Abstract
Rationale and Objectives
Inefficient transfer of personal health records among providers negatively impacts quality of health care and increases cost. This multicenter study evaluates the implementation of the first Internet-based image-sharing system that gives patients ownership and control of their imaging exams, including assessment of patient satisfaction.
Materials and Methods
Patients receiving any medical imaging exams in four academic centers were eligible to have images uploaded into an online, Internet-based personal health record. Satisfaction surveys were provided during recruitment with questions on ease of use, privacy and security, and timeliness of access to images. Responses were rated on a five-point scale and compared using logistic regression and McNemar's test.
Results
A total of 2562 patients enrolled from July 2012 to August 2013. The median number of imaging exams uploaded per patient was 5. Most commonly, exams were plain X-rays (34.7%), computed tomography (25.7%), and magnetic resonance imaging (16.1%). Of 502 (19.6%) patient surveys returned, 448 indicated the method of image sharing (Internet, compact discs [CDs], both, other). Nearly all patients (96.5%) responded favorably to having direct access to images, and 78% reported viewing their medical images independently. There was no difference between Internet and CD users in satisfaction with privacy and security and timeliness of access to medical images. A greater percentage of Internet users compared to CD users reported access without difficulty (88.3% vs. 77.5%, P < 0.0001).
Conclusion
A patient-directed, interoperable, Internet-based image-sharing system is feasible and surpasses the use of CDs with respect to accessibility of imaging exams while generating similar satisfaction with respect to privacy.
Keywords: Personal health record, Image sharing, Internet, Integrating the healthcare enterprise
INTRODUCTION
Patients increasingly receive medical care from multiple providers, often in different practices, institutions, or geographic locations. In this complex healthcare delivery system, protected health information must be exchanged efficiently and in a manner that ensures its privacy and security, as mandated by the federal Health Insurance Portability and Accountability Act (1–4). Portable media, namely compact discs (CDs), are most commonly used to exchange medical images beyond the local environment. However, CDs may be misplaced or damaged, and data may be written in proprietary formats that the recipient is unable to access, often with image display software requiring administrative permission to install (5–7).
Several Internet-based systems for electronic sharing of medical images are now being employed (5,8). These new technologies must meet public expectations of seamless connectivity and privacy, as experienced with online banking, online shopping, and social networks, and must foster patient engagement and partnership with their providers. Currently, little evidence exists on the satisfaction of patients with technologies that pursue such goals in radiology (9,10).
The Radiological Society of North America (RSNA) has recently developed the RSNA Image Share Network (ISN), a standards-based solution built on image-enabled online personal health records (PHRs). The RSNA ISN is unique in the way it incorporates the principle of patients’ ownership of their medical records, enabling unaffiliated providers to share radiological images over the Internet with the patient's permission (8). This study reports the preliminary experience with a multicenter implementation of this image-exchange system, assessing feasibility and patient satisfaction with the use of this technology, as compared to the use of CDs.
MATERIALS AND METHODS
Setting
This study was approved by the institutional review boards of the participating sites and is compliant with the Health Insurance Portability and Accountability Act. The RSNA, with a grant from the National Institute of Biomedical Imaging and Bioengineering, developed the RSNA ISN, to facilitate the exchange of radiologic images between providers and their patients through the use of PHRs. Technical details of the system have been reported elsewhere and involved developers at academic medical centers and in the vendor community (11). The RSNA ISN was implemented in four medical centers starting in 2011.
Patient Enrollment
All patients receiving medical imaging, such as computed tomography, magnetic resonance imaging, ultrasound, mammography, conventional X-ray, nuclear tests, interventional radiology, or fluoroscopy, in outpatient or inpatient settings, were eligible to participate in the RSNA ISN. An outline of the RSNA ISN program was printed on handouts distributed in the hospital radiology locations and presented by research coordinators in the outpatient waiting area. Handouts included a telephone helpline to assist patients with the use of the system. Informed consent was obtained from patients and/or their parents or guardians. A PHR uploaded with recent imaging exams with a two-factor authentication key (a personal eight-digit code and a patient-created password), was created for the participants at the time of enrollment. Between July 2012 and August 2013, for different periods at the participating institutions (3 months up to 1 year), patients enrolling into the program were asked to complete and return a brief survey after sharing their medical images with their healthcare provider. A preaddressed, stamped envelope was provided with the survey and, in two sites, a $20 gift card reward was offered for returned surveys. Enrollment in the RSNA ISN did not preclude the use of any other modality of image sharing. For example, in addition to the PHR, patients could obtain CDs to store and transfer their images.
Survey
The survey consisted of 17 questions drafted by a committee of two radiologists, one internist, and a policy analyst (Appendix S1). Clarity of wording, brevity, and content validity (credibility, accuracy, and relevance of the survey elements in relation to the topic) were verified by the coauthors and by additional expert opinion. A summary score of overall satisfaction was outside the purpose of this study. Patients required approximately 5 minutes to complete the survey. The questions assessed (1) what modality (CD alone, Internet alone, both CD and Internet, other, none) was used to share images and reports; (2) the perceived importance of rapid availability of images to the doctor; (3) satisfaction with access, privacy and security, and timeliness; (4) whether imaging exams had to be repeated because of problems with their availability; (5) whether images were viewed by the patient independently of the doctor; and (6) history of computer use, Internet purchasing, and social networking. Satisfaction was expressed using a five-point Likert scale where 1 = strongly agree, 2 = agree, 3 = neutral, 4 = disagree, and 5 = strongly disagree.
Analysis
Descriptive statistics were computed for patient demographics, imaging exams uploaded into PHRs, and survey responses. For continuous variables, mean and standard deviation, and median and interquartile range were reported. For continuous and categorical variables, t test and chi-square test were used to assess association between groups, respectively. Because of the skewed distribution and low frequencies within some response categories, the five-point Likert scale was dichotomized into two groups: agreement “strongly agree + agree” vs. all others. To assess the sensitivity of the dichotomization, analyses were also run with two additional ways of grouping responses: “strongly agree + agree + neutral” vs. all others and “strongly agree” only vs. all others.
The association between ease of access and the use of Internet or CDs was analyzed using McNemar's test of paired data and restricted to patients who reported having used both methods. For all other questions, the association between survey response and modality was modeled using logistic regressions. Odds ratio, 95% confidence interval, and P value are reported. All statistical analyses were done using SAS version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
Characteristics of the Population
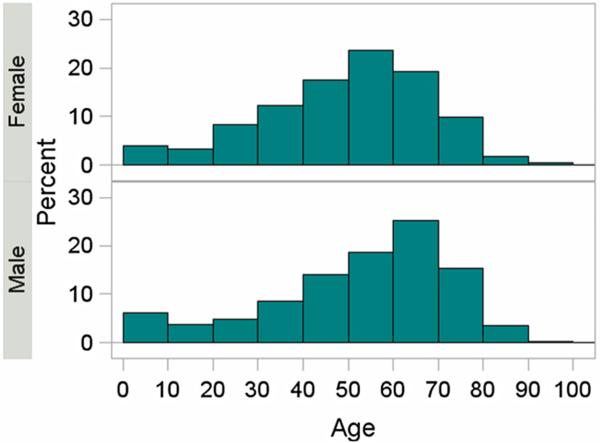
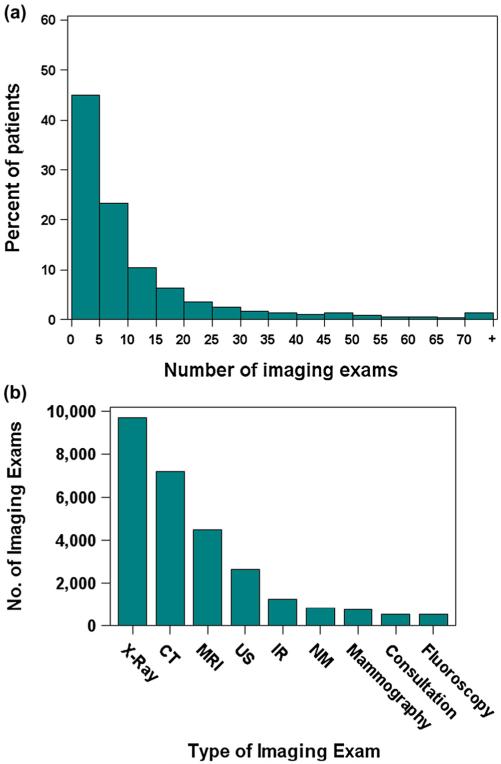
The cohort included 2562 patients (1381 females, 1181 males) with a broad age distribution mean age of 50.4 years (±19.4) (Fig 1). A total of 27,961 exams performed on these patients were uploaded into PHRs. The number of exams per participant varied from less than five to more than 70 (Fig 2a). The mean number of imaging exams per patient was 11 (standard deviation = 16) and the median number of imaging exams per patient was 5 (interquartile range: 2–12). The most common were plain X-rays (34.7%), followed by computed tomography (25.7%) and magnetic resonance imaging (16.1%) (Fig 2b).
Figure 1.
Age distribution by gender of patients enrolled into the RSNA Image Share Network program in 1 year (2012–2013). Aggregate data from four pilot sites are shown.
Figure 2.
(a) Number of imaging studies per patient and (b) type of images uploaded into the online personal health records.
In all, 502 (19.6%) patients returned the survey. The rate of return for the institutions offering gift cards was higher than the rate of return for institutions that did not offer gift cards: 30.2% vs. 11.2%. There were no significant differences in age (P = 0.36) nor gender (P = 0.09) between patients who returned the surveys and those who did not. In 54 surveys, either the doctor did not view the images or the viewing modality was not specified. These were excluded and the remaining 448 surveys were analyzed.
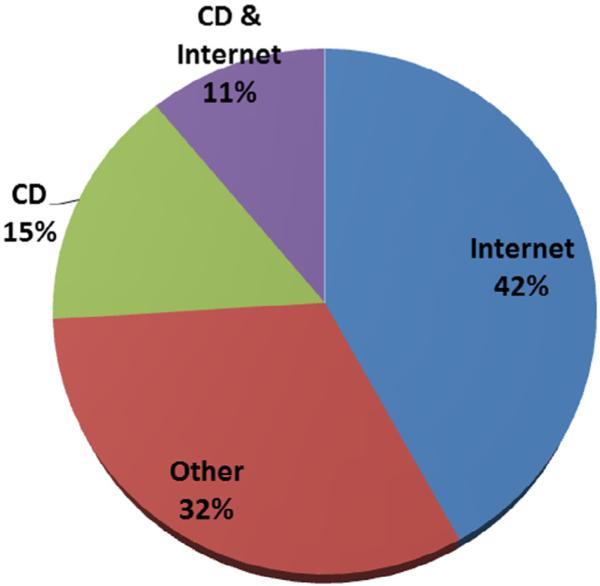
Selection of Modality to Transfer and View Images
The percentages of respondents using different methods to share their imaging exams with their physicians are shown in Figure 3. Despite enrollment into this program, 15% reported having used CD only. For 32% of respondents, the ordering physician and the radiologist were affiliated with the same institution, a situation that obviates a role for the patients in the transfer of their own images unless the patients were seeking the opinion of additional providers.
Figure 3.
Modality used by patients to share their medical images with their physicians.
Among respondents, 78% viewed medical images by themselves, often through the Internet (55%). Five (1%) respondents reported having repeated the exam for problem with access.
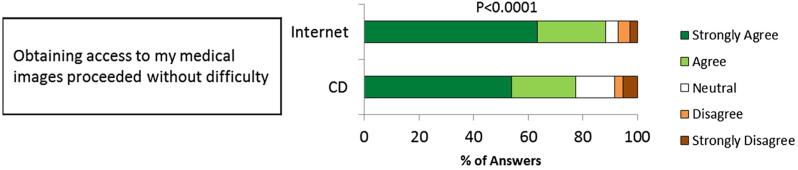
Experience With Access
Ease of access to medical images through both the Internet and the CD modality was assessed by 213 respondents. Access without difficulty was reported more frequently with Internet as compared to CD use (88.3% vs. 77.5%, P < 0.0001) (Fig 4). One hundred sixty-three patients rated ease of access for the Internet and CDs but did not report using both modalities in the survey. Among the 50 patients who reported having used both modalities, 94% reported that access to images proceeded without difficulty with the Internet-based RSNA ISN, compared to 80.0% who reported no difficulty in access to images with CDs (P < 0.0001).
Figure 4.
Survey responses on patients’ experience with image access. Rates of agreement “agree + strongly agree” were analyzed with McNemar's test for paired data (n = 213).
Experience With Sharing
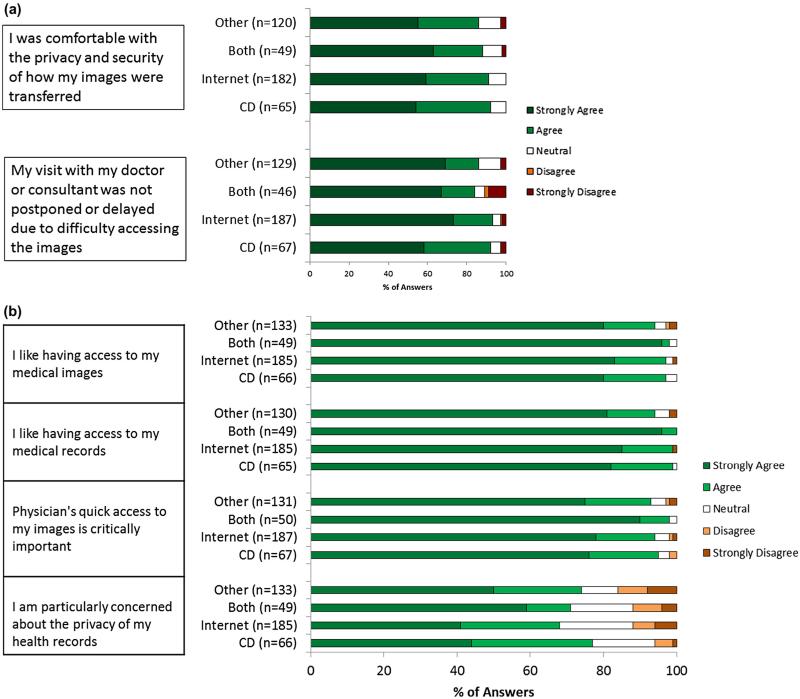
Patients’ responses about their recent experience with sharing images and their opinions on issues related to this topic were grouped by the method they used to share images (Fig 5a,b). Satisfaction with privacy and security was not significantly different between those who used the Internet and those who used other methods (Table 1). Similarly, visits were not delayed or postponed because of difficulty in accessing patient images. Results from a narrower (strongly agree only) and a broader (strongly agree + agree + neutral) definition of the category agreement are shown in Appendix S2.
Figure 5.
Patients’ experience (a) and opinions (b) by modality used to share images. Rates of agreement (“agree + strongly agree”) were analyzed by logistic regression using the Internet as the reference.
TABLE 1.
Patient Answers to Survey Questions
| Survey Question | Agreement vs. All Others* | ||
|---|---|---|---|
| OR (95% CI)** | |||
| Patient experience | I was comfortable with the privacy and security | CD | 1.18 (0.41, 3.35) |
| Both | 0.68 (0.25, 1.83) | ||
| Other | 0.58 (0.28, 1.21) | ||
| Visit was not delayed or postponed | CD | 0.84 (0.31, 2.27) | |
| Both | 0.53 (0.19, 1.46) | ||
| Other | 0.50 (0.24, 1.04) | ||
| Patient perspective | I like having direct access to my exam images | CD | 0.72 (0.13, 4.02) |
| Both | 1.04 (0.11, 9.51) | ||
| Other | 0.35 (0.10, 1.17) | ||
| I like having direct access to my medical records | CD | 0.36 (0.04, 3.51) | |
| Both | 0.79 (0.03, 20.20) | ||
| Other | 0.13 (0.02, 0.79) | ||
| It was critically important that my doctor viewed my medical image quickly | CD | 0.93 (0.30, 2.88) | |
| Both | 6.42 (0.36, 113.94) | ||
| Other | 0.83 (0.34, 2.04) | ||
| In general, I am particularly concerned about maintaining the privacy of my health records | CD | 1.49 (0.79, 2.83) | |
| Both | 1.26 (0.62, 2.56) | ||
| Other | 1.36 (0.83, 2.24) | ||
Answers were grouped by modality of image sharing used by patients.
The Likert scale was dichotomized into two groups for the analysis: agree and strongly agree combined vs neutral, disagree, and strongly disagree combined.
Results of logistic regression using the Internet as the reference group.
A high proportion of respondents (94%) agreed that enabling physicians to quickly access medical images was critically important and appreciated having the ability to directly access their own images (96%) and medical reports (98%) (Fig 5b). The privacy of health records was a significant concern for 68% of Internet users and 77% of CD users.
To evaluate the possibility that a reward for returning the survey influenced patient answers, we compared results of centers that did and did not offer gift cards. There were no significant differences in the responses received by these centers.
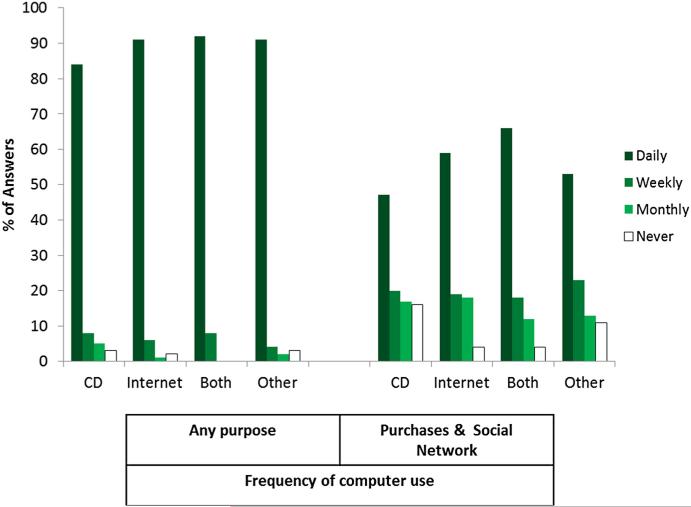
History of Computer Use
The majority (90%) of patients reported daily computer use. Frequency of Internet use, including purchasing and social networking activities, did not differ significantly between those who shared their images through the Internet and those who shared their images using all other modalities (Fig 6).
Figure 6.
Frequency of computer use for general purposes and for purposes requiring exchange of private information by modality used to share images.
DISCUSSION
Inefficient communication of imaging exams impacts the quality and cost of health care, and is increasingly frustrating for a public accustomed to seamless communication and transfers of digital data (1–3,12,13). Solutions for sharing medical images across unaffiliated providers must guarantee privacy and security of personal health information and address the desire of patients to become more active and informed participants in the medical decisions that concern them (14). Among the current solutions, the RSNA ISN is the first that places access to medical images directly under patient control. Our study reports the use and the satisfaction of patients with the initial implementation of this system.
Previous observations have indicated a demand for direct patient access to medical data and dissatisfaction with the prevailing paradigm, in which clinical information (such as laboratory test and imaging results) is provided verbally, and often days if not weeks later (15–19). Confirming these earlier observations, our findings show that nearly all respondents were favorable to having direct access to images and reports (Fig 5b). Furthermore, 78% viewed their medical images independently, mostly through the Internet. Patients’ access to their data is a core requirement of the Office of the National Coordinator for Health Information Technology Meaningful Use program, and is believed to enhance patients’ self-management, engagement, and participation in treatment decisions and potentially improve health outcomes (12,18,20,21).
Barriers exist against using the Internet to exchange health information, including computer literacy and uncertainties about security (14,22). In our study, many patients who established an online PHR still relied on carrying CDs, or requested their images and reports to be mailed in CD format to their doctor. Of note, more patients used the Internet to view their images than to exchange their images. As patients gain confidence with the privacy and the security of their electronic PHRs overtime, the gap between their use as a repository of personal health information for exclusive personal access and their use as a tool for information exchange, may likely diminish. Encouragingly, satisfaction with privacy and security of CD users and Internet users were similar (Fig 5a, Table 1). Local networks that link referring physicians and radiologists directly via picture archiving and communication systems or electronic medical records, captured in our study in the category “other,” obviated the role of patients in transferring test results. Clearly, the PHR was of greater value for transferring images to providers outside the originating healthcare system.
Ease of access is a critical element to the adoption of this new technology (23). In this study, the Internet-based RSNA ISN was rated more favorably than CDs (Fig 4). Compared to CDs, the Internet offers several clear advantages in the ability to organize, store, view, and retrieve health information. Elderly patients, the demographic with the greatest healthcare utilization, often perceive or experience significant barriers in using information technology (24,25). However, the substantial representation of elderly patients among the early adopters of this program demonstrates their interest in tools that could facilitate management of their complex medical records and communication with their providers (Fig 1). In fact, patients with complex medical histories may have been particularly receptive to the potential advantages of using the Internet, as reflected by the high number of imaging exams per patient among participants (Fig 2).
Delays in transferring imaging data can be a source of anxiety or even affect medical decisions, treatment plans, and potentially, health outcomes. The Internet might eliminate the time associated with mailing or physically bringing the CDs to the healthcare provider or the unexpected delays arising from incompatible formats, damaged CDs, or nonstandard, difficult to use or install image viewers. Equal perception about physician ease of access to medical images and equal assessment of delays due to technical access issues between PHR and CD users, suggested a similar impact on physicians’ workflow. By focusing on the most recent medical imaging test performed on the patient, however, our survey does not fully capture the increased ease with which image-enabled PHRs permit access to historical data.
The majority of respondents were frequent computer users familiar with tasks that require the input of personal information, such as online banking and online shopping. Familiarity with a computer might be an important determinant in the choice of the modality to exchange images; however, some-what surprisingly, there were only minor differences in frequency of computer use between patients who shared their medical images through the Internet and patients who used CDs (Fig 6). Online exchange of personal health data, specifically medical images, may be associated with different barriers, specific to the medical sphere, with higher thresholds for gaining trust in the protection of privacy and security.
Study Limitations
First, a minority of the patients (20%) returned the survey. These respondents, therefore, may not be representative of the general population. Offering a gift card increased return rates. Although, theoretically, rewards could influence not only return rates but also responses, for example, by inducing more favorable opinions, patients with and without compensation showed no difference in the way they regarded their own image sharing experience. Second, the scope of the survey was limited to assess basic information about ease of use, interest in having direct access to images, concerns about privacy, and impact on the timeliness of the visit. Whether health information was provided in a format that permitted and enhanced patient comprehension or engagement in care remains to be explored. Third, participation implied having responded to a solicitation to use an “Internet-based system.” Thus, patients with a negative predisposition to this service opted out, which may affect the generalizability of our results. Finally, we did not examine the specific indications for medical imaging or patient's clinical history.
CONCLUSIONS
We implemented a patient-directed Internet-based image sharing system at multiple centers across the country, achieving widespread utilization. Our preliminary experience indicates that the RSNA ISN functions well to permit a secure exchange of medical images and surpasses CDs with respect to ease of access for patients. Patients responded highly favorably having ownership of and access to their medical images using Internet PHR, at least as much as other established methods for image sharing, such as CDs. The online PHR also meets patients’ expectations regarding timeliness and privacy. This was intended as a pilot and model program. The program itself is dynamic and changes are continually being introduced to meet the needs of the end users. It provides one of several possible long-term solutions to easy but secure interoperability; one that emphasizes patient engagement. Future work is necessary to explore the impact of patient-directed online medical image sharing with respect to quality of care metrics and utilization.
Supplementary Material
ACKNOWLEDGMENTS
This project is supported by the National Heart Lung and Blood Institute and the National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health: Contract Award Number HHSN268201200078C “Medical Image Sharing Through a Patient-Controlled Exchange System”.
The authors wish to thank Drs. David E. Avrin and Omer Awan for their critical contributions to the Radiological Society of North America Image Share Network and their comments on this study. The authors are also indebted to Seth Goldfarb for his assistance in data management.
Abbreviations
- PHI
protected health information
- CD
compact disc
- PHR
personal health record
- ISN
Image Share Network
Footnotes
APPENDIX. SUPPLEMENTARY MATERIAL
Supplementary data to this article can be found online at doi:10.1016/j.acra.2015.10.012.
REFERENCES
- 1.Mendelson DS, Bak PR, Menschik E, et al. Informatics in radiology: image exchange: IHE and the evolution of image sharing. Radiographics. 2008;28:1817–1833. doi: 10.1148/rg.287085174. [Epub 2008/09/06]. [DOI] [PubMed] [Google Scholar]
- 2.Bodenheimer T. Coordinating care—a perilous journey through the health care system. N Engl J Med. 2008;358:1064–1071. doi: 10.1056/NEJMhpr0706165. [Epub 2008/03/07.]. [DOI] [PubMed] [Google Scholar]
- 3.Kuperman GJ. Health-information exchange: why are we doing it, and what are we doing? J Am Med Inform Assoc. 2011;18:678–682. doi: 10.1136/amiajnl-2010-000021. [Epub 2011/06/17]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orszag PR. Evidence on the costs and benefits of health information technology. Statement of the Director of the Congressional Budget Office. 2008 [Google Scholar]
- 5.Ge Y, Ahn DK, Unde B, et al. Patient-controlled sharing of medical imaging data across unaffiliated healthcare organizations. J Am Med Inform Assoc. 2013;20:157–163. doi: 10.1136/amiajnl-2012-001146. [Epub 2012/08/14]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hagiwara H, Nemoto A, Inoue T. Burden on university hospitals of handling Portable Data for Imaging (PDI) media. Appl Clin Inform. 2014:46–57. doi: 10.4338/ACI-2013-07-RA-0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Erickson BJ. Experience with importation of electronic images into the medical record from physical media. J Digit Imaging. 2011;24:694–699. doi: 10.1007/s10278-011-9364-3. [Epub 2011/02/03]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mendelson DS, Rubin DL. Imaging informatics: essential tools for the delivery of imaging services. Academic radiology. 2013;20:1195–212. doi: 10.1016/j.acra.2013.07.006. [Epub 2013/09/14]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaelber DC, Jha AK, Johnston D, et al. A research agenda for personal health records (PHRs). J Am Med Inform Assoc. 2008;15:729–736. doi: 10.1197/jamia.M2547. [Epub 2008/08/30]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gadd CS, Ho Y-X, Cala CM, et al. User perspectives on the usability of a regional health information exchange. J Am Med Inform Assoc. 2011;18:711–716. doi: 10.1136/amiajnl-2011-000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Langer SG, Tellis W, Carr C, et al. The RSNA image sharing network. J Digit Imaging. 2014;28:53–61. doi: 10.1007/s10278-014-9714-z. [Epub 2014/07/20]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363:501–504. doi: 10.1056/NEJMp1006114. [Epub 2010/07/22]. [DOI] [PubMed] [Google Scholar]
- 13.Flanders AE. Medical image and data sharing: are we there yet? Radiographics. 2009;29:1247–1251. doi: 10.1148/rg.295095151. [Epub 2009/09/17]. [DOI] [PubMed] [Google Scholar]
- 14.Mandl KD, Szolovits P, Kohane IS. Public standards and patients’ control: how to keep electronic medical records accessible but private. BMJ. 2001;322:283–287. doi: 10.1136/bmj.322.7281.283. [Epub 2001/02/07]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson AJ, Frankel RM, Williams LS, et al. Patient access to radiology reports: what do physicians think? J Am Coll Radiol. 2010;7:281–289. doi: 10.1016/j.jacr.2009.10.011. [Epub 2010/04/07]. [DOI] [PubMed] [Google Scholar]
- 16.Keselman A, Slaughter L, Smith CA, et al. Towards consumer-friendly PHRs: patients’ experience with reviewing their health records. AMIA Ann Symp Proceed. 2007:399–403. [Epub 2008/08/13]. [PMC free article] [PubMed] [Google Scholar]
- 17.Wen KY, Kreps G, Zhu F, et al. Consumers’ perceptions about and use of the internet for personal health records and health information exchange: analysis of the 2007 Health Information National Trends Survey. J Med Internet Res. 2010;12:e73. doi: 10.2196/jmir.1668. [Epub 2010/12/21]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tang PC, Lansky D. The missing link: bridging the patient-provider health information gap. Health Aff (Millwood) 2005;24:1290–1295. doi: 10.1377/hlthaff.24.5.1290. [Epub 2005/09/16]. [DOI] [PubMed] [Google Scholar]
- 19.Johnson AJ, Easterling D, Williams LS, et al. Insight from patients for radiologists: improving our reporting systems. J Am Coll Radiol. 2009;6:786–794. doi: 10.1016/j.jacr.2009.07.010. [Epub 2009/11/03]. [DOI] [PubMed] [Google Scholar]
- 20.Ball MJ, Costin MY, Lehmann C. The personal health record: consumers banking on their health. Stud Health Technol Inform. 2008;134:35–46. [Epub 2008/04/01]. [PubMed] [Google Scholar]
- 21.Delbanco T, Berwick DM, Boufford JI, et al. Healthcare in a land called PeoplePower: nothing about me without me. Health Expect. 2001;4:144–150. doi: 10.1046/j.1369-6513.2001.00145.x. [Epub 2001/08/09]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Whiddett R, Hunter I, Engelbrecht J, et al. Patients’ attitudes towards sharing their health information. Int J Med Inform. 2006;75:530–541. doi: 10.1016/j.ijmedinf.2005.08.009. [Epub 2005/10/04]. [DOI] [PubMed] [Google Scholar]
- 23.Tang PC, Ash JS, Bates DW, et al. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13:121–126. doi: 10.1197/jamia.M2025. [Epub 2005/12/17]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yamin CK, Emani S, Williams DH, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;171:568–574. doi: 10.1001/archinternmed.2011.34. [Epub 2011/03/30]. [DOI] [PubMed] [Google Scholar]
- 25.Wyatt E. Most of U.S. is wired, but millions aren't plugged in. August. Vol. 19. New York Times; 2013. p. 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.