Abstract
Background
This review was conducted to update the Children’s Oncology Group (COG) Long-Term Follow-Up Guidelines (COG-LTFU Guidelines; version 4.0) regarding screening for psychosocial late effects of pediatric cancer.
Procedure
Articles published between August 2009 and January 2011 that addressed psychosocial late effects of long-term survivors of pediatric cancer (n = 35) were reviewed by a multidisciplinary team of COG late effect experts.
Results
The majority of studies in this time period indicate that survivors experience few psychosocial problems in long-term survivorship. A critical subset, however, are at increased risk for psychosocial late effects secondary to treatment. Highlighted findings from this review include increased rates of suicidal ideation (SI), and health beliefs as robust predictors of SI, anxiety, and global distress. Survivors’ health beliefs were associated with their perceptions of physical limitations, overall late effects, and cancer-related pain. While many survivorship studies continue to specify risk factors for anxiety and post-traumatic stress symptoms (PTSS)/disorder (PTSD), others outcomes (e.g. developmental, interpersonal, and familial factors) appear to be emerging in importance.
Conclusions
Although the majority of childhood cancer survivors do not experience psychosocial problems, a subset will. The recent research findings have been included in the new COG-LTFU guidelines that will assist in the targeted assessment and treatment of survivors’ psychosocial health.
Keywords: Psychosocial Late Effects, Pediatric Cancer, Long-Term Follow-Up Guidelines, Children’s Oncology Group
Introduction
Survivors of childhood cancer develop psychosocial late effects secondary to cancer and its treatment [1]. As cure rates increase and more survivors live to adulthood, anticipating and meeting this group’s long-term psychosocial healthcare needs has become a priority. New challenges include developing an improved understanding of survivors’ transition to adulthood [2], the implementation of new research findings in survivor assessment and intervention, and balancing favorable psychosocial outcomes with the cost-extensive resources needed by few [3]. The objectives of this report are to summarize the evidence which informed recommendations in the Children’s Oncology Group (COG) Long-Term Follow-Up Guidelines (COG-LTFU Guidelines; version 4.0), outline methods of screening for psychosocial late effects of pediatric cancer, and increase awareness regarding the latest research on psychosocial functioning among survivors of childhood cancer.
This review targeted studies of psychosocial outcomes among pediatric cancer survivors who were two or more years post completion of therapy. Previous guidelines (COG-LTFU Guidelines; version 3.0) have suggested that depression [1, 4], anxiety, and post-traumatic stress symptoms/disorder [5, 6] were experienced at disproportionately high rates among survivors. Yet, current studies continue to confirm that while most survivors do well psychosocially, a subset of survivors are at increased risk for elevated distress [3, 4, 7] and poor psychosocial outcomes [8–11]. Furthermore, many positive outcomes are also seen as a result of the pediatric cancer experience, including resiliency, post-traumatic growth and benefit finding [12–14]. Incorporating these research findings into the COG-LTFU Guidelines 4.0 will facilitate clinical screening and intervention while contributing to the preventive efforts of protecting the psychosocial health of survivors.
Methods
In 2003, COG released their first risk-based, exposure-driven guideline designed to direct follow-up care for practitioners across disciplines when caring for asymptomatic pediatric cancer survivors who are two or more years post therapy completion [15]. For the current review, multidisciplinary teams of physicians, psychologists, social workers, and nursing independently updated the COG LTFU Guidelines 4.0 for the following outcomes: Neurocognitive, Social/Quality of Life, Sleep/Fatigue, and Health Behaviors. The current authors composed the COG LTFU Psychosocial panel that developed new recommendations for the monitoring and intervention of psychosocial late effects among survivors based on the extant literature. This panel identified five broad a priori areas of psychosocial late effects from COG LTFU Guidelines 3.0 to guide their literature review: 1) Depression, 2) Anxiety, 3) Global Distress, 4) Resilience and Positive Growth, and 5) Developmental Barriers to Normative Adjustment. The panel was also open to new or emerging topics during the literature review, with access to psychosocial care being an example of such.
Research published between August 2009 and January 2011 was included in the current review. These dates were chosen based on the completion of the last LTFU update and ended three months post initiation of the committee’s work on this project. Eligibility criteria consisted of: 1) manuscript published in a peer-reviewed journal, 2) population included survivors of childhood or adolescent cancer, 3) study abstract was available in PubMed or PsycInfo databases. Search terms used are listed in Appendix A. Literature searches were conducted and cross-reviewed by a multidisciplinary panel of late effect experts consisting of two psychologists, one social worker, and two pediatric nurse practitioners representing multiple COG sites. Bi-weekly conference calls and email communications were conducted over a 3-month period across reviewers and relevant findings were discussed. The panel member leading the review for each category completed the following tasks: a) provision of categorical references and articles one week prior to team conference call; b) provision of a summarized evidence table specific to identified articles one week prior to conference call; c) lead and facilitate a critical discussion of the presented articles during conference call; d) provide a written summary of their assigned category and recommendations for the Task Force co-chairs.
Scoring of the quality of evidence for the COG-LTFU Guidelines followed a modified version of the National Comprehensive Cancer Network “Categories of Consensus” system [16]. In short, “high-level evidence” was defined as findings derived from high quality case control and cohort studies. “Lower-level evidence” was defined as findings derived from non-experimental studies, case reports, review articles and expert opinion. Articles were further classified based on the uniformity of consensus among reviewers regarding strength of evidence and appropriateness of the screening recommendation. Final recommendations were made by the Psychosocial Late Effects panel regarding the classification of study findings into one of three categories: “confirmatory” findings of previous literature or well-established theories for this population, “disputable” evidence of issues that need further confirmatory support in the literature, and “novel” or emerging findings that need to be followed with increased methodological rigor. This is the methodology used in previous COG-LTFU Guidelines. At project completion, the leader of the multidisciplinary panel provided an overview and detailed summary of recommendations to the chairs of the Neuropsychological/Psychosocial Task Force who later summarized and presented the proposals to the COG Guideline Core Leadership Committee for potential inclusion in the upcoming version of the COG-LTFU Guidelines 4.0 (See Table I).
TABLE I. Summary of Findings: Psychosocial Late Effects.
Children’s Oncology Group, Long-Term Follow-Up Guidelines, Version 4.0
| Level of Findings | Findings |
|---|---|
| 1. Confirmatory: | Survivors generally have similar psychosocial outcomes compared to controls. Subsets are at increased risk for: |
| 2. Disputable: | Treatment intensity associates with psychosocial outcomes: |
| 3. Novel: |
|
Materials
Thirty five articles meeting study criteria were identified and reviewed by the panel. The 35 articles included: one randomized controlled trial, one non-randomized controlled trial, 24 of observational design (i.e. cohort, cross-sectional, or case-control), 2 studies of non-experimental design, 6 general review or meta-analytic articles, and one expert opinion. Of the 35 articles, 3 were published as part of the Childhood Cancer Survivor Study (CCSS) cohort, 4 were studies conducted with other international registries, and 4 were single institution studies with ≤ 50 participants. In addition, the articles included heterogeneous methodologies, cohorts (i.e. age at assessment and time since diagnosis), and measures used to assess psychosocial late effects.
Results
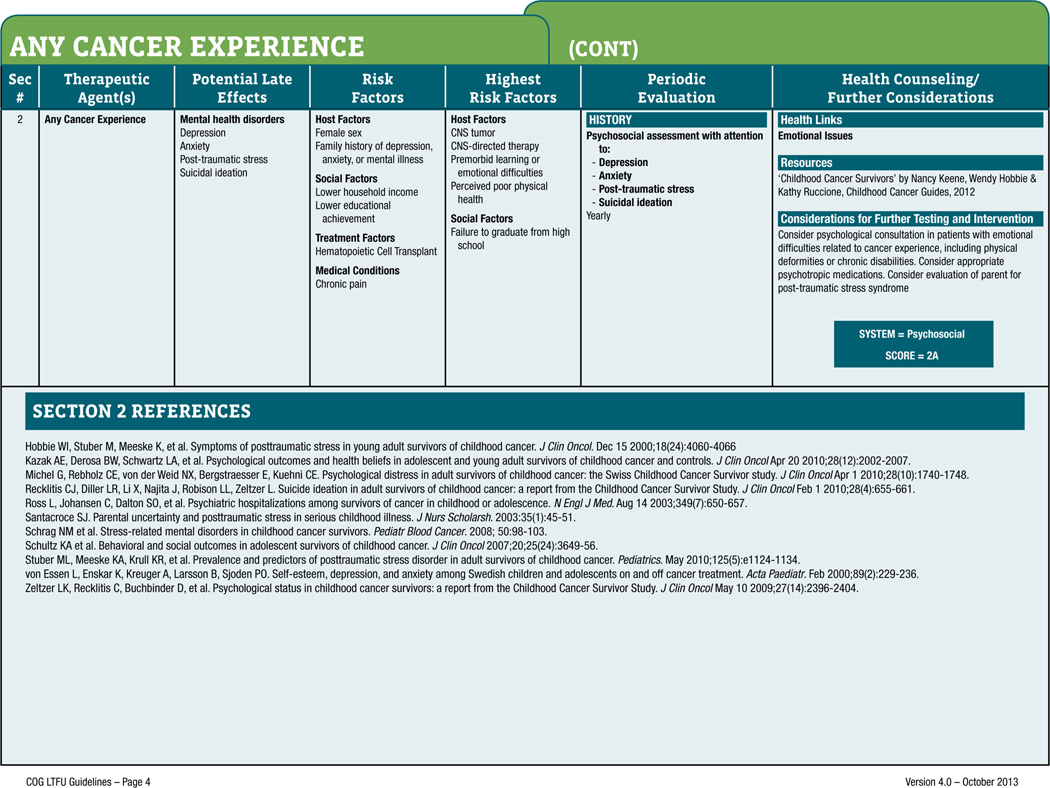
Results of this systemic review revealed several important findings that were incorporated into the updated revision of the COG-LTFU Guidelines 4.0. These included the panels’ Confirmatory findings that screening for suicidal ideation (SI) [10] and consideration of survivors’ health beliefs (e.g. perceptions of physical limitations, overall late effects, and cancer related pain) as robust predictors of suicidal ideation, anxiety, and global distress – over and above provider ratings [8, 10, 11] - be included in version 4.0 (See Table I). As such, SI (under Potential Late Effects and Periodic Evaluation), Chronic pain (under Risk Factors / Medical Conditions), and Perceived poor physical health (under Highest Risk Factors / Host Factors) have been added to the list of recommendations in the COG-LTFU Guidelines 4.0 (see Figure 1). Table I also outlines findings of Disputable and Novel areas that should be considered in future research and clinical care with this population. Finally, the panel recommended several updated citations to the References section in the new Guidelines [3, 8–11] (see Figure 1).
Figure 1.
From the Children’s Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent and Young Adult Cancers, Version 4.0, October 2013, used with permission.
Depression
Overall, survivors do not appear to be at heightened risk for depression [8]. In fact, several studies have reported lower depressive symptoms for survivors compared to the general population [20, 21]. However, survivors’ risk for depression may increase based on specific demographic and treatment factors, including: gender, diagnosis, age at diagnosis, unemployment, low income levels, and those reporting physical late effects of cancer therapy [3]. As such, depression is a significant issue within a limited subset of survivors.
Paramount to the current review, recent research has confirmed that a subgroup of survivors are at heightened risk for SI compared to sibling controls (7.8% vs. 4.6%, respectively, [10]), with robust associations between SI and survivor reported health, cancer-related pain, depression, and primary CNS diagnosis. This cluster of physical health, pain, and emotional concerns has previously been observed [8, 9, 22, 23]. Poor survivor-reported health was significantly associated with SI even after controlling for demographics, diagnosis and treatment factors, and depression. Interestingly, SI was not significantly associated with current age, age at diagnosis, gender, cancer therapy, recurrence or second malignancy [10]. This confirmatory finding indicates that SI and depression are distinct problems for some survivors and highlights the necessity for comprehensive assessment and treatment of SI at medical follow up. Figure 1 includes the updated COG-LTFU Guidelines 4.0 for mental health disorders.
Anxiety Disorders
The association between a childhood cancer diagnosis and increased rates of anxiety and posttraumatic stress symptoms for survivors has been well studied [5, 6]. Prior research has elucidated that survivors who are female, unmarried, unemployed, have low household income, lower educational attainment, lack health insurance, or a chronic health condition are at increased risk for developing and maintaining an anxiety disorder [24].
Stuber [11] utilized the CCSS cohort and healthy sibling controls to compare the prevalence of post-traumatic stress disorder (PTSD). Previous research has historically assessed PTSD symptoms while rarely considering functional impairment. As such, this literature is composed of methodological heterogeneity regarding assessment modalities and a focus on either specific cancer vs. other life events, or the cumulative effect of stressful life events [25–27]. Stuber concluded that survivors had more than a fourfold greater risk of PTSD compared with siblings (9% vs. 2%, respectively [11]), while replicating many of the risk factors for PTSD noted above. Furthermore, this study found that being over age 30 and having a history of more intense cancer treatment were significant predictors of meeting full PTSD criteria [11, 28]. Survivors who experienced a relapse or recurrent disease were not at increased risk for PTSD, whereas those receiving cranial radiation at < 4 years of age were at an increased risk (OR: 2.05 [95% CI: 1.41 – 2.97]). This large study of survivors and their siblings suggests a heightened incidence of survivors who meet full PTSD criteria while clarifying the many risk factors which could be targeted for intervention within this population [11].
In contrast to the literature cited above, other research has found that adolescent and young adult (AYA) survivors do not differ significantly from controls on measures of anxiety and other psychological outcomes [8]. Most AYA survivors appear to be in relatively good psychosocial health. Among long-term survivors, however, those diagnosed during adolescence and receiving the highest treatment intensity reported relatively higher levels of anxiety and post-traumatic stress symptoms (i.e. arousal and re-experiencing) [8]. Also within this AYA sample, survivors’ report of the number of their health problems was strongly and negatively associated with their psychosocial functioning. In contrast, health providers’ report of the survivors’ number of health problems was not correlated with psychosocial functioning. Overall, AYA survivors had less positive health beliefs (i.e. “I’m not as healthy as other people my age”) than their peer controls [8]. This study confirmed the overall psychosocial health of AYA survivors, offered specific age and treatment factors associated with poor outcomes, and highlighted survivor-centered health beliefs as specific targets that providers can intervene with this population [8].
Family functioning has emerged as a salient factor in the prevalence of anxiety and PTSD for survivors [29, 30]. Recent literature has reported that 75% of adolescent survivors with PTSD (8% of sample) came from families with categorically poor family functioning [29]. Likewise a study of Japanese adolescent survivors noted the families with the poorest family functioning reported the highest levels of anxiety, post-traumatic stress symptoms (PTSS), and depression [30]. Although cross-sectional in design, these studies indicate that family functioning may be an important component of survivors’ psychosocial outcomes.
Global Distress
Researchers and clinicians often assess “global distress” in efforts to gain a comprehensive view of survivors’ psychological functioning. For example, global distress is frequently assessed for survivors via the Brief Symptom Inventory (BSI and BSI-18; [31]). The BSI-18 is widely utilized by the CCSS and other national registries for survivors. Much of the literature over the past several years has continued to focus and clarify the variety of medical and demographic risk factors that place survivors at risk for elevated global distress.
In accordance with the depression and anxiety literature cited above, survivors are only at increased risk for global distress when certain risk factors are present [1, 4, 7]. Risk factors included: female gender, being unmarried, being a single child, a brain tumor diagnosis, diagnosed during adolescence, and receiving more intensive treatment [3, 8]. Survivors with such risk factors often show disproportionately high rates of psychosocial distress compared to the general population (i.e. 16.9% vs. 10%, respectively) and their subjective beliefs and perceptions of their health problems correlated positively and strongly with their psychosocial distress [9]. Furthermore, many social and demographic factors appear to cascade and build over time, with lower educational attainment, being unemployed, no health insurance, and lower household income all being significant predictors of high global distress [3]. Importantly, survivors with high distress were subsequently found to have risky health behaviors (i.e. increased smoking and alcohol use) and poor health outcomes (i.e. fatigue and altered sleep) [3, 8].
Resilience and Positive Growth
For many years the focus of psychosocial research has been on the perceived maladjustment during and following the cancer experience. However, as outlined above, most survivors do not have poor psychosocial functioning. Some survivors find benefit from their encounter with life-threatening illness [32] and may even experience post-traumatic growth [12].
Michel [13] recently examined how demographic and medical variables affect benefit finding in childhood cancer survivors. Survivors reported a positive relationship between benefit finding and each of the following: optimism, a leukemia diagnosis (compared to CNS and solid tumor diagnoses), and the belief that the illness still affected their lives. Results supported the use of the Benefit Finding Scale in this population and further confirmed previous studies that showed children diagnosed prior to age 5 experience less benefit finding than those diagnosed later in childhood [13]. A study of Japanese survivors found that they reported both higher rates of post-traumatic stress and higher post-traumatic growth than matched siblings [33], highlighting the notion that survivors may experience both positive and negative aspects of their illness simultaneously [34]. Other studies reported ongoing work to develop and test research tools that may be used to further our understanding of positive psychological outcomes following childhood cancer treatment; examples included the Youth Life Orientation Test [35], the Health Competence Beliefs Inventory [36], and the Impact of Cancer Scale [37].
Developmental Considerations and Barriers Affecting Normative Development
The survivor population is increasing in size and lifespan, highlighting the need of this group to acquire adult skills and independence [38]. Survivors must now master skills such as normative social functioning, coping strategies, emotional development, and the formation of appropriate educational and vocational goals. Overall, an improved understanding of these developmental factors will help guide the timing, content, and intensity of future interventions [39].
One study reported that the career decision-making of Israeli childhood cancer survivors was impacted by their perceptions of vulnerability, optimism, and time perspective [40]. Two other studies from our review implemented interventions on coping and social skills for survivors. Judge Santacroce [18] demonstrated that a randomized telephone intervention was effective in delivering coping skills training to AYA survivors struggling with the uncertainty of their future health. Barrera and Schulte [17] conducted a small feasibility study focusing on a non-randomized group social skills intervention with brain tumor survivors. Results for this 8-week program showed promising recruitment, acceptability, and retention with significant improvements to parent-report of survivor’s self-control, social skills, and quality of life. These are two examples of a growing literature that indicates that targeting interventions to at-risk populations during developmentally vulnerable times may be particularly effective. Given survivors’ robust psychosocial health, researchers have suggested that assessing developmental struggles – such as social skills, intimate relationships [41], and vocational satisfaction – may be the most accurate measure of their current functioning, predictors of future outcomes, and should be the focus of future research and interventions [20].
Access to Psychosocial Care
Overall, survivors struggling with psychosocial late effects of their cancer experience often receive fragmented medical and psychosocial follow up care [2]. This was an area of the literature review that was not identified a priori by the panel but emerged in our work. Whereas Recklitis [42] historically demonstrated that psychosocial screening can be incorporated into a survivorship follow up clinic visit, a large study of the German Childhood Cancer Registry indicated that survivors received little psychological or psychiatric care when experiencing clinically relevant symptoms of depression or anxiety (12% and 13.6%, respectively; [19]). Moreover, more than a quarter of German AYA survivors did not attend regular oncology follow-up visits [19] and only a minority of US survivors received medical care based on their previous cancer or specific risk-reduction screenings (31.5% & 17.8%, respectively; [2]). Therefore, consistent cancer-related medical and psychosocial follow-up care, especially as survivors’ transition into adulthood, continues to be a significant problem for this population.
Discussion
The COG Psychosocial Late Effects multidisciplinary panel highlighted several recommendations that have been incorporated into the revised COG LTFU Guidelines, version 4.0. Increased rates of SI among survivors indicate the need for universal screening and timely referrals by providers. While the current research on SI and survivors is sound, this clinically important area has historically been understudied. More work needs to be conducted to understand the etiology, risk-factors, and best screening/treatment practices for survivors with SI. For example, symptoms of depression and SI appear to be distinct, and need to be assessed independently. Also, current researchers [10] assessed SI by survivors’ response to one item on the BSI-18. However, the clinical significance of the problem (and opportunity for risk reduction) is such that expanded and effective screening and interventions should become standard as part of survivor care [43]. The current state of fragmented medical and psychosocial follow up for survivors throughout the lifespan is a critical issue that complicates the need for effective assessment and treatment of SI.
Our review indicates that many interpersonal factors impact survivors’ emotional and physical functioning, and that survivor self-report may be the most accurate way to assess functioning within these domains. Examples include survivor self-report of poor physical functioning, extent of their late effects, cancer-related pain, and health beliefs – especially in comparison to their peers – that correlates strongly with their psychosocial functioning and is a more robust predictor of psychosocial functioning relative to provider reports [8–10]. In addition to the current practice of measuring Host, Social, and Treatment Risk Factors (see Figure 1), future guidelines should outline specific patient-reported outcomes (PRO) and psychosocial screening tools that accurately assess these risk factors and assists care planning [44, 45].
Demographic and treatment related risk-factors continue to be correlated with survivors’ psychosocial functioning. For example, AYA survivors diagnosed as adolescents were significantly more likely to experience heightened global distress in survivorship than their peers diagnosed earlier in life [8]. Adolescent survivors’ ability to be aware of their cancer experience (e.g. fear of death, anxiety, social and educational adjustments) from diagnosis through survivorship appears to be a developmental factor which predicts later psychosocial functioning. This highlights the need to assess both the psychosocial functioning of survivors diagnosed as adolescents and the possible effectiveness of targeting this group for interventions. Additionally, survivors who were diagnosed ≤ four years of age who received cranial radiotherapy were at a significant risk for developing clinical levels of PTSD [11]. These survivors may possess a host of physical and cognitive late effects that contribute to their psychosocial functioning in survivorship [11]. Taken together, these age and treatment intensity factors add to the previous list (e.g. education and income level, being unmarried or unemployed) that providers should specifically assess and target for intervention.
Limitations to the Current Review
The narrow time period of manuscripts reviewed and the need to incorporate the current findings into previously established COG recommendations resulted in an update that may not fully attend to all psychosocial aspects of the childhood cancer survivor population. As such, this update and its citation list are representative and not comprehensive of all COG-LTFU Guideline recommendations. The narrow time period of review ending in January of 2011 is an additional limitation to the current guidelines.
As noted throughout, we continued to observe many methodological differences across studies. For example, various ages at diagnosis, age at assessing survivors’ psychosocial adjustment, and diagnostic spread are an understandable yet continued problem within the literature that national registry studies have sought to remedy. In addition, psychosocial problems being assessed via a variety of self-report measures and the inconsistent inclusion of other diagnostic modalities (e.g. diagnostic interviews and level of functional impairment) should also be considered in the interpretation of these findings. While this review benefited from several studies of international registries [9, 19, 30, 33, 40], their generalizability and future applications across cultures may be a limitation.
Areas for Future Research
Future researchers should use longitudinal methods with predictive or meditational models that increase our understanding of the etiology and development of psychosocial late effects of survivors. For example, it is currently unknown whether survivors who initially present with poor psychosocial adjustment at diagnosis or early in treatment continue to be the survivors with the poorest outcomes. Mediational models that assess the causality of psychosocial problems associated with demographic, social, and interpersonal correlates over time will help us understand how they unfold across the survivors’ lifespan. Finally, increased depth and specificity of such late effects (vs. global distress) are needed to guide the targeted and timely interventions of the future [46].
Interventions that target and effectively treat the psychosocial late effects of survivors is the continued critical next step for behavioral health providers [3, 19, 23, 47, 48]. While much attention has been given to the many recruitment and retention barriers to these interventions [48–50], several studies serve as quality examples of their success [51–53]. Financial and programmatic restraints continue to be the largest barriers to well-powered and methodologically rigorous interventions within this population [47]. However, the failure of behavioral health providers to demonstrate robust effects in future interventions may hamper future funding opportunities, and the ability to solidify the roles of the behavioral health providers within the larger pediatric oncology health care team.
Future research should mirror our medical colleagues’ focus on health outcomes for adult survivors of childhood cancer throughout their lifespan [54]. New data indicates that by age 45, survivors have a 95.5% estimated cumulative prevalence rate of having a chronic health condition and 80.5% have a serious/disabling or life-threatening chronic condition [54]. Since our current review highlights the importance of survivor-reported beliefs of poor physical functioning, extent of their late effects, cancer-related pain, and health beliefs on their psychosocial functioning, the life-long cumulative incidence of a serious chronic condition underscores the need for effective and readily available psychosocial assessment and interventions as survivors’ age into adulthood.
Conclusion
The majority of long-term survivors of childhood cancer are living longer lives with relatively few psychosocial late effects of their treatment. When psychosocial late effects are present, however, they appear to severely impact many realms of their lives. As such, there continues to be a critical subset of survivors that are in need of effective evaluation and targeted interventions that treat their psychosocial problems. It is unknown how many survivors may develop psychosocial problems later in life as the incidence of having a chronic medical condition accumulates. Importantly, these survivors access their medical care in a variety of settings (i.e. oncology specialty centers vs. the primary care setting) and during chronological ages where transitions from pediatric to adult medical providers make identification of a medical home challenging. Therefore, all potential healthcare providers must be aware of survivors’ possible psychosocial late effects and effective treatment options.
Supplementary Material
Acknowledgements
This research was supported by the Children’s Oncology Group Chair’s Grant U10 CA098543. Grant sponsor: National Cancer Institute, National Institutes of Health, Bethesda, MD, USA.
Abbreviations
- COG
Children’s Oncology Group
- LTFU
Long-Term Follow-Up
- PTSS / PTSD
post-traumatic stress symptoms / post-traumatic stress disorder
- SI
Suicidal ideation
Footnotes
Conflict of Interests Statement
The authors report no conflict of interest.
References
- 1.Zebrack BJ, Zeltzer LK, Whitton J, Mertens AC, Odom L, Berkow R, Robison LL. Psychological outcomes in long-term survivors of childhood leukemia, hodgkin’s disease, and non-hodgkin’s lymphoma: A report from the childhood cancer survivor study. Pediatrics. 2002;110(1):42–52. doi: 10.1542/peds.110.1.42. [DOI] [PubMed] [Google Scholar]
- 2.Nathan PC, Greenberg ML, Ness KK, Hudson MM, Mertens AC, Mahoney MC, Gurney JG, Donaldson SS, Leisenring WM, Robison LL, et al. Medical care in long-term survivors of childhood cancer: A report from the childhood cancer survivor study. J Clin Oncol. 2008 Sep 20;26(27):4401–4409. doi: 10.1200/JCO.2008.16.9607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeltzer LK, Recklitis C, Buchbinder D, Zebrack B, Casillas J, Tsao JC, Lu Q, Krull K. Psychological status in childhood cancer survivors: A report from the childhood cancer survivor study. J Clin Oncol. 2009 May 10;27(14):2396–2404. doi: 10.1200/JCO.2008.21.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zebrack BJ, Zevon MA, Turk N, Nagarajan R, Whitton J, Robison LL, Zeltzer LK. Psychological distress in long-term survivors of solid tumors diagnosed in childhood: A report from the childhood cancer survivor study. Pediatric Blood & Cancer. 2007;49(1):47–51. doi: 10.1002/pbc.20914. [DOI] [PubMed] [Google Scholar]
- 5.Hobbie WL, Stuber M, Meeske K, Wissler K, Rourke MT, Ruccione K, Hinkle A, Kazak AE. Symptoms of posttraumatic stress in young adult survivors of childhood cancer. J Clin Oncol. 2000 Dec 15;18(24):4060–4066. doi: 10.1200/JCO.2000.18.24.4060. [DOI] [PubMed] [Google Scholar]
- 6.Stuber ML, Kazak AE, Meeske K, Barakat L, Guthrie D, Garnier H, Pynoos R, Meadows A. Predictors of posttraumatic stress symptoms in childhood cancer survivors. Pediatrics. 1997 Dec;100(6):958–964. doi: 10.1542/peds.100.6.958. [DOI] [PubMed] [Google Scholar]
- 7.Zebrack BJ, Gurney JG, Oeffinger K, Whitton J, Packer RJ, Mertens A, Turk N, Castleberry R, Dreyer Z, Robison LL, et al. Psychological outcomes in long-term survivors of childhood brain cancer: A report from the childhood cancer survivor study. J Clin Oncol. 2004 Mar 15;22(6):999–1006. doi: 10.1200/JCO.2004.06.148. [DOI] [PubMed] [Google Scholar]
- 8.Kazak AE, Derosa BW, Schwartz LA, Hobbie W, Carlson C, Ittenbach RF, Mao JJ, Ginsberg JP. Psychological outcomes and health beliefs in adolescent and young adult survivors of childhood cancer and controls. J Clin Oncol. 2010 Apr 20;28(12):2002–2007. doi: 10.1200/JCO.2009.25.9564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Michel G, Rebholz CE, von der Weid NX, Bergstraesser E, Kuehni CE. Psychological distress in adult survivors of childhood cancer: The swiss childhood cancer survivor study. Journal of Clinical Oncology. 2010 Apr 01;28(10):1740–1748. doi: 10.1200/JCO.2009.23.4534. [DOI] [PubMed] [Google Scholar]
- 10.Recklitis CJ, Diller LR, Li X, Najita J, Robison LL, Zeltzer L. Suicide ideation in adult survivors of childhood cancer: A report from the childhood cancer survivor study. J Clin Oncol. 2010 Feb 1;28(4):655–661. doi: 10.1200/JCO.2009.22.8635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stuber M, Meeske K, Krull K, Leisenring W, Stratton K, Kazak A, Huber M, Zebrack B, Uijtdehaage S, Mertens A, et al. Prevalence and predictors of posttraumatic stress disorder in adult survivors of childhood cancer. Pediatrics. 2010;125(5):e1124. doi: 10.1542/peds.2009-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barakat LP, Alderfer MA, Kazak AE. Posttraumatic growth in adolescent survivors of cancer and their mothers and fathers. J Pediatr Psychol. 2006 May;31(4):413–419. doi: 10.1093/jpepsy/jsj058. [DOI] [PubMed] [Google Scholar]
- 13.Michel G, Taylor N, Absolom K, Eiser C. Benefit finding in survivors of childhood cancer and their parents: Further empirical support for the benefit finding scale for children. Child Care Health Dev. 2010 Jan;36(1):123–129. doi: 10.1111/j.1365-2214.2009.01034.x. [DOI] [PubMed] [Google Scholar]
- 14.Zebrack BJ, Stuber ML, Meeske KA, Phipps S, Krull KR, Liu Q, Yasui Y, Parry C, Hamilton R, Robison LL, et al. Perceived positive impact of cancer among long-term survivors of childhood cancer: A report from the childhood cancer survivor study. Psychooncology. 2011 Mar 22; doi: 10.1002/pon.1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Landier W, Bhatia S, Eshelman DA, Forte KJ, Sweeney T, Hester AL, Darling J, Armstrong FD, Blatt J, Constine LS, et al. Development of risk-based guidelines for pediatric cancer survivors: The children's oncology group long-term follow-up guidelines from the children's oncology group late effects committee and nursing discipline. J Clin Oncol. 2004 Dec 15;22(24):4979–4990. doi: 10.1200/JCO.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 16.Winn RJ, Botnick WZ. The NCCN guideline program: A conceptual framework. Oncology (Williston Park) 1997 Nov;11(11A):25–32. [PubMed] [Google Scholar]
- 17.Barrera M, Schulte F. A group social skills intervention program for survivors of childhood brain tumors. Journal of Pediatric Psychology. 2009 Nov 01;34(10):1108–1118. doi: 10.1093/jpepsy/jsp018. [DOI] [PubMed] [Google Scholar]
- 18.Judge Santacroce S, Asmus K, Kadan-Lottick N, Grey M. Feasibility and preliminary outcomes from a pilot study of coping skills training for adolescent--young adult survivors of childhood cancer and their parents. J Pediatr Oncol Nurs. 2010 Jan-Feb;27(1):10–20. doi: 10.1177/1043454209340325. [DOI] [PubMed] [Google Scholar]
- 19.Dieluweit U, Seitz DC, Besier T, Debatin KM, Grabow D, Kaatsch P, Goldbeck L. Utilization of psychosocial care and oncological follow-up assessments among german long-term survivors of cancer with onset during adolescence. Klin Padiatr. 2011 Apr 1; doi: 10.1055/s-0031-1271779. [DOI] [PubMed] [Google Scholar]
- 20.Recklitis CJ, Parsons SK, Shih M, Mertens A, Robison LL, Zeltzer L. Factor structure of the brief symptom inventory--18 in adult survivors of childhood cancer: Results from the childhood cancer survivor study. Psychol Assess. 2006;18(1):22. doi: 10.1037/1040-3590.18.1.22. [DOI] [PubMed] [Google Scholar]
- 21.Zeltzer LK, Lu Q, Leisenring W, Tsao JC, Recklitis C, Armstrong G, Mertens AC, Robison LL, Ness KK. Psychosocial outcomes and health-related quality of life in adult childhood cancer survivors: A report from the childhood cancer survivor study. Cancer Epidemiol Biomarkers Prev. 2008 Feb;17(2):435–446. doi: 10.1158/1055-9965.EPI-07-2541. [DOI] [PubMed] [Google Scholar]
- 22.Finnegan L, Campbell R, Ferrans C, Wilbur J, Wilkie D, Shaver J. Symptom cluster experience profiles in adult survivors of childhood cancers. J Pain Symptom Manage. 2009;38(2):258. doi: 10.1016/j.jpainsymman.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wakefield CE, McLoone J, Goodenough B, Lenthen K, Cairns DR, Cohn RJ. The psychosocial impact of completing childhood cancer treatment: A systematic review of the literature. J Pediatr Psychol. 2010 Apr;35(3):262–274. doi: 10.1093/jpepsy/jsp056. [DOI] [PubMed] [Google Scholar]
- 24.Langeveld N, Grootenhuis M, Voute P, De Haan R. Posttraumatic stress symptoms in adult survivors of childhood cancer. Pediatric Blood & Cancer. 2004;42(7):604–610. doi: 10.1002/pbc.20024. [DOI] [PubMed] [Google Scholar]
- 25.Kazak AE, Barakat LP, Meeske K, Christakis D, Meadows AT, Casey R, Penati B, Stuber ML. Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia and their mothers and fathers. J Consult Clin Psychol. 1997;65(1):120. doi: 10.1037//0022-006x.65.1.120. [DOI] [PubMed] [Google Scholar]
- 26.Currier JM, Jobe-Shields LE, Phipps S. Stressful life events and posttraumatic stress symptoms in children with cancer. J Trauma Stress. 2009;22(1):28–35. doi: 10.1002/jts.20382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Phipps S, Klosky JL, Long A, Hudson MM, Huang Q, Zhang H, Noll RB. Posttraumatic stress and psychological growth in children with cancer: Has the traumatic impact of cancer been overestimated? J Clin Oncol. 2014 Mar 1;32(7):641–646. doi: 10.1200/JCO.2013.49.8212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Werba BE, Hobbie W, Kazak AE, Ittenbach RF, Reilly AF, Meadows AT. Classifying the intensity of pediatric cancer treatment protocols: The intensity of treatment rating scale 2.0 (ITR-2) Pediatric Blood & Cancer. 2007;48(7):673–677. doi: 10.1002/pbc.21184. [DOI] [PubMed] [Google Scholar]
- 29.Alderfer MA, Navsaria N, Kazak AE. Family functioning and posttraumatic stress disorder in adolescent survivors of childhood cancer. Journal of Family Psychology. 2009;23(5):717. doi: 10.1037/a0015996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ozono S, Saeki T, Mantani T, Ogata A, Okamura H, Nakagawa S, Ueda K, Inada H, Yamawaki S. Psychological distress related to patterns of family functioning among japanese childhood cancer survivors and their parents. Psychooncology. 2010;19(5):545. doi: 10.1002/pon.1606. [DOI] [PubMed] [Google Scholar]
- 31.Derogatis LR. BSI 18, brief symptom inventory 18: Administration, scoring and procedures manual. NCS Pearson, Incorporated. 2001 [Google Scholar]
- 32.Zebrack BJ, Chesler MA. Quality of life in childhood cancer survivors. Psycho-Oncology. 2002;11(2):132–141. doi: 10.1002/pon.569. [DOI] [PubMed] [Google Scholar]
- 33.Kamibeppu K, Sato I, Honda M, Ozono S, Sakamoto N, Iwai T, Okamura J, Asami K, Maeda N, Inada H, et al. Mental health among young adult survivors of childhood cancer and their siblings including posttraumatic growth. Journal of Cancer Survivorship. 2010;4(4):303. doi: 10.1007/s11764-010-0124-z. [DOI] [PubMed] [Google Scholar]
- 34.Currier JM, Hermes S, Phipps S. Brief report: Children's response to serious illness: Perceptions of benefit and burden in a pediatric cancer population. J Pediatr Psychol. 2009 Nov-Dec;34(10):1129–1134. doi: 10.1093/jpepsy/jsp021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams NA, Davis G, Hancock M, Phipps S. Optimism and pessimism in children with cancer and healthy children: Confirmatory factor analysis of the youth life orientation test and relations with health-related quality of life. J Pediatr Psychol. 2010 Jul;35(6):672–682. doi: 10.1093/jpepsy/jsp084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DeRosa BW, Kazak AE, Doshi K, Schwartz LA, Ginsberg J, Mao JJ, Straton J, Hobbie W, Rourke MT, Carlson C, et al. Development and validation of the health competence beliefs inventory in young adults with and without a history of childhood cancer. Ann Behav Med. 2011 Feb;41(1):48–58. doi: 10.1007/s12160-010-9228-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zebrack BJ, Donohue JE, Gurney JG, Chesler MA, Bhatia S, Landier W. Psychometric evaluation of the impact of cancer (IOC-CS) scale for young adult survivors of childhood cancer. Qual Life Res. 2010 Jan 8; doi: 10.1007/s11136-009-9576-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mulder RL, Hudson MM, Skinner R, Kremer LC. Health problems in survivors of childhood cancer: The need for international collaboration in long-term follow-up care. Future Oncol. 2013 Nov;9(11):1667–1670. doi: 10.2217/fon.13.107. [DOI] [PubMed] [Google Scholar]
- 39.Zebrack BJ. Cancer survivor identity and quality of life. Cancer Pract. 2000;8(5):238–242. doi: 10.1046/j.1523-5394.2000.85004.x. [DOI] [PubMed] [Google Scholar]
- 40.Stern M, Krivoy E, Foster RH, Bitsko M, Toren A, Ben-Arush M. Psychosocial functioning and career decision-making in israeli adolescent and young adult cancer survivors. Pediatric Blood & Cancer. 2010;55(4):708–713. doi: 10.1002/pbc.22642. [DOI] [PubMed] [Google Scholar]
- 41.Thompson AL, Marsland AL, Marshal MP, Tersak JM. Romantic relationships of emerging adult survivors of childhood cancer. Psychooncology. 2009 Jul;18(7):767–774. doi: 10.1002/pon.1471. [DOI] [PubMed] [Google Scholar]
- 42.Recklitis C, O'Leary T, Diller L. Utility of routine psychological screening in the childhood cancer survivor clinic. J Clin Oncol. 2003 Mar 1;21(5):787–792. doi: 10.1200/JCO.2003.05.158. [DOI] [PubMed] [Google Scholar]
- 43.Rapoff MA. Editorial: Assessing and enhancing clinical significance/social validity of intervention research in pediatric psychology. J Pediatr Psychol. 2010 Mar;35(2):114–119. doi: 10.1093/jpepsy/jsp102. [DOI] [PubMed] [Google Scholar]
- 44.Fairclough DL. Patient reported outcomes as endpoints in medical research. Stat Methods Med Res. 2004 Apr;13(2):115–138. doi: 10.1191/0962280204sm357ra. [DOI] [PubMed] [Google Scholar]
- 45.Lipscomb J, Gotay CC, Snyder CF. Patient-reported outcomes in cancer: A review of recent research and policy initiatives. CA: A Cancer Journal for Clinicians. 2007;57(5):278–300. doi: 10.3322/CA.57.5.278. [DOI] [PubMed] [Google Scholar]
- 46.Lund LW, Schmiegelow K, Rechnitzer C, Johansen C. A systematic review of studies on psychosocial late effects of childhood cancer: Structures of society and methodological pitfalls may challenge the conclusions. Pediatric Blood & Cancer. 2011;56(4):532–543. doi: 10.1002/pbc.22883. [DOI] [PubMed] [Google Scholar]
- 47.Patenaude AF, Kupst MJ. Psychosocial functioning in pediatric cancer. J Pediatr Psychol. 2005 Jan-Feb;30(1):9–27. doi: 10.1093/jpepsy/jsi012. [DOI] [PubMed] [Google Scholar]
- 48.Kahana S, Drotar D, Frazier T. Meta-analysis of psychological interventions to promote adherence to treatment in pediatric chronic health conditions. J Pediatr Psychol. 2008 Jul;33(6):590–611. doi: 10.1093/jpepsy/jsm128. [DOI] [PubMed] [Google Scholar]
- 49.Kazak AE, Simms S, Alderfer MA, Rourke MT, Crump T, McClure K, Jones P, Rodriguez A, Boeving A, Hwang WT, et al. Feasibility and preliminary outcomes from a pilot study of a brief psychological intervention for families of children newly diagnosed with cancer. J Pediatr Psychol. 2005 Dec;30(8):644–655. doi: 10.1093/jpepsy/jsi051. [DOI] [PubMed] [Google Scholar]
- 50.Stehl ML, Kazak AE, Alderfer MA, Rodriguez A, Hwang WT, Pai AL, Boeving A, Reilly A. Conducting a randomized clinical trial of an psychological intervention for parents/caregivers of children with cancer shortly after diagnosis. J Pediatr Psychol. 2009 Sep;34(8):803–816. doi: 10.1093/jpepsy/jsn130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Butler RW, Copeland DR, Fairclough DL, Mulhern RK, Katz ER, Kazak AE, Noll RB, Patel SK, Sahler OJZ. A multicenter, randomized clinical trial of a cognitive remediation program for childhood survivors of a pediatric malignancy. J Consult Clin Psychol. 2008;76(3):367. doi: 10.1037/0022-006X.76.3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kazak AE, Rourke MT, Alderfer MA, Pai A, Reilly AF, Meadows AT. Evidence-based assessment, intervention and psychosocial care in pediatric oncology: A blueprint for comprehensive services across treatment. J Pediatr Psychol. 2007 Oct;32(9):1099–1110. doi: 10.1093/jpepsy/jsm031. [DOI] [PubMed] [Google Scholar]
- 53.Sahler OJZ, Fairclough DL, Phipps S, Mulhern RK, Dolgin MJ, Noll RB, Katz ER, Varni JW, Copeland DR, Butler RW. Using problem-solving skills training to reduce negative affectivity in mothers of children with newly diagnosed cancer: Report of a multisite randomized trial. J Consult Clin Psychol. 2005;73(2):272. doi: 10.1037/0022-006X.73.2.272. [DOI] [PubMed] [Google Scholar]
- 54.Hudson MM, Ness KK, Gurney JG, Mulrooney DA, Chemaitilly W, Krull KR, Green DM, Armstrong GT, Nottage KA, Jones KE. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. 2013;309(22):2371–2381. doi: 10.1001/jama.2013.6296. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.