Abstract
Background
Environmental and host predictors of asthma control in older asthmatic patients (>65 years old) are poorly understood.
Objective
To examine the effects of residential exposure to traffic exhaust and other environmental and host predictors on asthma control in older adults.
Methods
One hundred four asthmatic patients 65 years of age or older from allergy and pulmonary clinics in greater Cincinnati, Ohio, completed the validated Asthma Control Questionnaire (ACQ), pulmonary function testing, and skin prick testing to 10 common aeroallergens. Patients had a physician’s diagnosis of asthma, had significant reversibility in forced expiratory volume in 1 second or a positive methacholine challenge test result, and did not have chronic obstructive pulmonary disease. The mean daily residential exposure to elemental carbon attributable to traffic (ECAT) was estimated using a land-use regression model. Regression models were used to evaluate associations among independent variables, ACQ scores, and the number of asthma exacerbations, defined as acute worsening of asthma symptoms requiring prednisone use, in the past year.
Results
In the adjusted model, mean daily residential exposure to ECAT greater than 0.39 µg/m3 was significantly associated with poorer asthma control based on ACQ scores (adjusted β = 2.85; 95% confidence interval [CI], 0.58–5.12; P = .02). High ECAT levels were also significantly associated with increased risk of asthma exacerbations (adjusted odds ratio, 3.24; 95% CI, 1.01–10.37; P = .05). A significant association was found between higher body mass index and worse ACQ scores (adjusted β = 1.15; 95% CI, 0.53–1.76; P < .001). Atopic patients (skin prick test positive) had significantly better ACQ scores than nonatopic patients (adjusted β = −0.39; 95% CI, −0.67 to −0.11; P < .01).
Conclusion
Higher mean daily residential exposure to traffic exhaust, obesity, and nonatopic status are associated with poorer asthma control among older asthmatic patients.
Introduction
The burden of asthma on adults 65 years and older is substantial and underappreciated.1–3 Up to two-thirds of asthma-related deaths occur in adults 65 years and older.4,5 The prevalence of asthma in this age group is as high as 10%.3,4 High morbidity rates and decreased quality of life associated with asthma are also characteristic of this population.1,6 Despite evidence suggesting that older asthmatic patients may represent a more severe clinical phenotype with distinct mechanisms of airways inflammation, studies regarding the causes of high morbidity and mortality are lacking.2,3
Environmental exposures and host factors contributing to poor asthma control in older asthmatic patients are poorly understood. 1,3 Because of age-related decline in antioxidant defenses, older asthmatic patients may be especially susceptible to the effects of air pollutants, including traffic exhaust.7 Older asthmatic patients may be at increased risk of hospital admissions and reduced lung function due to acute elevations in nitrogen dioxide, ozone, and particles with diameters less than 2.5 µm.8,9 Previous studies also indicate that they might be at higher risk for poorly controlled asthma due to long-term exposure to nitrogen dioxide and ozone.10,11 Notably, these studies did not evaluate the effect of ultrafine particles (<100 nm), an important component of diesel exhaust exhibiting a strong spatial gradient and associated with significant health consequences in younger populations.12 In addition, these studies did not incorporate validated measures of asthma control.13,14 Thus, further study regarding the effect of long-term, residential exposure to traffic pollutants, including diesel exhaust, on asthma control in older adults is warranted.1,11
The objective of this study was to examine the relationship between mean daily residential exposure to traffic exhaust and asthma control in asthmatic patients 65 years and older. Our hypothesis was that higher mean daily exposure to elemental carbon attributable to traffic (ECAT), a surrogate for diesel particulate exposure, would be significantly associated with poorer asthma control.15,16
Methods
Study participants
To test this hypothesis, we conducted a study of 104 asthmatic patients 65 years or older recruited from 2 allergy and pulmonary clinical practices in greater Cincinnati, Ohio, and from the Cincinnati Veterans Administration Allergy Clinic. These practices included patient residences that were distributed across the greater Cincinnati area, had approximately equal numbers of males and females (in aggregate), and provided a study sample that was enriched for more severe asthma phenotypes. All potential study participants from these practices with a physician’s diagnosis of asthma who were 65 years or older as of April 1, 2010, and lived in greater Cincinnati were invited to participate. Study inclusion required objective confirmation of asthma, including either: (1) 12% or greater and 200-mL or greater improvement in forced expiratory volume in 1 second (FEV1) after administration of inhaled albuterol; or (2) a positive methacholine challenge test result based on American Thoracic Society criteria (provocation concentration that caused a decrease in FEV1 of 20% at or below 4 mg/mL).17,18 Exclusion criteria included a physician’s diagnosis of chronic obstructive pulmonary disease or class 3 or greater congestive heart failure. Enrollment proceeded simultaneously from the 3 sites. Between April 2010 and March 2011, 225 potential study participants initially identified by International Classification of Diseases, Ninth Revision (ICD-9) codes were contacted by telephone, and 122 consented to a screening visit. Of these, 18 did not meet inclusion and exclusion criteria. Participants signed an informed consent approved by the University of Cincinnati institutional review board.
Data collection
Enrolled patients completed a standardized, close-ended questionnaire that included demographics (sex, race, income, residence, and employment), tobacco exposure (current and previous, first- and second-hand, quantity, and years exposed), age of asthma onset, and other medical comorbidities. Medical history was obtained by a board-certified allergist and verified with medical records. Patients completed the Asthma Control Questionnaire (ACQ), and spirometry was performed according to American Thoracic Society guidelines.19,20 Height and weight were recorded, and a physical examination was performed. Skin prick testing (SPT) was performed for 10 common regional aeroallergens (cat, dog, timothy grass, white oak, maple mix, short ragweed, dust mite mix [50% Dermatophagoides farinae and 50% Dermatophagoides pteronyssinus], Alternaria alternata, Aspergillus fumigatus, and German cockroach [ALK-Abell00F3;, Round Rock, Texas]). A positive SPT result was defined as a wheal at least 3 mm in diameter greater than the saline control along with a flare larger than the accompanying wheal.
Exposure to traffic-related air pollutants
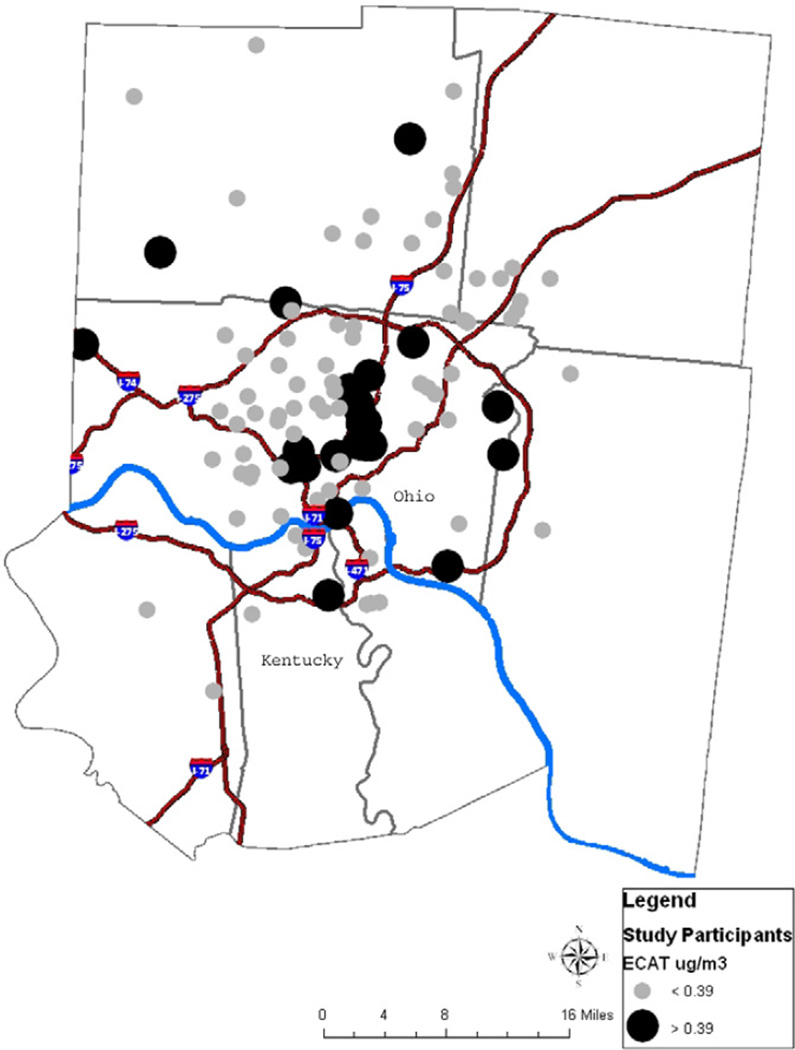
The mean daily concentration of ECAT was estimated using a previously developed land-use regression (LUR) model.12,15 LUR models integrate traffic and local geographic and land-use variables in estimating air pollution exposure.16 The model for this study was based on ambient air sampling conducted at 27 sites from December 2001 to December 2006. The mean daily concentration of ECAT for each sampling site was determined.12 The final LUR model relating ECAT measured at the 27 sampling sites to land-use and traffic variables had an r2 of 0.73 and included elevation, truck traffic within 400 m, and length of bus routes within 100 m.15 Repeat sampling conducted in 2010 at 4 sites indicated that the concentration of elemental carbon in ambient air was consistent and similar to the concentrations in 2001–2006 (S. Grinshpun unpublished data 2011). Residential addresses from participants in this study were geocoded using EZLocate (TeleAtlas, Lebanon, New Hampshire) and ArcGIS 9.0 (Environmental Systems Research Institute, Redlands, California). The LUR model was applied to estimate ECAT exposure based on the patient’s current residential address (Fig 1).
Fig. 1.
Map of elemental carbon attributable to traffic (ECAT) estimates based on residential addresses for 104 asthmatic patients 65 years or older from Cincinnati, Ohio. Larger, darker circles indicate ECAT concentrations of 0.39 to 0.63 µg/m3; smaller, lighter circles represent ECAT concentrations of 0.23 to 0.38 µg/m3. Thin, dark lines represent interstates or highways. The thick blue line is the Ohio river and county lines are gray.
Outcome measures
The primary outcome measure was the validated 6-item ACQ, which captures information regarding asthma symptoms and rescue medication use (short-acting bronchodilator) during the previous week. The ACQ was originally developed based on the input of expert physicians and demonstrates strong evaluative and discriminative properties for both clinical and cross-sectional studies.19–22 The 7-item ACQ, which includes prebronchodilator FEV1, was also evaluated. In the principal analyses, ACQ scores were analyzed continuously, given that various cut points to define control exist in the literature (ie, >1 or <1, >0.83 or <0.83, >1.5, etc).13,23 The number of asthma exacerbations in the last year, defined as acute worsening of asthma symptoms requiring prednisone, was a secondary outcome measure. On the basis of the Expert Panel Report 3 guidelines, 2 or more courses of prednisone per year identify patients at increased risk for severe exacerbations.24 The number of unscheduled visits to a physician or the emergency department for treatment of asthma in the last year was also examined. Unscheduled visits were self-reported and confirmed by medical records when available.
Statistical analysis
A general linear regression model was applied to investigate the association between the covariates and the ACQ score. Body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) and ECAT concentration were log-transformed to approximate normality. Atopy was defined as at least 1 positive SPT result to a panel of 10 common aeroallergens. Potential covariates listed in Tables 1 and 2 were removed by a backward elimination based on P < .15. The linear and nonlinear components of the relationship between ACQ scores and the log of ECAT were evaluated by smooth curves fitted to predicted values of ACQ from generalized additive models that included all final covariates. Straight lines (linear spline functions), defined on separate intervals of the log of ECAT where generalized additive model slopes changed, were included in the final multiple linear regression models and slope parameters were tested for significance. The lines were connected at an ECAT concentration of 0.39 µg/m3, which was identified as the point above which the effect of ECAT on asthma control increased and was statistically significant.
Table 1.
Characteristics of 104 asthmatic patients 65 years or older and mean 6-item ACQ scoresa
| Characteristic | No. (% of 104 with characteristic) |
Mean (SD) ACQ score |
|---|---|---|
| Age, y | ||
| 65–69 | 38 (37) | 0.64 (0.79) |
| 70–74 | 26 (25) | 0.73 (0.80) |
| 75–79 | 20 (19) | 0.63 (0.63) |
| >80 | 20 (19) | 0.68 (0.61) |
| Male | 51 (49) | 0.59 (0.74) |
| Female | 53 (51) | 0.75 (0.70) |
| Race/ethnicity | ||
| White | 83 (80) | 0.64 (0.70) |
| African American | 17 (16) | 0.72 (0.83) |
| Hispanic | 3 (3) | 1.11 (0.92) |
| Asian | 1 (1) | 0.67 |
| Annual income, $ | ||
| <40,000 | 46 (44) | 0.79 (0.82) |
| >40,000 | 58 (56) | 0.57 (0.63) |
| Body mass index | ||
| <25 | 23 (23) | 0.54 (0.50) |
| 25–29.99 | 37 (35) | 0.50 (0.52) |
| 30–34.99 | 25 (24) | 0.57 (0.61) |
| >35 | 19 (18) | 1.27 (1.08) |
| GERDb | 62 (60) | 0.80 (0.79) |
| No GERD | 42 (40) | 0.47 (0.55) |
| Atopic (SPT positive)c | 72 (70) | 0.57 (0.73) |
| Nonatopic | 31 (30) | 0.91 (0.67) |
| Mixed rhinitisd (both nonallergic and allergic triggers) | 48 (47) | 0.78 (0.87) |
| Allergic or nonallergic triggers for rhinitis (not both) | 54 (53) | 0.55 (0.55) |
| Age of asthma symptom onset, ye,f | ||
| 0–18 | 29 (28) | 0.62 (0.78) |
| 19–40 | 28 (27) | 0.72 (0.71) |
| 41–64 | 34 (33) | 0.74 (0.78) |
| >65 | 13 (12) | 0.47 (0.44) |
Abbreviations: ACQ, Asthma Control Questionnaire; GERD, gastroesophageal reflux disease; SPT, skin prick test.
A higher ACQ score indicates poorer asthma control.
On the basis of previous physicians’ diagnosis.
At least 1 positive SPT result to a panel of 10 aeroallergens. Data available for 103 subjects.
Mixed rhinitis included a previous diagnosis, verified by medical records, of both nonallergic and allergic triggers for rhinitis. The reference group included patients without rhinitis or with either allergic or nonallergic triggers for rhinitis (but not both). Data available for 102 patients.
Wheezing, shortness of breath, or chronic cough not explained by another health problem.
Additional characteristics included a physician’s diagnosis of chronic rhinitis (n = 99 [95%]), allergic rhinitis (n = 76 [73%]), nasal polyps (n = 23 [22%]), chronic rhinosinusitis (n = 19 [18%]), eczema or atopic dermatitis (n = 16 [16%]), eosinophilic esophagitis (n = 1 [1%]), and work-related asthma (n = 8 [8%]).
Table 2.
Exposures reported for 104 asthmatic patients 65 years or older and mean 6-item ACQ scoresa
| Exposure | No. (% of 104 with characteristic) |
Mean (SD) ACQ score |
|---|---|---|
| Personal tobacco useb | ||
| Ever smoked cigarettes, cigars, or a pipe | 52 (50) | 0.76 (0.79) |
| Never smoked | 52 (50) | 0.57 (0.65) |
| Smoke = 10 pack-years | 26 (25) | 0.64 (0.63) |
| Smoked >10 pack-years | 78 (75) | 0.68 (0.76) |
| Second-hand tobacco exposureb | ||
| Ever lived with a smoker | 80 (77) | 0.68 (0.66) |
| Never lived with a smoker | 24 (23) | 0.61 (0.92) |
| ECAT concentrationc | ||
| Low (0.23–0.38 µg/m3) | 77 (75) | 0.59 (0.59) |
| High (0.39–0.63 µg/m3) | 25 (25) | 0.93 (1.02) |
Abbreviations: ACQ, Asthma Control Questionnaire; ECAT, elemental carbon attributable to traffic.
A higher ACQ score indicates poorer asthma control.
Pack-years is number of years smoked times number of packs per day. One cigar or pipe equals one pack of cigarettes. The mean (SD) ACQ score for current smokers (n = 2) was 0.25 (0.35). The mean (SD) ACQ score for patients currently living with a smoker (n = 2) was 0.33 (0.47).
Low vs high ECAT exposure was based on a linear spline model. Data available for 102 patients.
To further evaluate the association between ECAT concentration and BMI, post hoc stratified analyses of the final regression model were performed for patients with BMIs less than 30 vs 30 or higher (the clinical cut point for obesity), and slopes of ECAT were compared. A separate logistic regression analysis was also conducted to evaluate the effect of a BMI of 30 or higher on asthma control. For this analysis, the ACQ score was dichotomized at 1.5, a validated clinical cut point for poorly controlled asthma.13 Other independent variables are consistent with those included in the final general linear model for ACQ. Additional statistical methods are included in the online supplement.
Results
Cohort description
Characteristics of the 104 patients and their mean 6-item ACQ scores are presented in Table 1. Approximately half were female, the mean age was 74 years, and the cohort included 83 whites, 17 African Americans, 3 Hispanics, and 1 Asian, which is representative of the greater Cincinnati area. The median income was approximately $40,000. Most were overweight (BMI = 25), with 24% classified as obese and 18% considered morbidly obese. Comorbid gastroesophageal reflux disease (GERD) occurred in 60%. On the basis of a previous physician’s diagnosis, 47% had both allergic and nonallergic triggers for rhinitis (mixed rhinitis, a condition thought to be more common in older adults).25 On the basis of SPT results, 70% of participants were atopic. A large number of patients developed asthma later in life, with 45% reporting symptom onset after 40 years of age and 12% after 65 years of age. The mean (SD) prebronchodilator FEV1 was 70.5% (17.8%) of predicted (National Health and Nutrition Examination Survey III predicted set), which is similar to although slightly lower than a community-based sample of older asthmatic patients.26
Exposure variables
The numbers of patients with exposures reported and mean 6-item ACQ scores are presented in Table 2. Consistent with other studies of this age group, 50% reported tobacco use during their lifetime, and 25% had smoked for 10 or more pack-years; only 2 were current smokers. The mean daily ECAT concentration ranged from 0.23 to 0.63 µg/m3. On the basis of the linear spline, 25% had high ECAT concentrations (>0.39 µg/m3). Patients lived at their current address for a mean (SD) of 24 (17) years, and 95% lived in their current homes during the sampling period. They spent a mean (SD) of 124 (30) hours per week (18 hours per day) at home.
Univariate findings for the 6-item ACQ score
Univariate regression coefficients (β) of covariates that were potentially associated (P < .15) with 6-item ACQ scores are listed in Table 3. Higher ACQ scores indicate poorer asthma control; a positive β coefficient therefore signifies that a covariate is associated with poorer asthma control. Findings included an association between a mean daily ECAT concentration of 0.39 µg/m3 or higher and higher ACQ scores (β = 2.43; 95% confidence interval [CI], −0.06 to −4.93; P = .06). Higher BMI levels were significantly associated with higher ACQ scores (β = 1.28; 95% CI, 0.64–1.93; P < .001). GERD was also significantly associated with higher ACQ scores (β = 0.33; 95% CI, 0.06–0.61; P = .02). Consistent with studies indicating that nonatopic asthma may be more difficult to control, being atopic (SPT positive) was significantly associated with lower ACQ scores and thus better asthma control (β = −0.35; 95% CI, −0.65 to −0.05; P = .02).27 There was a trend toward mixed rhinitis (nonallergic and allergic triggers) being associated with higher ACQ scores (β = 0.23; 95% CI, −0.05 to 0.74; P = .11). An annual income of $40,000 or less was associated with higher ACQ scores, although this finding was not statistically significant (β = 0.22; 95% CI, −0.05 to 0.51; P = .11).
Table 3.
Regression analysis of the association between independent variables and ACQ Scores for 104 asthmatic patients 65 years or oldera
| Independent variable | Univariate β (95% CI); P value |
Multivariate β (95% CI); P value |
|---|---|---|
| ECAT concentration, µg/m3 | ||
| 0.23–0.38 | −0.35 (−1.62 to −0.91); .58 | −0.78 (−1.96 to 0.40); .19 |
| 0.39–0.63 | 2.43 (−0.06 to −4.93); .06 | 2.85 (0.58 to 5.12); .02 |
| BMIb | 1.28 (0.64 to 1.93); <.001 | 1.15 (0.53 to 1.76); <.001 |
| GERD (yes vs no) | 0.33 (0.06 to 0.61); .02 | |
| Mixed rhinitis (yes vs no) | 0.23 (−0.05 to 0.74); .11 | 0.28 (0.02 to 0.54); .04 |
| Atopic (SPT positive) (yes vs no) | −0.35 (−0.65 to −0.05); .02 | −0.39 (−0.67 to −0.11); <.01 |
| Annual income <$40,000 (vs >$40,000) | 0.22 (−0.05 to 0.51); .11 |
Abbreviations: ACQ, Asthma Control Questionnaire; BMI, body mass index; CI, confidence interval; ECAT, elemental carbon attributable to traffic; GERD, gastroesophageal reflux disease; SPT, skin prick test.
A general linear model was used to analyze the relationship between the 6-item ACQ score on a continuous scale vs independent variables. A positive β-coefficient indicates poorer asthma control. Variables with P < .15 in the univariate or multivariate analysis are listed. Ninety-nine patients had sufficient data for analysis.
BMI was analyzed as a continuous, log-transformed variable.
Multivariate findings for the 6-item ACQ score
The results of the multivariate model (P < .15) for the 6-item ACQ are also given in Table 3. Mean daily exposure to ECAT concentrations of 0.39 µg/m3 or higher was significantly associated with higher 6-item ACQ scores (adjusted β = 2.85; 95% CI, 0.58–5.12; P = .02). An increase in ECAT concentrations from approximately 0.39 to 0.51 µg/m3 resulted in a 0.5-unit increase in the ACQ score, which is considered a clinically meaningful change.19 The association between ECAT and ACQ scores was not affected by the number of years patients lived at their current address, whether or not they changed addresses during or after the sampling period (5% of patients), or the number of hours they spent at home.
The significant association between BMI and higher ACQ scores also persisted (adjusted β = 1.15; 95% CI, 0.53–1.76; P < .001). Patients with a BMI of 30 or higher (obese) were more than 5 times as likely to have an ACQ score greater than 1.5 (adjusted odds ratio [OR], 5.7; 95% CI, 0.98–33.47; P = .05). In a post hoc analysis, the association between an ECAT concentration of 0.39 µg/m3 or higher and higher 6-item ACQ scores was only present among those with BMIs of 30 or higher (adjusted β = 3.82; 95% CI, −0.19 to 7.83; P = .06) but not among those with BMIs less than 30 (adjusted β = 0.13; 95% CI, −2.76 to 3.02; P = .93). In addition, atopic (SPT positive) patients had significantly lower (better) ACQ scores than nonatopic patients (adjusted β for atopic patients = −0.39; 95% CI, −0.67 to −0.11; P < .01), indicating that nonatopic status (SPT negative) was associated with poorer asthma control. Having mixed rhinitis (non-allergic and allergic triggers) was also significantly associated with higher ACQ scores and therefore poorer asthma control (adjusted β = 0.28; 95% CI, 0.02–0.54; P = .04). Findings for the 7-item ACQ were very similar to those for the 6-item ACQ (data not shown).
Asthma exacerbations in the last year
Eighteen patients were prescribed 2 or more courses of prednisone for asthma exacerbations in the last year (Table 4). Eight of 27 patients (32%) with exposure to ECAT concentrations of 0.39 µg/m3 or higher were prescribed at least 2 courses of prednisone compared with 10 of 77 patients (13%) with exposure to ECAT concentrations of less than 0.39 µg/m3 (P = .03). After adjustment for BMI, atopy, and mixed rhinitis, patients with exposure to ECAT concentrations of 0.39 µg/m3 or higher were more than 3 times more likely to need 2 or more courses of prednisone (adjusted OR, 3.24; 95% CI, 1.01–10.37; P = .05).
Table 4.
Predictors for 2 or more prednisone courses in the last 12 months among 104 asthmatic patients 65 years or oldera
| Independent variable | Adjusted odds ratio (95% CI) |
P value |
|---|---|---|
| High vs low ECAT concentrationb | 3.24 (1.01–10.37) | .05 |
| BMI (25th–75th percentile)c | 2.25 (1.02–4.95) | .04 |
| Atopic (SPT positive)d (yes vs no) | 0.39 (0.12–1.26) | .12 |
| Mixed rhinitis (yes vs no) | 0.85 (0.26–2.76) | .79 |
Abbreviations: ACQ, Asthma Control Questionnaire; BMI, body mass index; CI, confidence interval; ECAT, elemental carbon attributable to traffic; SPT, skin prick test.
Multivariate logistic regression was used in this analysis; 99 patients had sufficient data for analysis. Two or more courses of prednisone were prescribed for 18 patients.
ECAT was analyzed as a dichotomous variable using the cut points from the spline for ACQ (high ECAT concentration defined as >0.39 µg/m3 and low ECAT concentration as <0.39 µg/m3).
BMI was analyzed as a continuous, log-transformed variable. The odds ratio presented is for a change in the log of BMI from the 25th to the 75th percentile.
At least 1 positive SPT result to a panel of 10 aeroallergens.
Thirty-five patients reported 62 unscheduled visits for asthma in the last year (eTable 1). After adjustment for other covariates, those with exposure to ECAT concentrations of 0.39 µg/m3 or higher had significantly higher numbers of unscheduled visits (mean, 1.12) vs those with exposure to ECAT concentrations of less than 0.39 µg/m3 (mean, 0.42; adjusted β = 0.65; 95% CI, 0.08–1.22; P = .03).
Asthma medications in the last month
Asthma medications used in the month before study participation are listed in eTable 2. On the basis of medication use, more than 80% of enrolled patients would be considered to have moderate to severe asthma.24 No significant differences were found in medications used in the last month based on ECAT levels.
Discussion
There are 3.1 million asthmatics 65 years of age and older in the United States, with that number expected to double in the next 25 years.28 Although mortality from asthma overall is less than 2.2 per 100,000 population, asthma-related mortality among older adults is almost 5 times greater, with 10.5 per 100,000 seniors dying of asthma.4 Predictors of asthma control among adults 65 years or older remain poorly understood, despite the increasing prevalence of and high rates of morbidity from asthma in older adults. To our knowledge, this is the first study to demonstrate that mean daily residential exposure to ECAT, a marker of diesel particulate exposure, is associated with significantly poorer asthma control among asthmatic patients 65 years or older. Higher ECAT levels were significantly associated with poorer scores on the validated ACQ and increased asthma exacerbations in the last year. In addition, although previous studies have linked obesity to poor asthma control in younger populations, this study also highlights the importance of obesity in determining asthma symptom control and exacerbations among adults 65 years or older.29 Intriguingly, the association between ECAT and asthma control was also more pronounced among obese individuals.
Studies using LUR methods have demonstrated that exposure to traffic-related particulate matter is associated with persistent wheezing in infants and the development of asthma in children.12,30 Exposure to elevated levels of nitric oxide, ozone, and particulates is associated with increased symptoms and exacerbations in younger asthmatic patients.31–33 Older asthmatic patients may be more susceptible to traffic pollutant effects because of potentially impaired responses to oxidative stress.7,9,11,34 Although there are data from older patients with chronic obstructive pulmonary disease regarding the effect of traffic-related particulates, these data are sparse in asthmatic patients older than 65 years.35,36
In this study, we used a LUR model to explore the relationship between mean daily ECAT exposure and asthma control in asthmatic patients 65 years or older. Previous studies found that ambient levels of elemental carbon reasonably approximate personal exposure levels in older adults, possibly because older adults spend more time at home on average.37 As a marker of diesel exposure, ECAT approximates the distribution of ultrafine particles, which are an important component of diesel exhaust exhibiting high spatial variation.38,39 ECAT estimates for this study were based on mean daily exposure and thus are likely to represent long-term rather than short-term exposure. The significant relationship between mean daily ECAT levels of 0.39 µg/m3 or higher and poorer ACQ scores was robust for both the 6- and 7-item ACQ. The magnitude of this effect also met validated criteria for clinical significance.19 It is noteworthy that the cut point of 0.39 µg/m3 approximates the threshold level of ECAT associated with the development of persistent wheeze during childhood in a recent birth cohort study.12
Asthma exacerbations are recognized as a separate indicator of asthma control (ie, risk domain) and are distinct from the ACQ, which is a measure of impairment.24 Patients with exposure to ECAT levels of 0.39 µg/m3 or higher were 3 times more likely to need 2 or more courses of prednisone for asthma exacerbations in the last year, thereby corroborating the association between ECAT and ACQ in older asthmatic patients. Notably, no differences were found in asthma controller medications in the last month between high and low ECAT exposed groups, indicating that findings related to ECAT cannot be explained by differences in medication use by high- vs low-exposure groups.
The negative effect of obesity on asthma control in younger populations is well described.29 In this study, we present the novel finding that elevated BMI is strongly associated with poorer asthma symptom control (ACQ scores) and increased asthma exacerbations in a population of older asthmatic patients. Obese patients were more than 5 times as likely to have an ACQ score higher than 1.5. The relationship between GERD and ACQ scores was not significant after adjustment for BMI, presumably because obesity is a risk factor for GERD. Obese asthmatic patients may represent a distinct phenotype that is poorly responsive to corticosteroids and characterized by unique inflammatory pathways.40 Pathophysiologic effects related to obesity may be particularly relevant to older asthmatic patients, given the high prevalence of obesity in this age group. The finding that obesity may modify the effect of ECAT exposure is intriguing and may be related to a distinct inflammatory milieu associated with obesity. Future mechanistic studies to explain these findings are warranted.
Consistent with other studies, nonatopic status and mixed (nonallergic and allergic triggers) rhinitis were also associated with poorer asthma control.27,41 In this study, these findings were the same regardless of whether asthma symptoms began later in life or during childhood. These results may have important prognostic and therapeutic implications for older asthmatic patients and should be replicated in a larger population using standardized methods.42
Although findings from this study are robust, there are limitations. We did not evaluate the relationship between other components of traffic exhaust besides ECAT or indoor sources of particulate matter and asthma control. The LUR model was originally developed for the Cincinnati Childhood Allergy and Air Pollution Study.15 Thus, the extent of the network and placement of sampling sites do not optimally represent patients residing in rural locations; however, only 13% lived in rural areas. In addition, ECAT concentrations at these sampling sites were derived from 2001–2006. Regardless, relative exposure (higher vs lower exposure when comparing residences) has remained fairly constant (S. Grinshpun unpublished data, 2011). Furthermore, 95% of patients lived in their current residence during the sampling period (2001–2006). Prospective, longitudinal studies will be needed to clarify the relationship between timing and duration of exposure to high ECAT and asthma control. Nevertheless, it is likely safe to assume that exposure to ECAT in this study was long term because almost all patients lived at their current address from the sampling period to the present and patients spent more than 70% of their time at home.
In summary, to our knowledge, this is the first study demonstrating that mean daily residential exposure to ECAT, a marker of diesel exhaust exposure, was significantly associated with poorer asthma control among asthmatic patients 65 years or older. Findings were robust for both the impairment and risk domains of asthma control. The threshold level of ECAT incurring a significant effect on asthma control was 0.39 µg/m3, which may be similar to the level affecting the development of asthma in children. In addition, obesity and nonatopic status were also associated with poorer asthma control in asthmatic patients 65 years or older. Future studies that will expand on these findings and further define the relationship between air pollution exposure and asthma control in older adults are needed.
Supplementary Material
Acknowledgments
We thank the clinical research staff at the Bernstein Clinical Research Center, the Cincinnati Veterans Administration Clinical Research Unit, Abraham Research Center, and the University of Cincinnati Immunology Clinical Research Center. We are especially grateful to the patients who participated in this study from the Bernstein Allergy Group, the Cincinnati VA Medical Center, and the Fragge Allergy & Asthma Clinic.
Funding Sources: This study was funded by National Institute of Environmental Health Services grants P30-ES006096 and ES11170, US Public Health Service grant UL1 RR026314. The project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant 8KL2 TR000078-04. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosures: Authors have nothing to disclose.
Supplementary data
Supplementary data associated with this article can be found, in the online version, at doi.10.1016/j.anai.2012.04.009.
References
- 1.Diaz-Guzman E, Mannino DM. Airway obstructive diseases in older adults: from detection to treatment. J Allergy Clin Immunol. 2010;126:702–709. doi: 10.1016/j.jaci.2010.08.022. [DOI] [PubMed] [Google Scholar]
- 2.Stupka E, deShazo R. Asthma in seniors, part 1: evidence for underdiagnosis, undertreatment, and increasing morbidity and mortality. Am J Med. 2009;122:6–11. doi: 10.1016/j.amjmed.2008.09.022. [DOI] [PubMed] [Google Scholar]
- 3.Gibson PG, McDonald VM, Marks GB. Asthma in older adults. Lancet. 2010;376:803–813. doi: 10.1016/S0140-6736(10)61087-2. [DOI] [PubMed] [Google Scholar]
- 4.Moorman JE, Rudd RA, Johnson CA, et al. National surveillance for asthma-United States, 1980–2004. MMWR Surveill Summ. 2007;56:1–54. [PubMed] [Google Scholar]
- 5.Australian Centre for Asthma Monitoring. Asthma in Australia 2008. Canberra: Australian Centre for Asthma Monitoring, Australian Institute of Health and Welfare; 2008. [Google Scholar]
- 6.Burrows B, Barbee RA, Cline MG, Knudson RJ, Lebowitz MD. Characteristics of asthma among elderly adults in a sample of the general population. Chest. 1991;100:935–942. doi: 10.1378/chest.100.4.935. [DOI] [PubMed] [Google Scholar]
- 7.Ciencewicki J, Trivedi S, Kleeberger SR. Oxidants and the pathogenesis of lung diseases. J Allergy Clin Immunol. 2008;122:456–468. doi: 10.1016/j.jaci.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson HR, Atkinson RW, Bremner SA, Marston L. Particulate air pollution and hospital admissions for cardiorespiratory diseases: are the elderly at greater risk? Eur Respir J Suppl. 2003;40:39s–46s. doi: 10.1183/09031936.03.00402203. [DOI] [PubMed] [Google Scholar]
- 9.Ko FW, Tam W, Wong TW, et al. Effects of air pollution on asthma hospitalization rates in different age groups in Hong Kong. Clin Exp Allergy. 2007;37:1312–1319. doi: 10.1111/j.1365-2222.2007.02791.x. [DOI] [PubMed] [Google Scholar]
- 10.Meng YY, Wilhelm M, Rull RP, English P, Ritz B. Traffic and outdoor air pollution levels near residences and poorly controlled asthma in adults. Ann Allergy Asthma Immunol. 2007;98:455–463. doi: 10.1016/S1081-1206(10)60760-0. [DOI] [PubMed] [Google Scholar]
- 11.Andersen ZJ, Bonnelykke K, Hvidberg M, et al. Long-term exposure to air pollution and asthma hospitalisations in older adults: a cohort study. Thorax. 2012;67:6–11. doi: 10.1136/thoraxjnl-2011-200711. [DOI] [PubMed] [Google Scholar]
- 12.Ryan PH, Bernstein DI, Lockey J, et al. Exposure to traffic-related particles and endotoxin during infancy is associated with wheezing at age 3 years. Am J Respir Crit Care Med. 2009;180:1068–1075. doi: 10.1164/rccm.200808-1307OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juniper EF, Bousquet J, Abetz L, Bateman ED. Identifying ’well-controlled’ and ’not well-controlled’ asthma using the Asthma Control Questionnaire. Respir Med. 2006;100:616–621. doi: 10.1016/j.rmed.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 14.Bousquet J, Mantzouranis E, Cruz AA, et al. Uniform definition of asthma severity, control, and exacerbations: document presented for the World Health Organization Consultation on Severe Asthma. J Allergy Clin Immunol. 2010;126:926–938. doi: 10.1016/j.jaci.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 15.Ryan PH, Lemasters GK, Levin L, et al. A land-use regression model for estimating microenvironmental diesel exposure given multiple addresses from birth through childhood. Sci Total Environ. 2008;404:139–147. doi: 10.1016/j.scitotenv.2008.05.051. [DOI] [PubMed] [Google Scholar]
- 16.Ryan PH, LeMasters GK. A review of land-use regression models for characterizing intraurban air pollution exposure. Inhal Toxicol. 2007;19(suppl 1):127–133. doi: 10.1080/08958370701495998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 18.Wubbel C, Asmus MJ, Stevens G, Chesrown SE, Hendeles L. Methacholine challenge testing: comparison of the two American Thoracic Society-recommended methods. Chest. 2004;125:453–458. doi: 10.1378/chest.125.2.453. [DOI] [PubMed] [Google Scholar]
- 19.Juniper EF, Svensson K, Mork AC, Stahl E. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med. 2005;99:553–558. doi: 10.1016/j.rmed.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 20.Juniper EF, O’Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14:902–907. doi: 10.1034/j.1399-3003.1999.14d29.x. [DOI] [PubMed] [Google Scholar]
- 21.Meltzer EO, Busse WW, Wenzel SE, et al. Use of the Asthma Control Questionnaire to predict future risk of asthma exacerbation. J Allergy Clin Immunol. 2011;127:167–172. doi: 10.1016/j.jaci.2010.08.042. [DOI] [PubMed] [Google Scholar]
- 22.Walter MJ, Castro M, Kunselman SJ, et al. Predicting worsening asthma control following the common cold. Eur Respir J. 2008;32:1548–15454. doi: 10.1183/09031936.00026808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sastre J, Olaguibel J, Vega JM, Del Pozo V, Picado C, Lopez Vina A. Cut-off points for defining asthma control in three versions of the Asthma Control Questionnaire. J Asthma. 2010;47:865–870. doi: 10.3109/02770903.2010.491149. [DOI] [PubMed] [Google Scholar]
- 24.National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program, Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Washington, DC: US Dept of Health and Human Services, National Institutes of Health; 2007. [Accessed September 28, 2009]. http://www.nhlbi.nih.gov/guidelines/asthma. [Google Scholar]
- 25.Sanico A, Togias A. Noninfectious, nonallergic rhinitis (NINAR): considerations on possible mechanisms. Am J Rhinol. 1998;12:65–72. doi: 10.2500/105065898782103043. [DOI] [PubMed] [Google Scholar]
- 26.Enright PL, McClelland RL, Newman AB, Gottlieb DJ, Lebowitz MD Cardiovascular Health Study Research Group. Underdiagnosis and undertreatment of asthma in the elderly. Chest. 1999;116:603–613. doi: 10.1378/chest.116.3.603. [DOI] [PubMed] [Google Scholar]
- 27.Ritz T, Kullowatz A, Kanniess F, Dahme B, Magnussen H. Perceived triggers of asthma: evaluation of a German version of the Asthma Trigger Inventory. Respir Med. 2008;102:390–398. doi: 10.1016/j.rmed.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 28.US Census Bureau. United States- Age and Sex; 2007 American Community Survey 1-Year Estimates. [Accessed September 30, 2009]; http://factfinder.census.gov.
- 29.Mosen DM, Schatz M, Magid DJ, Camargo CA., Jr The relationship between obesity and asthma severity and control in adults. J Allergy Clin Immunol. 2008;122:507–511. doi: 10.1016/j.jaci.2008.06.024. [DOI] [PubMed] [Google Scholar]
- 30.Gehring U, Wijga AH, Brauer M, et al. Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. Am J Respir Crit Care Med. 2010;181:596–603. doi: 10.1164/rccm.200906-0858OC. [DOI] [PubMed] [Google Scholar]
- 31.Lipsett M, Hurley S, Ostro B. Air pollution and emergency room visits for asthma in Santa Clara County, California. Environ Health Perspect. 1997;105:216–222. doi: 10.1289/ehp.97105216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gent JF, Triche EW, Holford TR, et al. Association of low-level ozone and fine particles with respiratory symptoms in children with asthma. JAMA. 2003;290:1859–1867. doi: 10.1001/jama.290.14.1859. [DOI] [PubMed] [Google Scholar]
- 33.McCreanor J, Cullinan P, Nieuwenhuijsen MJ, et al. Respiratory effects of exposure to diesel traffic in persons with asthma. N Engl J Med. 2007;357:2348–2358. doi: 10.1056/NEJMoa071535. [DOI] [PubMed] [Google Scholar]
- 34.Alexeeff SE, Litonjua AA, Wright RO, et al. Ozone exposure, antioxidant genes, and lung function in an elderly cohort: VA normative aging study. Occup Environ Med. 2008;65:736–742. doi: 10.1136/oem.2007.035253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kelly FJ, Fussell JC. Air pollution and airway disease. Clin Exp Allergy. 2011;41:1059–1071. doi: 10.1111/j.1365-2222.2011.03776.x. [DOI] [PubMed] [Google Scholar]
- 36.Peacock JL, Anderson HR, Bremner SA, et al. Outdoor air pollution and respiratory health in patients with COPD. Thorax. 2011;66:591–596. doi: 10.1136/thx.2010.155358. [DOI] [PubMed] [Google Scholar]
- 37.Sarnat JA, Brown KW, Schwartz J, Coull BA, Koutrakis P. Ambient gas concentrations and personal particulate matter exposures: implications for studying the health effects of particles. Epidemiology. 2005;16:385–395. doi: 10.1097/01.ede.0000155505.04775.33. [DOI] [PubMed] [Google Scholar]
- 38.Ryan PH, Lemasters GK, Biswas P, et al. A comparison of proximity and land use regression traffic exposure models and wheezing in infants. Environ Health Perspect. 2007;115:278–284. doi: 10.1289/ehp.9480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu S, McDonald R, Martuzevicius D, et al. UNMIX modeling of ambient PM(2.5) near an interstate highway in Cincinnati, OH, USA. Atmos Environ. 2006;40:378–395. doi: 10.1016/j.atmosenv.2006.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lessard A, Turcotte H, Cormier Y, Boulet LP. Obesity and asthma: a specific phenotype? Chest. 2008;134:317–323. doi: 10.1378/chest.07-2959. [DOI] [PubMed] [Google Scholar]
- 41.Moore WC, Meyers DA, Wenzel SE, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med. 2010;181:315–323. doi: 10.1164/rccm.200906-0896OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brandt D, Bernstein JA. Questionnaire evaluation and risk factor identification for nonallergic vasomotor rhinitis. Ann Allergy Asthma Immunol. 2006;96:526–532. doi: 10.1016/S1081-1206(10)63546-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.