Abstract
Background: Cardiovascular disease (CVD) is the cause of one third of deaths worldwide and this will progress because of increasing CVD's risk factors. The most basic task of dealing with the epidemic of CVD is primary prevention of risk factors. As Atherogenic Index of Plasma (AIP) is a strong marker to predict the risk of atherosclerosis and coronary heart disease, we assessed the correlation between AIP and other important factors.
Methods: This cross-sectional study was a part of national non-communicable risk factors surveillance system data that has been established since 2004 in Iran. This was done on 1000 people between 2008 and 2010. The study was approved by Ethics Committee of Mashhad University of Medical Science. Chi square, Mann-Whitney U, correlation tests were used in this study. Statistical analysis was performed using SPSS version 11. In all calculations, p <0.05 was considered as statistically significant level.
Results: The study population consisted of 500 men and 500 women with mean±SD age 41.9±14.2 years. According to the AIP category, 9.8% (98) were in low risk group, 12.7% (127) were in intermediate risk and 77.5% (775) were in increased risk of CVD. AIP was significantly correlated with waist circumference (r=0.35, p<0.001), BMI (r=0.33, p<0.001) and physical activity (r=-0.09, p<0.01).
Conclusion: AIP can be used as a regular monitoring index of CVD in every day practice, especially in persons with other cardiovascular risk factors.
Keywords: Risk Factor, Cardiovascular Disease, Atherogen
Introduction
Cardiovascular disease (CVD) is the cause of one third of deaths worldwide and this statue will progress because of increasing CVD's risk factors (1). In the United States the life time risk for incidence of CVD at age forty is 50% in men and 32% in women (2). The most basic task of dealing with the epidemic of CVD is primary prevention of risk factors and understanding how they interact together.
The most important risk factors for CVD consist of dyslipidemia, HTN, obesity, physical inactivity, poor diet and smoking (1,3-6). Among these, lipid profile of plasma is the major risk factors and predictor for CVD (7,8).
Dyslipidemia describe as elevated plasma concentration of lipid (triglyceride (TG) and total cholesterol (TC) and their blood transporting lipoproteins; HDL- Cholesterol, LDL-Cholesterol, VLDL-Cholesterol) (9-12). Strong scientific evidence indicates that there is a strong association between incidence of CVD and high level of LDL-C and also low level of HDL-C (12,13); therefore the LDL-C/HDL-C ratio is often calculated to estimate cardiovascular risk (14). On the other hand, high level of TG has been related with an increased LDL-C particles and increased cardiovascular risk (12,15). On that basis, atherogenic dyslipidemia, defined as high LDL-C/HDL-C ratio and hyper TG, is associated with high cardiovascular risk (14,16).
Many clinical studies make effort to introduce a better marker of atherogenic dyslipidemia that can predict the risk of CVD to be useful for evaluating response to treatment instead of the classical ratio (14). It has been shown that Atherogenic Index of Plasma (AIP) is a strong marker to predict the risk of atherosclerosis and coronary heart disease (12,17-22). AIP reflect the true relationship between protective and atherogenic lipoprotein and is associated with the size of pre- and anti- atherogenic lipoprotein particle (23). AIP is calculated according to the formula, log(TG/HDL-C) (8,12,14,17,18,24). It has been suggested that an AIP value of under 0.11 is associated with low risk of CVD; the values between 0.11 to 0.21 and upper than 0.21 are associated with intermediate and increased risks, respectively (23,25).
As we know, a large number of cardiovascular risk factors are modifiable, and so far, many efforts have been done but much more is needed (1). For this purpose it is necessary to know how these different risk factors affect each other. Within this context, we assessed the correlation between AIP, as a major risk factor of CVD, and the other important factors, like physical activity, BMI, waist circumference, HTN, FBS and lipid status. The result of this study can be applied to return the bleak prognosis of CVD and also can help policy makers to implement a population strategy in association with a high risk group strategy for CVD prevention and reduce the burden of cardiovascular disease in the future decades.
Methods
Study population
This cross-sectional study was a part of national non-communicable risk factors surveillance system data that has been established since 2004 in Iran. This study has been done on 1000 people (500 men and 500 women) between 2008 and 2010, who were referred to different urban health centers of Razavi Khorasan Province. Primary care physicians were trained to complete the check list. All study participants signed an informed consent and the study was approved by Ethics Committee of Mashhad University of Medical Science.
Blood Sampling
Blood samples were taken from all participants after 12-14 hours fasting to determine the lipid profile and FBS. All samples were checked in central laboratory of state health center.
Body Mass Index
Body Mass Index (BMI) was calculated based on the following formula, weight (kg) divided by the square of height (m2) (26). As we know, BMI is associated with whole body fat mass (27) and to some extent can reflect the physiological effect of whole body fat mass, although it has some limitations (28), it has been used widely because it is easy to calculate.
Body weight was measured using an analogue scale and participants only had one uniform layer and height was measured using stadiometer. Participants were divided into four groups according to their BMI: Underweight (BMI<18.5), Normal (18.5≤ BMI<25), Over weight (25≤BMI<30) and Obesity (BMI≥30) (26).
Physical Activity
The American Heart Association recommends 30-60 minutes of aerobic exercise 3-4 times per week to prevent cardiovascular disease (29). According to this category our participants were divided into three groups. In our study, physical activity included aggregation of occupational activity, transport related activity, and recreational activity per week, therefore:
Low active person: person with less than 90 minutes of physical activity during a week.
Active person: person with 90-240 minutes of physical activity during a week.
Highly active person: person with more than 240 minutes of physical activity during a week.
Waist Circumference
BMI indicate total body fat mass whereas waist circumference is indicator of central body fat mass and is associated with abdominal obesity (30,31). Evidence demonstrate that abdominal obesity is a strong risk factor for cardiovascular disease and type 2 Diabetes Mellitus (32).
According to the National Institute of Health guidelines, men with waist circumference more than 102 cm and women with waist circumference more than 88 cm are at higher risk of obesity disorders than the other persons (33). Recent studies show that these measures are useful for the purpose of predicting the risk of metabolic disorder (34,35).
Waist circumference was measured using a flexible tape, in the standing position and in midway between the lowest rib and the superior border of iliac crest.
Blood Pressure
We measured participant's blood pressure in three fold after 5 to 10 minutes rest using OMRON-M7 brand digital blood pressure monitors. All monitors were adjusted every day.
Statistical Analysis
Participant characteristics were described by percentage, means and standard deviation (SD). Initially, in each participant we investigate the relation between AIP and physical activity and at a second stage we check the relation between AIP and BMI and also waist circumference, blood pressure, FBS and lipid profile was measured using correlation tests. In order to compare two groups or more, we used chi square test or Mann-Whitney U test. Statistical analysis was performed using the SPSS version 11. In all calculations, p<0.05 was considered as statistically significant level.
Results
The study population consisted of 500 men and 500 women aged 17-67 years (mean±SD 41.9±14.20). About 54% (n=536) of our participants were living in urban areas. While 432 (43.2%) and 362 (36.2%) were employee and housewives respectively; only 44 (4.4%) subjects were unemployed.
In clinical examination, the mean±SD of AIP was 0.4±0.23 and 0.3±0.24 respectively in men and women, according to the AIP category that mentioned before, 9.7% (n=97) were in low risk group, 12.7% (n=127) were in intermediate risk and 77.5% (n=775) were in increased risk of CVD.
Overally, mean±SD BMI was 25.1±5.20; within underweight (BMI<18.5) and normal (18.5<BMI<24.9) ranges, men had taken the dominance, but women had taken the lead in obese (BMI>30) and very obese (BMI>35) ranges with much higher ratios.
The mean±SD of waist circumference was 85.9±13.20 for men and 86.7±14.60 for women. Considering the normal ranges, it was found that 714 subjects (71.4%) had normal waist circumference.
While 192 (19.2%) participants reported having a job that requires vigorous activity, 566 (56.6%) had a job with moderate activity. In recreational time, 131 (13.1%) reported having a hobby or sport that elevated their respiration and heart beat for more than 10 minutes. Besides, 207 (20.7%) had hobbies with moderate activity. When we pooled theses three dimensions of activity and used the AHA categories, it was revealed that 186 (18.8%) were low active, 167 (16.9%) were active and 638 (64.4%) were highly active. This variable was significantly different in two genders (p<0.001).
As shown in Table 1, more than 76.5% of both genders had normal blood pressure. Mean systolic blood pressure had higher levels in men while mean diastolic blood pressure had higher levels in women, both were statistically significant. By evaluating the past medical history of subjects, it was revealed that 8% of subjects had a history of drug prescription for hypertension.
Table 1 . Descriptive statistics of comparison between two genders by multiple factors .
| Male | Female | p | |
| Atherogenic Index of Plasma | 0.41±0.23* | 0.35±0.24 | p=0.001 |
| BMI (kg/m2) | 24.2±4.9 | 25.9±5.30 | p<0.001 |
| Systolic Blood Pressure (mmHg) | 125±18.2 | 121.5±21.40 | p=0.006 |
| Diastolic Blood Pressure (mmHg) | 78.4±12.7 | 80.3±13.30 | p=0.025 |
| Triglyceride (mg/dl) | 119±45 | 119.3±70.20 | p=0.947 |
| Total Cholesterol (mg/dl) | 186.5±42.40 | 194.2±48.10 | p=0.019 |
| HDL (mg/dl) | 45.7±17.90 | 50.6±15.70 | p<0.001 |
| LDL (mg/dl) | 118.9±38.40 | 121.1±46.30 | p=0.477 |
|
FBS (mg/dl) Waist circumference(cm) |
88.2±24.00 85.9±13.20 |
89.8±29.70 86.7±14.60 |
p=0.424 p=0.378 |
*Mean± SD, ** Not Significant
Although having a higher level of HDL is preferred, women had higher levels of total cholesterol, and LDL. Thirty four subjects (4.4%) had previously diagnosed diabetes, 41 (5.3%) had impaired fasting glucose and rest of them (90.3%) had normal blood sugar. The mean FBS was 89 mg/dl.
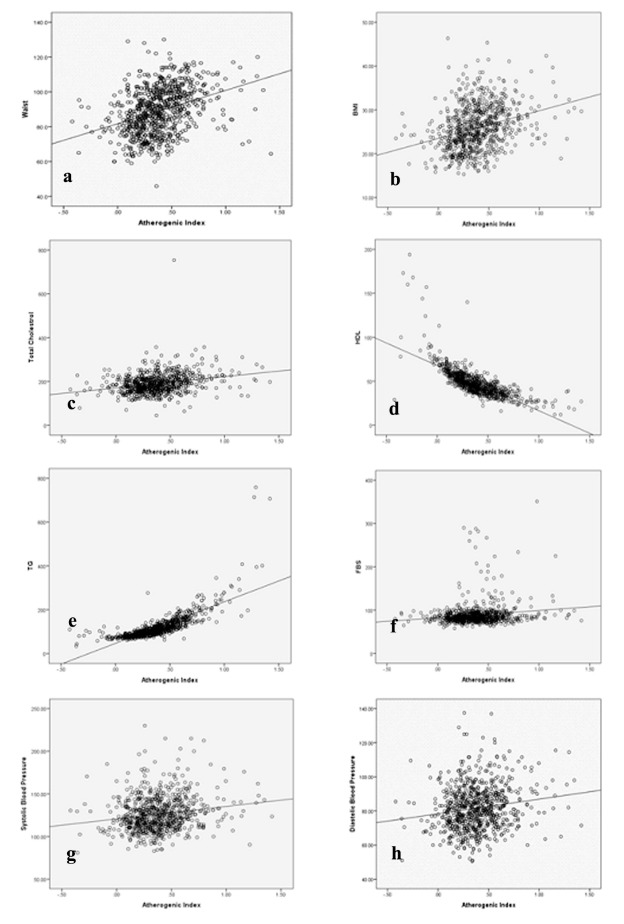
Regarding the waist circumference, a correlation of 0.35 with p<0.001 was found with AIP, in which no gender differences was detected (Fig. 1-a).
Fig. 1 .
Correlation of atherogenic index of plasma with a) Waist Circumferance, b) BMI, c) Total Cholestrol, d) HDL, e) TG, f) FBS, g) Systolic Blood Pressure, h) Diastolic Blood Pressure.
The atherogenic index and BMI were significantly (p<0.001) correlated with a correlation coefficient of 0.33 (Fig. 1-b).
AIP was also significantly correlated with mean systolic blood pressure (r=0.13, p<0.001), mean diastolic blood pressure (r=0.16, p<0.001), HDL (r=-0.72, p<0.001), LDL (r=0.29, p<0.001), serum triglycerides (r=0.77, p<0.001), total cholesterol (r=0.27, p<0.001), and fasting blood sugar (r=0.14, p<0.001) (Fig. 1-c to h).
AIP was correlated with physical activity (r=-0.09, p<0.01). When data was analyzed separately for two genders, a stronger correlation was found in men (r=-0.18, p<0.001) but the correlation was not statistically significant in women.
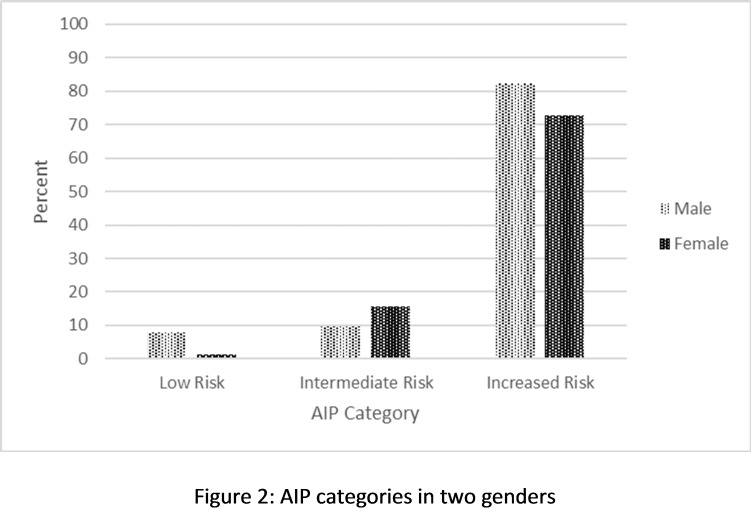
In the increased risk AIP category, men had taken the dominance and the difference between the two sex was statistically significant (p<0.001) (Fig. 2).
Fig. 2 .
AIP categories in two genders
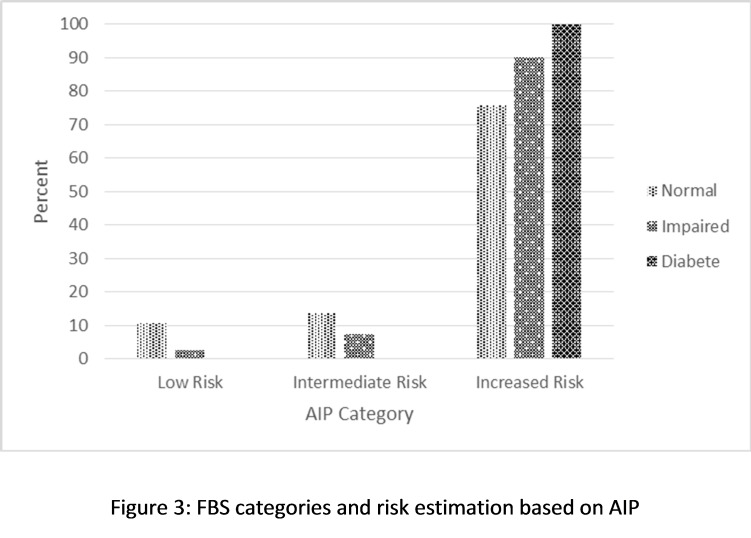
According to Fig. 3, all of the diabetic participants and 90% of person with impaired fasting glucose were in AIP increased risk category and this association was statistically significant (p<0.001).
Fig. 3 .
FBS categories and risk estimation based on AIP
The chi-square test didn’t show significant difference in AIP categories according to BP status (p=0.06).
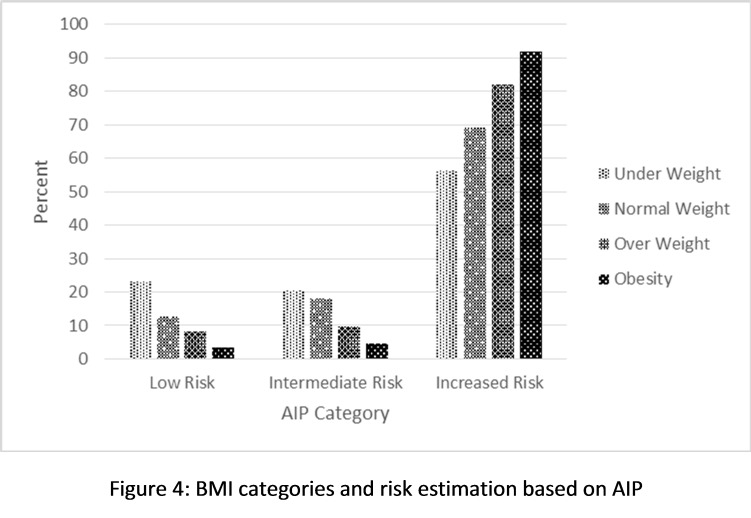
As Fig. 4 shows, 92% of obese and 82% of overweight BMI group had increased risk according to the AIP category and this association was statistically significant (p<0.001).
Fig. 4 .
BMI categories and risk estimation based on AIP
Discussion
In this study, we estimated the cross-sectional association between AIP and other risk factors of CVD. Most of participants were in over weight and obese category, and this property was dominant in women. It was observed that participants with higher BMI and also waist circumferences had a higher AIP too. These findings are in agreement with previous studies that show strong association between abnormalities of blood lipoproteins and different habits of people, such as life style and eating habits (8,36).
Furthermore, this study demonstrated that there is a concordance between increased BMI and significant increase in value of HDL-C, LDL-C, TC and TG as well as systolic blood pressure and diastolic blood pressure and also FBS. This result is similar to the results of Karen Kearns et al. and several cross sectional studies that showed chronic disease like hypertension, diabetes, dyslipidemia and osteoarthritis are more prevalent in obese persons (37-40).
As previous research has shown, regular physical activity can help to control BMI, improve lipid profile and decrease the risk of coronary heart disease, heart attack, high BP and diabetes (36). This study also demonstrated an inverse association between AIP and the level of physical activity. This association was higher in men than women. In women, we observed a positive but not significant correlation between physical activities and AIP.
Furthermore, we found a significant association between AIP and FBS. In agreement with our study, Tariq M Ali Rajab showed that diabetic dyslipidemia is characterized by an increased TG level and also decreased HDL-C value, a main feature of lipoproteins abnormalities in diabetic patients (22,41,42). Another studies concluded that hyperglycemia, abnormal lipid profile and to some extent HTN are all participated in development of atherosclerosis (22,25,43). Nevertheless, this study did not show significant difference in AIP categories between hypertensive and normotensive groups, which may be due to high number of normotensive participants.
According to the value of AIP as previously mentioned, this study showed that male participants were dominant in increased risk AIP category and so they were at a higher risk of developing coronary heart disease. This finding was in agreement with Mudhaffa Sami Khazaál study (14).
Collective information from various studies illustrated a strong correlation between AIP and lipoprotein particle size, therefore AIP could be considered as an indicator of atherogenic lipoprotein status (25,44). As we observed in present study, significant increase in AIP was detected with increasing TC, TG and LDL-C and decreasing HDL-C.
It has been reported that AIP plays as predictive value for atherosclerosis (20,21), and can be used as an available index of highest sensitivity for assessing cardiovascular risk factors, and for predicting the acute coronary events (45). Moreover, in situations where all atherogenic parameter are normal, AIP may be the alternative screening tool (14). Although in this study most of participants (77.5%) were in the increased risk AIP category, many of them didn’t have any risk factor.
This study was a national and provincial large scale survey that was a marked strength of it (46). In this study, all subjects were representative of a limited geographical region (Iran) and may not reflected the AIP patterns from the other countries. So that future large population based multi-center studies are recommended. Furthermore, our cross sectional study cannot conclude on causality or temporal trends. As a result, it is unclear if longitudinal changes in BMI, abdomen obesity or physical activity can result in corresponding changes in AIP.
Conclusion
Our findings showed that increasing in AIP is associated with other cardiovascular risk factors; therefore change in these risk factors affects the AIP index. Based on the present study, and according to the epidemiological transition of disease, life style change, performing regular exercise and healthy diet modification is recommended. In addition, AIP should be used as a regular monitoring index of CVD in every day practice, especially in persons with another cardiovascular risk factors. It is also associated with other major risk factors of heart disease and it is sensitive measure that can be easily calculated especially when other lipid values are within normal range.
Conflict of Interest
The authors declared no conflict of interest.
Cite this article as: Niroumand Sh, Khajedaluee M, Khadem-Rezaiyan M, Abrishami M, Juya M, Khodaee Gh, Dadgarmoghaddam M. Atherogenic Index of Plasma (AIP): A marker of cardiovascular disease. Med J Islam Repub Iran 2015 (25 July). Vol. 29:240.
References
- 1.Deaton C, Froelicher ES, Wu LH, Ho C, Shishani K, Jaarsma T. The global burden of cardiovascular disease. Eur J Cardiovasc Nurs. 2011 Jul;10 Suppl 2:S5–13. doi: 10.1016/S1474-5151(11)00111-3. [DOI] [PubMed] [Google Scholar]
- 2.Mensah GA, Brown DW. An overview of cardiovascular disease in the United States. Health affairs. 2007;26(1):38–48. doi: 10.1377/hlthaff.26.1.38. [DOI] [PubMed] [Google Scholar]
- 3. Rang HP, Dale MM, Ritter JM, Moore PK. Pharmacology. 5th ed. Elsevier: India. 2005 ISBN: 81-8147-917-3.
- 4.Martirosyan DM, Miroshnichenko LA, Kulokawa SN, Pogojeva AV, Zoloedov VI. Amaranth oil application for heart disease and hypertension. Lipids Health Dis. 2007;6:1. doi: 10.1186/1476-511X-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shen GX. Lipid Disorders in Diabetes Mellitus and Current Management Curr Pharmaceut. Analys. 2007;3:17–24. [Google Scholar]
- 6.Takasaki Y. Serum Lipid Levels and Factors Affecting Atherogenic Index in Japanese Children. Journal of Physiological Anthropology and Applied Human Science. 2005;24(4):511–515. doi: 10.2114/jpa.24.511. [DOI] [PubMed] [Google Scholar]
- 7.Parinita K. Study of serum lipid profile in individuals residing in and around Nalgonda. Int J pharm Bio Sci. 2012;2:110–116. [Google Scholar]
- 8.Kanthe PS, Patil BS, Bagali Sh, Deshpande A, Shaikh G, Aithala M. Atherogenic Index as a Predictor of Cardiovascular Risk among Women with Different Grades of Obesity. IJCRIMPH. 2012;4(10):1767–1774. [Google Scholar]
- 9.Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A. et al. Evidence-Based Nutrition Principles and Recommendations for the Treatment and Prevention of Diabetes and Related Complications. Diabetes Care. 2002;25:148–198. doi: 10.2337/diacare.25.1.148. [DOI] [PubMed] [Google Scholar]
- 10.Shen GX. Lipid Disorders in Diabetes Mellitus and Current Management Curr Pharmaceut. Analys. 2007;3:17–24. [Google Scholar]
- 11.Cummings KC. Lipid and Cardiac Risk profiles. Clinical Chemistry. 2003;47:407–9. [Google Scholar]
- 12.Nwagha UI, Ikekpeazu EJ, Ejezie FE, Neboh EE, Maduka IC. Atherogenic index of plasma as useful predictor of cardiovascular risk among postmenopausal women in Enugu, Nigeria. African Health Sciences Sep. 2010;10(3):248–252. [PMC free article] [PubMed] [Google Scholar]
- 13.Igweh JC, Nwagha IU, Okaro JM. The Effects of Menopause on the Serum lipid profile of Normal Females of South East Nigeria. Nigerian Journal of Physiological Sciences. 2005;20(1-2):48–53. [PubMed] [Google Scholar]
- 14.Mudhaffar SK. Atherogenic Index of Plasma (AIP) As a Parameter in Predicting Cardiovascular Risk in Males Compared To the Conventional Dyslipidemic Indices (Cholesterol Ratios) Karbala J Med. 2013 June;6(1):1506–1513. [Google Scholar]
- 15.Guerin M, Legoff W, Lassel TS, VanTol A, Steiner G, Chapman MJ. Proatherogenic role of elevated CE transfer from HDL to VLDL and dense LDL in type 2 diabetics. Arterioscler Thromb Vasc Biol. 2001;21:282–87. doi: 10.1161/01.atv.21.2.282. [DOI] [PubMed] [Google Scholar]
- 16.Manninen V, Tenkanen L, Koshinen P, Huttunen JK, Mänttäri M, Heinonen OP. et al. Joint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study: implications for treatment. Circulation. 2002;85:37–45. doi: 10.1161/01.cir.85.1.37. [DOI] [PubMed] [Google Scholar]
- 17.Dobiasova M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apo B- lipoprotein-depleted plasma (FERHDL) Clin Biochem. 2001;34:583–88. doi: 10.1016/s0009-9120(01)00263-6. [DOI] [PubMed] [Google Scholar]
- 18.Tan MH, Johns D, Glazer NB. Pioglitazone reduces atherogenic index of plasma in patients with type 2 diabetes. Clin Chem. 2004;50:1184–88. doi: 10.1373/clinchem.2004.031757. [DOI] [PubMed] [Google Scholar]
- 19.Nwagha UI, Igweh JC. Atherogenic Index of Plasma: A significant indicator for the onset of Atherosclerosis during menopause in hypertensive females of South East Nigeria. Journal of College of Medicine. 2005;10(2):67–71. [Google Scholar]
- 20.Njajou O, Kanaya AM, Holvoet P, Connelly S, Harris T. Association between oxidized LDL-C, obesity and type 2 diabetes Diabetes Metab. Res rev. 2009;25(8):733–9. doi: 10.1002/dmrr.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daniels LB, Laughlin G, Sarno MJ. Lp- PLA2 is an independent predictor of incident coronary heart disease in apparently healthy older population J Am Col. Cadiol. 2008;51:913–9. doi: 10.1016/j.jacc.2007.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tariq M, Ali Rajab. Comparative study for Atherogenic Index of Plasma (AIP) in patient with type1 Diabetes Mellitus, type2 Diabetes Mellitus, Betathalassemia and Hypothyroidism. Int J Chem Res. 2012;2(1-9) [Google Scholar]
- 23.Dobiášová M, Frohlich J, Šedová M, Cheung MC, Brown BG. Cholesterol esterification and atherogenic index of plasma correlate with lipoprotein size and findings on coronary angiography. J Lipid Res. 2011;52(3):566–571. doi: 10.1194/jlr.P011668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dobiášová M, Frohlich J. The plasma parameter log (TG/HDL) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER HDL) Clinical Biochemistry. 2001;34:583–588. doi: 10.1016/s0009-9120(01)00263-6. [DOI] [PubMed] [Google Scholar]
- 25.Dobiasova M. AIP—atherogenic index of plasma as a significant predictor of cardiovascular risk: from research to practice. VnitrLek. 2006;52(1):64–71. [PubMed] [Google Scholar]
- 26. Global Health Observatory. Mean Body Mass Index. World Health Organisation (WHO). Available from: http://www.who.int/gho/ncd/risk_factors/bmi_text/en Accessed on Sep 2014.
- 27.Ioanna S, Havenetidis K, Kostoulas I, Paxinos T. Body Fat Percentage and Body Mass Index as Predictors of Cadets' Physical Performance. The Open Sports Sciences Journal. 2014;7(Suppl-1, M9):53–59. [Google Scholar]
- 28.Prentice AM, Jebb SA. Beyond body mass index. Obes Rev. 2001;2(3):141–7. doi: 10.1046/j.1467-789x.2001.00031.x. [DOI] [PubMed] [Google Scholar]
- 29.Nelson ME, Rejeski J, Blair SN, Duncan PW, Judge JO, King AC. et al. Physical Activity and Public Health in Older Adults, Recommendation From the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 30.Rankinen T, Kim SY, Perusse L, Despres JP, Bouchard C. The prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysis. Int J Obes Relat MetabDisord. 1999;23:801–809. doi: 10.1038/sj.ijo.0800929. [DOI] [PubMed] [Google Scholar]
- 31.Katzmarzyk PT, Srinivasan SR, Chen W, Malina RM, Bouchard C, Gerald S. Berenson Body Mass Index, Waist Circumference, and Clustering of Cardiovascular Disease Risk Factors in a Biracial Sample of Children and Adolescents. PEDIATRICS August. 2004;114(2):198–205. doi: 10.1542/peds.114.2.e198. [DOI] [PubMed] [Google Scholar]
- 32.Rexrode KM, Buring JE, Manson JE. Abdominal and total adiposity and risk of coronary heart disease in men. Int J Obes Relat Metab Disord. 2001;25:1047–1056. doi: 10.1038/sj.ijo.0801615. [DOI] [PubMed] [Google Scholar]
- 33. National Institutes of Health. Clinical Guidelines for the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Bethesda, MD: National Institutes of Health; 1998.
- 34.Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med. 2002;162:2074–2079. doi: 10.1001/archinte.162.18.2074. [DOI] [PubMed] [Google Scholar]
- 35.Ardern CI, Katzmarzyk PT, Janssen I, Ross R. Discrimination of health risk by combined body mass index and waist circumference. Obes Res. 2003;11:135–142. doi: 10.1038/oby.2003.22. [DOI] [PubMed] [Google Scholar]
- 36. Flier JS. Biology of Obesity. In: Kasper DL, Fauci AS, Longo DL, Braunwald E, Hauser SL, Jameson JL. eds. Harrison’s Principles of Internal Medicine.17th ed. New York, NY: McGraw-Hill; 2008:462-464.
- 37.Kearn K, Dee A, Fitzgerald AP, Doherty E, Perry IJ. Chronic disease burden associated with overweight and obesity in Ireland: the effects of a small BMI reduction at population level. BMC Public Health. 2014 Feb;14:143. doi: 10.1186/1471-2458-14-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jiang Y, Chen Y, Manuel D, Morrison H, Mao Y. Quantifying the impact of obesity category on major chronic diseases in Canada. Sci World J. 2007;7:1211–1221. doi: 10.1100/tsw.2007.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Turley M, Tobias M, Paul S. Non‒fatal disease burden associated with excess body mass index and waist circumference in New Zealand adults. Aust New Zealand J Public health. 2006;20:231–237. doi: 10.1111/j.1467-842x.2006.tb00863.x. [DOI] [PubMed] [Google Scholar]
- 40.Kress AM, Hartzel MC, Peterson MR. Burden of disease associated with overweight and obesity among US military retirees and their dependents, aged 38–64, 2003. Prevent Med. 2005;41:63–69. doi: 10.1016/j.ypmed.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 41.Susanti E, Donosepoetro M, Patellong I, Arif M. Differences between several atherogenic parameters in patients with controlled and uncontrolled type 2 Diabetes Mellitus. Med J Indones. 2010;19(2):103–108. [Google Scholar]
- 42.Kavitha G, Ramani G, Dhass PK, Aruna RM. Oxidative stress, interleukin (il-6) and atherogenic index of plasma in diabetic nephropathy. I JABPT. 2011;2(2):211–217. [Google Scholar]
- 43.Wassink AM, Graaf VG, Sabita Y, Spiering W, Frank L. Metabolic syndrome and incidence of type 2 diabetes in patients with manifest vascular disease Diabetes Vasc. Dis Res. 2008;5:114–22. doi: 10.3132/dvdr.2008.019. [DOI] [PubMed] [Google Scholar]
- 44.Dobiasova M, Frohlich J. The plasma parameter log (TG/HDL-C-C) as an atherogenic index. Clin Biochem. 2001;34:583–8. doi: 10.1016/s0009-9120(01)00263-6. [DOI] [PubMed] [Google Scholar]
- 45.Dobiavosa M, Urbanova Z, Samanek M. Relation between particle size of HDL and LDL Lipoproteins and cholesterol Esterification rate. Physiol Res. 2005;54:159–165. [PubMed] [Google Scholar]
- 46.Dadgarmoghaddam M, Khajedaluee M, Khaodem- Rezaiyan M, Niroumand SH, Abrishami M, Joya M, Khodaee GH. Risk Factors for Non-communicable Disease: a population based study in Mashhad (Iran) BJMMR. 2015;7(6):503–511. [Google Scholar]