Abstract
Background: Nowadays, for quality improvement, measuring patient safety culture (PSC) in healthcare organizations is being increasingly used. The aim of this study was to clarify PSC status in Iranian hospitals using a meta-analysis method.
Methods: Six databases were searched: PubMed, Scopus, Google Scholar, Cochrane Library, Magiran, SID and IranMedex using the search terms including patient safety, patient safety culture, patient safety climate and combined with hospital (such as "hospital survey on patient safety culture"), measurement, assessment, survey and Iran. A total of 11 articles which conducted using Hospital Survey on Patient Safety Culture (HSOPSC) questionnaire initially were reviewed. To estimate overall PSC status and perform the meta-analyses, Comprehensive Meta-Analysis (CMA) software v. 2 was employed.
Results: The overall PSC score based on the random model was 50.1%. "Teamwork within hospital units" dimension received the highest score of PSC (67.4%) and "Non-punitive response to error" the lowest score (32.4%). About 41% of participants in reviewed articles evaluate their hospitals’ performance in PSC as ‘excellent/very good’. Approximately %52.7 of participants did not report any adverse event in the past 12 months.
Conclusion: The results of this study show that Iranian hospitals’ performances in PSC were poor. Among the 12 dimensions of HSOPSC questionnaire, the "Non-punitive response to error" achieved the lowest score and could be a priority for future interventions. In this regard, hospitals staff should be encouraged to report adverse event without fear of punitive action.
Keywords: Patient safety, Culture, Quality improvement, HSOPSC questionnaire, Iranian hospitals, Meta-analysis
Introduction
Quality in healthcare has different dimensions and elements (1-4), of which patient safety (PS) is one of the most important dimensions (5). PS is a serious global challenge and a very important dimension of healthcare quality (6-8). According to WHO, in low and middle income countries (LMIC) one out of ten patients is harmed while receiving health services (9). Institute of Medicine (IOM) report entitled "To Err Is Human" showed that more than 98 thousand patients die in the United States every year as a result of medical errors (10). For this reason PS has received considerable focus from policy-makers and other stakeholders (11).
Patient Safety Culture (PSC) is an important factor of PS in healthcare system (12). The IOM offers that the very important challenge to achieve a safer healthcare system is to improve the PSC (13). Measurement of PSC is a top priority aim to improve quality of PS (14-20). Neiva and Sorra (15) defined PSC as: “the product of individual and group values, attitudes, perceptions, competencies, and patterns of behavior that determine the commitment to, and the style and proficiency of, an organization's safety management”. Previous studies results show that there is a positive relationship between high PSC and safety performance in hospitals (good PS) (14,21).
Globally, several international organizations attempted to promote PSC: the World Alliance for Patient Safety (WAPS), the National Patient Safety Agency (NPSA), the Agency for Healthcare Research and Quality (AHRQ) and the Australia Commission of Safety and Quality (ACSQ) (22-24). In this regard, several instruments have been developed to measure PSC (25-27). The Hospital Survey on Patient Safety Culture (HSOPSC) of AHRQ is a valid and reliable instrument to measure PSC in the hospitals (28-31). This tool is translated to many languages and validated psychometrically (32-34).
A review of the literature showed that PSC status in Iranian hospitals is not satisfactory (35). Thus, the aim of the current study was to clarify PSC status in Iranian hospitals through a meta-analysis of studies which used HSOPSC instrument in Iran.
Methods
A Meta-Analysis study was conducted in 2014, and the required data were collected searching following keywords: patient safety, patient safety culture, patient safety climate and its combination with hospital (such as “hospital survey on patient safety culture”), measurement, assessment, survey, and Iran, in Google Scholar, PubMed, Scopus, Cochrane Library, Magiran, Iranian scientific information (SID) and IranMedex. Manual journal and website searching was also conducted. To increase confidence level of identification of the articles, the reference lists of the selected articles were also searched through. Articles published from 2000 to 2014 were recruited.
The inclusion criteria for the study were: articles published in Persian and English languages, articles that measured PSC in hospital, and articles that measured PSC using HSOPSC instrument. Exclusion criteria included: articles that measured overall safety culture, articles that measured PSC in primary healthcare, articles that not measured all dimension of HSOPSC instrument, conference presentations, case reports, and interventional and qualitative studies. Two reviewers evaluated the articles according to the checklist of Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) (Appendix 1).
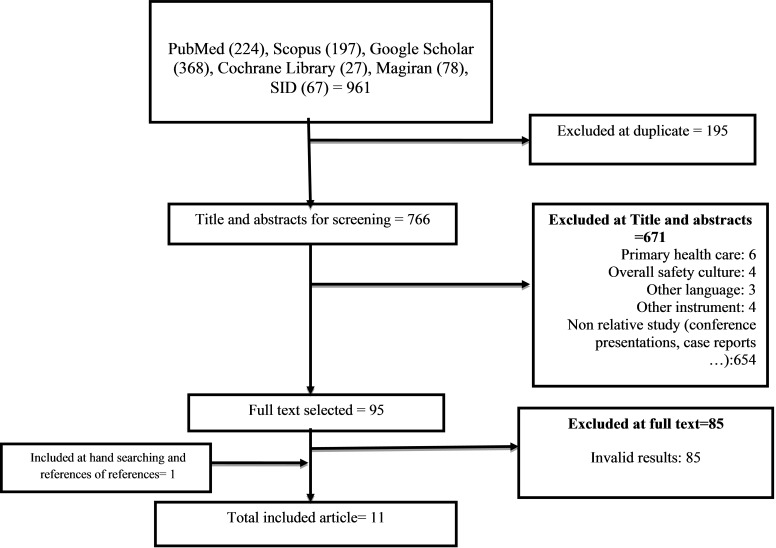
Of 961 retrieved articles, 11 articles were entered in the study (Fig. 1). After accurately studying and extracting the required data, the extracted data were summarized in the extraction table. Excel 2010 software was used to draw graphs. Endnote X5 software was used for organizing titles and abstracts and also identification of duplication studies (36). To calculate the overall PSC score, Comprehensive Meta-Analysis (CMA) software v. 2 and to report the results, forest plot were used. In forest plot, the size of each square shows sample size and lines on each side of the square show confidence interval.
Fig. 1 .
Literature review and retrieval flow diagram
PSC score was calculated based on random model with 95% confidence interval. In random models either all or some of the variables are treated as if they are from random causes. Random model was in contrast to fixed model that demonstrate the observed quantities in regard of explanatory variables which are treated as if the variables are not random.
HSOPSC questionnaire was designed by AHRQ. This instrument has 3 parts, 12 dimensions, 44 items and 2 single questions (Box. 1). All of questions are in the 5-point Likert scale (“Strongly disagree” to “Strongly agree”) or frequency (“Never” to “Always”) (37,38).
Box 1 . HSOPSC instrument dimensions (n = 12) .
| Dimensions | Number of Items |
| Outcome measure | |
| 1. Overall perception of safety | 4 |
| 2. Frequency of incident reporting | 3 |
| Unit level | |
| 3. Supervisor/manger expectations and actions promoting safety | 4 |
| 4. Organizational learning — continuous improvement | 3 |
| 5. Teamwork within hospital units | 4 |
| 6. Communication openness | 3 |
| 7. Feedback and communication about error | 3 |
| 8. Non punitive response to error | 3 |
| 9. Staffing | 4 |
| Hospital level | |
| 10. Hospital management support for patient safety | 3 |
| 11. Teamwork across hospital units | 4 |
| 12. Hospital handoffs and transitions | 4 |
| Number of incidents reported (last 12 month) | 1 |
| Patient safety grade | 1 |
Results
A total of 11articles initially were reviewed (39-49).The characteristics of the reviewed articles are shown in Table 1. The overall numbers of participants were 2972 (270 each study).
Table 1 . Characteristics of PSC studies that used HSOPSC in Iran .
| References | Sample size | 1* | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Mean±SD |
| Ravaghi et al;2012 | 216 staff | 49.2 | 65 | 53.8 | 62.8 | 14.8 | 12.2 | 44.3 | 45.8 | 57.2 | 37.3 | 45.4 | 40.5 | 44±16.5 |
| Ebadi fard azar et al;2010 | 145 staff | 64 | 66 | 66 | 67 | 51 | 57 | 62 | 62 | 61 | 63 | 63 | 61 | 61.9±4.3 |
| Abdi et al: 2010 | 311 staff | 15 | 19.5 | 27.5 | 47.2 | 17.8 | 35 | 24 | 18.2 | 19.9 | 29.7 | 19.9 | 14.1 | 23.9±9.5 |
| Agharahimi et al:2012 | 94 staff | 62 | 70.6 | 72.8 | 67.6 | 68.8 | 59.4 | 62.2 | 61.4 | 59.4 | 56.4 | 63.8 | 63.4 | 64±4.9 |
| Boghaei et al.:2010 | 500 staff | 59 | 69 | 67 | 80 | 31 | 36 | 49 | 55 | 62 | 45 | 56 | 42 | 54.25±14.3 |
| Izadi et al.;2012 | 196 staff | 67 | 73 | 76 | 75 | 54 | 48 | 65 | 62 | 69 | 68 | 70 | 66 | 66±8.2 |
| Arabloo et a; 2012 | 145 staff | 60 | 62 | 61 | 65 | 44 | 47 | 54 | 53 | 60 | 53 | 56 | 58 | 56.08±6.2 |
| Moghri et al;2013 | 725 staff | 53 | 62 | 55 | 65 | 23 | 35 | 43 | 42 | 48 | 42 | 44 | 46 | 47±10.3 |
| Adibi et al; 2012 | 90 staff | 44.6 | 67.9 | 51.9 | 69.8 | 21.9 | 26 | 29.6 | 29 | 46.3 | 50.9 | 65.9 | 50.3 | 46.2±16.6 |
| Yaghobi Far;2012 | 207 staff | 58.3 | 69.1 | 54.15 | 73.6 | 13 | 22.3 | 52.5 | 52.6 | 56.3 | 37.2 | 47.4 | 43.6 | 48.3±3.6 |
| Moghri etal; 2012 | 343 staff | 55 | 66 | 54 | 69 | 18 | 23 | 34 | 40 | 47 | 39 | 41 | 42 | 44±5.4 |
*1- Overall perception of safety, 2- Organizational learning/continuous improvement, 3- Supervisor/manager expectations & actions promoting safety,4- Teamwork within hospital units, 5- Non-punitive response to error, 6- Staffing, 7- Hospital management support for patient safety, 8- Teamwork across hospital units, 9- Hospital handoffs & transitions, 10- Communication openness, 11- Feedback & communication about error, 12- Adverse event reporting & recording, **including wide range of health care provider in hospital such as: physicians, nurses, clinical and non-clinical staff, pharmacy and laboratory staff, supervisors and hospital managers
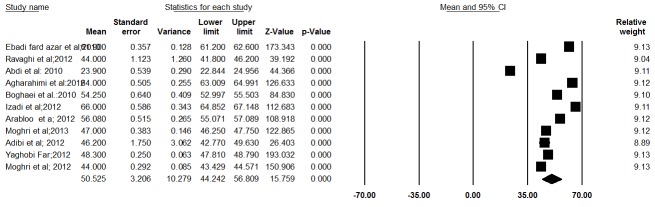
The PSC score based on the random effect model was determined to be 50.1% (95% confidence interval, lower limit= 43.4%, upper limit= 56.9%, I2= 99.8, Q-value= 5716.2, df = 10, and p< 0.001) (Fig. 2).
Fig. 2 .
Patients’ safety culture score in the evaluated studies with 95% CI (based on random model)
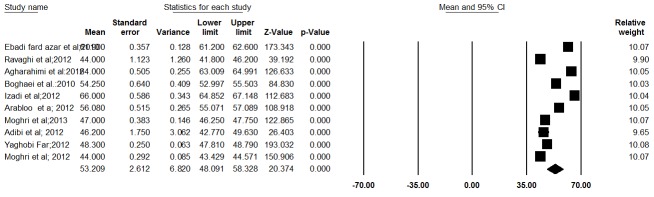
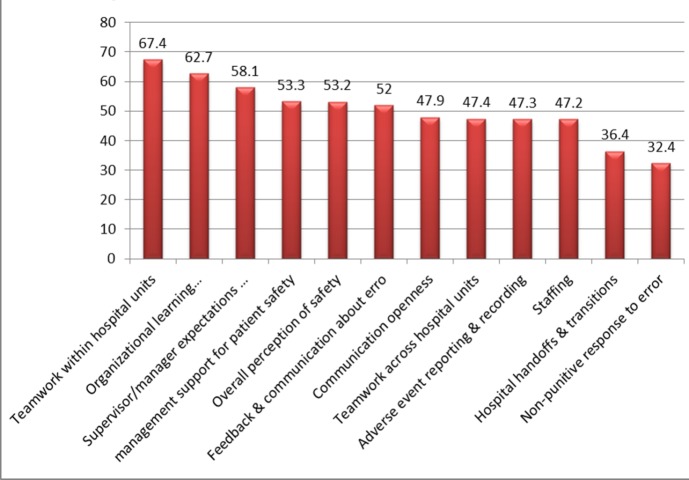
In this study due to high heterogeneity, sensitive analysis was done by excluding one of the studies (Abdi et al, 2010). Finally, after excluding this study, the PSC score changed to 52.8% (95% confidence interval, lower limit= 48%, upper limit= 57.6%, I2=96.8, Q-value= 3456.2, df = 9, p< 0.001) (Fig. 3). Mean of dimensions of HSOPSC questionnaire are shown in Fig. 4.
Fig. 3 .
Patients’ safety culture score in the evaluated studies with 95%CI (based on random model) after sensitive analysis (Abdi et al: 2010)
Fig. 4 .
Mean of 12 dimensions of HSOPSC in Iran
As shown in Fig. 4, “Teamwork within hospital units” dimension has the highest score of PSC (67.4%) and “Non-punitive response to error” has the lowest score (32.4%).
Mean of PSC status (excellent, very good, acceptable, poor, failing) in HSOPSC questionnaire are shown in Fig. 5. Accordingly, “very good” grade has the highest mean (%32.3) and “excellent” the lowest (%8.3).
Fig. 5 .
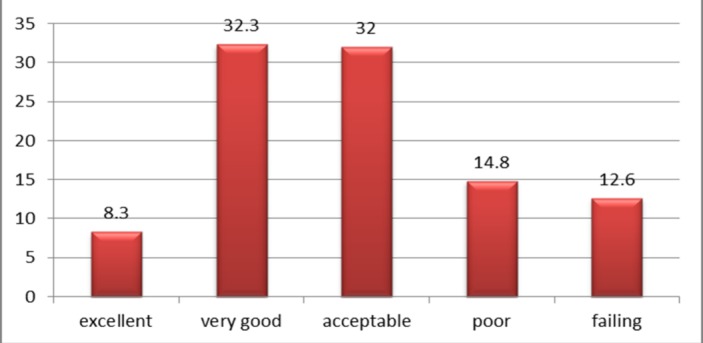
Average percentage of respondents giving their PSC grade
Mean of reporting number of adverse events in the past 12 months are shown in Fig. 6, which shows that approximately %52.7 of participants did not report any adverse event in the past 12 months.
Fig. 6 .
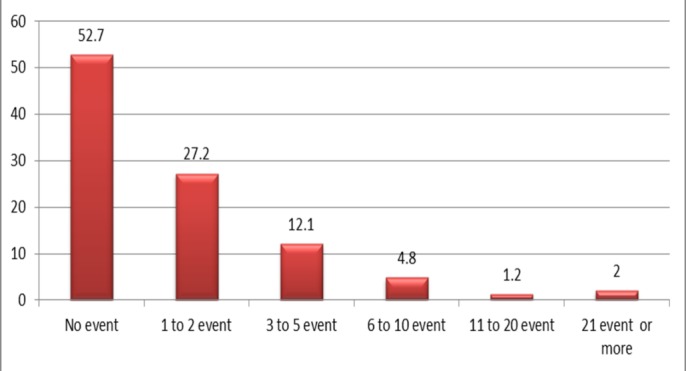
Average percentage reporting events in the past 12 months
Funnel plot of PSC shows that there is no symmetry in gathered data (Fig. 7).
Fig. 7 .
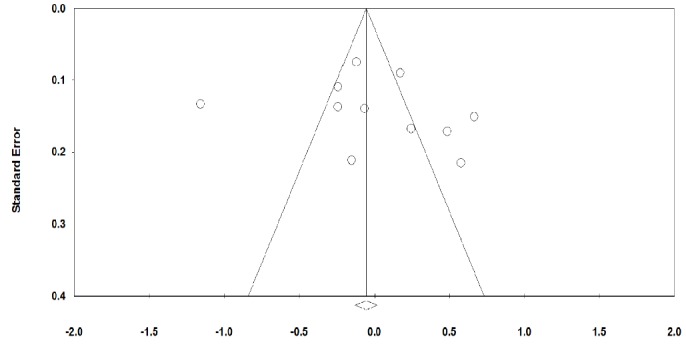
Funnel plot of Patients’ safety culture studies in Iran
Discussion
The HSOPSC questionnaire has been used to measure PSC in the High Income Countries (HICs), especially, the United States. In present study, we systematically reviewed the PSC status in Iran using studies that administered HSOPSC tool.
Overall, the mean response rate for the 12 PSC dimensions of the HSOPSC questionnaire in Iranian hospitals was 50.5%. This was lower than many of other previous studies, especially in HICs (15,16,50-54). Also mean response rate in some studies in LMIC was higher compared to that of current study (55-57).
Furthermore, the findings of this study demonstrated that "non-punitive response to error" dimension has lowest score among 12 dimensions of the HSOPSC questionnaire. Similar results were found in previous studies (57-59). van Geest and Cummings’ study showed that absence of a non-punitive response system to errors is an important barrier for identifications and reduction of errors in healthcare setting (60).Non-punitive response system defined as "the extent to which personnel feel that their mistakes are not held against them and that mistakes are not recorded in their personnel document" (61). Punitive response system can lead to underreporting adverse events in hospitals. Unreserved system is an effective method for risk reduction in hospitals, which can start with adverse event reporting without punishing, and continue with encourage to report and learning from adverse events.
The present study revealed that about 41% of participants evaluate their hospitals’ PSC status as ‘excellent /very good’. El-Jardali and colleagues study in Lebanese hospitals demonstrated that about 70% of participants evaluated their hospitals PSC status as ‘excellent/very good’ (55). One study reported a higher ‘excellent/very good’ for PSC than this study (62,63).
According to the reviewed articles in this study, about 52% of participants did not report any adverse event in the past 12 months. Contrary to this study, El-Jardali and colleagues showed that about 60% of participants did not completed any event in the past 12 months (55). Also, Jasti and colleagues showed that 64% of internal medicine house staff in academic teaching hospital did not report an adverse event in the past 12 months (62). Possible reasons for lower rate of reporting adverse events in current study might be the followings: no adverse event occurred in the hospitals during this period; or, staff did not report adverse events due to punishment system in the hospitals. The first reason seems to be impossible due to frequent reports of adverse events or medical errors in the hospitals (64-66). Therefore, hospitals managers better off to change current punishment system into participating system for improvement of PS. Hospital managers should try to remove scold, fear and silence from their system (67).
According to published years of reviewed articles in this study (from 2010 to 2013), it revealed that PSC is a very new concept in Iranian hospitals and unfortunately this issue has been neglected. In Iran, the PSC received attention due to PS friendly hospital initiatives since 2010, which was started in 10 hospitals and recently, Ministry of Health and Medical Education (MOHME) has decided to expand this program to 50 more hospitals (68). Also from 2009 in Iranian healthcare system, Clinical governance has been introduced as a framework to quality improving of hospitals services (69,70). These and other similar programs such as hospital accreditation are very useful and important for PSC improvement, but, it should be noted that improvement of PSC in hospitals and other organizations is highly related to Continues Quality Improvement (CQI) culture, organization leadership commitment, creating learning atmosphere in hospitals and a customer-oriented culture in hospitals in long-run.
The present study has some limitations such as no access to some of databases, and that, included articles were conducted only in hospitals.
Conclusion
Nowadays, measuring PSC in healthcare organizations is being increasingly welcome, especially in the HICs, and by Iranian hospitals. In this regard, review of related studies showed that Iranian hospitals’ performance in PSC filed is weak. Hence, improving PSC should be prioritized in Iranian hospitals. In this regard hospitals staff should be encouraged to report adverse events without fear of punishment.
Apendix1
Prevalence Critical Appraisal Instrument
Apendix1 . STROBE Statement-checklist of items that should be included in reports of observational studies .
| Item No | Recommendation | |
| Title and abstract | 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract |
| (b) Provide in the abstract an informative and balanced summary of what was done and what was found | ||
| Introduction | ||
| Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported |
| Objectives | 3 | State specific objectives, including any prespecified hypotheses |
| Methods | ||
| Study design | 4 | Present key elements of study design early in the paper |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection |
| Participants | 6 |
(a) Cohort study—Give the eligibility criteria, and the sources and methods of selection of participants. Describe methods of follow-up Case-control study—Give the eligibility criteria, and the sources and methods of case ascertainment and control selection. Give the rationale for the choice of cases and controls Cross-sectional study—Give the eligibility criteria, and the sources and methods of selection of participants |
|
(b)Cohort study—For matched studies, give matching criteria and number of exposed and unexposed Case-control study—For matched studies, give matching criteria and the number of controls per case |
||
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable |
| Data sources/ measurement | 8* | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group |
| Bias | 9 | Describe any efforts to address potential sources of bias |
| Study size | 10 | Explain how the study size was arrived at |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding |
| (b) Describe any methods used to examine subgroups and interactions | ||
| (c) Explain how missing data were addressed | ||
|
(d) Cohort study—If applicable, explain how loss to follow-up was addressed Case-control study—If applicable, explain how matching of cases and controls was addressed Cross-sectional study—If applicable, describe analytical methods taking account of sampling strategy |
||
| (e) Describe any sensitivity analyses | ||
| Result | ||
| Participants | 13* | (a) Report numbers of individuals at each stage of study—eg numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analyzed |
| (b) Give reasons for non-participation at each stage | ||
| (c) Consider use of a flow diagram | ||
| Descriptive data | 14* | (a) Give characteristics of study participants (eg demographic, clinical, social) and information on exposures and potential confounders |
| (b) Indicate number of participants with missing data for each variable of interest | ||
| (c) Cohort study—Summarize follow-up time (eg, average and total amount) | ||
| Outcome data | 15* | Cohort study—Report numbers of outcome events or summary measures over time |
| Case-control study—Report numbers in each exposure category, or summary measures of exposure | ||
| Cross-sectional study—Report numbers of outcome events or summary measures | ||
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (eg, 95% confidence interval). Make clear which confounders were adjusted for and why they were included |
| (b) Report category boundaries when continuous variables were categorized | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | ||
| Other analyses | 17 | Report other analyses done—eg analyses of subgroups and interactions, and sensitivity analyses |
| Discussion | ||
| Key results | 18 | Summarize key results with reference to study objectives |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence |
| Generalizability | 21 | Discuss the generalizability (external validity) of the study results |
| Other information | ||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based |
*Give information separately for cases and controls in case-control studies and, if applicable, for exposed and unexposed groups in cohort and cross-sectional studies.
Note: An Explanation and Elaboration article discusses each checklist item and gives methodological background and published examples of transparent reporting. The STROBE checklist is best used in conjunction with this article (freely available on the Web sites of PLoS Medicine at http://www.plosmedicine.org/, Annals of Internal Medicine at http://www.annals.org/, and Epidemiology at http://www.epidem.com/). Information on the STROBE Initiative is available at www.strobe-statement.org
Cite this article as: Azami-Aghdash S, Ebadifard Azar F, Rezapour A, Azami A, Rasi V, Klvany Kh. Patient safety culture in hospitals of Iran: a systematic review and meta-analysis. Med J Islam Repub Iran 2015 (23 August). Vol. 29:251.
References
- 1.Azami-Aghdash S, Mohammadi R. Using Tracer Methodology in Clinical Setting and Research to Measure and Improve Quality. J Clin Res Gov. 2013;2:39–40. [Google Scholar]
- 2.Azami-Aghdash S, Ghaffari S, Sadeghi-Bazargani H, Tabrizi JS, Yagoubi A, Naghavi-Behzad M. Developing Indicators of Service Quality Provided for Cardiovascular Patients Hospitalized in Cardiac Care Unit. JCTR. 2013;5(1):23–8. doi: 10.5681/jcvtr.2013.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tabrizi J, Gholipoor K, Asghari jafarabadi M, Farahbakhsh M, Mohammadzedeh M. Customer quality and maternity care in Tabriz urban health centers and health posts. J Clin Res Gov. 2012;1:12–5. [Google Scholar]
- 4.Farahbakhsh M, Sadeghi-Bazargani H, Nikniaz AR, Tabrizi JS, Zakeri A, Azami-Aghdash S. . Iran's Experience of Health Cooperatives as a Public-Private Partnership Model in Primary Health Care: A Comparative Study in East Azerbaijan HPP. 2012;2(2):287–98. doi: 10.5681/hpp.2012.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tabrizchi N, Sedaghat M. The first study of patient safety culture in Iranian primary health centers. Acta Med Iran. 2012;50(7):505–10. [PubMed] [Google Scholar]
- 6.Ebadi Fardazar F, Safari H, Habibi F, Akbari Haghighi F, Rezapour A. Hospitals' readiness to implement clinical governance. Int J Health Policy Manag. 2014;4(2):69–74. doi: 10.15171/ijhpm.2014.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arab M, Akbari Sari A, Movahed Kor E, Hos¬seini M, Toloui Rakhshan S, Ezati M. Patient Safety in Tehran University of Medical Sciences? General Hospitals, Iran. Iran J Public Health. 2013;42(3):306–13. [PMC free article] [PubMed] [Google Scholar]
- 8.Sheikhtaheri A. Near Misses and Their Importance for Improving Patient Safety. Iran J Public Health. 2014;43(6):853–4. [PMC free article] [PubMed] [Google Scholar]
- 9. 10 facts on patients safety. WHO, 2007.
- 10. Kohn L, Corrigan J, Donaldson M. To err is human: building a safer health system. Washington DC: National Academy Press; 2000. [PubMed]
- 11.Feng X, Bobay K, Weiss M. Patient safety culture in nursing: a dimensional concept analysis. J Adva Nurs. 2008;3(2):310–19. doi: 10.1111/j.1365-2648.2008.04728.x. [DOI] [PubMed] [Google Scholar]
- 12.Sochalski J. Quality of care, nurse staffing, and patient outcomes. Policy Polit Nurs Pract. 2001;2:9–18. [Google Scholar]
- 13. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed]
- 14.Mardon R, Khanna K, Sorra J, Dyer N, Famolaro T. exploring relationships between hospital patient safety culture and adverse events. J Patient Saf. 2010;6(4):226–32. doi: 10.1097/PTS.0b013e3181fd1a00. [DOI] [PubMed] [Google Scholar]
- 15.Ballangruda R, Hedelinb B, Louise Hall-Lord M. Nurses’ perceptions of patient safety climate in intensive care units: A cross-sectional study. Intensive Crit Care Nurs. 2012;28:344–54. doi: 10.1016/j.iccn.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Smits M, Wagner C, Spreeuwenberg P, van der Wa lG, Groenewe-gen PP. Measuring patient safety culture: an assessment of the clustering of responses at unit level and hospital level. Qual Saf Health Care. 2009;18:292–6. doi: 10.1136/qshc.2007.025965. [DOI] [PubMed] [Google Scholar]
- 17. Mohanty RP, Lakhe RR. TQM in service sectors. 2 ed. India: Jaico publishing; 2006.
- 18.Silimp eri D, Franco LM, Veldhuyze n T. et al. A framework for institutionalising quality assurance. Int J Qual Health Care. 2002;14:S67–73. doi: 10.1093/intqhc/14.suppl_1.67. [DOI] [PubMed] [Google Scholar]
- 19.Vatankhah S, Khalesi N, Ebadifardazar F, Ferdousi M, Naji H, Farahabadi SM. The role of nurse practitioners in health sector reform in Iran (2011) Iran J Nurs Midwifery Res. 2013;18(5):367–70. [PMC free article] [PubMed] [Google Scholar]
- 20.Bastani P, Vatankhah S, Salehi M. Performance Ratio Analysis: A National Study on Iranian Hospit?als Affiliated to Ministry of Health and Medical Educa-tion. Iran J of Pub Health. 2013;42(8):876–82. [PMC free article] [PubMed] [Google Scholar]
- 21.Singer S, Lin S, Falwell A, Gaba D, Baker L. Relationship of safety climate and safety performance in hospitals. Health Serv Res. 2009;44(2):399–420. doi: 10.1111/j.1475-6773.2008.00918.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen I, Li H. Measuring patient safety culture in Taiwan using the Hospital Survey on Patient Safety Culture (HSOPSC) BMC Health Serv Res. 2010;10:152–62. doi: 10.1186/1472-6963-10-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matsubara S, Hagihara A, Nobutomo K. Development of a patient safety climate scale in Japan. Int J Quality in Health Care. 2008;20(3):211–20. doi: 10.1093/intqhc/mzn003. [DOI] [PubMed] [Google Scholar]
- 24.Nie Y, Mao X, Cui H, He S, Li J, Zhang M. Hospital surv ey on patient safety cul ture in China. BMC Health Serv Res. 2013;13:228. doi: 10.1186/1472-6963-13-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campbell SM, Braspenning J, Hutchinson A, Marshall M. Research methods used in developing and applying quality indicators in primary care. Qual Saf Health Care. 2002;11:358–64. doi: 10.1136/qhc.11.4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chiu W, Yang C, Lin H. Development and implementation of a nationwide health care quality indicator system in Taiwan. Int J Qual Health Care. 2007;19:21–8. doi: 10.1093/intqhc/mzl063. [DOI] [PubMed] [Google Scholar]
- 27.Kirk S, Parker D, Claridge T, Esmail A, Marshall M. Patient safety culture in primary care: developing a theoretical framework for practical use. Qual Saf Health Care. 2007;16(4):313–20. doi: 10.1136/qshc.2006.018366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. A Draft National Strategy for Clinical Indicators in Scotland.NHS Quality Improvement Scotland 2006 2007; Available from: http://www.nhshealthquality.org.
- 29. Audit Commission. On Target: the practice of performance indicators. Audit Commission for Local Authorities and the National Health Service in England and Wales; 2000. Available online from: http://www.audit-commission.gov.uk/Products/NATIONAL-REPORT/266D51B7-0C33-4b4b-9832-7484511275E6/archive_mptarget.pdf.
- 30.Turpin RS, Darcy LA, McMahill C, Meyne K, Morton D, Rodriguez J. et al. A Model to Assess the Usefulness of Performance Indicators. Int J Qual Health Care. 1996;8(4):321–9. doi: 10.1093/intqhc/8.4.321. [DOI] [PubMed] [Google Scholar]
- 31. Marshall M, Campbell Stephen. Introduction to quality indicators in general practice. Marshall M, Campbell Stephen, Hacker J, Roland M, (Eds) In: Quality indicators for general practice: A practical guide for health professionals and managers. The Royal Society of Medicine Press Ltd; 2002.
- 32.Haugen A, Softeland E, Eide G, Nortvedt M, Karina Aase K, Harthug S. Patient safety in surgical environments: cross-countries comparison of psychometric properties and results of the Norwegian version of the hospital survey on patient safety. BMC Health Serv Res. 2010;10:279. doi: 10.1186/1472-6963-10-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bodur S, Filiz E. Validity and reliability of Turkish version of “ hospital survey on patient safety culture ” and perception of patient safety in public hospitals in turkey. BMC Health Serv Res. 2010;10:28. doi: 10.1186/1472-6963-10-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smits M, Dingelhoff IC, Wagner C, van der Wal G, Groenewegen WP. The psychometric properties of the 'Hospital Survey on Patien t Safety Culture' in Dutch hospitals. BMC Health Serv Res. 2008;8:230. doi: 10.1186/1472-6963-8-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moghri J, Nateghi E, Arab M, Moghri M, Akbari Sari AA, Omranikhoo H. et al. Measurement of Patient Safety Culture in Iranian hospitals: A National Baseline Study. J Clin Res Gov. 2013;2:47–52. [Google Scholar]
- 36.Sadeghi-Bazargani H, Tabrizi JS, Azami-Aghdash S. Barriers to evidence-based medicine: a systematic review. J Eval Clin Pract. 2014;20(6):793–802. doi: 10.1111/jep.12222. [DOI] [PubMed] [Google Scholar]
- 37. American Hospital Association, Risk Management Self - Assessment Manual. Chicago: American Hospital Association, 2000.
- 38. Adapted from Towards excellence in clinical governance: a framework for integrated quality, safety and risk management across HSE service providers, HSE, 2009.
- 39. Ravaghi H, Barati Marnani A, Hoseini A, Takbiri A. The Relationship between Health Care Providers' Perceptions of Patient Safety Culture and Patients' Perceptions of Medical Errors in Teaching Hospitals in Tehran: 2011. Health Management 2012;15(48):57-68.[In Persian].
- 40.Ebadi fard azar F, Rezapoor A, Tanoomand Khoushehmehr A, Bayat R, Arabloo J, Rezapoor Z. Study of patients’safety culture in Selected Training hospitals affiliated whith Tehran university of medical sciences. Hospital Quarterly. 2011;11(2):55–63. [In Persian]. [Google Scholar]
- 41.Abdi Z, Maleki M, Khosravi A. Staff perception about patient safety culture in selected hospitals of Tehran University of Medical Sciences. Payesh Quarterly. 2012;10(4):411–9. [In Persian]. [Google Scholar]
- 42.Agharahimi Z, Mostofi M, Jafari M, Raesi AR. Evaluation of staff attitudes about patients’ safety culture in Noor & Ali Asghar hospitals in Isfahan-2011. Hospital Quarterly. 2012;11(3):17–26. [In Persian]. [Google Scholar]
- 43.Baghaei R, Nourani D, Khalkhali H, Pirnejad H. Evaluating Patient Safety Culture in Personnel of Academic Hospitals in Urmia University of Medical Sciences in 2011. J of nurs and midwife faculty of Urmia. 2012;10(2):155–64. [In Persian]. [Google Scholar]
- 44.Izadi A, Drikvand J, Ebrazeh A. The Patient Safety Culture in Fatemeh Zahra Hospital of Najafabad, Iran. Health Information Management. 2013;9(6):895–907. [In Persian]. [Google Scholar]
- 45.Arabloo J, Rezapour A, Ebadi Fard Azar F, Mobasheri Y. Measuring Patient Safety Culture in Iran Using the Hospital Survey on Patient Safety Culture (HSOPS): an Exploration of Survey Reliability and Validity. IJHR. 2012;1(1):15–28. [Google Scholar]
- 46.Moghri J, Nateghi E, Arab M, Moghri M, Sari AA, Omranikhoo H. et al. Measurement of Patient Safety Culture in Iranian hospitals: A National Baseline Study. J Clin Res Gov. 2013;2:47–52. [Google Scholar]
- 47.Adibi H, Khalesi N, Ravaghi H, Jafari M, Jeddian AR. Development of an effective risk management system in a teaching hospital. JDMD. 2012;11(15):1–7. doi: 10.1186/2251-6581-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yaghobi Far MA, Takbiri A, Haghgoshaye E, Tabarraye Y. The survey of patient safety culture and recognizing its weaknesses and strengths in Sabzevar hospitals: 2011 Sabzevar Uni Med Sci J. 2012;20(2):154164[In Persian]. [Google Scholar]
- 49.Moghri j, Akbari Sari A, Rahimi Forooshani A, Arab M. Patient Safety Culture Status in General Hospitals Affiliated to Tehran University of Medical Sciences. Hakim Rese J. 2013;16(3):243–50 [In Persian]. [Google Scholar]
- 50.Campbell EG, Singer S, Kitch BT, Iezzoni LI, Meyer GS. Patient Safety Climate in Hospitals: Act Locally on Variation Across Units. The Joint Commission Journal on Quality and Patient Safety. 2010;36(7):319–26. doi: 10.1016/s1553-7250(10)36048-x. [DOI] [PubMed] [Google Scholar]
- 51.Moss F, Palmberg M, Plsek P. Quality improvement around the world: how much we can learn from each other. Qual Health Care. 2000;9:63–6. doi: 10.1136/qhc.9.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Seddon M, Marshall M, Campbell S. Systematic review of studies of clinical care in general practice in the United Kingdom Australia and New Zealand. Qual Health Care. 2001;10:152–8. doi: 10.1136/qhc.0100152... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Joint Commission Sentinel Event Glossary of Terms, 2005, http://www.jointcommission.org/ sentinalevents/se_glossary.htm (accessed November 11, 2008).
- 54. Health Information and Quality Authority. National Standards for Safer Better Healthcare: June 2012. Dublin: Health Information and Quality Authority; 2012.
- 55.El-Jardali F, Jaafar M, Dimassi H, Jamal D, Hamdan R. The current state of patient safety culture in Lebanese hospitals: a study at baseline. Int J Qual Health Care. 2010;22:386–95. doi: 10.1093/intqhc/mzq047. [DOI] [PubMed] [Google Scholar]
- 56.Chen IC, Li HH. Measuring patient safety culture in Taiwan using the Hospital Survey on Patient Safety Culture (HSOPSC) BMC Health Serv Res. 2010;10:152–62. doi: 10.1186/1472-6963-10-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.A AH. Measuring Patient Safety Culture in Riyadh's Hospitals: A Comparison between Public and Private Hospitals. J Egypt Public Health Assoc. 2009;84(5):479–500. [PubMed] [Google Scholar]
- 58.Handler S, Castle N, Studentski S, Perera S, Fridsma D, Nace D. Patient safety culture assessment in the nursing home. Qual Saf HealthCare. 2006;15:400–4. doi: 10.1136/qshc.2006.018408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Alahmadi HA. Assessment of patient safety culture in Saudi Arabian hospitals. Qual Saf HealthCare. 2010;19:1–5. doi: 10.1136/qshc.2009.033258. [DOI] [PubMed] [Google Scholar]
- 60. Van Geest J, Cummins D. An educational needs assessment for improving patient safety: results of a national study of phys-icians and nurses. National Patient Safety Foundation, 2003.
- 61.Jeongeun K, Kyungeh A, Minah K, Yoonsook H. Nurses' Perception of Error Reporting and Patient Safety Culture in Korea. Western J Nursing Res. 2007;29(7):827–44. doi: 10.1177/0193945906297370. [DOI] [PubMed] [Google Scholar]
- 62.Jasti H, Sheth H, Verrico M, Perera S, Bump G, Simak D. et al. Assessing Patient Safety Culture of Internal Medicine House Staff in an Academic Teaching Hospital. J Grad Med Educ. 2009:1–12. doi: 10.4300/01.01.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nie Y, Mao X, Cui H, He S, Li J, Zhang M. Hospital survey on patient safety culture in China. BMC Health Serv Res. 2013;13(228):1–11. doi: 10.1186/1472-6963-13-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kohn K, Corrigan J, Donaldson M. To err is human: building a safer health system. Washington (DC): National Academy Press; 1999. [PubMed]
- 65.Solberg LI, Ache SE, Averback BM, Hayek A, Schmitt MS, Lindquist TC. Can patient safety be measured by surveys of patient experiences? Jt Comm J Qual Patient Saf. 2008;34(5):266–74. doi: 10.1016/s1553-7250(08)34033-1. [DOI] [PubMed] [Google Scholar]
- 66.Akbari Sari A, Doshmangir L. An overview of methods for identifying and measuring adverse events in health care and their strengths and weaknesses. JHOSP. 2009;32:51–6. [Google Scholar]
- 67.Brandi A, Brasiliani L, Belli S, Ferrara A, Macconi L, Marilli R. et al. [Retrospective survey on falls among hospitalized patients] Assist Inferm Ric. 2002;21(3):125–30. [PubMed] [Google Scholar]
- 68.Holmstrom AR, Airaksinen M, Weiss M, Wuliji T, Chan XH, Laaksonen R. National and local medication error reporting systems: a survey of practices in 16 countries. J Patient Saf. 2012;8(4):165–76. doi: 10.1097/PTS.0b013e3182676cf3. [DOI] [PubMed] [Google Scholar]
- 69.Sadeghi-Bazargani H, Saadati M, Tabrizi JS, Jannatid A, Pourasghare F, Azami-Aghdash S. et al. Tabriz Clinical Governance Research Project (TCGRP): Study Protocol. J Clin Res Gov. 2014;2:76–80. [Google Scholar]
- 70.Azami-Aghdash S, Sadeghi-Bazargani H, ghasemi B, Mirzaei A, Abdollahi L, Asghari G. Preparation and priority setting of clinical governance performance indicators in dimensions of risk management and clinical effectiveness from the healthcare staff viewpoints. Int J Health Syst Disaster Manage. 2013;1(1):16–21. [Google Scholar]