Abstract
Background
Substantial racial/ethnic disparities exist in HIV infection among people who inject drugs (PWID) in many countries. To strengthen efforts to understand the causes of disparities in HIV-related outcomes and eliminate them, we expand the “Risk Environment Model” to encompass the construct “racialized risk environments,” and investigate whether PWID risk environments in the United States are racialized. Specifically, we investigate whether black and Latino PWID are more likely than white PWID to live in places that create vulnerability to adverse HIV-related outcomes.
Methods
As part of the Centers for Disease Control and Prevention’s National HIV Behavioral Surveillance, 9,170 PWID were sampled from 19 metropolitan statistical areas (MSAs) in 2009. Self-reported data were used to ascertain PWID race/ethnicity. Using Census data and other administrative sources, we characterized features of PWID risk environments at four geographic scales (i.e., ZIP codes, counties, MSAs, and states). Means for each feature of the risk environment were computed for each racial/ethnic group of PWID, and were compared across racial/ethnic groups.
Results
Almost universally across measures, black PWID were more likely than white PWID to live in environments associated with vulnerability to adverse HIV-related outcomes. Compared to white PWID, black PWID lived in ZIP codes with higher poverty rates and worse spatial access to substance abuse treatment and in counties with higher violent crime rates. Black PWID were less likely to live in states with laws facilitating sterile syringe access (e.g., laws permitting over-the-counter syringe sales). Latino/white differences in risk environments emerged at the MSA level (e.g., Latino PWID lived in MSAs with higher drug-related arrest rates).
Conclusion
PWID risk environments in the US are racialized. Future research should explore the implications of this racialization for racial/ethnic disparities in HIV-related outcomes, using appropriate methods.
Keywords: risk environments, critical race theory, National HIV Behavioral Surveillance, injection drug use, HIV, residence characteristics
Introduction
A recent systematic review of international evidence found that HIV prevalence among people who inject drugs (PWID) is twice as high among racial/ethnic minority PWID than among racial/ethnic majority PWID (Des Jarlais, Cooper et al. 2012). Disparities in HIV prevalence among PWID are particularly stark in the United States (US), where HIV prevalence is six and eleven times higher among Latino and non-Hispanic black PWID, respectively, than among non-Hispanic white PWID (Centers for Disease Control and Prevention 2006, Laffoon, Satcher Johnson et al. 2011, Lansky, Finlayson et al. 2014). The broad ranges of these disparities reflect geographic variation in the distribution of HIV within and across racial/ethnic groups. These disparities have persisted since the early days of the epidemic in the US (Friedman, Quimby et al. 1997, Kottiri, Friedman et al. 2002). Racial/ethnic differences in risk behaviors do not explain them: Latino and non-Hispanic black PWID are as likely or often less likely to report injection-related and sexual risk behaviors than non-Hispanic white PWID (Friedman, Young et al. 1993, Cooper, Des Jarlais et al. 2011, Centers for Disease Control and Prevention 2012, Linton, Celentano et al. 2013, Williams, Eisenberg et al. 2013). Racial/ethnic disparities also exist in the progression of HIV infection among HIV-positive PWID in the US (Grigoryan, Hall et al. 2009). Accordingly, the US Centers for Disease Control and Prevention (CDC), the White House, the Department of Health and Human Services, and investigators have called for research and interventions into the ways in which social factors, including characteristics of the places people live, create and perpetuate these disparities (National Minority AIDS Council 2006, Friedman, Cooper et al. 2009, National Institute on Drug Abuse of the National Institutes of Health 2009, The White House Office of National AIDS Policy 2010, Centers for Disease Control and Prevention 2011, Centers for Disease Control and Prevention 2012, Office of Disease Prevention and Health Promotion in the U.S. Department of Health and Human Services 2012).
The Risk Environment Model is a powerful theoretical framework to guide studies of the social determinants of HIV-related outcomes among PWID; a particular strength is its focus on how characteristics of the places where PWID live, work, and engage in drug-related activities shape vulnerability (Rhodes 2002, Rhodes, Mikhailova et al. 2003, Rhodes, Singer et al. 2005, Rhodes 2009, Strathdee, Hallett et al. 2010). The Risk Environment Model has, however, been underutilized in studies of racial/ethnic disparities in HIV-related outcomes among PWID. This paper develops the concept of “racialized risk environments” and empirically investigates the extent to which PWID who are Latino, non-Hispanic black, and non-Hispanic white (hereafter referred to as black and white, respectively) live in different geographically-defined risk environments in the US. Fundamentally at issue in this analysis is whether black and Latino PWID live in riskier environments than white PWID.
Risk Environment Model
The Risk Environment Model foregrounds the social situations, structures, and places that generate vulnerability to HIV transmission and other drug-and HIV-related harms among PWID (Rhodes 2002, Rhodes, Mikhailova et al. 2003, Rhodes, Singer et al. 2005, Rhodes 2009, Strathdee, Hallett et al. 2010). The “risk environment” is defined as the “space… [where] factors exogenous to the individual interact to increase the chances of HIV transmission” (Rhodes, Singer et al. 2005, p. 1026) and other drug- and HIV-related harms, including HIV-related morbidity and mortality (Milloy, Marshall et al. 2012). This environment consists of four types of influence: influences that are social, economic, political, or physical (Rhodes 2002, Rhodes, Singer et al. 2005). Some of these influences may be features of places (e.g., neighborhood poverty rates), while others may not be rooted in place (e.g., risk networks, interpersonal discrimination).
The model posits that each type of influence operates at multiple, intersecting levels to affect individual vulnerability (Rhodes 2002, Rhodes, Mikhailova et al. 2003, Rhodes, Singer et al. 2005, Rhodes 2009, Strathdee, Hallett et al. 2010).
A large body of evidence testifies to the explanatory power of the Risk Environment Model (Rhodes, Singer et al. 2005, Degenhardt, Mathers et al. 2010, Strathdee, Hallett et al. 2010). Studies have used it to identify policies and other contextual factors that seem to influence HIV acquisition and disease progression among PWID (Strathdee, Hallett et al. 2010, Milloy, Marshall et al. 2012); to describe vulnerability to HIV among non-injection drug users (Goldenberg, Strathdee et al. 2011); and to inform mathematical models that explore the relationships between environmental factors and HIV (Strathdee, Hallett et al. 2010). This model has rarely, however, been applied to study racial/ethnic disparities in HIV-related outcomes among PWID.
Racialized Risk Environments
To advance research and interventions into disparities in HIV-related outcomes among PWID, we have previously proposed that place-based features of risk environments may be “racialized” in the US (Cooper, Bossak et al. 2009). A risk environment is racialized when racial/ethnic groups of PWID inhabit places that differ systematically in the availability of protective features (e.g., substance abuse treatment programs) and in the presence of harmful features (e.g., police drug crackdowns). In addition to being rooted in the Risk Environment Model, the construct “racialized risk environments” has origins in Critical Race Theory (Bonilla-Silva 2001). Central to Critical Race Theory is the concept of racialized social systems in which
“…economic, political, social, and ideological [hierarchies] are partially structured by the placement of actors in racial categories…The race placed in the superior position tends to receive greater economic remuneration and access to better occupations and prospects in the labor market, occupies a primary position in the political system, is granted higher social estimation…, often has the license to draw physical (segregation) as well as social (racial etiquette) boundaries…and receives what W.E.B. DuBois called a ‘psychological wage.’ “ (Bonilla-Silva 2001, p. 37).
In the US, racialized social systems can manifest geographically. Within metropolitan areas, racial/ethnic residential segregation sorts members of different racial/ethnic groups into neighborhoods that are both separate and unequal (Massey and Denton 1989, Massey and Denton 1993, Logan and Stults 2011). In US metropolitan areas in 2010, the average black resident lived in a census tract in which 45% of the other residents were black, 35% were white, and 15% were Latino (Logan and Stults 2011). A parallel pattern existed for Latinos (Logan and Stults 2011). The average white resident lived in a tract where 75% of the other residents were white and just 8% were black and 11% were Latino (Logan and Stults 2011). Within segregated metropolitan areas, predominately black neighborhoods (often measured as census tracts) tend to have fewer social, economic, political, and physical resources and more hazards than predominately white neighborhoods; the same is true for predominately Latino neighborhoods, though perhaps to a lesser extent (Massey and Denton 1989, Massey and Denton 1993). For example, in urban areas predominately black neighborhoods tend to have higher densities of abandoned buildings, worse municipal services, and poorer housing quality than predominately white neighborhoods (Williams and Collins 2001).
Members of different racial/ethnic groups may also experience different living environments in larger geographic areas (e.g., counties, municipalities, metropolitan areas). To illustrate, municipalities with higher proportions of black residents invest less in parks (Joassart-Marcelli 2010).
Racial/ethnic differences in features of the environments where people live are associated with disparities in several health outcomes in the general population (Do, Finch et al. 2008, Bleich, Thorpe et al. 2010, Laveist, Pollack et al. 2011). For example, an analysis of the US National Health Interview Survey data found that differences in neighborhood context explained 38%–76% (depending on the age group) of the black/white disparity in self-rated health among men, after adjusting for individual-level factors (Do, Finch et al. 2008); self-rated health strongly predicts mortality (Idler and Kasl 1991, Idler and Benyamini 1997, Idler, Russell et al. 2000). Conversely, disparities in diabetes and obesity disappear and disparities in hypertension are reduced when black and white adults live in racially integrated neighborhoods (Bleich, Thorpe et al. 2010, Laveist, Pollack et al. 2011).
Despite the promise of studies on the environments where people live and health disparities in the general population, the prominence of the Risk Environment Model in studies of PWID health, and the magnitude of disparities in HIV infection and HIV disease progression among PWID, research on whether and how place characteristics predict racial/ethnic disparities in HIV-related outcomes among PWID remains rare. To support the development of this line of inquiry and of the Risk Environment Model, this paper describes the extent to which place-based features of risk environments are racialized in a large sample (N=9170) of PWID living in the US.
Methods
Study description and analytic sample
We integrated 2009 surveillance data about PWID living in 19 US metropolitan statistical areas (MSAs) with Census data and data from other existing administrative sources to describe features of the environments where PWID lived. Data on individual PWID were drawn from the 2009 cycle of the CDC’s National HIV Behavioral Surveillance (NHBS) (Gallagher, Sullivan et al. 2007). NHBS collects data on HIV serostatus, HIV-related risk behaviors, and health service use among PWID, men who have sex with men, and heterosexuals at high risk for HIV infection (Gallagher, Sullivan et al. 2007).
NHBS has two units of analysis: MSAs and individuals. MSAs contain at least one central city and its neighboring counties that have a high degree of socioeconomic integration with the central city (Office of Management and Budget 2013); typically, an MSA consists of at least one central city and its surrounding suburbs. In 2009, NHBS surveyed 20 MSAs with the highest AIDS burden: MSAs represented approximately 60% of all people living with diagnosed HIV infection who had ever been diagnosed with AIDS in urban areas with a population size ≥500,000 at the end of 2009 (Centers for Disease Control and Prevention 2012, Centers for Disease Control and Prevention 2012,Broz, Wejnert et al. 2014). One MSA, San Juan-Bayamon, was excluded from the present analyses because of the lack of racial/ethnic diversity in the PWID sample (98% were Latino), creating a sample size of 19 MSAs.
PWID were sampled in each MSA using respondent-driven sampling (RDS) (Lansky, Abdul-Quader et al. 2007). Recruitment chains began with <15 seeds; each seed was asked to recruit ≤5 PWID (Centers for Disease Control and Prevention 2012). People were eligible to participate if they reported injecting drugs in the past 12 months and provided proof of injection (e.g., track marks); lived in the target MSA; and were ≥18 years old (Lansky, Abdul-Quader et al. 2007).
Recruitment continued for 6 months, on average, until approximately 500 people were enrolled in each MSA. A total of 9,741 PWID were enrolled across the 19 MSAs. Participants who lacked valid ZIP code information (n=402, 4.1%) were excluded from analyses. Participants who identified as non-Hispanic “other race” or had missing race information were excluded (N=169, 1.7%), creating a final sample size of 9170.
Measures
Individual race/ethnicity
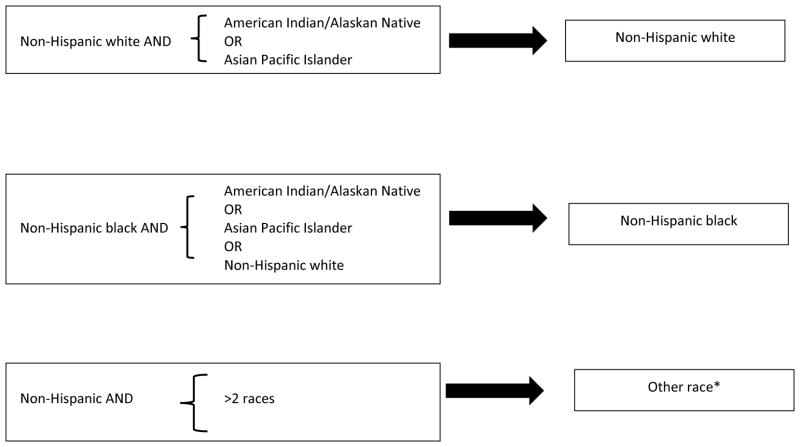
We analyzed NHBS participants’ self-report data to create three mutually exclusive racial/ethnic groups: Latino, white, and black. Two-hundred and seventy four (3%) participants reported that they belonged to two racial groups and were not Latino. To assign these individuals to a single racial/ethnic group we followed the Office of Management and Budget’s “plurality” guidelines (Figure 1) (U.S. Office of Management and Budget 2000). Plurality guidelines are based on analyses of National Household Interview Survey data linking responses to items allowing individuals to identify as a member of multiple racial/ethnic groups with items requiring individuals to identify with a single racial/ethnic group (U.S. Office of Management and Budget 2000).
Figure 1.
Applying plurality guidelines to assign non-Hispanic PWID who identified as being members of multiple racial groups to a single racial group
*Members of other racial/ethnic groups were excluded from analyses because of their small numbers.
Geographic areas
Participants reported the ZIP code area and county where they lived. Homeless participants were assigned to ZIP codes and counties based on the place where they usually slept. Participants were linked to MSAs based on the site of data collection and to states based on county of residence.
Other individual-level covariates
For descriptive purposes, data on participant sociodemographic characteristics, HIV serostatus, and drug-related behaviors were extracted from NHBS.
Features of the risk environment
Table 1 presents the features of the risk environment studied here, the geographic scale at which each feature was operationalized, and data sources. Features were selected based on past research about place-based exposures and HIV-related outcomes among PWID; we also included some place-based exposures that have been associated with HIV-related outcomes (e.g., infection with other sexually transmitted infections [STIs], condom use) in other key populations and could plausibly predict HIV among PWID as well (e.g., alcohol outlet density). Unless otherwise noted in Table 1, data captured features of the risk environment in 2009.
Table 1.
Constructs and Variables Studied and Data Sources Used to Operationalize Constructs
| Types of Influence | Construct | Variables (Geographic Scale) | Data Source(s) |
|---|---|---|---|
| Social | Availability of sex partners | Male:female sex ratio for adults (18–64 yrs; ZIP, county, MSA) | 2010 Decennial Census1, 2 |
| Racial/ethnic composition | Percent of total population who are non- Hispanic white, non-Hispanic black/ African-American, or Latino (ZIP) | American Community Survey (ACS) 5-year Estimates (2007–2011) | |
| Exposure to violence | Rate of reported violent crimes, per 1000 residents (county, MSA) | Numerator (reported number of violent crimes, as defined by the FBI): 2009 Inter- university Consortium for Political and Social Research (ICPSR) county-level detailed arrest and offense data. Denominator (population): ACS 5-year Estimates (2007–2011) | |
| Racial/ethnic residential segregation | Black Isolation Index (MSA)3 | 2010 US Decennial Census | |
| Latino Isolation Index (MSA)3 | 2010 US Decennial Census | ||
| Economic | Exposure to economic disadvantage | Median household income (ZIP; county; MSA) | ACS 5-year Estimates (2007–2011) |
| Percent of households below federal poverty line (ZIP; county; MSA) | ACS 5-year Estimates (2007–2011) | ||
| Percent of adults (≥16 yrs) in labor force who are unemployed (ZIP; county; MSA) | ACS 5-year Estimates (2007–2011) | ||
| Percent of adults (≥25 yrs) without a high school diploma or general equivalency diploma (ZIP; county; MSA) | ACS 5-year Estimates (2007–2011) | ||
| Income inequality | Gini Coefficient of Income Inequality (MSA)4 | 2010 Decennial Census | |
| Health and law enforcement interventions | Spatial access to drug- and HIV-related programs | Density of HIV testing sites per square mile (ZIP) | Numerator (testing sites): CDC’s 2009 National HIV Prevention Program Monitoring & Evaluation database Denominator (square miles): US Census Tiger Files |
| Spatial access to substance abuse treatment programs, (a) overall and (b) specifically to methadone maintenance programs (MMTPs; ZIP) | Described in the text. | ||
| Spatial access to syringe exchange programs (SEP) | Described in the text. | ||
| Access to general health care | Percent of adults (18–64 yrs) who are uninsured (county) Percent of residents living in a medically underserved area (county) |
2012–2013 Area Health Resource File5 2013 Health Professional Shortage Area Dataset1, 6 | |
| HIV epidemic among PWID7 | HIV prevalence among PWID | HIV prevalence data for 2002 were drawn from the Community Vulnerability and Response among drug-user related HIV/AIDS8 | |
| Exposure to law enforcement | Arrest rate for hard drug possession9, per 1000 adults (18–64 yrs; county, MSA) | Numerator (possession arrests): 2009 ICPSR county-level detailed arrest and offense data); Denominator (adults 18–64 yrs): ACS 5-year Estimates (2007–2011) | |
| Arrest rate for possession of any drug, per 1000 adults (18–64 yrs; county, MSA) | Numerator (possession arrests): 2009 ICPSR county-level detailed arrest and offense data Denominator (adults 18–64 yrs): ACS 5-year estimates (2007–2011) |
||
| Jail incarceration rate, per 1000 adults (18–64 yrs; MSA) | Numerator (jail inmates): 2010 Decennial census Denominator (adults 18–64 yrs): 2010 Decennial Census |
||
| Policies governing syringe access | Law permits purchase of syringes without a prescription (state) | Des Jarlais’ Robert-Wood Johnson Foundation (RWJF) study of laws governing over the counter (OTC) sales of syringes | |
| Law permits possession of a syringe without a prescription (state) | |||
| Law permits SEPs to operate (state) | |||
| Health and Law enforcement expenditures | Per capita expenditures on police (MSA) | Numerator (expenditures in USD): 2007 Census of Governments County Area Finances File Denominator (total population): US Census Bureau Population Estimates Program |
|
| Per capita expenditures on health (MSA) | |||
| Per capita expenditures on corrections (MSA) | |||
| Physical | Access to alcohol | Density per square mile of businesses licensed to sell alcohol for off-premises consumption (ZIP) | Numerator (premises): 2009 U.S Census Bureau’s Zip Code Business Patterns Denominator (square miles): US Census Tiger Files |
| Exposure to abandoned buildings | Density per square mile of abandoned property, (a) overall, and of (b) residential units, and (c) commercial properties (ZIP) | Numerator (housing or commercial properties): 2009 United States Postal Service (USPS) Delivery Statistics Product Denominator (square miles): US Census Tiger Files |
We operationalized each feature at its most conceptually appropriate geographic scale or at the geographic scale that had received the most empirical support in past studies. For example, we assessed racial/ethnic residential segregation (measured using the Isolation Index, as described in Table 1) within MSAs, and not within ZIP codes or counties, because segregation has been produced, in part, by the exodus of whites from central cities to suburbs (though white suburban workers continue to work in central cities) (Massey and Denton 1993, Frey 2011). Because evidence indicates a relationship between spatial access to alcohol outlets in small geographic areas and HIV-related health outcomes (Cohen, Ghosh-Dastidar et al. 2006), we operationalized alcohol outlet density within ZIP codes. In some cases, however, there was little evidence about operationalizing a feature at a particular scale; in these cases we operationalized it at several scales to permit comparisons.
We tailored the Risk Environment Model to suit the study’s aims in three ways. First, we defined a new type of influence: healthcare service and law enforcement interventions (Table 1). We constructed several measures of drug-related law enforcement activities and of drug- and HIV-related health service access because these risk environment features are strongly associated with HIV prevalence and injection-related risk behaviors among PWID (Cooper, Moore et al. 2005, Friedman, Cooper et al. 2006, Cooper, Des Jarlais et al. 2011, Cooper, Des Jarlais et al. 2012). Given the number of measures and their potential impact, we decided that they constituted their own type of influence. We included HIV prevalence among PWID in this set of influences because HIV prevalence is often used to locate service sites. Second, we eliminated the “political” type of influence. Few measures of political environments were available across all 19 MSAs; additionally, we shifted several features of the risk environment that are usually classified as political influences to the newly created health care service/law enforcement type of influence (e.g., policies governing syringe access). This analysis thus described the following types of influence: features of the social, economic, healthcare service/law enforcement, and physical environments.
Third, we altered the way in which the model classified “levels.” The Risk Environment Model typically has three levels: the microlevel, which includes networks, norms, and local settings; the mesolevel, which encompasses institutions and organizations; and the macrolevel, which covers policies, cultural factors, and social inequalities (Rhodes 2002, Rhodes, Mikhailova et al. 2003, Rhodes, Singer et al. 2005, Rhodes 2009, Strathdee, Hallett et al. 2010). Our analysis had many variables that could not be mapped onto these levels. For example, the violent crime rate in a county could not be classified as a feature of the microenvironment because counties are too large; cannot be classified as a feature of the mesoenvironment because violent crime is neither an institution nor an organization; and cannot be classified as feature of the macroenvironment because it is not a policy, inequality, or cultural factor. We therefore classified each type of influence according to the geographic scale(s) at which it was measured (i.e., ZIP code area, county, MSA, state).
Table 1 provides information on the construction of each variable. Creating measures of spatial access to substance abuse treatment and syringe exchange programs (SEPs), however, involved several assumptions, and so we describe the construction of those measures for the sake of transparency. We used gravity based methods (GBM) to measure spatial access to SEPs and substance abuse treatment (overall and for methadone maintenance treatment programs [MMTPs] specifically); GBMs are commonly used to assess spatial access to health service providers (Haynes and Fotheringhan 1984, Bailey and Gastrell 1995, Wang 2006, Cooper, Bossak et al. 2008, Cooper, Bossak et al. 2009, Cooper, Des Jarlais et al. 2011, Cooper, Des Jarlais et al. 2012, Cooper, Des Jarlais et al. 2012). GBMs assume that spatial access to providers is a function of (a) the travel distance between participant i’s home and each service site that is within a “reasonable travel distance” of his/her home; (b) a distance decay formula; and (c) the number of service opportunities at each site (Haynes and Fotheringhan 1984, Bailey and Gastrell 1995, Wang 2006). The spatial access measure ignores local need for services (e.g., total number of PWID, for the SEP access measure). We calculated these components as follows:
Estimating travel distance required locating both participants and programs in space. Because NHBS does not gather data on participants’ home addresses, we approximated each participant’s home address using the population-weighted center of his/her ZIP code area (i.e., “population-weighted centroid”), a common practice when street addresses are unavailable (Hwang and Rollow 2000, Luo and Wang 2003); on average ZIP codes were 9.17 square miles (standard deviation=17.96). Street address data on SEP site locations in 2009 were extracted from Des Jarlais’ “Dave Purchase Memorial Syringe Exchange Program Survey”(McKnight, Des Jarlais et al. 2005). Data on the street addresses of substance abuse treatment programs were drawn from the National Directory of Drug and Alcohol Abuse Treatment Programs (Office of Applied Studies in the Substance Abuse and Mental Health Services Administration 2010). Population-weighted centroids and program addresses were geocoded to their latitude and longitude. Based on past studies (Jacoby 1991, Fortney, Rost et al. 2000, Beardsley, Wish et al. 2003, Williams and Metzger 2010), “reasonable travel distance” between home and service sites was set to three miles. Thus, any program site located <3 miles of a ZIP code area’s population-weighted centroid along the local road network was included in that ZIP code area’s GBM calculation.
To recognize that sites that are farther away might be less attractive, the distance decay weight allowed access to decline with distance from home. We set this weight to 1.5 (Schuurman, Berube et al. 2010).
We did not know the number of treatment slots at each program or the number of syringes distributed by each SEP site. We therefore set the number of service opportunities=1 for each site.
GBM produced a unitless spatial access value for each ZIP code that ranged from 0 to the total number of sites ≤3 miles from home; higher values indicate better access.
We could not use GBM methods to assess spatial access to HIV testing sites because we did not have street address information for these sites; data were only available on number of testing sites in each ZIP code. We therefore calculated spatial density of testing sites per square mile.
Analyses
Variables describing the social, economic, health services/law enforcement, and physical features of risk environments were merged with NHBS data via the ZIP code area, county, MSA, and state where NHBS participants lived. We examined the distribution of each feature across each racial/ethnic group of PWID and calculated the mean and standard deviation (SD) of each feature for each racial/ethnic group. We initially used ANOVAs to compare means for each feature across racial/ethnic groups and determined whether white, black, and Latino PWID lived in different risk environments. With a sample of 9,710, however, p-values identified statistically significant differences in means even when means were quite similar across racial/ethnic groups. We re-calculated p-values using the number of geographic units (e.g., the number of ZIP codes when comparing ZIP-code level poverty rates across racial/ethnic groups). This process produced a new problem: because there were many more ZIP codes than counties and more counties than MSAs or states, racial/ethnic differences in means were much more likely to attain statistical significance when features were measured at the ZIP-code level. We thus chose a measure of substantive significance to determine whether white, black, and Latino PWID lived in different risk environments. We calculated the percent difference in means for each feature across pairs of racial/ethnic groups:
and classified differences of ≥20% as “substantively significant.” Consistent with guidelines to measure disparities using the group with the “more favorable” status (Keppel, Pamuk et al. 2005), our “reference group” (i.e., Group A) was whites for black/white and Latino/white comparisons. We had no a priori expectations about whether black or Latino PWID would live in “more favorable” areas, and so used the largest group (Black PWID) as the reference for black/Latino comparisons (Keppel, Pamuk et al. 2005). As a form of sensitivity analysis, we used the same methods to compare medians across racial/ethnic groups.
We also determined whether there were racial/ethnic differences in exposure to the combination of two features of the risk environment known to be broadly harmful to health: MSA-level black isolation and ZIP-level poverty (Waitzman and Smith 1998, Williams and Collins 2001). Specifically, we used established cutpoints to identify MSAs that were hypersegregated (black isolation index >70) and ZIPs that were sites of concentrated poverty (poverty rates>20%), and calculated and compared the percentages of white, black, and Latino PWID living in these areas.
Ethics
The Emory University Institutional Review Board approved study protocols. Additionally, all state and local jurisdictions participating in NHBS obtained human subject protections approval before conducting the 2009 NHBS survey among PWID. CDC approved NHBS activities and this study protocol.
Results
The 9,170 PWID in the analytic sample lived in 15 states, 19 MSAs, 51 counties, and 969 ZIP codes. On average there were 611.33 participants (SD=308.13) living in each state; 482.63 participants (SD=93.84) in each MSA; 179.80 participants (SD=227.23) in each county, and 9.47 participants (SD=20.05) in each ZIP code area (Table 2). Participants had lived in the MSA where they were sampled for an average of 31.69 years (SD=19.44). Over half (51.79%) of the participants were black; 30.24% were white; and 17.97% were Latino. Slightly more than a quarter (28.40%) were female and the average age was 45.76 (SD=10.55). Most participants were impoverished and 39.80% were currently homeless. Participants had injected drugs for an average of 23.27 years (SD=12.98); primarily injected heroin; and most injected more than once a day. HIV serostatus varied by race/ethnicity, with 10.70% of black PWID, 7.60% of Latino PWID, and 6.24% of white PWID testing positive.
Table 2.
Characteristics of the sample of people who inject drugs (PWID), drawn from the 2009 Centers for Disease Control and Prevention’s National HIV Behavior Surveillance
| Characteristic | No. (%) or mean (SD) N=9170 |
|---|---|
|
| |
| Age (yrs) | 45.76 (10.55) |
|
| |
| Sex | |
| Male | 6566 (71.60%) |
| Female | 2604 (28.40%) |
|
| |
| Race/ethnicity | |
| Non-Hispanic Black/African-American | 4749 (51.79%) |
| Non-Hispanic White | 2773 (30.24%) |
| Latino/Hispanic | 1648 (17.97%) |
|
| |
| Annual household income (USD) | |
| ≤$4,999 | 3434 (37.64%) |
| $5,000 – $9,999 | 2130 (23.35%) |
| $10,000 – $14,999 | 1423 (15.60%) |
| $15,000 – $19,999 | 676 (7.41%) |
| ≥$20,000 | 1461 (16.01%) |
|
| |
| High-school graduate/General equivalency diploma | 6101 (66.54%) |
|
| |
| Employed full-time | 402 (4.38%) |
|
| |
| Currently homeless | 3649 (39.80%) |
|
| |
| Drug primarily injected | |
| Heroin | 5562 (60.79%) |
| Cocaine | 442 (4.83%) |
| Speedball | 599 (6.55%) |
| Combination of heroin, cocaine, speedball | 1547 (16.91%) |
| Other | 999 (10.92%) |
|
| |
| Injection Frequency | |
| >1/day | 5612 (61.33%) |
| 1/day | 1186 (12.96%) |
| >1/week | 1396 (15.26%) |
| 1/week | 258 (2.82%) |
| Less than weekly | 698 (7.63%) |
|
| |
| Number of years since first injection | 23.27 (12.98) |
|
| |
| Tested positive for HIV | |
| Overall | 8.79% (801) |
| Black PWID | 10.70% (504) |
| Latino PWID | 7.60% (125) |
| White PWID | 6.24% (172) |
|
| |
| Geographic region | |
| Northeast | 2165 (23.61%) |
| South | 3678 (40.11%) |
| Midwest | 949 (10.35%) |
| West | 2378 (25.93%) |
|
| |
| Number of participants in each… | |
| State | 611.33 (308.13) |
| Metropolitan statistical area (MSA) | 482.63 (93.84) |
| County | 179.80 (227.23) |
| ZIP code area | 9.47 (20.05) |
|
| |
| Number of years living in the MSA | |
| Overall | 31.69 (19.44) |
| Black PWID | 39.98 (17.21) |
| Latino PWID | 25.99 (17.85) |
| White PWID | 20.88 (17.32) |
|
| |
| Number (%) of MSAs (N=19) with no participants who are… | |
| White | 0 (0%) |
| Black | 0 (0%) |
| Latino | 1 (5.26%) |
|
| |
| Number (%) of counties (N=51) with no participants who are… | |
| White | 72 (15.69%) |
| Black | 77 (25.49%) |
| Latino | 81 (33.33%) |
|
| |
| Number (%) of ZIP codes (N=969) with no participants who are… | |
| White | 374 (38.60%) |
| Black | 429 (44.27%) |
| Latino | 554 (57.17%) |
In the text that follows, we limit the discussion to features of the risk environment that met the 20% cutpoint – that is, where racial/ethnic differences in mean exposure to the feature were >20%.
Features of the Social Environment
On average, black and Latino PWID lived in MSAs that were more segregated than white PWID (Table 3). On average, black PWID lived in MSAs with a black isolation index value of 43.97 and Latino PWID lived in MSAs with Latino isolation index values of 40.31, values indicating moderate segregation (Biello, Kershaw et al. 2012). White PWID, in contrast, lived in MSAs with lower black and Latino isolation index values (means of 32.51 and 28.15, respectively). Relatedly, PWID lived in ZIP codes where the plurality of their neighbors shared their race/ethnicity. White and Latino PWID lived in ZIP codes where, on average, approximately 43% of residents were of their same racial/ethnic group; black PWID lived in ZIP codes where 56.58% (SD=30.00) of residents were black.
Table 3.
Characteristics of the geographic areas where a sample of people who inject drugs live (N=9170), and racial/ethnic differences in exposure to these characteristics
| Type of influence and geographic scale | White | Black | Latino | % difference10 | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Mean or % | SD or N | Mean or % | SD or N | Mean or % | SD or N | White vs. Black | White vs. Latino | Black vs Latino | |
|
| |||||||||
| Social | |||||||||
|
| |||||||||
| Male:female sex ratios | |||||||||
| ZIP | 1.12 | 0.39 | 1 | 0.26 | 1.05 | 0.24 | 11 | 6 | −5 |
| County | 0.97 | 0.06 | 0.95 | 0.05 | 0.96 | 0.06 | 2 | 1 | −1 |
| MSA | 0.97 | 0.04 | 0.96 | 0.03 | 0.96 | 0.03 | 1 | 1 | 0 |
|
| |||||||||
| Racial/ethnic composition (ZIP) | |||||||||
| % white | 43.62 | 23.84 | 19.05 | 19.26 | 25.18 | 22.92 | 56* | 42* | −32* |
| % black | 20.52 | 21.64 | 56.58 | 30 | 22.74 | 21.7 | −18* | −11 | 60* |
| % Latino | 22.71 | 19.93 | 17.98 | 20.44 | 43.12 | 24.79 | 21* | −90* | −140* |
|
| |||||||||
| Violent crime rate (per 1000) | |||||||||
| County | 7.24 | 3.03 | 8.99 | 3.49 | 6.91 | 2.14 | −25* | 5 | 24* |
| MSA | 5.11 | 1.48 | 5.87 | 2.29 | 5.34 | 1.37 | −15 | −5 | 9 |
|
| |||||||||
| Residential isolation (MSA) | |||||||||
| Black | 32.51 | 19.94 | 43.97 | 18.39 | 36.03 | 18.58 | −35* | −11 | 18 |
| Latino | 28.15 | 16.33 | 28.7 | 14.6 | 40.31 | 14.12 | −2 | −43* | −40* |
|
| |||||||||
| Economic | |||||||||
|
| |||||||||
| Median Income (US $) | |||||||||
| ZIP | 46734.67 | 19896.94 | 37197.47 | 15835.05 | 40707.51 | 16413.61 | 20* | 13 | −9 |
| County | 56025.08 | 13404.93 | 52519.91 | 12016.89 | 52490.86 | 10726.97 | 6 | 6 | 0 |
| MSA | 67635.60 | 12038.13 | 65912.22 | 15291.89 | 65080.42 | 11522.28 | 3 | 4 | 1 |
|
| |||||||||
| Poverty Rate (%) | |||||||||
| ZIP | 23.24 | 11.26 | 29 | 9.93 | 26.54 | 10.9 | −25* | −14 | 9 |
| County | 17 | 5.29 | 18.26 | 4.45 | 17.82 | 4.69 | −7 | −5 | 2 |
| MSA | 12.92 | 2.92 | 13.4 | 4.11 | 14.05 | 2.8 | −4 | −8 | −5 |
|
| |||||||||
| Unemployment (%) | |||||||||
| ZIP | 10.38 | 4.56 | 15.1 | 6.4 | 12.16 | 4.4 | −45* | −17 | 19 |
| County | 9.4 | 2.07 | 10.47 | 2.73 | 9.99 | 1.64 | −11 | −6 | 6 |
| MSA | 8.41 | 1.28 | 8.93 | 2.78 | 8.97 | 0.9 | −6 | −7 | 0 |
|
| |||||||||
| No high-school diploma or general equivalency diploma (%) | |||||||||
| ZIP | 19.35 | 11.49 | 23.77 | 10.5 | 27.75 | 13.37 | −23* | −43* | −17 |
| County | 16.18 | 4.84 | 17.41 | 4.49 | 19.39 | 5.08 | −8 | −20* | −11 |
| MSA | 13.83 | 4.24 | 14.71 | 3.72 | 16.39 | 4.65 | −6 | −19 | −11 |
|
| |||||||||
| Gini coefficient of Income Inequality | 0.47 | 0.02 | 0.47 | 0.02 | 0.48 | 0.02 | 1 | −2 | −3 |
|
| |||||||||
| Health and law enforcement interventions | |||||||||
|
| |||||||||
| Spatial density of HIV testing sites per sq mile (ZIP) | 6.68 | 14.13 | 8.93 | 15.35 | 6.92 | 12.46 | −34* | −4 | 23* |
|
| |||||||||
| Spatial access to substance abuse treatment programs (ZIP) | 2.45 | 2.74 | 1.59 | 1.95 | 2.63 | 3.08 | 36* | −6 | −66* |
|
| |||||||||
| Spatial access to MMTPs | 0.41 | 0.75 | 0.29 | 0.54 | 0.47 | 1.00 | 30* | −14 | −63* |
|
| |||||||||
| Spatial access to SEPs (ZIP) | 0.18 | 0.32 | 0.16 | 0.36 | 0.15 | 0.24 | 11 | 20* | 10 |
|
| |||||||||
| Percent of residents living in a medically underserved area (County) | 15.14 | 24.39 | 19 | 22.92 | 12.19 | 13.06 | −26* | 19 | 36* |
|
| |||||||||
| Percent of residents without health insurance (County) | 21.48 | 8.61 | 24.16 | 8.98 | 24.74 | 8.46 | −12 | −15 | −2 |
|
| |||||||||
| Per capita expenditures on health (USD; MSA) | 172.00 | 175.00 | 135.00 | 140.00 | 150.00 | 147.00 | 22* | 13 | −11 |
|
| |||||||||
| HIV prevalence among PWID in 2002, per 1000 PWID | 8.08 | 5.85 | 9.21 | 5.19 | 11.33 | 7.80 | −14 | −40* | −23* |
|
| |||||||||
| Arrest rate for hard drug possession, per 1000 | |||||||||
| County | 5.15 | 4.42 | 6.24 | 6.65 | 5.72 | 2.19 | −21* | −11 | 8 |
| MSA | 3.77 | 1.98 | 3.86 | 2.07 | 4.62 | 1.79 | −2 | −23* | −20* |
|
| |||||||||
| Arrest rate for possession of any drug, per 1000 | |||||||||
| County | 9.27 | 7.46 | 11.30 | 10.54 | 10.92 | 5.22 | −22* | −18 | 3 |
| MSA | 7.2 | 3.84 | 7.81 | 3.53 | 9.19 | 4.12 | −8 | −28* | −18 |
|
| |||||||||
| Jail incarceration rate, per 1000 (MSA) | |||||||||
| Overall | 0.33 | 0.16 | 0.33 | 0.17 | 0.29 | 0.11 | 0 | 12 | 12 |
| Black | 1.14 | 0.39 | 0.9 | 0.45 | 0.98 | 0.33 | 21* | 14 | −9 |
| White | 0.18 | 0.07 | 0.19 | 0.09 | 0.15 | 0.07 | −6 | 17 | 21* |
| Latino | 0.4 | 0.28 | 0.32 | 0.24 | 0.35 | 0.25 | 20* | 13 | −9 |
|
| |||||||||
| Per capita expenditures on police (USD; MSA) | 312.16 | 74.7 | 305.33 | 66.51 | 347.27 | 67.52 | 2 | −11 | −14 |
|
| |||||||||
| Per capita expenditures on corrections (USD; MSA) | 92.00 | 43.00 | 77.00 | 42.00 | 87.00 | 35.00 | 16 | 5 | −13 |
|
| |||||||||
| Law permits purchase of a syringe without a prescription (State) | 75.3% | 2088 | 45.3% | 2151 | 66.8% | 1101 | 40* | 11 | −47* |
|
| |||||||||
| Law permits possession of a syringe without a prescription (State) | 72.6% | 2013 | 42.3% | 2008 | 76.2% | 1256 | 42* | −5 | −80* |
|
| |||||||||
| Law permits SEPs to operate (State) | 55.5% | 1539 | 35.0% | 1662 | 57.9% | 954 | 37* | −4 | −65* |
|
| |||||||||
| Physical | |||||||||
|
| |||||||||
| Density of abandoned building per sq mile (ZIP) | |||||||||
| Commercial | 118.27 | 246.15 | 56.95 | 109.08 | 76.88 | 156.45 | 52* | 35* | −35* |
| Residential | 83.20 | 106.85 | 175.92 | 207.00 | 93.04 | 108.06 | −111* | −12 | 47* |
| Total | 201.47 | 259.61 | 232.86 | 233.56 | 169.92 | 187.05 | −16 | 16 | 27* |
|
| |||||||||
| Density of businesses licensed to sell alcohol for off-premises consumption, per sq mile (ZIP) | 16.93 | 26.88 | 8.55 | 11.02 | 19.52 | 26.98 | 50* | −15 | −128* |
While there were no substantively significant racial/ethnic differences in mean exposure to MSA-level violent crime rates, on average black PWID lived in counties that had higher rates of violent crime than white or Latino PWID (means of 8.99/, 7.24/, and. 6.91/1000, respectively).
Racial/ethnic differences in mean sex ratios did not cross the threshold for substantive significance, regardless of geographic scale. Black and Latino PWID, however, lived in ZIP codes with equitable sex ratios (commonly defined as ranging from 0.95–1.05) while white PWID lived in ZIP codes where there were more men than women (mean=1.12; SD=0.39).
Features of the Economic Environment
There were marked black/white differences in economic conditions at the ZIP code level. While both black and white PWID lived in ZIP codes that, on average, met the definition of a federal poverty area (i.e., a poverty rate ≥20%), white PWID lived in ZIP codes where the poverty rate was lower than black PWID (means of 23.24% vs. 29.00%, respectively). A similar pattern was evident for median income and the percentage of adults who had dropped out of high-school, and was particularly stark for the percentage of adults in the labor force who were unemployed: on average, white PWID lived in ZIP codes where the percentage of unemployed adults was about half that of the ZIP codes where black PWID lived.
Latino/white differences in features of the economic environment were evident for just one measure: educational attainment. On average, Latino PWID lived in ZIP codes and counties with higher percentages of adults who had not graduated from high school or obtained a GED. There were no Latino/black differences in economic environments.
Features of the Healthcare Service and Law Enforcement Environment
Significant racial/ethnic differences existed in all but one measure of the healthcare service environment, though the nature of these differences depended on service type. Black PWID lived in ZIP codes that had, on average, higher spatial densities of HIV testing sites than white or Latino PWID (means of 8.93 vs. 6.68 sites/square mile, and of 8.93 vs. 6.92 sites/square mile, respectively). In contrast, white and Latino PWID tended to live in ZIP codes that had greater spatial access to MMTPs and to other forms of substance abuse treatment. On average, white and black PWID had similar spatial access to SEPs, and white PWID had better spatial access to SEPs than Latino PWID.
On average, black, Latino, and white PWID lived in counties with similar proportions of residents who lacked health insurance. Black PWID, however, tended to live in counties with higher percentages of residents in medically underserved areas than white or Latino PWID (means of 19.00%, 15.14%, and 12.19%, respectively). Notably, Latino PWID lived in MSAs with higher HIV prevalences than both black and white PWID (means of 11.33%, 9.21%, and 8.08%, respectively).
On average, black and Latino PWID lived in geographic areas with higher drug-related arrest rates than white PWID, though the racialization of this feature was evident at different geographic scales. Black PWID lived in counties with higher mean drug-related arrest rates than white PWID. Latino PWID lived in MSAs that had higher mean drug-related arrest rates than white PWID (and than black PWID).
Compared to black PWID, white and Latino PWID were more likely to live in states where laws facilitated access to sterile syringes. While 35% of black PWID lived in states that permitted SEPs to operate, 56–58% of white and Latino PWID lived in such states. The majority (2/3 to 3/4) of white and Latino PWID lived in states that allowed people to purchase or possess a syringe without a prescription, compared to roughly half of black PWID.
On average, white PWID lived in MSAs that spent more dollars per capita on public health activities. No racial/ethnic differences were detected in MSA-level per capita expenditures on police departments or corrections.
Features of the Physical Environment
On average, black PWID lived in ZIP codes with substantially higher densities of abandoned residences (mean=175.92 abandoned residences/square mile; SD=207.00) than white or Latino PWID (means of 83.20 and 93.04/square mile, respectively). White PWID, however, had the greatest exposure to abandoned commercial properties (mean=118.27/square mile; SD=246.15), followed by Latino PWID (mean=76.88/square mile; SD=156.45). White and Latino PWID also tended to live in ZIP codes with higher spatial densities of businesses licensed to sell alcohol for off-premises consumption (16.93 and 19.52 of these businesses per square mile, respectively) than black PWID (8.55/square mile; SD=11.02).
In our exploration of exposure to the combination of hypersegregated MSAs and ZIPs with concentrated poverty, we found that 0.76% of white PWID, 0% of Latino PWID, and 7.4% of black PWID lived in such areas.
We also compared median values of each feature across racial/ethnic groups of PWID (data available upon request). Overarching conclusions were similar across the two measures of central tendency, though comparisons of medians revealed more differences between Latino PWID and PWID of other races/ethnicities. For example, when medians were compared, Latino PWID lived in MSAs with more per capita investment in health and in corrections than black PWID, and Latino PWID lived in ZIP codes with higher median incomes than black PWID and with better spatial access to HIV testing services and to MMTPs than white PWID.
Discussion
This analysis of 9170 PWID living in 19 MSAs reveals the extent to which risk environments in the US are “racialized.” Risk environments varied by race/ethnicity, though the extent and nature of this racialization depended on the type of influence, geographic scale, and the racial/ethnic groups compared. Given the extensive literature linking features of the risk environment studied here to vulnerability to HIV and to HIV disease progression among PWID (Friedman, Perlis et al. 2001, Rhodes, Singer et al. 2005, Friedman, Cooper et al. 2006, Degenhardt, Mathers et al. 2010, Strathdee, Hallett et al. 2010, Cooper, Des Jarlais et al. 2011, Cooper, Des Jarlais et al. 2012, Milloy, Marshall et al. 2012), these findings have implications for the substance and methods of future research on disparities in HIV-related outcomes among PWID.
Black PWID lived in MSAs with moderately high levels of black isolation, and the nature and geographic scale of black/white differences in risk environments found here are broadly consistent with patterns of racial/ethnic segregation in the US (Massey and Denton 1993, Logan and Stults 2011). In the general population, discriminatory processes (e.g., denying mortgages to non-Whites) sort black and white households within MSAs into separate neighborhoods (Massey and Denton 1993, Dawkins 2004). Predominately black neighborhoods tend to garner less investment and services and more police attention than predominately white neighborhoods (Massey and Denton 1993, Williams and Collins 2001, Cooper, Wypij et al. 2005, Cooper, Bossak et al. 2009, Cooper, Des Jarlais et al. 2012). The present analysis revealed a parallel cross-sectional pattern in features of the risk environment among PWID. Almost universally across measures, black PWID in the 2009 NHBS sample were more likely than white PWID to live in environments that past research indicates are associated with vulnerability to HIV and to poorer outcomes among people living with HIV; these differences were most consistently evident at the level of ZIP codes (crudely analogous to neighborhoods in this analysis), though they were also evident at other scales. Black PWID lived in more socially and economically distressed areas; had poorer spatial access to substance abuse treatment; experienced greater exposure to drug-related law enforcement activities; and were isolated in local environments that were not racially or ethnically diverse. Black PWID were also more likely than white (and Latino) PWID to experience the combination of hypersegregation and concentrated poverty. Analyses revealed a more complex pattern of black/white differences in PWID physical environments, with black PWID experiencing greater exposure to abandoned homes and white PWID experiencing greater exposure to abandoned businesses and to businesses licensed to sell alcohol for off-premises consumption. Possibly, black PWID tended to live in ZIP codes with smaller commercial areas and thus fewer businesses that could be abandoned or licensed to sell alcohol.
When coupled with past research, these findings allow us to conceptualize a possible pathway through which racial/ethnic residential segregation may generate a “dual vulnerability” to HIV infection and HIV-related morbidity and mortality among black residents. Our past research suggests that the prevalence of injection drug use itself is higher among black adults living in MSAs that have higher levels of black isolation (Cooper, Friedman et al. 2007). One interpretation of the present findings is that, within these segregated MSAs, black PWID may live in ZIP codes and counties that have social, economic, and healthcare/law enforcement environments that may create vulnerability to HIV transmission and to HIV-related morbidity and mortality among HIV-positive PWID. One finding about the social environment may be particularly important to conceptualizing and analyzing the mechanisms through which segregation may amplify HIV incidence among black PWID: on average in this sample black PWID lived in ZIP codes where 56% of other residents were also black. While predominately black neighborhoods can foster social support and resilience to discrimination (Kramer and Hogue 2009), they may also elevate HIV transmission by generating racially/ethnically assortative injecting and sexual networks, a possibility supported by sociological research on the influence of local racial/ethnic composition on peer networks (Hallinan 1982, Quillian and Campbell 2003). Given the high prevalence of HIV among black PWID (Laffoon, Satcher Johnson et al. 2011), racially/ethnically assortative risk networks would create vulnerability to higher levels of HIV transmission among black PWID (Kottiri, Friedman et al. 2002). Integrating the present findings with past research allows one to develop and analyze hypotheses about segregation and HIV-related outcomes among PWID that is plausible and critical, though largely untested using cross-sectional or longitudinal designs.
Two findings about black/white differences in risk environments merit further discussion. First, while black PWID had better spatial access to HIV testing than white PWID and comparable access to SEPs, they had worse access to substance abuse treatment. US public health systems have implemented initiatives to increase HIV testing among black adults (e.g., Centers for Disease Control and Prevention 2013). Black PWIDs’ relatively high spatial access to testing sites may reflect the success of these initiatives. Our findings suggest that similar initiatives are needed to increase spatial access to substance abuse treatment among black PWID. As Semaan and colleagues have noted (Semaan, Des Jarlais et al. 2011), providing access to substance abuse treatment respects PWID human rights and is an evidence-based way to reduce HIV infection.
Second, black PWID tended to live in states with laws that did not facilitate access to sterile syringes (i.e., laws permitting SEPs and purchase and possession of syringes without a prescription). Laws restricting syringe access are associated with higher HIV prevalence among PWID (Friedman, Perlis et al. 2001), and many states have altered these laws to facilitate sterile syringe access in an effort to prevent HIV transmission (Burris, Anderson et al. 2010). The specific pattern of these laws found in this analysis may reflect the tendency in the US to embrace a law and order approach to substance misuse where people who misuse substances are more likely to be thought of as black, and a public health approach where people who misuse substances are believed to be white (Courtwright 2001, Steiner and Argothy 2001, Zerai and Banks 2002, Cooper 2004, Mauer 2009, Alexander 2010, Semaan, Des Jarlais et al. 2011). Regardless of their origins, black PWID’s greater exposure to laws limiting sterile syringe access may exacerbate racial/ethnic disparities in HIV prevalence.
A different picture emerged when we compared the risk environments where Latino and white PWID lived. Overall, for most features studied, Latino PWID lived in ZIP codes with similar risk environments to white PWID. For example, with the exception of educational attainment, there were no Latino/white differences in economic indicators. Likewise, with the exception of SEPs, Latino and white PWID had similar spatial access to healthcare services, and Latino PWID lived in counties where fewer residents were in medically underserved areas. Findings about the healthcare service environment are corroborated by a Brookings Institute study of three MSAs, which found that Latinos living in high poverty urban areas had high spatial access to health and social services (Allard 2004). More Latino/white differences might have been observed had we explored differences by Latino subgroup. In the general population, for example, Latinos of Puerto Rican descent experience higher levels of segregation than other Latinos (Massey and Bitterman 1985). These subgroup differences in risk environments may have implications for HIV Puerto Rican drug users have higher HIV–prevalence than other Latino drug users (Montoya, Bell et al. 1999, Deren, Gelpí-Acosta et al. 2014) –and we could not explore them here.
Perhaps the most striking finding from comparisons of black and Latino PWID risk environments was that Latino PWID access to almost all healthcare services was greater than that of black PWID. Both groups lived in MSAs in which their racial/ethnic group was isolated. Our findings may thus testify to a fundamental difference in Latino and black isolation. Latino isolation can indicate Latino enclaves, which may provide social resources that promote resilience (Ostir, Eschbach et al. 2003, Patel, Eschbach et al. 2003); similar to Allard (2004), our findings suggest that these resources include healthcare facilities. As noted, black isolation in contrast typically is associated with fewer resources.
These findings may have methodological implications for future research on risk environments and disparities among PWID. None of the quantitative methods that are widely applied to investigate the relationships of features of the risk environment to HIV-related outcomes (e.g., ordinary-least squares regression, logistic regression, multilevel models) are able to capture the extent to which exposure to these features is racialized. Regressions ignore variations in exposure prevalence across populations, and our results reveal considerable variations in exposure to key features of the risk environment across racial/ethnic groups. Racial/ethnic-specific population attributable risk percents (PAR%s), however, synthesize information about magnitude of the relationship between an exposure and an outcome (generated by regressions) with information about exposure prevalence (Hennekens and Buring 1987). By synthesizing these two parameters, the PAR% captures “…the proportion of disease in the study population that is attributable to the exposure, and thus could be eliminated if the exposure were eliminated” (Hennekens and Buring 1987, p. 92). In light of the present findings, we recommend that future research calculate racial/ethnic-specific PAR%s to provide a more comprehensive and accurate picture of the role that specific features of PWID risk environments play in generating racial/ethnic disparities in HIV-related outcomes. PAR%s assume a causal relationship between exposures and outcomes and are strongest when generated using longitudinal data (Hennekens and Buring 1987); given that such relationships might not have been established, perhaps one could call these PAR%’s “exploratory PAR%s” and note restrictions on causal inference.
We urge others working outside the US to explore the extent to which the construct “racialized risk environment” is relevant to PWID living in other countries. As noted earlier, a recent international meta-analysis of HIV prevalence among racial/ethnic minority PWID versus racial/ethnic majority PWID found substantial disparities in many countries (Des Jarlais, Cooper et al. 2012). Large disparities were noted in Canada (First Nations minority group), China (Uighur and various “hill tribes” as minority groups), and in Eastern and Central Europe (Roma as minority group). For some of these groups–perhaps the Roma are the most well-documented example (Greenberg 2010)–vulnerability to HIV may be elevated by systematic differences in exposure to high-risk environments that perpetuate broader systems of social inequality.
Limitations and Strengths
These findings must be interpreted in light of several limitations. NHBS intentionally sampled MSAs with the highest burdens of AIDS; our findings may thus not be generalizable to MSAs with lower AIDS prevalences or to rural areas. Additionally, and as is the case with most studies of PWID, the NHBS sample may not reflect the underlying population of PWID. While characteristics of the true underlying populations are unknown, RDS has been shown to produce samples which differ from those obtained with other methods (Robinson, Risser et al. 2006, Kral, Malekinejad et al. 2010).
Our analysis is limited to risk environments surrounding NHBS participants’ homes. PWID, however, may spend many of their waking hours outside the ZIP codes and counties where they live, and may intentionally engage in drug-related activities away from their own neighborhoods. These non-residential activity spaces may substantially impact HIV-related outcomes (Williams and Metzger 2010), and we were unable to describe them.
We used ZIP codes to capture features of the risk environment that were relatively close to where PWID lived. This may have led us to misclassify some PWID’s local exposures: ZIP codes are designed by the US Postal Service to facilitate mail delivery and may not map onto participants’ subjectively defined neighborhoods. This misclassification was likely nondifferential across racial/ethnic groups, and thus rendered local environments more similar than they actually are.
The NHBS sample provided an unprecedented opportunity to document the risk environments of thousands of PWID living in the MSAs hardest hit by the HIV/AIDS epidemic in the US, and allowed us to describe these risk environments at multiple geographic scales simultaneously. Additionally, by integrating data from a range of existing sources we were able to document features of PWID risk environments circa 2009 (the year of NHBS data collection) across racial/ethnic groups more comprehensively than has been done previously.
Conclusions
PWID risk environments in the US appear to be racialized, with black PWID living, on average, in environments that past research has found to be associated with increased vulnerability to adverse HIV-related outcomes. Future longitudinal research should assess the extent to which differential exposure to features of risk environments is associated with disparities in these outcomes among PWID, using appropriate methods.
Highlights.
Racial/ethnic disparities in HIV infection and disease progression are large globally
We develop the concept “racialized risk environments” to explain these disparities
Our analyses find that injectors’ risk environments are deeply racialized in the USA
Acknowledgments
This research was supported by two NIH grants: “Place Characteristics & Disparities in HIV in IDUS: A Multilevel Analysis of NHBS” (DA035101; Cooper, PI) and the Emory Center for AIDS Research (P30 AI050409; Curran, PI). It was also supported by the Centers and Disease Control and Prevention, and the National HIV Behavioral Surveillance Study Group: Atlanta, GA: Jennifer Taussig, Shacara Johnson, Jeff Todd;Baltimore, MD: Colin Flynn, Danielle German; Boston, MA: Debbie Isenberg, Maura Driscoll, Elizabeth Hurwitz; Chicago, IL: Nikhil Prachand, Nanette Benbow; Dallas, TX: Sharon Melville, Richard Yeager, Jim Dyer, Alicia Novoa; Denver, CO: Mark Thrun, Alia Al-Tayyib; Detroit, MI: Emily Higgins, Eve Mokotoff, Vivian Griffin; Houston, TX: Aaron Sayegh, Jan Risser, Hafeez Rehman; Los Angeles, CA: Trista Bingham, Ekow Kwa Sey; Miami, FL: Lisa Metsch, David Forrest, Dano Beck, Gabriel Cardenas; Nassau-Suffolk, NY: Chris Nemeth, Lou Smith, Carol-Ann Watson; New Orleans, LA: William T. Robinson, DeAnn Gruber, Narquis Barak; New York City, NY: Alan Neaigus, Samuel Jenness, Travis Wendel, Camila Gelpi-Acosta, Holly Hagan; Newark, NJ: Henry Godette, Barbara Bolden, Sally D’Errico; Philadelphia, PA: Kathleen A. Brady, Althea Kirkland, Mark Shpaner; San Diego, CA: Vanessa Miguelino-Keasling, Al Velasco; San Francisco, CA: H. Fisher Raymond; San Juan, PR: Sandra Miranda De León, Yadira Rolón-Colón; Seattle, WA: Maria Courogen, Hanne Thiede, Richard Burt; St Louis, MO: Michael Herbert, Yelena Friedberg, Dale Wrigley, Jacob Fisher; Washington, DC: Marie Sansone, Tiffany West-Ojo, Manya Magnus, Irene Kuo; Behavioral Surveillance Team. We would like to thank the NHBS participants for making this study possible. We also thank and acknowledge Mr. Scott Burris and Ms. Mona Bennett for their help documenting laws governing syringe access.
1 People who were institutionalized (e.g., incarcerated) were excluded from calculations.
2 When data from the Census Bureau were used to calculate ZIP-code level variables, ZIP code tabulation areas were used instead of ZIP codes. ZIP code tabulation areas are Census approximations of ZIP codes.
3 The isolation index measures “the extent to which minority members are exposed only to one another” within census tracts in an MSA (Massey and Denton, p. 288) and was calculated per Massey and Denton (1988). The isolation index varies from 0 (no isolation) to 100 (complete isolation). A value of 44 for black isolation in an MSA would mean, for example, that there is a probability of 0.44 that the next person that a black resident of the MSA will see in his/her census tract will also be black.
4 The Gini Coefficient ranges from 0.0 (a situation of total equality in which all income generated by a population is equally distributed across all families or households in that population) and 1.0 (a situation of total inequality in which all income generated by a population is held by a single family or household). For more information, see http://www.census.gov/prod/2000pubs/p60-204.pdf. The Gini coefficient generated by the 2010 Decennial Census measures inequality in 2009 income. For this measure alone, we drew MSA-level data directly from the Census Bureau. Note that the Census Bureau’s definitions of MSAs and MSA Divisions included more counties than did those of NHBS. Specifically, the census-delineated MSAs included 20 more counties than the NHBS-delineated MSAs, and the NHBS-delineated MSAs included one county that the census-delineated MSAs excluded.
5 This database contained historical data and so it was possible to capture conditions for 2009.
6 The US Health Resources and Services Administration calculates medically underserved areas using a weighted combination of data on (1) the ratio of primary care physicians to residents; (2) rates of poverty and infant mortality; and the percentage of residents aged ≥65 years. Additional information can be found at http://www.hrsa.gov/shortage/mua/.
7 We included HIV prevalence among PWID in this set of influences because HIV prevalence is often used to locate service sites.
8 MSA definitions differed somewhat between this study and the present one. HIV prevalence estimates published in Tempalski B, Lieb S, Cleland CM, Cooper H, Brady JE, Friedman SR. HIV prevalence rates among injection drug users in 96 large US metropolitan areas, 1992–2002. Journal of Urban Health. 2009;86(1):132–154.
9 “Hard” drugs included opium, cocaine, cocaine derivatives (e.g., crack) and “truly addicting” synthetic or other dangerous non-narcotic drugs
10 As noted in the text, the percent difference in means for each feature across pairs of racial/ethnic groups was calculated as [(Mean for Group A Mean for Group B)/(Mean for Group A)] * 100. Differences of ≥20% were classified as “substantively significant” and are asterisked in this table. Consistent with guidelines to measure disparities using the group with the “more favorable” status, our “reference group” (i.e., Group A) was whites for black/white and Latino/white comparisons. We had no a priori expectations about whether black or Latino PWID would live in “more favorable” areas, and so used the largest group (Black PWID) as the reference for black/Latino comparisons.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alexander M. The New Jim Crow: Mass Incarceration in the Age of Colorblindness. New York: [Jackson, Tenn.], New Press ; Distributed by Perseus Distribution; 2010. [Google Scholar]
- Allard S. Metropolitan Policy Program Survey Series. The Brookings Institution. Washington, DC: The Brookings Institution; 2004. Access to Social Services: The Changing Urban Geography of Poverty and Service Provision. [Google Scholar]
- Bailey TC, Gastrell AC. Interactive Spatial Data Analysis. Essex, England: Longman Scientific and Technical; 1995. [Google Scholar]
- Beardsley K, Wish E, Fitzelle D, O’Grady KE, Arria A. Distance traveled to outpatient drugtreatment and client retention and client retention. Journal of Substance Abuse Treatment. 2003;25(4):279–285. doi: 10.1016/s0740-5472(03)00188-0. [DOI] [PubMed] [Google Scholar]
- Biello KB, Kershaw T, Nelson R, Hogben M, Ickovics J, Niccolai LM. Racial residential segregation and rates of gonorrhea in the United States, 2003–2007. American Journal of Public Health. 2012;102(7):1370–1377. doi: 10.2105/AJPH.2011.300516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich SN, Thorpe RJ, Jr, Sharif-Harris H, Fesahazion R, Laveist TA. Social context explains race disparities in obesity among women. Journal of Epidemiology & Community Health. 2010;64(5):465–469. doi: 10.1136/jech.2009.096297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonilla-Silva E. White Supremacy and Racism in the Post-civil Rights Era. Lynne Rienner Publishers; 2001. [Google Scholar]
- Broz D, Wejnert C, Pham HT, DiNenno E, Heffelfinger JD, Cribbin M, Krishna N, Teshale EH, Paz-Bailey G National HIV Behavioral Surveillance System Study Group. HIV infection and risk, prevention, and testing behaviors among injecting drug users -- National HIV Behavioral Surveillance System, 20 U.S. cities, 2009. MMWR. Surveillance Summaries. 2014;63(6):1–51. [PubMed] [Google Scholar]
- Burris S, Anderson ED, Craigg A, Davis C, Case P. Racial disparities in injection-related HIV: A case study of toxic law. Temple Law Review. 2010 Spring-Summer;(2010):1–51. [Google Scholar]
- Centers for Disease Control and Prevention Racial/ethnic disparities in diagnoses of HIV/AIDS--33 states, 2001–2004. MMWR. 2006;55(5):121–125. [Google Scholar]
- Centers for Disease Control and Prevention. Strategic Plan: The Division of HIV/AIDS Prevention 2011 through 2015. Atlanta, GA: CDC; 2011. [Google Scholar]
- Centers for Disease Control and Prevention. HIV Surveillance Report. Atlanta, GA: CDC; 2012. Diagnoses of HIV infection among adults and adolescents, by sex and transmission category, 2010—46 states and 5 U.S. dependent areas; p. 22. [Google Scholar]
- Centers for Disease Control and Prevention. HIV infection and HIV-associated behaviors among injecting drug users - 20 cities, United States, 2009. MMWR. 2012;61(8):133–138. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Integrated prevention services for HIV infection, viral hepatitis, sexually transmitted diseases, and tuberculosis for persons who use drugs illicitly: summary guidance from CDC and the U.S. Department of Health and Human Services. MMWR. Recommendations & Reports. 2012;61(RR-5):1–40. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Expanded Testing Initiative. 2013 Apr 17; Retrieved Nov 13 2014, 2014, from http://www.cdc.gov/hiv/policies/eti.html.
- Cohen DA, Ghosh-Dastidar B, Scribner R, Miu A, Scott M, Robinson P, Farley TA, Bluthenthal RN, Brown-Taylor D. Alcohol outlets, gonorrhea, and the Los Angeles civil unrest: a longitudinal analysis. Social Science and Medicine. 2006;62:3062–3071. doi: 10.1016/j.socscimed.2005.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H, Bossak B, Tempalski B, Friedman S, Des Jarlais D. Temporal trends in spatial access to pharmacies that sell over-the-counter syringes in New York City health districts: Relationship to local racial/ethnic composition and need. Journal of Urban Health. 2009;86(6):929–945. doi: 10.1007/s11524-009-9399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H, Des Jarlais DC, Ross Z, Tempalski B, Bossak B, Friedman SR. Spatial access to syringe exchange programs and pharmacies selling over-the-counter syringes as predictors of drug injectors’ use of sterile syringes. American Journal of Public Health. 2011;101(6):1118–1125. doi: 10.2105/AJPH.2009.184580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H, Des Jarlais DC, Ross Z, Tempalski B, Bossak B, Friedman SR. Spatial access to sterile syringes and the odds of injecting with an unsterile syringe among injectors: a longitudinal multilevel study. Journal of Urban Health. 2012;89(4):678–696. doi: 10.1007/s11524-012-9673-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H, Friedman SR, Tempalski B, Friedman R. Residential segregation and the prevalence of injection drug use among black adult residents of US metropolitan areas. American Journal of Public Health. 2007;97(2):344–352. doi: 10.2105/AJPH.2005.074542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors’ ability to practice harm reduction: a qualitative study. Social Science & Medicine. 2005;61(3):673–684. doi: 10.1016/j.socscimed.2004.12.030. [DOI] [PubMed] [Google Scholar]
- Cooper HL. Medical theories of opiate addiction’s aetiology and their relationship to addicts’ perceived social position in the United States: an historical analysis. International Journal of Drug Policy. 2004;15(5–6):435–445. [Google Scholar]
- Cooper HL, Bossak BH, Tempalski B, Des Jarlais DC, Friedman SR. Geographic approaches to quantifying the risk environment: Drug-related law enforcement and access to syringe exchange programmes. International Journal of Drug Policy. 2008;20:217–226. doi: 10.1016/j.drugpo.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Des Jarlais DC, Tempalski B, Bossak BH, Ross Z, Friedman SR. Drug-related arrest rates and spatial access to syringe exchange programs in New York City health districts: combined effects on the risk of injection-related infections among injectors. Health & Place. 2012;18(2):218–228. doi: 10.1016/j.healthplace.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Wypij D, Krieger N. Police drug crackdowns and hospitalization rates for illicit-injection-related infections in New York City. International Journal of Drug Policy. 2005;16:150–160. [Google Scholar]
- Courtwright D. Dark Paradise: A History of Opiate Addiction in America. Cambridge, Massachusetts: Harvard University Press; 2001. [Google Scholar]
- Dawkins C. Recent evidence on the continuing causes of Black-White residential segregation. Journal of Urban Affairs. 2004;26(3):379–400. [Google Scholar]
- Degenhardt L, Mathers B, Vickerman P, Rhodes T, Latkin C, Hickman M. Prevention of HIV infection for people who inject drugs: why individual, structural, and combination approaches are needed. Lancet. 2010;376(9737):285–301. doi: 10.1016/S0140-6736(10)60742-8. [DOI] [PubMed] [Google Scholar]
- Deren S, Gelpí-Acosta C, Albizu-García C, González A, Des Jarlais DC, Santiago-Negrón S. Addressing the HIV/AIDS epidemic among Puerto Rican people who inject drugs: The need for a multiregion approach. American Journal of Public Health. 2014;104(11):2030–2036. doi: 10.2105/AJPH.2014.302114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Cooper HLF, Bramson H, Deren S, Hatzakis A, Hagan H. Racial and ethnic disparities and implications for the prevention of HIV among persons who inject drugs. Current Opinion in HIV & AIDS. 2012;7(4):354–361. doi: 10.1097/COH.0b013e328353d990. [DOI] [PubMed] [Google Scholar]
- Do DP, Finch BK, Basurto-Davila R, Bird C, Escarce J, Lurie N. Does place explain racial health disparities? Quantifying the contribution of residential context to the Black/white health gap in the United States. Social Science & Medicine. 2008;67(8):1258–1268. doi: 10.1016/j.socscimed.2008.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortney J, Rost K, Warren J. Comparing alternative methods of measuring geographic access to health services. Health Services & Outcomes Research Methodology. 2000;1(2):173–184. [Google Scholar]
- Frey W. Metropolitan Policy Program at Brookings. Washington, DC: The Brookings Institute; 2011. Melting Pot Cities and Suburbs: Racial and Ethnic Change in Metro America in the 2000s. [Google Scholar]
- Friedman S, Cooper H, Tempalski B, Keem M, Friedman R, Flom P, Des JD. Relationships of deterrence and law enforcement to drug-related harms among drug injectors in US metropolitan areas. AIDS. 2006;20(1):93–99. doi: 10.1097/01.aids.0000196176.65551.a3. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Cooper HLF, Osborne AH. Structural and social contexts of HIV risk among african americans.[Erratum appears in Am J Public Health. 2009 Aug;99(8):1352] American Journal of Public Health. 2009;99(6):1002–1008. doi: 10.2105/AJPH.2008.140327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Perlis T, Des Jarlais DC. Laws prohibiting over-the-counter syringe sales to injection drug users: relations to population density, HIV prevalence, and HIV incidence. American Journal of Public Health. 2001;91(5):791–793. doi: 10.2105/ajph.91.5.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Quimby E, Sufian M, Abdul-Quader A, Des Jarlais DC. Network and sociohistorical approaches to the HIV epidemic among drug injectors. In: Catalan J, Sherr L, Hedge B, editors. The Impact of AIDS: Psychological and Social Aspects of HIV Infection. Amsterdam, The Netherlands: Harwood Academic Publishers; 1997. pp. 89–113. [Google Scholar]
- Friedman SR, Young PA, Snyder FR, Shorty V, Jones A, Estrada AL, Consortium NADR. Racial differences in sexual behaviors related to AIDS in a nineteen city sample of street-recruited drug injectors. AIDS Education and Prevention. 1993;5(3):196–211. [PubMed] [Google Scholar]
- Gallagher K, Sullivan PS, Lansky A, Onorato I. Behavioral surveillance among people at risk for HIV infection in the U.S.: the National HIV Behavioral Surveillance System. Public Health Reports. 2007;122(Suppl 1):32–38. doi: 10.1177/00333549071220S106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg SM, Strathdee SA, Gallardo M, Rhodes T, Wagner KD, Patterson TL. O”. ver here, it’s just drugs, women and all the madness”: The HIV risk environment of clients of female sex workers in Tijuana, Mexico. Soc Sci Med. 2011;72(7):1185–1192. doi: 10.1016/j.socscimed.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg J. Report on Roma education today: From slavery to segregation and beyond. Columbia Law Review. 2010;110(4):919–1001. [Google Scholar]
- Grigoryan A, Hall HI, Durant T, Wei X. Late HIV diagnosis and determinants of progression to AIDS or death after HIV diagnosis among injection drug users, 33 US States, 1996–2004. PLoS ONE [Electronic Resource] 2009;4(2):e4445. doi: 10.1371/journal.pone.0004445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallinan MT. Classroom racial composition and children’s friendships. Social Forces. 1982;61(1):56–72. [Google Scholar]
- Haynes KE, Fotheringhan AS. Gravity and Spatial Interaction Models. Beverly Hills, CA: Sage publications; 1984. [Google Scholar]
- Hennekens CH, Buring JE. Epidemiology in Medicine. Boston, MA: Little, Brown and Company; 1987. [Google Scholar]
- Hwang H-L, Rollow J. Data processing procedures and methodology for estimating trip distances for the 1995 American Travel Survey (ATS)’. Oak Ridge, TN: Oak Ridge National Laboratory; 2000. [Google Scholar]
- Idler E, Kasl SV. Health perceptions and survival: Do global evaluations of health status really predict mortality? Journal of Gerontology: Social Sciences. 1991;46(2):S55–S65. doi: 10.1093/geronj/46.2.s55. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health & Social Behavior. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Idler EL, Russell LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I Epidemiologic Follow-up Study, 1992. First National Health and Nutrition Examination Survey. American Journal of Epidemiology. 2000;152(9):874–883. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- Jacoby I. Geographic distribution of physician manpower: the GMENAC (Graduate Medical Education National Advisory Committee) legacy. Journal of Rural Health. 1991;7(4 Suppl):427–436. [PubMed] [Google Scholar]
- Joassart-Marcelli P. Leveling the playing field? Urban disparities in funding for local parks and recreation in the Los Angeles region. Environment and Planning A. 2010;42(5):1174–1192. [Google Scholar]
- Keppel K, Pamuk E, Lynch J. Vital and Health Statistics. Bethesda, MD: National Center for Health Statistics; 2005. Methodological issues in measuring health disparities; p. 2. [PMC free article] [PubMed] [Google Scholar]
- Kottiri B, Friedman S, Neaigus A, Curtis R, Des Jarlais D. Risk networks and racial/ethnic differences in the prevalence of HIV infection among injection drug users. JAIDS. 2002;30(1):95–104. doi: 10.1097/00042560-200205010-00013. [DOI] [PubMed] [Google Scholar]
- Kral AH, Malekinejad M, Vaudrey J, Martinez AN, Lorvick J, McFarland W, Raymond HF. Comparing respondent-driven sampling and targeted sampling methods of recruiting injection drug users in San Francisco. Journal of Urban Health. 2010;87(5):839–850. doi: 10.1007/s11524-010-9486-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiologic Reviews. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laffoon B, Satcher Johnson A, Cohen S, Hu X, Shouse R. Disparities in diagnoses of HIV infection between Blacks/African Americans and other racial/ethnic populations --- 37 states, 2005--2008. MMWR. 2011;60(4):93–98. [PubMed] [Google Scholar]
- Lansky A, Abdul-Quader AS, Melissa C, Hall T, Finlayson TJ, Garfein RS, Lin LS, Sullivan PS. Developing an HIV behavioral surveillance system for injecting drug users: the National HIV Behavioral Surveillance System. Public Health Reports. 2007;122(Suppl 1):48–55. doi: 10.1177/00333549071220S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansky A, Finlayson T, Johnson C, Holtzman D, Wejnert C, Mitsch A, Gust D, Chen R, Mizuno Y, Crepaz N. Estimating the number of persons who inject drugs in the united states by meta-analysis to calculate national rates of HIV and hepatitis C virus infections. PLoS ONE [Electronic Resource] 2014;9(5):e97596. doi: 10.1371/journal.pone.0097596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laveist T, Pollack K, Thorpe R, Jr, Fesahazion R, Gaskin D. Place, not race: disparities dissipate in southwest Baltimore when blacks and whites live under similar conditions. Health Affairs. 2011;30(10):1880–1887. doi: 10.1377/hlthaff.2011.0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linton SL, Celentano DD, Kirk GD, Mehta SH. The longitudinal association between homelessness, injection drug use, and injection-related risk behavior among persons with a history of injection drug use in Baltimore, MD. Drug Alcohol Depend. 2013;132(3):457–465. doi: 10.1016/j.drugalcdep.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan JR, Stults B. The Persistence of Segregation in the Metropolis: New Findings from the 2010 Census. Providence, Rhode Island: Brown University; 2011. [Google Scholar]
- Luo W, Wang F. Measures of spatial accessibility to health care in a GIS environment: synthesis and a case study in the Chicago region. Environment and Planning B: Planning and Design. 2003;30:865–884. doi: 10.1068/b29120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey D, Denton N. American Apartheid: Segregation and the Making of the Underclass. Cambridge, Massachusetts: Harvard University Press; 1993. [Google Scholar]
- Massey DE, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- Massey DS, Bitterman B. Explaining the paradox of Puerto Rican segregation. Social Forces. 1985;64(2):306–331. [Google Scholar]
- Massey DS, Denton NA. Hypersegregation in U.S. metropolitan areas: black and Hispanic segregation along five dimensions. Demography. 1989;26(3):373–391. [PubMed] [Google Scholar]
- Mauer M. Changing Racial Dynamics of the War on Drugs. Washington, DC: The Sentencing Project; 2009. [Google Scholar]
- McKnight C, Des Jarlais C, Perlis T, Eigo K, Krim M, Auerbach J, Purchase D, Jones T, Garfein RS. Update: Syringe Exchange Programs -- United States, 2002. Morbidity and Mortality Weekly Report. 2005;54(27):673–676. [PubMed] [Google Scholar]
- Milloy MJ, Marshall BD, Kerr T, Buxton J, Rhodes T, Montaner J, Wood E. Social and structural factors associated with HIV disease progression among illicit drug users: a systematic review. AIDS. 2012;26(9):1049–1063. doi: 10.1097/QAD.0b013e32835221cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montoya I, Bell D, Richard A, Carlson J, Trevino R. Estimated HIV risk among Hispanics in a national sample of drug users. J Acquir Immune Defic Syndrome. 1999;21(1):42–50. doi: 10.1097/00126334-199905010-00006. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse of the National Institutes of Health. NIH Health Disparities Strategic Plan, Fiscal Years 2009–2013. National Institute on Drug Abuse; Bethesda, MD: NIH; 2009. [Google Scholar]
- National Minority AIDS Council. African Americans, Health Disparities, and HIV/AIDS: Recommendations for Confronting the Epidemic in Black America. Washington, DC: National Minority AIDS Council; 2006. [Google Scholar]
- Office of Applied Studies in the Substance Abuse and Mental Health Services Administration. National Directory of Drug and Alcohol Abuse Treatment Programs 2010. Bethesda, MD: SAMHSA; 2010. [Google Scholar]
- Office of Disease Prevention and Health Promotion in the U.S. Department of Health and Human Services. Healthy People 2020. Washington, DC: Department of Health and Human Services; 2012. [Google Scholar]
- Office of Management and Budget. Revised Delineations of Metropolitan Statistical Areas, Micropolitan Statistical Areas, and Combined Statistical Areas, and Guidance on Uses of the Delineations of These Areas. Washington, DC: Office of Management and Budget; 2013. [Google Scholar]
- Ostir GV, Eschbach K, Markides KS, Goodwin JS. Neighbourhood composition and depressive symptoms among older Mexican Americans. Journal of Epidemiology & Community Health. 2003;57(12):987–992. doi: 10.1136/jech.57.12.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel KV, Eschbach K, Rudkin LL, Peek MK, Markides KS. Neighborhood context and self-rated health in older Mexican Americans. Annals of Epidemiology. 2003;13(9):620–628. doi: 10.1016/S1047-2797(03)00060-7. [DOI] [PubMed] [Google Scholar]
- Quillian L, Campbell M. Beyond black and white: The present and future of multiracial friendship segregation. American Sociological Review. 2003;68(4):540–566. [Google Scholar]
- Rhodes T. The ‘risk environment’: a framework for understanding and reducing drug-related harm. International Journal of Drug Policy. 2002;13(2):85–94. [Google Scholar]
- Rhodes T. Risk environments and drug harms: A social science for harm reduction approach. International Journal of Drug Policy. 2009;20:193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Mikhailova L, Sarang A, Lowndes C, Rylkov A, Khutorskoy M, Renton A. Situational factors influencing drug injecting, risk reduction and syringe exchange in Togliatti City, Russian Federation: a qualitative study of micro risk environment. Social Science & Medicine. 2003;57(1):39–54. doi: 10.1016/s0277-9536(02)00521-x. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Social Science & Medicine. 2005;61(5):1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- Robinson WT, Risser JM, McGoy S, Becker AB, Rehman H, Jefferson M, Griffin V, Wolverton M, Tortu S. Recruiting injection drug users: a three-site comparison of results and experiences with respondent-driven and targeted sampling procedures. Journal of Urban Health. 2006;83(6 Suppl):i29–38. doi: 10.1007/s11524-006-9100-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuurman N, Berube M, Crooks VA. Measuring potential spatial access to primary health care physicians using a modified gravity model. The Canadian Geographer. 2010;54(1):29–45. [Google Scholar]
- Semaan S, Des Jarlais DC, Malinowska-Sempruch K, Kirby A, Sharpe TT. Human rights and HIV prevention among drug users. In: Beracochea E, Weinstein C, Evans D, editors. Rights-based approaches to public health. New York: Springer Publishing Company; 2011. pp. 210–220. [Google Scholar]
- Steiner BD, Argothy V. White addiction: racial inequality, racial ideology, and the war on drugs. Temple. Political & Civil Rights Law. Review. 2001:443–476. [Google Scholar]
- Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, Hankins CA. HIV and risk environment for injecting drug users: the past, present, and future. Lancet. 2010;376(9737):268–284. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The White House Office of National AIDS Policy. National HIV/AIDS Strategy. Washington, DC: The White House Office of National AIDS Policy; 2010. [Google Scholar]
- U.S. Office of Management and Budget. Provisional guidance on the implementation of the 1997 standards for federal data on race and ethnicity. Washington, DC: Office of Management and Budget; 2000. [Google Scholar]
- Waitzman NJ, Smith KR. Phantom of the area: poverty-area residence and mortality iin the United States. American Journal of Public Health. 1998;88:973–976. doi: 10.2105/ajph.88.6.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F. Quantitative Methods in Applications in GIS. New York: Taylor and Francis; 2006. [Google Scholar]
- Williams C, Eisenberg M, Becher J, Davis-Vogel A, Fiore D, Metzger D. Racial disparities in HIV prevalence and risk behaviors among injection drug users and members of their risk networks. J Acquir Immune Defic Syndr. 2013;63(Suppl 1):S90–94. doi: 10.1097/QAI.0b013e3182921506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams C, Metzger D. Race and distance effects on regular syringe exchange program use and injection risks: A geobehavioral analysis. American Journal of Public Health. 2010;100(6):1068–1074. doi: 10.2105/AJPH.2008.158337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Reports. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerai A, Banks R. Nightmare. United Kingdom: Ashgate; 2002. Dehumanizing Discourse, Anti-Drug Law, and Policy in America: A “Crack Mother’s”. [Google Scholar]