Abstract
Background
Suicide risk is challenging to quantify due to reliance on self-report, which is limited by individuals’ lack of insight and the desire to conceal such intentions. Non-suicidal self-injury (NSSI) is one of the most robust predictors of suicidal ideation (SI) and suicide attempts (SA). Although NSSI often leads to permanent scarring, which can be assessed by objective physical examination, no research has examined whether scarring denotes tangible risk for SI and SA. The present study examined whether NSSI scar presence and number predict current SI and SA history. Further, we examined whether brooding would exacerbate the effects of NSSI scarring on SI or SA.
Methods
Young adults (N = 231; M = 21.24 years; 78% female) completed self-report questionnaires assessing SA history, frequency of NSSI, presence/number of NSSI scars, brooding, current depressive symptoms, and SI.
Results
NSSI scar presence and number predicted current SI and SA history after controlling for current depressive symptoms. Moreover, scar presence and number predicted current SI over and above the effects of SA history and NSSI frequency, method, and medical severity. Further, NSSI scar presence and number predicted SI more strongly among individuals with greater levels of brooding than among individuals with lower levels of brooding.
Conclusions
The presence and number of NSSI scars are objective physical indicators of risk for SI and SAs. Brooding may further heighten the risk of SI for individuals bearing NSSI scars.
Keywords: non-suicidal self-injury, scars, brooding, suicidal ideation, suicide attempts
1. Introduction
Suicidal thoughts and behaviors (STBs) occur at relatively high rates among young adults, with suicide the third leading cause of death among individuals ages 15–24 (Center for Disease Control, 2010). Prevention efforts have been hampered by the field’s reliance on self-report to quantify risk for suicide-relevant outcomes, which relies on an individual’s inherently subjective responses provided with deliberate intention (Nosek, 2007). Relying entirely on self-report is a major problem, given that many suicidal individuals conceal their ideation. Therefore, a more objective means is needed to identify those who may be at highest risk for suicide-relevant outcomes.
Non-suicidal self-injury (NSSI), the intentional self-destruction of one’s tissue without associated suicidal intent (Nock, 2006), is one of the most robust predictors of STBs (Hamza et al., 2012; Lewinsohn et al., 1994; Wilkinson et al., 2011; Whitlock et al., 2013). The rates of NSSI are particularly alarming among young adults, with as many as 38% of college students reporting a history of the behavior (Gratz, et al., 2002; Saraff and Pepper, 2014; Wilcox et al., 2012; Whitlock, et al., 2006). Injuries from NSSI can leave markings, extending the effects of the behavior from the acute act to anywhere from a short duration (in which acute injuries heal) to permanency. Scarring is one characteristic of NSSI that may help to account for the relationship between NSSI and STBs. Furthermore, it is a characteristic that could be assessed by objective physical examination, allowing clinicians to rely less on often unreliable self-reports.
1.1 Relationship between NSSI Characteristics and STBs
The majority of studies investigating the relationship between NSSI and STBs have found that any history of NSSI is associated with STBs, with correlational studies citing medium to large effect sizes (e.g. Asarnow et al., 2010; Glenn and Klonsky, 2009; Whitlock and Knox, 2007; Whitlock et al., 2013). Beyond presence versus absence of NSSI, NSSI frequency, and methods, far less research has examined the relationship between alternative specific characteristics of NSSI and suicide-relevant outcomes, such as the impact of NSSI pain experience, functions, and context of the behavior (Glenn and Klonsky, 2008; Nock and Prinstein, 2005; Paul et al., 2015). Therefore, given that a significant proportion of those with a history of NSSI do not report STBs (Whitlock et al., 2013), significantly more research is needed to identify unique characteristics of NSSI that help clinicians to better determine high-risk cases.
1.2 Relationship between NSSI Scarring and STBs
Although permanent scarring is a well-known consequence of NSSI, no empirical studies to our knowledge have reported the presence and number of scars resulting from the behavior among psychiatric or community samples. Furthermore, only two empirical studies have directly examined the psychological effects of scarring from NSSI (Dyer et al., 2012; Dyer et al., 2014). Specifically, Dyer and colleagues (2012, 2014) found, and then replicated their findings, that among females and males, recruited specifically for scarring, those with NSSI scarring endorsed a significantly more negative body image in general and after scarring than those with scars of alternate origins, even after controlling for scar size and appearance. These studies provide important preliminary evidence that the presence of NSSI scarring might be psychologically damaging.
In addition, it is possible that scars from NSSI may serve as physical reminders of painful memories or even shame about engaging in NSSI. Weaver et al. (2007) found that among individuals with a history of intimate partner violence (IPV), the relationship between body image distress and post-traumatic stress disorder was stronger among those with scarring from IPV than those without scarring. The authors concluded that the residual injuries sustained from the IPV might function as a physical reminder of the violent event (Weaver et al., 2007). Similarly, given that individuals often report engaging in NSSI to regulate very painful emotions and for self-punishment purposes (Nock and Prinstein, 2004), viewing a particular scar might activate negative emotions related to the circumstances that prompted engagement and trigger distressing memories. Thus, it is possible that NSSI scarring may be associated with elevated levels of distress, which in turn, may augment one’s vulnerability for exhibiting STBs. However, no research has investigated the relationship between the presence of NSSI scars and STBs.
1.3 Ruminative Brooding as a Moderator of NSSI Scarring and STBs
Ruminative brooding, which is characterized by a passive and perseverative focus on the presence, causes and consequences of one’s negative affect (Nolen-Hoeksema, 1991), is an additional factor that is relevant to suicide-related outcomes (for a review, see Morrison and O’Connor, 2008). The cognitive catalyst model suggests that brooding may amplify the effects of negative cognitive and affective states on psychopathology (Ciesla and Roberts, 2007; Stange et al., 2013), NSSI (Cohen et al., 2015), and SI (Stange et al., 2015). Thus, we conjecture that individuals who tend to passively think about the causes and consequences of negative mood may be particularly affected by visual reminders of negative affect, such that the scars may trigger powerful ruminative cycles. Moreover, individuals who tend to brood may brood not only about negative mood, but also about the origins of the scars themselves and their consequences, thus increasing their risk of STBs.
1.4 The Current Study
Considerable literature supports NSSI as a strong predictor of STBs. However, few studies have examined characteristics of NSSI that may confer heightened risk for STBs and no studies have examined whether NSSI scarring may be related to STBs. The current study addresses these gaps in the literature by examining a sample of individuals at an undergraduate institution. Undergraduate samples are ideal to examine NSSI and suicide-relevant outcomes, because they consistently demonstrate high rates of both lifetime non-suicidal self-injury (17%–38%; Gratz et al., 2002; Whitlock et al., 2006) and suicidal ideation and behavior (11.4% and 7.1%, respectively; Toprak et al., 2011). Given the relatively high rates of these behaviors in undergraduate samples of young adults, coupled with the fact that nearly 21 million individuals between the ages of 18 and 24 in the United States are currently enrolled in college courses (U.S. Department of Education, 2015), it is important to clarify the etiology of these self destructive behaviors in undergraduate samples.
We hypothesized that the presence and number of NSSI scars would be related to current SI as well as history of SAs, controlling for current symptoms of depression, and frequency, medical severity, and method of NSSI. Second, we hypothesized that scarring from NSSI would predict STBs more strongly among individuals with high levels of brooding than among those with low levels of brooding.
2. Method
2.1 Participants
Participants were Temple University (TU) students who were recruited by advertising enrollment (e.g. via announcements in classes, flyers) in a study developed to understand responses to stress. Interested individuals with access to the TU online research system were directed to an online questionnaire hosted by Fluid Surveys and were considered enrolled once consent was obtained. Participants were 231 undergraduates (M=21.24 years; SD=4.02) who completed all study questionnaires in exchange for research credit. The present sample was 78% female (N = 181) and the racial background of the participants was 56% (N = 130) Caucasian, 21% (N = 49) African American, 6% (N = 14) East Asian, 4% (N = 8) South Asian, 6% (N = 14) Biracial, and 7% (N = 15) other racial background. Participant demographics were largely representative of the TU undergraduate student population; however, there were more females in the present sample than in the full TU sample. The Temple University Institutional Review Board approved the procedures.
2.2 Measures
2.2.1 Non-Suicidal Self-Injury
The Deliberate Self Harm Inventory (DSHI; Gratz, 2001) assesses the frequency, medical severity, and methods of NSSI behaviors (e.g., cutting, carving, burning, biting, head-banging). The DSHI asks how often the participant has engaged in each of 16 types of NSSI behaviors with the prompt, “Have you ever intentionally (i.e., on purpose) _______?” as well as one additional prompt asking the frequency of NSSI methods not explicitly listed. We modified the DSHI to add the clause, “without intending to kill yourself” to each of the 17 questions to ensure participants did not record any suicidal behaviors throughout the questionnaire. For each endorsed NSSI behavior, respondents are asked about lifetime frequency and whether the behavior ever resulted in hospitalization or required medical treatment (a dichotomous variable indicating more (1) or less (0) medically severe NSSI behaviors). For this study, we minimized the variability of lifetime NSSI frequency by classifying NSSI into categories (0, 1, 2–5, 6–20, 21–50, and 51+ NSSI acts; Burke et al., 2015; Cohen et al., 2015; Whitlock et al., 2013). Further, we also added 2 questions asking whether any form of NSSI engaged in over the lifetime ever resulted in a permanent mark or scar. If participants indicated yes, they were asked to indicate number of permanent marks/scars. Thus, we included the dichotomized variable of scar presence (1) versus absence (0) and the number of NSSI scars (categorized: 0, 1, 2–5, 6–20, 21–50, and 51+ NSSI scars) as our primary predictor variables. Research has supported the DSHI’s test-retest reliability, and construct, discriminant, and convergent validity in a university-student sample (Gratz, 2001; Fleige et al., 2006).
2.2.2 Suicidal Ideation
The Beck Scale for Suicidal Ideation (BSS; Beck and Steer, 1991) was employed to assess SI over the previous week. The BSS measures passive and active SI, as well as suicide plans, preparations, and access to means to carry out plans. The BSS is highly correlated (.90) with a clinician administered interview version of the BSS (Beck et al., 1988). Further, research indicates that participants may be more likely to report current SI on anonymous self-report measures due to stigma and possible threat of hospitalization associated with in-person endorsement (Greist et al., 1973; Kaplan et al., 1994). The scale has adequate internal consistency, as well as concurrent and construct validity in a sample of undergraduates (Chioqueta and Stiles, 2006). In the present sample, Cronbach’s alpha was 0.85.
2.2.3 Suicidal Behavior
To assess history of SAs, participants were asked, “Have you ever attempted to kill yourself?” SAs were dichotomized as the presence (1) or absence (0) of a history of SAs.
2.2.4 Depressive Symptoms
The Beck Depression Inventory-II (BDI-II; Beck et al., 1996) is a self-report measure that assesses the severity of symptoms of depression during the previous two weeks. The BDI-II has been well validated in undergraduate samples (Storch et al., 2004) (α = .95 in the current sample).
2.2.5 Ruminative Brooding
The Ruminative Responses Scale (RRS; Treynor, Gonzalez, & Nolen-Hoeksema, 2003) is a 10-item questionnaire that assesses the extent to which individuals engage in two subtypes of rumination, brooding and reflection, in response to dysphoric mood. Brooding rumination measures individuals’ tendency to passively and perseveratively focus on the meaning, causes, and consequences of their negative affect (Treynor et al., 2003). The RRS-BR has demonstrated adequate internal consistency and retest reliability (Treynor et al., 2003) (α = .83 in the present sample).
2.3 Statistical Method
To examine our hypotheses that both the presence and number of NSSI scars would predict current SI or SA history, we conducted a series of hierarchical linear and logistic regressions, respectively. First, we separately examined the effects of NSSI scar presence and NSSI scar frequency on SI and SA, controlling for depressive symptoms. Second, we conducted a more conservative test of our hypotheses controlling for current depressive symptoms, NSSI frequency, method, and medical severity (based on report of NSSI resulting in hospitalization or medical treatment), and history of SAs (when predicting to current SI). Further, to determine the independent effects of either the presence or number of NSSI scars on current SI and history of SAs, we then examined both NSSI scar presence and frequency in the same model. Finally, we evaluated whether the association between NSSI scars and SI would be stronger among individuals with higher levels of brooding.
3. Results
3. 1 Preliminary Analyses
Demographics broken down by NSSI category (0 = No NSSI; 1 = NSSI with no scars; 2 = NSSI with scars) are presented in Table 1. To determine whether there were significant differences between NSSI categories on demographic characteristics or primary study variables, we conducted analysis of variance (ANOVA) tests and independent t-tests. There were no significant differences across categories on gender or age. However, there were differences between groups on race, such that those with NSSI without scars were more likely to identify as African American. In addition, Table 2 provides information about the bivariate correlations among primary study variables. Unsurprisingly, all study variables were positively correlated with one another. Specifically, number of scars and scar presence were positively correlated with NSSI frequency, NSSI severity, a history of SAs, and levels of suicidal ideation and depressive symptoms.
Table 1.
Demographic characteristics of the sample by NSSI category
| No NSSI (N = 153) | NSSI/No Scars (N = 35) | NSSI/Scars (N = 43) | Statistical Test (F or χ2) | |
|---|---|---|---|---|
| Age | 21.51 (4.32) | 20.94 (3.70) | 20.53 (3.00) | 1.11 |
| Sex | 78% female | 77% female | 86% female | 6.89 |
| Race | 51% Caucasian | 57% Caucasian | 74% Caucasian | 16.68*** |
| 27% African | 17% African | 5% African | ||
| American | American | American | ||
| 9% Asian/Pacific | 9% Asian/Pacific | 14% Asian/Pacific | ||
| Islander | Islander | Islander | ||
| 6% Biracial | 9% Biracial | 5% Biracial | ||
| 7% Other | 8% Other | 2% Other | ||
| BDI | 8.33 (9.27) | 15.26 (11.56) | 17.37 (14.35) | 15.06*** |
| RRS-BR | 10.84 (3.87) | 12.26 (3.88) | 13.51 (4.10) | 8.46*** |
| BSS | .34 (1.19) | .71 (1.82) | 3.09 (1.82) | 18.48*** |
p < .01,
p < .001.
Note. NSSI = Non suicidal self-injury; BDI = Beck Depression Inventory; RRS-BR = Ruminative Response Styles- Brooding; BSS = Beck Suicide Scale.
Table 2.
Bivariate Correlations of Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1 BDI | — | ||||||||
| 2 RRS-BR | .58*** | — | |||||||
| 3 BSS | .52*** | .45*** | — | ||||||
| 4 NSSI Freq | .35*** | .32*** | .37*** | — | |||||
| 5 NSSI Med Sev | .18** | .14* | .22*** | .36*** | — | ||||
| 6 SA | .20** | .20** | .26*** | .36*** | .36*** | — | |||
| 7 Scar Presence | .27*** | .23*** | .37*** | .74*** | .37*** | .38*** | — | ||
| 8 Scar Freq | .27*** | .25*** | .43*** | .78*** | .48*** | .37*** | .87*** | — | |
| 9 NSSI Method | .34*** | .28*** | .33*** | .75*** | .33*** | .32*** | .75*** | .70*** | — |
p < .05,
p < .01,
p < .001.
Note. BDI = Beck Depression Inventory; RRS-BR = Ruminative Response Styles- Brooding; BSS = Beck Suicide Scale; NSSI = Non suicidal self-injury; Freq = Frequency; SA = Suicide Attempt.
Approximately 16% (N = 37) of the sample exhibited any active SI, and approximately 6.5% (N = 15) of the sample endorsed at least one suicide attempt over their lifetimes. We also examined the extent of NSSI scarring. Overall, 33.8% (N = 78) of the sample reported at least one NSSI incident. Among those with a NSSI history, 55.1% (N =43) reported having a scar from engaging in NSSI behavior. Specifically, of those with NSSI scars, 20.9% (N = 9) reported having 1 scar, 46.5% (N = 20) reported having 2–5 scars, 18.6% (N = 8) reported having 6–20 scars, 7.0% (N = 3) reported having 20–50 scars, and 2.3% (N = 1) reported having over 50 scars (4.7% declined to provide information about number of scars).
A series of independent samples t-tests examining only participants with a history of NSSI were conducted to determine whether the frequency, severity, and methods of NSSI differed between those with and without scars. Cutting was the only specific NSSI method that differed between those with and without scars (t=−5.62, p < .001). In addition, individuals with NSSI scars engaged in the behavior more frequently than those with a history of NSSI but without scars (t=−4.34, p < .001). Furthermore, those with NSSI scarring were more likely to have reported hospitalization or required medical attention from their NSSI than those who engaged in NSSI with no scars (t =−2.50, p <. 01). To perform conservative tests of whether the presence of NSSI scars predicted current SI and history of SAs beyond these other factors associated with scarring, we controlled for each of these factors in subsequent analyses.
3.2 Does NSSI scarring predict current suicidal ideation?
Consistent with our hypotheses, the presence of NSSI scars predicted current SI beyond the effects of current depressive symptoms (β = .25, t = 4.344, p < .001), NSSI frequency, method, severity, and history of SAs (Table 3). Further, individuals with a greater number of scars were at greater risk for experiencing current SI controlling for depressive symptoms (β = .31, t = 5.54, p < .001), and controlling for history of SAs, frequency, method, and severity of NSSI (Table 3). Of note, however, current depressive symptoms remained the strongest predictor of current suicidal ideation. When NSSI scar presence and frequency were added into the model simultaneously, NSSI scar frequency remained significant; however, NSSI scar presence was no longer significant (Table 3). Thus, as individuals increased in number of scars, the severity of SI increased by one on the BSS.
Table 3.
Scar Presence and Scar Frequency as Predictors of Suicidal Ideation
| NSSI Scar Presence Only | NSSI Scar Frequency Only | NSSI Scar Presence and Frequency | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Variable | β | SE | t | ΔR2 | β | SE | t | ΔR2 | β | SE | t | ΔR2 |
| BDI | .44 | .02 | 7.56*** | .46 | .01 | 7.94*** | .46 | .01 | 7.93*** | |||
| Method (Cutting) | −.07 | .62 | −.77 | −.02 | .58 | −.22 | −.03 | .63 | −.30 | |||
| NSSI Med Sev | .03 | 1.00 | .40 | −.03 | 1.02 | −.54 | −.03 | 1.03 | −.51 | |||
| NSSI Frequency | .06 | .16 | .59 | −.04 | .17 | −.43 | −.04 | .17 | −.43 | |||
| Suicide Attempt | .10 | .69 | 1.68 | .10 | .70 | 1.69 | .10 | .70 | 1.70 | |||
| Scar Presence | .23 | .66 | 2.51 | .02* | .03 | .89 | .24 | |||||
| Scar Frequency | .33 | .28 | 3.53*** | .04** | .31 | .38 | 2.45* | .04** | ||||
p < .05,
p < .01,
p < .001.
Note. NSSI = Non-suicidal self-injury; BDI = Beck Depression Inventory; NSSI Med Sev = Non-suicidal self-injury medical lethality. Linear regressions were conducted to examine these hypotheses; thus, the full sample (N = 231) was included in these analyses.
3.3 Is NSSI scarring associated with history of suicide attempts?
A history of a SA was associated with the presence of NSSI scars (B = 1.81, SE = .59, Wald Z = 9.42, p < .01; OR = 6.09; CI = 1.92–19.28) and scar frequency (B = .84, SE = .22, Wald Z = 14.85, p < .001; OR = 2.31; CI = 1.51–3.53), controlling for current depressive symptoms. However, when entering the other NSSI predictors in the model (NSSI frequency, method, and medical severity), neither scar presence nor frequency was associated with a history of SA (results available upon request).
3.4 Does ruminative brooding moderate the relationship between NSSI scarring and SI?
To examine our second hypothesis that brooding would exacerbate the association of NSSI scarring with current SI, we conducted moderation analyses. First, we entered NSSI frequency, method, and severity, history of SAs, and current depressive symptoms as covariates. Then, we entered the main effects of NSSI scarring and brooding, followed by the interaction of NSSI scarring and brooding. We separately conducted moderation analyses for NSSI scar presence and frequency, but controlled for the other NSSI scar variable when each was the primary predictor of interest. Given that there were only 15 SAs, our power was too small to determine whether brooding moderated the relationship between NSSI scars and suicidal behaviors.
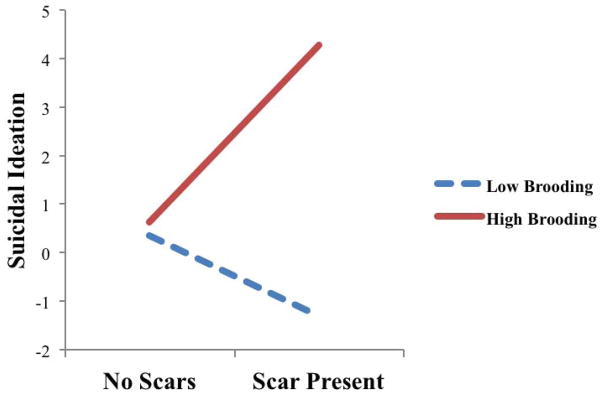
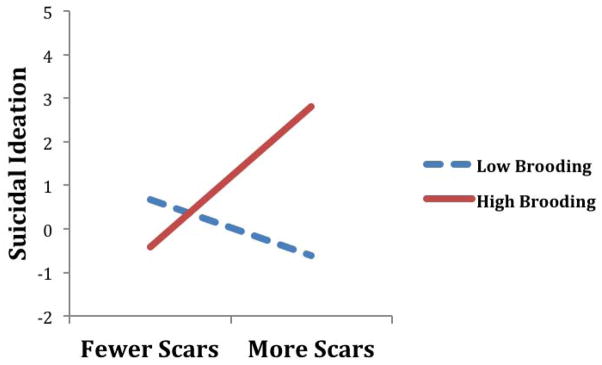
There was a significant interaction between scar presence and brooding in predicting current SI (Table 4; Figure 1). Consistent with hypotheses, NSSI scar presence predicted a greater likelihood of exhibiting current SI among individuals with higher levels of brooding (B = 3.66, SE = 0.65, t = 5.67, p <. 001). Surprisingly, there was a significant slope among individuals with lower levels of brooding, such that individuals with NSSI scarring and lower levels of brooding were at reduced risk for experiencing current SI (B = −1.66, SE = 0.73, t = −2.26, p = .03). Further, consistent with hypotheses, the number of NSSI scars significantly interacted with brooding to predict current SI (Table 4; Figure 2), such that individuals with more NSSI scars and greater tendency to brood were most at risk for experiencing current SI (B = 1.72, SE = 0.26, t = 6.72, p <. 001). Similar to our findings for scar presence, individuals with more NSSI scars and lower levels of brooding were at reduced risk for experiencing current SI (B = −0.68, SE = 0.31, t = −2.17, p = .03).
Table 4.
Rumination as a Moderator of the Relationship between Scar Presence and Scar Frequency and Suicidal Ideation
| Interaction between Rumination and Scar Presence Predicting SI
| |||
|---|---|---|---|
| Predictor | Effect | SE | t |
| T1 BDI | 0.07 | 0.02 | 4.51*** |
| Method (Cutting) | −0.53 | 0.55 | −0.97 |
| NSSI Med Sev | −0.16 | 0.89 | −0.18 |
| NSSI Frequency | 0.01 | 0.14 | 0.07 |
| Suicide Attempt | 0.98 | 0.61 | 1.60 |
| Brooding | 0.03 | 0.04 | 0.67 |
| NSSI Scar Presence | 1.05 | 0.59 | 1.78 |
| Brooding x Scar Presence | 0.66 | 0.08 | 7.45*** |
|
| |||
| ΔR2 = .13, F = 55.57, p < .001 | |||
| Interaction between Rumination and Scar Frequency Predicting SI
| |||
|---|---|---|---|
| Predictor | Effect | SE | t |
| T1 BDI | 0.07 | 0.01 | 4.93*** |
| Method (Cutting) | 0.08 | 0.50 | 0.16 |
| NSSI Med Sev | −2.40 | 0.91 | −2.63** |
| NSSI Frequency | −0.13 | 0.15 | −0.87 |
| Suicide Attempt | 0.93 | 0.61 | 1.53 |
| Brooding | 0.14 | 0.04 | 3.54*** |
| NSSI Scar Frequency | 0.51 | 0.25 | 2.07* |
| Brooding x Scar Frequency | 0.29 | 0.04 | 8.37*** |
|
| |||
| ΔR2 = .15, F =69.97, p < .001 | |||
p < .05,
p < .01,
p < .001.
Note. BDI = Beck Depression Inventory; NSSI = Non suicidal self-injury; NSSI Med Sev = Non-suicidal self-injury medical lethality. Linear regressions were conducted to examine these hypotheses; thus, the full sample (N = 231) was included in these analyses.
Figure 1.
Brooding moderates the relationship between scar presence and suicidal ideation
Figure 2.
Brooding moderates the relationship between scar frequency and suicidal ideation
4. Discussion
This study is the first examination of the association between NSSI and STBs. We hypothesized that the presence and number of NSSI scars would predict current SI as well as be associated with SA history. We further hypothesized that the association between scarring and SI and SAs would be amplified among individuals with a tendency to brood. Generally, the results were consistent with our hypotheses. First, both NSSI scar presence and frequency predicted current SI, even after controlling for current depressive symptoms, history of SAs, NSSI frequency, method, and medical severity. Second, both of these relationships were moderated by the presence of brooding, such that scar presence and number predicted SI only at high levels of brooding. Third, contrary to our hypotheses, although scar presence and number were associated with SA history in independent logistic regressions controlling for current depressive symptoms, when controlling for NSSI frequency, method, and medical severity, these relationships no longer were significant.
To our knowledge, this is the first study to report the extent of NSSI scarring among self-injurers, and in community samples in general. Among those in our sample endorsing a history of NSSI, over half reported at least one permanent scar from the behavior and the majority with scarring reported two or more scars. Moreover, individuals with NSSI scars engaged in NSSI more frequently and were more likely to report that their NSSI resulted in hospitalization or injury severe enough to require medical treatment than individuals without scars. This demographic information alone suggests that scars secondary to NSSI are relatively common and hold immense importance.
Yet, most notable was the finding that the presence and frequency of NSSI scars predicted SI beyond SA history, current depressive symptoms, NSSI frequency, method, and medical severity. By controlling for these NSSI characteristics, the results indicate that the presence of NSSI scars may be a stronger predictor of STBs than the occurrence of NSSI, and that there may be something specific about scarring that heightens risk for SI. This is a significant addition to the current literature, as NSSI presence, frequency, and method are typically believed to be some of the strongest indicators of suicide risk (e.g., Wilkinson et al., 2011; Whitlock et al., 2013).
State dependent memory (for review see Bower, 1981) may be at least partially responsible for the association between scars and SI. Speculatively, it may be that when an individual views one’s scar, it conjures up memories related to the events that provoked NSSI engagement as well as memories of the experience from when that scar was formed. These memories then may induce a phenomenological experience that contains similar negative mood states associated with the prior self-injury. In turn, these negative mood states, often characterized by self-criticism and brooding (Claes et al., 2010; Klonsky, 2007; Selby et al., 2008), are risk factors for STBs (Morrison and O’Connor, 2008; Stange et al., 2015).
Our findings further suggest that the presence and number of scars may heighten the risk of current SI more strongly among individuals with greater ruminative brooding. These results are consistent with the cognitive catalyst model and suggest that brooding may amplify the extent to which scars confer risk for SI. This interaction is also consistent with our speculations regarding state dependent memory, as viewing one’s scars may activate negative cognitive and affective states (e.g., painful memories) that are exacerbated by brooding, perhaps leading to SI as a potential means of escape. Surprisingly, our moderation results also suggest that NSSI scarring might be protective against current SI among those with low levels of brooding. For those who do not engage in brooding, scars may serve as useful reminders of a difficult past that one has persevered through, demonstrating one’s ability to overcome difficulties in the future, thereby decreasing SI risk. However, this interpretation is speculative and future research is needed to confirm such a crossover interaction before drawing firm conclusions.
Finally, contrary to our hypothesis, neither scar presence nor number predicted SA history when controlling for NSSI characteristics of frequency, method, and medical severity. It is important to note, however, that our data do not contain information regarding when the SA occurred. Thus, the temporal relationship between NSSI scar formation and SA is unclear, making it difficult to know the directionality of effects. Indeed, research suggests that individuals are as likely to engage in NSSI before SAs as after SAs (Whitlock et al., 2012).
4.1 Clinical Implications
This study’s findings suggest several possible targets for suicide risk assessment and intervention. First, assessing presence and number of scars will be important to quantify risk for suicide-relevant outcomes. The presence and number of NSSI scars are likely more reliable measures of suicide risk among self-injurers than self-report NSSI presence, frequency, and method. This is particularly useful for clinicians seeking an accurate risk assessment in circumstances in which practitioners may suspect that a patient is not divulging all salient information, a situation common in suicide risk assessments (Busch et al., 2003). Second, treatment protocols aimed at decreasing ruminative brooding (e.g. rumination-focused cognitive behavioral therapy; Watkins et al., 2011) may build resilience to STBs, among those with NSSI scarring.
4.2 Limitations and Future Directions
This is a novel study of the association between NSSI scarring and suicide-related outcomes and the interactive association with brooding. However, several limitations should be acknowledged. First, the measures in the study assessed phenomena across different periods of time and associations were only tested concurrently, precluding an evaluation of whether scars truly precede STBs. Longitudinal designs are a logical next step to make causal claims about the directionality of relationships and determine if scars predict STBs prospectively. However, given that we measured SI experienced over the past week, it is highly likely that scars were formed prior to our measurement of SI. Second, the current study only controlled for depressive symptoms; however, it is possible that other mental disorders may account for the associations identified in this study. For example, NSSI has been found to occur among individuals with personality disorders (Gerson and Stanley, 2002) and eating disorders (Svirko and Hawton, 2007), and future studies may consider controlling for such symptomatology. Third, our sample included only 15 individuals who endorsed a SA history, limiting our power to detect significant effects. Thus, we were unable to examine the potential interactive effects of brooding and scarring on SAs. Notably, the low base rate of SAs in our sample is likely attributable to the non-clinical sample utilized in the present study. Future research should seek to attain larger sample sizes or specifically select a sample for SAs to evaluate whether scars confer risk for future SAs. Future studies also may consider employing a large sample of individuals from both community and psychiatric settings to both attain higher numbers of those with NSSI to ensure sufficient power when replicating results and to ensure the generalizability of results. Fourth, although SI and SA have conceptual overlap, not all individuals who experience SI go on to make a SA, so the extent to which our results involving SI would extend to SA is not clear. Indeed, there is some evidence that SI and SA may serve as different phenotypes (Brezo et al. 2006; Mann et al. 2009), a possibility that should be explored further in future research. Finally, all study measures were self-report and the appraisal of bodily disfigurement is subjective (Cash, 2004). Future research should have impartial observers appraise NSSI scars to gain more objective information about NSSI scar presence, surface area, discoloration, number, and locations. However, given the low base rate and distinctly private nature of NSSI, self-report does seem a reasonable mode of assessment for novel preliminary analyses.
In the current study, medical severity of NSSI was operationalized as requiring medical treatment or hospitalization due to NSSI. Although NSSI scarring was significantly correlated with medical severity in our sample (see Table 2), NSSI scarring remained significant in predicting SI after controlling for NSSI medical severity (in addition to other commonly employed proxy variables for NSSI severity, such as NSSI method and NSSI frequency). However, it is possible that NSSI scarring may represent self-injuries that resulted in physical injury to the tissue, but were not medically severe enough to require medical intervention. In fact, in the current sample, only 9% of self-injurers reported having ever received medical attention for their NSSI, generally in line with prevalence estimates from other large samples of undergraduates (e.g. 5% in a sample of 1,776 self-injurers; Whitlock et al., 2011). On the other hand, among those with a positive history of NSSI in the current sample, 55% reported at least one permanent scar from the behavior. In this sense, scarring may identify a subset of medically significant self-injuries not requiring medical treatment, which in turn, may explain a portion of the variance in the relationship between scarring and SI. For example, it is possible that an individual may have engaged in NSSI only on one or two occasions using a non-severe method, and never needed medical intervention; with the field’s current understanding, this individual may not be identified as at particularly high suicide attempt risk. Our study suggests otherwise and highlights the importance of amending assessment tools to inquire about NSSI scarring, which can occur even if these other NSSI severity cutoffs are not met. Future research might further examine this mechanism in explaining the relationship between scarring and STBs utilizing a more fine-grained assessment of scarring by impartial observers (as mentioned previously) to better capture the physical severity of scarring.
4.3 Conclusions
This study significantly extends extant NSSI research by finding that the permanent consequences of NSSI serve as an objective physical indicator of risk for STBs. Importantly, NSSI scar presence and number predicted current SI, beyond a history of SBs and other characteristics of NSSI (i.e., frequency, method, and medical severity). Moreover, ruminative brooding moderated this relationship. These results have substantial implications for clinical assessment. Furthermore, our findings emphasize the importance of studying the prevalence of NSSI scarring in a range of populations and in understanding their psychosocial correlates and prospective relationships with negative outcomes.
Acknowledgments
Taylor A. Burke was supported by a National Science Foundation Graduate Research Student Fellowship. Jessica L. Hamilton was supported by National Research Service Award F31MH106184 from NIMH. Jonathan P. Stange was supported by National Research Service Award F31MH099761 from NIMH. Lauren B. Alloy was supported by the National Institute of Mental Health grant MH77908.
Footnotes
Contributors: Taylor A. Burke contributed to the study design, data collection, analyses, and manuscript preparation. Jessica L. Hamilton contributed to the study design, data collection, and manuscript preparation. Jonah N. Cohen contributed to study design and manuscript preparation. Jonathan P. Stange contributed to data analyses and manuscript preparation. Lauren Alloy contributed to manuscript preparation.
The funding sources had no role in study design, in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andover MS, Gibb BE. Non-suicidal self-injury, attempted suicide, and suicidal intent among psychiatric inpatients. Psychiatry Res. 2010;178:101–105. doi: 10.1016/j.psychres.2010.03.019. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Porta G, Spirito A, et al. Suicide attempts and nonsuicidal self-Injury in the treatment of resistant depression in adolescents: Findings from the TORDIA study. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:772–781. doi: 10.1016/j.jaac.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. 2. San Antonio, TX: The Psychological Association; 1996. BDI-II. [Google Scholar]
- Beck A, Steer R. Beck Scale for Suicide Ideation Manual. San Antonio, TX: Harcourt Brace; 1991. [Google Scholar]
- Beck AT, Steer RA, Ranieri WF. Scale for Suicide Ideation: psychometric properties of a self-report version. J Clin Psychol. 1988;44:499–505. doi: 10.1002/1097-4679(198807)44:4<499::aid-jclp2270440404>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Bower GH. Mood and memory. American Psychologist. 1981;36:129. doi: 10.1037//0003-066x.36.2.129. [DOI] [PubMed] [Google Scholar]
- Brausch AM, Boone SD. Frequency of nonsuicidal self-injury in adolescents: Differences in suicide attempts, substance use, and disordered eating. Suicide Life Threat. 2015 doi: 10.1111/sltb.12155. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Brausch AM, Muehlenkamp JJ. Body image and suicidal ideation in adolescents. Body Image. 2007;4:207–212. doi: 10.1016/j.bodyim.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Brezo J, Paris J, Turecki G. Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: a systematic review. Acta Psychiatrica Scandinavica. 2006;113:180–206. doi: 10.1111/j.1600-0447.2005.00702.x. [DOI] [PubMed] [Google Scholar]
- Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. J Clin Psychiatry. 2003;64:14–19. doi: 10.4088/jcp.v64n0105. [DOI] [PubMed] [Google Scholar]
- Burke TA, Stange JP, Hamilton JL, et al. Cognitive and emotion-regulatory mediators of the relationship between behavioral approach system sensitivity and nonsuicidal self-injury frequency. Suicide Life Threat. 2015 doi: 10.1111/sltb.12145. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. [Accessed April 5, 2015];Web-based Injury Statistics Query and Reporting System (WISQARS) website. www.cdc.gov/injury/wisqars/index.html. Updated April 5, 2015.
- Darke S, Torok M, Kaye S, Ross J. Attempted suicide, self-harm, and violent victimization among regular illicit drug users. Suicide Life Threat. 2010;40:587–596. doi: 10.1521/suli.2010.40.6.587. [DOI] [PubMed] [Google Scholar]
- Chioqueta AP, Stiles TC. Psychometric properties of the Beck Scale for Suicide Ideation: A Norwegian study with university students. Nordic Journal of Psychiatry. 2006;60:400–404. doi: 10.1080/08039480600937645. [DOI] [PubMed] [Google Scholar]
- Ciesla JA, Roberts JE. Rumination, negative cognition, and their interactive effects on depressed mood. Emotion. 2007;7:555–565. doi: 10.1037/1528-3542.7.3.555. [DOI] [PubMed] [Google Scholar]
- Claes L, Houben A, Vandereycken W, et al. Brief report: The association between non-suicidal self-injury, self-concept and acquaintance with self-injurious peers in a sample of adolescents. Journal of Adolescence. 2010;33:775–778. doi: 10.1016/j.adolescence.2009.10.012. [DOI] [PubMed] [Google Scholar]
- Cohen JN, Heimberg RG, Burke TA, et al. The interaction of affective states and cognitive vulnerabilities in the prediction of non-suicidal self-injury. Cognition and Emotion 2015. 2014;29:539–9. doi: 10.1080/02699931.2014.918872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer A, Hennrich L, Borgmann E, White AJ, Alpers GW. Body image and noticeable self-inflicted scars. J Nerv Ment Dis. 2013;201:1080–1084. doi: 10.1097/NMD.0000000000000057. [DOI] [PubMed] [Google Scholar]
- Dyer A, Mayer-Eckhard L, White AJ, Alpers GW. The role of scar origin in shaping men’s body image. American Journal of Men’s Health 2015. 2014;9:115–123. doi: 10.1177/1557988314531446. [DOI] [PubMed] [Google Scholar]
- Fliege H, Kocalevent R, Walter OB, et al. Three assessment tools for deliberate self-harm and suicide behavior: evaluation and psychopathological correlates. J Psychosom Res. 2006;61:113–121. doi: 10.1016/j.jpsychores.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Gerson J, Stanley B. Suicidal and self-injurious behavior in personality disorder: Controversies and treatment directions. Current Psychiatry Reports. 2002;4:30–38. doi: 10.1007/s11920-002-0009-6. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Klonsky ED. Social context during non-suicidal self-injury indicates suicide risk. Personality and Individual Differences. 2009;46:25–29. [Google Scholar]
- Gratz KL. Measurement of deliberate self-harm: Preliminary data on the deliberate self-harm inventory. Journal of Psychopathology and Behavioral Assessment. 2001;23:253–263. [Google Scholar]
- Gratz KL, Conrad SD, Roemer L. Risk factors for deliberate self-harm among college students. American Journal of Orthopsychiatry. 2002;72:128–140. doi: 10.1037//0002-9432.72.1.128. [DOI] [PubMed] [Google Scholar]
- Greist JH, Gustafson DH, Stauss FF, Rowse GL, Laughren TP, Chiles JA. A computer interview for suicide-risk prediction. Am J Psychiatry. 1973;130:1327–1332. doi: 10.1176/ajp.130.12.1327. [DOI] [PubMed] [Google Scholar]
- Kaplan ML, Asnis GM, Sanderson WC, Keswani L, De Lecuona JM, Joseph S. Suicide assessment: clinical interview vs. self-report. J Clin Psychol. 1994;50:294–298. doi: 10.1002/1097-4679(199403)50:2<294::aid-jclp2270500224>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Klonsky ED. The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review. 2007;27:226–239. doi: 10.1016/j.cpr.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Arango VA, Avenevoli S, et al. Candidate endophenotypes for genetic studies of suicidal behavior. Biol Psychiatry. 2009;65:556–63. doi: 10.1016/j.biopsych.2008.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison R, O’Connor RC. A systematic review of the relationship between rumination and suicidality. Suicide Life Threat. 2008;38:523–538. doi: 10.1521/suli.2008.38.5.523. [DOI] [PubMed] [Google Scholar]
- Nock MK, Joiner J, Thomas E, et al. Non-suicidal self-injury among adolescents: Diagnostic correlates and relation to suicide attempts. Psychiatry Res. 2006;144:65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ. A functional approach to the assessment of self-mutilative behavior. Journal of Consulting and Clinical Psychology. 2004;72:885–890. doi: 10.1037/0022-006X.72.5.885. [DOI] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ. Contextual features and behavioral functions of self-mutilation among adolescents. J Abnorm Psychol. 2005;114:140–146. doi: 10.1037/0021-843X.114.1.140. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. J Abnorm Psychol. 1991;100:569. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- O’Connor RC, Noyce R. Personality and cognitive processes: Self-criticism and different types of rumination as predictors of suicidal ideation. Behaviour Research and Therapy. 2008;46:392. doi: 10.1016/j.brat.2008.01.007. [DOI] [PubMed] [Google Scholar]
- Paul E, Tsypes A, Eidlitz L, Ernhout C, Whitlock J. Frequency and functions of non-suicidal self-injury: associations with suicidal thoughts and behaviors. Psychiatry Res. 2015;225:276–282. doi: 10.1016/j.psychres.2014.12.026. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Nock MK, Simon V, Aikins JW, Cheah CSL, Spirito A. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. J Consult Clin Psychol. 2008;76:92–103. doi: 10.1037/0022-006X.76.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saraff PD, Pepper CM. Functions, lifetime frequency, and variety of methods of non-suicidal self-injury among college students. Psychiatry Res. 2014;219:298–304. doi: 10.1016/j.psychres.2014.05.044. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. MyiLibrary. Mindfulness-Based Cognitive Therapy for Depression. New York: Guilford Press; 2013. [Google Scholar]
- Stange JP, Boccia AS, Shapero BG, et al. Emotion regulation characteristics and cognitive vulnerabilities interact to predict depressive symptoms in individuals at risk for bipolar disorder: A prospective behavioral high-risk study. Cognition & Emotion. 2013;27:63–84. doi: 10.1080/02699931.2012.689758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Hamilton JL, Burke TA, et al. Negative cognitive styles synergistically predict suicidal ideation in bipolar spectrum disorders: A 3-year prospective study. Psychiatry Res. 2015;226:162–168. doi: 10.1016/j.psychres.2014.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Roberti JW, Roth DA. Factor structure, concurrent validity, and internal consistency of the Beck Depression Inventory-Second Edition in a sample of college students. Depress Anxiety. 2004;19:187–189. doi: 10.1002/da.20002. [DOI] [PubMed] [Google Scholar]
- Surrence K, Chan S, Miranda R. Subtypes of rumination in the relationship between negative life events and suicidal ideation. Arch Suicide Res. 2009;13:123. doi: 10.1080/13811110902835015. [DOI] [PubMed] [Google Scholar]
- Svirko E, Hawton K. Self-injurious behavior and eating disorders: the extent and nature of the association. Suicide & Life-Threatening Behavior. 2007;37:409–421. doi: 10.1521/suli.2007.37.4.409. [DOI] [PubMed] [Google Scholar]
- Toprak S, Cetin I, Guven T, Can G, Demircan C. Self-harm, suicidal ideation and suicide attempts among college students. Psychiatry Research. 2011;187:140–144. doi: 10.1016/j.psychres.2010.09.009. [DOI] [PubMed] [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27:247–259. [Google Scholar]
- U.S. Department of Education. Digest of Education Statistics. N.p: National Center for Education Statistics; [Google Scholar]
- Watkins ER, Mullan E, Wingrove J, et al. Rumination-focused cognitive-behavioural therapy for residual depression: Phase II randomised controlled trial. The British Journal of Psychiatry: The Journal of Mental Science. 2011;199:317. doi: 10.1192/bjp.bp.110.090282. [DOI] [PubMed] [Google Scholar]
- Weaver TL, Resnick HS, Kokoska MS, Etzel JC. Appearance-related residual injury, posttraumatic stress, and body image: Associations within a sample of female victims of intimate partner violence. J Trauma Stress. 2007;20:999–1008. doi: 10.1002/jts.20274. [DOI] [PubMed] [Google Scholar]
- Whitlock J, Eckenrode J, Silverman D. Self-injurious behaviors in a college population. Pediatrics. 2006;117:1939–1948. doi: 10.1542/peds.2005-2543. [DOI] [PubMed] [Google Scholar]
- Whitlock J, Knox KL. The relationship between self-injurious behavior and suicide in a young adult population. Arch Pediatr Adolesc Med. 2007;161:634–640. doi: 10.1001/archpedi.161.7.634. [DOI] [PubMed] [Google Scholar]
- Whitlock J, Muehlenkamp J, Eckenrode J, et al. Nonsuicidal self-injury as a gateway to suicide in young adults. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2013;52:486–492. doi: 10.1016/j.jadohealth.2012.09.010. [DOI] [PubMed] [Google Scholar]
- Whitlock J, Muehlenkamp J, Purington A, Eckenrode J, Barreira P, Baral Abrams G, Knox K. Nonsuicidal self-injury in a college population: General trends and sex differences. Journal of American College Health. 2011;59:691–698. doi: 10.1080/07448481.2010.529626. [DOI] [PubMed] [Google Scholar]
- Wilcox HC, Arria AM, Caldeira KM, et al. Longitudinal predictors of past-year non-suicidal self-injury and motives among college students. Psychol Med. 2012;42:717–726. doi: 10.1017/S0033291711001814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson P, Kelvin R, Roberts C, et al. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the adolescent depression antidepressants and psychotherapy trial (ADAPT) Am J Psychiatry. 2011;168:495–501. doi: 10.1176/appi.ajp.2010.10050718. [DOI] [PubMed] [Google Scholar]