Abstract
Background
Post-traumatic stress disorder (PTSD) has been linked with migraine in prior studies.
Objective
To evaluate the individual and joint burdens of migraine and PTSD in a population-based cohort.
Methods
The National Comorbidity Survey-Replication (NCS-R) is a general population study conducted in the United States from February 2001–April 2003. PTSD and migraine were assessed, and four groups defined based on their migraine and PTSD status. The four groups included those with no migraine and no PTSD (controls, n=4535), those with migraine and without PTSD (migraine alone, n=236), those with PTSD and without migraine (PTSD alone, n=244), and those with both migraine and PTSD (mig+PTSD, n=68). Logistic and Poisson regression models were used to assess the association between dichotomous/multilevel outcome variables indicating financial, health, and interpersonal burdens and each migraine/PTSD group.
Results
Compared to controls, those with Mig+PTSD were more likely to be in the low poverty index (48% vs 41%, AOR 2.16; CI: 1.10, 4.24) and were less likely to be working for pay or profit in the past week (50% vs 68%, AOR 0.42; CI: 0.24, 0.74) but not those with migraine or PTSD alone. Additionally, the number of days where work quality was cut due to physical or mental health or substance abuse in the past month was greater in all groups compared to controls: (1) migraine alone: mean 2.57 (SEM 0.32) vs mean 1.09 (SEM 0.08) days, ARR=2.39; CI: 2.19, 2.62; (2) PTSD alone: mean 2.43 (SEM 0.33) vs mean 1.09 (SEM 0.08) days, ARR=2.09; CI: 1.91, 2.29; (3) mig+PTSD: mean 8.2 (SEM 0.79) vs 1.09 (SEM 0.08) days, ARR 6.79; CI 6.16, 7.49; and was over 2.5-fold greater in those mig+PTSD than migraine alone (mean 8.0 [SEM 0.79] vs 2.6 days [SEM 0.72], ARR 2.77; CI: 2.45, 3.14). The likelihood of having difficulty getting along or maintaining a social life was also increased in all groups relative to controls: (1) migraine alone: 21% vs 5.4%, AOR 4.20; CI: 2.62, 6.74; (2) PTSD alone: 18% vs 5.4%, AOR 3.40; CI: 2.40, 4.82; (3) Mig+PTSD: 39% vs 5.4%, AOR 9.95; CI: 5.72, 17.32, and was 2-fold greater in those with Mig+PTSD as compared to those with migraine alone (AOR 2.32; CI: 1.15, 4.69).
Conclusions
These findings support the need for those who treat migraine patients to be aware of the comorbidity with PTSD, as these patients may be particularly prone to adverse financial, health, and interpersonal disease burdens.
Keywords: migraine, post-traumatic stress disorder, disability, economic burden, societal burden
Introduction
Although mood disorders such as depression and anxiety have long been described as comorbid with migraine, it is only over the past decade that the association between post-traumatic stress disorder (PTSD) and migraine has become well-recognized.1-3 In general population studies, 22-26% of those with migraine fulfilled PTSD criteria, as compared to only 5% of those without headache and 14% of those with nonmigraine headache or no headache.4,5 Not surprisingly, in special populations with headache disorders (eg, pain clinic patients, veterans, and medical students) PTSD prevalence rates have been estimated at higher rates, approximately 22-59%.6-10
Migraine by itself is a common and often disabling disorder.11,12 In addition to the personal burden, a significant societal burden exists, with the annual direct medical care of those with migraine estimated at about one billion dollars, and the cost to American employers due to missed days or impaired work function due to migraine estimated at approximately $13 billion a year.13 Previous research supports that comorbid psychiatric disorders increase the disability and burden associated with migraine.14-16 However, although some research supports that the presence of PTSD in those with migraine is associated with greater headache-related disability,4,7 no study has conducted a detailed, focused analysis of the personal and societal disease burden comorbid PTSD entails for those with migraine. This study investigates the impact of PTSD on the disease burden of migraine. We hypothesized that individuals with both migraine and PTSD would have greater financial, health-related, and interpersonal disease burdens as compared to those without headache and PTSD and those with migraine alone.
Methods
The National Comorbidity Survey-Replication (NCS-R) is a nationally representative face-to-face survey of adults 18 years of age and older in the United States, which was conducted between February 2001 and April 2003. The NCS-R interviews were conducted in two parts as previously described.4,17 In brief, all participants were administered a core diagnostic interview including mood and trauma and stressor-related disorders in Part I. Part II was administered to all part I participants with lifetime disorders in part I plus a probability subsample of other participants and assessed risk factors, service use, correlates, and other disorders including migraine. The overall response rate for the NCS-R data collection was 70.9%. The Human Subjects Committees of Harvard Medical School and the University of Michigan approved recruitment, consent, and field procedures.4,17
Sample
Given the complex sampling design of NCS-R, the sample was weighted to adjust for survey procedures, differential probability of selection, differential sampling into Part II and residual discrepancies between sample and census population sociodemographic and geographic distributions as previously described in detail.18,19
Demographics
Sociodemographic characteristics including age, sex, race, martial status, education, median income, and smoking history were evaluated as previously described.18
DSM-IV Disorders
DSM-IV disorders were assessed with the World Health Organization's Composite International Diagnostic Interview (CIDI). The CIDI is a structured, lay-administered interview that generates International Classification of Diseases, 10th Revision (ICD-10) and DSM-IV diagnoses. Twelve-month DSM-IV disorders considered herein include major depressive disorder (MDD), PTSD, and substance abuse.4,17
Migraine
All participants were asked whether they ever experienced “frequent or severe headaches.” Those responding affirmatively were asked more detailed questions including headache duration, location, severity, quality, and presence of nausea, photophobia or phonophobia. Aggravation of pain by activity was not assessed. Current migraine (within 12 months) was then classified based on the International Classification of Headache Disorders, second edition (ICHD-II) as previously described.4,20 Participants with remote (ie, most recent attack more than 12 months before the interview) and probable migraine were excluded.
Group Characterization
Based on their migraine and PTSD classification, participants were characterized into one of four groups. Group A included those without either migraine or PTSD (controls). Group B included those fulfilling PTSD but not migraine criteria (PTSD alone). Group C included those fulfilling migraine but not PTSD criteria (migraine alone). Group D include those fulfilling criteria for both migraine and PTSD, (mig+PTSD).
Disease Burden
All part II participants were asked a series of questions pertaining to financial, health, and interpersonal disease burden. Tables 2 and 3 include brief descriptors of each variable.
Table 2. Unadjusted, Prevalence of Financial, Health-Related, and Personal Disease Burden Indicators by Migraine and PTSD.
| (A) – Migraine– PTSD (N=.4535) | (B) – Migraine + PTSD (n=244) | (C) + Migraine – PTSD (n=236) | (D) + Migraine + PTSD (n=68) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||||
| Disease Burden Indicator | n | % | n | % | P value (B vs A) | n | % | P value (C vs A) | n | % | P value (D vs A) | P value (D vs C) | |
| FINANCIAL | |||||||||||||
| Have enough money to meet needs. | Just enough | 2492 | 56.4 | 118 | 49.4 | .03 | 125 | 53.6 | .006 | 32 | 48.5 | .05 | .62 |
| Not enough | 1092 | 24.7 | 88 | 36.7 | .0002 | 82 | 35.2 | .0002 | 31 | 45.7 | .0002 | .21 | |
| More than enough [ref] | 835 | 18.9 | 33 | 13.9 | 26 | 11.2 | 4 | 5.8 | |||||
| 4419 | 239 | 233 | 67 | ||||||||||
| Poverty Index | Low | 1847 | 40.7 | 110 | 45.0 | .002 | 114 | 48.4 | .004 | 33 | 48.4 | .02 | .55 |
| Middle | 1374 | 30.3 | 78 | 32.1 | .08 | 67 | 28.4 | .38 | 25 | 36.3 | .19 | .47 | |
| High [ref] | 1314 | 29.0 | 56 | 22.9 | 55 | 23.2 | 10 | 15.3 | |||||
| 4535 | 100% | 244 | 100% | 236 | 100% | 68 | 100% | ||||||
| Received welfare/public assistance since 18 yo | Yes | 529 | 12.8 | 66 | 30.0 | .0002 | 60 | 27.7 | .0002 | 21 | 36.0 | .0002 | .11 |
| No [ref] | 3598 | 87.2 | 154 | 70.0 | 156 | 72.3 | 37 | 64.0 | |||||
| 4127 | 100% | 219 | 100% | 216 | 100% | 58 | 100% | ||||||
| Worked for pay or profit in the last week | Yes | 2898 | 67.7 | 167 | 69.8 | .61 | 150 | 67.3 | .52 | 32 | 49.8 | .0002 | .002 |
| No [ref] | 1383 | 32.3 | 72 | 30.2 | 73 | 32.7 | 32 | 50.2 | |||||
| 4281 | 100% | 239 | 100% | 223 | 100% | 64 | 100% | ||||||
| Health insurance, covered by employer or union | Yes | 2808 | 62.0 | 143 | 58.5 | .01 | 148 | 62.8 | .73 | 37 | 54.3 | .08 | .19 |
| No [ref] | 1720 | 38.0 | 101 | 41.5 | 88 | 37.2 | 31 | 45.7 | |||||
| 4528 | 100% | 244 | 100% | 236 | 100% | 68 | 100% | ||||||
| Health insurance, covered by insurance company | Yes | 700 | 15.5 | 22 | 9.0 | .008 | 24 | 10.4 | .03 | 6 | 9.1 | .19 | .90 |
| No [ref] | 3810 | 84.5 | 220 | 91.0 | 211 | 89.6 | 62 | 90.9 | |||||
| 4510 | 100% | 242 | 100% | 235 | 100% | 68 | 100% | ||||||
| HEALTH-RELATED | |||||||||||||
| Overall mental health status in past 30 days | Better | 471 | 10.4 | 51 | 20.9 | .0002 | 31 | 13.2 | .77 | 10 | 15.2 | .16 | .30 |
| Worse | 166 | 3.7 | 23 | 9.5 | .0002 | 25 | 10.4 | .0002 | 11 | 16.2 | .0002 | .12 | |
| About the same [ref] | 3895 | 85.9 | 170 | 69.6 | 180 | 76.4 | 46 | 68.6 | |||||
| 4532 | 100% | 244 | 100% | 236 | 100% | 68 | 100% | ||||||
| Difficulty with concentration/memory/thinking in last month due to health problems | Yes | 354 | 7.9 | 77 | 31.4 | .0002 | 67 | 28.7 | .0002 | 30 | 45.0 | .0002 | .0002 |
| No [ref] | 4147 | 92.1 | 168 | 68.6 | 166 | 71.3 | 37 | 55.0 | |||||
| 4501 | 100% | 244 | 100% | 233 | 100% | 68 | 100% | ||||||
| Overall physical health during past 30 days | Better | 566 | 12.5 | 38 | 15.6 | .22 | 22 | 9.1 | .34 | 11 | 15.9 | .32 | .16 |
| Worse | 384 | 8.5 | 33 | 13.7 | .002 | 38 | 16.2 | .002 | 14 | 20.5 | .002 | .35 | |
| About the same [ref] | 3582 | 79.0 | 173 | 70.7 | 176 | 74.7 | 43 | 63.6 | |||||
| 4532 | 100% | 244 | 100% | 236 | 100% | 68 | 100% | ||||||
| Frequency physical discomfort in past 30 days | All of the time | 140 | 3.1 | 20 | 8.3 | .0002 | 17 | 7.2 | .0002 | 10 | 15.4 | .0002 | .02 |
| Most of the time | 178 | 3.9 | 16 | 6.6 | .0002 | 22 | 9.4 | .0002 | 15 | 22.3 | .0002 | .02 | |
| Some of the time | 516 | 11.4 | 53 | 21.6 | .0002 | 64 | 27.2 | .0002 | 19 | 27.4 | .0002 | .18 | |
| A little of the time | 1158 | 25.5 | 73 | 29.9 | .0002 | 80 | 33.9 | .0002 | 17 | 25.1 | .0002 | .89 | |
| None of the time [ref] | 2541 | 56.1 | 82 | 33.6 | 53 | 22.3 | 7 | 9.8 | |||||
| 4533 | 100% | 244 | 100% | 236 | 100% | 68 | 100% | ||||||
| Taken antidepressants in the last 12 months | Yes | 331 | 7.3 | 62 | 25.2 | .0002 | 56 | 23.6 | .0002 | 28 | 41.1 | .0002 | .002 |
| No [ref] | 4198 | 92.7 | 183 | 74.8 | 180 | 76.4 | 40 | 58.9 | |||||
| 4529 | 100% | 245 | 100% | 236 | 100% | 68 | 100% | ||||||
| Taken tranquilizers in the last 12 months | Yes | 120 | 2.7 | 21 | 8.4 | .0002 | 28 | 11.9 | .0002 | 12 | 17.6 | .0002 | .02 |
| No [ref] | 4408 | 97.3 | 224 | 91.6 | 208 | 88.1 | 56 | 82.4 | |||||
| 4528 | 100% | 244 | 100% | 236 | 100% | 68 | 100% | ||||||
| Taken antipsychotic in the last 12 months | Yes | 21 | 0.5 | 8 | 3.4 | .0002 | 3 | 1.0 | .05 | 3 | 4.5 | .0002 | .09 |
| No [ref] | 4509 | 99.5 | 236 | 96.6 | 233 | 99.0 | 64 | 95.5 | |||||
| 4529 | 100% | 244 | 100% | 236 | 100% | 67 | 100% | ||||||
| PERSONAL | |||||||||||||
| Difficulty getting along or maintaining social life due to health problems | Yes | 244 | 5.4 | 44 | 17.9 | .0002 | 48 | 20.6 | .0002 | 27 | 39.3 | .0002 | .0002 |
| No [ref] | 4257 | 94.6 | 201 | 82.1 | 185 | 79.4 | 41 | 60.7 | |||||
| 4501 | 100% | 244 | 100% | 233 | 100% | 68 | 100% | ||||||
| No. of biological children | le | 752 | 16.6 | 57 | 23.5 | .01 | 52 | 21.8 | .08 | 14 | 20.3 | .26 | .89 |
| 2e | 1084 | 23.9 | 57 | 23.4 | .86 | 57 | 24.2 | .40 | 22 | 33.1 | .08 | .27 | |
| 3 or more | 1247 | 27.5 | 58 | 23.8 | .38 | 65 | 27.7 | .38 | 18 | 25.9 | .17 | .44 | |
| None [ref] | 1448 | 32.0 | 72 | 29.3 | 62 | 26.3 | 14 | 20.7 | |||||
| 4531 | 100% | 244 | 100% | 236 | 100% | 68 | 100% | ||||||
All analyses represent the unadjusted weighted frequencies (%) from the NCS-R. Pearson chi-square tests were used for categorical variables; and ANOVA tests were used for continuous variables. All P values were calculated using FDR analyses to adjust for multiple comparisons.
Table 3. Adjusted OR and 95% CI of Disease Burden Indicators by Migraine and PTSD Status.
| (B) — Migraine: + PTSD | (C) –Migraine –PTSD | (D) + Migraine +PTSD | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| Disease Burden Indicator | (A) – Migraine –PTSD | OR (95% CI) | P value (B vs A) | OR (95% CI) | P value (C vs A) | OR (95% CI) | P value (D vs A) | P value (D vs C) |
| FINANCIAL | ||||||||
| Have enough money to meet needs | ||||||||
| Just enough† | Ref | 1.12 (0.68, 1.85) | .66 | 1.56 (0.95, 2.58) | .16 | 2.42 (1.17, 5.00) | .006 | .41 |
| Not enough† | Ref | 1.65 (0.86, 3.17) | .20 | 2.10 (1.16, 3.83) | .04 | 4.42 (1.78, 10.97) | .04 | .63 |
| Poverty Index | ||||||||
| Low‡ | Ref | 1.07 (0.73, 1.57) | .69 | 1.46 (0.86, 2.48) | .21 | 2.16 (1.10, 4.24) | .04 | .40 |
| Middle‡ | Ref | 1.23 (0.79, 1.90) | .40 | 1.16 (0.77, 1.75) | .58 | 2.23 (1.19, 4.19) | .02 | .21 |
| Received welfare/public assistance since 18 yo | Ref | 2.05 (1.33, 3.18) | .006 | 1.63 (1.07, 2.49) | .06 | 2.19 (1.27, 3.79) | .02 | .63 |
| Worked for pay or profit in the last week | Ref | 1.20 (0.85, 1.70) | .39 | 0.81 (0.59, 1.11) | .28 | 0.42 (0.24, 0.74) | .01 | .07 |
| Health insurance, covered by employer or union | Ref | 0.97 (0.74, 1.27) | .83 | 1.00 (0.74, 1.27) | .96 | 0.75 (0.40, 1.41) | .41 | .41 |
| Health insurance, covered by insurance company | Ref | 0.59 (0.35, 0.98) | .09 | 0.79 (0.52, 1.20) | .37 | 0.68 (0.33, 1.40) | .37 | .96 |
| HEALTH-RELATED | ||||||||
| Overall mental health status in past 30 days | ||||||||
| Better§ | Ref | 2.26 (1.45, 3.52) | .003 | 1.32 (0.85, 2.02) | .30 | 1.69 (0.93, 3.05) | .18 | .61 |
| Worse§ | Ref | 2.67 (1.69, 4.21) | .0003 | 2.59 (1.81, 3.71) | .0003 | 4.53 (2.65, 7.74) | .0003 | .09 |
| Difficulty with concentration/memory/thinking in last month due to health problems | Ref | 4.72 (3.52, 6.32) | .0003 | 4.24 (3.02, 5.96) | .0003 | 8.42 (5.63, 12.60) | .0003 | .02 |
| Overall physical health during past 30 days | ||||||||
| Better§ | Ref | 1.36 (0.90, 2.06) | .21 | 0.78 (0.48, 1.25) | .40 | 1.60 (0.85, 3.01) | .21 | .12 |
| Worse§ | Ref | 1.68 (1.17, 2.42) | .02 | 1.93 (1.20, 3.11) | .02 | 2.83 (1.53, 5.25) | .006 | .39 |
| Frequency experienced physical discomfort in past 30 days | ||||||||
| All of the time# | Ref | 4.66 (2.73, 7.96) | .0003 | 7.42 (4.12, 13.34) | .0003 | 30.11 (11.36, 79.86) | .0003 | .07 |
| Most of the time# | Ref | 2.70 (1.67, 4.36) | .0003 | 5.95 (2.81, 12.59) | .0003 | 30.70 (14.49, 65.06) | .0003 | .02 |
| Some of the time# | Ref | 3.01 (1.98, 4.56) | .0003 | 5.59 (3.33, 9.39) | .0003 | 12.21 (5.35, 27.89) | .0003 | .22 |
| A little of the time# | Ref | 1.81 (1.26, 2.60) | .0003 | 2.99 (1.85, 4.82) | .0003 | 5.10 (2.21, 11.78) | .01 | .21 |
| Taken antidepressants in the last 12 months | Ref | 3.44 (2.35, 5.05) | .0003 | 3.34 (2.25, 4.96) | .0003 | 7.23 (4.83, 10.83) | .0003 | .02 |
| Taken tranquilizers in the last 12 months | Ref | 3.02 (2.13, 4.28) | .0003 | 5.18 (3.33, 8.05) | .0003 | 7.35 (4.69, 11.53) | .0003 | .40 |
| Taken antipsychotic in the last 12 months | Ref | 7.06 (3.78, 13.16) | .0003 | 3.08 (1.16, 8.22) | .06 | 10.47 (3.58, 30.63) | .0003 | .07 |
| PERSONAL | ||||||||
| Difficulty getting along or maintaining social life due to health problems | Ref | 3.40 (2.40, 4.82) | .0003 | 4.20 (2.62, 6.74) | .0003 | 9.95 (5.72, 17.32) | .0003 | .04 |
| Number of biological children | ||||||||
| 1‖ | Ref | 1.39 (0.88, 2.19) | .21 | 1.47 (0.94, 2.29) | .16 | 1.26 (0.54, 2.92) | .66 | .82 |
| 2‖ | Ref | 1.15 (0.74, 1.78) | .61 | 1.39 (0.96, 2.02) | .13 | 1.68 (0.81, 3.46) | .22 | .84 |
| 3 or more‖ | Ref | 1.18 (0.80, 1.76) | .44 | 1.78 (1.15, 2.76) | .04 | 1.31 (0.55, 3.12) | .61 | .44 |
Logistic regression or multinomial logistic regression models used, as appropriate for all results in Table. All models adjusted for age, income, sex, race, marital status, and smoking status, except for poverty index in which with income was not adjusted for, as it was used in creation of outcome variable; all P values were calculated using FDR analyses to adjust for multiple comparisons.
Comparison to “more” response choice.
Comparison to high income class group.
Comparison to “about the same” response choice.
Comparison to “none” response choice.
Comparison to “0” response choice.
PTSD = post-traumatic stress disorder.
Financial burden indicators included assessments of health insurance coverage (employer or union or an insurance company), employment history (including the numbers of days in the past month where their work quality was reduced due to their physical or mental health or due to substance abuse, the number of weeks an individual worked for profit in the past 12 months and the number of hours the individual worked for pay or profit in an average week), as well as the reception of public assistance, the participants perception of the amount of money they had to meet their needs (not enough, just enough, more than enough), and the poverty index as described below.
Poverty Index
The poverty index was calculated using the annual household income divided by the 2001 Health and Human Services' poverty guidelines, with a minimum value of 0 and a maximum value of 24.21 Poverty index values were then assigned as follows: <3 = low, ≥3 to <6 = middle, ≥6 high as previously described.22
Health-related variables included assessments of the participants' overall physical and mental health (better, about the same, and worse) difficulty with concentration, memory, and thinking, and the frequency of experiencing physical discomfort (all, most, some, or a little of the time) in the past 30 days as compared to usual, as well as their total number of different prescription and nonprescription medication utilized in the past 7 days, and the use of antidepressants, tranquilizers, and antipsychotics in the past 12 months.
Personal disease burden outcomes that were assessed included the number of biological children, and whether or not they experienced difficulty getting along or maintaining a social life due to their health problems.
Statistical Analyses
Disease burden variables with 10% or more missing data were excluded from analyses. Pearson chi-square, median tests, and analysis of variance (ANOVA) tests were used, as appropriate, to determine the association between migraine/PTSD subgroup and participant characteristics at baseline.
Associations between outcomes and migraine/PTSD groups were further assessed using regression models as described below. Variables were included as possible confounders if P<.10 in univariate analyses, and included age, sex, race, income, and marital and smoking status. Models were first run unadjusted and then adjusted for age, sex, race, income, marital status, and smoking status. Logistic regression/multinomial logistic regression was used to assess the association between dichotomous/multilevel outcome variables indicating financial or social disability and headache/PTSD subgroup. Nonparametric regression models were used to determine the associations between non-normally distributed continuous outcomes of financial or social disability and headache/PTSD subgroup. Poisson regression was used to determine the association between count outcomes of financial or social disability and headache/PTSD subgroup. Finally, we considered the validity of the inclusion of MDD as a covariate in our models. Due to over-adjustment concerns, (given the overlap in individual symptoms required for fulfillment of PTSD [eg, constricted affect, diminished interest in activities, and sleep disturbance] and MDD diagnostic criteria), confirmed by a significant correlation between MDD and PTSD (rφ=0.15, P<.001), we a priori chose to adjust for MDD in sensitivity analyses rather than include it in our primary models. The MDD-adjusted results are thus presented as Supporting Information with the recognition that careful consideration and interpretation of such findings may be of interest to those with appropriate expertise.
Univariate, logistic, multinomial logistic, and nonparametric regression analyses were conducted using survey procedures in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and adjusted for weight, cluster and primary sampling unit, to take into consideration the complex sampling design. Poisson models were conducted with SAS 9.4 using genmod procedures, with class, strata, and weight statements to adjust for weight, cluster, and primary sampling unit, as survey procedures were not available. To correct for multiple comparisons and exclude false positives, we applied the false discovery rate (FDR). All reported P values are FDR-adjusted and can be compared to a P value of .05 to assess statistical significance.
Results
Participants
A total of 5692 participants had complete headache and PTSD information and positive weights allowing use of survey procedures in SAS. Of those, 609 individuals only fulfilled criteria for remote migraine or probable migraine criteria, and were excluded from analyses, leaving an analytic sample of 5083.
Demographics
Of the 5083 participants, 89.2% had no migraine and no PTSD, (herein referred to as controls,) 4.8% had PTSD alone, 4.6% had migraine alone, and 1.3% had mig+PTSD. As compared to controls, the majority of participants with PTSD alone, migraine alone, and with mig+PTSD were women, younger, and more likely to be current smokers and to have MDD, (Table 1). The median income of those with mig+PTSD ($47 K; P=.007), but not PTSD alone ($53 K; P=.07), or migraine alone ($54 K; P=.26), was less than the median income of controls ($60 K). Those with mig+PTSD were slightly older (39.9±1.2 vs 37.8±0.6; P=.0003) and had a lower median income ($47 K vs $54 K; P=.04) than those with migraine alone, (Table 1).
Table 1. Demographic Characteristics of NCS-R Respondents by Migraine and PTSD Status.
| Demographic characteristic | (A) – Migraine –PTSD (n=4535) | (B) – Migraine + PTSD (n=244) | P value (B vs A) | (C) + Migraine – PTSD (n=236) | P value (C vs A) | (D) + Migraine + PTSD (n=68) | P value (D vs A) | P value (C vs D) |
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| N (%) | N (%) | N (%) | N (%) | |||||
| Mean age (SE) | 45.4 (0.5) | 42.1 (0.9) | .005 | 37.8 (0.6) | .0003 | 39.9 (1.2) | .0003 | .0003 |
| Female sex | 2216 (48.9) | 178 (73.0) | .0003 | 188 (79.4) | .0003 | 55 (81.2) | .0003 | .79 |
| Race | ||||||||
| White | 3258 (71.8) | 177 (72.3) | .35 | 185 (78.2) | .01 | 50 (74.0) | .65 | .59 |
| Black | 587 (12.9) | 38 (15.7) | 9 (4.0) | 5 (7.9) | ||||
| Hispanic | 521 (11.5) | 19 (7.6) | 29 (12.2) | 9 (13.8) | ||||
| Other | 169 (3.7) | 11 (4.4) | 13 (5.7) | 3 (4.4) | ||||
| Marital status | ||||||||
| Married | 2543 (56.1) | 110 (44.9) | .002 | 135 (57.1) | .90 | 44 (64.7) | .32 | .51 |
| Divorced/separated/widowed | 907 (20.0) | 75 (30.8) | 48 (20.5) | 13 (18.7) | ||||
| Never married | 1084 (23.9) | 59 (24.3) | 53 (22.4) | 11 (16.6) | ||||
| Education | ||||||||
| <High school | 748 (16.5) | 47 (19.2) | .51 | 47 (19.7) | .31 | 17 (25.3) | .35 | .83 |
| High school | 1477 (32.6) | 67 (27.5) | 77 (32.7) | 18 (27.1) | ||||
| College | 1244 (27.4) | 70 (28.5) | 72 (30.5) | 19 (28.8) | ||||
| Post-college | 1066 (23.5) | 60 (24.7) | 40 (17.1) | 13 (18.9) | ||||
| Median income (USD)† | $60,216 | $52,777 | .07 | $54,171 | .26 | $47,313 | .007 | .04 |
| Smoking history | ||||||||
| Never | 2210 (48.7) | 84 (34.2) | .0003 | 103 (43.5) | .04 | 20 (30.0) | .0003 | .26 |
| Former | 1248 (27.5) | 62 (25.3) | 55 (23.4) | 16 (22.9) | ||||
| Current | 1076 (23.7) | 99 (40.5) | 78 (33.0) | 32 (47) | ||||
| MDD, 12 mo | 206 (4.5) | 48 (19.8) | .0003 | 41 (17.2) | .0003 | 17 (25.2) | .0003 | .15 |
All analyses represent the weighted means (SE) and frequencies (%) from the NCS-R. Pearson chi-square tests were used for categorical variables; and ANOVA tests were used for continuous variables. All P values were calculated using FDR analyses to adjust for multiple comparisons.
SD = standard deviation; USD = US dollars.
The median household income in 2013 was $51,939; the median household income for the entire study population (2001-2003) was $47,500.
Financial, Health-Related, and Personal Disease Burdens
The unadjusted prevalence and adjusted odds ratio (OR) and 95% confidence intervals for financial, health, and personal burden indicators are presented in Tables 2 and 3 by migraine and PTSD status. Adjusted rate ratios and 95% confidence limit (CL) for employment and medication utilization indicators by migraine and PTSD status are presented in Table 4.
Table 4. Adjusted Rate Ratios and 95% CL for Employment and Medication Utilization Indicators by Migraine and PTSD Status.
| (A) – Migraine –PTSD (n=4535) | (B) – Migraine + PTSD (n=244) | (C) + Migrairne – PTSD (n=236) | (D) + Migraine +PTSD (n=68) | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| RR (95% CL) | P value (B vs A) | RR (95% CL) | P value (C vs A) | RR (95% CL) | P value (D vs A) | P value (C vs D) | ||
| Employment | ||||||||
| Number of days in last 30 days where work quality was cut due to physical or mental health or substance abuse (0-30) | Ref | 2.09 (1.91, 2.29) | .0002 | 2.39 (2.19, 2.62) | .0002 | 6.79 (6.16, 7.49) | .0002 | .0002 |
| Number of years employed at least 6 months (0-78) | Ref | 1.09 (1.06, 1.13) | .0002 | 1.02 (0.99, 1.06) | .21 | 1.05 (0.99, 1.12) | .10 | .10 |
| Number of weeks worked for profit in last 12 months (0-52) | Ref | 1.05 (1.03, 1.07) | .0002 | 0.98 (0.96, 1.00) | .08 | 0.88 (0.84, 0.92) | .0002 | .0002 |
| Number of hours worked for pay or profit in average week (0-96) | Ref | 1.06 (1.04, 1.09) | .0002 | 1.01 (0.98, 1.04) | .47 | 1.10 (1.04, 1.16) | .0002 | .001 |
| Medication Utilization | ||||||||
| Number of different prescription medications taken in last 7 days (0-50) | Ref | 1.61 (1.47, 1.78) | .0002 | 1.87 (1.70, 2.06) | .0002 | 2.17 (1.86, 2.54) | .0002 | .10 |
| Number of different nonprescription medications taken in last 7 days (0-53) | Ref | 1.29 (1.17, 1.42) | .0002 | 1.25 (1.13, 1.39) | .0002 | 1.42 (1.19, 1.70) | .0002 | .22 |
Poisson regression used for all results. Models adjusted for age, income, sex, race, marital status, and smoking status.
RR=rate ratio. All P values were calculated using FDR analyses to adjust for multiple comparisons.
Financial and Employment Burdens
As compared to controls, individuals with mig+PTSD (OR 4.42; CI: 1.78, 10.97) and migraine alone (OR 2.10, CI: 1.16, 3.83), but not PTSD alone (OR 1.65; CI: 0.86, 3.17), were more likely to report not having enough money to meet their needs as compared to reporting having more than enough money (Tables 2 and 3). Additionally, as compared to controls, those with mig+PTSD, but not migraine alone or PTSD alone, were more likely to be in the low (OR 2.16; CI 1.10, 4.24) or middle poverty index (OR 2.23; CI: 1.19, 4.19) as compared to the high poverty index. Those with mig+PTSD (OR 2.19; CI: 1.27. 3.79, P=.006) and PTSD alone (OR 2.05; CI: 1.33, 3.18, P=.02), but not migraine alone (OR 1.63; CI: 1.07, 2.49, P=.06), were significantly more likely to receive welfare or public assistance than controls; however there was no difference between those with migraine alone and those with mig+PTSD, (Tables 2 and 3).
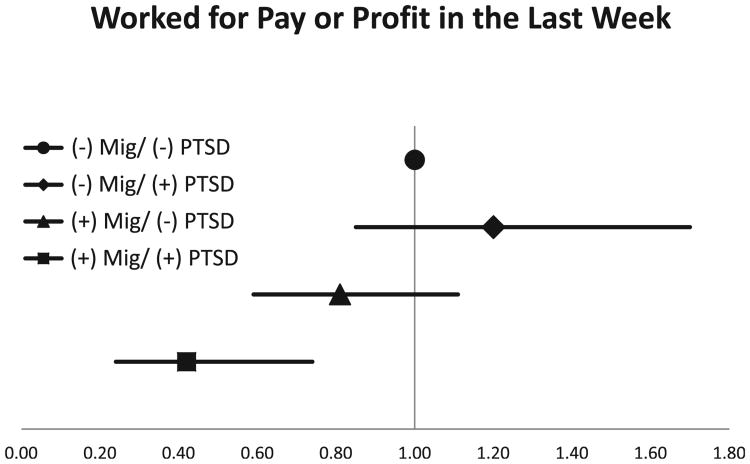
The number of days where work quality was cut due to physical or mental health or substance abuse in the past month was greater in all three groups as compared to controls: (1) migraine only: mean 2.57 (SEM 0.32) vs mean 1.09 (SEM 0.08) days, RR=2.39; CI: 2.19, 2.62; (2) PTSD only: mean 2.43 (SEM 0.33) vs mean 1.09 (SEM 0.08) days, RR=2.09; CI: 1.91, 2.29; (3) mig+PTSD: mean 8.2 (SEM 0.79) vs 1.09 (SEM 0.08) days, RR 6.79; CI 6.16, 7.49; and was almost 3-fold greater in those mig+PTSD than migraine alone (mean 2.57 [SEM 0.72] days, RR 2.77; CI: 2.45, 3.14), (Table 4). As compared to controls, those with mig+PTSD (0.42; CI: 0.24, 0.74), but not those with migraine alone or PTSD alone, were less likely to have worked for pay or profit in the last week, (Table 3, Fig. 1). Further, while those with migraine alone (OR 0.98; CI: 0.96, 1.00) worked a comparable number of weeks in the past 12 months as compared to controls, individuals with mig+PTSD (OR 0.88; CI: 0.84, 0.92) worked slightly less and those with PTSD alone (OR 1.05; CI: 1.03, 1.07) slightly more number of weeks in the past year than controls. However, both those with mig+PTSD (OR 1.10; CI: 1.04, 1.16) and PTSD alone (OR 1.06; CI: 1.04, 1.09), but not migraine alone (OR 1.01; CI: 0.98, 1.04), worked more hours for pay or profit in an average week as compared to controls (Table 4).
Fig. 1.
Odds ratio and 95% confidence interval of those who worked for pay or profit in the last week across migraine and PTSD groups in the NCS-R. The model was adjusted for age, sex, race, marital status, income, and smoking.
There was no difference in health insurance coverage across groups (Tables 2 and 3).
Health-Related Burdens
As compared to controls, all groups (PTSD alone, migraine alone, Mig+PTSD) had an increased odds of reporting their overall mental health was worse in the past 30 days and that they had difficulty with concentration, memory, and thinking due to health problems (Tables 2 and 3). In addition, as compared to those with migraine alone, individuals with mig+PTSD were over 2-fold more likely to report difficulty with concentration, memory, and thinking in the past month due to health problems (OR 2.32, CI: 1.15, 4.69).
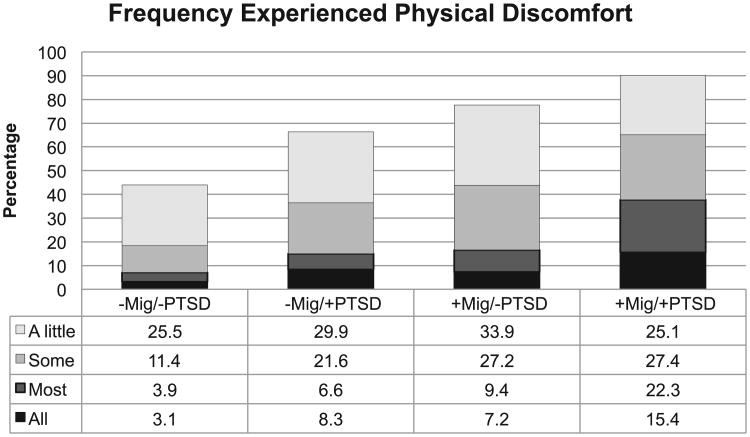
All groups (PTSD alone, migraine alone, Mig+PTSD) reported worse physical health and more physical discomfort in the past 30 days as compared to controls (Table 2 and 3, Fig. 2). Additionally, individuals with mig+PTSD had over a 5-fold increased odds of experiencing physical discomfort most of the time in the past 30 days as compared to those with migraine alone (OR 5.4; CI: 1.55, 18.84).
Fig. 2.
Physical discomfort across migraine and PTSD groups in the NCS-R. The percentages are crude rates. The adjusted odds of reporting physical discomfort in most of the last 30 days was increased in all groups as compared to controls (those without either disorder), and was over 5-fold increased in those with both migraine and PTSD as compared to individuals with migraine alone (OR 5.4; CI: 1,55, 18.84).
As compared to controls, although all groups (PTSD alone, migraine alone, Mig+PTSD) were over 60% more likely to have used a greater number of prescription medications, and over 24% more likely to have used a greater number of nonprescription medications in the past 7 days, the number of nonprescription and prescription medications used was not different between individuals with Mig+PTSD as compared to those with migraine alone (nonprescription: OR 1.14; CI: 0.93, 1.40, P=.22; prescription: OR 1.17; CI: 0.98, 1.40, P=.10) (Table 4).
All groups (PTSD alone, migraine alone, Mig+PTSD) were also more likely than controls to have taken antidepressants and tranquilizers in the last 12 months. However, only those PTSD alone or Mig+PTSD were more likely to have taken anti-psychotics in the last 12 months. Those with mig+PTSD were also more likely than those with migraine alone to have taken antidepressants, but not tranquilizers or antipsychotics, in the past 12 months (Table 2).
Interpersonal Burdens
All groups reported difficulty getting along or maintaining their social life due to health problems (Tables 2 and 3, Fig. 3). Specifically, those with PTSD alone, migraine alone, and Mig+PTSD were 3- to 10-fold more likely than controls to report such difficulty (PTSD alone: OR 3.4; CI: 2.40, 4.82; migraine alone: OR 4.20; CI: 2.62, 6.74; mig+PTSD: OR 9.95; CI: 5.72, 17.32), and this was significantly different between those with mig+PTSD and migraine alone (OR 2.32; CI: 1.15, 4.69).
Fig. 3.
Difficulty getting along and maintaining a social life across migraine and PTSD groups in the NCS-R. The percentages are crude rates; P values indicate pairwise comparisons of each group to those with no migraine and no PTSD. The adjusted odds of having difficulty or getting along/maintaining a social life was increased almost 10-fold in those with both migraine and PTSD vs those without either disorder (OR 9.95; CI: 5.72, 17.32) and 2-fold increased as compared to individuals with migraine alone (OR 2.06; CI: 1.21, 3.51). * p value <0.01 as compared to controls (−Mig/−PTSD). # p value <0.05 as compared to those with migraine alone (+Mig/−PTSD).
There were no differences in the odds of reporting having 1, 2, or 3 children across groups, with the exception that those with migraine alone were more likely than controls to have 3 or more children as compared to no children (Tables 2 and 3).
Burdens in Migraine and PTSD Groups Controlling for Depression
As hypothesized, there was a significant correlation between MDD and PTSD (rφ= 0.15, P<.0001). Given this correlation, our a priori concern for including MDD as a covariate was supported and the interpretation of the MDD-adjusted results (Supplemental Tables 1 and 2) is of uncertain and limited meaning. With this caveat, the financial, health-related, and interpersonal burdens in the MDD-adjusted model (ie, adjusted for demographics, smoking, and MDD) remained largely the same for most, although not all, outcome measures. For example, after adjustments including MDD, there was no longer a difference in poverty levels among the four groups (ie, control, PTSD alone, Migraine alone, Mig+PTSD). Other outcomes that lost significance after adjusting for MDD include overall mental health being worse in the past 30 days (in those with migraine alone vs those with Mig+PTSD), use of an antipsychotic in the last 12 months (in those with migraine alone vs controls as well as in those with migraine alone vs Mig+PTSD), and having health insurance covered by an insurance company (in those with PTSD alone vs controls). See Supplemental Information Tables 1 and 2 for full details.
Discussion
Migraine is a common and often disabling disorder that is comorbid with PTSD.23 In this study, we conducted a cross-sectional, general population study to evaluate the impact of PTSD in those with migraine on several indicators of financial, health-related, and interpersonal disease burdens. We compared these indicators in those without either migraine or PTSD (controls) to each of the following three groups: (1) those with PTSD alone, (2) those with migraine alone, and (3) those with both migraine and PTSD, as well as between those with migraine alone and those with both migraine and PTSD.
Our study has two primary findings. First, the current study supports previous research demonstrating that the presence of migraine or PTSD alone is sufficient to result in substantial personal and societal disease burdens.14,24-27 Second, this study extends these findings to demonstrate that the presence of PTSD in migraineurs may entail an even greater personal and societal burden than is found in individuals with migraine alone for several indicators of financial, health-related, and interpersonal disease burdens.
Previous research has shown that both work absenteeism and presenteeism (reduced functional status while remaining at work) contribute to the personal and societal financial burden of migraine.12,28-31 On average it has been estimated that those with migraine have a 50% or greater reduction in productivity during acute attacks,31 work fewer hours because of headache,13 and miss approximately 4-10 work or school days per year.12,28,32
In this study, individuals with mig+PTSD were over 6.5-fold more likely than controls to have had their work-quality cut due to their physical or mental health in the past month, a finding which was over 2.5-fold greater than those with migraine alone. In addition, individuals with migraine and PTSD were 58% less likely than controls to have worked for pay or profit in the past week, whereas there was no difference as compared to controls for those with migraine alone or PTSD alone. Further, in contrast to migraineurs with PTSD, individuals with migraine alone (ie, without PTSD) were comparable to controls in the odds of having worked and the number of hours worked in the past week for pay or profit. These findings support that the presence of PTSD substantially contributes to the work-related financial burden in migraineurs, and suggests that the presence of PTSD may have, at least in part, been a significant contributor to the work-related disease burden described in previous studies. Additionally, in this study, although there was no difference between those with migraine alone and controls, those with mig+PTSD were slightly (10%) more likely to work more hours for pay or profit in the average week, suggesting that those with mig+PTSD may be working more hours when they are able to work to compensate for the reduction in work quality and the decreased number of weeks they are able to work in a year.
In addition to lost productivity several other markers of societal burden are notable. Although both those with migraine alone and mig+PTSD were more likely than controls to report not having enough money to meet their needs, differences between those with mig+PTSD and migraine alone were seen in the crude median income (mig+PTSD: $47K, migraine alone $54K, controls: $60K) as well as the poverty index. Specifically, as compared to controls, individuals with mig+PTSD were over 2-fold more likely to be in the low poverty index as compared to the high index, while there was no significant difference in poverty index levels between those with migraine alone and controls. Data are conflicting on the migraine-SES association, with some studies supporting that that the risk of migraine is increased in those of low socioeconomic status33-36 and others supporting no association or an increased risk in those of high SES.37-39 Notably, none of these studies included PTSD (or depression) as a covariate in their evaluations of the migraine-SES association. Given our current findings it is possible that the presence or absence of PTSD may contribute to the migraine-SES association, and may, at least in part, have contributed to the differences across previous studies evaluating the migraine-SES association.
In addition to financial burdens, several markers of health-care related and interpersonal burdens were also evaluated. Not surprisingly, as compared to controls, all groups (PTSD alone, Migraine alone, mig+PTSD) were more likely to report their overall mental and physical health status as worse, to have difficulty with concentration, memory, or thinking and to be more likely to report physical discomfort most of the time in the past 30 days. Additionally, as compared to those with migraine alone, those with mig+PTSD were 2-fold more likely to have difficulty with concentration, memory, or thinking and were almost 5-fold more likely to experienced physical discomfort most of the time in the past 30 days.
Differences in interpersonal disease burdens were also found in this study. Previous research has reported that 29% of migraineurs acknowledge arguments as more common due to their headaches, 20-60% report negative effects on relationships at home, and 32% avoid making plans for fear of cancellation due to their headaches.40 Our current findings are compatible with these findings, with all groups being more likely to report difficulty getting along or maintaining their social life due to their health problems as compared to controls (PTSD alone: over 3-fold; migraine alone: over 4-fold; mig+PTSD: almost 10-fold) and which was 2-fold greater in those with mig+PTSD than those with migraine alone.
Given the personal and societal burdens the presence of PTSD in migraineurs entail, these data have several potential clinical and research implications. Specifically, it supports the need for enhanced physician awareness of the migraine-PTSD association, enhanced screening of migraine patients for PTSD, and the consideration of medications (eg, serotonin norepinephrine reuptake inhibitors) and psychotherapies (eg, cognitive behavioral therapy) that treat both disorders in those migraineurs with comorbid PTSD.41 Future research evaluating the effect of PTSD therapy on migraine severity, disability, and treatment response may also assist in advancing our understanding of the clinical implications of the migraine-PTSD association.
The NCS-R has several strengths. First, this study permitted assessment of the impact of PTSD on the personal and societal burdens in individuals with and without migraine in a large, population-based sample, not subject to the inherent biases that can be present in clinical and selected populations (eg, pain clinics, trauma centers, and military cohorts). Second, both migraine and PTSD were determined based on standardized diagnostic criteria.
However, several cautions are warranted in interpreting these results. Limitations exist in regards to headache classification in the NCS-R. The headache screener question was based on persons having “frequent or severe” headaches and which likely eliminated those with having less severe or infrequent headaches who may have fulfilled migraine criteria. Additionally although migraine diagnoses were based on the ICHD criteria, one part of the ICHD criteria C (aggravation by activity) was not queried. Previous research utilizing the NCS-R database for migraine studies has shown that the failure to include this criterion resulted in a loss of only a limited number of participants; and thus is not likely to have significantly impacted our current findings.4 The NCS-R headache questions have also not been validated for migraine as compared to a physician diagnosis of ICHD-II migraine.
A second limitation to consider is that the NCS-R utilizes the DSM-IV PTSD criteria, and PTSD prevalence may be slightly higher using DSM-IV compared to DSM-V.42 Although we have no reason to believe this change would have affected migraine differentially, it is possible that the results reported herein might have been different if we had used DSM-V criteria for PTSD. Additionally, although we consider MDD as a possible confounder, and we provided supplemental models with the inclusion of MDD as a covariate, this information was presented cautiously and with the caveat that reliable or meaningful interpretation was deemed not possible given the significant diagnostic overlap between the two disorders. Finally, this dataset was collected in 2001-2003 and it is possible that the current findings would differ for more recent time periods. However, we have no reason to believe that the cumulative burden of PTSD in migraine in this civilian population is different now than when this dataset was collected.
Despite these limitations, our results highlight the impact of PTSD on the already substantial financial, health-related, and interpersonal disease burden present in those with migraine. These findings support the need for those who treat migraine patients to be aware of the potential comorbidity with PTSD and to ensure that patients are properly screened and treated for PTSD when present. In this manner, clinicians can help to limit the personal and societal burdens associated with PTSD in those with migraine.
Supplementary Material
Supplemental Table 1. Depression-adjusted Indicators of financial or social burden by migraine and PTSD status.
Supplemental Table 2. Depression-adjusted Employment and medication utilization by migraine and PTSD status.
Acknowledgments
The authors would like to acknowledge and thank Jian-Ping He for her advice and guidance.
Funding: The National Comorbidity Survey-Replication (NCS-R) is supported by the United States (U.S.) National Institute of Mental Health (NIMH; U01-MH60220) with supplemental support from the National Institute of Drug Abuse, the Substance Abuse and Mental Health Services Administration, the Robert Wood Johnson Foundation (Grant#044780) and the John W. Alden Trust. Collaborating NCS-R investigators include Dr. Merikangas (co-principal investigator, NIMH). This study was also supported by funding from the National Institute of Health/National Institute of Neurological Disorders and Stroke (K23-NS078345) to Dr. Peterlin. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or the U.S. government. Dr. Peterlin had full access to all of the data in the study and takes responsibility of the integrity of the data and the accuracy of the data analysis.
Footnotes
Statistical Analysis: All statistical analyses were conducted by Dr. Andrea L. Metti.
Conflict of Interest: Dr Scher is an Associate editor for Cephalalgia and Pain Medicine. She has grant support from the CNRM and CDMRP unrelated to the current study and is a consultant/advisory board member for Allergan. Dr Peterlin serves on the editorial boards for Headache, Neurology, and BMC Neurology and has unrelated investigator-initiated grant support from Egalet Corporation and the Landenberger Foundation. Dr. Rao, Ms. Vieiria, Dr. Merikangas, and Dr. Metti have no conflicts of interest to disclose.
Supporting Information: Additional Supporting Information may be found in the online version of this article.
-
(a) Conception and DesignAnn I. Scher, B. Lee Peterlin
-
(b) Acquisition of DataKathleen R. Merikangas, Andrea L. Metti
-
(c) Analysis and Interpretation of DataAruna S. Rao, Ann I. Scher, Rebeca V.-A. Vieira, Kathleen R. Merikangas, Andrea L. Metti, B. Lee Peterlin
-
(a) Drafting the ManuscriptAruna S. Rao, Andrea L. Metti, B. Lee Peterlin
-
(b) Revising It for Intellectual ContentAruna S. Rao, Ann I. Scher, Rebeca V.-A. Vieira, Kathleen R. Merikangas, Andrea L. Metti, B. Lee Peterlin
-
(a) Final Approval of the Completed ManuscriptAruna S. Rao, Ann I. Scher, Rebeca V.-A. Vieira, Kathleen R. Merikangas, Andrea L. Metti, B. Lee Peterlin
Contributor Information
Aruna S. Rao, Department of Neurology, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
Ann I. Scher, Uniformed Services University, Bethesda, MD, USA.
Rebeca V.A. Vieira, Department of Psychology, Federal University of Rio Grande do Sul, Porto Alegre, Brazil.
Kathleen R. Merikangas, National Institute of Mental Health, National Institutes of Health, Bethesda, MD, USA.
Andrea L. Metti, Metti Consulting, Pittsburgh, PA, USA.
B. Lee Peterlin, Department of Neurology, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
References
- 1.Peterlin BL, Katsnelson MJ, Calhoun AH. The associations between migraine, unipolar psychiatric comorbidities, and stress-related disorders and the role of estrogen. Curr Pain Headache Rep. 2009;13:404–412. doi: 10.1007/s11916-009-0066-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merikangas KR, Stevens DE. Comorbidity of migraine and psychiatric disorders. Neurol Clin. 1997;15:115–123. doi: 10.1016/s0733-8619(05)70298-x. [DOI] [PubMed] [Google Scholar]
- 3.Breslau N, Davis GC, Schultz LR, Peterson EL. Joint 1994 Wolff award presentation. Migraine and major depression: A longitudinal study. Headache. 1994;34:387–393. doi: 10.1111/j.1526-4610.1994.hed3407387.x. [DOI] [PubMed] [Google Scholar]
- 4.Peterlin BL, Rosso AL, Sheftell FD, Libon DJ, Mossey JM, Merikangas KR. Post-traumatic stress disorder, drug abuse and migraine: New findings from the national comorbidity survey replication (NCS-R) Cephalalgia. 2011;31:235–244. doi: 10.1177/0333102410378051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smitherman TA, Kolivas ED. Trauma exposure versus posttraumatic stress disorder: Relative associations with migraine. Headache. 2013;53:775–786. doi: 10.1111/head.12063. [DOI] [PubMed] [Google Scholar]
- 6.de Leeuw R, Schmidt JE, Carlson CR. Traumatic stressors and post-traumatic stress disorder symptoms in headache patients. Headache. 2005;45:1365–1374. doi: 10.1111/j.1526-4610.2005.00269.x. [DOI] [PubMed] [Google Scholar]
- 7.Peterlin BL, Tietjen GE, Brandes JL, et al. Post-traumatic stress disorder in migraine. Headache. 2009;49:541–551. doi: 10.1111/j.1526-4610.2009.01368.x. [DOI] [PubMed] [Google Scholar]
- 8.Afari N, Harder LH, Madra NJ, et al. PTSD, combat injury, and headache in veterans returning from Iraq/Afghanistan. Headache. 2009;49:1267–1276. doi: 10.1111/j.1526-4610.2009.01517.x. [DOI] [PubMed] [Google Scholar]
- 9.Balaban H, Semiz M, Senturk IA, et al. Migraine prevalence, alexithymia, and post-traumatic stress disorder among medical students in Turkey. J Headache Pain. 2012;13:459–467. doi: 10.1007/s10194-012-0452-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlson KF, Taylor BC, Hagel EM, Cutting A, Kerns R, Sayer NA. Headache diagnoses among Iraq and Afghanistan war veterans enrolled in VA: A gender comparison. Headache. 2013;53:1573–1582. doi: 10.1111/head.12216. [DOI] [PubMed] [Google Scholar]
- 11.Lipton RB, Stewart WF, Scher AI. Epidemiology and economic impact of migraine. Curr Med Res Opin. 2001;17(Suppl 1):s4–s12. doi: 10.1185/0300799039117005. [DOI] [PubMed] [Google Scholar]
- 12.Steiner TJ, Scher AI, Stewart WF, Kolodner K, Liberman J, Lipton RB. The prevalence and disability burden of adult migraine in England and their relationships to age, gender and ethnicity. Cephalalgia. 2003;23:519–527. doi: 10.1046/j.1468-2982.2003.00568.x. [DOI] [PubMed] [Google Scholar]
- 13.Hu XH, Markson LE, Lipton RB, Stewart WF, Berger ML. Burden of migraine in the United States: Disability and economic costs. Arch Intern Med. 1999;159:813–818. doi: 10.1001/archinte.159.8.813. [DOI] [PubMed] [Google Scholar]
- 14.Saunders K, Merikangas K, Low NC, Von Korff M, Kessler RC. Impact of comorbidity on headache-related disability. Neurology. 2008;70:538–547. doi: 10.1212/01.wnl.0000297192.84581.21. [DOI] [PubMed] [Google Scholar]
- 15.Brady RO, Barton NW, Grabowski GA. The role of neurogenetics in Gaucher disease. Arch Neurol. 1993;50:1212–1224. doi: 10.1001/archneur.1993.00540110088009. [DOI] [PubMed] [Google Scholar]
- 16.Kessler RC, Shahly V, Stang PE, Lane MC. The associations of migraines and other headaches with work performance: Results from the national comorbidity survey replication (NCS-R) Cephalalgia. 2010;30:722–734. doi: 10.1177/0333102410363766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: Results from the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: Results from the national comorbidity survey replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 19.Kessler RC, Berglund P, Chiu WT, et al. The US national comorbidity survey replication (NCS-R): Design and field procedures. Int J Methods Psychiatr Res. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peterlin BL, Rosso AL, Williams MA, et al. Episodic migraine and obesity and the influence of age, race, and sex. Neurology. 2013;81:1314–1321. doi: 10.1212/WNL.0b013e3182a824f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Proctor BD, Dalaker J. Poverty in the United States: 2001. Washington, DC: U.S. Government Printing Office; 2002. Current population reports. [Google Scholar]
- 22.Jeon-Slaughter H. Economic factors in of patients' nonadherence to antidepressant treatment. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1985–1998. doi: 10.1007/s00127-012-0497-6. [DOI] [PubMed] [Google Scholar]
- 23.Peterlin BL, Nijjar SS, Tietjen GE. Post-traumatic stress disorder and migraine: Epidemiology, sex differences, and potential mechanisms. Headache. 2011;51:860–868. doi: 10.1111/j.1526-4610.2011.01907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lipton RB, Buse DC, Serrano D, Holland S, Reed ML. Examination of unmet treatment needs among persons with episodic migraine: Results of the american migraine prevalence and prevention (AMPP) study. Headache. 2013;53:1300–1311. doi: 10.1111/head.12154. [DOI] [PubMed] [Google Scholar]
- 25.Blumenfeld AM, Varon SF, Wilcox TK, et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: Results from the international burden of migraine study (IBMS) Cephalalgia. 2011;31:301–315. doi: 10.1177/0333102410381145. [DOI] [PubMed] [Google Scholar]
- 26.Seedat S, Lochner C, Vythilingum B, Stein DJ. Disability and quality of life in post-traumatic stress disorder: Impact of drug treatment. Pharmacoeconomics. 2006;24:989–998. doi: 10.2165/00019053-200624100-00006. [DOI] [PubMed] [Google Scholar]
- 27.Karatzias T, Chouliara Z, Power K, et al. Life satisfaction in people with post-traumatic stress disorder. J Mental Health. 2013;22:501–508. doi: 10.3109/09638237.2013.819418. [DOI] [PubMed] [Google Scholar]
- 28.Stewart WF, Lipton RB, Simon D. Work-related disability: Results from the American Migraine Study. Cephalalgia. 1996;16:231–238. doi: 10.1046/j.1468-2982.1996.1604231.x. discussion 215. [DOI] [PubMed] [Google Scholar]
- 29.Dahlof CGH. Benefits of treatment on headache disability-a personal view on selected data. In: Olesen J, steiner TJ, lipton RB, editors. Frontiers in Headache Research: Reducing the Burden of Headache. Oxford University Press; 2003. pp. 27–41. [Google Scholar]
- 30.Lipton RB, Stewart WF, von Korff M. Burden of migraine: Societal costs and therapeutic opportunities. Neurology. 1997;48(Suppl 3):S4–S9. doi: 10.1212/wnl.48.3_suppl_3.4s. [DOI] [PubMed] [Google Scholar]
- 31.Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: Data from the American Migraine Study II. Headache. 2001;41:646–657. doi: 10.1046/j.1526-4610.2001.041007646.x. [DOI] [PubMed] [Google Scholar]
- 32.MacGregor EA, Brandes J, Eikermann A, Giammarco R. Impact of migraine on patients and their families: The migraine and zolmitriptan evaluation (MAZE) survey—Phase III. Curr Med Res Opin. 2004;20:1143–1150. doi: 10.1185/030079904125004178. [DOI] [PubMed] [Google Scholar]
- 33.Winter AC, Berger K, Buring JE, Kurth T. Associations of socioeconomic status with migraine and non-migraine headache. Cephalalgia. 2012;32:159–170. doi: 10.1177/0333102411430854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the United States. Relation to age, income, race, and other sociodemographic factors. JAMA. 1992;267:64–69. [PubMed] [Google Scholar]
- 35.Queiroz LP, Peres MF, Piovesan EJ, et al. A nationwide population-based study of migraine in Brazil. Cephalalgia. 2009;29:642–649. doi: 10.1111/j.1468-2982.2008.01782.x. [DOI] [PubMed] [Google Scholar]
- 36.Stewart WF, Roy J, Lipton RB. Migraine prevalence, socioeconomic status, and social causation. Neurology. 2013;81:948–955. doi: 10.1212/WNL.0b013e3182a43b32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lucchetti G, Peres MF. The prevalence of migraine and probable migraine in a Brazilian favela: Results of a community survey. Headache. 2011;51:971–979. doi: 10.1111/j.1526-4610.2011.01899.x. [DOI] [PubMed] [Google Scholar]
- 38.Molarius A, Tegelberg A, Ohrvik J. Socio-economic factors, lifestyle, and headache disorders— A population-based study in Sweden. Headache. 2008;48:1426–1437. doi: 10.1111/j.1526-4610.2008.01178.x. [DOI] [PubMed] [Google Scholar]
- 39.O'Brien B, Goeree R, Streiner D. Prevalence of migraine headache in Canada: A population-based survey. Int J Epidemiol. 1994;23:1020–1026. doi: 10.1093/ije/23.5.1020. [DOI] [PubMed] [Google Scholar]
- 40.Lipton RB, Bigal ME, Kolodner K, Stewart WF, Liberman JN, Steiner TJ. The family impact of migraine: Population-based studies in the USA and UK. Cephalalgia. 2003;23:429–440. doi: 10.1046/j.1468-2982.2003.00543.x. [DOI] [PubMed] [Google Scholar]
- 41.Warner CH, Warner CM, Appenzeller GN, Hoge GW. Identifying and managing posttraumatic stress disorder. Am Fam Physician. 2013;88:827–834. [PubMed] [Google Scholar]
- 42.Kilpatrick DB, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26:537–547. doi: 10.1002/jts.21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Depression-adjusted Indicators of financial or social burden by migraine and PTSD status.
Supplemental Table 2. Depression-adjusted Employment and medication utilization by migraine and PTSD status.