Abstract
Background:
Neuroimaging is the cornerstone for guiding thrombolytic and interventional therapy for stroke. Beneficial outcome can only be obtained within a rather short time of less than 3-4.5 hours of symptom onset. Challenges in developing countries like Nigeria often lead to delayed presentation of stroke patients in hospitals. We sought to study the time and pattern of presentation of stroke patients for CT imaging in a Nigerian tertiary hospital.
Methods:
Of the 271 stroke patients who had cranial CT between 2008 and 2010, eighty-three (30.6%) with full retrievable CT records, were included in this study. They were categorized into six time groups cross-tabulated with their CT findings.
Results:
Forty-two patients (50.6%) had cerebral infarction while 23 (27.7%) had haemorrhagic stroke. However, 18 (21.7%) patients had apparently normal CT findings. The mean presentation time for CT imaging was 70 hours (SD ±94 hours). Only 31% of all stroke patients presented for CT imaging within 12 hours, and none, within 3 hours. Forty-six percent did not present within 24 hours of symptom onset. Significantly more patients with ischemic stroke (72.3%) than hemorrhagic stroke (27.7%) presented after 12 hours of ictus (X2 = 4.027 d=1, P =0.045). Age (X2=0.008, P =0.931) and gender (X21.742, d=1,P =0.187) had no statistically significant relationship with the time of presentation for CT imaging.
Conclusion:
None of our patients met the time criteria for thrombolytic therapy. Ischemic stroke patients presented for imaging later than patients with intracerebral haemorrhage. There is a need to increase the awareness regarding early recognition, presentation and diagnosis of stroke for timely intervention in Nigeria.
Keywords: Time, Stroke, CT Imaging, Nigeria
INTRODUCTION
Stroke is the second leading cause of death worldwide, 1 with over two-thirds of these deaths occurring in developing regions of the world, such as sub-Saharan Africa (SSA) 2. Stroke has remained a leading cause of morbidity worldwide leaving up to 50% of its survivors chronically disabled with reduced health-related quality of life and depression.2, 3
The incidence of stroke in developing countries like Nigeria is expected to rise in the future as the population undergoes a "health transition" , from less of infectious diseases, and diseases related to poverty and malnutrition to more of non-communicable diseases. Stroke is broadly classified into ischemic and hemorrhagic stroke.1,4 The current prevalence of stroke in Nigeria is 1.14 per 1000 while the 30-day case fatality rate is as high as 40%.3 A changing pattern with an increasing frequency of hemorrhagic stroke has been reported in our population.5 Due to the substantial economic, social and medical problems stroke poses worldwide, there is a need to reduce its effects, by prompt institution of intensive management which has imaging diagnosis at its foundation and core.
The diagnosis and determination of stroke type requires neuroimaging with computed tomography (CT).6 A detailed history and imaging will usually exclude stroke mimics. A brain CT is usually the first line imaging modality required to differentiate ischemic from haemorrhagic stroke.6- 8 With the increasing availability of CT scanners in Nigeria and increased scanner sensitivity for ischemic stroke, it is recommended that a suspected stroke patient should have a CT within 3 hours of symptom onset to allow for appropriate intervention to arrest progression of neurological deficits. 6,9-12However, early stroke presentation in developing countries, within this limited time window is extremely difficult for several reasons; ranging from poor stroke recognition to limited socio-economic and infrastructural facilities13-16.
The CT scan presentation time for stroke patients has been shown to differ from one center to the other across countries. In developing countries like Nigeria, the presentation time of stroke patients for imaging has not been determined and delays in imaging are common even in developed countries 11-15. We set out to determine the time lag between stroke onset and acquisition of brain CT in patients presenting to our Radiology Department with recognized features of stroke.
METHODS
This was a retrospective study which evaluated CT imaging records and clinical data of all stroke patients referred for CT scan in the Department of Radiology, University College Hospital, Ibadan between 2008 and 2010. The stroke type and CT imaging presentation time of stroke patients from the approximate time of onset of their symptoms, was recorded. The estimated time of onset of symptoms was based on the record of the time of event stated by the requesting physician on the Radiology request card, and the time of performance of the CT was obtained from the CT imaging records. Out of the 271 cranial CT scan requests for stroke that were evaluated, only 83 had complete records to be included in the study. The eligible subjects were then categorized into 6 groups, based on the interval between the onset of symptoms and time of performance of CT, as follows: (I) less than 3 hours, (II) 3-6 hours (III) 7-12 hours (IV) 13-24 hours(V) 2 - 7 days (VI) > 7 days. We evaluated the CT images of these patients and classified them according to the CT findings into 3 groups: (a) Normal (b) Haemorrhagic stroke (c) Ischaemic stroke. All cranial CT images were acquired with a multi-detector 8-slice GE brightspeed SCT scanner using a standard head protocol. The images were evaluated for evidence of haemorrhage, infarct, early ischemic changes and associated complications. The clinical data and CT findings were analyzed using the statistical package for social sciences (SPSS) version 20.0.
Descriptive statistics, frequencies and percentages were computed for demographic characteristics of patients and variables such as type of stroke and time of presentation for cranial CT scan. The mean and standard deviation were calculated for continuous variable such as age, while Chi-square test was used to determine possible associations between qualitative data such as sex, age group, pattern of CT finding and time of onset of stroke.
RESULTS
Eighty-three stroke patients were retrospectively evaluated. The age range of the study subjects was 3 to 84 years; mean age was 55.3 ± 15.3 years. The male to female ratio was 1.2:1. Majority of patients, 42(50.6%) had cerebral infarction compared with 23(27.7%) who had hemorrhagic events. However, 18(21.7%) patients had apparently normal CT findings. We found that only 31% of all stroke patients presented for imaging within 12 hours, while 46% failed to present within 24 hours of symptom onset.
The mean presentation time for CT imaging was 70 hours (SD ± 94 hours) with a median time of 24 hours. No patient presented in the time frame of less than 3 hours. Only 6 (7.2%) patients presented for CT within six hours of their onset of symptoms. Also the estimated CT presentation time revealed that 57 (68.7%) patients presented more than 12 hours after the onset of symptoms (Table 1).
Table 1.
Distribution of CT finding by time of presentation for CT Imaging in stroke patients before or after a 12-hour period.
| CT presentation time | CT finding | Total N (%) | X2 | P-value | |
|---|---|---|---|---|---|
|
| |||||
| Haemorrhagic | Infarct + | ||||
| Normal* | |||||
|
| |||||
| ≥12 hours | 11(13.2) | 15(24.1) | 26(31.3) | ||
| >12hours | 12(14.5) | 45(54.2) | 57(68.7) | ||
| 23(27.7) | 60(72.3) | 83(100.0 | 4.027 | 0.045 | |
all patients with an apparent normal CT finding had a clinical syndrome of stroke indicating a non-identification of an ischemic infarct
Of those who presented within 12 hours of ictus, more were haemorrhagic (Table 1). Sixty patients (72.3%) were diagnosed with non-haemorrhagic stroke on CT (p<0.05). Only 24% of patients with intra-cerebral hemorrhage (ICH) presented after 24 hours. Forty-five (78.9%) of the patients that presented after 12 hours of onset of their symptoms had either a normal CT finding or a definite ischemic stroke (P < 0.05). Patients with ICH presented for CT imaging earliest, with 60.1% presenting within 24 hours compared with 51.7% of those with cerebral infarct (CI). Furthermore, less than 25% of patients with ICH presented after 24 hours.
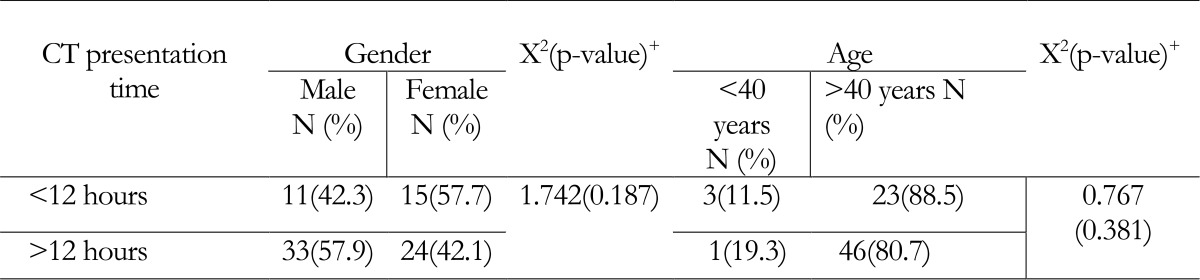
Age had no statistically significant influence on the CT imaging presentation time. (p=0.381) (Table 2). Gender also did not significantly influence the time of CT imaging. (P=0.187)
Table 2.
Age and sex distribution of stroke patients by time of presentation for CT Imaging before or after a 12-hour period
(p<0.05 is considered significant)
There were more male patients 26 (40.0%) compared with their female counterparts 16 (24.6%) with cerebral infarction, while more female patients 13 (20.0%) had haemorrhagic stroke compared to their male counterparts 10 (15.4%). This was also not statistically significant (p=0.153).
DISCUSSION
This study primarily examined the presentation time for computed tomography among Nigerian stroke patients and found that it varied significantly with stroke type. The greatest delay for neuroimaging was observed in patients with cerebral infarction (CI). This was not unexpected, since some patients with CI may present with only mild deficits and may lack significant alterations in speech, strength, or gait and may not present with dramatic symptoms such as loss of consciousness. Other contributory factors maybe the occasional hope that symptoms resolve spontaneously, use of alternative therapy or delay by a poor referral and transportation system.14
The scarcity of facilities and human resources for prevention, investigation, acute care and rehabilitation of stroke patients in Nigeria and other parts of Africa is widely reported.14-16
Cerebral infarcts in stroke patients often result from small-vessel disease, producing lacunar infarcts that sometimes have milder symptoms and signs than a large middle cerebral artery stroke or an intracerebral haemorrhage (ICH). In our study, patients with ICH presented for neuroimaging earlier, with 60.1% presenting within 24 hours compared with 51.7% of those with CI. Furthermore, less than a quarter of patients with ICH presented after 24 hours. This is understandable since ICH typically presents with rapid and dramatic alteration in mental status, features of raised intracranial pressure and/or marked focal signs and symptoms that usually necessitate immediate hospital visit. Additionally, we may make an assumption that, patients who had apparently normal CT findings despite being symptomatic for stroke probably had an ischemic event that was not immediately obvious on CT. Such assumptions still did not positively influence their presentation time for imaging. A diffusion weighted imaging (DWI) study using MRI would normally have revealed areas of fluid restriction indicative of hyperacute or acute ischaemic stroke that was not instantly evident on CT.
With the advances made in thrombolytic therapy for eligible stroke patients, who are usually selected on the basis of the index stroke not being greater than 4.5 hours; the need for early presentation and imaging diagnosis is paramount to stroke management. Information obtained from witnesses, is known to be unreliable17 . Therefore early presentation and imaging cannot be overemphasized and the goal of any healthcare system regarding stroke care would be to achieve this time window for the most favorable outcome for the patient. None of our patients presented for imaging within 3 hours of ictus. There are several possible explanations for this delay. Some of these factors have been enumerated by previous authors working in similar environments.14, 17 Recent studies from Nigeria and other parts of Africa indicate that a great proportion of people were not aware of the warning signs of a stroke 19-22 .This supports the assertion that patients' lack of knowledge about stroke may be a major factor responsible for delayed presentation in hospitals 16.
Previous authors in Nigeria had examined the pattern and presentation of stroke in the hospitals. These reports, focused majorly on the arrival times and clinical impression with no report of the timing of imaging 18, 20. This study however is arguably the first to evaluate the pattern of presentation for neuroimaging in Nigeria. This is even more relevant with the changing and updated definitions of stroke, which is now based on imaging finding.20
Stroke currently represents about 5 to 11% of medical admissions in Nigeria.20-22 With this growing burden, it becomes imperative to strengthen hospital protocols to ensure early imaging diagnosis for stroke patients as it has been aptly described that 'Time is brain' .23,24 The slightly higher proportion of males 1.2:1 is in keeping with other studies that reported male preponderance in stoke patients.25
The age range in this study covers a spectrum of relatively all age groups with a mean age of 55 years. This age bracket is where the risk factors for stroke are most prevalent and is in keeping with other studies on the epidemiology of stroke in Nigeria 26-28.
Age did not present as a relevant factor in the determination of the stroke type or the presentation time for imaging. Sixty (72.3%) had ischaemic stroke while 23 (27.7%) had intracerebral haemorrhage (ICH). This pattern is relatively comparable with other Nigerian studies.24, 25 We also found no significant sex predilection to particular stroke type, a finding also previously reported in South-West Nigeria.25
Despite the fact that imaging is regarded as the rate limiting step in the management of stroke patients, several worldwide studies have shown that pre-hospital delays constitute a major component to the delay in treatment 29. A comprehensive review of these delays however failed to represent Africa not withstanding the growing burden of stroke in African states. Our study highlights the dismal presentation times that may be seen in many centers in Africa. This relatively long time delay time excludes many patients from being considered for thrombolytic therapy with recombinant tissue Plasminogen Activator (r-tPA) and may contribute to longer subsequent in-hospital delays if imaging evaluation is performed before planning of care. Majority of those who may benefit from early/ timely intervention with r-tPA are patients with ischemic stroke but because of the delayed pattern of their presentation for imaging, such patients may never be able to access such treatments which are intricately time bound. Globally and mostly in Nigeria, few studies have explored pre-hospital delay which may consequently affect in-hospital delay times for stroke patients, particularly given that these events are not independent of one another.30-31 With an understanding of the possible multifactorial challenges that results in pre and in -hospital delays, local quality improvement initiatives such as the World Health Organization's stepwise approach to stroke should be developed by developing countries like Nigeria.21,32
This would help address and improve treatment care indicators, especially timely initiation of care for groups most likely to obtain the greatest benefit such as ischaemic stroke patients. In our next effort we would explore more closely some of the possible predictors of delays in stroke imaging in our hospitals in Nigeria.
Limitations
There is a possibility of under or over estimating the actual delay preceding time of presentation for neuroimaging in this study. This is because, many patients at our center after receiving a request for a CT still have to source for funds, undergo rigorous processes of registration and payment before the service is rendered. In addition, information regarding timing of the event is often obtained from a relative; therefore, the time given is usually an estimate or the "best guess" as is often the case with cases of CI, who wake up with a deficit that may have occurred during sleep; 17 which indicates that the onset was probably some hours prior. Other limitations include; the use of request cards and not case files which may have provided additional details. Also, there is a likelihood of a selection bias as about 60% of cases were discarded for incomplete information.
CONCLUSION
A mean CT imaging presentation time of about 70 hours for stroke patients in a major tertiary Nigerian hospital represents a significant delay in stroke care and management. This undesirable delay is also considerably greater among ischemic stroke patients. The long time interval before imaging diagnosis leaves little room for meaningful intervention that could limit disability in stroke patients.
ACKNOWLEDGEMENT
The authors would like to recognize the support NIH/ NINDS grant (1RN25NS080949) "Improving Neurologic Outcome Measurement for Interventional Research in Ibadan, Nigeria" , which helped in developing research capacity to carry out this work.
Conflict of interest
The authors disclose that they have no conflict of interest in their participation in this work.
REFERENCES
- 1.Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990-2010: Findings from the Global Burden of Disease Study 2010. The Lancet. 2014; 383: 245–255. doi: 10.1016/s0140-6736(13)61953-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Owolabi MO. Consistent determinants of poststroke health-related quality of life across diverse cultures: Berlin-Ibadan study. Acta Neurol Scand. 2013 Nov;128(5):311–320. doi: 10.1111/ane.12126. [DOI] [PubMed] [Google Scholar]
- 3.Wilkinson PR, Wolfe CD, Warburton FB, et al. A long term follow-up of stroke patients. Stroke. 1997; 28:507–512. doi: 10.1161/01.str.28.3.507. [DOI] [PubMed] [Google Scholar]
- 4.Reed DM. The paradox of high risk of stroke in populations with low risk of coronary heart disease. Am J Epidemiol. 1990; 131:579–588. doi: 10.1093/oxfordjournals.aje.a115542. [DOI] [PubMed] [Google Scholar]
- 5.O Donnell MJ, Xavier D, Liu L, et al. INTERSTROKE investigators. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010 Jul ;376(9735):112–23. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 6.Sacco RL, Kasner SE, Broderick JP, et al. American Heart Association Stroke Council, Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention; Council on Peripheral Vascular Disease;Council on Nutrition, Physical Activity and Metabolism. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064–2089. doi: 10.1161/STR.0b013e318296aeca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paul SL, Srikanth VK. The large and growing burden of stroke. Curr Drug Targets. 2007;8:786–793. doi: 10.2174/138945007781077418. [DOI] [PubMed] [Google Scholar]
- 8.Nor AM, Davis J, Sen B, et al. The Recognition of Stroke in the Emergency Room (ROSIER) scale: development and validation of a stroke recognition instrument. Lancet Neurol. 2005;4:727–734. doi: 10.1016/S1474-4422(05)70201-5. [DOI] [PubMed] [Google Scholar]
- 9.Wahab K. The burden of stroke in Nigeria. International journal of stroke. 2008. pp. 290–2. [DOI] [PubMed]
- 10. Sagui E. Stroke in sub-Saharan Africa. Med Trop. 2007; 67: 596–600. [PubMed] [Google Scholar]
- 11.Adams HP , Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups. Stroke. 2007; 38:1655–1711. doi: 10.1161/STROKEAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- 12.Ogun SA, Ojini FI, Ogungbo B, et al. Stroke in South-West Nigeria. Stroke. 2005; 36:1120–1122. doi: 10.1161/01.STR.0000166182.50840.31. [DOI] [PubMed] [Google Scholar]
- 13. Wardlaw JM. Diagnosis of stroke on neuroimaging. BMJ. 2004. pp. 328–655. [DOI] [PMC free article] [PubMed]
- 14.Ogbole GI, Ogunseyinde AO, Obajimi MO, et al. Experience with three-dimensional computed tomographic angiography in Ibadan, Nigeria. Niger J Clin Pract. 2010; 13:187–194. [PubMed] [Google Scholar]
- 15.Kaukab S, Mazhar B. How Much Time Lapses Between Stroke onset and Acquisition of CT Scan Brain? Ann. Pak. Inst. Med. Sci. 2009; 5: 269–270. [Google Scholar]
- 16.Clifton RL, Suh D, Bueno M, Kostis JB. Delay in Presentation and Evaluation for Acute Stroke. Stroke. 2001;32:63–66. doi: 10.1161/01.str.32.1.63. [DOI] [PubMed] [Google Scholar]
- 17.Yu RF, San J, Maria CZ, et al. Sources and reasons for delays in the care of acute stroke patients. J Neurol Sci. 2002;15:199:49–54. doi: 10.1016/s0022-510x(02)00103-x. [DOI] [PubMed] [Google Scholar]
- 18.Owolabi LF, Ibrahim A. Stroke in young adults: a prospective study from northwestern Nigeria. ISRN Neurol. 2012; 2012:468706. doi: 10.5402/2012/468706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Owolabi MO. Taming the burgeoning stroke epidemic in Africa: stroke quadrangle to the rescue. West Indian med. j. 2011; 60: 412–421. [PubMed] [Google Scholar]
- 20.Ekeh B, Isamade E. Time of presentation of stroke patients in a tertiary hospital in Northern Nigeria, West Africa. J Med Investig Pract . 2014;9:1–4. [Google Scholar]
- 21.Chukwuemeka O Eze, Christian E. Agu, Uma A Kalu, Chidiegwu A Maduanusi Sunday Nwali T, Chika, Igwenyi The Pattern and Presentation of Stroke in Federal Teaching Hospital Abakaliki (FETHA) South-East Nigeria Journal of Biology, Agriculture and Healthcare . 2013;3(No.11) [Google Scholar]
- 22.Owolabi LF, Nagoda M. Stroke in Developing Countries: Experience at Kano, Northwestern Nigeria. Sudan journal of medical sciences. 2012;7:9–14. [Google Scholar]
- 23.Barriers of Thrombolysis Therapy in Developing Countries. Stroke Research andTreatment. 2011. http://dx.doi.org/10.4061/2011/686797 . [DOI] [PMC free article] [PubMed]
- 24.Gonzalez RG. Imaging-Guided Acute Ischemic Stroke Therapy: From "Time is Brain" to "Physiology is Brain". AJNR Am J Neuroradiol . 2006 . Apr 27, pp. 728–735. [PMC free article] [PubMed]
- 25.Ogun SA, Ojini FI, Ogungbo B, et al. Stroke in Southwest Nigeria. A 10-year review. Stroke. 2005;36: 1120–1122. doi: 10.1161/01.STR.0000166182.50840.31. [DOI] [PubMed] [Google Scholar]
- 26.Owolabi MO, Ugoya Platz T. Racial disparities in stroke risk factors: the Berlin-Ibadan experience; a retrospective study. Acta Neurol Scand. [DOI] [PubMed]
- 27. Wahab KW. The burden of stroke in Nigeria. International Journal of Stroke. 3: 290–292. doi: 10.1111/j.1747-4949.2008.00217.x. [DOI] [PubMed] [Google Scholar]
- 28.Morris DL, Rosamond W, Madden K, et al. Prehospital and emergency department delays after acute stroke: the Genentech Stroke Presentation Survey. Stroke. 2000; 31:2585–2590. doi: 10.1161/01.str.31.11.2585. [DOI] [PubMed] [Google Scholar]
- 29.Marshall J. Diurnal variation in occurrence of strokes. Stroke. 1977; 8:230–231. doi: 10.1161/01.str.8.2.230. [DOI] [PubMed] [Google Scholar]
- 30. Moser D, Kimble L, Alberts M, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: A scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circ. 2006; 114:175–189. doi: 10.1097/01.JCN.0000278963.28619.4a. [DOI] [PubMed] [Google Scholar]
- 31.Katzan IL, Graber TW, Furlan AJ, et al. Cuyahoga County operation stroke speed of emergency department evaluation and compliance with National Institutes of Neurological Disorders and Stroke time targets. Stroke. 2003; 34:994–998. doi: 10.1161/01.STR.0000060870.55480.61. [DOI] [PubMed] [Google Scholar]
- 32.Dalal P, Bhattacharjee M, Vairale J, Bhat P. Mumbai Stroke Registry (2005-2006) - Surveillance using WHO Steps Stroke Instrument - Challenges and Opportunities. J Assoc Physician India. 2008. pp. 675–680. Accessed at http://www.japi.org/september_2008/o_675.pdf . [PubMed]