Abstract
Objective
New regulations and guidelines require implementation of screening and evidence based psychological treatment (EBT) for cancer patients, but little research exists to assist psychosocial care providers with implementation. This study aimed to develop a conceptual framework for community providers to consider as they embark on implementation of EBTs.
Methods
Full-time psychosocial care providers received training in delivery of a cancer-specific EBT and then received implementation support. Qualitative data were collected in two phases. In Phase I, after training, trainees (N=63) participated in six monthly group conference calls with 6-8 trainees and EBT trainers. Qualitative data from the calls were analyzed using a grounded theory paradigm. In Phase II, the resultant framework was piloted with additional trainees (N=73) during EBT training to prompt early planning for implementation at their home institutions.
Results
In Phase I, themes of “person” (i.e., attitudes, vocalizations, and behaviors of others) and “environment” factors (i.e., material, monetary, and time resources of organizations) affecting implementation emerged. It appeared that both factors influenced how easily barriers could be addressed, though positive person factors also appeared to positively influence environment factors. In Phase II, trainees found the framework acceptable and considered it when generating solutions for implementation challenges.
Conclusions
The framework suggests tailoring implementation efforts to consider person and environment factors. As person support is developed, any resource limitations of the environment may be more easily addressed.
Keywords: cancer, oncology, implementation, barriers, facilitators, evidence-based treatments
Evidence-based psychological treatments (EBTs) exist for addressing the stress, psychological, and quality of life impacts of cancer [1-5], but they have not been widely adopted in the community [6-9]. Dissemination of EBTs to psychosocial care providers and their implementation (DI) in cancer control is in the earliest of stages [10], and policy leaders characterize the process as “stymied,” with little DI research occurring [11]. Nevertheless, the Commission on Cancer of the American College of Surgeons, the accrediting body for the nation's cancer clinics and hospitals, mandated psychosocial screening of all patients, and the American Society of Clinical Oncology published guidelines for screening and treatment – including delivery of EBTs – for depressive and anxiety symptoms in patients [12; 13]. Thus, ready or not, cancer clinics across the country must move toward implementation of EBTs to meet current standards of care.
Background
Several major theories guide DI research. Though they range in scale, specificity, and definition of terms, theorists agree that “context” is important [14-17]. In their Consolidated Framework for Implementation Research, Damschroder and colleagues define context as “the set of circumstances or unique factors that surround a particular implementation effort” [p.3; 17]. Within an institution, context includes such person factors as medical provider attitudes as well as more environmental factors such as staffing levels which contribute to the success or failure of an implementation effort [14-17]. A recent review by Gray, Joy, Plath, and Webb documents 15 categories of contextual barriers and facilitators to implementation, including attitudes toward EBTs, lack of resources, and time constraints [18]. Leaders’ influence or control of contextual factors are often key [14-16; 19; 20]. These theories as well as frameworks such as RE-AIM [21] provide excellent guidance for the evaluation of implementation efforts, but offer little “hands on” guidance to the provider attempting to implement an EBT.
Data on implementation of EBTs for cancer patients are not available, but data on implementation of distress screening may provide insight into the contextual challenges. The literature suggests that health care providers can be resistant to implementation, citing lack of time, impracticality, and belief that a distress assessment is not needed [22-25]. Resources and appropriate staff for addressing psychosocial needs are often lacking [22; 23], and heavy workloads can interfere with referral or follow up [10]. Most centers rely on general operating funds or philanthropic contributions to finance psychosocial support for cancer patients [11], sources vulnerable to institutional changes or external factors, such as an unstable economic climate. Thus, those attempting implementation of an EBT often do so in organizations that may be understaffed, underfunded, or unaware of cancer patients’ psychosocial needs [26].
This study aimed to provide a framework to guide psychosocial providers in community cancer centers planning implementation of EBTs. As part of an ongoing dissemination effort, mental health professionals attended three-day training institutes to learn an evidence-based biobehavioral intervention for reducing stress and improving health outcomes in newly diagnosed cancer patients [27]. Treatment components are stress reduction, disease and treatment information, treatment adherence, seeking information, problem solving, social network identification and support, assertive communication, sexuality, and health behaviors (e.g., diet, exercise, smoking cessation). Training was offered at no cost, and trainees travelling more than 70 miles were offered stipends. As manualized, the group-format intervention consists of 90 minute sessions occurring weekly for 4 months, followed by 8 monthly sessions [28]. Recommended group sizes range from 8-12 individuals with one or two therapists. Trainees were informed that the treatment could be delivered individually and that this was a good strategy to practice content delivery. Data on the efficacy of the training are described elsewhere [see 27]. In brief, multimodal education utilized didactics, structured role-plays, and group discussions, addressing both the delivery of the intervention and its implementation at trainees’ home institutions. Following the institutes, trainees were provided support for implementation via conference calls. Research was conducted in two phases, first developing a conceptual framework of contextual factors which may impact EBT implementation, and second, piloting the framework as a practical aide for subsequent trainees implementing the EBT.
Phase I
Methods
Participants
Trainees from two institutes (N = 63; Cancer to Health, http://cancertohealth.osu.edu) were studied for the development of the framework. They were licensed providers of psychosocial services (44% social workers, 37% psychologists, 5% mental health nurses, 14% other). They were 87% female, 86% Caucasian, and employed full time at National Cancer Institute designated cancer centers (26%) or community hospital cancer programs (26%), with others at freestanding community oncology practices (10%), Veterans Affairs facilities (8%), academic medical centers (5%), community supportive care facilities (5%), or elsewhere (20%) [26].
Procedures
Trainees consented to participating in research and procedures were approved by the Office of Responsible Research Practices. Post-institute, trainees participated in trainer-led conference calls discussing treatment fidelity, adaptation of the treatment to the setting, and implementation (i.e., group problem solving for contextual barriers). Calls were scheduled once a month for six months for small cohorts (5-8 trainees each) with 1-2 trainers and lasted one hour. Trainees attended a median of 3 conference calls each, with 52 (83%) attending at least one call; transcripts were available for 40 calls.
Analytic strategy
The project manager transcribed calls in real time with additions by the trainer conducting the call. An effort was made toward remaining as true to the trainees’ own words as possible, resulting in notes that were near-verbatim. These notes were analyzed qualitatively using grounded theory with the aim of developing a framework of contextual barriers and facilitators [26]. Transcripts were first coded line-by-line for meaning by the first author, with constant comparison among codes. Emerging concepts were identified, described, and labeled until no new concepts were found. These concepts were grouped into interrelated, overarching themes. Themes and the developed framework were discussed with conference call trainers to confirm interpretation of findings. Quotations are provided below to illustrate the findings.
Results
Two themes, those related to “person” and “environment,” emerged during discussions of anticipated implementation. Person factors included attitudes, statements, and behaviors of key individuals in the institution, such as staff responses to new practices, administrators’ opinions, and medical providers’ referrals for treatment. Environment factors were primarily monetary resources currently or potentially available, including funds for materials, personnel and personnel time, and related others. Examples of factor-related problems are provided in Table 1. The factors could range from negative to positive for implementation.
Table 1.
Examples of problems and solutions to implementation of evidence-based treatment described by trainees within the factors of Person and Environment.
| Problems | Solutions | |
|---|---|---|
| Person | Medical providers • Lack knowledge about psychosocial benefits of EBTs • Regard patients' psychosocial needs as met • Feel criticized for not meeting patient psychosocial needs • Forgets or is too busy to refer patients Administrators • Need proof that EBT is valuable/will offer return on investment • Bureaucratic “red tape” • Offer verbal support without taking action |
Medical providers • Present EBT information at staff meetings or rounds • Identify a “champion” supporter to speak with other medical providers • Frame EBT as reducing medical provider burden by managing psychosocial needs • Share empirical evidence for EBT • Share patient testimonials • Build relationships with nurses, patient navigators, support staff, etc. • Link distress screening to referral for EBT • Make referral easier (e.g., provide “prescription pads” to medical providers with EBT information to offer patients) Administrators • Do a business plan including proposed budget and predicted funding/revenue stream • Do a cost/savings analysis • Frame EBT within institutional mission statement, accreditation requirements, etc. • Pilot on small scale to demonstrate EBT benefits • Present program evaluation or patient reported outcome data demonstrating psychosocial needs are unmet • Generate patient demand (“pull”) for EBT through media coverage, community health events • Identify “champion” supporters in key positions to influence adoption |
| Environment | Insufficient funds or resources for: • Therapist time • Support staff • Space • EBT materials (e.g., manuals) • Marketing the EBT |
• Seek grants from community organizations, national philanthropic groups, etc. • Seek donations from community members, businesses, organizations • Hold fundraisers • Offer a plan for reallocating existing resources • Bill for EBT provision • Use interns, residents, other trainees as support personnel • Seek volunteers for support tasks • Partner with internal or external organizations for supplies, staff, space, etc. • Barter for resources in exchange for services |
Person factors
Negative
Resistance from medical providers was common. Ten of fifty-two trainees discussed concerns that medical providers would not refer patients to the EBT. Trainees often attributed this to misunderstanding of the purpose or benefits of the EBT.
[Physicians] feel like they’re taking care of the whole patient, so why would they need to refer them on to somebody else for support? ... So they feel like they’re addressing all their patients’ needs ... in a 15 minute visit ... they’re addressing you know, depression, anxiety, they’re addressing the physical symptoms.
Opposition also came from administrators, such as concerns about funding a new program. Seventeen of fifty-two trainees discussed problems with administrators, bureaucracy, and organizational politics. Some administrators cited concerns that the intervention would not serve all patients equally:
Their concern is that they consider it “elitist.” Say 10 folks sign up for a group [treatment]; we’re only reaching 10 people. I had to explain recruiting, multiple groups, etc. To do multiple groups is not that difficult. But they see it as a problem, a big problem. They see the piece-meal groups [i.e., open support groups or 1 hour psychoeducation workshops] [as doing] it all, and then don’t know why we would only reach 10 people.
Others called for a pilot intervention including less EBT material and fewer sessions (i.e., reducing treatment fidelity) to demonstrate the feasibility of implementation, but trainees worried that reducing fidelity would dilute the empirically demonstrated effects and produce poorer outcomes than the full treatment. Some administrators simply did not believe that implementation of the EBT would serve the goals of their institution or found it to be of a much lower priority than other institutional goals. In such cases, trainees were often unable to proceed with implementation.
Neutral
Other trainees described indifference from administrators, medical providers, and other important people in the organization, leaving implementation solely to the trainee:
On one hand [the administrators] want me to do anything [services for patients] that I want to do. On the other hand, if we had zero services ... that would be ok for them, too.
In some cases, there was no opposition per se, but implementation was made difficult because of institutional upheaval (e.g., hospital reorganization), which might result in support staff being moved to other projects, personnel leaving, or threats to job security. Fourteen trainees discussed such changing person factors:
There have been a lot of institutional and structural changes going on here. It didn’t really allow us to start marketing a new program with all sorts of layoffs and such happening ... No one in our support program was laid off, but there were some advocates [i.e., champions] for our program who were. It made it a little bit scary. Those in power who had some [influence] had been laid off. We were really left on our own at that point.
Although institutional flux made implementation nearly impossible, some reappraised this situation positively:
I think that the institutional changes are still happening ... There are a lot of new faculty and oncologists ... it may be a new start for us. Think about how our practice may mold well with the new practitioners ... Perhaps we can get the new oncologists to start referring to the program, increase the participation.
Thus, trainees recognized that implementation might be impossible during institutional reorganization, but that the period following these changes might offer them new and perhaps better opportunities to implement the EBT.
Positive
Some who were in favor of the new program, “champions,” took action to make implementation happen:
[We have] several oncologists in favor of this [the EBT]. Nurses are starting to see patients at diagnosis, sometimes going with them to other appointments. They’re now introducing them to the [EBT] via flyer or postcard.
Administrative leadership made a significant difference in moving implementation forward:
Our cancer director is all about it. ... About 6 months before the [training] institute, they finalized an agreement between our agencies that [mental health providers] would be more available to the cancer center. If they refer patients to us, we would be able to do same-day services. When I went to the institute and contacted them with the [treatment] info, the hospital was all for it. ... The physicians had actually been asking when we could start.
Often such supporters removed environment barriers, as described below.
Environment factors
Negative
The 14 trainees above who discussed the person impacts of institutional change also discussed consequent environment resource impacts. Institutions often cut budgets or reorganized due to the difficult economic climate (i.e., recession) during the time of this study. These changes sometimes resulted in the loss of resources for implementation:
I had staff working on the [administrative approvals] for me, and they were taken away from me. ... I have not had time to recover yet and fix the application ... it has been difficult getting things nailed down there, not in a clinical way but more so in an administrative way, [such as] filling staff [positions].
Such losses forced trainees to spend more of their own time and effort on implementation, sometimes delaying it indefinitely. In an example of the interaction of person and environmental factors, even when trainees presented solutions to environment barriers, it did not always convince others:
They see barriers; I just try to give solutions to the barriers. I think it's foreign [to them]. They don’t understand what group [psychological treatments] are about. Maybe the idea of just having them see it in action and taking baby steps is the best thing to do.
Thus, despite trainees’ proposed solutions to environmental barriers (i.e., lack of funding), administrators were sometimes unwilling or unable to prioritize a new EBT offering in the face of financial limitations.
Neutral
In most cases, at least some environment resources existed, although they might be in high demand:
Well, it's outpatient and staff time. We do a number of [mental health] programs here. ... So we just need to make sure that we have space available at the facility, and then staff time so it's not overlapping with another population, and then have enough time for marketing.
Access to resources was not guaranteed, but trainees recognized that most could be procured with funding from internal or external sources with the support of important others:
Financial will be the biggest problem for us. ... [We’re looking for] departmental funding from oncology or going to our fund or going to donors. ... It's not enthusiasm or interest, that's all there. It's more about funding, getting those pieces together.
Conversely, when some resources were available but direct supervisors – though verbally supportive – did not assist trainees in redistributing their workloads, trainees struggled to fit necessary implementation work into their days:
Anything created in psychosocial falls on me – I am the sole [mental health] provider here ... If there were more of me, it would be easy. ... Basically it's my workload. There is very little wiggle room.
One commonly cited barrier, even when most environmental resources were available, was the chronic problem for patients of parking costs; 4/52 trainees discussed this concern specifically, while eight others discussed their inability to assist with patient transportation difficulties. When institutions did offer parking vouchers, they were exclusively for medical, not psychosocial appointments, and trainees’ departments could not mitigate these costs:
It's hard to get people to come back for a group to my location because there are parking hassles, there's a fee for parking ... there are issues of inconvenience that make it really difficult when somebody's going through their medical treatment.
Thus, implementation could be difficult due to key missing environmental factors, even when most environmental resources and some person support were in place.
Positive
There were notable examples of environment support being high. For example, some institutions already offered psychosocial services at no cost to patients:
We're not running into the same logistical issues. We don’t bill [for mental health services] so it's not necessarily taking away any of my work time because [the treatment] is during normal hours.
Trainees at institutions with many resources also identified existing personnel such as patient navigators who directed patients to appropriate services, experts on relevant topics unique to this intervention (e.g., dieticians) who could assist, spaces in which to meet with patients, and others.
In another example of the relationship between person and environment resources, when trainees had leadership advocating for the program, environment barriers rarely arose. One trainee described having to do little, as the administration fully supported implementation:
They're actually having a meeting ... to talk about getting the group [treatment] started, there's pretty significant interest in terms of finding funding for it and figuring it out. ... The meeting is with the heads of the center including the physicians and so there should be some direct referral resource there ... The Vice President of behavioral health ... kind of jumped all over the group [treatment] thing.
Thus, trainees with high positive person support might be provided the needed resources with very little effort on their part.
Summary
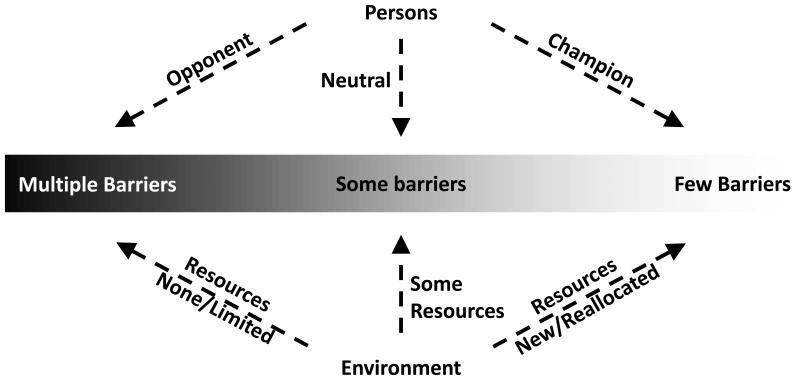
Figure 1 provides a representation of the findings. Trainees generally discussed both factors, and both influenced the ease of implementation. Positive person support appeared to help trainees generate both further person support and environmental support, whereas increasing environmental resources did not appear to convince more key individuals to support implementation. Environmental barriers could be overcome using resource-focused solutions as well, such as applying for grants (see Phase II). Thus, our Phase I findings suggested targeting person support first to mitigate and address multiple barriers.
Figure 1.
Person and environment effects on ease of implementation.
In some cases, such as organizations undergoing significant changes or with very few resources overall, implementation efforts were understandably stymied. Administrators’ priorities or flexibility in distributing resources in such cases might be restricted by the economic situations of their environments. The bottom line for our trainees, however, was that the administration did not (or could not) support their implementation plans. When confronted with such barriers, some trainees found it best to wait for conditions to change before attempting implementation.
Phase II
Methods
Participants
The framework was piloted with trainees (N = 73) from three subsequent institutes. They were licensed mental health professionals (41% social workers, 36% psychologists, 1% mental health nurses); four psychology post-doctoral fellows, not yet licensed, were also included. The group was 90% female and 77% Caucasian, employed full time at National Cancer Institute designated cancer centers (30%) or community hospital cancer programs (25%), with others at Veterans Affairs facilities (8%), community supportive care facilities (12%), academic medical centers (12%) or elsewhere (13%).
Procedures
Trainees were introduced to the framework on day one of the three-day institute. They completed a self-evaluation survey of their home institution, rating the likely availability of person support and environment support for EBT implementation on two visual analogue scales with 0 and 100 anchors. Expected patient barriers were also assessed on a visual analogue scale. Item texts, means, and standard deviations of trainee ratings may be found in Table 2. Two trainers visually compared ratings and placed 4-6 trainees with similar needs into a group: one focused on person factors, two focused on environment factors, and one focused on patient factors. Four trainers led each hour-long problem solving discussions with 6-8 trainees aimed at increasing support or reducing barriers in their assigned category. Discussions were video recorded and transcribed verbatim.
Table 2.
Visual analogue scale items, means, and standard deviations
| M | SD |
|---|---|
| Person support: Attitudes that important others in your institution have about offering psychological interventions in general or this intervention specifically. Think about the key decision makers in your organization. For example: How supportive do you think your supervisor would be in implementing this intervention? How supportive are the cancer health providers in referring patients for your services? How supportive is the leader of the oncology department in participating in psychological interventions? Rate how much person support you have for implementation. (Range: “Total opposition from everyone” to “total support from everyone.”) | |
| 68.93 | 22.56 |
| Environmental support includes tangible needs like a room in which to run the group, funding for your time and supplies, and staff to help you implement the intervention. Think about the resources at your institution. For example: What space will you use to conduct the group? How will your time to conduct the group be funded? How will the patient materials be made available to patients? Rate how much environmental support you have for implementation. (Range: “No resources at all” to “all the resources I need.”) | |
| 60.42 | 28.42 |
| Patient barriers prevent your patients from receiving services. They include cultural attitudes about mental health treatment, willingness to commit to treatment, and transportation needs. Think about the population you serve. For example: How accepting are your patients of mental health treatment? How likely is it that your patients would commit to a multi-session intervention? What transportation barriers do your patients have in order to attend a multi-session intervention? Rate your patients’ ability and willingness to attend. (Range: “Patients can't and won't attend” to “patients will be at every session”) | |
| 46.57 | 21.74 |
Analytic strategy
Transcripts of group discussions were analyzed using the same methods described above to determine whether similar categories of anticipated or experienced problems emerged, whether trainees found the framework acceptable, and whether their generated solutions aligned with the framework. Representative quotes are provided.
Results
As described above, four small groups were formed on the basis of trainee reported contextual support at each institute. Led by a trainer, trainees first defined the “problem” (i.e., how implementation would occur at their institutions), enumerated anticipated difficulties, and then brainstormed for potential solutions. Exemplar problems and solutions for both person and environmental factors are provided in Table 1.
Those with environmental support needs often worried about their workload, and this problem was representative of how trainees discussed environmental barriers. Several trainees suggested finding interns or students who could gain experience while supporting EBT delivery. One trainee suggested exchanging services between institutions and departments:
When I was in a nonprofit, we always bartered. You know, call up this agency and say hey, I could provide this, can you provide that? We exchange services and staff and personnel resources.
Both groups assigned to discuss environment factors came to the conclusion that many of their needs could be met by garnering funding for implementation, such as through billing patients for services or applying for small community grants. Trainees’ solutions were often first aimed at generating person support as a step to obtain environmental resources:
My mind goes immediately to focusing on the money, then. Because that solves a lot of these [environmental problems], if you have financing for it ... How can I implement this and get someone else who would be happy to have their money go to a good cause?
In fact, all groups generated solutions such as presenting EBT information at medical provider and administrator meetings to garner person support. Trainees suggested that medical and administrative leaders who supported implementation could help with both person and environment barriers. They generated several ways to market the EBT to medical providers who might believe the EBT unnecessary:
Well, I think you have to be somewhat of a salesman. And so if the physician says to you, “well I’m already [providing psychosocial care].” well, agree with them. ... But then sell it as a vehicle to sort of streamline all of what he's doing already ... Or [explain that it will] take away some of their work.
Another trainee suggested:
[Tell them] that [the EBT] might increase – get him more business, increase his referrals. Give him a better name.
Trainees also planned on selecting medical providers who might, in turn, convince others:
Strategically pick a physician that you have a good relationship with, and sit down and sell it to him. Almost in an – I don't want to say informal manner – but just convey to him that you have something that you think he would agree to.
Conclusions
A grounded theory paradigm was used to develop a conceptual framework of factors relevant to planning EBT implementation. Data came from full time psychosocial care providers employed in facilities ranging from comprehensive cancer centers to freestanding non-profits. Qualitative data from Phase I resulted in a framework anchored by factors of person and environment, both of which could range from negative to positive. Person factors are attitudes, statements, and behaviors of others in the institution, whereas environment factors are material, personnel, and related fiscal resources of the organization. The factors could interact, with positive person support helping providers with environmental resources and negative person support reducing their access to environmental resources.
For Phase II, a second sample of psychosocial providers were presented the framework in small group problem solving discussions aimed at garnering support and reducing barriers in person, environment, and patient domains. Their solutions supported the conceptual framework in that garnering person support was suggested as a way to address both person and environment barriers in addition to solutions generated within each factor. This test suggested the framework could be used as a practical representation for psychosocial care providers to think about and generate strategies to address implementation challenges.
For researchers attempting to disseminate EBTs to the community, providing this framework when offering EBT trainings may be useful for psychosocial care providers as they move from learning to doing. At its core is the idea that, while context as a whole is important, achieving person support may be key. When most others in the institution are eager to see implementation succeed (i.e., high positive person factors), their support may be leveraged. When most others are opposed to implementation (i.e., high negative person factors), they may create barriers by persuading others to oppose implementation, blocking the use of resources, or refusing to provide necessary administrative approvals, for example. While opponents are unlikely to become supporters, the psychosocial care provider's verbal persuasion or actions might change their attitudes to non-obstructive indifference. Others who are indifferent may be ones that the psychosocial care provider could influence to be supportive. It may also help providers to consider implementation feasibility. If opponents have staunch opinions or see the EBT as not directly relevant to the goals or mission of the organization, persuasion may not be sufficient for substantive change.
Contributions of the framework notwithstanding, we note strengths and limitations of the study. Psychosocial care providers applying to the training institutes attested to interest in learning a specific EBT. The providers were multidisciplinary, came from across the country, and were employed in a range of public and private facilities. Support letters from a supervisor or administrator were requested to provide early institutional awareness of the EBT implementation. The data is thus from motivated providers of the particular EBT who had at least a minimum level of organizational awareness of the EBT opportunity. Lastly, some trainees discussed general patient barriers to treatment, but the institute focused predominantly on barriers to implementation of EBTs. The framework does not address patients, but presumably many barriers could be addressed by considering the person and environment factors solutions such as those provided in Table 1. For example, medical providers could assist in mitigating transportation difficulties by joint scheduling of EBT and oncology visits.
Delivering EBTs to patients who need them is a central problem in psychosocial oncology that cannot be solved without systematic DI efforts [18], yet the most effective means of implementation remain unclear. Our results reinforce prevailing theoretical models in emphasizing context and organizational leadership as determinants of implementation success [12-15]. While previous work has noted the importance of these factors in implementing mental health treatments [27-30] and distress screening [19-22] for cancer patients, this study is the first to our knowledge to consider context in the implementation of a cancer-specific EBT. Our findings explicitly place the support or opposition of others at the forefront. The framework clarifies the context of implementation, the person and environment circumstances which may pose barriers, and provides examples of strategies to address them. It offers a practical framework for psychosocial oncology providers to conceptualize and plan efforts to move EBTs into their clinical practice.
Acknowledgements
This work was supported by funding from the National Institutes of Health National Cancer Institute (CA163917, CA098133). The authors thank the remaining trainers of the institutes (Drs. Kristen Carpenter, Georita Frierson, Rebecca Shelby, and Lisa Thornton), the provider trainees who made this study possible, Kyle Patterson for call transcription, and the Stress and Immunity Cancer Project research staff and graduate students who provided ongoing assistance.
Footnotes
The authors report no conflicts of interest.
References
- 1.Badr H, Krebs P. A systematic review and meta-analysis of psychosocial interventions for couples coping with cancer. Psycho-Oncology. 2013;22(8):1688–1704. doi: 10.1002/pon.3200. doi: 10.1002/pon.3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Faller H, Schuler M, Richard M, Heckl U, Weis J, Küffner R. Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: Systematic review and meta-analysis. Journal of Clinical Oncology. 2013 doi: 10.1200/JCO.2011.40.8922. doi: 10.1200/jco.2011.40.8922. [DOI] [PubMed] [Google Scholar]
- 3.Hart SL, Hoyt MA, Diefenbach M, Anderson DR, Kilbourn KM, Craft LL, Stanton AL. Meta-analysis of efficacy of interventions for elevated depressive symptoms in adults diagnosed with cancer. Journal of the National Cancer Institute. 2012;104(13):990–1004. doi: 10.1093/jnci/djs256. doi: 10.1093/jnci/djs256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Piet J, Wurtzen H, Zachariae R. The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: a systematic review and meta-analysis. Journal of Consulting and Clinical Psychology. 2012;80(6):1007–1020. doi: 10.1037/a0028329. doi: 10.1037/a0028329. [DOI] [PubMed] [Google Scholar]
- 5.Sheinfeld Gorin S, Krebs P, Badr H, Janke EA, Jim HSL, Spring B, Jacobsen PB. Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. Journal of Clinical Oncology. 2012 doi: 10.1200/JCO.2011.37.0437. doi: 10.1200/jco.2011.37.0437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chambers SK, Girgis A, Occhipinti S, Hutchison S, Turner J, Morris B, Dunn J. Psychological distress and unmet supportive care needs in cancer patients and carers who contact cancer helplines. European Journal of Cancer Care. 2012;21(2):213–223. doi: 10.1111/j.1365-2354.2011.01288.x. doi: 10.1111/j.1365-2354.2011.01288.x. [DOI] [PubMed] [Google Scholar]
- 7.Fallowfield L, Ratcliffe D, Jenkins V, Saul J. Psychiatric morbidity and its recognition by doctors in patients with cancer. British Journal Of Cancer. 2001;84(8):1011–1015. doi: 10.1054/bjoc.2001.1724. doi: 10.1054/bjoc.2001.1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Passik SD, Dugan W, McDonald MV, Rosenfeld B, Theobald DE, Edgerton S. Oncologists’ recognition of depression in their patients with cancer. Journal of Clinical Oncology. 1998;16(4):1594–1600. doi: 10.1200/JCO.1998.16.4.1594. [DOI] [PubMed] [Google Scholar]
- 9.Werner A, Stenner C, Schüz J. Patient versus clinician symptom reporting: how accurate is the detection of distress in the oncologic after-care? Psycho-Oncology. 2012;21(8):818–826. doi: 10.1002/pon.1975. doi: 10.1002/pon.1975. [DOI] [PubMed] [Google Scholar]
- 10.Pollack LA, Hawkins NA, Peaker BL, Buchanan N, Risendal BC. Dissemination and translation: A frontier for cancer survivorship research. Cancer Epidemiology Biomarkers & Prevention. 2011;20(10):2093–2098. doi: 10.1158/1055-9965.EPI-11-0652. doi: 10.1158/1055-9965.epi-11-0652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alfano CM, Smith T, de Moor JS, Glasgow RE, Khoury MJ, Hawkins NA, Leach CR. An action plan for translating cancer survivorship research into care. Journal of the National Cancer Institute. 2014;106(11) doi: 10.1093/jnci/dju287. doi: 10.1093/jnci/dju287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American College of Surgeons Commission on Cancer . Cancer program standards 2012: Ensuring patient-centered care. American College of Surgeons; Chicago, IL: 2012. [Google Scholar]
- 13.Andersen BL, DeRubeis RJ, Berman BS, Gruman J, Champion VL, Massie MJ, Somerfield MR. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: An American Society of Clinical Oncology guideline adaptation. Journal of Clinical Oncology. 2014;32(15) doi: 10.1200/JCO.2013.52.4611. JCO. 2013.2052. 4611. doi: 10.1200/JCO.2013.52.4611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aarons GA, Horowitz JD, Dlugosz LR, Ehrhart MG. The role of organizational processes in dissemination and implementation research. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. Oxford University Press; New York: 2012. pp. 128–153. [Google Scholar]
- 15.Rycroft-Malone J. The PARIHS Framework—A framework for guiding the implementation of evidence-based practice. Journal of nursing care quality. 2004;19(4):297–304. doi: 10.1097/00001786-200410000-00002. doi: 10.1097/00001786-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Shoenwald SK, McHugh RK, Barlow DH. The science of dissemination and implementation. In: McHugh RK, Barlow DH, editors. Dissemination and Implementation of Evidence-Based Psychological Interventions. Oxford University Press; New York: 2012. pp. 16–42. [Google Scholar]
- 17.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science. 2009;4(1):50. doi: 10.1186/1748-5908-4-50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gray M, Joy E, Plath D, Webb SA. Implementing evidence-based practice: A review of the empirical research literature. Research on Social Work Practice. 2013;23(2):157–166. doi: 10.1177/1049731512467072. [Google Scholar]
- 19.Aarons GA. Transformational and transactional leadership: Association with attitudes toward evidence-based practice. Psychiatric services. 2006;57(8):1162–1169. doi: 10.1176/appi.ps.57.8.1162. doi: 10.1176/appi.ps.57.8.1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aarons GA, Sommerfeld DH. Leadership, innovation climate, and attitudes toward evidence-based practice during a statewide implementation. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(4):423–431. doi: 10.1016/j.jaac.2012.01.018. doi: 10.1016/j.jaac.2012.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health. 1999;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dudgeon D, King S, Howell D, Green E, Gilbert J, Hughes E, Sawka C. Cancer Care Ontario's experience with implementation of routine physical and psychological symptom distress screening. Psycho-Oncology. 2012;21(4):357–364. doi: 10.1002/pon.1918. doi: 10.1002/pon.1918. [DOI] [PubMed] [Google Scholar]
- 23.Riblet N, Skalla K, McClure A, Homa K, Luciano A, Davis TH. Addressing distress in patients with head and neck cancers: A mental health quality improvement project. Journal of the National Comprehensive Cancer Network. 2014;12(7):1005–1013. doi: 10.6004/jnccn.2014.0097. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell AJ, Lord K, Slattery J, Grainger L, Symonds P. How feasible is implementation of distress screening by cancer clinicians in routine clinical care? Cancer. 2012;118(24):6260–6269. doi: 10.1002/cncr.27648. doi: 10.1002/cncr.27648. [DOI] [PubMed] [Google Scholar]
- 25.Absolom K, Holch P, Pini S, Hill K, Liu A, Sharpe M, Palliative Care Research, C The detection and management of emotional distress in cancer patients: the views of health-care professionals. Psycho-Oncology. 2011;20(6):601–608. doi: 10.1002/pon.1916. doi: 10.1002/pon.1916. [DOI] [PubMed] [Google Scholar]
- 26.Juliet Corbin AS. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 3rd ed. SAGE Publications, Inc.; Thousand Oaks, CA: 2008. [Google Scholar]
- 27.Brothers BM, Carpenter KM, Shelby RA, Thornton LM, Frierson GM, Patterson KL, Andersen BL. Dissemination of an evidence-based treatment for cancer patients: Training is a necessary first step. Translational behavioral medicine. 2014 doi: 10.1007/s13142-014-0273-0. doi: 10.1007/s13142-014-027/3-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Andersen BL, Golden-Kreutz DM, Emery CF, Thiel DL. Biobehavioral Intervention for cancer stress: Conceptualization, components, and intervention strategies. Cognitive and Behavioral Practice. 2009;16(3):253–265. doi: 10.1016/j.cbpra.2008.11.002. [Google Scholar]
- 29.Ekehammar B. Interactionism in personality from a historical perspective. Psychological Bulletin. 1974;81(12):1026–1048. doi: 10.1037/h0037457. doi: 10.1037/h0037457. [DOI] [PubMed] [Google Scholar]