||||
| <20 000 | 54 528 | 24 | 9624 | 30 | 44 904 | 23 |
| 20 000-49 999 | 72 291 | 31 | 10 595 | 32 | 61 696 | 31 |
| 50 000-74 999 | 37 833 | 16 | 4776 | 15 | 33 057 | 16 |
| 75 000+ | 58 882 | 28 | 6808 | 24 | 52 074 | 29 |
| Residence | ||||||
| MSA 1 million or more persons | 90 241 | 50 | 11 525 | 46 | 78 718 | 51 |
| MSA <1 million persons | 108 329 | 42 | 16 575 | 45 | 91 754 | 41 |
| Segment not in a CBSA | 24 964 | 8 | 3703 | 9 | 21 261 | 8 |
| Year when survey was conducted | ||||||
| 2004 | 27 782 | 12 | 4307 | 14 | 23 475 | 12 |
| 2005 | 28 099 | 13 | 4179 | 13 | 23 920 | 12 |
| 2006 | 27 438 | 13 | 4027 | 13 | 23 411 | 12 |
| 2007 | 27 144 | 13 | 3937 | 13 | 23 207 | 13 |
| 2008 | 27 828 | 12 | 3978 | 12 | 23 850 | 12 |
| 2009 | 27 589 | 12 | 3939 | 12 | 23 650 | 13 |
| 2010 | 28 596 | 12 | 3764 | 12 | 24 832 | 13 |
| 2011 | 29 058 | 13 | 3672 | 11 | 25 386 | 13 |
CBSA, core-based statistical area.
Proportions are weight-adjusted estimates.
Figure 1 shows the age-specific fitted probabilities of heroin initiation, as well as the fitted probabilities of survival from heroin initiation, given prior history of nonmedical use of prescription opioid use. The fitted hazard of heroin initiation increased over time, peaked at ages 16-18 years, and decreased thereafter. The hazard of heroin initiation was 13.12 times higher among adolescents and young adults with a prior history of nonmedical use of prescription opioids than among those with no prior history of nonmedical use of prescription opioid use (95% CI 10.73, 16.04) (Table II, model 1). Blacks had a lower hazard of heroin initiation than Whites (hazard ratio [HR] 0.16; 95% CI 0.10, 0.25).
Figure 1.
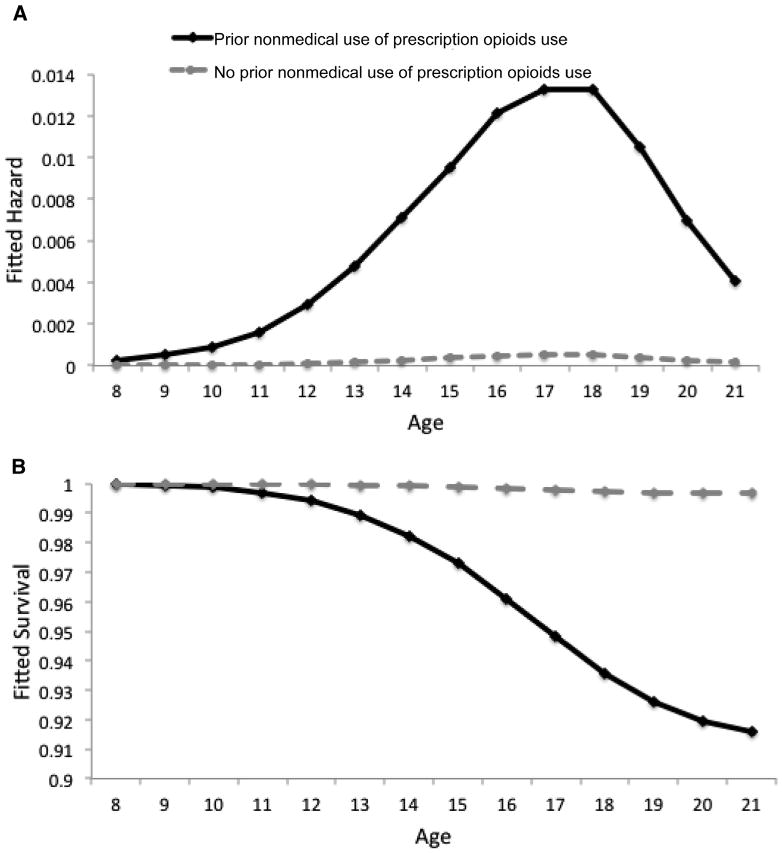
Fitted probability of A, heroin initiation and B, survival by prior nonmedical prescription opioid use among adolescents and young adults, NSDUH (2004-2001).
Table II. HR of heroin use initiation by prior nonmedical prescription of opioid use among adolescents and young adults, NSDUH, 2004-2011*.
| Model 1 | Model 2† | Model 3‡ | Model 4§ | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Prior history of nonmedical use of prescription opioids | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 13.12 | (10.73, 16.04) | 9.68 | (5.97, 15.7) | 9.76 | (6.34, 15.02) | 14.66 | (9.64, 22.29) |
| Prior nonmedical use of prescription opioids history by age of initiation of nonmedical use of prescription opioids (y) | ||||||||
| Nonmedical use of prescription opioids initiated at 8-9 | 1.53 | (0.64, 3.63) | ||||||
| Nonmedical use of prescription opioids initiated at initiated at 10-12 | 1.84 | (1.13, 2.99) | ||||||
| Nonmedical use of prescription opioids initiated at 13-15 | 1.59 | (1.01, 2.51) | ||||||
| Nonmedical use of prescription opioids initiated at initiated at 16-18 | 0.97 | (0.62, 1.54) | ||||||
| Nonmedical use of prescription opioids initiated at initiated at 19-21 | 1.00 | |||||||
| Race/ethnic group | ||||||||
| White | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Hispanic | 0.80 | (0.62, 1.02) | 0.79 | (0.62, 1.01) | 1.03 | (0.71, 1.49) | 0.79 | (0.98, 1.62) |
| Black | 0.16 | (0.10, 0.25) | 0.16 | (0.10, 0.24) | 0.19 | (0.09, 0.41) | 0.16 | (0.12, 0.32) |
| Other | 1.07 | (0.74, 1.53) | 1.05 | (0.73, 1.50) | 1.13 | (0.61, 2.10) | 1.07 | (0.88, 2.05) |
| Prior nonmedical use of prescription opioids history by race | ||||||||
| Nonmedical use of prescription opioids among Whites | 1.00 | |||||||
| Nonmedical use of prescription opioids among Hispanics | 0.69 | (0.43, 1.12) | ||||||
| Nonmedical use of prescription opioids among Blacks | 0.75 | (0.26, 2.22) | ||||||
| Nonmedical use of prescription opioids among others | 0.92 | (0.50, 1.71) | ||||||
| Income ($) | ||||||||
| <20 000 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 20 000-49 999 | 1.09 | (0.92, 1.28) | 1.07 | (0.91, 1.26) | 1.08 | (0.92, 1.28) | 1.00 | (0.70, 1.42) |
| 50 000-74 999 | 1.20 | (0.95, 1.51) | 1.19 | (0.95, 1.50) | 1.20 | (0.95, 1.52) | 0.81 | (0.51, 1.31) |
| 75 000+ | 1.11 | (0.90, 1.36) | 1.12 | (0.91, 1.38) | 1.11 | (0.90, 1.36) | 0.89 | (0.56, 1.41) |
| Prior nonmedical use of prescription opioids history by income | ||||||||
| Nonmedical use of prescription opioids given income <20 000 | 1.00 | |||||||
| Nonmedical use of prescription opioids given income 20 000-49 999 | 0.74 | (0.43, 1.30) | ||||||
| Nonmedical use of prescription opioids given income 50 000-74 999 | 0.83 | (0.53, 1.32) | ||||||
| Nonmedical use of prescription opioids given income 75 000+ | 1.24 | (0.67, 2.29) | ||||||
| Goodness of fit statistics (Wald test)¶ | ||||||||
| F-test model fit compared with model 1 (DF) | 146.81 (5, 116) | 0.83 (3, 118) | 1.11 (3, 118) | |||||
| P value | 0.0000 | 0.48 | 0.35 | |||||
DF, degrees of freedom.
Significant estimates are in bold.
All models controlled for time (modeled as a cubic order polynomial), previous initiation of any substance use (other than nonmedical use of prescription opioids and heroin), previous initiation of alcohol use, sex, age, MSA, and year of survey.
Model 2: Adds an interaction term between prior use of nonmedical use of prescription opioids and categories of age of initiation of nonmedical use of prescription opioids to model 1.
Model 3: Adds an interaction term between prior use of nonmedical use of prescription opioids and race/ethnicity to model 1.
Model 4: Adds an interaction term between prior use of nonmedical use of prescription opioids and income to model 1.
The Wald test is used to test the null hypothesis that the coefficients of new variables introduced to the model are equal to 0.
The hazard of heroin initiation associated with nonmedical use of prescription opioid use varied by age of nonmedical use of prescription opioid initiation. A model that estimated the hazard of heroin initiation given prior nonmedical use of prescription opioid separately by age category of nonmedical use of prescription opioid initiation provided a better fit to the data than a model that estimated the average hazard of heroin initiation given prior nonmedical use of prescription opioids across age categories (Table II, model 2: F = 146.81; P value < .001). Figure 2 shows the hazard of heroin initiation associated with nonmedical use of prescription opioids by age category: the adjusted hazard of heroin initiation associated with nonmedical use of prescription opioids was highest when respondents started using nonmedical use of prescription opioids at ages 10-12 years (HR 17.77, 95% CI 13.00, 24.30) followed by ages 13-15 years (HR 15.42, 95% CI 12.44, 19.11), and 8-9 years (HR 14.79, 95% CI 6.67, 32.77).
Figure 2.
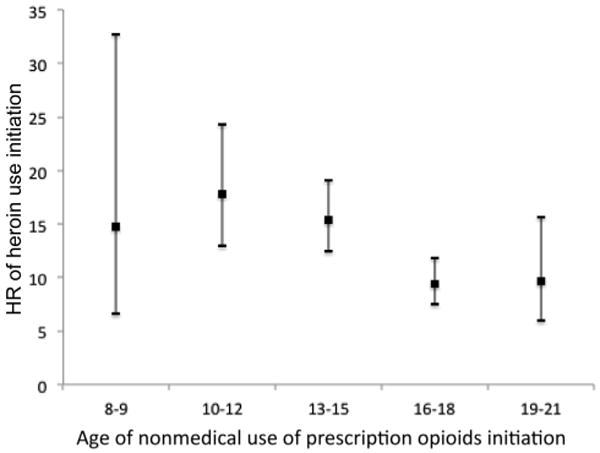
Fitted HRs of heroin initiation associated with prior nonmedical prescription opioid use, by age of nonmedical prescription opioid use initiation (NSDUH, 2004-2011).
Models 3 and 4 (Table II) evaluated whether the association of nonmedical use of prescription opioids with heroin initiation differed by race/ethnicity and income. Specifying a separate relationship between nonmedical use of prescription opioids and heroin use by racial/ethnic group (model 3) or by income group (model 4), did not improve model fit (F = 0.83, P = .48 and F = 1.11, P = .35, respectively), indicating that there was no evidence of heterogeneity in the effect of nonmedical use of prescription opioids on heroin initiation by race/ethnicity or income.
Discussion
We found that prior use of nonmedical use of prescription opioids is a strong predictor of heroin use onset among adolescents and young adults. Over the study period, the risk of heroin initiation was 13 times higher among respondents who reported prior nonmedical use of prescription opioid use than among those who did not previously use nonmedical use of prescription opioids. Importantly, the risk of heroin initiation was greatest among individuals who were first exposed to nonmedical use of prescription opioids in early adolescence (ie, ages 10-12 years). The average risk of heroin initiation was lower among Blacks and Hispanics compared with Whites, a finding that is reflective of the changing profile of the typical heroin user in the US, from primarily inner-city minorities to suburban and rural Whites.21-23 Further, and contrary to our a priori hypothesis, there was no evidence of heterogeneity in the effect of nonmedical use of prescription opioids on heroin initiation by race/ethnicity or income, suggesting that the risk of transition from nonmedical use of prescription opioids to heroin use may be an important generalizable concern across sociodemographic groups.
The fact that those initiating nonmedical use of prescription opioids at ages 10-12 years had the highest risk of initiating heroin use by young adulthood has a number of important public health implications. First, increased resources for primary nonmedical use of prescription opioid prevention efforts focused in late childhood are urgently needed. Such programs may have not only the benefit of preventing nonmedical use of prescription opioids and related harms, but also a downstream effect of preventing transitions into more severe drugs, such as heroin. Second, our results highlight the importance of early identification and screening programs to identify adolescents who have initiated nonmedical use of prescription opioids. Given that the peak period of heroin initiation was observed to be in individuals aged 17-18 years, an important “window of opportunity” exists for secondary prevention in early adolescence to prevent transitions to heroin use among adolescent nonmedical use of prescription opioid users. Our findings are consistent with prior studies, which found that early initiation of nonmedical use of prescription opioids is associated with higher risk for later prescription opioid abuse and dependence.5,12
The strong association between nonmedical use of prescription opioid use in early adolescence and heroin initiation in young adulthood is a particular concern at the present time. Most states have now implemented prescription drug monitoring programs to support the appropriate use of prescription drugs, and third-party prescription payment systems run by pharmacy benefit managers or health insurers have also been used to detect prescription drug abuse.24-26 To the extent that such regulations reduce access and increase the street price of prescription opioids, they may have the unintended effect of contributing to drug diversion from nonmedical use of prescription opioid to heroin use.14 Hence, concurrent investment in substance abuse prevention and treatment programs should be a public health priority to prevent such unintended consequences.
This study expands prior research in several ways. First, we examined the relationship between nonmedical use of prescription opioid use history and time to heroin initiation among adolescents and young adults. This builds on 2 prior studies using NSDUH data, which compared the incidence of heroin use by prior nonmedical use of prescription opioid status in the 12-year-old and older population.7,23 Second, we tested whether the risk of heroin use given a prior history of nonmedical use of prescription opioids was concentrated in certain racial/ethnic or income groups. Our study revealed that, at least among adolescents and young adults, the risk of transition from nonmedical use of prescription opioid to heroin cuts across social groups. Third, we identified an age range, 10-12 years, when initiation of nonmedical use of prescription opioid places adolescents at particular risk for later initiation of heroin.
Study contributions should be considered in context of the following limitations. First, the NSDUH is representative of English and Spanish-speaking adolescents in the US, and not of institutionalized individuals, including those in residential drug use treatment centers, who may be at particularly high risk for heroin use.27 At the present time, it is unclear whether the magnitude of the association between nonmedical use of prescription opioid and heroin use would be different for that population. Second, we may have underestimated the true rate of heroin initiation, as some heroin users may not have reported their use in a survey interview. Robust and rigorous NSDUH procedures that provide privacy to participants (including the use of audio computer-assisted self interview [ACASI]) and protect the confidentiality of respondents somewhat allay these concerns. Third, this study is based on retrospective reports of age of onset of nonmedical use of prescription opioid and heroin use. Respondents may recall their age of onset as later than it actually occurred.28,29 Fourth, the NSDUH is a cross-sectional survey; hence, we cannot conclusively establish temporality, and our findings should be replicated in a prospective longitudinal study. Fifth, adolescents and young adults may not accurately report their family income. This may have limited our ability to detect whether family income modified the association between prior nonmedical use of prescription opioid and heroin initiation.
In conclusion, prior use of nonmedical use of prescription opioids is a strong predictor of heroin use onset among adolescents and young adults, regardless of the user's race/ ethnicity or income. Our study shows that 2 windows of opportunity exist for the prevention of heroin initiation by investing in the primary prevention of nonmedical use of prescription opioids in childhood, before the adolescent years, as well as secondary prevention of heroin use among users of nonmedical use of prescription opioids in early adolescence, before the peak of heroin use.
Acknowledgments
Funded by the National Institute of Drug Abuse-National Institutes of Health (NIDA-NIH; DA023434 [to S.M.], K01DA030449 [to M.C.]; T32DA031099-01A1 [PI: Hasin; to J.K.], R03DA037770 [to B.M.]), and the Eunice Kennedy Shriver National Institute of Child and Human Development NICHD/NIH (HD020667 [to S.M.]). J.S. is a recipient of a Doctoral Research Scholarship from the Fulbright Commission. S.M. serves as a consultant for Purdue Pharma.
Glossary
- HR
Hazard ratio
- MSA
Metropolitan statistical area
- NSDUH
National Survey on Drug Use and Health
Appendix 1. Prescription opioids included in cards provided to users of nonmedical prescription opioid use
Darvocet-n®, Darvon®, or Tylenol® with codeine
Percocet®, Percodan®, or Tylox®
Vicodin®, Lortab®, or Lorcet®/Lorcet plus®
Codeine
Demerol®
Dilaudid®
Fioricet®
Fiorinal®
Hydrocodone
Methadone
Morphine
Oxycontin®
Phenaphen® with codeine
Propoxyphene
SK-65®
Stadol® (no picture)
Talacen®
Talwin®
Talwin® NX
Tramadol
Ultram®
Appendix 2. Sample card provided to nonmedical users of prescription opioids in the National Survey on Drug Use and Health
Footnotes
The other authors declare no conflicts of interest.
References
- 1.SAMHSA. NSDUH Series H-48, HHS Publication No (SMA) 14–4863. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. [Google Scholar]
- 2.SAMHSA. NSDUH Series H-44, HHS Publication No (SMA) 12–4713. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings. [Google Scholar]
- 3.Lankenau SE, Schrager SM, Silva K, Kecojevic A, Bloom JJ, Wong C, et al. Misuse of prescription and illicit drugs among high-risk young adults in Los Angeles and New York. J Public Health Res. 2012;1:22–30. doi: 10.4081/jphr.2012.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mars SG, Bourgois P, Karandinos G, Montero F, Ciccarone D. “Every ‘never’ I ever said came true”: transitions from opioid pills to heroin injecting. Int J Drug Policy. 2014;25:257–66. doi: 10.1016/j.drugpo.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lankenau SE, Teti M, Silva K, Bloom JJ, Harocopos A, Treese M. Initiation into prescription opioid misuse amongst young injection drug users. Int J Drug Policy. 2012;23:37–44. doi: 10.1016/j.drugpo.2011.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCabe SE, Cranford JA, Boyd CJ, Teter CJ. Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addict Behav. 2007;32:562–75. doi: 10.1016/j.addbeh.2006.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers - United States, 2002-2004 and 2008-2010. Drug Alcohol Depend. 2013;132:95–100. doi: 10.1016/j.drugalcdep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Center for Substance Abuse Treatment. Clinical Guidelines for the Use of Buprenorphine in the Treatment of Opioid Addiction. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2004. [PubMed] [Google Scholar]
- 9.Nestler EJ. Is there a common molecular pathway for addiction? Nat Neurosci. 2005;8:1445–9. doi: 10.1038/nn1578. [DOI] [PubMed] [Google Scholar]
- 10.Kosten TR, George TP. The neurobiology of opioid dependence: implications for treatment. Sci Pract Perspect. 2002;1:13–20. doi: 10.1151/spp021113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.SAMHSA. NSDUH Series H-46. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. [Google Scholar]
- 12.McCabe SE, West BT, Morales M, Cranford JA, Boyd CJ. Does early onset of non-medical use of prescription drugs predict subsequent prescription drug abuse and dependence? Results from a national study Addiction. 2007;102:1920–30. doi: 10.1111/j.1360-0443.2007.02015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chambers RA, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: a critical period of addiction vulnerability. Am J Psychiatry. 2003;160:1041–52. doi: 10.1176/appi.ajp.160.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cicero TJ, Ellis MS, Surratt HL. Effect of abuse-deterrent formulation of OxyContin. N Engl J Med. 2012;367:187–9. doi: 10.1056/NEJMc1204141. [DOI] [PubMed] [Google Scholar]
- 15.Coplan PM, Kale H, Sandstrom L, Landau C, Chilcoat HD. Changes in oxycodone and heroin exposures in the National Poison Data System after introduction of extended-release oxycodone with abuse-deterrent characteristics. Pharmacoepidemiol Drug Saf. 2013;22:1274–82. doi: 10.1002/pds.3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morral AR, McCaffrey DF, Chien S. Measurement of adolescent drug use. J Psychoactive Drugs. 2003;35:301–9. doi: 10.1080/02791072.2003.10400013. [DOI] [PubMed] [Google Scholar]
- 17.Singer J, Willett J. Chapter 12: extending the discrete-time hazard model. In: Singer J, Willett J, editors. Applied longitudinal data analysis: modeling change and event occurrence. New York, NY: Oxford University Press, Inc; 2003. [Google Scholar]
- 18.Engle RF. Wald, likelihood ratio, and lagrance multiplier test in econometrics. In: Griliches Z, I MD, editors. Handbook of econometrics. Amsterdam: North-Holland; 1984. pp. 775–879. [Google Scholar]
- 19.STATA. StataCorp Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- 20.SAMHSA. National Survey on Drug Use and Health, 2010 Codebook. Rockville, MD: 2010. [Google Scholar]
- 21.Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71:821–6. doi: 10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- 22.Cicero TJ, Kuehn BM. Driven by prescription drug abuse, heroin use increases among suburban and rural whites. JAMA. 2014;312:118–9. doi: 10.1001/jama.2014.7404. [DOI] [PubMed] [Google Scholar]
- 23.Muhuri P, Gfroerer J, Davies M. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 24.Brady JE, Wunsch H, DiMaggio C, Lang BH, Giglio J, Li G. Prescription drug monitoring and dispensing of prescription opioids. Public Health Rep. 2014;129:139–47. doi: 10.1177/003335491412900207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shepherd J. Combating the prescription painkiller epidemic: a national prescription drug reporting program. Am J Law Med. 2014;40:85–112. doi: 10.1177/009885881404000103. [DOI] [PubMed] [Google Scholar]
- 26.Davis CS, Pierce M, Dasgupta N. Evolution and convergence of state laws governing controlled substance prescription monitoring programs, 1998-2011. Am J Public Health. 2014;104:1389–95. doi: 10.2105/AJPH.2014.301923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greene JM, Ennett ST, Ringwalt CL. Substance use among runaway and homeless youth in three national samples. Am J Public Health. 1997;87:229–35. doi: 10.2105/ajph.87.2.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Darke S. Self-report among injecting drug users: A review. Drug Alcohol Depend. 1998;51:253–63. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- 29.Anthony JC, Petronis KR. Early-onset drug use and risk of later drug problems. Drug Alcohol Depend. 1995;40:9–15. doi: 10.1016/0376-8716(95)01194-3. [DOI] [PubMed] [Google Scholar]


