Abstract
BACKGROUND
British Columbia, Canada’s provincial methadone program recently replaced their existing methadone formulation with a formulation ten times more concentrated. The transition raised concerns about heightened risk of accidental overdose, leading two organizations to disseminate methadone overdose warning posters during the transitional period. This study explores people who use drugs’ (PWUD) perceptions of these warning posters.
METHODS
Qualitative interviews were conducted with thirty-four PWUD enrolled in methadone maintenance treatment in Vancouver. Participants were recruited from ongoing cohort studies of drug-using individuals. Interview transcripts were analyzed thematically, focusing on participants’ perceptions of the warning posters and potential impacts on drug-related risks.
RESULTS
Overdose warning posters constituted a key source of information about the methadone formulation change, but did not provide adequate information for all participants. Participants articulated a preference for descriptive language, focusing on changes in concentration rather than “strength”, and universal hazard symbols to effectively communicate overdose risks.
CONCLUSION
Participants indicated that warnings employing descriptive language more effectively communicated risk of methadone overdose. Future overdose warnings for drug-using populations must provide adequate information for the intended audience, and be communicated to PWUD through multiple channels.
Keywords: Methadone, drug policy, health communication, public health warning, overdose, drug use
BACKGROUND
Traditional health communication efforts focused on reducing risk behaviors often aim to impact individual-level decisions (Moore, 2004). However, this approach frequently fails to account for the complex environmental contexts that shape the interpretation of health messaging and consequently influences the audience’s decision-making (Dietze, Jolley, Fry, Bammer & Moore, 2006). A small body of research has investigated health communication relating to illicit substance use, specifically public health warnings about overdose risks associated with the presence of adulterated heroin in cities in Canada and Australia (Baljak, Greer, Amlani, Sampson & Buxton, 2015; Kerr, Small, Hyshka, Maher & Shannon, 2013; Miller, 2007). The warnings alerted people who use drugs (PWUD) to the high potency of heroin that had become available in these settings (Kerr et al., 2013; Miller, 2007). Among PWUD managing drug dependence in the context of extreme poverty, the warnings were found to be ineffective at preventing harm, and, in some instances, prompted them to seek out substances able to provide a more potent high (Baljak, Greer, Amlani, Sampson & Buxton, 2015; Freeman & French, 1995; Kerr et al., 2013; Miller, 2007). Recent research in Vancouver, Canada exploring PWUD’s perceptions of illicit drug overdose warnings similarly found that effective drug alerts must be clear, simple, and avoid language highlighting drug potency (Baljak et al., 2015).
In 2015, a ‘natural experiment’ relating to opioid use occurred within the context of British Columbia, Canada’s provincial methadone maintenance treatment (MMT) program. In British Columbia, MMT is strictly regulated by the College of Physicians and Surgeons of British Columbia (CPSBC) and the College of Pharmacists of British Columbia (CPSBC, 2014). Individuals enrolled in MMT can only receive a methadone prescription from a physician registered with the provincial MMT program and are required to refill this prescription monthly (CPSBC, 2014). In order to limit the diversion of methadone to street-based drug markets, MMT patients are required to ingest their daily dosage under direct pharmacist supervision unless they are considered to be adequately stable to receive take-home dosages of methadone (CPSBC, 2014). Conditions for stability include attending all scheduled appointments, no missed methadone doses, and the availability of locked containers in which to store dosages (CPSBC, 2014), and are rarely met by those living in extreme poverty or within entrenched drug scene areas (McNeil, Kerr, Anderson, Maher, Keewatin, et al., 2015).
Beginning February 1, 2014, British Columbia patients enrolled in MMT were required to transition from an anhydrous methadone solution compounded in pharmacies (1 mg/mL) to a concentrated formulation called Methadose® (10 mg/mL). The two formulations also differ in color (orange vs. red), taste (orange vs. cherry flavor), viscosity, and volume (10 to 1 volume ratio). The change introduced concerns about the potential risks and harms for MMT patients during the transition period (McNeil et al., 2015), and in particular the risk of accidental overdoses among both those enrolled in the MMT program and those consuming illicit diverted methadone. Warning posters were distributed to warn people of the formulation change, particularly in Vancouver’s Downtown Eastside (DTES), a roughly ten-block neighborhood home to one of North America’s largest drug scenes and a large proportion of Vancouver’s methadone-dispensing pharmacies (British Columbia Ministry of Health, 2015).
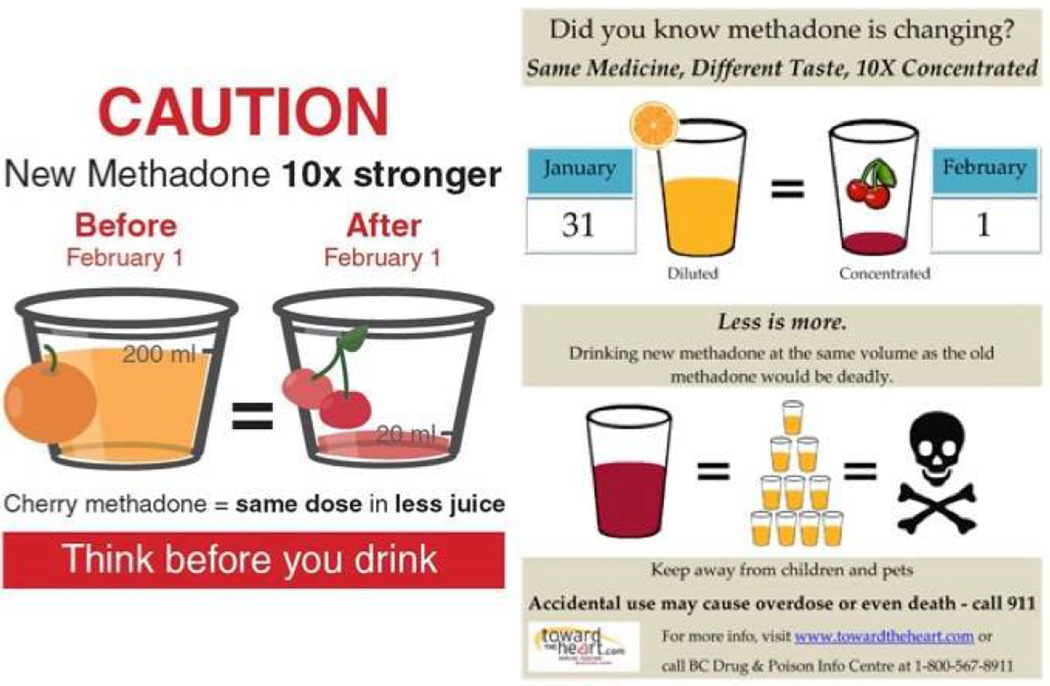
Two organizations in British Columbia created and distributed posters to warn of the methadone formulation change (see Figure 1). One poster, developed by the College of Pharmacists of British Columbia (CPBC) read, “CAUTION: New Methadone 10x Stronger” and included a graphic illustrating that the old, orange methadone would be equivalent to a smaller volume of the new, red formulation. This warning poster was most prevalent within the DTES, as a local methadone consumer’s group (British Columbia Association of People on Methadone) posted them in public places throughout the neighborhood. A second poster, developed by Toward the Heart, an initiative of the British Columbia Centre for Disease Control’s Harm Reduction Program, included a similar graphic, use of the word “Caution,” and an additional image equating a large volume of new, red methadone with a skull and cross-bones, a universal hazard symbol for death. The second poster also stated that the new methadone formulation was “10X concentrated” and provided contact information for further details. While this poster was not as widely distributed within the neighborhood, it was posted in harm reduction distribution sites and other locations frequented by PWUD. The current study investigates PWUD’s perceptions of these two posters about the change to Methadose®, as well as their responses to the warnings.
Figure 1.
Methadose® warning posters created by College of Physicians and Surgeons of British Columbia (left) and Toward the Heart (right)
Note: Also included in separate .jpg file
METHODS
Semi-structured interviews were conducted with PWUD enrolled in BC’s MMT program in the six-month period immediately following the methadone formulation change (February – July 2014). Study participants were recruited from two on-going prospective cohorts operating in Vancouver and consisting of more than 2000 PWUD: the Vancouver Injection Drug Users Study (VIDUS) and the AIDS Care Cohort to Evaluate Exposure to Survival Services (ACCESS). These studies have been described in detail elsewhere (Strathdee et al., 1997; Wood et al., 2003). At baseline and every six months thereafter, cohort research staff administer questionnaires and collect clinical data from cohort participants at a storefront research office located in the DTES. Recruitment for this qualitative study occurred through frontline staff at the research office. Cohort research staff explained the study to those ACCESS and VIDUS participants who attended follow-up appointments, and who reported enrolment in MMT during the period when the regulatory changes were introduced to the provincial MMT program. Participants were then invited to participate in a qualitative interview. We restricted our recruitment to MMT patients in order to obtain feedback on a variety of topics relating to the MMT program, including the regulatory changes and warning posters. No one refused an invitation to participate, although several people did not show up for scheduled interviews.
Trained interviewers used a semi-structured interview guide to facilitate interviews. In addition to questions about the warning posters, guides contained questions about participants’ experiences with the MMT program, including topics such as dispensation and incentives, discontinuation, and side effects of the switch to Methadose®. Copies of the posters were used as an elicitation tool to prompt discussion, and participants were asked whether or not they had previously seen them posted anywhere in the DTES. Informed consent was obtained prior to interviews and participants received remuneration of $30 (CAD). Interviews were audio-recorded and transcribed, and transcripts were imported into NVivo, a qualitative data analysis software program. A coding framework comprised of a priori categories extracted from the interview guide was used during the analysis and revised as coding progressed. Once the final categories were established, sections of the data were recoded to verify their representativeness. Analysis and reporting of results focused upon participants’ perceptions of the warning posters.
Ethical approval was obtained from the University of British Columbia/Providence Healthcare research ethics board.
RESULTS
The 34 individuals participating in qualitative interviews included 14 women and 20 men. 24 participants identified as White, while the remaining participants identified as Aboriginal (n=9) or African-Canadian (n=1). The mean age of participants was 46 years (range = 26–59 years). All participants confirmed that they were enrolled in the BC methadone program upon recruitment.
Posters as a source of information
While some participants learned of the methadone formulation by “word of mouth”, other participants became aware of the change once “those posters started getting posted up everywhere.” When asked whether they had seen the methadone warning posters, all participants reported that they had seen the CPSBC posters that had been posted “all over” the neighborhood (e.g., telephone poles, bus stops), while only some had seen the Toward the Heart poster. As the following interview excerpt illustrates, participants identified their peer networks and warning posters as the primary ways that people learned of the formulation change:
[I] just heard [from] other people and with posters going up here and there saying that they were going to change the methadone.” [White Man, 51 years old]
Participants emphasized that other sources of information about the risks associated with the methadone formulation change were limited. Most participants reported that their healthcare providers had not given them advanced warning of the methadone formulation change, with some emphasizing that their healthcare providers “must have just assumed that we saw all the postings.” Some participants felt that, while the posters successfully alerted individuals about the transition, they did not provide the detailed information that was needed regarding the new methadone formulation and associated risks. As one participant explained:
They [i.e., physicians and pharmacists] didn’t do enough information…Like, they have these big posters up everywhere. Like, ‘Duh.’ Okay, we all know that [i.e., aware of the transition]… There’s nothing else out there. [White Woman, 50 years old]
Seeking “stronger” methadone
Participants expressed concerns about the poster created by CPSBC, which cautioned, “New Methadone 10x stronger”. Specifically, participants articulated that the description of a “new”, “stronger” product might be misinterpreted to indicate the presence of a higher potency product. Participants also emphasized how those ingesting illicit methadone might be unfamiliar with the new formulation and therefore experience heightened overdose risk. For example:
I’ve seen a lot of that [poster]. And, it’s like [pause] I think by having by having this being ‘ten times stronger’… there’s a lot of people that get carries [i.e., take home doses of methadone]. They sell their methadone, so, now that it’s stronger, they may sell it to somebody that’s never even experienced it and, you know, might overdose. […] A lot of people, they’re up on, like high doses and they’ll take half of it and sell the other half. [White Man, 51 years old]
Further, participants communicated their opinions that individuals obtaining diverted Methadose® might not have access to other sources of information about the product, such as healthcare providers, and would therefore rely almost exclusively upon posters for accurate information.
Need for adequate information
Participants indicated the Toward the Heart poster was preferable because it provided additional, detailed information about the nature of the change - namely, it clearly described a difference in methadone concentration, and communicated the potential risks associated with consuming the new formulation. For example:
“Same medicine, different taste, 10 times concentrated.” This [poster] tells you a little bit more. […] I do believe this one would let me know more in depth – “Danger”, “Beware”. [White Woman, 52 years old]
Participants reported that this combination of “straightforward” language and the skull and cross-bones graphic reinforced overdose risks, and was accessible to those with limited literacy skills. Participants expressed that the wording of the Toward the Heart poster was therefore less likely to prompt people to seek out diverted methadone than the CPSBC poster. For example:
It tells you right there it’s ten to one [i.e. volume ratio between old and new formulations]… [It’s] more explanatory – it says “concentrated” instead of “stronger” ’cause that’s what it is. It’s more concentrated. It’s not stronger. […] If they wanna buy [illicit methadone], they’re looking for more stronger stuff. [White Man, 42 years old]
DISCUSSION
Our findings add to a growing body of research informing best practices in health communication for drug-using populations. Participants articulated the need for adequate information regarding overdose risks, and indicated that warning posters and peers were key sources of information about Methadose®. Participants also communicated that language focusing upon volume and concentration of the product, as well as universal hazard symbols (e.g., skull and crossbones), conveyed the potential for overdose harm better than messages that warned of “stronger” methadone. In future, increased use of these communication tools might be prudent. Our findings build upon past research by demonstrating that overdose-related public health messages are more effective when they focus warnings upon heightened potential for harm, rather than the potency of a substance (Baljak et al., 2015; Freeman & French, 1995; Kerr et al., 2013; Miller, 2007). Previous studies illustrate that this approach may help avoid unintended increased drug-seeking behaviors and subsequent harms (Kerr et al., 2013; Miller, 2007).
In addition to the use of descriptive language, our study highlighted the need to capitalize upon effective, pre-existing channels for health communication to PWUD. In the context of methadone, overdose warnings must be designed for two sub-groups of methadone consumers: (i) PWUD who are prescribed methadone by a healthcare provider; and, (ii) people who obtain illicit diverted methadone, often through sale of individual prescribed doses or pharmacy thefts (Bell, 2010; Vancouver Police Department, 2014). Our findings suggest that many MMT patients did not attain adequate information about the change to Methadose® from primary care providers despite their involvement in a formal MMT service delivery structure (e.g., monthly physician visits, daily pharmacy attendance), and instead accessed information through other PWUD and warning posters in the neighborhood. Meanwhile, illicit methadone consumers are not required to regularly engage with pharmacists and prescribing physicians, and, therefore, have few opportunities to attain such information through the healthcare system. While improvements in patient-provider information might have the potential to improve access to pertinent information among MMT patients, communication channels rooted in the daily activities and locations of licit and illicit methadone consumers, such as PWUD networks or community organizations, are required to ensure important information reaches MMT patients.
Our findings echo recent research, also conducted with populations in Vancouver’s DTES, which found that PWUD did not consider healthcare providers to be key conduits of information about illicit drugs (Baljak et al., 2015). Instead, respondents identified drug dealers, other PWUD, and overdose warning posters as sources of information about illicit drug quality and adulteration (Baljak et al., 2015). Our findings build upon this research by pointing to important parallels between health communication concerning both licit and illicit substances. In particular, it suggests that the broader shared environment within which warnings occur (i.e., marginalized populations within an entrenched drug scene) creates dynamics that impact the delivery of all health warnings, irrespective of the contrasting regulatory contexts of licit and illicit substances.
Our findings also indicate that MMT patients desired varying levels of information. While some participants found that the posters provided adequate information to alert them to the upcoming MMT changes, others indicated that more detailed information about the formulation should be provided on posters. For example, posters could be altered to include relevant information about changes to methadone dispensation. Participant responses highlight how comprehensive warning strategies integrating multiple vectors of risk information are needed, providing a combination of simplified and more detailed information. Participants specifically indicated the importance of peer-to-peer communication channels; peer-delivered public health warnings may therefore constitute an underutilized strategy for drug warnings, and health communication with PWUD in general. In similar contexts, these strategies have been shown to provide low-barrier health outreach and were highly effective at accessing high-risk PWUD (Aitken, Kerger & Crofts, 2002; McNeil, Small, Lampkin, & Kerr, 2015; Small et al., 2012). While further research exploring alternative channels for health communication to marginalized PWUD is required, peer-delivered health warning systems represent a promising approach to more effectively generating and delivering overdose warnings to PWUD.
Our study has several limitations. Our sample only involved people recruited from the DTES currently enrolled in British Columbia’s MMT program. Our results might not be transferable to other settings with different regulatory contexts or methadone client populations. Our study also focused specifically on the experiences of individuals enrolled in MMT, and may therefore have overlooked risks and considerations associated with illicit methadone diversion. Finally, our study explored participants’ perspectives of poster content only. Further studies are required to determine the impact of geographic and temporal distribution on warning effectiveness, and to evaluate the processes by which posters were developed.
In conclusion, our findings underscore the need for drug-related health communication that better describes the potential for risk and harm, rather than simply emphasizing drug potency. Comprehensive communication strategies that integrate multiple channels of information are required to meet the needs of all methadone consumers, and peer-delivered solutions represent a promising approach for improved health communication with consumers of both licit and illicit methadone.
Highlights.
Posters used to alert people to methadone formulation change in Vancouver, Canada.
Study explores people who use drugs’ (PWUD) views of two warning posters.
Warnings of “stronger” methadone were perceived to increase drug-related risks.
Descriptive language and universal hazard symbols more effectively conveyed risk.
Posters and other PWUD were key sources of information about formulation change.
Acknowledgments
The authors thank the study participants for their contributions to this research. We thank Bill Coleman, Tricia Collingham, Cameron Dilworth, Steve Kain, William Lee, Jenny Matthews, Aaron McKinny, Carmen Rock, Kristie Starr, Guido Thylmann, Vanessa Volkommer, and Cristy Zonnefeld for the research and administrative assistance. This study was supported by the US National Institutes of Health (R01DA033147, R01DA011591, and R01DA021525). Ryan McNeil and Will Small are supported by the Michael Smith Foundation for Health Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Aitken CK, Kerger M, Crofts N. Peer-delivered hepatitis C testing and counselling: A means of improving the health of injecting drug users. Drug and Alcohol Review. 2002;21(1):33–37. doi: 10.1080/09595230220119327. [DOI] [PubMed] [Google Scholar]
- Bell J. The global diversion of pharmaceutical drugs. Addiction. 2010;105(12):1531–1537. doi: 10.1111/j.1360-0443.2010.03014.x. [DOI] [PubMed] [Google Scholar]
- British Columbia Ministry of Health, Medical Beneficiary and Pharmaceutical Services Division. Methadone maintenance payment program: Review. 2015 [Google Scholar]
- Dietze P, Jolley D, Fry CL, Bammer G, Moore D. When is a little knowledge dangerous? Circumstances of recent heroin overdose and links to knowledge of overdose risk factors. Drug and Alcohol Dependence. 2006;84(3):223–230. doi: 10.1016/j.drugalcdep.2006.02.005. [DOI] [PubMed] [Google Scholar]
- Freeman RC, French JF. What is the addicts’ grapevine when there’s “bad dope”? An investigation in New Jersey. Public Health Reports. 1995;110(5):621–624. [PMC free article] [PubMed] [Google Scholar]
- Kerr T, Small W, Hyshka E, Maher L, Shannon K. “It’s more about the heroin”: Injection drug users’ response to an overdose warning campaign in a Canadian setting. Addiction. 2013;108(7):1270–1276. doi: 10.1111/add.12151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeil R, Kerr T, Anderson S, Maher L, Keewatin C, Milloy MJ, Wood E, Small W. Negotiating structural vulnerability following regulatory changes to a provincial methadone program in Vancouver, Canada: A qualitative study. Social Science & Medicine. 2015;133:168–176. doi: 10.1016/j.socscimed.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeil R, Small W, Lampkin H, Kerr T. “We need somewhere to smoke crack”: An ethnographic study of an ‘unsanctioned’ safer smoking room in Vancouver, Canada. International Journal of Drug Policy. 2015;26(7):645–652. doi: 10.1016/j.drugpo.2015.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller PG. Media reports of heroin overdose spates: Public health messages, moral panics or risk advertisements? Critical Public Health. 2007;17(2):113–121. [Google Scholar]
- Moore D. Governing street-based injecting drug users: A critique of heroin overdose prevention in Australia. Social Science & Medicine. 2004;59(7):1547–1557. doi: 10.1016/j.socscimed.2004.01.029. [DOI] [PubMed] [Google Scholar]
- Morgan GM, Fischhoff B, Bostrom A, Atman CJ. Risk Communication: A mental models approach. West Nyack, NY, USA: Cambridge University Press; 2001. [Google Scholar]
- Small W, Wood E, Tobin D, Rikley J, Lapushinsky D, Kerr T. The Injection Support Team: A peer-driven program to address unsafe injecting in a Canadian setting. Substance Use & Misuse. 2012;47(5):491–501. doi: 10.3109/10826084.2012.644107. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Patrick DM, Currie SL, Cornelisse PG, Rekart ML, Montaner JS, Schechter MT, O`Shaughnessy MV. Needle exchange is not enough: Lessons from the Vancouver injecting drug use study. AIDS. 1997;11(8):F59–F65. doi: 10.1097/00002030-199708000-00001. [DOI] [PubMed] [Google Scholar]
- Wood E, Kerr T. What do you do when you hit rock bottom? Responding to drugs in the city of Vancouver. International Journal of Drug Policy. 2006;17(2):55–60. [Google Scholar]
- Wood E, Montaner JS, Yip B, Tyndall MW, Schechter MT, O’Shaughnessy MV, Hogg RS. Adherence and plasma HIV RNA responses to highly active antiretroviral therapy among HIV-1 infected injection drug users. Canadian Medical Association Journal. 2003;169(7):656–661. [PMC free article] [PubMed] [Google Scholar]
- Vancouver Police Department. Potent methadone stolen in pharmacy break-in [News bulletin] 2014 Retrieved 7 January 2015 from http://mediareleases.vpd.ca/2014/02/06/potent-methadone-stolen-in-pharmacy-break-in/ [Google Scholar]