Abstract
Variability of heat stress illness (HSI) by urbanicity and climate region has rarely been considered in previous HSI studies. We investigated temporal and geographic trends in HSI emergency department (ED) visits in CDC Environmental Public Health Tracking Network (Tracking) states for 2005–2010. We obtained county-level HSI ED visit data for 14 Tracking states. We used the National Center for Health Statistics Urban-Rural Classification Scheme to categorize counties by urbanicity as 1) large central metropolitan (LCM), 2) large fringe metropolitan (LFM), 3) small–medium metropolitan (SMM), or 4) nonmetropolitan (NM). We also assigned counties to one of six US climate regions. Negative binomial regression was used to examine trends in HSI ED visits over time across all counties and by urbanicity for each climate region, adjusting for pertinent variables. During 2005–2010, there were 98,462 HSI ED visits in the 14 states. ED visits for HSI decreased 3.0 % (p < 0.01) per year. Age-adjusted incidence rates of HSI ED visits increased from most urban to most rural. Overall, ED visits were significantly higher for NM areas (IRR = 1.41, p < 0.01) than for LCM areas. The same pattern was observed in all six climate regions; compared with LCM, NM areas had from 14 % to 90 % more ED visits for HSI. These findings of significantly increased HSI ED visit rates in more rural settings suggest a need to consider HSI ED visit variability by county urbanicity and climate region when designing and implementing local HSI preventive measures and interventions.
Keywords: Heat illness, Emergency department, Urbanization, Metropolitan, Nonmetropolitan, Time trend
Introduction
The relationship between environmental exposure to extreme heat and mortality is well established [1, 2]. An increasing number of studies have also established a link between extreme heat and morbidity. Periods of extreme heat are often followed by increases in all-cause hospitalizations [3]; cause-specific hospitalizations, such as renal [3–5], respiratory [3, 4, 6–8], and cardiovascular diseases [4, 5, 7]; mental health issues [4]; and heat-related illness, also known as heat stress illness (HSI) [4, 5, 8, 9]. HSI includes various heat-related disorders, ranging from heat cramps (most mild) and heat syncope to heat exhaustion and heat stroke (most severe) [10].
Heat-related morbidity is an emerging public health concern. Research has focused on risk factor analyses and recommendations for preventive measures and interventions. Previous studies have identified groups at increased risk for HSI or heat-related death from extreme heat exposures [5, 9, 11–19]. These include the elderly, the very young, men, populations without access to air conditioning, persons with chronic medical problems, and those taking certain medications. Although these groups are at higher risk, any person can develop HSI following extreme heat exposure, and prevention is the most effective intervention against HSI [10]. Because the Intergovernmental Panel on Climate Change projects that more frequent, more intense heat waves will occur over a wider geographic area due to climate change [20], public health preventive measures and interventions to protect populations from HSI might become even more important and relevant in the coming decades and beyond.
Many locales that have experienced substantial mortality and morbidity from heat waves have developed community warning systems and heat emergency response plans to prepare for future extreme heat emergencies [21–25]. Response plans that consider at-risk persons, integrate meteorological information, and promote individual protective behaviors are likely to be effective in reducing heat-related morbidity and mortality [26]. However, locally tailored intervention strategies are needed. Climate change is projected to produce extreme heat events at varying spatial scales, and affected communities may increasingly vary by demographics, climate, and geography [20, 26].
One local factor rarely considered in HSI studies is county urbanicity (i.e., urban–rural classification). Many prevention efforts included in community preparation and response plans that are aimed at reducing HSI have been developed for urban settings [26]. However, two recent studies, one focusing on North Carolina [9] and the other using a sample of US hospital-based emergency departments (EDs) participating in the Healthcare Cost and Utilization Project [15], have found higher ED visit rates in rural counties than in urban counties. HSI encompasses many clinical outcomes that often are severe enough to warrant treatment (e.g., hyperthermia, heat exhaustion, and heat stroke) [10]. Consequently, EDs provide a valuable source of HSI data that can be consistently tracked across space and time for heat-related health surveillance [5, 27]. County-level data on monthly number of HSI ED visits (for May through September) are available from the Centers for Disease Control (CDC) National Environmental Public Health Tracking Program (Tracking Program), allowing for multi-state, multi-region trend analyses over time [28].
The objectives of this study were to describe temporal and geographic trends in HSI ED visits and describe variability by urbanicity, overall and by US climate region. Understanding how HSI ED visits have changed over time and vary by geography can help guide decisions about how HSI prevention measures and intervention strategies could be modified based on regional characteristics, local demographics, and urbanicity.
Methods
Data Sources
The Tracking Program receives data from 18 states for HSI ED visits occurring May 1 through September 30. We obtained county-level monthly HSI ED visit counts for 2005–2010 by sex and age group from the 14 states that had complete data [29]. Those states were California, Connecticut, Florida, Iowa, Maine, Massachusetts, Minnesota, Missouri, New Jersey, New York, South Carolina, Utah, Vermont, and Wisconsin. The remaining 4 states were missing one or more years of HSI ED visit data from 2005–2010 and were therefore not included in analysis. The data included ED visits occurring May 1 through September 30 for each year 2005–2010, having any International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code in the range of 992.0–992.9 (effects of heat and light) or cause of injury code E900.0 (excessive heat due to weather conditions) or E900.9 (excessive heat of unspecified origin), excluding ED visits with a code of E900.1 (heat of man-made origin), listed as the primary or any other diagnosis. Age was categorized as 0–4, 5–14, 15–34, 35–64, and ≥65 years. County population data were obtained from the US Census Bureau via the Tracking Program. Intercensal estimates were used for 2005–2009, and the decennial censal estimate was used for 2010 [30].
We used the National Center for Health Statistics (NCHS) 2013 Urban–Rural Classification Scheme for Counties as the measure of county urbanicity. This scheme is the only nationally consistent urban–rural classification that separates counties in metropolitan statistical areas (MSAs) of 1 million or more in population into two groups shown to vary in some measures of health status; the division is based on the containment of, or being contained by, the population of the largest principal city in the MSA [31]. The classification scheme was downloaded from the CDC website [32], and the six NCHS urban–rural categories were collapsed into four categories: large central metropolitan (LCM), large fringe metropolitan (LFM), small–medium metropolitan (SMM), and nonmetropolitan (NM).
Data on annual percent of people in poverty by county were obtained from the US Census Bureau American Community Survey via the Tracking Program for 2005–2010 [33].
Climate region classification was obtained from the National Oceanic and Atmospheric Administration (NOAA) National Climatic Data Center’s US Climate Regions map. The map delineates nine regions of the contiguous US that are each climatically consistent [34, 35].
Hourly meteorological predictions from the North American Land Data Assimilation System Phase 2 (NLDAS) model [36], available at 0.125 degrees grid resolution, were made available to the Tracking Program as part of an interagency agreement between CDC and National Aeronautics and Space Administration. We used a multi-stage geo-imputation approach to convert grid-level meteorological data to county-level estimates. We first calculated the population within each NLDAS grid cell using 2010 population estimates by US Census blocks. We then converted NLDAS grid polygons with population information to centroids and related all the grid cell centroids to the counties in the conterminous US based on a containment relationship. If a county did not have a grid cell centroid within its boundary, we assigned a grid cell centroid closest to the county boundary. Finally, we created a population-weighted average from all the grid cell centroids to obtain county-level estimates of daily maximum heat index using temperature and relative humidity information [37]. We used the daily estimates to calculate the county-level monthly mean maximum heat index in degrees Fahrenheit for May–September, 2005–2010.
The final urban–rural classification, annual percent of people in poverty, climate region, and monthly mean maximum heat index were merged with the ED visit data by state and county Federal Information Processing Standard codes.
Analyses
We used population data from the US Census Bureau to calculate crude incidence rates of HSI ED visits per 100,000 population. Age-adjusted incidence rates were calculated by the direct method using weights from the 2000 US standard population [38] and 18 age groups defined by the World Health Organization [39].
For temporal and geographic trends, we made univariate regression models for month, year, sex, age group, county urbanicity, percent of people in poverty, climate region, and monthly mean maximum heat index as predictors of number of monthly ED visits by county. We used variables significantly associated (at the p = 0.05 level) with number of monthly HSI ED visits on univariate analyses to construct multivariable regression models. The models were used to examine temporal and geographic trends in the number of monthly HSI ED visits at the county level. For temporal trends, we examined monthly and yearly trends across all counties, adjusting for sex, age group, urbanicity, poverty, climate region, and monthly mean maximum heat index. We also examined geographic trends by urbanicity for each climate region, adjusting for month, year, sex, age group, poverty, and monthly mean maximum heat index.
Rate regression models using SAS PROC GENMOD were used with a negative binomial log link to compensate for overdispersion in the number of monthly HSI ED visits. All models included population offset and accounted for repeated measures at the county level using the autoregressive AR(1) correlation structure. Backward elimination was used for model building. Confounding was determined by ≥10 % change in beta coefficients of the primary predictor. Model fits were compared using the quasi-likelihood under the independence model criterion [40]. All analyses were performed using SAS 9.3 (Cary, NC, USA).
Results
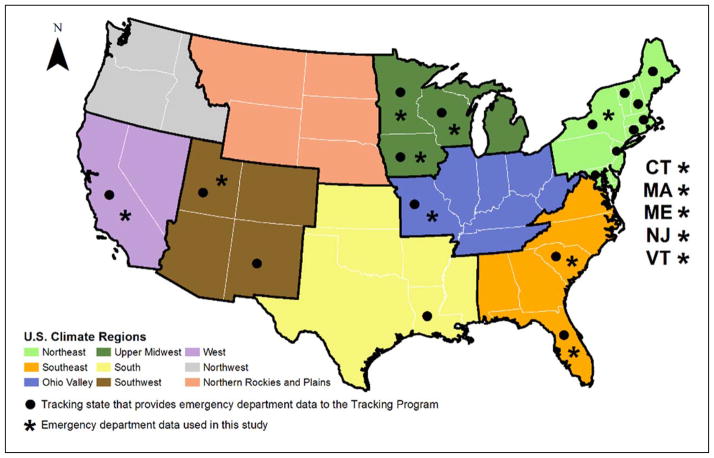
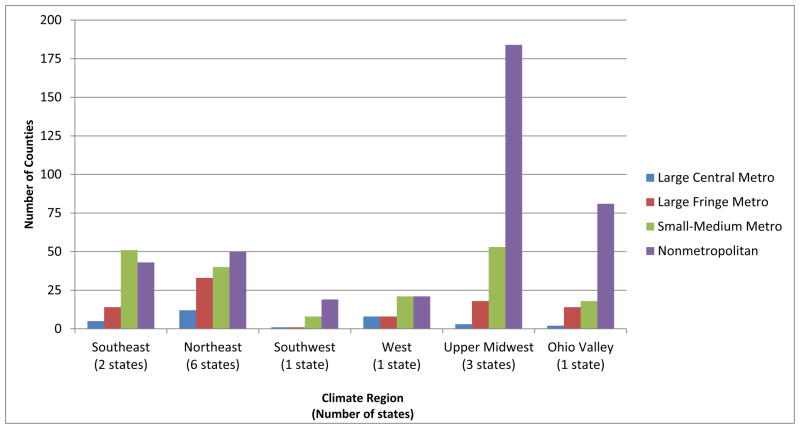
The 14 states included in the analysis covered six climate regions (Southeast, Northeast, Southwest, West, Upper Midwest, and Ohio Valley) (Figure 1) and included 708 counties, with all four urbanicity categories represented in each climate region (Figure 2). Data were not available from states in the Northwest, Northern Rockies and Plains, and South climate regions.
Fig. 1.
The 14 National Environmental Public Health Tracking states across 6 NOAA National Climatic Data Center US Climate Regions used in the analysis
Fig. 2.
County urbanicity breakdown of 14 National Environmental Public Health Tracking states, by climate region
During May 1–September 30 of years 2005–2010 there were 98,462 ED visits with HSI as the primary or any other diagnosis (Table 1). The overall crude incidence rate was 32.2 per 100,000 person-years, and the overall age-adjusted incidence rate was 31.9 per 100,000 person-years. Males accounted for 66.6 % of the HSI ED visits. The age-adjusted incidence rate was 43.5 per 100,000 person-years for males and 20.7 per 100,000 person-years for females. The 15–34 years age group had the highest age-adjusted incidence rate among all age groups (41.8 per 100,000 person-years). The lowest age-adjusted incidence rate was among children aged 0–4 years (9.7 per 100,000 person-years). The lowest age-adjusted incidence rate by year was in 2009 (25.1 per 100,000 person-years), and the highest was in 2010 (38.0 per 100,000 person-years). The year 2006 accounted for a similar proportion of HSI ED visits as 2010 (19.2% for 2006 and 20.1% for 2010), and 2006 had a similar age-adjusted incidence rate as 2010 (37.2 per 100,000 person-years for 2006), compared to the other years. By month, July accounted for the largest proportion of HSI ED visits (34.3 %). July also had the highest age-adjusted incidence rate (53.9 per 100,000 person-years). By climate region, age-adjusted incidence rates ranged from 19.5 per 100,000 person-years in the Southwest to 67.6 per 100,000 person-years in Ohio Valley. Age-adjusted incidence rates increased from most urban to most rural. LCM had the lowest age-adjusted incidence rate (22.1 per 100,000 person-years) and NM had the highest (48.8 per 100,000 person-years).
Table 1.
Characteristics and incidence rates for emergency department visits for heat stress illness in 14 National Environmental Public Health Tracking states, 2005–2010
| Number of heat stress illness emergency department visits | Proportion of HSI ED visits (%) | Crude incidence rate (per 100,000 person-years) | Age-adjusted incidence rate (per 100,000 person-years) | |
|---|---|---|---|---|
| Overall | 98,462 | 100 | 32.2 | 31.9 |
| Sex | ||||
| Male | 65,562 | 33.4 | 43.6 | 43.5 |
| Female | 32,900 | 66.6 | 21.1 | 20.7 |
| Age group (years) | ||||
| 0–4 | 1,918 | 1.9 | 9.7 | 9.7 |
| 5 to 14 | 6,854 | 7.0 | 17.0 | 16.7 |
| 15–34 | 35,250 | 35.8 | 41.9 | 41.8 |
| 35–64 | 39,327 | 39.9 | 32.4 | 32.8 |
| 65 or older | 15,113 | 15.3 | 37.7 | 37.3 |
| Year | ||||
| 2005 | 16,975 | 17.2 | 33.9 | 33.7 |
| 2006 | 18,947 | 19.2 | 37.6 | 37.2 |
| 2007 | 15,570 | 15.8 | 30.7 | 30.4 |
| 2008 | 14,113 | 14.3 | 27.6 | 27.3 |
| 2009 | 13,035 | 13.2 | 25.3 | 25.1 |
| 2010 | 19,822 | 20.1 | 38.2 | 38.0 |
| Month | ||||
| May | 8,085 | 8.2 | 13.0 | 13.0 |
| June | 22,329 | 22.7 | 37.2 | 36.9 |
| July | 33,770 | 34.3 | 54.5 | 53.9 |
| August | 25,463 | 25.9 | 41.1 | 40.8 |
| September | 8,815 | 9.0 | 14.7 | 14.6 |
| Climate region | ||||
| Southwest | 1,258 | 1.3 | 19.1 | 19.5 |
| Upper Midwest | 8,396 | 8.5 | 24.1 | 24.0 |
| Northeast | 24,972 | 25.4 | 24.9 | 24.5 |
| West | 24,297 | 24.7 | 26.5 | 26.5 |
| Southeast | 29,622 | 30.1 | 51.5 | 51.9 |
| Ohio Valley | 9,917 | 10.1 | 66.8 | 67.6 |
| Urbanicity | ||||
| Large central metropolitan | 26,541 | 27.0 | 22.2 | 22.1 |
| Large fringe metropolitan | 23,880 | 24.3 | 31.5 | 31.5 |
| Small–medium metropolitan | 34,965 | 35.5 | 42.0 | 42.0 |
| Nonmetropolitan | 13,076 | 13.3 | 47.9 | 48.8 |
Table 2 presents the multivariable regression model results. After adjusting for month, year, age group, urbanicity, percent of people in poverty, climate region, and monthly mean of daily maximum heat index, the rate of HSI ED visits for females was 29 % lower than the rate for males, and this was statistically significant (p < 0.01). Two age groups had statistically significantly higher HSI ED visit rates than the reference age group of 35–64 years, after adjusting for covariates; the 15–34 years age group had a 39 % higher ED visit rate (p < 0.01), and the ≥65 years age group had a 14 % higher ED visit rate (p < 0.01).
Table 2.
Incidence rate ratio stratified by covariates for the 14 National Environmental Public Health Tracking states, 2005–2010
| IRR | 95% CI | p-value | |
|---|---|---|---|
| Sex | |||
| Male | referent | ||
| Female | 0.71 | 0.69–0.72 | <0.01 |
| Age group (years) | |||
| 0–4 | 0.28 | 0.25–0.30 | <0.01 |
| 5–14 | 0.51 | 0.48–0.54 | <0.01 |
| 15–34 | 1.39 | 1.35–1.44 | <0.01 |
| 35–64 | referent | ||
| ≥65 | 1.14 | 1.07–1.21 | <0.01 |
| Year | |||
| Overall | 0.97 | 0.96–0.98 | <0.01 |
| 2005 | referent | ||
| 2006 | 1.16 | 1.13–1.19 | <0.01 |
| 2007 | 0.98 | 0.95–1.00 | 0.08 |
| 2008 | 0.92 | 0.90–0.95 | <0.01 |
| 2009 | 0.84 | 0.81–0.87 | <0.01 |
| 2010 | 1.07 | 1.03–1.10 | <0.01 |
| Month | |||
| Overall | 0.83 | 0.81–0.84 | <0.01 |
| May | referent | ||
| June | 1.40 | 1.36–1.45 | <0.01 |
| July | 1.37 | 1.31–1.45 | <0.01 |
| August | 1.07 | 1.02–1.13 | 0.01 |
| September | 0.55 | 0.51–0.59 | <0.01 |
| Climate region | |||
| Southeast | 1.07 | 0.89–1.29 | 0.45 |
| Northeast | 1.57 | 1.36–1.82 | <0.01 |
| Southwest | 1.00 | 0.86–1.17 | 0.99 |
| West | 1.21 | 1.02–1.43 | 0.03 |
| Upper Midwest | referent | ||
| Ohio Valley | 1.51 | 1.29–1.76 | <0.01 |
| Urbanicity | |||
| Large central metropolitan | referent | ||
| Large fringe metropolitan | 0.94 | 0.86–1.02 | 0.13 |
| Small–medium metropolitan | 1.06 | 0.99–1.13 | 0.07 |
| Nonmetropolitan | 1.41 | 1.31–1.52 | <0.01 |
| Percent of people in poverty | 1.01 | 1.00–1.02 | 0.13 |
| Monthly mean maximum heat index | 1.07 | 1.06–1.07 | <0.01 |
IRR = incidence rate ratio, CI = confidence interval
Overall, HSI ED visits decreased a significant 3.0 % (p < 0.01) per year (Table 2). Compared with the reference year 2005, 2006 had a 16 % higher HSI ED visit rate, and 2010 had a 7 % higher ED visit rate. Both rates were statistically significant after adjusting for covariates (p < 0.01). In sensitivity analysis where year 2010 data were excluded, this significant decrease in HSI ED visits increased to 5.9 % per year (p < 0.01). Compared with the reference month of May, three months (June, July, and August) had statistically significantly higher HSI ED visit rates. Of these, June and July had substantially higher rates than May (up to 40 % higher for June).
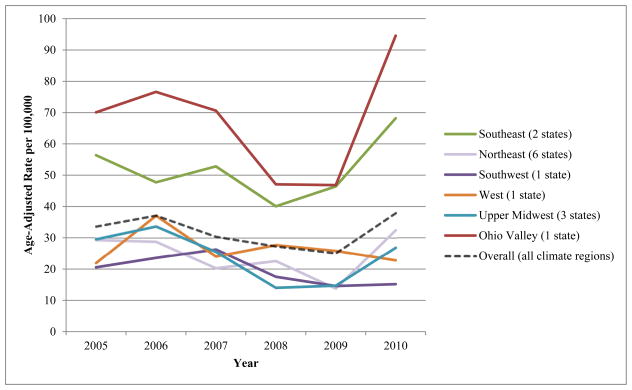
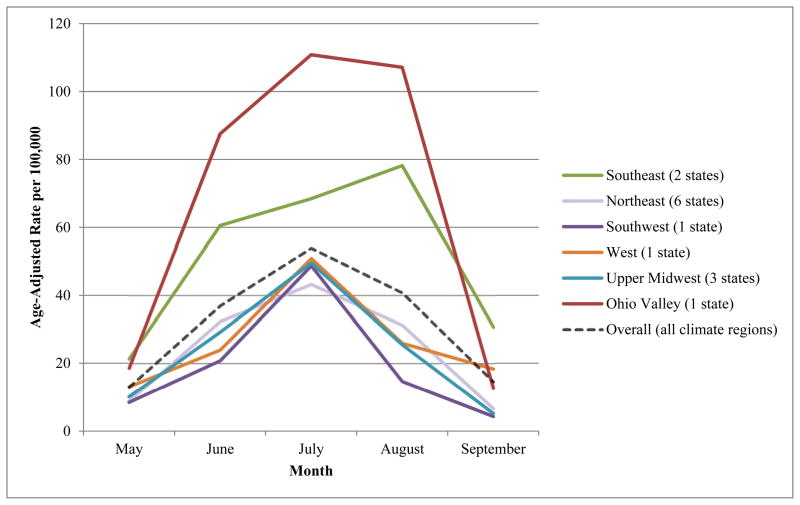
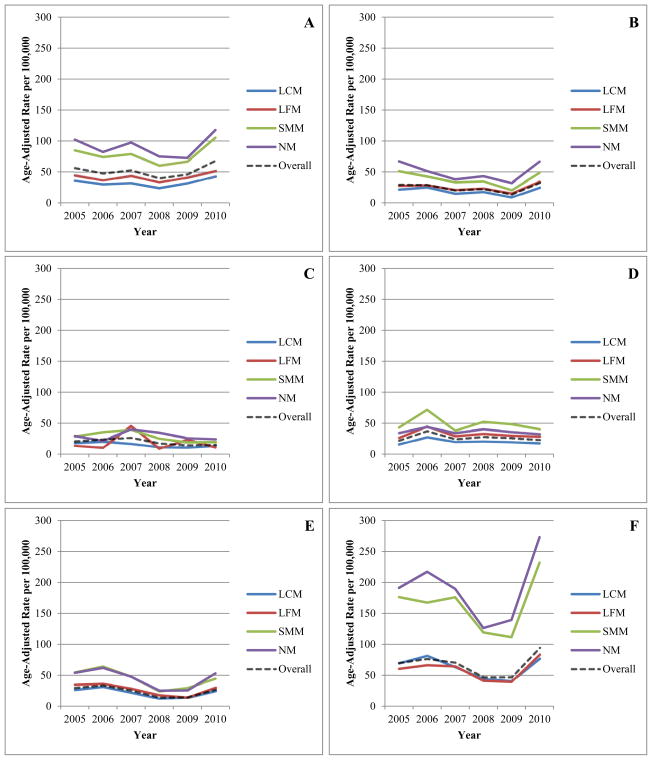
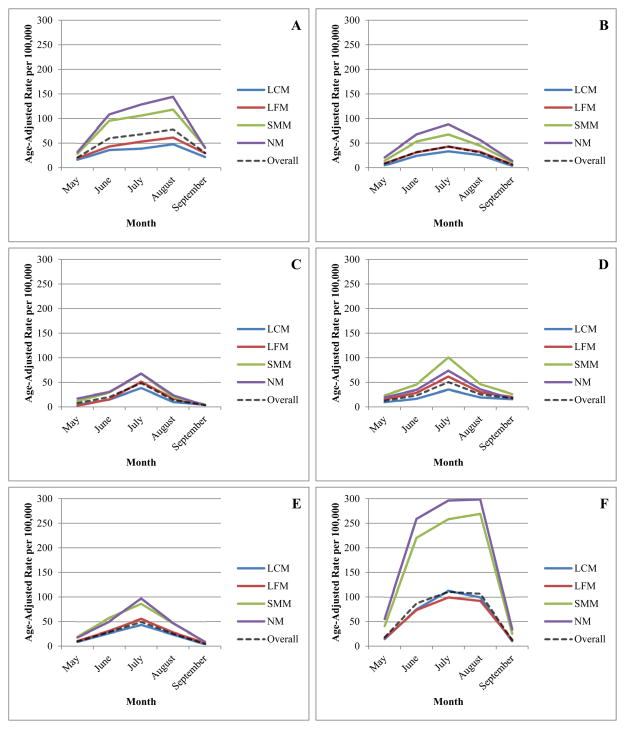
Figure 3 shows climate region–specific age-adjusted rates of HSI ED visits over time. All climate regions except the West had overall decreasing annual rates during 2005–2009, followed by an increase in 2010. Figure 4 shows climate region–specific age-adjusted rates of HSI ED visits by month. The rates peak in most climate regions in July. The Ohio Valley and Southeast climate regions had substantially higher peak rates than other climate regions in July and August, respectively.
Fig. 3.
Annual age-adjusted incidence rates for emergency department visits for heat stress illness by climate region over time in 14 National Environmental Public Health Tracking states, 2005–2010
Fig. 4.
Monthly age-adjusted incidence rates for emergency department visits for heat stress illness by climate region in 14 National Environmental Public Health Tracking states, 2005–2010
Table 3 shows multivariable regression model results for geographic trends by urbanicity and climate region. Overall, after adjusting for month, year, sex, age group, poverty, climate region, and monthly mean maximum heat index, LFM had lower HSI ED visits compared to LCM, and SMM had higher HSI ED visits than LCM, although these were not statistically significant. Overall, visits were 41 % significantly higher in NM than LCM (p < 0.01). Three of the six climate regions showed a similar pattern, with varying statistical significance. In the Southeast and Northeast, SMM had a significantly higher ED visit rate than LCM (22 % higher and 17 % higher, respectively), and NM had a significantly higher HSI ED visit rate than LCM (39 % higher and 73 % higher, respectively) (all p < 0.01). In the Southwest, LFM had a 17 % significantly lower HSI ED visit rate (p < 0.01), and NM had a 49 % significantly higher HSI ED visit rate (p < 0.01) than LCM. The West differed from the overall pattern, with SMM having significantly lower HSI ED visits (p = 0.02) than LCM. However, similar to the overall pattern, NM had 90 % significantly higher HSI ED visits (p < 0.01) than LCM. Upper Midwest and Ohio Valley patterns also differed from the overall pattern but were similar to each other. Although not statistically significant, Upper Midwest and Ohio Valley LFM had higher HSI ED visits and SMM had lower HSI ED visits than LCM. However, similar to the overall pattern, NM in both of these climate regions had significantly higher HSI ED visits than LCM: 14 % higher (p = 0.02) and 15 % higher (p < 0.01), respectively. Figure 5 shows climate region–specific age-adjusted rates of HSI ED visits by year and urbanicity. All climate regions had higher age-adjusted incidence rates in more rural counties compared with the most urban counties. Figure 6 shows climate region–specific age-adjusted rates of HSI ED visits by month and urbanicity. In most climate regions, peak HSI ED visit rates occurred in July.
Table 3.
Geographic trends by urbanicity in emergency department visits for heat stress illness in National Environmental Public Health Tracking states, by region, 2005–2010
| Region | Urbanicity*
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Large central metropolitan (LCM) | Large fringe metropolitan (LFM)
|
Small-medium metropolitan (SMM)
|
Nonmetropolitan (NM)
|
|||||||
| IRR | 95% CI | p-value | IRR | 95% CI | p-value | IRR | 95% CI | p-value | ||
| Overall† | referent | 0.94 | 0.86–1.02 | 0.13 | 1.06 | 0.99–1.13 | 0.07 | 1.41 | 1.31–1.52 | <0.01 |
| Southeast | referent | 0.87 | 0.73–1.05 | 0.14 | 1.22 | 1.06–1.39 | <0.01 | 1.39 | 1.11–1.74 | <0.01 |
| Northeast | referent | 0.87 | 0.75–1.01 | 0.07 | 1.17 | 1.06–1.29 | <0.01 | 1.73 | 1.55–1.92 | <0.01 |
| Southwest | referent | 0.83 | 0.74–0.93 | <0.01 | 1.06 | 0.93–1.21 | 0.37 | 1.49 | 1.21–1.82 | <0.01 |
| West | referent | 0.91 | 0.81–1.03 | 0.15 | 0.82 | 0.70–0.96 | 0.02 | 1.90 | 1.67–2.17 | <0.01 |
| Upper Midwest | referent | 1.12 | 0.94–1.34 | 0.21 | 0.85 | 0.71–1.01 | 0.06 | 1.14 | 1.02–1.26 | 0.02 |
| Ohio Valley | referent | 1.09 | 0.94–1.25 | 0.26 | 0.99 | 0.88–1.10 | 0.81 | 1.15 | 1.03–1.27 | 0.01 |
IRR = incidence rate ratio, CI = confidence interval
Adjusted for month, year, sex, age group, poverty, and monthly mean of daily maximum heat index
Additionally adjusted for climate region
Fig. 5.
Annual age-adjusted incidence rates for emergency department visits for heat stress illness by county urbanicity (LCM = large central metropolitan, LFM = large fringe metropolitan, SMM = small–medium metropolitan, and NM = nonmetropolitan) in 14 National Environmental Public Health Tracking states, 2005–2010, by climate region (A = Southeast, B = Northeast, C = Southwest, D = West, E = Upper Midwest, F = Ohio Valley)
Fig. 6.
Monthly age-adjusted incidence rates for emergency department visits for heat stress illness by county urbanicity (LCM = large central metropolitan, LFM = large fringe metropolitan, SMM = small–medium metropolitan, and NM = nonmetropolitan) in 14 National Environmental Public Health Tracking states, 2005–2010, by climate region (A = Southeast, B = Northeast, C = Southwest, D = West, E = Upper Midwest, F = Ohio Valley)
Discussion
HSI is the most common cause of ED visits from environmental exposure-related injuries in the US [41]. In an analysis of six US climate change–related events, the health costs of a single event, the 2006 heat wave in California, exceeded $5.3 billion [42]. HSIs represent an opportunity to create and implement prevention measures to reduce morbidity and mortality and prevent the economic costs associated with extreme heat events [43]. This study summarizes the temporal and geographic trends by urbanicity of HSI ED visits in 14 Tracking Network states across six climate regions. The results identify the importance of considering local and regional factors when developing extreme heat event preventive measures and interventions.
Males consistently have been shown to have a higher risk for HSI ED visits or hospitalizations after an extreme heat exposure [9, 15, 17, 41]. In the current study, males had an age-adjusted HSI ED visit incidence rate more than twice that of females. This difference is thought to be related to recreational and occupational exposure differences between males and females [41]. Similarly, recreational and occupational differences among age groups might be responsible for the highest age-adjusted incidence rate in the 15–34 years age group, which had 39 % higher HSI ED visits than the 35–64 years age group. This is consistent with work-related and sports-related increases in HSI reported in other studies [18, 41]. Our results are also consistent with previous studies that show adults aged ≥65 years are also at increased risk for HSI [5, 15, 18].
Although an overall significant downward trend in HSI ED visits was seen over time, HSI ED visits increased significantly in 2010. This pattern was consistent across all climate regions except the West, and to a lesser degree the Southwest. Warmer than average temperatures affected the eastern US in the spring and summer of 2010 [44], while the West Coast was cooler than normal, compared with the same periods during 1951–1980 [45, 46]. In addition, the HSI ED visit incidence rate peak in the West climate region in 2006 might be reflective of the July 2006 California heat wave [5]. The sensitivity analysis suggests that inclusion of year 2010 data dampens the overall average decrease in HSI ED visits per year. Therefore, when data become available, future analyses could include more years of ED data. Incorporating additional years before 2005 and after 2010 could show if the overall decrease in HSI ED visits is part of a long-term decreasing trend, despite the changing climate, or if the sudden increase in 2010 is suggestive of an overall increase over a longer period that is not apparent using these six years of data.
Interpretation of HSI ED visit rates should also be made in the context of regional climate to account for the influence of broader climate variability leading to local differences in observed HSI ED visit rates within a region. In addition, although data for this study were limited to six climate regions, NOAA’s National Climatic Data Center has classified the contiguous U.S. into nine climatically consistent regions [34, 35]. The Ohio Valley climate region had the highest HSI ED visit incidence rates. This high incidence rate might be explained by the Ohio Valley climate region including only one Tracking Network state, Missouri, where hyperthermia (defined as a physician-diagnosed case of heat exhaustion or heat stroke) is a reportable condition [47]. However, sensitivity analyses that excluded Missouri from the multivariate analyses showed no substantial differences in temporal or geographic trends of HSI ED visits, compared with when Missouri was included in the analyses. The Southeast climate region had the second highest age-adjusted incidence rate. That rate was substantially different from the remaining four climate regions. This finding is consistent with a recent trend analysis of HSI hospitalizations [48], further demonstrating the importance of considering regional factors in the prevention of HSI, even when accounting for known risk factors such as age and sex.
Previous studies suggest that urban residents are more likely than rural residents to be hospitalized or die after an extreme heat event [49, 50] or be admitted to the hospital or die in the ED from HSI [15]. Public health intervention measures aimed at reducing HSI are well described. Examples include developing heat wave warning systems, increasing availability of cool environments by providing air-conditioned cooling centers (malls, recreation facilities, and community centers), and extending opening hours of public swimming pools and other public facilities. Other examples include community-based programs to check on elderly residents or those who live alone to ensure precautionary measures are taken, built environment modifications (such as increased ventilation and using colors that decrease heat retention), and public education and messaging on personal behavioral changes such as increasing fluid intake and limiting outside activity during daytime hours [13, 26, 43]. These prevention measures have been implemented after notable heat waves have affected large urban areas and have largely focused on non-rural environments [26, 43]; therefore, many of these measures are more easily implemented in urban areas where access and travel to areas of relief are aided by public transportation and advertisement of personal behavioral measures might be more prominent.
The current study found that age-adjusted HSI ED visit rates in the included Tracking states were higher in rural counties than in urban counties. Consistent with two recent studies [9, 15], HSI ED visit rates in the most rural counties were significantly higher than in the most urban counties, both overall (across all climate regions) and within each of the six climate regions. Potential factors explaining increasing HSI ED visit rates with decreasing urbanicity include occupational or recreational differences that result in more outdoor exposure in rural areas [9, 18], air conditioning prevalence or use in homes or public places, or local temperature and precipitation patterns. In addition, persons in rural areas might have less access or exposure to interventions aimed at HSI prevention. They might, for example, be less willing or able to travel longer distances to reach cooling respite areas and services or participate in community organized HSI prevention programs. They also might have less access to medical oversight or care of chronic medical conditions that increase the risk for HSI. As a result, they would have less opportunity learn from healthcare providers about prevention strategies recommended by the American Medical Association [13]. Another possibility is rural residents might visit EDs more frequently for less severe HSI manifestations, as evidenced by urban residents having higher odds of hospital admission or death in the ED following an HSI ED visit [15].
One benefit of using the NCHS Urban-Rural Classification Scheme is the separation of MSAs into central and fringe categories. As in the NCHS categorization, we chose to keep the separation of LCM and LFM. Testing of the NCHS categorization in its ability to identify health differences across urbanization levels repeatedly showed LCM and LFM residents differed substantially on multiple health measures, including health status, health access, and health-related behaviors [31]. We chose to combine the NCHS categories of medium metropolitan and small metropolitan into SMM and the micropolitan and noncore categories NM, because the members of these pairs faired more similarly in measures of health status than LCM and LFM. In the current analyses, we found no significant difference in HSI ED visits between LCM and LFM overall, nor for five of the six climate regions for the health measure being studied. One potential reason could be because access to HSI prevention and intervention measures might be similar between centrally located urban areas and fringe areas, which are typically suburban communities. The Southwest climate region was the only region that had significantly lower HSI ED visits in LFM than LCM. That finding underscores the importance of considering climate region variability in HSI studies.
A strength of the current study is the use of population-based ED data that provide statewide representation for all included states. Additional strengths include temporal trend analysis to identify patterns over time, inclusion of climate region and reporting of climate-region–specific results in addition to overall results, and demonstrated use of Tracking Network surveillance data.
The current study also has a few key limitations. Individual data were not available; therefore, as an ecologic study, we cannot control for other factors known to be associated with HSI ED visits on an individual level or if the ED visit was associated with an extreme heat event. ED data were available only for the 18 Tracking Network states that provide that information to the Tracking Program, which did not include all climate regions. Complete 2005–2010 data were available for 14 of these 18 Tracking Network states. In some cases, data were available for only one state in a climate region. Therefore, results might not be representative of the entire climate region. General limitations of ED-based data using ICD-9-CM codes also apply. Because a race/ethnicity variable often is not included or is unreliable, it was not available for analyses. ED data only capture information on those who seek care, so results might best represent the more severe forms of HSI (e.g., heat exhaustion, heat stroke). Use of ICD-9-CM codes are used primarily for billing purposes, so reimbursement rates could influence providers’ choice of ICD-9-CM codes. An ICD-9-CM code for HSI does not guarantee HSI was the cause of the ED visit, and ED visits are ascribed to the patients’ residential address, which may or may not be where the patient developed HSI. Transfers between EDs for the same HSI event might vary by geographical area, which could impact HSI rates. Additionally, the number of EDs in operation could change over time.
Conclusions
Population-based ED data are valuable for trend analyses over time and space for health outcomes that often require medical care. The current study uses ED data from 14 Tracking Program states across six climate regions to examine temporal and geographic trends in HSI ED visits. The significantly increased HSI ED visit rates in more rural settings identify the need to consider HSI ED visit variability by county, urbanicity, and climate region in implementing effective HSI prevention techniques, especially in rural areas. A potentially useful strategy might be to locally adapt interventions originally geared for urban settings. Although forecasters consider local climatological conditions and community acclimation when issuing heat wave warnings [4], public health professionals might consider HSI variation by urbanicity and climate region when developing local HSI preventive measures and interventions. Further analyses that include additional years of data could help interpret the increase in HSI ED visits in 2010 in a long-term perspective.
Acknowledgments
Funded by National Center for Environmental Health, Centers for Disease Control and Prevention.
We thank W. Dana Flanders for expert advice and consultation and the 14 National Environmental Public Health Tracking state programs that submitted the data used in the study.
Footnotes
Conflict of interest: None.
Disclaimer: The opinions expressed by authors contributing to this manuscript do not necessarily reflect the opinions of the Centers for Disease Control and Prevention or the institutions with which the authors are affiliated.
References
- 1.Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environmental Health. 2009;8:40. doi: 10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiologic Reviews. 2002;24(2):190–202. doi: 10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- 3.Gronlund CJ, Zanobetti A, Schwartz JD, Wellenius GA, O’Neill MS. Heat, heat waves, and hospital admissions among the elderly in the United States, 1992–2006. Environmental Health Perspectives. 2014;122(11):1187–1192. doi: 10.1289/ehp.1206132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guirguis K, Gershunov A, Tardy A, Basu R. The impact of recent heat waves on human health in California. Journal of Applied Meteorology and Climatology. 2014;53(1):3–19. [Google Scholar]
- 5.Knowlton K, Rotkin-Ellman M, King G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environmental Health Perspectives. 2009;117(1):61–67. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson GB, Dominici F, Wang Y, McCormack MC, Bell ML, Peng RD. Heat-related emergency hospitalizations for respiratory diseases in the Medicare population. American Journal of Respiratory and Critical Care Medicine. 2013;187(10):1098–1103. doi: 10.1164/rccm.201211-1969OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin S, Luo M, Walker RJ, Liu X, Hwang SA, Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20(5):738–746. doi: 10.1097/EDE.0b013e3181ad5522. [DOI] [PubMed] [Google Scholar]
- 8.Mastrangelo G, Fedeli U, Visentin C, Milan G, Fadda E, Spolaore P. Pattern and determinants of hospitalization during heat waves: an ecologic study. BMC Public Health. 2007;7:200. doi: 10.1186/1471-2458-7-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lippmann SJ, Fuhrmann CM, Waller AE, Richardson DB. Ambient temperature and emergency department visits for heat-related illness in North Carolina, 2007–2008. Environmental Research. 2013;124:35–42. doi: 10.1016/j.envres.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 10.Lugo-Amador NM, Rothenhaus T, Moyer P. Heat-related illness. Emergency Medicine Clinics of North America. 2004;22(2):315–327. doi: 10.1016/j.emc.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Batscha C. Heat stroke: keeping your clients cool in the summer. Journal of Psychosocial Nursing and Mental Health Services. 1997;35(7):12–17. doi: 10.3928/0279-3695-19970701-19. [DOI] [PubMed] [Google Scholar]
- 12.Beggs PJ, Vaneckova P. Admission to hospital for effects of heat and light: NSW, 1993–94 to 2003–04. New South Wales Public Health Bulletin. 2008;19(7–8):132–137. doi: 10.1071/nb07004. [DOI] [PubMed] [Google Scholar]
- 13.Blum LN, Bresolin LB, Williams MA. Heat-related illness during extreme weather emergencies. JAMA. 1998;279(19):1514. doi: 10.1001/jama.279.19.1514. [DOI] [PubMed] [Google Scholar]
- 14.Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the Eastern U.S. American Journal of Epidemiology. 2002;155(1):80–87. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- 15.Hess JJ, Saha S, Luber G. Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environmental Health Perspectives. 2014;122(11):1209–1215. doi: 10.1289/ehp.1306796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Naughton MP, Henderson A, Mirabelli MC, et al. Heat-related mortality during a 1999 heat wave in Chicago. American Journal of Preventive Medicine. 2002;22(4):221–227. doi: 10.1016/s0749-3797(02)00421-x. [DOI] [PubMed] [Google Scholar]
- 17.Pillai SK, Noe RS, Murphy MW, et al. Heat illness: predictors of hospital admissions among emergency department visits — Georgia, 2002–2008. Journal of Community Health. 2013;39(1):90–98. doi: 10.1007/s10900-013-9743-4. [DOI] [PubMed] [Google Scholar]
- 18.Rhea S, Ising A, Fleischauer AT, Deyneka L, Vaughan-Batten H, Waller A. Using near real-time morbidity data to identify heat-related illness prevention strategies in North Carolina. Journal of Community Health. 2012;37(2):495–500. doi: 10.1007/s10900-011-9469-0. [DOI] [PubMed] [Google Scholar]
- 19.Stollberger C, Lutz W, Finsterer J. Heat-related side-effects of neurological and non-neurological medication may increase heatwave fatalities. European Journal of Neurology. 2009;16(7):879–882. doi: 10.1111/j.1468-1331.2009.02581.x. [DOI] [PubMed] [Google Scholar]
- 20.Kirtman B, Power SB, Adedoyin JA, et al. Near-term climate change: projections and predictability. In: Stocker TF, Qin D, Plattner GK, Tignor M, Allen SK, Boschung J, Nauels A, Xia Y, Bex V, Midgley PM, editors. Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. New York, NY: Cambridge University Press; 2013. pp. 953–1028. [Google Scholar]
- 21.Bernard SM, McGeehin MA. Municipal heat wave response plans. American Journal of Public Health. 2004;94(9):1520–1522. doi: 10.2105/ajph.94.9.1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.California Governor’s Office of Emergency Services. State of California contingency plan for excessive heat emergencies. 2014 Retrieved August 13, 2014 from http://www.calema.ca.gov/PlanningandPreparedness/Documents/Heat%20Contingency%20Plan%20Rev%20June%202014.pdf.
- 23.Changnon SA, Kunkel KE, Reinke BC. Impacts and responses to the 1995 heat wave: a call to action. Bulletin of the American Meteorological Society. 1996;77(7):1497–1506. [Google Scholar]
- 24.Missouri Department of Health and Senior Services. Data and statistical reports | hyperthermia. 2014 Retrieved July 25, 2014 from http://health.mo.gov/living/healthcondiseases/hyperthermia/data.php.
- 25.Semenza JC, Rubin CH, Falter KH, et al. Heat-related deaths during the July 1995 heat wave in Chicago. New England Journal of Medicine. 1996;335(2):84–90. doi: 10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- 26.McGeehin MA, Mirabelli M. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environmental Health Perspectives. 2001;109(Suppl 2):185–189. doi: 10.1289/ehp.109-1240665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention National Environmental Public Health Tracking Program. Centers for Disease Control and Prevention Standards for Nationally Consistent Data and Measures within the Environmental Public Health Tracking Network. 2013 Retrieved July 21, 2014 from http://ephtracking.cdc.gov/docs/CDC_NCDM_v3.pdf.
- 28.Centers for Disease Control and Prevention National Environmental Public Health Tracking Program. Environments climate change indicators — CDC Tracking Network. 2014 Retrieved July 25, 2014 from http://ephtracking.cdc.gov/showClimateChangeIndicators.action.
- 29.Centers for Disease Control and Prevention. Environmental Public Health Tracking Network. State emergency department visits data. 2014 Retrieved February 5, 2014 from http://www.cdc.gov/ephtracking.
- 30.Centers for Disease Control and Prevention. National Vital Statistics System. Bridged-race population estimates. Accessed from Environmental Public Health Tracking Network. 2014 Retrieved February 10, 2014 from http://www.cdc.gov/ephtracking.
- 31.Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. National Center for Health Statistics. Vital Health Statistics. 2014;2(166) [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention National Center for Health Statistics. Data access — Urban-rural classification scheme for counties. 2014 Retrieved June 4, 2014 from http://www.cdc.gov/nchs/data_access/urban_rural.htm.
- 33.United States Census Bureau. American Community Survey. Socioeconomic measures. Accessed from Environmental Public Health Tracking Network. 2014 Retrieved December 16, 2014 from http://www.cdc.gov/ephtracking.
- 34.Karl TR, Koss WJ. Regional and national monthly, seasonal, and annual temperature weighted by area, 1895–1983. Asheville, NC: National Climatic Data Center; 1984. [Google Scholar]
- 35.National Oceanic and Atmospheric Administration. Climate at a glance: time series | National Climatic Data Center (NCDC) 2014 Retrieved May 21, 2014 from http://www.ncdc.noaa.gov/monitoring-references/maps/us-climate-regions.php.
- 36.Mitchell KE, Lohmann D, Houser PR, et al. The multi-institution North American Land Data Assimilation System (NLDAS): utilizing multiple GCIP products and partners in a continental distributed hydrological modeling system. Journal of Geophysical Research. 2004;109:D07S90. doi: 10.1029/2003jd003823. [DOI] [Google Scholar]
- 37.Rothfusz LP. The heat index “equation” (or, more than you wanted to know about heat index) (SR 90-23) Fort Worth, TX: National Weather Service Southern Region Headquarters; 1990. [Google Scholar]
- 38.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People Statistical Notes. 2001;20:1–12. [PubMed] [Google Scholar]
- 39.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. World Health Organization; 2001. Retrieved February 10, 2014 from http://www.who.int/healthinfo/paper31.pdf. [Google Scholar]
- 40.Pan W. Akaike’s Information Criterion in Generalized Estimating Equations. Biometrics. 2001;57(1):120–125. doi: 10.1111/j.0006-341x.2001.00120.x. [DOI] [PubMed] [Google Scholar]
- 41.Sanchez CA, Thomas KE, Malilay J, Annest JL. Nonfatal natural and environmental injuries treated in emergency departments, United States, 2001–2004. Family and Community Health. 2010;33(1):3–10. doi: 10.1097/FCH.0b013e3181c4e2fa. [DOI] [PubMed] [Google Scholar]
- 42.Knowlton K, Rotkin-Ellman M, Geballe L, Max W, Solomon GM. Six climate change-related events in the United States accounted for about $14 billion in lost lives and health costs. Health Affairs. 2011;30(11):2167–2176. doi: 10.1377/hlthaff.2011.0229. [DOI] [PubMed] [Google Scholar]
- 43.O’Neill MS, Carter R, Kish JK, et al. Preventing heat-related morbidity and mortality: new approaches in a changing climate. Maturitas. 2009;64(2):98–103. doi: 10.1016/j.maturitas.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.NOAA National Climate Data Center. State of the climate: global analysis for June 2010. 2010 Retrieved August 1, 2014 from http://www.ncdc.noaa.gov/sotc/global/2010/6.
- 45.NASA Goddard Space Flight Center Earth Observatory. How warm was summer 2010? NASA Goddard Space Flight Center; 2010. Retrieved August 1, 2014 from http://earthobservatory.nasa.gov/IOTD/view.php?id=46159&eocn=image&eoci=related_image. [Google Scholar]
- 46.NASA Goddard Space Flight Center Earth Observatory. GISS surface temperature analysis: how warm was this summer? NASA Goddard Institute for Space Studies; 2013. Retrieved August 1, 2014 from http://data.giss.nasa.gov/gistemp/2010summer/ [Google Scholar]
- 47.Missouri Department of Health and Senior Services. Rules of Department of Health and Senior Services Division 20—Division of Community and Public Health Chapter 20—Communicable Diseases (19 CSR 20-20) St. Louis, MO: Missouri State Government; 2008. [Google Scholar]
- 48.Choudhary E, Vaidyanathan A. Heat stress illness hospitalizations — Environmental Public Health Tracking Program, 20 states, 2001–2010. Morbidity and Mortality Weekly Report Surveillance Summaries. 2014;63(SS-13):1–10. [PubMed] [Google Scholar]
- 49.Clarke JF. Some effects of the urban structure on heat mortality. Environmental Research. 1972;5(1):93–104. doi: 10.1016/0013-9351(72)90023-0. [DOI] [PubMed] [Google Scholar]
- 50.Jones TS, Liang AP, Kilbourne EM, et al. Morbidity and mortality associated with the July 1980 heat wave in St. Louis and Kansas City, MO. JAMA. 1982;247(24):3327–3331. [PubMed] [Google Scholar]