Abstract
Objective
Screening adolescents for depression is recommended by the U.S. Preventive Services Task Force. We sought to evaluate the impact of positive depression screens in an adolescent population on healthcare utilization and costs from a payer perspective.
Methods
We conducted depression screening among 13-17 year olds adolescents enrolled in a large integrated care system using the 2- and 9-item Patient Health Questionnaires (PHQ). Healthcare utilization and cost data were obtained from administrative records. Chi-square, Wilcoxon rank-sum, and t-tests were used to test for statistical differences in outcomes between adolescents based on screening status.
Results
Of the 4,010 adolescents who completed depression screening, 3,707 (92.4%) screened negative (PHQ-2 < 2 or PHQ-9 < 10), 186 (3.9%) screened positive for mild depression (PHQ-9 = 10-14), and 95 (2.4%) screened positive for moderate-to-severe depression (PHQ-9 ≥ 15). In the 12-months after screening, screen-positive adolescents were more likely than screen-negative adolescents to receive any emergency department visit or inpatient hospitalization, and had significantly higher utilization of outpatient medical (mean (SD) = 8.3 (1.5) vs. 3.5 (5.1)) and mental health (3.8 (9.3) vs. 0.7 (3.5)) visits. Mean total healthcare system costs for screen-positive adolescents ($5,083 ($10,489)) were more than twice as high as those of screen-negative adolescents ($2,357 ($7,621)).
Conclusion
Adolescent depressive symptoms, even when mild, are associated with increased healthcare utilization and costs. Only a minority of the increased costs is attributable to mental health care. Implementing depression screening and evidence-based mental health services may help to better control healthcare costs among screen-positive adolescents.
Keywords: Depression, Mental Health, Adolescent Health, Costs, Economic Analysis
INTRODUCTION
In 2011, 28.5% of adolescents reported feeling sad or hopeless almost every day for two weeks or more, close to 16% of adolescents seriously considered attempting suicide, and almost 13% of adolescents made a suicide plan.1 An estimated 14% of adolescents experience a mood disorder, such as major depressive disorder or bipolar disorder, by age 18.2 Adolescents with major depressive disorder are more likely to smoke, to use alcohol, have anxiety or other mental disorders, and to have made a suicide attempt.3,4 One study estimated that patients who were diagnosed with major depressive disorder as children have lifetime annual healthcare expenditures that are nearly double those of their peers.5
Both the U.S. Preventive Services Task Force (USPSTF, 2009) and the American Academy of Pediatrics (AAP, 2014) recommend that medical practitioners screen adolescents for depression when systems are in place to ensure accurate diagnosis, treatment, and follow-up. 6 Screening positive for depression could affect adolescent productivity and educational attainment.7 As healthcare providers decide whether to implement broad-based depression screening in their practices, it is important to understand the effect adolescent depression has on healthcare utilization and payer's expenditures. Many studies have examined the percentage of adolescents with depression who use mental health services and have found that treatment is underutilized. Estimates of mental healthcare utilization among adolescents with depression range from 18-60%.4,8-11
While cost-effectiveness analyses of several adolescent depression screening and treatment interventions have been previously reported12,13, few studies have been conducted to describe the economic healthcare cost of adolescent depression. In an analysis of data from the 1996 U.S. Medical Expenditure Panel Survey, Guevara et al. found that children who had been diagnosed with depression, anxiety and other emotional disorders had annual healthcare expenditures of $2,237 (95% CI: $1,426, $3,050), higher than annual expenditures of children with physical disorders such as asthma or diabetes ($1,245, 95% CI: $106, $2,386), children with behavioral disorders such as ADHD ($1,167, 95% CI: $903, $1,340), and otherwise healthy children ($834, 95% CI: $11, $1,658) (all estimates in 1996 USD). 14,15 Another study of data from a large integrated healthcare system by Richardson et al. found that the payer-incurred healthcare expenditures for youth with depression and asthma were 51% higher than those for youth with asthma alone.16
Unfortunately, study populations for many analyses conducted to date have been limited to youth with a coded diagnosis of major depressive disorder (MDD), which does not represent the full spectrum and prevalence of clinical depression.17 In this study, we aimed to use a reliable, validated depression screening instrument and automated utilization data from a large integrated healthcare system to evaluate the payer-incurred cost of adolescent depressive symptoms and the types of services used by adolescents with clinically significant depressive symptoms. We hypothesized that annual expenditures for adolescents who screened positive for depression would be significantly higher than those for adolescents who did not screen positive for depression and that only a small percentage of costs would be due to mental health treatment. 18-21
METHODS
This analysis was conducted as part of the Reaching Out to Adolescents in Distress (ROAD) study. ROAD was a randomized clinical trial to evaluate a collaborative care intervention for adolescent depression in primary care settings. 21 Adolescents from nine primary care clinics in the Group Health (GH) integrated healthcare system were screened for depression. Adolescents who screened positive were invited to participate in a follow-up evaluation. All individuals who continued to screen positive were either invited to participate in the ROAD intervention study or assisted with connecting with other resources if they were found to be depressed but not eligible for intervention participation due to exclusion criteria. Those who wished to participate and met study eligibility criteria were randomized to intervention (n = 50) or usual care (n = 51). The ROAD study intervention included the provision of care managers who would assist youth in initiating and maintaining evidence based treatments, including antidepressants and brief psychotherapy delivered by the care manager in the primary care clinic. 21 This study utilizes administrative data from all participants who were screened for symptoms of MDD to assess eligibility for the ROAD study. It therefore includes the ROAD study participants as a subsample of the current study population. The Seattle Children's Hospital and GH Institutional Review Boards approved the study protocol.
Participants
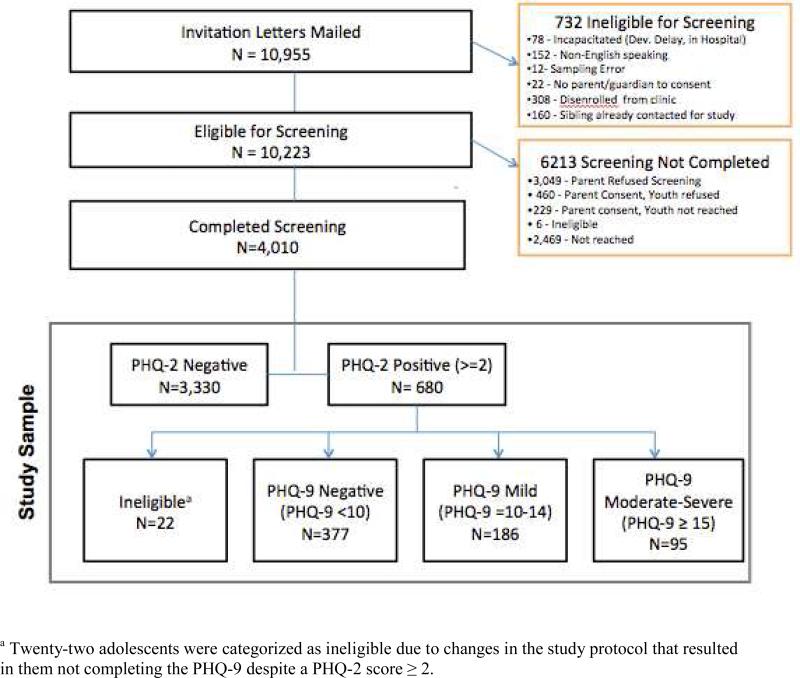
Participants were recruited between April 2010 and March 2012 from the population of 13-17 year olds enrolled in any of nine urban primary care GH clinics in western Washington State. 10,955 adolescents were contacted first by mail, and subsequently by phone, to participate in the study. Participants were excluded from the analysis if they were unable to complete survey questions due to developmental delay or being hospitalized, non-English speaking, no longer enrolled in Group Health, had a sibling who had already been invited to participate in the study, if there was no parent or guardian to consent, or due to sampling error. (Figure 1)
Figure 1.
ROAD Study Sample
Screening
Depression screening was conducted using the Patient Health Questionnaire (PHQ) Depression Scales, validated self-report instruments that are extensively used to screen for depressive disorders in primary care settings.22 Screening was conducted in two steps within the same phone call. First, adolescents completed the PHQ-2, a two-item screening tool that inquires about symptoms of depression and anhedonia over the past two weeks. 23 A PHQ-2 score of 2 or greater has a sensitivity of 100% and a specificity of 62% for detecting MDD among adolescent populations.23 Those that scored 2 or greater then completed the remaining seven items of the full PHQ-9, a nine-item questionnaire that further identifies the presence and severity of depressive symptoms.24 A PHQ-9 score of 10 or greater has a sensitivity of 89.5% and a specificity of 72.1% for detecting MDD among adolescents.24 Both the PHQ-2 and the PHQ-9 were administered by phone, which has been shown to be a valid method for assessing depressive symptoms in adult and adolescent populations. 23-25
Depressive symptom severity was categorized based on the results of the PHQ-2 and PHQ-9 screening. A PHQ-2 score < 2 or a PHQ-2 score ≥ 2 with a PHQ-9 score < 10 represented a low likelihood of MDD, a PHQ-9 score of 10-14 represented probable mild MDD and a PHQ-9 score ≥ 15 represented probable moderate-to-severe MDD.
Study Measures
Baseline demographic and health characteristics, including age, gender, public insurance coverage, race/ethnicity, body mass index (BMI) z-score, and BMI class (i.e. normal weight, overweight, or obese), were assessed from GH administrative data records and a participant survey. We also calculated each patient's Pediatric Chronic Disease Score (PCDS), a measure of chronic disease burden estimated using data on prescription drug fills from the 12 months prior to screening.26 The PCDS was calculated both including and excluding data on antidepressant prescription drug fills.
GH is an integrated care provider which coordinates both care and coverage for its members. We collected data from GH administrative records on each patient's healthcare utilization and expenditures related to outpatient visits, inpatient visits, emergency department (ED) visits, prescription drugs, and diagnostic lab tests in the 12 months after PHQ screening. Utilization was categorized as mental health or non-mental health-related care based on GH provider specialty. GH expenditure data includes estimates of direct costs related to administering patient healthcare, overhead costs in GH clinics, and costs related to approved out of plan services paid by GH. Overhead costs consisted of costs related to facilities, payroll, and other administrative departments. Therefore, the cost analysis was conducted from the perspective of the payer, GH. All costs were incurred between February 2010 and March 2013. All costs were inflated to 2013 common dollars using the medical care component of the U.S. Consumer Price Index. 15 Grant-funded intervention costs related to the conduct of the ROAD intervention study21, specifically including costs related to coordinated care management and cognitive behavioral therapy sessions provided as part of the intervention, were excluded from this analysis.
Statistical Analysis
Demographic, health, utilization, and expenditure data were summarized for groups of patients defined by depression screening status. Bivariate analyses were performed using Pearson's X2 tests to examine the differences in categorical characteristics (i.e. gender, type of insurance, race/ethnicity, and BMI class) by level of depressive symptom severity. T-tests were used to compare continuous predictors (i.e. age, PCDS, and BMI z-score) between groups. As utilization and expenditure data tend to have non-normal, skewed distributions, the nonparametric Wilcoxon-Mann-Whitney and Kruskal-Wallis tests were used to test for statistically significant differences in utilization and expenditures between groups. All statistical analyses were conducted using SAS, version 9.3 (© 2012, SAS Institute Inc., Cary, North Carolina).
RESULTS
Participants
Parental and adolescent consent was obtained for 4,010 of the 10,955 patients originally invited to participate in the study. (Figure 1) Of those for whom consent was obtained, 3,330 adolescents (83.0%) screened negative for depression using the PHQ-2 and 680 adolescents (17.0%) screened positive for depression. Of 680 adolescents that screened positive for depression on the PHQ-2, 377 (55.4%) screened negative for depression and 281 (41.3%) screened positive for depression based on a score of 10 or greater on the PHQ-9. Twenty-two adolescents (3.2%) were categorized as ineligible due to changes in the study protocol that resulted in them not completing the PHQ-9 despite have a PHQ-2 score of 2. Among the 281 adolescents who screened positive for depression on the PHQ-9, 186 (66.2%) were categorized as probable mild MDD (PHQ-9 of 10 to 14) and 95 (33.8%) were categorized as probable moderate-to-severe MDD (PHQ-9 ≥ 15).
Healthcare Utilization and Payer-Incurred Expenditures
Adolescents who screened positive for any depression were significantly more likely to be female (69% vs. 49%, p < 0.01), publicly insured (13% vs. 9%, p < 0.01), and obese (14% vs. 9%, p = 0.02). Screen-positive adolescents were slightly older than their screen-negative counterparts (15.2 vs. 15.0 years old, p < 0.01). The Pediatric Chronic Disease Score, a measure of chronic disease burden, increased with increased severity of depressive symptoms (p < 0.01), indicating higher medical disease burden even when excluding antidepressant prescriptions. (Table 1)
Table 1.
Population Characteristics by Severity of Probable Major Depressive Disorder (MDD)
| Screen negative+ n= 3707 | Screen Positive+ | p | |||
|---|---|---|---|---|---|
| Mild MDD n= 186 | Moderate-to-Severe MDD n= 95 | All MDD n= 281 | |||
| Demographic Characteristics a | |||||
| Age in years, mean (SD) | 15.0 (1.4) | 15.3 (1.3) | 15.1 (1.3) | 15.2 (1.3) | 0.01c |
| Female Gender | 49.3% | 67.2% | 73.7% | 69.4% | < 0.01c |
| Public Insurance | 8.5% | 14.5% | 10.5% | 13.2% | 0.02c |
| Race/ethnicity | 0.09 | ||||
| White Non-Hispanic | 59.5% | 59.7% | 67.4% | 62.3% | |
| African-American Non-Hispanic | 7.5% | 8.6% | --d | 7.5% | |
| Hispanic | 6.7 | 6.5% | --d | 6.0% | |
| Asian/Pacific Islander | 8.3% | 5.9% | --d | 5.3% | |
| Other/Unknown | 18.1% | 19.4% | 17.9% | 18.9% | |
| Health Characteristics § | |||||
| Pediatric Chronic Disease Score26 | |||||
| Total, mean (SD) | 412.5 (687.7) | 520.9 (655.9) | 831.9 (1091.3) | 626.0 (840.1) | < 0.01c |
| Excluding antidepressants, mean (SD) | 403.4 (673.6) | 472.5 (627.8) | 725.4 (902.3) | 558.0 (740.3) | < 0.01c |
| BMI z-score, mean (SD) | 0.48 (0.98) | 0.66 (1.0) | 0.67 (0.99) | 0.66 (1.0) | 0.02c |
| Obese | 9.2% | 13.9% | 12.6% | 13.5% | 0.03c |
All results are expressed as percentages unless otherwise indicated
b Probable depression severity was categorized by PHQ-2 and PHQ-9 screening results. A PHQ-2 score < 2 OR a PHQ-2 score ≥ 3 and a PHQ-9 score < 10 represented a probably non-depressed patient, a PHQ-9 score of 10-14 represented a probably mildly depressed patient, and a PHQ-9 score ≥ 15 represented a probable moderately-to-severely depressed patient
Statistically significant difference between depression screen-negative, screen positive for mild MDD, and screen positive for moderate-to severe MDD groups at p = 0.05 level or below
Sample size too small (n ≤ 5) to report sub-categories
Healthcare utilization in the study population also increased linearly along with the severity of depressive symptoms (Table 2). In the 12 months after the screening was conducted, screen-negative adolescents had the lowest levels of outpatient utilization (3.5 visits), followed by adolescents with probable mild MDD (6.5 visits) and adolescents with probable moderate-to-severe MDD (12.0 visits) (p < 0.01). The pattern was similar for mental health visits, with screen-negative, probable mild MDD, and probable moderate-to-severe MDD adolescents having 0.7, 2.5, and 6.4 mental health visits, respectively (p < 0.01). Screen-positive adolescents were significantly more likely than screen-negative adolescents to receive hospital care; the probability of any ED utilization was 11.5%, 21.0% and 29.5% for screen-negative, probable mild MDD, and probable moderate-to-severe MDD adolescents, respectively. The probability of having any inpatient hospitalization was a respective 1.2%, 3.8%, and 8.4% among screen-negative, probable mild MDD, and probable moderate-to-severe MDD adolescents. To reduce the risk of individual identification, results are not reported for cell sizes smaller than 5 youth, including inpatient mental health and non-mental health care utilization.
Table 2.
Healthcare utilization, 12 months post-screening, by severity of depressive symptoms
| Type of utilizationa | Screen Negativeb n= 3,707 | Screen Positiveb | p | ||
|---|---|---|---|---|---|
| Mild MDD n= 186 | Moderate-to-Severe MDD n= 95 | All MDD n= 281 | |||
| Outpatient Visits, mean (SD) | 3.5 (5.1) | 6.5 (8.2) | 12.0 (15.5) | 8.3 (11.5) | < 0.01c |
| Outpatient Mental Health Visits, mean (SD) | 0.7 (3.5) | 2.5 (6.1) | 6.4 (13.3) | 3.8 (9.3) | < 0.01c |
| Any Inpatient Care Utilization | 1.2% | 3.8% | 8.4% | 5.3% | < 0.01c |
| Any Inpatient Mental Health Utilization | 0.2% | --d | --d | 3.2% | -- |
| Any Inpatient Medical Utilization | 1.1% | --d | --d | 3.2% | -- |
| Any Emergency Department Utilization | 11.5% | 21.0% | 29.5% | 23.8% | < 0.01c |
All results are expressed as percentages unless otherwise indicated
Probable depression severity was categorized by PHQ-2 and PHQ-9 screening results. A PHQ-2 score < 2 OR a PHQ-2 score ≥ 3 and a PHQ-9 score < 10 represented a probably non-depressed patient, a PHQ-9 score of 10-14 represented a probably mildly depressed patient, and a PHQ-9 score ≥ 15 represented a probable moderately-to-severely depressed patient
Statistically significant difference between depression screen-negative, screen positive for mild MDD, and screen positive for moderate-to severe MDD groups at p = 0.05 level or below
Sample size too small (n ≤ 5) to report sub-categories
Higher utilization among screen-positive adolescents translated into higher expenditures. From the payer's perspective, mean total healthcare expenditures for screen-positive (either probable mild MDD or moderate-to-severe MDD) adolescents ($5,083) were more than twice as high as those for other adolescents ($2,357). Higher expenditures were primarily driven by outpatient expenditures ($4,004 vs. $2,203), followed by inpatient ($1,079 vs. $334), ED ($634 vs. $145), pharmacy ($521 vs. $280) and diagnostic test-related expenditures ($195 vs. $108) (p < 0.01 for all comparisons). Consistent with the differences in utilization, adolescents with moderate-to-severe probable MDD had higher expenditures than those with mild probable MDD in all categories of expenditures. Total annual expenditures for mild and moderate-to-severe probable MDD adolescents were $3,505 and $8,173, respectively—49% and 247% higher than total expenditures for screen-negative adolescents. (Table 3)
Table 3.
Mean unadjusted healthcare expenditures (with standard deviations), 12 months post-screening by severity of depressive symptoms
| Type of expendituresa | Screen Negativeb ($) n =3,707 | Screen Positiveb ($) | p | ||
|---|---|---|---|---|---|
| Mild Depression n= 186 | Moderate-to-Severe Depression n= 95 | All n= 281 | |||
| Outpatient | 2,203 (4,531) | 2,951 (4,152) | 6,067 (7,771) | 4,004 (5,818) | < 0.01c |
| Inpatient | 334 (4,500) | 554 (3,592) | 2,105 (9,701) | 1,079 (6,376) | < 0.01c |
| Inpatient Mental Health Care | 24 (730) | --d | --d | 416 (2973) | < 0.01c |
| Inpatient Medical Care | 310 (4427) | --d | --d | 663 (4917) | < 0.01c |
| Emergency Department | 145 (801) | 411 (2,182) | 1,129 (3,789) | 634 (2,843) | < 0.01c |
| Pharmacy | 280 (1,236) | 453 (881) | 654 (1,231) | 521 (1,015) | < 0.01c |
| Diagnostic tests (laboratory and radiology) | 108 (476) | 163 (229) | 257 (437) | 195 (317) | < 0.01c |
| Total costs | 2,357 (7,621) | 3,505 (6819) | 8,173 (14,887) | 5,083 (10,489) | < 0.01c |
All results are expressed as mean (SD) in 2013 US dollars
Probable depression severity was categorized by PHQ-2 and PHQ-9 screening results. A PHQ-2 score < 2 OR a PHQ-2 score ≥ 3 and a PHQ-9 score < 10 represented a probably non-depressed patient, a PHQ-9 score of 10-14 represented a probably mildly depressed patient, and a PHQ-9 score ≥ 15 represented a probable moderately-to-severely depressed patient
Statistically significant difference between depression screen-negative, screen positive for mild MDD, and screen positive for moderate-to severe MDD groups at p = 0.05 level or below
Sensitivity analyses that excluded ROAD intervention youth from the analysis indicated that non-intervention youth (n = 3960) had slightly, but not significantly higher expenditures than intervention youth (n=50). (Appendix Tables 1 and 2)
DISCUSSION
We examined healthcare utilization and associated expenditures among a population of adolescents enrolled in an integrated healthcare system that were screened for depression. We found that adolescents who screened positive for depression had significantly higher utilization and expenditures than adolescents who screened negative for depression in each component of medical utilization including outpatient medical, outpatient mental health, emergency visits, pharmacy, diagnostic testing, and inpatient admissions from the perspective of the payer. Only a small percentage of the increase in utilization was specifically due to mental health care and prescription drug use. Screening positive for depression was associated with a 49% increase in expenditures for those with mild probable MDD and a 247% increase in expenditures for those with moderate-to-severe probable MDD.
We also found that mental health visits comprised less than half of all outpatient visits for screen-positive patients (Table 2). Similar findings have been observed among adult populations, in which fewer than 10% of outpatient expenditures were specifically for the treatment of depression.27 It is possible that some of the encounters in primary care included discussion of mental health and resulted in antidepressant prescriptions. While we could capture pharmacy charges, we are not able to ascertain primary care-based mental health counseling from current data. Adolescents who screened positive for depression had a higher Pediatric Chronic Disease Score even when antidepressant prescriptions were excluded from the pharmacy-based risk calculation algorithm. This may reflect the high rates of co-occurrence between depressive symptoms and chronic illness, which has been associated with increased healthcare utilization and medical costs in depressed adult and adolescent populations. 16,27,28 Most of the increase in costs in both adolescent and adult populations with depression and chronic diseases are due to higher utilization for somatic symptoms such as headache and fatigue. 16,27 Many studies have shown that comorbid depression also maladaptively affects self-care of chronic medical conditions (i.e. decreasing adherence to medication or cessation of smoking), which may also increase medical costs. 29,16,28 Several large randomized trials have shown that collaborative care interventions that improved depressive outcomes in adult patients with comorbid depression and medical illness were associated with total medical costs savings compared to patients treated in usual primary care. 27,30,31 The Reaching Out to Adolescents in Distress intervention demonstrated that implementing a collaborative care program to treat depression in primary care settings is feasible and could result in significant improvements in depressive symptoms. 21
One strength of this study relative to the existing literature 14,16 is that we used the PHQ-9, as opposed to coded diagnoses of depression to identify adolescents with depressive symptoms, making this study a more comprehensive analysis of expenditures for patients who exhibit symptoms of depression, whether they have been diagnosed or not. Only 20% to 50% of adolescents with depression are accurately diagnosed by primary care physicians32,33, therefore dependence on ICD-9 codes is likely to have missed up to half of depression cases. Also, pediatric coding practices vary widely by provider and many pediatricians are reluctant to use mental health codes for their patients17, decreasing the reliability of analyses that use coded diagnoses to classify depressed patients. While use of ICD-9 coding would allow us to examine mental health-specific utilization in ED (e.g. suicidal ideation), relying on diagnostic codes for this purpose risks a significant under-representation of the actual reason for health care use among children.34 Moreover, compared to other studies of healthcare utilization among adolescents with MDD4,8-11, we assessed utilization and expenditures from administrative data as opposed to patient self-report, and analyses assessed all healthcare utilization, not just mental health disorder-specific utilization.
Given the association between positive screens for depression and increased utilization of a wide range of healthcare services, screening adolescents for depressive symptoms in the primary care setting using an easily administered instrument like the PHQ-9 may be a viable strategy for providers to identify patients who could benefit from evidence-based team approaches like ROAD or the Youth Partners-in-Care programs. 21,35 However, providers may need additional training in order to increase screening in practice.36 Collaborative depression care programs have been shown to improve the quality of mental health care and health outcomes of patients with depression37,38, including patients with comorbid medical conditions.39 In the ROAD collaborative care intervention, adolescents in the intervention arm had a 5.2 higher odds of remission of depressive symptoms compared to adolescents receiving usual care.21 Future research should examine the impact of such collaborative care programs on healthcare utilization and expenditures.
Limitations
This analysis was subject to limitations. These data are from a single healthcare system. We were unable to assess the degree of non-response bias among those who refused to participate in the screening study. Additionally, there were significant differences between screen-positive and screen-negative populations in other baseline characteristics including weight status, gender, and chronic disease score that may have driven some of the differences in utilization and expenditure estimates. Moreover, adolescents that screened positive for depression were more likely to have public health insurance, and presumably also lower socieoeconomic status, compared to those that screened negative for depression. However, healthcare utilization by children with continuous public insurance coverage is comparable to utilization by children with continuous private coverage.40 Due to limitations of consent obtained, this is a purely descriptive study of group data; we were unable to conduct individual-level analyses that would allow us to control for differences between groups that might be contributing to cost differences. Future analyses should analyze utilization and expenditures, controlling for factors that may influence service use in pediatric populations.41
We calculated the PCDS for the 12 months prior to PHQ-2 screening. Our enrollment criteria did not specify that adolescents had to be enrolled for the entire 12 month period before screening, and so our PCDS estimates may be conservative. 26 Additionally, the PCDS cannot provide information about whether health conditions are chronic or acute, however the PCDS has shown to be comparable to the ICD-9-based Ambulatory Care Groups in predicting one-year health utilization and health care costs. 26
This study cannot make determinations about the causality of the relationship between medical problems and the incidence of depressive symptoms, which can have complex bidirectional associations. Furthermore, we have limited information about co-occuring anxiety, substance abuse, poverty, and other factor that could affect a child's mental health. Future work should use more extensive questionnaires to explore these mechanisms further.
Finally, the analysis was conducted from the healthcare payer perspective. Any family-incurred expenditures related to transportation, medical supplies, or out-of-network care not approved by GHC were not captured in expenditure estimates. Moreover, any indirect costs related to parents’ missed workdays or lost leisure time were not captured. Additionally, the exclusion of ROAD intervention-related costs may bias non-therapy-related cost differences toward the null. Therefore, the economic analysis may be somewhat conservative.
CONCLUSIONS
Depressive symptoms among adolescents are associated with increased healthcare utilization and expenditures, even among patients who only exhibit mild depressive symptoms. Only a small percentage of the increased healthcare utilization among adolescents who screened positive for depression are attributable to increased mental health and prescription drug utilization. As in adult populations, adolescent depressive symptoms were found to be associated with marked increases in all components of medical utilization and costs. Screening adolescents for depressive symptoms in primary care settings and intervening to provide evidence-based health services interventions may help to decrease healthcare expenditures. Future studies are needed to better understand whether improving adolescent depression care could decrease non-mental health-related utilization.
What's new on this subject: This study estimates the impact of positive adolescent depression screens, not just coded diagnoses of depression, on healthcare utilization and payer-incurred expenditures. These data inform the development of strategies to improve care for youth with depressive symptoms while minimizing costs.
Acknowledgments
Funding Sources: This study was funded by the NIH National Institute of Mental Health (R01 MH085645-01A1). The sponsor of this study had no role in the study design, in the collection, analysis, and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Abbreviations
- GH
Group Health
- MDD
Major depressive disorder
- PHQ
Patient Health Questionnaire
- PCDS
Pediatric Chronic Disease Score
- ROAD
Reaching Out to Adolescents in Distress
Appendix
Table A1.
Healthcare utilization for non-intervention adolescents (n = 3960), 12 months post-screening, by severity of depressive symptoms
| Type of utilizationa | Screen Negativeb n= 3,707 | Screen Positiveb | p | ||
|---|---|---|---|---|---|
| Mild MDD n= 162 | Moderate-to-Severe MDD n= 69 | All MDD n= 231 | |||
| Outpatient Visits, mean (SD) | 3.5 (5.1) | 6.5 (8.6) | 13.3 (17.7) | 8.0 (15.2) | < 0.01c |
| Outpatient Mental Health Visits, mean (SD) | 0.7 (3.5) | 2.6 (6.5) | 8.0 (15.2) | 3.8 (9.3) | < 0.01c |
| Any Inpatient Care Utilization | 1.2% | 3.7% | 10.1% | 5.6% | < 0.01c |
| Any Inpatient Mental Health Utilization | 0.2% | --d | --d | 3.5% | -- |
| Any Inpatient Medical Utilization | 1.1% | --d | --d | 3.5% | -- |
| Any Emergency Department Utilization | 11.5% | 21.0% | 29.5% | 19.8% | < 0.01c |
| Any Antidepressant Prescription | 5.0% | 19.8% | 34.8% | 24.2% | < 0.01c |
All results are expressed as percentages unless otherwise indicated
Probable depression severity was categorized by PHQ-2 and PHQ-9 screening results. A PHQ-2 score < 2 OR a PHQ-2 score ≥ 3 and a PHQ-9 score < 10 represented a probably non-depressed patient, a PHQ-9 score of 10-14 represented a probably mildly depressed patient, and a PHQ-9 score ≥ 15 represented a probable moderately-to-severely depressed patient
Statistically significant difference between depression screen-negative, screen positive for mild MDD, and screen positive for moderate-to severe MDD groups at p = 0.05 level or below
Sample size too small (n ≤ 5) to report sub-categories
Table A2.
Mean unadjusted healthcare expenditures (with standard deviations) non-intervention adolescents (n = 3960), 12 months post-screening by severity of depressive symptoms
| Type of expendituresa | Screen Negativeb ($) n =3,707 | Screen Positiveb ($) | p | ||
|---|---|---|---|---|---|
| Mild Depression n= 162 | Moderate-to-Severe Depression n= 69 | All n= 231 | |||
| Outpatient | 2,203 (4,531) | 2778 (3703) | 6760 (8714) | 3968 (5949) | < 0.01c |
| Inpatient | 334 (4,500) | 545 (3679) | 2772 (11285) | 1210 (6940) | < 0.01c |
| Inpatient Mental Health Care | 24 (730) | 438 (3409) | 536 (2781) | 468 (3228) | < 0.01c |
| Inpatient Medical Care | 310 (4427) | 107 (1317) | 2235 (9433) | 743 (5336) | < 0.01c |
| Emergency Department | 145 (801) | 273 (888) | 1483 (4390) | 634 (2561) | < 0.01c |
| Pharmacy | 280 (1,236) | 430 (870) | 765 (1405) | 530 (1067) | < 0.01c |
| Diagnostic tests (laboratory and radiology) | 108 (476) | 169 (238) | 287 (496) | 204 (449) | < 0.01c |
| Total costs | 2,357 (7,621) | 3323 (6786) | 9532 (17076) | 5178 (11250) | < 0.01c |
All results are expressed as mean (SD) in 2013 US dollars
Probable depression severity was categorized by PHQ-2 and PHQ-9 screening results. A PHQ-2 score < 2 OR a PHQ-2 score ≥ 3 and a PHQ-9 score < 10 represented a probably non-depressed patient, a PHQ-9 score of 10-14 represented a probably mildly depressed patient, and a PHQ-9 score ≥ 15 represented a probable moderately-to-severely depressed patient
Statistically significant difference between depression screen-negative, screen positive for mild MDD, and screen positive for moderate-to severe MDD groups at p = 0.05 level or below
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: The authors have no conflicts of interest to report.
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Clinical Trial Registration: NCT01140464
CONTRIBUTOR'S STATEMENTS:
Davene R. Wright: Dr. Wright contributed to the study design, analyzed and interpreted the data, and drafted the initial manuscript.
Wayne J. Katon ,Evette Ludman and Elizabeth McCauley: Drs. Katon, Ludman and McCauley contributed to the study design and critically revised and reviewed the manuscript.
Malia Oliver: Ms. Oliver conducted the data analysis for the study and critically reviewed and revised the manuscript.
Jeffrey Lindenbaum: Dr. Lindenbaum contributed to the study design and critically reviewed and revised the manuscript.
Laura P. Richardson: Dr. Richardson conceptualized and designed the study, obtained funding, and critically reviewed and revised the manuscript.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
- 1.Centers for Disease Control and Prevention [February 19, 2014];Youth Risk Behavior Survey. 2011 www.cdc.gov/yrbs.
- 2.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weissman MM, Wolk S, Goldstein RB, et al. Depressed adolescents grown up. JAMA. 1999;281(18):1707–1713. doi: 10.1001/jama.281.18.1707. [DOI] [PubMed] [Google Scholar]
- 4.Lewinsohn PM, Rohde P, Seeley JR. Treatment of adolescent depression: frequency of services and impact on functioning in young adulthood. Depress Anxiety. 1998;7(1):47–52. doi: 10.1002/(sici)1520-6394(1998)7:1<47::aid-da6>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 5.Knapp M, McCrone P, Fombonne E, Beecham J, Wostear G. The Maudsley long-term follow-up of child and adolescent depression: 3. Impact of comorbid conduct disorder on service use and costs in adulthood. Br J Psychiatry. 2002;180:19–23. doi: 10.1192/bjp.180.1.19. [DOI] [PubMed] [Google Scholar]
- 6.2014 recommendations for pediatric preventive health care. Pediatrics. 2014;133(3):568–570. doi: 10.1542/peds.2013-4096. [DOI] [PubMed] [Google Scholar]
- 7.Asarnow JR, Jaycox LH, Duan N, et al. Depression and role impairment among adolescents in primary care clinics. J Adolesc Health. 2005;37(6):477–483. doi: 10.1016/j.jadohealth.2004.11.123. [DOI] [PubMed] [Google Scholar]
- 8.Merikangas KR, He JP, Burstein M, et al. Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2011;50(1):32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goodman SH, Lahey BB, Fielding B, Dulcan M, Narrow W, Regier D. Representativeness of clinical samples of youths with mental disorders: a preliminary population-based study. J Abnorm Psychol. 1997;106(1):3–14. doi: 10.1037//0021-843x.106.1.3. [DOI] [PubMed] [Google Scholar]
- 10.Essau CA. Frequency and patterns of mental health services utilization among adolescents with anxiety and depressive disorders. Depress Anxiety. 2005;22(3):130–137. doi: 10.1002/da.20115. [DOI] [PubMed] [Google Scholar]
- 11.Wu P, Hoven CW, Bird HR, et al. Depressive and disruptive disorders and mental health service utilization in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1999;38(9):1081–1090. doi: 10.1097/00004583-199909000-00010. discussion 1090-1082. [DOI] [PubMed] [Google Scholar]
- 12.Mihalopoulos C, Vos T, Pirkis J, Carter R. The population cost-effectiveness of interventions designed to prevent childhood depression. Pediatrics. 2012;129(3):e723–730. doi: 10.1542/peds.2011-1823. [DOI] [PubMed] [Google Scholar]
- 13.Lynch FL, Hornbrook M, Clarke GN, et al. Cost-effectiveness of an intervention to prevent depression in at-risk teens. Arch Gen Psychiatry. 2005;62(11):1241–1248. doi: 10.1001/archpsyc.62.11.1241. [DOI] [PubMed] [Google Scholar]
- 14.Guevara JP, Mandell DS, Rostain AL, Zhao H, Hadley TR. National estimates of health services expenditures for children with behavioral disorders: an analysis of the medical expenditure panel survey. Pediatrics. 2003;112(6 Pt 1):e440. doi: 10.1542/peds.112.6.e440. [DOI] [PubMed] [Google Scholar]
- 15.Bureau of Labor Statistics [February 19, 2014];Consumer Price Index. 2013 http://data.bls.gov/timeseries/CUUR0000SAM.
- 16.Richardson LP, Russo JE, Lozano P, McCauley E, Katon W. The effect of comorbid anxiety and depressive disorders on health care utilization and costs among adolescents with asthma. Gen Hosp Psychiatry. 2008;30(5):398–406. doi: 10.1016/j.genhosppsych.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rushton JL, Felt BT, Roberts MW. Coding of pediatric behavioral and mental disorders. Pediatrics. 2002;110(1 Pt 1):e8. doi: 10.1542/peds.110.1.e8. [DOI] [PubMed] [Google Scholar]
- 18.Asarnow JR, Jaycox LH, Anderson M. Depression among youth in primary care models for delivering mental health services. Child Adolesc Psychiatr Clin N Am. 2002;11(3):477–497, viii. doi: 10.1016/s1056-4993(02)00006-8. [DOI] [PubMed] [Google Scholar]
- 19.Zuckerbrot RA, Cheung AH, Jensen PS, Stein RE, Laraque D. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): I. Identification, assessment, and initial management. Pediatrics. 2007;120(5):e1299–1312. doi: 10.1542/peds.2007-1144. [DOI] [PubMed] [Google Scholar]
- 20.Cheung AH, Zuckerbrot RA, Jensen PS, Ghalib K, Laraque D, Stein RE. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): II. Treatment and ongoing management. Pediatrics. 2007;120(5):e1313–1326. doi: 10.1542/peds.2006-1395. [DOI] [PubMed] [Google Scholar]
- 21.Richardson LP, Ludman E, McCauley E, et al. Improving outcomes for adolescents with depression in primary care: a randomized controlled trial. JAMA. 2014;312(8):809–816. doi: 10.1001/jama.2014.9259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 23.Richardson LP, Rockhill C, Russo JE, et al. Evaluation of the PHQ-2 as a brief screen for detecting major depression among adolescents. Pediatrics. 2010;125(5):e1097–1103. doi: 10.1542/peds.2009-2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richardson LP, McCauley E, Grossman DC, et al. Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics. 2010;126(6):1117–1123. doi: 10.1542/peds.2010-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pinto-Meza A, Serrano-Blanco A, Penarrubia MT, Blanco E, Haro JM. Assessing depression in primary care with the PHQ-9: can it be carried out over the telephone? J Gen Intern Med. 2005;20(8):738–742. doi: 10.1111/j.1525-1497.2005.0144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fishman PA, Shay DK. Development and estimation of a pediatric chronic disease score using automated pharmacy data. Med Care. 1999;37(9):874–883. doi: 10.1097/00005650-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Katon WJ, Lin E, Russo J, Unutzer J. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003;60(9):897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]
- 28.Garrison MM, Katon WJ, Richardson LP. The impact of psychiatric comorbidities on readmissions for diabetes in youth. Diabetes Care. 2005;28(9):2150–2154. doi: 10.2337/diacare.28.9.2150. [DOI] [PubMed] [Google Scholar]
- 29.Katon W. The impact of major depression on chronic medical illness. Gen Hosp Psychiatry. 1996;18(4):215–219. doi: 10.1016/0163-8343(96)00065-5. [DOI] [PubMed] [Google Scholar]
- 30.Sullivan M, Simon G, Spertus J, Russo J. Depression-related costs in heart failure care. Arch Intern Med. 2002;162(16):1860–1866. doi: 10.1001/archinte.162.16.1860. [DOI] [PubMed] [Google Scholar]
- 31.Simon GE, Katon WJ, Lin EH, et al. Diabetes complications and depression as predictors of health service costs. Gen Hosp Psychiatry. 2005;27(5):344–351. doi: 10.1016/j.genhosppsych.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 32.Richardson LP, Russo JE, Lozano P, McCauley E, Katon W. Factors associated with detection and receipt of treatment for youth with depression and anxiety disorders. Acad Pediatr. 2010;10(1):36–40. doi: 10.1016/j.acap.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Katon WJ, Richardson L, Russo J, Lozano P, McCauley E. Quality of mental health care for youth with asthma and comorbid anxiety and depression. Med Care. 2006;44(12):1064–1072. doi: 10.1097/01.mlr.0000237421.17555.8f. [DOI] [PubMed] [Google Scholar]
- 34.Lozano P, Fishman P, VonKorff M, Hecht J. Health care utilization and cost among children with asthma who were enrolled in a health maintenance organization. Pediatrics. 1997;99(6):757–764. doi: 10.1542/peds.99.6.757. [DOI] [PubMed] [Google Scholar]
- 35.Asarnow JR, Jaycox LH, Duan N, et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: a randomized controlled trial. JAMA. 2005;293(3):311–319. doi: 10.1001/jama.293.3.311. [DOI] [PubMed] [Google Scholar]
- 36.Fallucco EM, Seago RD, Cuffe SP, Kraemer DF, Wysocki T. Primary Care Provider Training in Screening, Assessment, and Treatment of Adolescent Depression. Acad Pediatr. 2015;15:326–332. doi: 10.1016/j.acap.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 37.Weingarten SR, Henning JM, Badamgarav E, et al. Interventions used in disease management programmes for patients with chronic illness-which ones work? Meta-analysis of published reports. BMJ. 2002;325(7370):925. doi: 10.1136/bmj.325.7370.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Butler M, Kane RL, McAlpine D, et al. Does integrated care improve treatment for depression? A systematic review. J Ambul Care Manage. 2011;34(2):113–125. doi: 10.1097/JAC.0b013e31820ef605. [DOI] [PubMed] [Google Scholar]
- 39.Simon GE, Katon WJ, Lin EH, et al. Cost-effectiveness of systematic depression treatment among people with diabetes mellitus. Arch Gen Psychiatry. 2007;64(1):65–72. doi: 10.1001/archpsyc.64.1.65. [DOI] [PubMed] [Google Scholar]
- 40.Duderstadt KG, Hughes DC, Soobader MJ, Newacheck PW. The impact of public insurance expansions on children's access and use of care. Pediatrics. 2006;118(4):1676–1682. doi: 10.1542/peds.2006-0004. [DOI] [PubMed] [Google Scholar]
- 41.Rhodes KV, Kenney GM, Friedman AB, et al. Primary Care Access for New Patients on the Eve of Health Care Reform. JAMA Intern Med. 2014 doi: 10.1001/jamainternmed.2014.20. [DOI] [PubMed] [Google Scholar]