Abstract
Introduction
Surgical mortality increases significantly with age. Wide variations across hospitals in mortality rates suggest potential levers for improvement. Failure to rescue has been posited as a potential mechanism underlying these differences.
Methods
We performed a review of the literature evaluating surgery, mortality, failure to rescue, and the elderly. We then included a review of ongoing studies and unpublished work aiming to better understand the mechanisms underlying variations in surgical mortality in elderly patients.
Results
Multiple hospital macro system factors, such as nurse staffing, available hospital technology, and teaching status are associated with differences in failure to rescue rates. There is emerging literature regarding important micro system factors associated with failure to rescue. These are grouped into three broad categories, hospital resources, attitudes, and behaviours. On-going work to produce interventions to reduce variations in failure to rescue rates include a focus on teamwork, communication, and safety culture. Researchers are using novel mixed-methods approaches and theories adapted from organizational studies in high reliability organizations in an effort to improve the care of elderly surgical patients
Conclusion
While elderly surgical patients experience failure to rescue events at much higher rates than their younger counterparts, patient level effects do not sufficiently explain these differences. Increased attention on the role of organizational dynamics in the hospitals’ ability to rescue these high risk patients will establish high yield interventions aimed at improving patient safety.
Introduction
Over 45 million patients undergo inpatient surgical procedures every year in the United States.1 Although the large majority of these procedures are associated with minimal risk, intra-abdominal procedures and cardiovascular surgery have substantial risks of morbidity and mortality. At least 100,000 Americans die every year as a direct consequence of surgery. Elderly patients comprise the large majority of these deaths as the risk of perioperative mortality rise exponentially with age. With pancreatectomy, for example, mortality rates increase from 4% in patients under 65, to over 15% in patients 80 years or older.2 Although they account for just over half of all patients undergoing cardiac, vascular, and abdominal surgery, patients over 65 years of age account for 80% of all surgical deaths.3
Wide variation in mortality rates across both hospitals and surgeons suggests that many surgical deaths may be avoidable.4-6 In response, payers, policy makers, and providers have implemented a broad array of quality improvement initiatives. Hospitals are implementing care protocols to minimize unwanted practice variation, mandating the use of checklists and “timeouts” to avoid simple mistakes and improve teamwork in the operating room. They are participating in national outcomes registries, such as the American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP) to benchmark their performance and target their improvement activities.7,8 Payers have established pay for performance programs with incentives for hospitals to be more compliant with evidenced-based prophylaxis against surgical site infections, venous thromboembolism, and cardiac events.9
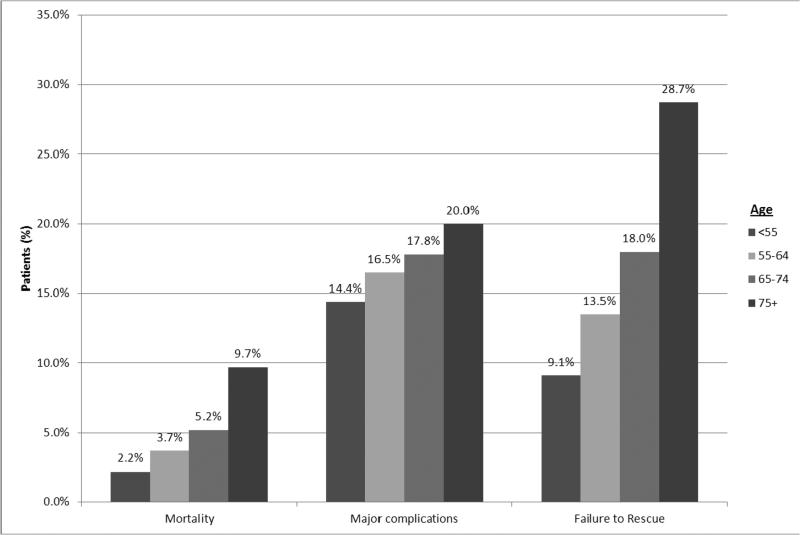
Although their collective impact has yet to be determined, these programs focus primarily on avoiding complications in the first place. While this goal is obviously important, reducing mortality may depend as much on what happens after complications have occurred. While their risks of surgical complications are only slightly higher than those of younger patients, the elderly have markedly higher case fatality rates once a serious complication occurs (Figure 1)—so-called failure to rescue (FTR).10,11 In most instances, perioperative deaths are the culmination of a cascade of discrete clinical events. Patients doing well initially suffer an initial “seminal” complication (e.g., an anastomotic leak after colon surgery), followed by escalation of care (e.g., reoperation, transfer to the intensive care unit) and additional, “domino” complications (e.g., ventilator-acquired pneumonia, acute renal insufficiency). They then experience irremediable complications or multi-system organ failure and succumb.
Figure 1.
FTR by age
Mechanisms underlying FTR in the elderly
Higher FTR rates in the elderly may reflect their diminished physiological reserve for surviving critical illness, which may not be immediately remediable. There is increasing attention being paid to the preparation of surgical patients in the preoperative setting, so-called prehabilitation. This may improve the recovery of elderly patients who do not suffer complications, but the literature is mixed with respect to prevention of morbidity and mortality. With an increase in the use of enhanced recovery pathways in disciplines such as colorectal surgery, the unintended consequences on elderly patients who are not optimized prior to surgery remain to be seen. Therefore, increased focus on the postoperative period and the ability to rebound from complications or hospitals’ ability to rescue elderly patients from major complications is becoming increasingly important.
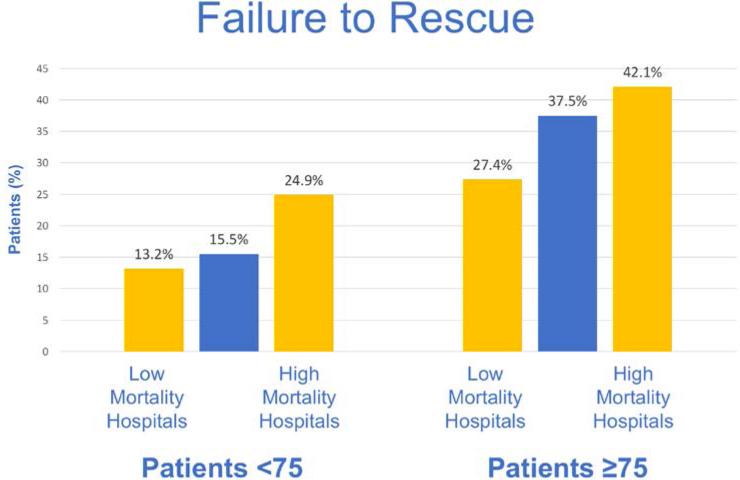
However, higher FTR rates cannot be solely attributed to the patient's age or comorbidities. Some hospitals clearly do better than others in managing complications among elderly patients. Recent research suggests that FTR rates in the elderly vary dramatically across hospitals (Figure 2).10-12 There have been several studies evaluating the availability of macro system hospital resources that account for up to a third of variation in FTR rates across hospitals.13-15 Examples of such resources include hospital bed size, nurse staffing levels, average occupancy, hospital technology, hospital procedural volume, and teaching status. A better understanding of hospital structure at the micro-system level, including details related to intensive care unit (ICU) staffing, physician coverage, and rapid response teams, would be more informative and remain areas of on-going work. The micro-system level where postoperative patients receive their care can be considered in three broad domains: resources, attitudes, and behaviours.
Figure 2.
FTR rates for young (<75 years) and elderly (≥75 years) patients across hospitals ranked by overall mortality. Failure to rescue correlates with mortality and is significantly higher in elderly patients.
Resources
The setting or “context” within which surgical care is delivered is likely a crucial determinant of a hospital's ability to effectively rescue a patient from a major complication. In other words, proficiency with regard to FTR may imply the availability of a requisite level of specific resources. Aiken and colleagues have examined the impact of nurse staffing (both quantity and quality) on inpatient units on both overall surgical mortality and FTR rates.16,17 There have been no studies however assessing the attributes of other clinical micro-systems crucial to the management of patients with complications after surgery, including rapid response teams and intensive care units (ICUs).
Attitudes
The ability of clinical staff to recognize postoperative patients in distress and respond quickly and effectively may be related to the safety culture of the clinical units where surgical care is delivered. Safety culture refers to the shared set of values, beliefs, and behavioural norms that reflect the extent to which caregivers direct their attention and actions towards minimizing patient harm. While safety culture has been studied extensively in other health care contexts, it has not been examined in relation to FTR after inpatient surgery.18-21
Behaviours
A hospital's proficiency with regard to FTR is no doubt influenced by safety-related behaviours of caregivers, as influenced by their attitudes, subjective norms, and perceived control over their environments.22 As summarized later, previous research has linked hospital staff safety organizing behaviours—e.g., collecting, analysing, and disseminating information from errors, proactive checks—to fewer medication errors.23,24 Although relationships between safety-related behaviours and FTR have not been studied, communication patterns and routines among caregivers from the ICU, inpatient wards, and rapid response teams may be critical in the timely detection and effective management of patients with surgical complications.
Despite these findings, there remains a difference in the ability to rescue elderly patients across hospitals with similar resources, attitudes, and behaviours. Therefore, there may be as yet unmeasured factors in how these hospitals utilize available resources to care for elderly adults. Ultimately, improving the proficiency by which hospitals recognize and manage complications in this subgroup of patients may be essential in efforts to reduce surgical mortality in this high-risk population.
Improving FTR in the Elderly
How best to achieve this goal is unclear, however. Successful rescue hinges on early recognition and timely management of serious complications once they occur, particularly during the early “golden hours” of clinical deterioration. Elderly patients appear to deteriorate more quickly and have fewer such “golden hours” to spare. Furthermore, there is a clear association between the type of seminal complication and the rapidity and frequency of an FTR event.12,25 In order to maximize the efficacy of existing resources available to hospitals and its providers in rescuing elderly patients from death, increased attention should be placed on the nuances of interactions between surgical team members in the postoperative setting. As such, on-going work moves beyond simple measurement of available resources to quantitative studies assessing the importance of hospital organizational factors and high-level measures of safety culture. Other organizational factors—including attitudes and behaviours around teamwork and safety—could be even more crucial in minimizing FTR.
While this work will help identify environmental factors associated with effective rescue, a more in depth understanding of interpersonal and interdisciplinary clinical interactions is essential to inform the design and implementation of targeted interventions. For example, the ability of clinical staff to recognize elderly postoperative patients in distress and respond quickly and effectively may be related to the safety culture and safety-related behaviours of the clinical units where surgical care is delivered. A better understanding of these factors and other critical elements, such as effective teamwork and communication, are vital to designing practical and effective interventions for improving rapid rescue, especially in the more vulnerable and frail elderly population. The authors’ research group has on-going work studying unit-level teamwork and other unit and organizational level dynamics underlying variation in FTR rates. Using a mixed methods approach, the key elements or domains of care are studied, with a particular focus on those related to effective multidisciplinary collaboration, such as communication routines, teamwork climate, and safety culture, necessary for complication rescue. (Table 1) This research will culminate in the development of an intervention aimed at promoting these elements and improving patient outcomes.
Table 1.
Relative importance of three key domains contributing to the timely recognition and effective management of complications in general surgical and elderly surgical populations
| Domain | Potential Importance to Rescue | Heightened Importance in Rescue of Elderly Patients |
|---|---|---|
| Communication | Maintaining clear, concise flow of information across care team during “golden hours” of clinical deterioration | Time critical reporting of information across multiple providers within a shortened “golden hour” of deterioration |
| Teamwork | Effective implementation of care protocols in setting of major complications and deference to expertise | Inter-professional management of multiple co-morbidities in conjunction with surgical management of complications |
| Safety Culture | Demonstrating a strong commitment to resilience and preoccupation with failure in order to engage in proactive and pre-emptive analysis and discussion | Heightened awareness amongst team members for the need to adapt, act, and speak up in the setting of impending or on-going crisis given complexities in care of the elderly |
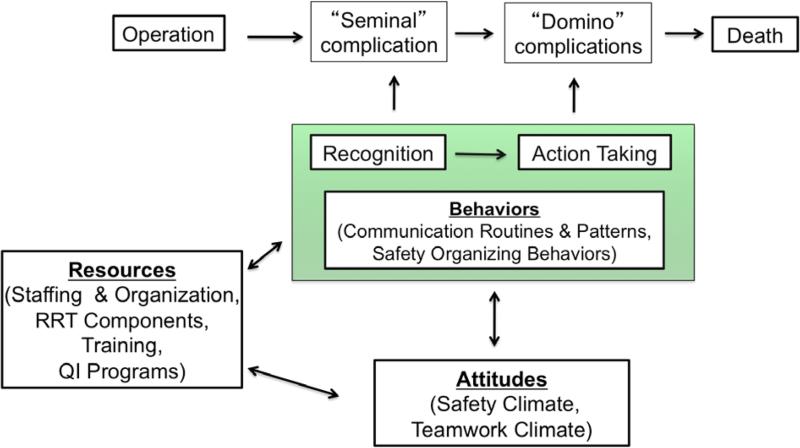
The theory behind such interventions is based on a conceptual model (Figure 3) adapted from work in organizational studies, grounded in the concepts of high reliability organizations26, and informed by the gaps in previous research described above. As noted earlier, most perioperative deaths are the culmination of a cascade of discrete clinical events. The bi-directional arrows in our model represent the critical interactions for successful rescue that remain poorly understood. As such, a clear understanding of the key elements, such as effective teamwork and communication, necessary for early recognition will inform the design of specific interventions aimed at wider implementation and improvement of hospital safety and patient rescue.
Figure 3.
Conceptual model of the organizational dynamics affecting complication rescue.4
Future Directions
The vital ingredients to create an organization that demonstrates the resilience needed to rescue elderly adults from the brink of death do not exist in a vacuum—rather they live in an environment defined by its culture. Healthcare has undergone a massive transformation over the last two decades to flatten the hierarchy in health systems that may have previously led to patient harm. The overwhelming appreciation for the importance of team-based care has led to numerous breakthroughs in patient safety such as tumour boards. However, in the acute care setting, there remains a paucity of data and “know-how” to implementing the optimal team. There is no setting more sensitive or urgent than the elderly patient who develops a major postoperative complication that goes unrecognized due to lapses in communication or provider's unwillingness to see the downward spiral occurring before them. Examples of fostering teams in healthcare through teamwork training include the Agency for Healthcare Research and Quality Team Strategies and Tools to Enhance Performance and Patient Safety (AHRQ TeamSTEPPS) program and the Veteran Affairs Medical Team Training Program. Unfortunately, while these efforts have provided some benefit in closed settings such as the intensive care unit or the operating room, they are one-size fits all approaches to team building. Creation of tailored interventions that account for the differences in hospital resources and personnel will require a fertile environment with buy-in from all stakeholders and a demonstration of a collaborative culture in the organization.
Acknowledgments
Disclosures: Dr. Ghaferi receives research funding from the Agency for Healthcare Research and Quality (K08 HS023621; P30 HS024403), the National Institute of Aging (R01 AG042340), and the Patient Centered Outcomes Research Institute. He also receives salary support from Blue Cross Blue Shield of Michigan as the Director of the Michigan Bariatric Surgery Collaborative. Dr. Dimick receives grant funding from the National Institutes of Health (NIH) and the Agency for Healthcare Research and Quality (AHRQ); and is a co-founder of ArborMetrix, a company that makes software for profiling hospital quality and efficiency.
References
- 1.Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007 summary. National health statistics reports. 2010;1-20:4. [PubMed] [Google Scholar]
- 2.Finlayson E, Fan Z, Birkmeyer JD. Outcomes in octogenarians undergoing high-risk cancer operation: a national study. J Am Coll Surg. 2007;205:729–34. doi: 10.1016/j.jamcollsurg.2007.06.307. [DOI] [PubMed] [Google Scholar]
- 3.Finlayson EV, Birkmeyer JD. Operative mortality with elective surgery in older adults. Eff Clin Pract. 2001;4:172–7. [PubMed] [Google Scholar]
- 4.Ghaferi AA, Dimick JB. Variation in mortality after high-risk cancer surgery: failure to rescue. Surg Oncol Clin N Am. 2012;21:389–95, vii. doi: 10.1016/j.soc.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361:1368–75. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 6.Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009;250:1029–34. doi: 10.1097/sla.0b013e3181bef697. [DOI] [PubMed] [Google Scholar]
- 7.Fink AS, Campbell DA, Jr., Mentzer RM, Jr., et al. The National Surgical Quality Improvement Program in non-veterans administration hospitals: initial demonstration of feasibility. Ann Surg. 2002;236:344–53. doi: 10.1097/00000658-200209000-00011. discussion 53-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall BL, Hamilton BH, Richards K, Bilimoria KY, Cohen ME, Ko CY. Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: an evaluation of all participating hospitals. Ann Surg. 2009;250:363–76. doi: 10.1097/SLA.0b013e3181b4148f. [DOI] [PubMed] [Google Scholar]
- 9.Rosenthal MB, Fernandopulle R, Song HR, Landon B. Paying for quality: providers' incentives for quality improvement. Health Aff (Millwood) 2004;23:127–41. doi: 10.1377/hlthaff.23.2.127. [DOI] [PubMed] [Google Scholar]
- 10.Sheetz KH, Waits SA, Krell RW, Campbell DA, Jr., Englesbe MJ, Ghaferi AA. Improving mortality following emergent surgery in older patients requires focus on complication rescue. Ann Surg. 2013;258:614–7. doi: 10.1097/SLA.0b013e3182a5021d. discussion 7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheetz KH, Guy K, Allison JH, et al. Improving the care of elderly adults undergoing surgery in Michigan. J Am Geriatr Soc. 2014;62:352–7. doi: 10.1111/jgs.12643. [DOI] [PubMed] [Google Scholar]
- 12.Sheetz KH, Krell RW, Englesbe MJ, Birkmeyer JD, Campbell DA, Jr., Ghaferi AA. The importance of the first complication: understanding failure to rescue after emergent surgery in the elderly. J Am Coll Surg. 2014;219:365–70. doi: 10.1016/j.jamcollsurg.2014.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital Characteristics Associated with Failure to Rescue from Complications following Pancreatectomy. J Am Coll Surg. 2010 doi: 10.1016/j.jamcollsurg.2010.04.025. In Press. [DOI] [PubMed] [Google Scholar]
- 14.Wakeam E, Hevelone ND, Maine R, et al. Failure to rescue in safety-net hospitals: availability of hospital resources and differences in performance. JAMA surgery. 2014;149:229–35. doi: 10.1001/jamasurg.2013.3566. [DOI] [PubMed] [Google Scholar]
- 15.Wakeam E, Asafu-Adjei D, Ashley SW, Cooper Z, Weissman JS. The association of intensivists with failure-to-rescue rates in outlier hospitals: results of a national survey of intensive care unit organizational characteristics. J Crit Care. 2014;29:930–5. doi: 10.1016/j.jcrc.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 16.Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational levels of hospital nurses and surgical patient mortality. JAMA. 2003;290:1617–23. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–93. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 18.McKeon LM, Cunningham PD, Oswaks JS. Improving patient safety: patient-focused, high-reliability team training. J Nurs Care Qual. 2009;24:76–82. doi: 10.1097/NCQ.0b013e31818f5595. [DOI] [PubMed] [Google Scholar]
- 19.Sexton JB, Makary MA, Tersigni AR, et al. Teamwork in the operating room: frontline perspectives among hospitals and operating room personnel. Anesthesiology. 2006;105:877–84. doi: 10.1097/00000542-200611000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Sexton JB, Paine LA, Manfuso J, et al. A check-up for safety culture in “my patient care area”. Jt Comm J Qual Patient Saf. 2007;33:699–703, 645. doi: 10.1016/s1553-7250(07)33081-x. [DOI] [PubMed] [Google Scholar]
- 21.Weingart SN, Farbstein K, Davis RB, Phillips RS. Using a multihospital survey to examine the safety culture. Jt Comm J Qual Saf. 2004;30:125–32. doi: 10.1016/s1549-3741(04)30014-6. [DOI] [PubMed] [Google Scholar]
- 22.Ajzen I. The Theory of Planned Behavior. Organ Behav Hum. 1991 Dec;50:179–211. [Google Scholar]
- 23.Vogus TJ, Sutcliffe KM. The impact of safety organizing, trusted leadership, and care pathways on reported medication errors in hospital nursing units. Med Care. 2007;45:997–1002. doi: 10.1097/MLR.0b013e318053674f. [DOI] [PubMed] [Google Scholar]
- 24.Vogus TJ, Sutcliffe KM. The Safety Organizing Scale: development and validation of a behavioral measure of safety culture in hospital nursing units. Med Care. 2007;45:46–54. doi: 10.1097/01.mlr.0000244635.61178.7a. [DOI] [PubMed] [Google Scholar]
- 25.Wakeam E, Hyder JA, Jiang W, Lipsitz SA, Finlayson S. Risk and patterns of secondary complications in surgical inpatients. JAMA surgery. 2015;150:65–73. doi: 10.1001/jamasurg.2014.1795. [DOI] [PubMed] [Google Scholar]
- 26.Weick KE, Sutcliffe KM. Managing the unexpected : assuring high performance in an age of complexity. 1st ed. Jossey-Bass; San Francisco: 2001. [Google Scholar]