Abstract
Substantial scholarship has been generated in medical anthropology and other social science fields on typically developing child–parent–doctor interactions during health care visits. This article contributes an ethnographic, longitudinal, discourse analytic account of a child with autism spectrum disorder (ASD)–parent–doctor interactions that occur during pediatric and neurology visits. The analysis shows that when a child with ASD walks into the doctor’s office, the tacit expectations about the visit may have to be renegotiated to facilitate the child’s, the parent’s and the doctor’s participation in the interaction. A successful visit then becomes a hard-won achievement that requires the interactional and relational work of all three participants. We demonstrate that communicative and sensory limitations imposed by ASD present unique challenges to all the participants and consider how health care disparities may invade the pediatric encounter, making visible the structural and interactional processes that engender them.
Keywords: autism spectrum disorder, child, parent, doctor interaction, health care disparities, electronic health record, pediatric health care
Autism spectrum disorder (ASD, American Psychiatric Association 2013) is defined in biomedicine as a neuro-developmental syndrome of wide phenotypic variability (Muhle et al. 2004). From a sociocultural perspective, it is a “contested category” (Silverman 2012:16): a lived experience, a way of being in the world, and a form of neurodiversity (Eddings Prince 2010; Grinker 2010). Because of this dualistic framing, ASD refracts in important ways the social science research on child–parent–doctor interactions during health care encounters (Tates and Meeuwesen 2001). This literature, however, focuses on health care encounters that meet the sociocultural expectations of normative development under implicitly “default” conditions (i.e., most children in these studies are typically developing, white, and middle-class).
We extend the scope of existing research by examining the health care encounters of African American children diagnosed with ASD. We describe the interactional work of mothers to ensure that their children’s developmental and health care needs are addressed by medical professionals in ways that acknowledge the children’s subjectivities. We offer a description of the mothers’ emic perspectives not only on their child’s health, development, and health care but also on the hidden intersections of race and disability. Such perspectives are exemplified in a mother’s reflection, drawn from our data, about her young son’s future: “He has the rest of his life being black and being labeled autistic” (Solomon and Lawlor 2013:107). As Mattingly (2010) notes: “Structural conditions, identities and power/knowledge discourses are concretely realized … not as necessary or inevitable workings of macrostructures, but as intimate dramas of dismissal, often in the face of great need” (p. 85). We examine the in situ linkages between the structural and interactional processes (Institute of Medicine 1999) that shape African American children’s health care visits and describe the challenges and dilemmas that these visits hold for the participants.
Background
Health Care Encounters: Typically Developing Children
Extensive research has been conducted on typically developing (TD) child–parent–doctor interactions. Metaphors of “social choreography” and “dance of three partners” (Aronsson and Rindstedt 2011; Gabe et al. 2004; Tates et al. 2002) capture the coordination of the participants’ social actions during pediatric visits. The dance, however, does not involve the children to the same degree as the adults: Most often it is the parent who is the primary informant about the child’s health (Clemente et al. 2008; Stivers 2007; Tates and Meeuwesen 2001). Nevertheless, communication during the visits is fundamentally triadic: Although the child is often an over-hearer rather than a speaker, he or she is always a “co-author” (Duranti 1986) of the illness experience.
In the last decade, researchers have called for greater attention to how children learn to “both participate in their medical visits and to be appropriately socialized into the role of an autonomous, accountable patient” (Stivers and Majid 2007:424). Stivers and Majid’s (2007) study of children’s video-recorded visits with pediatricians in community practices in Los Angeles identified a gradual attribution of competence to the child by the adults, realized through the child’s increased opportunities (22% for each additional year of age), to verbally participate in the interaction. When the parent was black, however, the odds that the child was selected as an informant was 78% less than when the parent was white, while no effect of race was found in the willingness of the children to answer the doctor’s questions. These findings suggest that black children are treated by providers as less-competent informants, which decreases their opportunities to be socialized into patient roles (Stivers and Majid 2007). These opportunities may become even scarcer when a child has been diagnosed with ASD.
Complexities of Health Care: Children with ASD
While there is a vast literature on health care utilization of children with ASD (e.g., Croen et al. 2006; Kogan et al. 2008; Liptak et al. 2006), research on health care encounters of both children and adults with ASD is scarce and consists mainly of clinical case studies (Accordino and Walkup 2015; Radcliff 2013; Smith et al. 2012). To our knowledge, this article is the first to provide an analysis of social interactions during pediatric visits involving a child with ASD.
The realization that limitations faced by individuals with ASD present challenges to their health care is a relatively new development in autism research (Lajonchere et al. 2012; Volkmar et al. 2014a). Verbal children may have difficulties in conversational turn-taking and meeting the listener’s informational needs (American Psychiatric Association 2013). One-third of all children with ASD are “minimally verbal” (i.e., have little or no spoken language by school age) (Bauman 2010; Tager-Flusberg and Kasari 2013). Difficulties may stem from the children’s reactivity to sensory stimuli, stereotypic behaviors and mannerisms, self- and other injurious behavior, and wandering and elopement tendencies (American Psychiatric Association 2013; Baranek et al. 2005; Solomon and Lawlor 2013).
Although limitations associated with ASD predictably present problems when there is an illness or an injury, research in this area is mostly lacking (Accordino and Walkup 2015). This is of special concern because many children with ASD have gastrointestinal, seizure and sleep disorders, and other co-occurring conditions (Lajonchere et al. 2012). These conditions are often difficult to diagnose and manage clinically because children with ASD may express their discomfort and pain differently than TD children (American Psychiatric Association 2013; Volkmar et al 2014a). This may lead to a misdiagnosis of underlying problems, over-medication with psychotropic drugs, and decreased participation in family and community life (Accordino and Walkup 2015; Bauman 2010; Goldson and Bauman 2007).
The role of health care providers in addressing this problem is multifaceted. Practice standards and policy mandates call on them to occupy a central role in the management of ASD (Committee on Children with Disabilities 2001a, 2001b; Myers and Johnson 2007; Volkmar et al. 2014b). The providers themselves voice uncertainty about delivering health care for children with ASD, feeling less competent in treating them compared to children with other neuro-developmental conditions (Golnik et al. 2009; Heidgerken et al. 2005).
Alternatively, families struggle to find providers with the skills to treat their children (Lajonchere et al. 2012), reporting less shared decision-making than families of children with special health care needs but without ASD (Bethell et al. 2014). Children with ASD are less likely to receive comprehensive health care services and specialty care compared to TD peers and are more likely to have unmet health care needs compared to both TD children and children with special health care needs but without ASD (Kogan et al. 2008; Liptak et al. 2006, 2008; Tregnago and Cheak-Zamora 2012). These unmet needs occur in the context of greater health care utilization (Croen et al. 2006; Zablotsky et al. 2015), which suggests that it is not the amount but the quality of communication that makes health care effective.
When racialization (Fassin 2011) enters into this picture, the persistent disparities in ASD diagnosis and services across race, ethnicity, states, and even neighborhoods become more extreme (Lord and Bishop 2015). These disparities are associated with unfavorable developmental and health outcomes (Liptak et al. 2008; Mandell et al. 2009). The consequences of these disparities, such as the children’s severe sensory, communicative, and behavioral challenges and undiagnosed health problems, may exceed what can be productively addressed during a health care visit.
In summary, health care visits for children with ASD, and especially for African American children, have not been sufficiently examined. Little is known about what constitutes a “successful” health care visit, how it is “interactionally achieved” (Schegloff 1995), and how the child’s subjectivity and illness experience are framed during these visits. This article addresses these issues from an ethnographic, discourse-analytic perspective, offering an analysis of the interactional and relational work carried out by the child with ASD, the mother, and the physician. Such an analysis generates insights into what it takes for the child with ASD, the mother, and the doctor to achieve a successful health care visit. While a discussion of African American families’ experiences of marginalization related to ASD diagnosis and services can be found elsewhere (Angell and Solomon 2014; Solomon and Lawlor 2013), in this article we consider how health care disparities may invade, in tangible and profound ways, the social interactions between a child with ASD, his mother, and his doctors.
Methods, Sample, and Data
The data are part of a three-year ethnographic, mixed methods study of African American families’ experiences of ASD diagnosis and services in Los Angeles County, California (“Autism in Urban Context: Linking Heterogeneity with Health and Service Disparities,” National Institute for Mental Health, R01 MH089474, 2009-2012, O. Solomon, P.I.). Part of a research tradition in occupational science and medical anthropology, the study draws on narrative, phenomenological, and interpretive approaches to understand families’ illness and disability experiences (Jacobs et al. 2011; Lawlor 2003, 2012; Lawlor and Mattingly 2009, 2014; Mattingly 2010, 2014).
Four California Department of Developmental Services regional centers, a university-affiliated hospital, and a center for developmental disabilities in Los Angeles County served as the study sites. Twenty-three families with a total of 25 children who were diagnosed with ASD participated in the study. Enrolled children were eight years old or younger at recruitment and ranged from four to 11 years during data collection. The children had an ASD diagnosis (American Psychiatric Association 2000) by a licensed professional and a projected need for interventions at one of the study sites. Their primary caregivers self-identified as African American and were all mothers except one family where it was the father. Adult participants included 22 mothers, 15 fathers and stepfathers, 17 extended family members, and 68 professionals, including physicians, occupational therapists, speech pathologists, teachers, and service coordinators. Ethical approval for the study was obtained from the University of Southern California Health Science Campus Institutional Review Board.
The data were collected via participant observation in the home, clinic, school, and community. The description of the data collected for the larger study can be found in Solomon and Lawlor (2013) and Angell and Solomon (2014). Four of the 23 participating families made it possible for us to observe their children’s visits with seven physicians— two developmental pediatricians, two gastroenterologists, one family practitioner, a pediatric neurologist, and a pediatric cardiologist. The observations included the entire visit from the time the child and the mother walked into the clinic until they left. For this article, we analyzed a sub-corpus of 16 observations of the children’s health care visits, 12 interviews with the mothers following these visits, four interviews with the physicians, and field notes.
Most of our analysis focuses on one family whom we followed over a three-year period: Noah, who was six years old at the start of the study, and his mother, Stella. We chose this family because nine of the 16 visits that we observed involved Noah and Stella: six with Dr. Saito, a developmental pediatrician, and three with Dr. Tran, a neurologist. The challenges and achievements that Noah, Stella, and Dr. Saito and Dr. Tran experienced during these visits, while particular and unique to this child, this mother, and these physicians, provide a conceptual framework to “think with” about the experiences of other children with ASD, their parents, and their doctors.
Findings
Collaborative Co-construction of the Child’s Action and Subjectivity
The title of this article (“You can turn off the light if you’d like”) are the first words that Dr. Tran said to Noah during one of the visits when he entered the examination room and saw that Noah had switched off the light. This comment projects several consequential actions: Dr. Tran acknowledges Noah’s sensitivity to the fluorescent light and ratifies an accommodation to meet Noah’s sensory needs. Three video-recorded visits over a six-month period, one with Dr. Tran and two with Dr. Saito, took place in various degrees of semi-darkness because Noah turned off the light and the adults did not turn it back on. There was also an observed, but unrecorded, visit with a specialist where Noah turned off the light while waiting for the doctor, prompting Stella’s light-hearted comment: “You are being energy efficient. Being a conservationist.” In that visit, leaving the light off was not an option afforded by the doctor; he turned the light back on as he entered, without a comment.
These ratifications of Noah’s turning off the light evince what Rapp and Ginsburg (2011) call “the paradox of recognition”: Parents of children with disabilities often seek to “demedicalize” their children to “situate them in a more holistic and communitarian context” (Ginsburg and Rapp 2013:187). This is a consistent theme in our data, but we found that the parents are not the only ones reckoning with this paradox; some of the doctors were engaged in these processes as well.
The following examples drawn from Noah’s video-recorded visits with Dr. Saito describe how this pediatrician’s acceptance of Noah’s sensory needs, combined with Stella’s ability to keep Noah occupied and calm, are linked to the “interactional achievement” (Schegloff 1995) of the visits.
Dr. Saito: Visit 1
Noah and Stella are in the examination room. The room is dark because Noah turned off the light. Only an examination lamp is on, shining a bright light on the wall. When Dr. Saito enters, smiling, Noah looks away from the toy with which he has been playing and says “Hi?” “H::i! Goo::d!” says Dr. Saito, acknowledging Noah’s greeting. Dr. Saito does not comment on the darkness in the room and Stella does not offer any explanation. He shakes hands with Stella and offers Noah his raised hand for a high five. It takes several seconds to coordinate their hands for a high five, but neither the doctor nor the boy give up. “Good job,” says Dr. Saito when their hands touch. “Good job!” Stella says, smiling. Then she begins her update: “We a::re-.” As he sits down, Dr. Saito asks the question that Stella has already begun to answer: “How are we doing overall?” Stella sighs: “One step back from where we’ve been. His behavior has become aggressive since you and I last spoke. If he does not get what he wants he actually comes charging at me.” Dr. Saito’s expression turns serious. He opens Noah’s medical chart and begins to write. Three minutes later, Stella points with frustration to the ceiling where the light would have been: “The light sensitivity thing is just—he is taking light bulbs out in my house! He is now climbing on the vanities in the bathrooms, so wherever Noah is, I have to be. If I don’t take a shower before he wakes up, I don’t get a shower until he goes to bed.”
The visit lasted 28 minutes, and the light was never turned on. During the visit, Stella and Dr. Saito discussed Noah’s complex challenges: gastrointestinal problems, unpredictable aggression, spitting at school, and public displays of sexuality. But Stella and Dr. Saito also talked about Noah’s developmental progress: naming more objects and becoming continent. Throughout this conversation, Noah lay on his side on the exam table playing with a bead-maze toy, his back turned to his mother and the doctor. Stella’s hand rested on Noah’s hip, as if to both calm him and hold him in place. This corporeal arrangement in the semi-dark room was what made this health care visit possible, providing Noah with a way of being self-regulated and occupied while his mother and the doctor talked (see Figure 1).
Figure 1.

Twelve minutes into the visit Dr. Saito had to examine Noah, still in semi-darkness, using the light from the exam lamp. Through all the manipulations of his body, Noah followed Dr. Saito’s instructions with no protest. Thirteen-and-a-half minutes into the visit, when for a second Noah turned the light on, Dr. Saito asked Stella, “This is just a new thing with the light?”
The example illustrates the participants’ complex interactional work during a health care visit for a child with ASD. The assumptions about what a health care visit is expected to be become suspended and new ground rules are followed (e.g., the light should remain off if this is what—as it is tacitly agreed on—Noah needs to stay calm). These ground rules are linked to how Noah’s subjectivity is framed by Stella and Dr. Saito in light of his sensory, communicative, and behavioral challenges. The “interactional achievement” (Schegloff 1995) of the visit is predicated on a transactional engagement of the doctor, the child, and the mother: The doctor’s acceptance of Noah’s need to have the light off affords Stella’s ability to hold Noah in place on the examination table, while Noah’s ability to occupy himself with a toy makes it possible for his mother and the doctor to talk. After the visit, Stella reflected: “I absolutely adore this child, but being a parent is hard work. I mean when I say ‘hard work,’ it’s exhausting, especially when you have a child with special needs.”
During the visit, Stella comments on her vigilance regarding Noah’s comportment and safety: “Wearing heels was not perhaps the wisest thing to do today.” Minutes later, she half-seriously says to Noah: “What are you thinking about doing? I may have the heels on and I may have tripped a couple times, but I can catch up with you.” Another mother in the study, Monica, shared similar concerns about wearing clothes and shoes that provided ease of movement to manage her daughter’s behavior during a health care visit: “I came really ready, gym shoes, yoga pants, cotton shirt, hair in a ponytail, like I’m ready to work, you know.”
After this visit, Dr. Saito reflected on his experiences: “It’s too easy to get frustrated and be dismissive of some of the difficult autistic children, because they’re running around the office more, they may be more destructive, it’s hard, very hard to do an exam, you don’t know how far you’re getting through.” In spite of these difficulties, Dr. Saito described children with ASD as intentional actors with rich subjectivity:
They have the logic going on in their own brain. They’re interpreting the world in a different way, they’re speaking a different language, so the burden is upon me to understand them as much as it is for them to understand our world. No, it’s not about decreased intelligence, it’s a different world. That’s what I keep in mind. That helps me.
Dr. Saito portrays ASD both as a disorder and a way of being, a view strikingly consistent with the “paradox of recognition” (Rapp and Ginsburg 2011).
Dr. Saito: Visit 2
A month later, Noah and Stella were back in Dr. Saito’s office. Noah again turned off the light, and the room was lit only by an examination lamp (see Figures 2–6). Sitting on the examination table, Noah has been shining the lamp on different parts of the room. Dr. Saito enters, smiling. “Hi, Doctor Saito!” says Stella, smiling. Noah turns and looks at Dr. Saito. Dr. Saito, looking at Noah, says: “Hello!” Noah turns away and begins to hum. Stella says: “Noah, say ‘Hi’!” Dr. Saito raises his hand in a greeting, positioning it for a high five. Noah softly says “Hi.” Dr. Saito looks at Noah and says, “How are you?” Noah looks away and does not answer (Figure 2). Stella puts her hand under Noah’s chin and turns his face toward Dr. Saito (Figure 3). “Eye contact!” she says. Dr. Saito leans forward and looks directly into Noah’s face (Figure 4). When Noah does not reply, Dr. Saito places his hand on top of Noah’s forehead, lifts Noah’s face slightly to have a more direct eye gaze and softly asks: “How are you?” (Figure 5). Stella voices a reply: “Good?” Dr. Saito offers another reply “Okay?” and moves his hand away from Noah’s forehead. Noah reaches for Dr. Saito’s hand and holds it for a few seconds, a gesture resembling a high five (Figure 6). Stella says to Noah: “Say ‘good.’” “Good,” Noah says softly. Stella says “Yeah!” Dr. Saito says, “Good job!” and, smiling, turns to Stella and asks her, “How are you doing? Still in the dark?” Stella laughs. “Yes!” Discussion of a surgery that Noah is planned to have in two weeks follows.
Figure 2.

Figure 6.
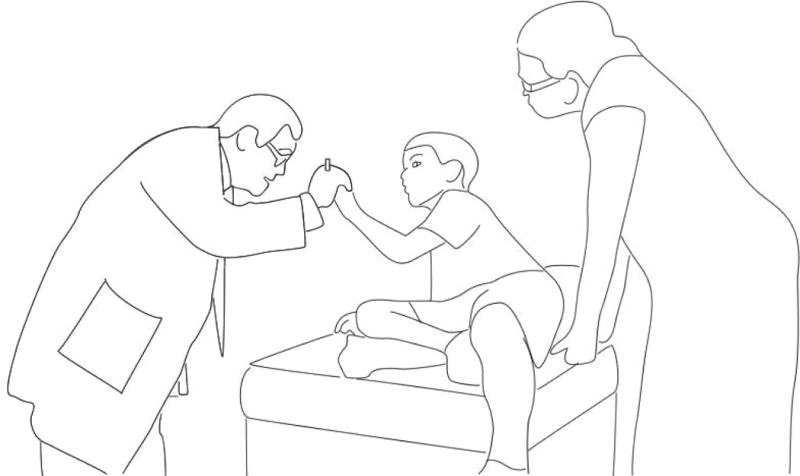
Figure 3.
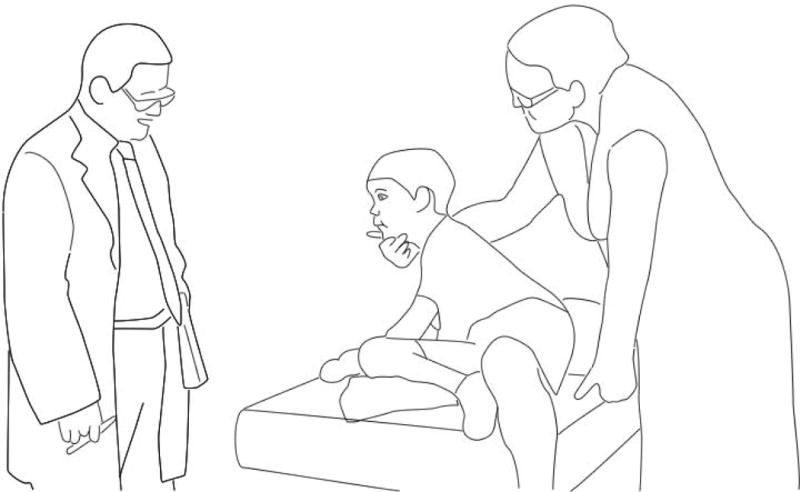
Figure 4.
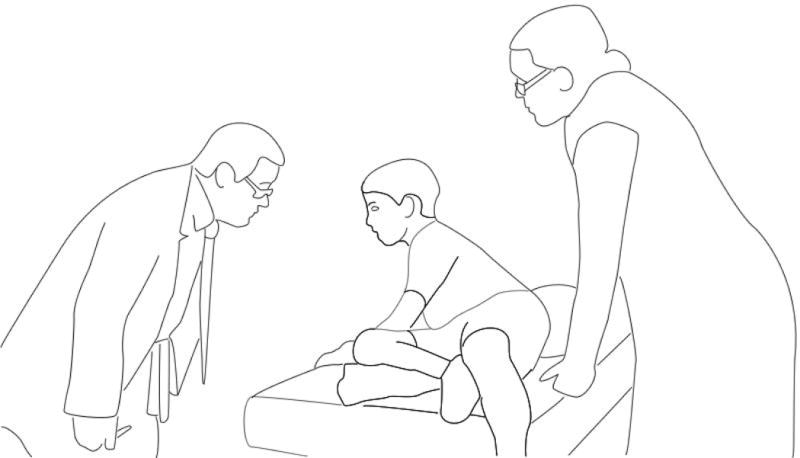
Figure 5.

As in the earlier visit, the light was never turned on. With the exception of Dr. Saito’s semi-humorous question to Stella, “How are you doing? Still in the dark?,” the fact that the three of them were in the dark again was never framed as a problem. This appears to be the ground rules of having a health care visit with Noah: Not make any changes in the physical environment that may set off problematic behaviors and not make the unusual nature of the situation explicit.
These ground rules, however, are not always designed to obscure the child’s limitations. Consider Dr. Saito’s greeting “How are you?” directed to Noah, compared to the greeting from the previous visit, “How are we doing overall?” Directed to both Stella and Noah, “How are we doing overall?” does something subtle: It indexes Noah as an “owner” of his experience but does not directly select him as a speaker and thus does not make him accountable if he does not reply. The greeting of the second health care visit, “How are you?” does the opposite: It makes Noah accountable to both know “how he is” and to reply. If Noah does not reply, it would produce a conditionally relevant absence (Schegloff 1996) (i.e., when an action is noticeably and accountably absent). When Noah does not respond, Stella physically molds his body, directing him to use eye contact and moving his head to face Dr. Saito (Solomon 2011). When Noah softly replies, “Good,” he has become a speaking and participating child. After this visit, Stella reflected:
He (Dr. Saito) took the time to interact with him, where a lot of time the doctors are like, “What’s the problem?,” you know, “What’s going on?” Talk to him! See, engage him! He’ll say something to you, you may not understand it right away, but he’ll tell you something, which is really important because, I think, if any child-, if you lower yourself to their eye level, they can relate to you. But Dr. Saito, he interacts with Noah, he talks to him.
Stella’s insistence that Noah be treated like any child at his eye level matches Dr. Saito’s view of children with ASD as social and intentional. As Stella makes clear in another interview, this perspective is not shared by every physician who sees Noah. For example, Stella remembers another doctor’s (we call him Dr. Simpson) response to Noah’s tantrum during a visit:
Noah had a meltdown that was probably ten times what you saw in there. And Noah wanted to write all over their door and I actually had to wash their door down (laughing). And at the end of the first time they met him, Dr. Simpson came over, shook my hand and said, “God bless you for having so much patience! Just-, God bless you!” I’m just like, I’m like (high-pitched, incredulous tone), “Wha::::t?”
Stella appears to be taken aback by Dr. Simpson’s thanking her for her patience during the visit. In another interview, she fleetingly comments that Dr. Simpson’s “bedside manner is just atrocious.” It seems significant that the doctor’s appreciation does not translate into asking someone from the office staff to wash the door on which Noah drew with his marker, holding Stella publicly accountable for Noah’s behavior.
Stella’s exasperation is shared by another mother in the study around the issue of adaptability of the clinic’s environment to the child’s needs and challenges. Monica, whom we quoted earlier, shared in an interview her frustration with how her daughter Roxanne’s psychotherapist treated her during a visit:
When you deal with a special needs person, you need to be prepared for that. I didn’t like the way Clara (the psychotherapist) treated me like I didn’t have a good attitude, but the first time we went in there I could tell that she judged us already, Roxanne was hyper and I couldn’t control her. Roxanne ran around the clinic, she ran out onto the roof, and that first time she didn’t end up having a tantrum in the clinic but when we left, you know how she gets, in the car she let it out.
Monica’s reflections on being judged and Stella’s account of Dr.
Simpson’s gratitude stand in stark contrast with Stella’s experiences of Noah’s visits with Dr. Saito and Dr. Tran. It would be unthinkable to imagine either Dr. Tran or Dr. Saito thanking Stella for her patience because it would mark the doctor as not having the patience, and stand in conflict with the “paradox of recognition” (Rapp and Ginsburg 2011) that resides in simultaneously seeing Noah’s challenges and his way of being in the world.
In an interview, Stella reflected on what makes the long drives to see Dr. Saito and Dr. Tran worth it: “It just fell into place for Noah. Dr. Saito and Dr. Tran work well together even though they’ve never met. I think Noah has a really good group of doctors. Dr. Saito and Dr. Tran are just phenomenal when it comes to him.” This quote exemplifies Stella’s recognition of the visits as an extended process of health care that has an important impact on Noah’s development, health, and well-being. In the next section, we examine the institutional practices that may hinder this hard-won achievement.
The Transactional Nature of Health Care Encounters
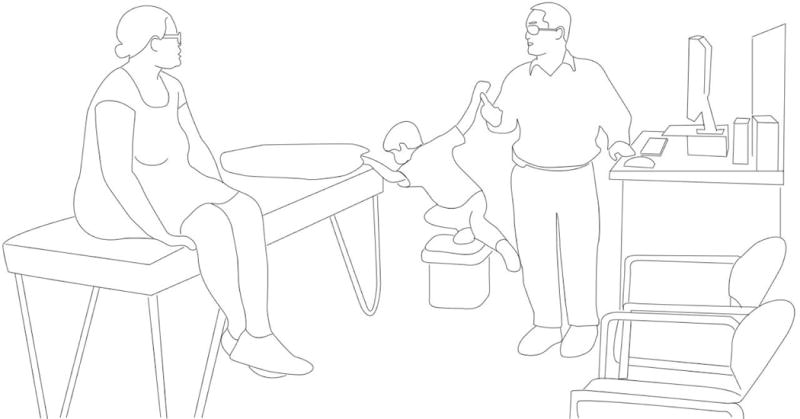
Noah’s three semi-annual visits with Dr. Tran show how the transition to an electronic health record system alters the situated practices of a health care visit. We identify the changes in participation (Goodwin 2007) across the visits and show how the participants orient toward each other and the relevant objects in their physical environment: the medical record and the computer (see Figures 7–14).
Figure 7.

Figure 14.
Dr. Tran: Visit 1
Noah and Stella enter the exam room and sit down at a child-sized table by the door. Noah begins to draw with markers that his mother carries for him in her backpack. Stella sits next to him, making encouraging comments. Eleven minutes later, Dr. Tran enters carrying Noah’s medical chart. He sits in a chair behind Noah, joining him and Stella in the child-centered part of the room (Figure 7). Noah is drawing, supervised by Stella who, because Noah is occupied in an activity, is able to speak with Dr. Tran. The visit begins with updates on medication (Figure 8). While talking with Dr. Tran, Stella also talks to Noah, encouraging him to draw. Dr. Tran stands up and looks over Stella’s shoulder, observing Noah’s drawing (Figure 9). Stella says to Dr. Tran: “He knows how to write his name now. And there’s one major thing, we are now completely potty trained. Number one and two!” Dr. Tran, writing in the chart, says, “That’s great” (Figure 10). Stella goes through her list of concerns about Noah’s sleep, his emerging sexuality, and unexpected responses to medication. Dr. Tran writes in the medical chart, alternating between looking up at Stella and looking down at the chart. When Stella says, “Another concern I’m having is …” or, “Some of my concern is …” Dr. Tran looks up at her from the chart. This “choreography of attention” (Tulbert and Goodwin 2011) provides a predictable interactional framework that renders Stella’s concerns recognized and acknowledged by the doctor.
Figure 8.

Figure 9.
Figure 10.
Five minutes into the visit, Noah draws on the wall and Stella takes the marker away. From this moment on, maintaining the conversation becomes increasingly difficult because Noah’s calm engagement in an activity will become impossible. Noah, upset, lies down on the floor and begins to cry. Stella lifts him up and puts him back in the chair. Noah becomes more upset, crying and stomping his feet.
As his cries grow louder, Stella begins to count backward from 30. At this point, Stella directs all her attention and energy to managing Noah’s behavior, and the conversation between her and Dr. Tran stops. Dr. Tran observes Stella and Noah and writes in the chart. When Stella stops counting, Noah asks “Pa::h” (it may be “pen” or “please”). But Stella cannot risk Noah drawing on the wall again and she puts the marker away.
Noah goes into a full-blown tantrum. Stella sits down with him on the floor, holding him with her arms and legs like a human restraint. Over Noah’s cries, Stella and Dr. Tran have a hard time hearing each other. Stella explains how she learned this method of calming Noah down:
Noah’s former teacher gave me the instruction to put him on the floor, to put your legs over his. But then I was being butted in the head. And I really need your—not necessarily your help—I’ve talked to Regional Center and they’ve talked about other methods, something with the diet but the problem is, he’s not eating.
Stella’s hesitant request for “not necessarily your help” with this problem shows her awareness that this issue is more in the jurisdiction of the regional center that authorizes behavioral services rather than Dr. Tran’s, who provides medication management. The medications are intended, as the American Academy of Pediatrics recommends, to help the child “benefit more optimally from educational interventions” (Myers and Johnson 2007:1163), rather than being an intervention on its own. The dilemma that Stella, Dr. Tran, and Dr. Saito have been facing is that Noah’s educational interventions have been limited and inconsistent. In the absence of a continuous, well-planned intervention program, the medical management of Noah’s behavior took the primary role, which it was not designed to have.
Our data reveal the complex linkages between structural and interactional dimensions of health care disparities (Institute of Medicine 1999). Although ASD alone is associated with a risk for substandard care (Bethell et al. 2014), disparities in autism interventions and services experienced by many African American children may further jeopardize the interactional achievement (Schegloff 1995) of their health care visits. The necessity to manage the child’s sensory, communicative, and behavioral challenges may become the primary focus during the visit, essentially stopping the conversation between the mother and the doctor. The range and severity of a child’s health and behavioral challenges may become impossible to consider and address within the limited time of a health care visit.
Dr. Tran: Visit 2
Six months later, Stella and Noah once again sit at the child-sized table while Noah works on a puzzle. When Dr. Tran walks in, he goes straight to a computer on the other side of the room, sits on a chair, and begins to type. Unlike the past visit when Dr. Tran joined Noah and Stella in the child-centered part of the room, this time Stella and Noah have to join Dr. Tran by the computer. This puts into motion a different participant organization than in the previous visit: It turns from being child-centered to being “computer-centered.”
Stella sits down, facing Dr. Tran at an angle. Noah sits in her lap, and they will now have to maintain his calm demeanor without the help of occupations such as drawing or doing a puzzle. It is now much harder for Noah to be calm and unobtrusive. Stella, excited, begins her update with a story about Noah’s developing sociality:
When I picked him up from school today, one of the boys in his class was crying because his aide was leaving. Noah out of the blue went over to where the tissues are kept, grabbed a tissue, went over to where the little boy was and wiped the tears off of his face! He had actually acknowledged the little boy! Other than that he won’t acknowledge the kids are there.
Dr. Tran types on the computer as she speaks. This second visit is organized around the competing demands introduced by the computer and Dr. Tran’s new obligation to type the notes rather than to write them down. He no longer has the flexibility to move around the room and observe Noah. He appears torn between wanting to look at Stella while listening to her—the choreography of attention (Tulbert and Goodwin 2011) of the previous visit—and having to type on the keyboard. In the middle of the visit, Dr. Tran stops typing long enough for the screen saver to turn on, as he listens to Stella’s story about the second time in a few weeks that Noah used his own feces to “paint” on the walls of his room. Dr. Tran offers several medications to manage this behavior as well as another problematic behavior, running away at school.
Throughout this visit, Noah is draped across Stella’s body, and for the most part, he remains relatively calm. He vocalizes at times as if in protest but never becomes upset as in the previous visit. Several times throughout the visit, he hits himself on the forehead but neither Stella nor Dr. Tran comment on it. The visit is “interactionally achieved” (Schegloff 1995) because Dr. Tran is able to shift his gaze and body orientation from the computer to Stella and Noah (Figure 11) and back to the computer without much disruption in the interaction (Figure 12). Stella is able to contain Noah during the visit in the absence of a child-centered organization of the room. Noah is able to remain relatively calm and content throughout the visit, which allows his mother and Dr. Tran to talk. In the end of the visit, Stella says to Noah: “You did so well.” The third visit, however, will prove to be more challenging.
Figure 11.
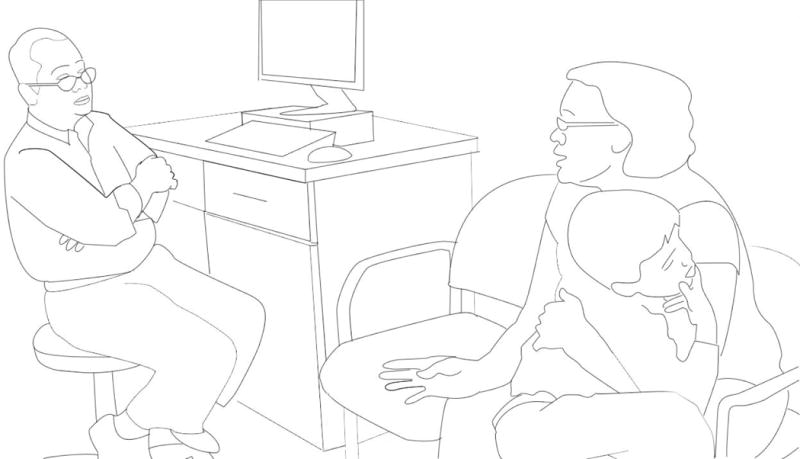
Figure 12.

Dr. Tran: Visit 3
Six months later, Noah and Stella are once again in Dr. Tran’s exam room. Stella sits at the child-size table by the door while Noah stands leaning against her. She asks him to point to animals on a wooden puzzle and then to point to his hair, shirt, and shoes. Dr. Tran enters and sees that Noah has turned off the light. Before uttering a greeting, he says, “You can turn off the light if you’d like. It’s okay with me.” He walks straight to the computer and begins to type. There is no chair by the computer, so Dr. Tran remains standing. Noah, unanchored by a drawing activity or by his mother’s body, begins to explore the room. Stella tries to hold Noah in her lap as she did in the previous visit, but this time she is unable to hold him in place.
What follows next can be interpreted as either a child’s disruptive behavior or a creative way to distract Dr. Tran from the computer. As Noah moves around the room, he touches Dr. Tran’s shoes and pants, then the computer mouse, keyboard, and screen. He runs back and forth from the window to the door, opens cabinets and drawers, stands on the trash can, turns on the water, grabs Dr. Tran’s glasses, and even wraps his arms around Dr. Tran’s neck and shoulders, hanging from his back. Of the many behaviors that Noah could have been engaged in, most of these are aimed at attracting Dr. Tran’s attention. Noah’s overtures, however, make Dr. Tran appear less and less attentive to Stella’s updates. “I have to type,” Dr. Tran says one time, trying to physically disengage from Noah when he takes Dr. Tran’s hand.
Stella, who has been trying to manage Noah’s behavior, now sits alone on the examination table. She continues to give Noah directions but has given up her efforts to physically manage him. She discusses Noah’s medications, often speaking to Dr. Tran’s back and gesticulating as he types on the keyboard (Figure 13). To make eye contact with Stella, Dr. Tran has to turn around, sometimes leaving one hand, as a pivot, on the mouse, posed to type as soon as he turns back to the computer (Figure 14).
Figure 13.

The analysis of this visit shows that the transactional nature of the child–mother–doctor interactions may not only enhance but also diminish the participants’ engagement. Noah is left without the child-centered space where he can engage himself in an activity or his mother’s body where he can remain calm. Dr. Tran must manage the new demands of entering information into Noah’s electronic health record while trying to listen to Stella and to preserve the choreography of attention (Tulbert and Goodwin 2011) that the two of them have enacted in previous visits. With Dr. Tran’s diminished ability to interactionally acknowledge Noah’s challenges and developmental victories, Stella has to work harder to get through her list of concerns. At the end of the visit, Dr. Tran, visibly exhausted, says, “I’ll see him back at the end of the year.”
Discussion and Conclusion
This article contributes an ethnographic, discourse analytic account of the situated health and development-focused work accomplished by the mother, the doctors, and the child with ASD. Our analysis reveals that the orchestration of pediatric health care visits for children with ASD presents new challenges and involves interactional, relational, and spatial work that differs in significant ways from findings reported for TD children.
Specifically, although there are three primary social actors, the interaction between them cannot be categorized as triadic, as is the case in the TD children’s visits. Rather, there are three separate dyadic interactions—child–mother, child–doctor, and mother–doctor—that take place during most of the visits described here. This may partly explain Liptak and colleagues’ (2006) finding that outpatient visits of children with ASD are twice as long as visits of other clinical populations of children.
Moreover, the child’s communicative, sensory and other limitations imposed by ASD present challenges to all the participants in the visit. We demonstrated how, when a child with autism walks into a doctor’s office, the encounter becomes a precarious, hard-won interactional achievement (Schegloff 1995) rather than a predictable event. We outlined the transactional nature of the work required from all three participants to achieve a “successful” health care visit. We considered the import of the physical environment in this achievement (e.g., the quality of light, the child-centeredness of the room, and the prominence of the computer).
We described how structural and interactional dimensions of health care disparities become intertwined and amplified when the child’s behavioral and educational services are inconsistent and showed how this impacts the child’s ability to participate in the visit and how it increases the range and magnitude of concerns that the mother and the physicians have to address.
Our analysis points to what is “at stake” (Kleinman 1988:55) in these visits as Stella vigilantly orchestrates interactions with the doctors to stay clear of “harsh judgment” while paying “respectful regard” to Noah’s subjectivity and humanity (Lawrence-Lightfoot and Davis 1997:52). Much has been written in anthropology and other social sciences about ways in which parents of children with disabilities “come to locate, interpret and often advocate for (their) personhood” (Gray 2002; Landsman 2003:1948; Ortega 2009). Stella’s interactional and relational work during the visits insists on Noah’s fundamental humanity while contesting potential “othering” categorizations related not only to ASD, but also to being African American. In one of the interviews, she told a story about filling out a form where she had to check a box indicating that Noah was black. “Instead of checking any of those off, I made my own box and I put ‘Human,’” she said.
This quote explicitly marks Stella’s commitment to another kind of vigilance: to oversee and anticipate the intersections of race and disability (i.e., the direct and implicit ways in which race can exacerbate potential impediments to her son’s care). There were many more subtle and nuanced ways, however, in which this work was undertaken. The “conditionally relevant absence” (Schegloff 1996) of the intrusion of race, disability, and disparities within the moments of health care visits was also evident. Stella’s actions often embodied her determination to insist on Noah’s humanity while avoiding the boxes denoting race and disability both on forms and during interactions with the doctors. Many of her elicitations and narrations of her son’s actions were designed to illuminate Noah’s capacities and attributes as first and foremost a child.
The physicians’ actions often supported and enhanced Stella’s interactional and relational work during the visits, enacting the expectation that Noah was a competent co-participant in obvious ways such as engaging in social greetings, but also in more subtle ways evident in statements like “I have to type.” These actions constituted Noah’s sociality and potentiality as a relational participant in the health care visit, standing in stark contrast to commonly held presumptions of the lack of sociality and diminished subjectivity in children with ASD.
The study has limitations in that health care visits data were collected for only four families of 23 who participated in the larger study. Some parents invited us to most of their children’s appointments that took place during data collection, while other families never did. The families may have invited us to observe visits mostly with providers with whom they had positive relationships that would not have been jeopardized by the presence of an outside observer. This potentially provided an overly positive view of the phenomena. Even this view, however, allowed a window into the challenges that the families faced in seeking health care for their children.
In spite of the consistently unmet health care needs of children with ASD and the mandate for health care providers’ central role in managing this medically complex and chronic condition, there have been few practical strategies to improve the provision of health care for children with ASD and their families. This article aimed to show that the health care visit is a promising site where such strategies can begin to be developed.
Acknowledgments
We are deeply grateful to the children, their families and the physicians who participated in this research. We thank our collaborators: Sharon Cermak, Ed.D., Marie Poulsen, Ph.D., Thomas Valente, Ph.D., and Marian Williams, Ph.D.
This study was supported by a grant “Autism in Urban Context: Linking Heterogeneity with Health and Service Disparities” (NIH/NIMH, R01 MH089474, 2009-2012, O. Solomon, P.I.). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the. The authors gratefully acknowledge the support of the USC Mrs. T.H. Chan Division of Occupational Science and Occupational Therapy at the Herman Ostrow School of Dentistry at the University of Southern California.
References Cited
- Accordino RE, Walkup JT. The Medical and Psychiatric Evaluation of the Nonverbal Child. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54:11–24. doi: 10.1016/j.jaac.2014.09.018. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: American Psychiatric Publications; 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. Arlington, VA: American Psychiatric Publications; 2013. [Google Scholar]
- Angell AM, Solomon O. The Social Life of Health Records: Understanding Families’ Experiences of Autism. Social Science & Medicine. 2014;117:50–57. doi: 10.1016/j.socscimed.2014.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aronsson K, Rindstedt C. Alignments and Facework in Paediatric Visits: Toward a Social Choreography of Multiparty Talk. In: Candlin CN, Sarangi S, editors. Communication in Professions and Organisations: Handbook of Applied Linguistics 3. Berlin: Mouton de Gruyter; 2011. pp. 121–142. [Google Scholar]
- Baranek GT, Parham D, Bodfish JW. Sensory and Motor Features in Autism: Assessment and Intervention. In: Volkmar F, Paul R, Klin A, Cohen D, editors. Handbook of Autism and Pervasive Developmental Disorders. 3rd. Vol. 2. Hoboken, NJ: John Wiley & Sons; 2005. pp. 831–857. [Google Scholar]
- Bauman ML. Medical Comorbidities in Autism: Challenges to Diagnosis and Treatment. Neurotherapeutics. 2010;7:320–327. doi: 10.1016/j.nurt.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethell CD, Lindly O, Kogan M, Zuckerman K. Health Care Quality for Children: The Position of Autism Spectrum Disorder. In: Patel VB, Preedy VR, Martin CR, editors. Comprehensive Guide to Autism. New York: Springer; 2014. pp. 139–165. [Google Scholar]
- Clemente I, Lee SH, Heritage J. Children in Chronic Pain: Promoting Pediatric Patients’ Symptom Accounts in Tertiary Care. Social Science & Medicine. 2008;66:1418–1428. doi: 10.1016/j.socscimed.2007.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Children with Disabilities. The Pediatrician’s Role in the Diagnosis and Management of Autistic Spectrum Disorder in Children. Pediatrics. 2001a;107:1221–1226. doi: 10.1542/peds.107.5.1221. [DOI] [PubMed] [Google Scholar]
- Committee on Children with Disabilities. The Pediatrician’s Role in Development and Implementation of an Individual Education Plan (IEP) and/or an Individual Family Service Plan (IFSP) Pediatrics. 2001b;104:124–127. doi: 10.1542/peds.104.1.124. [DOI] [PubMed] [Google Scholar]
- Croen LA, NajjarG DV, Ray T, Lotspeich L, Bernal P. A Comparison of Health Care Utilization and Costs of Children with and without Autism Spectrum Disorders in a Large Group-model Health Plan. Pediatrics. 2006;118:e1203–e1211. doi: 10.1542/peds.2006-0127. [DOI] [PubMed] [Google Scholar]
- Duranti A. The Audience as Co-author: An Introduction. Text. 1986;6:239–247. [Google Scholar]
- Eddings Prince D. An Exceptional Path: An Ethnographic Narrative Reflecting on Autistic Parenthood from Evolutionary, Cultural, and Spiritual Perspectives. Ethos. 2010;38:56–68. [Google Scholar]
- Fassin D. Racialization: How to Do Races with Bodies. In: Mascia-Lees FE, editor. A Companion to the Anthropology of the Body and Embodiment. West Sussex, UK: Wiley-Blackwell; 2011. pp. 419–434. [Google Scholar]
- Gabe JN, Olumide G, Bury M. “It Takes Three to Tango”: A Framework for Understanding Patient Partnership in Paediatric Clinics. Social Science & Medicine. 2004;59:1071–1079. doi: 10.1016/j.socscimed.2003.09.035. [DOI] [PubMed] [Google Scholar]
- Ginsburg F, Rapp R. Entangled Ethnography: Imagining a Future for Young Adults with Learning Disabilities. Social Science & Medicine. 2013;99:187–193. doi: 10.1016/j.socscimed.2013.11.015. [DOI] [PubMed] [Google Scholar]
- Goldson E, Bauman M. Medical Health Assessment and Treatment Issues in Autism. In: Gabriels RL, Hill DE, editors. Growing up with Autism: Working with School Aged Children. New York: The Guilford Press; 2007. pp. 39–57. [Google Scholar]
- Golnik A, Ireland M, Borowsky IW. Medical Homes for Children with Autism: A Physician Survey. Pediatrics. 2009;123:966–971. doi: 10.1542/peds.2008-1321. [DOI] [PubMed] [Google Scholar]
- Goodwin C. Participation, Stance and Affect in the Organization of Activities. Discourse & Society. 2007;18:53–73. [Google Scholar]
- Gray D. Everybody Just Freezes. Sociology of Health and Illness. 2002;24:734–749. [Google Scholar]
- Grinker RR. Commentary: On Being Autistic, and Social. Ethos. 2010;38:172–178. [Google Scholar]
- Heidgerken AD, Geffken G, Modi A, Frakey L. A Survey of Autism Knowledge in a Health Care Setting. Journal of Autism and Developmental Disorders. 2005;35:323–330. doi: 10.1007/s10803-005-3298-x. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Measuring the Quality of Health Care. Washington, DC: National Academy Press; 1999. [Google Scholar]
- Jacobs L, Lawlor MC, Mattingly C. I/We narratives among African American Families Raising Children with Special Needs. Culture, Medicine, and Psychiatry. 2011;35:3–25. doi: 10.1007/s11013-010-9196-5. [DOI] [PubMed] [Google Scholar]
- Kleinman A. The Illness Narratives: Suffering, Healing, and the Human Condition. New York: Basic Books; 1988. [Google Scholar]
- Kogan MD, StricklandS BB, Blumberg J, Singh GK, Perrin JM, van Dyck PC. A National Profile of the Health Care Experiences and Family Impact of Autism Spectrum Disorder among Children in the United States, 2005–2006. Pediatrics. 2008;122:e1149–e1158. doi: 10.1542/peds.2008-1057. [DOI] [PubMed] [Google Scholar]
- Lajonchere C, Jones N, Coury DL, Perrin JM. Leadership in Health Care, Research, and Quality Improvement for Children and Adolescents with Autism Spectrum Disorders: Autism Treatment Network and Autism Intervention Research Network on Physical Health. Pediatrics. 2012;130(Supp. 2):S62–S68. doi: 10.1542/peds.2012-0900C. [DOI] [PubMed] [Google Scholar]
- Landsman G. Emplotting Children’s Lives: Developmental Delay vs. Disability. Social Science & Medicine. 2003;56:1947–1960. doi: 10.1016/s0277-9536(02)00215-0. [DOI] [PubMed] [Google Scholar]
- Lawlor MC. The Significance of Being Occupied: The Social Construction of Childhood Occupations. The American Journal of Occupational Therapy. 2003;57:424–434. doi: 10.5014/ajot.57.4.424. [DOI] [PubMed] [Google Scholar]
- Lawlor MC. The Particularities of Engagement: Intersubjectivity in Occupational Therapy Practice. OTJR: Occupation, Participation & Health. 2012;32:151–159. [Google Scholar]
- Lawlor MC, Mattingly C. Understanding Family Perspectives on Illness and Disability Experience. In: Crepeau EB, Cohn ES, Schell BAB, editors. Willard & Spackman’s Occupational Therapy. Philadelphia: Wolters Kluwer Lippincott Williams & Wilkins; 2009. pp. 33–44. [Google Scholar]
- Lawlor MC, Mattingly C. Family Perspectives on Occupation, Health and Disability. In: Schell B, Gillen G, Scaffa M, editors. Willard & Spackman’s Occupational Therapy. Philadelphia: Lippincott Williams & Wilkins; 2014. pp. 149–162. [Google Scholar]
- Lawrence-Lightfoot S, Davis JH. The Art and Science of Portraiture. San Francisco: Jossey-Bass; 1997. [Google Scholar]
- Liptak GS, Benzoni LB, Mruzek DW, Nolan KW, Thingvoll MA, Wade CM, Fryer GE. Disparities in Diagnosis and Access to Health Services for Children with Autism: Data from the National Survey of Children’s Health. Journal of Developmental & Behavioral Pediatrics. 2008;29:152–160. doi: 10.1097/DBP.0b013e318165c7a0. [DOI] [PubMed] [Google Scholar]
- Liptak GS, Stuart T, Auinger P. Health Care Utilization and Expenditures for Children with Autism: Data from US National Samples. Journal of Autism and Developmental Disorders. 2006;36:871–879. doi: 10.1007/s10803-006-0119-9. [DOI] [PubMed] [Google Scholar]
- Lord C, Bishop SL. Recent Advances in Autism Research as Reflected in DSM-5 Criteria for Autism Spectrum Disorder. Annual Review Clinical Psychology. 2015;11:7.1–7.18. doi: 10.1146/annurev-clinpsy-032814-112745. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Wiggins LD, Carpenter LA, Daniels J, DiGuiseppi C, Durkin MS, Giarelli E, Morrier MJ, Nicholas JS, Pinto-Martin J, Shattuck PT, Thomas KC, Yeargin-Allsopp M, Kirby RS. Racial/Ethnic Dsparities in the Identification of Children with Autism Spectrum Disorders. American Journal of Public Health. 2009;99:493–498. doi: 10.2105/AJPH.2007.131243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattingly C. The Paradox of Hope: Journeys through a Clinical Borderland. Berkeley: University of California Press; 2010. [Google Scholar]
- Mattingly C. Moral Laboratories: Family Peril and the Struggle for a Good Life. Oakland: Univesity of California Press; 2014. [Google Scholar]
- Muhle R, Trentacoste SV, Rapin I. The Genetics of Autism. Pediatrics. 2004;113:e472–e486. doi: 10.1542/peds.113.5.e472. [DOI] [PubMed] [Google Scholar]
- Myers SM, Johnson CP. Management of Children with Autism Spectrum Disorders. Pediatrics. 2007;120:1162–1182. doi: 10.1542/peds.2007-2362. [DOI] [PubMed] [Google Scholar]
- Ortega F. The Cerebral Subject and the Challenge of Neurodiversity. BioSocieties. 2009;4:425–445. [Google Scholar]
- Radcliff L. Breast Cancer and Autism. Journal of the Advanced Practitioner in Oncology. 2013;4:113–117. [PMC free article] [PubMed] [Google Scholar]
- Rapp R, Ginsburg FD. The Paradox of Recognition: Success or Stigma for Children with Learning Disabilities. In: McLaughlin J, editor. Contesting Recognition: Contemporary Cultural and Institutional Disputes. New York: Palgrave; 2011. pp. 166–186. [Google Scholar]
- Schegloff EA. Discourse as an Interactional Achievement III: The Omnirelevance of Action. Research on Language and Social Interaction. 1995;28:185–211. [Google Scholar]
- Schegloff EA. Issues of Relevance for Discourse Analysis: Contingency in Action, Interaction and Co-participant Context. In: Hovy EH, Scott DR, editors. Computational and Conversational Discourse: Burning Issues—An Interdisciplinary Account. Berlin: Springer; 1996. pp. 3–35. [Google Scholar]
- Silverman C. Understanding Autism: Parents, Doctors, and the History of a Disorder. Princeton: Princeton University Press; 2012. [Google Scholar]
- Smith MD, Graveline PJ, Smith JB. Autism and Obstacles to Medical Diagnosis and Treatment: Two Case Studies. Focus on Autism and Other Developmental Disabilities. 2012;27:189–195. [Google Scholar]
- Solomon O. Body in Autism: A View from Social Interaction. In: McPherron P, Ramanathan V, editors. Language, Body, and Health. Boston: De Gruyter Mouton; 2011. pp. 105–141. [Google Scholar]
- Solomon O, Lawlor MC. “And I Look Down and He Is Gone”: Narrating Autism, Elopement and Wandering in Los Angeles. Social Science & Medicine. 2013;94:106–114. doi: 10.1016/j.socscimed.2013.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stivers T. Prescribing under Pressure: Parent–Physician Conversations and Antibiotics. New York: Oxford University Press; 2007. [Google Scholar]
- Stivers T, Majid A. Questioning Children: Interactional Evidence of Implicit Bias in Medical Interviews. Social Psychology Quarterly. 2007;70:424–441. [Google Scholar]
- Tager-Flusberg H, Kasari C. Minimally Verbal School-aged Children with Autism Spectrum Disorder: The Neglected End of the Spectrum. Autism Research. 2013;6:468–478. doi: 10.1002/aur.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tates K, Elbers E, Meeuwesen L, Bensing J. Doctor–Parent–Child Relationships: A “Pas de Trois.”. Patient Education and Counseling. 2002;48:5–14. doi: 10.1016/s0738-3991(02)00093-9. [DOI] [PubMed] [Google Scholar]
- Tates K, Meeuwesen L. Doctor–Parent–Child Communication. A (Re)view of the Literature. Social Science & Medicine. 2001;52:839–851. doi: 10.1016/s0277-9536(00)00193-3. [DOI] [PubMed] [Google Scholar]
- Tregnago MK, Cheak-Zamora NC. Systematic Review of Disparities in Health Care for Individuals with Autism Spectrum Disorders in the United States. Research in Autism Spectrum Disorders. 2012;6:1023–1031. [Google Scholar]
- Tulbert E, Goodwin MH. Choreographies of Attention: Multimodality in a Routine Family Activity. In: Streeck J, Goodwin C, LeBaron C, editors. Embodied Interaction: Language and Body in the Material World. Cambridge: Cambridge University Press; 2011. pp. 79–92. [Google Scholar]
- Volkmar FR, Rowberry J, De Vinck-Baroody O, Gupta AR, Leung J, Meyers J, Vaswani N, Weisner LA. Medical Care in Autism and Related Conditions. In: Volkmar FR, Paul R, Pelphrey K, editors. Handbook of Autism and Developmental Disorders. Hoboken, NJ: John Wiley & Sons; 2014a. pp. 532–554. [Google Scholar]
- Volkmar F, Siegel M, Woodbury-Smith M, King B, McCracken J, State M, American Academy of Child and Adolescent Psychiatry Committee on Quality Issues (CQI) Practice Parameter for the Assessment and Treatment of Children and Adolescents with Autism Spectrum Disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2014b;53:237–257. doi: 10.1016/j.jaac.2013.10.013. [DOI] [PubMed] [Google Scholar]
- Zablotsky B, Pringle BA, Colpe LJ, Kogan MD, Rice C, Blumberg SJ. Service and Treatment Use among Children Diagnosed with Autism Spectrum Disorders. Journal of Developmental & Behavioral Pediatrics. 2015;36:98–105. doi: 10.1097/DBP.0000000000000127. [DOI] [PMC free article] [PubMed] [Google Scholar]


