Abstract
Background
Patients suffering in-hospital cardiac arrest often show signs of physiological deterioration before the event. The purpose of this study was to determine the prevalence of abnormal vital signs 1–4 hours before cardiac arrest, and to evaluate the association between these vital sign abnormalities and inhospital mortality.
Methods
We included adults from the Get With the Guidelines® - Resuscitation registry with an in-hospital cardiac arrest. We used two a priori definitions for vital signs: abnormal (heart rate (HR) ≤ 60 or ≥ 100 min−1, respiratory rate (RR) ≤ 10 or > 20 min−1 and systolic blood pressure (SBP) ≤ 90 mm Hg) and severely abnormal (HR ≤ 50 or ≥ 130 min−1, RR ≤ 8 or ≥ 30 min−1 and SBP ≤80 mm Hg). We evaluated the association between the number of abnormal vital signs and in-hospital mortality using a multivariable logistic regression model.
Results
7,851 patients were included. Individual vital signs were associated with in-hospital mortality. The majority of patients (59.4%) had at least one abnormal vital sign 1–4 hours before the arrest and 13.4% had at least one severely abnormal sign. We found a step-wise increase in mortality with increasing number of abnormal vital signs within the abnormal (odds ratio (OR) 1.53 (CI: 1.42 – 1.64) and severely abnormal groups (OR 1.62 [CI: 1.38 – 1.90]). This remained in multivariable analysis (abnormal: OR 1.38 [CI: 1.28 – 1.48], and severely abnormal: OR 1.40 [CI: 1.18 – 1.65]).
Conclusion
Abnormal vital signs are prevalent 1–4 hours before in-hospital cardiac arrest on hospital wards. Inhospital mortality increases with increasing number of pre-arrest abnormal vital signs as well as increased severity of vital sign derangements.
Keywords: cardiopulmonary resuscitation, heart arrest, heart rate, blood pressure, respiration, mortality
1. Introduction
Over 200,000 adult in-hospital cardiac arrests (IHCA) occur in the United States yearly.[1, 2] Mortality remains high, with 22–23% surviving to hospital discharge,[1] and early identification of patients at risk for deterioration is crucial.[3, 4] Multiple intra-event factors have been associated with cardiac arrest mortality.[5]–[6] However, the impact of pre-event abnormalities on post-event outcomes has not been examined previously in a large cohort.
Several small studies have shown that abnormal vital signs before IHCA are common[7–11] and predictive of progression to cardiac arrest.[12, 13] Retrospective expert reviews have found that 18–66% of cardiac arrests may be preventable.[14, 15] Common reasons for preventability in one study included not acting on clinical signs prior to the event and “inappropriate” area of treatment such as a general ward when an intensive care unit setting was warranted.[14] These investigations led to the widespread use of rapid response teams as a means of preventing progression to cardiac arrest on hospital wards by optimizing early treatment.[16] Previous studies in out-of-hospital[17, 18] and inhospital cardiac arrest[19] have shown that pre-arrest factors (such as abnormal vital signs) may be associated with post-event outcome. However, neither the prevalence of abnormal vital signs prior to in-hospital cardiac arrest nor their association with post-event survival has been examined previously in a large multicenter cohort.
The present study aimed to characterize the prevalence of abnormal vital signs 1–4 hours before a treated cardiac arrest using a large national registry database, and to evaluate the association between these vital sign abnormalities and in-hospital mortality.
2. Methods
Study design
We conducted a post-hoc analysis of prospectively collected data from a large United States registry of IHCA.
Data Source
Data were collected from the Get With the Guidelines® - Resuscitation (GWTG-R) registry, a national American Heart Association (AHA) sponsored quality improvement IHCA registry. Details of data collection and reliability have been described previously.[20] Patients were excluded if they had prior do-not-resuscitate orders or cardiopulmonary resuscitation events beginning outside of the hospital.
The registry utilizes the Utstein-style template, standardized to facilitate uniform reporting across hospitals.[21, 22] Data integrity is ensured through rigorous certification of data entry personnel and data are evaluated for completeness and accuracy with standardized software.[23] Pre-arrest vital signs were a mandatory field during our study period.
Study Population, Vital Signs and Outcomes
We included adult patients from acute-care hospitals that submitted clinical data to the GWTG-R registry between July 2007 and September 2010. We included only index events occurring on an inpatient ward. We included locations coded as “General Inpatient Area” and “Telemetry Unit or Step-Down Unit”. The GWTG-R registry collects up to four sets of vital signs taken in the 4 hours prior to the cardiac arrest. No detailed data on how the vital signs are recorded are provided but no rounding rules are provided to data abstractors. We excluded patients with missing data on survival or vital signs 1 – 4 hours before the arrest. We included only sets of vital signs with at least heart rate, respiratory rate and systolic blood pressure. If there was more than one set of vital signs within the 1 to 4 hour time period we used the set closest to 4 hours. This was done to avoid confounding by acute interventions performed by the rapid response team or including patients actively being moved to the intensive care unit, and to best assess the predictive nature of vital sign derangements, even when more temporally remote from the event.
We defined abnormal vital signs a priori based on standard clinical definitions and consensus within the author team: Heart rate ≤ 60 or ≥ 100 min−1, respiratory rate ≤ 10 or > 20 min−1 and systolic blood pressure ≤ 90 mm Hg. We defined a subgroup of severely abnormal vital signs, based on consensus and previous studies related to rapid response teams.[24, 25], as follows: Heart rate ≤ 50 or ≥ 130 min−1, respiratory rate ≤ 8 or ≥ 30 min−1 and systolic blood pressure ≤80 mm Hg.
Statistical Analyses
The study population was characterized using descriptive statistics. Categorical variables are reported as counts and frequencies, continuous variables as medians with 1st and 3rd quartiles due to non-normal distribution of the data. Categorical data were compared using the Chi-Square test, continuous data with the Wilcoxon Rank Sum test.
First, we assessed the relationships between individual vital signs and mortality. We assumed these were non-linear and delineated pre-defined vital sign categories. We assessed the mortality within each category using descriptive statistics, then compared the different categories using univariate logistic regression where the reference category was that with the lowest mortality.
To assess the independent association between individual pre-arrest vital signs and mortality we applied a multivariable logistic regression model with generalized estimating equations with an exchangeable (compound symmetry) correlation matrix to account for within hospital clustering. The following pre-determined variables (see Table 1) were entered into the multivariable model: age, gender, race, illness category, pre-existing conditions, whether the arrest was monitored or witnessed, location, time of week, time of day, first documented pulseless rhythm, whether a hospital wide response was activated and year of arrest (with 2007 as the reference). We included all three vital signs in the same model and also included the time from vital signs to loss of pulse.
Table 1.
Characteristics of the Study Populationa
| All Patients (n = 7,851) | |
|---|---|
| Demographics | |
| Age – median years (quartiles) | 72 (59 – 81) |
| Sex (female) – no. (%) | 3,298 (42) |
| Race – no. (%) | |
| White | 5,573 (74) |
| Black | 1,695 (22) |
| Other | 277 (4) |
| Type of Admission – no. (%) | |
| Medical – non-cardiac | 3,963 (51) |
| Medical – cardiac | 2,437 (31) |
| Surgical – non-cardiac | 1,029 (13) |
| Surgical – cardiac | 323 (4) |
| Trauma | 94 (1) |
| Pre-existing Conditions – no. (%) | |
| Cardiac | |
| Arrhythmia | 2,412 (31) |
| History of MI | 1,246 (16) |
| MI this admission | 877 (11) |
| History of heart failure | 1,852 (24) |
| Heart failure this admission | 1,540 (20) |
| Non-Cardiac | |
| Respiratory insufficiency | 2,407 (31) |
| Diabetes mellitus | 2,762 (35) |
| Renal insufficiency | 2,635 (34) |
| Metastatic/hematologic malignancy | 1,206 (15) |
| Hypotension/hypoperfusion | 1,042 (13) |
| Pneumonia | 1,162 (15) |
| Baseline depression in CNS function | 848 (11) |
| Metabolic/electrolyte abnormality | 922 (12) |
| Septicemia | 1,010 (13) |
| Acute CNS non-stroke event | 504 (6) |
| Hepatic insufficiency | 497 (6) |
| Acute stroke | 312 (4) |
| Major trauma | 160 (2) |
| Arrest Characteristics – no. (%) | |
| Location | |
| Floor without telemetry | 3,735 (48) |
| Floor with telemetry | 4,116 (52) |
| Time of day (night [11:00pm – 6:59am]) | 2,746 (35) |
| Time of week (Friday 11pm to Monday 7am) | 2,473 (32) |
| Hospital wide cardiac arrest response activated | 7,576 (97) |
| Monitored | 5,618 (72) |
| Witnessed | 4,980 (63) |
| First rhythm shockable (VT or VF) | 1,208 (16) |
MI indicates myocardial infarction, CNS: central nervous system, VT: ventricular tachycardia, and VF: ventricular fibrillation
We then conducted a univariate logistic regression analysis to assess the association between the number of abnormal vital signs before cardiac arrest and mortality. The number of abnormal vital signs was treated as a continuous variable (ranging from zero to three). We next applied a similar multivariable logistic regression model as outlined above and with the same co-variables to assess the independent association between the number of pre-cardiac arrest abnormal vital signs and mortality.
For the multivariable analyses we included only patients with no missing data on any included covariates (91% of all patients). As a sensitivity analysis we performed all univariate analysis including only patients with full data. The results were similar to those performed with the full cohort, presented here. As a secondary sensitivity analysis we conducted all multivariable logistic regressions excluding variables occurring after the recording of the vital signs (whether the event was witnessed and monitored, the location of the arrest and the initial rhythm) that could theoretically be causally affected by the vital signs. The results were similar to the main analysis (changes in odds ratio (OR) point estimates between 0 and 13%) so are not reported here. We performed a sensitivity analysis such that if patients had more than one set of vital signs within the 1 to 4 hour time period we included the set closest to the 1 hour time point (as opposed to the 4 hour time point). Results were essentially identical to our primary analysis and are not presented here. As a post-hoc sensitivity analysis, we performed multiple imputations as described in the supplemental material.
All results from the logistic regressions are presented as OR with 95% confidence intervals (CI). Statistical analyses were conducted with the use of SAS software, version 9.3 (SAS Institute, Cary, NC, USA). All hypothesis tests were two-sided, with a significance level of p < 0.05.
3. Results
Characteristics of the Study Population
There were 64,806 adult IHCA patients in the GWTG registry between July 2007 and September 2010. 7,851 patients from 300 hospitals met study criteria (see Figure 1). Median age was 72 years (quartiles: 59 – 81), 42% were female and 74% were white. Half (52%) of the arrests were in a ward setting with telemetry, 63% were witnessed and 97% elicited a hospital-wide response. Additional patient and arrest characteristics are reported in Table 1. Mortality was 78%. Median time from the included set of vital signs to arrest was 156 minutes (quartiles: 110 – 199); 30% of included vital signs were between 1 and 2 hours prior to the cardiac arrest event, 33% between 2 and 3 hours, and 37% between 3 and 4 hours. There was no difference in the number of patients having at least one abnormal or severely abnormal vital sign between the three time periods. Median heart rate was 88 minute−1 (quartiles: 74 – 103), median respiratory rate 20 minute−1 (18 – 22), and median systolic blood pressure 118 mm Hg (101 – 137). The distributions of the individual vital signs are shown in Supplemental Figure 1.
Figure 1. Patient Inclusion/Exclusion Criteria.
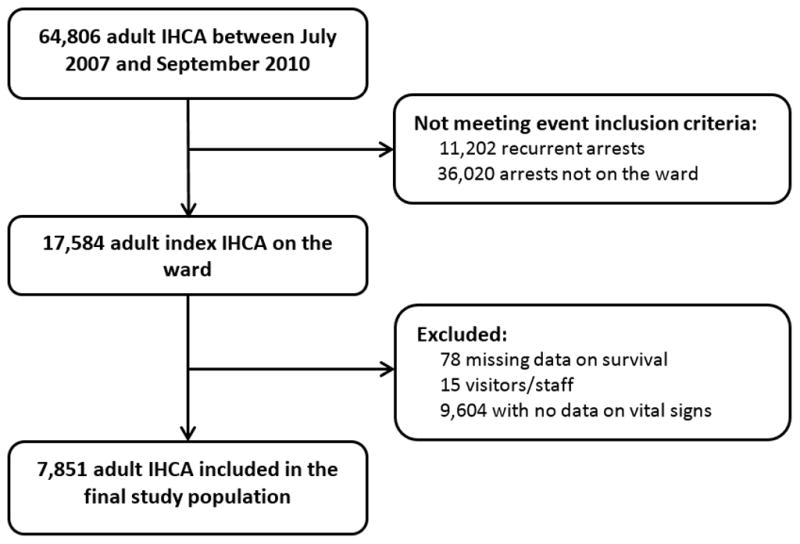
A total of 7,851 patient were included in the primary study cohort
Individual Vital Signs and Mortality
The mortality associated with incremental values for heart rate, respiratory rate and systolic blood pressure are presented in Figure 2. For heart rate, mortality was lowest at 50–59 min−1, with a step-wise increase with increasing heart rate. The lowest mortality was found with a blood pressure of 170 – 179 mm Hg with a step-wise increase in mortality with lower blood pressure.. The variability in mortality with various respiratory rates was not as profound as for the other two vital signs, although mortality was lowest in patients with a respiratory rate between 10 and 14. The results of the multivariable logistic regression for the individual vital signs in increments are shown in Supplemental Figure 2 and demonstrate a similar pattern.
Figure 2. The Association Between Individual Vital Signs and Mortality – Univariate Analysis.
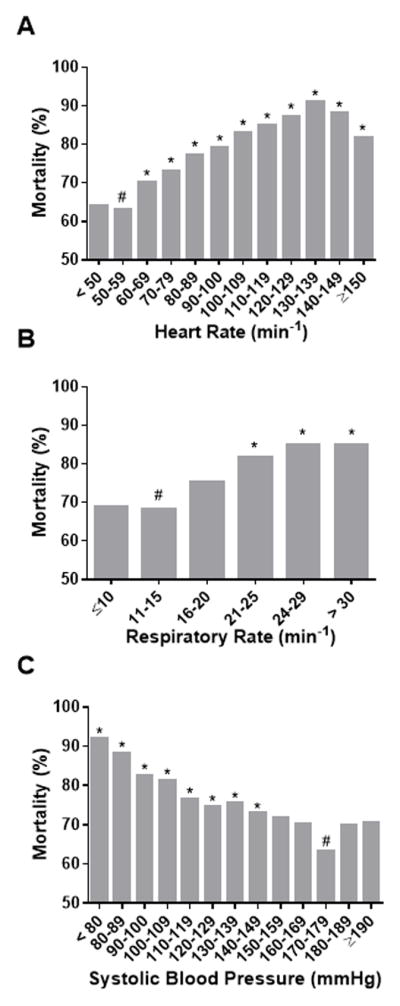
The * indicates statistical significance compared to the reference group (marked with a #) defined as the group with the lowest mortality (50–59 min−1 for heart rate [A], 11–15 min−1 for respiratory rate [B] and 170–179 mm Hg for systolic blood pressure [C]).
Number of Abnormal Vital Signs and Mortality
59.4% of patients had at least one abnormal vital sign within 1 – 4 hours before cardiac arrest, and 13.4% had a least one severely abnormal vital sign. (Table 2) We found a step-wise increase in mortality with increasing number of abnormal vital signs using both of our predefined categories.(Figure 3) In the abnormal category, the odds ratio for mortality was 1.53 (CI: 1.42 – 1.64, p < 0.001) for each additional abnormal vital sign and this remained in multivariable analysis (adjusted OR 1.38 [CI: 1.28 – 1.48], p < 0.001). Results were similar in the severe category (OR 1.62 [CI: 1.38 – 1.90], p-value < 0.001), persisting in multivariable analysis (adjusted OR 1.40 [CI: 1.18 – 1.65], p < 0.001). Using multiple imputation techniques, we found similar results in multivariable analysis for both the abnormal (adjusted OR 1.42 [CI: 1.34 – 1.53], p < 0.001) and the severely abnormal category (adjusted OR 1.42 [CI: 1.22 – 1.67], p < 0.001). Patients with a cardiac arrest with an initial shockable rhythm were less likely to have at least one abnormal pre-arrest vital sign than patients with an initial non-shockable rhythm (abnormal: 51% vs. 61% and severely abnormal 10% vs. 14%, both p < 0.001). The number of abnormal (OR: 1.26 [95%CI: 1.15 – 1.38], p < 0.001) and severely abnormal (OR: 1.24 [95%: 1.03 – 1.50], p = 0.03) vital signs was independently associated with a nonshockable initial rhythm in multivariable analysis. In the 5000 (63.7%) patients with ROSC, pre-arrest abnormal (OR: 1.39 [95%: 1.29 – 1.51]. p < 0.001) and severely abnormal (OR: 1.46 [95%: 1.22 – 1.74]. p < 0.001) vital signs were still associated with increased odds of mortality.
Table 2.
Number of Abnormal Vital Signs within Predefined Categories
| Abnormal | Severely abnormal | ||||
|---|---|---|---|---|---|
| Definitions of abnormal | Heart rate | ≤ 60 or ≥ 100 | ≤ 50 or ≥ 130 | ||
| Respiratory rate | ≤ 10 or > 20 | ≤ 8 or ≥ 30 | |||
| Systolic blood pressure | ≤ 90 | ≤ 80 | |||
| No. | % | No. | % | ||
| Number of abnormal vital signs | 0 | 3,189 | 40.6 | 6,802 | 86.6 |
| 1 | 3,043 | 38.8 | 946 | 12.1 | |
| 2 | 1,446 | 18.4 | 96 | 1.2 | |
| 3 | 173 | 2.2 | 7 | 0.1 | |
Figure 3. The Association Between Number of Abnormal Vital Signs and Mortality.
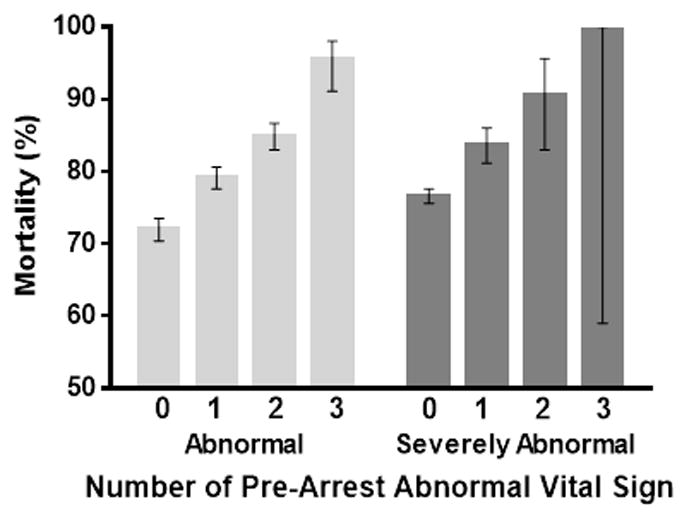
We found a step-wise increase in mortality with increasing number of abnormal vital signs using both of our predefined categories (abnormal: OR 1.53 (CI: 1.42 – 1.64) per increased abnormal vital sign, and severely abnormal: OR 1.62 [CI: 1.38 – 1.90] per increased abnormal vital sign). Error bars represent exact binomial 95% confidence intervals.
Patients with no Documented Vital Signs
Many patients (9,640) were excluded from our primary analysis as they lacked a full set of documented vital signs within 1 to 4 hours before the cardiac arrest. A comparison of baseline and arrest characteristics between those patients and those included in our analysis appears in Supplemental Table 1. The statistically significant differences between the groups were most likely related to the large sample size as the standardized differences between groups were very small (i.e. < 0.10) in most cases. Notably, patients with recorded vital signs had higher prevalence of pre-existing cardiac conditions and were more likely to have their cardiac arrest on a ward with telemetry and during the daytime hours between Monday and Friday. The two groups had similar prevalence of non-cardiac pre-existing conditions. Mortality was slightly higher in those excluded based on missing vital signs (79% vs. 78%, p = 0.02).
4. Discussion
Utilizing a large national registry we are the first to report that vital signs preceding IHCA are independently associated with in-hospital mortality in a “dose-response” fashion. This relationship persists after adjustment for multiple potential confounders. We found a high prevalence of abnormal vital signs preceding cardiac arrest on the wards. The number of pre-arrest abnormal vital signs was associated with a step-wise increase in in-hospital mortality using two different categories based on the degree of abnormality.
Several previous studies have investigated the prevalence of abnormal vital signs and their association with progression to cardiac arrest,[7–9, 12, 13] and have found a high prevalence of abnormal vital signs in the hours preceding IHCA.[7–9] Our study confirms this in a large, multicenter cohort. Some previous studies have found substantially higher incidence of pre-cardiac arrest abnormalities then the current study.[7, 10, 19] The current study however only included patients on inpatient wards (as compared to also including the emergency department and ICU), used a narrow time interval (1 – 4 hours prior to the cardiac arrest), and only included abnormalities in three vital signs.
Studies with control groups (i.e. hospitalized patients without a cardiac arrest) generally show that the presence of abnormal vital signs is associated with progression to cardiac arrest.[12, 13] We, however, analyzed patients who develop cardiac arrest and evaluated the association of preceding vital signs with post-event mortality, similar to a few previous smaller studies.[17–19] Our findings indicate that vital signs prior to arrest are associated with mortality after the event in what appears to be a “dose-dependent” fashion. For example, systolic blood pressure < 80 mm Hg is associated with the highest mortality whereas higher blood pressures are associated with lower mortality. This suggests not only that a patient who is severely hypotensive (< 80 mm Hg) prior to the event could have worse outcome, but also that either “relative hypotension” may be harmful in some patients or that higher blood pressures are somehow protective. We found the opposite relationship between heart rate and mortality, with lower heart rate being associated with better outcome. The relationship between respiratory rate and mortality was not as robust, which could be due to the inherent subjectivity of this vital sign as respiratory rate is still generally observed and calculated by the clinical team rather than by automated devices. This may introduce some imprecision in the measurement.
The finding that small differences in pre-event vital signs may impact outcome after cardiac arrest has important implications for quality improvement as well as tracking the epidemiology of cardiac arrest outcomes. There has been a decrease in mortality from cardiac arrest over the past decade.[26] Numerous potential reasons have been suggested, including event-related factors such as quality of cardiopulmonary resuscitation and post-event interventions. Our findings suggest that future studies should also consider pre-event physiological variables as potential influences on outcomes, as cardiac arrest that is truly sudden (i.e., no pre-event vital sign abnormalities) is associated with better overall survival than cardiac arrest preceded by physiologic perturbations.
While rapid response teams are being implemented across the United States and other countries, the optimal methods for detecting a deteriorating patient remain unknown.[16, 27] As summarized in a recent review article[16] many hospitals in the United Kingdom use the Modified/National Early Warning System,[28, 29] an additive score combining various vital signs and mental status. A number of American[25, 30] and Australian[24] hospitals use the presence of any single abnormality as a trigger for activation of the team. As illustrated in Figure 3 we found that the presence of “severely abnormal” vital signs resulted in a relatively minor increase in mortality compared to “abnormal” signs., There was, however, an incremental increase in mortality with increasing numbers of abnormal vital signs such that patients with three abnormal vital signs had more than 20% higher mortality than those with zero abnormal vital signs. While these results are not directly applicable to the activation of rapid response teams they do raise the hypothesis that the cumulative number of abnormal vital signs has a stronger association with mortality than any individual vital sign. Our results are comparable to those reported by Bleyer et al. who, in a single-center study, investigated the association between abnormal vital signs and mortality in a large group of undifferentiated patients on in-hospital wards.[31] Though vital sign definitions and study populations differ substantially between the two studies, Bleyer also found an increase in mortality with an increasing number of abnormal vital signs.[31] Although the mortality in the Bleyer study was much lower overall than in the present study due to our focus on patients with IHCA as opposed to the general ward population, the difference in mortality with increasing number of abnormal vital signs was similar, suggesting there is a strong association between abnormal vital signs and in-hospital mortality which was also seen in a study by Smith et al.[32]
5. Limitations
The findings should be interpreted in the context of the study design. Despite the thorough training and certification processes of the GWTG-R registry, there may be slight discrepancies in data reporting across sites. We accounted for any systematic difference between hospitals by using generalized estimating equations in our logistic regression which accounts for within hospital clustering. Participation in the GWTG-R registry is voluntary and thus raises the potential for selection bias and lack of generalizability to hospitals not participating in the reporting. Whether the results are generalizable to settings outside the United States where practice patterns may differ remains unknown. Misclassification of vital signs may have occurred in bedside data recording or transcription. However, we consider it likely that such misclassification would be non-differential (i.e. not related to the outcome) and would therefore generally result in bias towards the null.
We excluded a large group of patients based on missing vital signs. Although pre-arrest vital signs was a required data field during our study period we cannot be certain as to whether these data were missing due to not being documented by the clinical team or because of omissions by data abstractors. Although the differences between those with and without missing vital signs reached statistical significance for some variables, the absolute differences between the groups were very low (standardized difference < 0.1) except for a few variables (location and monitored status, see supplemental material). We do not have data on the activation of rapid response teams or any response by the patient’s clinical team to the abnormal vital signs. However, we do know that this patient population remained on the ward (as compared to being transferred to the ICU) indicating that there might have been an opportunity for earlier intervention prior to the cardiac arrest event if the vital signs could serve as an early warning of impending deterioration.
For the current study we a priori decided to only include full sets of heart rate, systolic blood pressure and respiratory rate within one to four hours before the arrest and only include patients on wards. Heart rate, systolic blood pressure and respiratory rate were chosen since they are uniformly and consistently measured among hospitalized patients and previous studies have found associations between these measurements and development of cardiac arrest.[12, 13] Other vital signs (e.g. temperature or oxygen saturation) or combinations of vital signs (e.g. mean arterial pressure or shock index [heart rate/systolic blood pressure]) may have stronger associations with outcome. Further studies are warranted to clarify this. The categorization of vital signs into abnormal and severely abnormal was based on clinical judgment and decided a priori. However, this specific selection is still arbitrary and other categorizations may have yielded different results.
6. Conclusion
Abnormal vital signs are common within one to four hours before in-hospital cardiac arrest events on hospital wards. Our study demonstrates incremental increases of overall in-hospital mortality with both increasing number of pre-arrest abnormal vital signs as well as increased severity of vital sign derangements.
Supplementary Material
Acknowledgments
Dr. Donnino had full access to all the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis. Andersen, Kim and Donnino were responsible for study concept and design, acquisition of data and drafting of the manuscript. Andersen and Novack conducted the statistical analysis. Andersen, Kim, Chase, Berg, Mortensen, Moskowitz, Novack, Cocchi and Donnino critically revised the manuscript for important intellectual content and approved the final version for submission. On behalf of all authors, the corresponding author states that there is no conflict of interest.
10. Funding Source
Dr. Donnino is supported by the NHLBI (1K02HL107447-01A1) and the American Heart Association (14GRNT200100002). Dr. Berg is supported by the American Heart Association (13CRP16930000). Dr. Cocchi is supported by the America Heart Association (15SDG22420010). Dr. Chase is supported by NIGMS (1K23GM101463-01K1).
Footnotes
7. Disclosures
Dr. Donnino is a paid consultant for the American Heart Association.
8. Conflict of Interest
None declared
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Critical care medicine. 2011;39:2401–6. doi: 10.1097/CCM.0b013e3182257459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. The New England journal of medicine. 1991;324:370–6. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- 4.Kohn LTCJ, Donaldson MS, editors. To err is human: building a safer health system. Washington, DC: national academy press; 2000. [PubMed] [Google Scholar]
- 5.Donnino MW, Salciccioli JD, Howell MD, et al. Time to administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: retrospective analysis of large in-hospital data registry. Bmj. 2014;348:g3028. doi: 10.1136/bmj.g3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan PS, Krumholz HM, Nichol G, Nallamothu BK American Heart Association National Registry of Cardiopulmonary Resuscitation I. Delayed time to defibrillation after in-hospital cardiac arrest. The New England journal of medicine. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 7.Kause J, Smith G, Prytherch D, et al. A comparison of antecedents to cardiac arrests, deaths and emergency intensive care admissions in Australia and New Zealand, and the United Kingdom--the ACADEMIA study. Resuscitation. 2004;62:275–82. doi: 10.1016/j.resuscitation.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 8.Smith AF, Wood J. Can some in-hospital cardio-respiratory arrests be prevented? A prospective survey. Resuscitation. 1998;37:133–7. doi: 10.1016/s0300-9572(98)00056-2. [DOI] [PubMed] [Google Scholar]
- 9.Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990;98:1388–92. doi: 10.1378/chest.98.6.1388. [DOI] [PubMed] [Google Scholar]
- 10.Hillman KM, Bristow PJ, Chey T, et al. Antecedents to hospital deaths. Internal medicine journal. 2001;31:343–8. doi: 10.1046/j.1445-5994.2001.00077.x. [DOI] [PubMed] [Google Scholar]
- 11.Franklin C, Mathew J. Developing strategies to prevent inhospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Critical care medicine. 1994;22:244–7. [PubMed] [Google Scholar]
- 12.Hodgetts TJ, Kenward G, Vlachonikolis IG, Payne S, Castle N. The identification of risk factors for cardiac arrest and formulation of activation criteria to alert a medical emergency team. Resuscitation. 2002;54:125–31. doi: 10.1016/s0300-9572(02)00100-4. [DOI] [PubMed] [Google Scholar]
- 13.Fieselmann JF, Hendryx MS, Helms CM, Wakefield DS. Respiratory rate predicts cardiopulmonary arrest for internal medicine inpatients. Journal of general internal medicine. 1993;8:354–60. doi: 10.1007/BF02600071. [DOI] [PubMed] [Google Scholar]
- 14.Hodgetts TJ, Kenward G, Vlackonikolis I, et al. Incidence, location and reasons for avoidable inhospital cardiac arrest in a district general hospital. Resuscitation. 2002;54:115–23. doi: 10.1016/s0300-9572(02)00098-9. [DOI] [PubMed] [Google Scholar]
- 15.Galhotra S, DeVita MA, Simmons RL, Dew MA Members of the Medical Emergency Response Improvement Team C. Mature rapid response system and potentially avoidable cardiopulmonary arrests in hospital. Quality & safety in health care. 2007;16:260–5. doi: 10.1136/qshc.2007.022210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones DA, DeVita MA, Bellomo R. Rapid-response teams. The New England journal of medicine. 2011;365:139–46. doi: 10.1056/NEJMra0910926. [DOI] [PubMed] [Google Scholar]
- 17.Nehme Z, Andrew E, Bray JE, et al. The significance of pre-arrest factors in out-of-hospital cardiac arrests witnessed by emergency medical services: a report from the Victorian Ambulance Cardiac Arrest Registry. Resuscitation. 2015;88:35–42. doi: 10.1016/j.resuscitation.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 18.Skrifvars MB, Boyd J, Kuisma M. Prearrest signs of shock and respiratory insufficiency in out-of-hospital cardiac arrests witnessed by crew of the emergency medical service. Am J Emerg Med. 2009;27:440–8. doi: 10.1016/j.ajem.2008.03.027. [DOI] [PubMed] [Google Scholar]
- 19.Skrifvars MB, Nurmi J, Ikola K, Saarinen K, Castren M. Reduced survival following resuscitation in patients with documented clinically abnormal observations prior to in-hospital cardiac arrest. Resuscitation. 2006;70:215–22. doi: 10.1016/j.resuscitation.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 21.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style’. American Heart Association. Circulation. 1997;95:2213–39. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 22.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–97. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 23.Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA: the journal of the American Medical Association. 2008;299:785–92. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 24.Bellomo R, Goldsmith D, Uchino S, et al. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Critical care medicine. 2004;32:916–21. doi: 10.1097/01.ccm.0000119428.02968.9e. [DOI] [PubMed] [Google Scholar]
- 25.Howell MD, Ngo L, Folcarelli P, et al. Sustained effectiveness of a primary-team-based rapid response system. Critical care medicine. 2012;40:2562–8. doi: 10.1097/CCM.0b013e318259007b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Girotra S, Nallamothu BK, Spertus JA, et al. Trends in survival after in-hospital cardiac arrest. The New England journal of medicine. 2012;367:1912–20. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steel AC, Reynolds SF. The growth of rapid response systems. Joint Commission journal on quality and patient safety/Joint Commission Resources. 2008;34:489–95. 33. doi: 10.1016/s1553-7250(08)34062-8. [DOI] [PubMed] [Google Scholar]
- 28.Gao H, McDonnell A, Harrison DA, et al. Systematic review and evaluation of physiological track and trigger warning systems for identifying at-risk patients on the ward. Intensive care medicine. 2007;33:667–79. doi: 10.1007/s00134-007-0532-3. [DOI] [PubMed] [Google Scholar]
- 29.Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation. 2013;84:465–70. doi: 10.1016/j.resuscitation.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 30.Foraida MI, DeVita MA, Braithwaite RS, Stuart SA, Brooks MM, Simmons RL. Improving the utilization of medical crisis teams (Condition C) at an urban tertiary care hospital. Journal of critical care. 2003;18:87–94. doi: 10.1053/jcrc.2003.50002. [DOI] [PubMed] [Google Scholar]
- 31.Bleyer AJ, Vidya S, Russell GB, et al. Longitudinal analysis of one million vital signs in patients in an academic medical center. Resuscitation. 2011;82:1387–92. doi: 10.1016/j.resuscitation.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 32.Smith GB, Prytherch DR, Schmidt PE, et al. Should age be included as a component of track and trigger systems used to identify sick adult patients? Resuscitation. 2008;78:109–15. doi: 10.1016/j.resuscitation.2008.03.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


