Abstract
The greatest advantages of laparoscopy when compared to open surgery include the faster recovery times, shorter hospital stays, decreased postoperative pain, earlier return to work and resumption of normal daily activity as well as cosmetic benefits. Laparoscopy today is considered the gold standard of care in the treatment of cholecystitis and appendicitis worldwide. Laparoscopy has even been adopted in colorectal surgery with good results. The technological improvements in this surgical field along with the development of modern techniques and the acquisition of specific laparoscopic skills have allowed for its utilization in operations with fully intracorporeal anastomoses. Further progress in laparoscopy has included single-incision laparoscopic surgery and natural orifice trans-luminal endoscopic surgery. Nevertheless, laparoscopy for emergency surgery is still considered challenging and is usually not recommended due to the lack of adequate experience in this area. The technical difficulties of operating in the presence of diffuse peritonitis or large purulent collections and diffuse adhesions are also given as reasons. However, the potential advantages of laparoscopy, both in terms of diagnosis and therapy, are clear. Major advantages may be observed in cases with diffuse peritonitis secondary to perforated peptic ulcers, for example, where laparoscopy allows the confirmation of the diagnosis, the identification of the position of the ulcer and a laparoscopic repair with effective peritoneal washout. Laparoscopy has also revolutionized the approach to complicated diverticulitis even when intestinal perforation is present. Many other emergency conditions can be effectively managed laparoscopically, including trauma in select hemodynamically-stable patients. We have therefore reviewed the most recent scientific literature on advances in laparoscopy for acute care surgery and trauma in order to demonstrate the current indications and outcomes associated with a laparoscopic approach to the treatment of the most common emergency surgical conditions.
Keywords: Laparoscopy, Acute care surgery, Single-incision laparoscopic surgery, Natural orifice trans-luminal endoscopic surgery, Trauma
Core tip: Although laparoscopy today represents the undisputed standard of care for the treatment of acute cholecystitis and appendicitis worldwide, laparoscopy for emergency surgery is still considered challenging and not recommended due to the lack of adequate experience and/or appropriate laparoscopic skills. However, the potential advantages of laparoscopy, both in terms of diagnosis and therapy, are clear. Like complicated appendicitis and cholecystitis, major advantages may be observed in cases with diffuse peritonitis secondary to perforated peptic ulcers, acute diverticulitis and many other often traumatic emergency conditions.
INTRODUCTION
Laparoscopy today is accepted as the gold standard in the treatment of cholecystitis and appendicitis worldwide. Currently, laparoscopy has even been adopted in colorectal surgery with good results. The advantages of laparoscopy include faster recovery, shorter hospital stay, decreased postoperative pain, earlier return to work and resumption of normal daily activity as well as cosmetic benefits[1].
The technological improvements in this field include the development and perfection of laparoscopic instruments, including endo-staplers and harmonic scalpels. The development of modern laparoscopic techniques and the acquisition of these skills by a growing number of surgeons have instilled confidence in the procedure.
Further progress in laparoscopy has been made by single-incision laparoscopic surgery (SILS). Through a single incision, usually transumbilical, a vast array of operations can be performed including cholecystectomies, appendectomies, colorectal resections and minor liver resections (e.g., left liver lobe resections). More recently, an innovative and challenging technique, natural orifice trans-luminal endoscopic surgery (NOTES), has been developed with the intent to greatly improve outcomes in terms of cosmetics, diminished postoperative pain and faster return to normal activity. NOTES consists of performing abdominal interventions by accessing the cavity through natural orifices such as the stomach, rectum, vagina or urinary bladder, thereby achieving truly scarless surgery. For the moment, NOTES remains a surgical procedure performed at only a few centers worldwide on highly selected patients.
Whereas it is used extensively for elective surgery, laparoscopy for emergency surgery is still considered too challenging and is not usually recommended. There are numerous reasons which include technical difficulties associated with diffuse peritonitis, large purulent collections and adhesions. It is also often very difficult to plan a laparoscopic approach for after hours emergency procedures or during a night shift because the procedure is limited by time as well as by the accessibility of equipment and surgical personnel, especially in rural hospitals. Nonetheless, the potential advantages of laparoscopy, both in terms of diagnosis and therapy, for acute abdomen have been highlighted[2].
Laparoscopy can be safely performed for the treatment of acute complicated appendicitis even in the presence of a large purulent abscess or diffuse peritonitis. Gangrenous or perforated cholecystitis can likewise be managed laparoscopically as well.
A perforated peptic ulcer (PPU) is another acute condition in which laparoscopy may serve as a diagnostic tool, permit the direct repair of the defect and allow the subsequent lavage of the peritoneal cavity, providing practical advantages in terms of less postoperative pain, faster recovery and earlier return to work[3].
This minimally-invasive approach becomes very useful in cases of peritoneal carcinomatosis, allowing diagnosis as well as palliative treatment (i.e., loop ileostomy) when appropriate.
Laparoscopy has also revolutionized the approach to complicated diverticulitis, even when intestinal perforation is present. In fact, laparoscopic lavage has recently emerged as an effective alternative for the treatment of perforated diverticula with purulent peritonitis. Furthermore, if a Hartmann’s Procedure is necessary, the sigmoid resection can be safely performed laparoscopically with the end stoma fashioned after the extraction of the specimen.
Finally, the stoma reversal can be performed laparoscopically two months later with a trans-anal stapled colon-rectal anastomosis. After such minimally-invasive procedures, adhesions are usually minimized when compared to an open intervention.
Other conditions can be effectively approached laparoscopically including small-bowel obstruction, especially if due to a single adhesive band, ischemic small-bowel strangulation by volvulus on a single band, large bowel obstruction by colon carcinoma, diffuse peritonitis with or without large intra-abdominal abscess, incisional hernia and many more.
Major contraindications to the use of laparoscopy for emergency surgery are haemodynamic instability caused by severe hemorrhagic or septic shock. Another challenge concerns the use of CO2 to create pneumoperitoneum due to the possible development of respiratory failure with hypercapnia and toxic shock syndrome in older patients with multi-comorbidities[4].
The objective of the present work is to describe state of the art laparoscopic implications for the most common emergency surgical conditions. The most recent scientific literature on the advances in laparoscopy for the treatment of the most critical surgical interventions will be summarized.
APPENDICITIS
Appendicitis is the most common cause of intra-abdominal surgical emergency in the Western world[5]. Clinical diagnosis of appendicitis remains imperfect and negative exploration, especially in females of childbearing age, is still as high as 34 percent[6].
Since its introduction, open appendectomy (OA) has been the gold standard of care for well over a century[7]. Laparoscopic appendectomy (LA) was first described back in 1983[8] and some of its benefits were immediatly apparent: superior visualization of the peritoneal cavity, enabling the diagnosis of alternative diseases in the case of a normal appendix and cosmetic considerations.
LA is now well accepted as the gold standard of care in cases of acute appendicitis[9,10]. Many studies demonstrate LA to be feasible, safe and effective[11-16]. These studies show LA to be superior to OA due to shortened hospital stays, lower complication rates, earlier return to work and resumption of normal activity[17,18].
Nonetheless, uniform usage of LA over OA has not yet been reached. The presumed higher costs for LA are one of its major limitations. Several studies indicate that laparoscopy incurred higher operating room and supply charges owing to the use of more expensive disposable medical devices[19-21]. Expenses do vary widely and can be influenced by both technique and surgical skill.
Operative times are predominantly surgeon-dependent and increases in the learning curve correlate with a reduction in surgical time[22].
Much of the costs for LA result from the routine employment of staplers as well as disposable devices. Although staplers are easy to use, quick and provide a secure closure of the appendicular stump, equally safe and inexpensive options have been described to secure the stump. Endoloops and intracorporeal knotting have been shown to be alternative methods[23]. Loops are not recommended in cases where there is a perforated base or when inflammation occurs on the caecum wall. In such cases a stapler is preferred as the safer method of closure.
Economic analyses have been performed for the use of staplers and other disposable devices as well as for the indirect costs associated with lost productivity during hospitalization and subsequent recuperative periods[14]. Considering these costs, studies indicate LA to be less expensive than OA overall. Even when high costs of Laparoscopic conversions to open procedures are factored into the cost analysis, LA remains the most cost-effective procedure in use today.
Over the last decade, an innovative technique, single incision laparoscopic surgery (SILS), has been developed with the intent to improve cosmesis, postoperative pain and return to normal activity[24,25]. Transumbilical SILS has recently attracted the attention of surgeons worldwide with the innovative possibility of performing virtually scarless surgery[26] (Figures 1 and 2). Several studies and randomized trials have tested and compared single incision laparoscopic appendectomy (SILA) with LA showing similar postoperative results[27,28]. Notwithstanding, the increased costs for SILA compared with LA is still a major disadvantage that limits this technique[29,30]. Moreover, the use of angled instruments and the loss of triangulation between them, due to coaxiality, makes SILS a difficult procedure requiring advanced laparoscopic skills. These factors may be associated with an increased rate of postoperative complications and longer surgical times[30].
Figure 1.
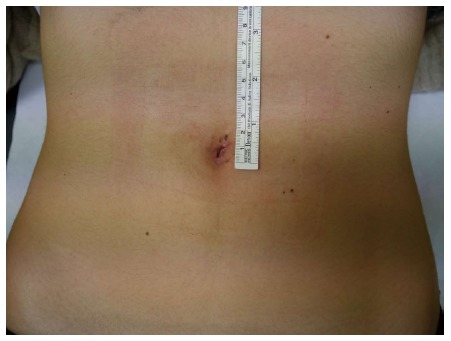
Single-incision laparoscopic surgery appendectomy in a 14 year old female: Umbelical scar after 8 post-operative days. Provided by personal courtesy of Dr. S. Di Saverio, MD, FACS, FRCS.
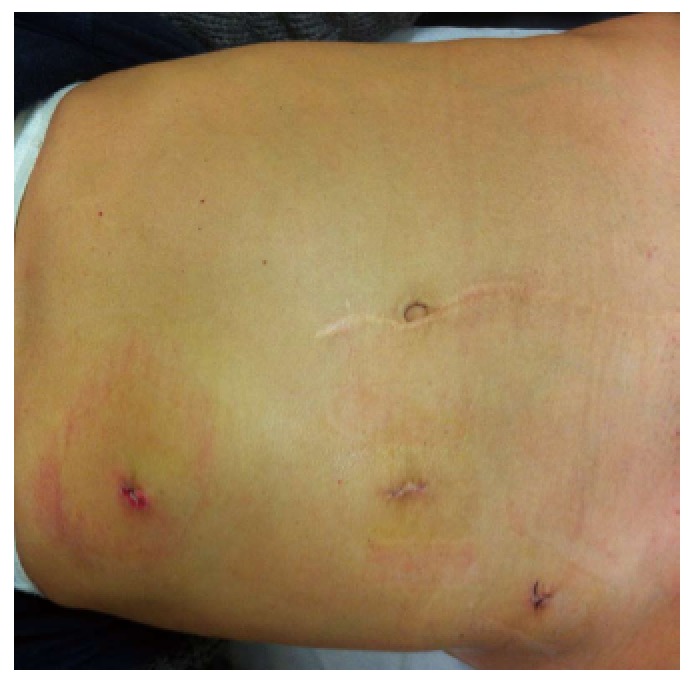
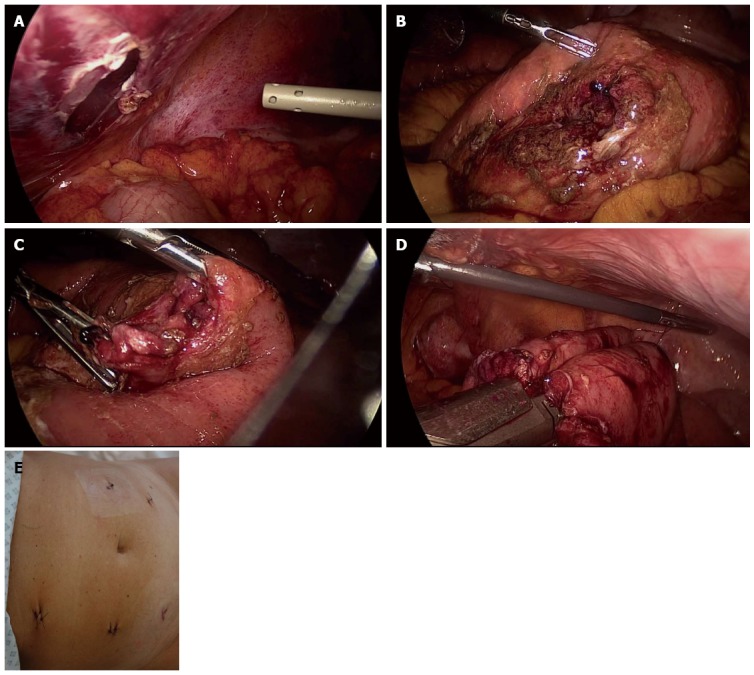
Figure 2.

Single-incision laparoscopic surgery to multiport laparoscopic conversion. Right colectomy for intended appendectomy: functional and aesthetic outcome. The procedure began as an intended single-incision laparoscopic surgery appendectomy. After discovering a wide perforation of the gangrenous cecum, the procedure was converted to a multiport laparoscopic right colectomy. With an umbelical port for the camera, two further trocars were inserted: a 5 mm trocar in the left iliac fossa and a 12 mm trocar in the left flank as an opertive port and for the insertion of the endostapler. Provided by personal courtesy of Dr. S. Di Saverio, MD, FACS, FRCS.
In addition to the cosmetic results related to the reduced number of incisions (and trocars), this has also been thought to decrease postoperative pain and to accelerate postoperative recovery. Nevertheless, the early trials did not achieve consensus on this issue[30-33].
As for the length of hospital stay and return to normal activity, SILA recovery time is nearly equal to LA[27,28] and is, therefore, not a singularly decisive factor in choosing one procedure over the other.
Although the low rate of surgical-site infection has been one of the primary advantages of LA over OA, the use of a single laparoscopic access point surprisingly emerged early-on to potentially increase the risk of postoperative wound infections[34,35]. Interestingly, a large retrospective study found that the wound infection rate became smaller over time, suggesting that the infection rate may depend more on the surgeon’s experience than with the technique[36].
Another matter of debate concerns the use of drainage. The decision to leave a drain at the end of the SILS procedure complicates the advantage of the single umbilical incision.
In conclusion, LA is the procedure of choice for the treatment of acute and complicated appendicitis, wherease SILA should be considered for the minimally-invasive treatment of acute appendicitis in selected cases at centers capable of this technique.
SMALL BOWEL OBSTRUCTION
Abdominal adhesions represent the most common cause of intestinal obstruction, responsible for 60% to 70% of small bowel obstruction (SBO)[37].
Laparotomy is one of the most important causes of adhesions in the abdominal cavity. The incidence of abdominal adhesions after laparotomy has been estimated to be as high as 94%-95%[37]. Nevertheless, open adhesiolysis has also been the primary surgical treatment for adhesive SBO.
Owing to the small working space and the inherent difficulty in localizing the site of the obstruction along with the very high risk of causing injury to the distended bowel, laparoscopic adhesiolysis for SBO has never been considered an appropriate procedural choice for intestinal adhesions in the past.
Laparoscopic adhesiolysis for SBO was first reported by Bastug et al[38] in 1991 for the division of a single adhesive band. However, the safety of laparoscopic surgery in the treatment of adhesive SBO is still unclear because only a few reports show its safety and no randomized controlled trials compare open with laparoscopic adhesiolysis[39].
The potential advantages of laparoscopic surgery for SBO are similar and include decreased length of hospital stay, fewer complications and shorter operative times (Figure 3). Higher rates of reoperation, unrecognized enterotomy, and inability to properly evaluate compromised bowel have all been cited as disadvantages to laparoscopic intervention for SBO[40]. In addition, a higher rate of bowel injury associated with laparoscopy for SBO has been reported[41]. This likely depends on the grade of the adhesions, surgeon experience[42], the use of thermal coagulation for dissection and the impaired tactile feedback during laparoscopic manipulation. Patients with no more than two prior operations, operated on early (24 h after hospitalization vs 48 h) for single band obstruction rather than diffuse adhesions are likely the most suitable for performing laparoscopic adhesiolysis[43]. One study[44] revealed that patients with SBO after only an appendectomy or a cholecystectomy are good candidates to be treated laparoscopically.
Figure 3.
Laparoscopic adhesiolysis for small bowel obstruction following pedriatic surgery with median laparotomy: Functional and aesthetic outcome. The camera was in the Hasson trocar in the paraumbelical port. Two operative 5 mm trocars were placed in the left hypocondrium and in the left iliac fossa respectively. Provided by personal courtesy of Dr. S. Di Saverio, MD, FACS, FRCS.
Therefore, laparoscopic adhesiolysis for SBO is recommended in selected patients with a maximum of two previous laparotomies, especially in cases of appendectomy or cholecystecomy, with a suspected single-band obstruction and after early onset of symptoms. Ultimately, adequate surgeon experience and advanced laparoscopic skills are mandatory to safely perform this practice.
DIVERTICULITIS
Although colonic diverticula affect approximately 60% of people over 80 years old[45], current data reveal that only 4% of them will eventually develop an acute episode of diverticulitis[46].
Nonetheless, acute diverticulitis represents an increasing surgical problem worldwide.
Based on the presence of complications such as abscess, fistula, obstruction or perforation, diverticulitis can be classified as either complicated or uncomplicated. Complicated diverticulitis, demonstrated by CT imaging and graded according to the Hinchey Classification[47], often requires operative or percutaneous intervention.
In the past, emergency surgery for acute diverticulitis was performed in 15% of cases to manage acute diverticulitis complicated by intra-abdominal or pelvic abscess[48]. Today, it is commonly assumed that a small abscess of less than 4 cm without peritonitis (Hinchey stage I) can be managed successfully with broad-spectrum antibiotics, bowel rest and observation only[49]; whereas, in cases of peridiverticular abscess larger than 4 cm (Hinchey stage II), CT-guided percutaneous drainage is recommended[49].
Hinchey stage III and IV diverticulitis, the presence of a large inaccessible abscess as well as the lack of improvement or deterioration within three days of conservative management, are all well accepted indications for emergency operative treatment[49].
The surgical approach for perforated diverticulitis has radically changed over the last few decades.
The Hartmann’s Procedure has been the undisputed primary procedure for perforated diverticulitis during the last century. More recently several studies have compared non-restorative resection with primary anastomosis[50-55]. Interestingly, significant differences have resulted in favour of primary anastomosis in terms of stoma reversal rate and other complications[56]. Furthermore, studies have investigated the role of laparoscopic resection and laparoscopic lavage as an alternative to the standard open procedures for the treatment of complicated diverticulitis[57].
Laparoscopy in perforated diverticulitis can not only confirm the diagnosis, but can also be therapeutic by allowing the lavage of the peritoneal cavity. Clear indications for laparoscopic lavage in the treatment of acute diverticulitis have not yet been reached[57]. Notwithstanding, current data suggest that laparoscopic lavage could potentially become the definitive treatment for perforated diverticulitis in selected cases[57]. Laparoscopic lavage requires careful patient selection and assessment for occult perforations. Also, it is suitable only in cases of purulent peritonitis (Hinchey III). If a perforation is identified, resection with or without primary anastomosis would be required[56].
In 1991 the first laparoscopic sigmoid colectomy for diverticular disease was reported by Jacobs[58]. To date, many studies and a few randomized trials have been published on this subject[57]. Elective laparoscopic resection emerged to be feasible and safe as well as associated with increased operative time with fewer postoperative complications and shorter hospital stay as compared to standard open colectomy[57]. Indications for laparoscopic colectomy remain uncertain and not yet widely accepted for Hinchey stage III or IV[59] (Figures 4 and 5). Laparoscopic colectomy is likely to become adopted as the standard surgical procedure for complicated diverticulitis when surgeons become more confident with the technique.
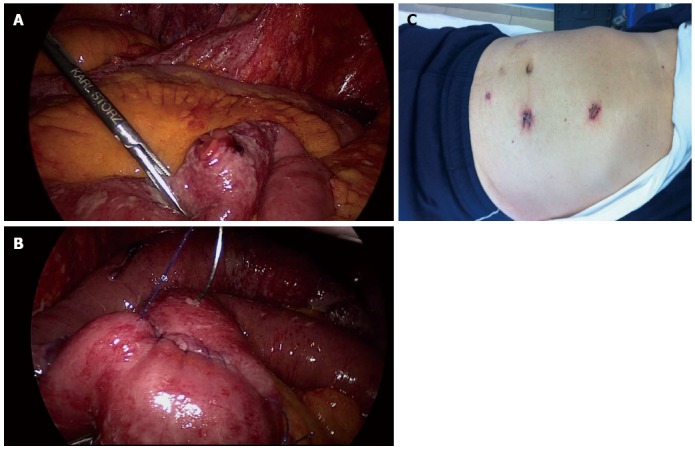
Figure 4.
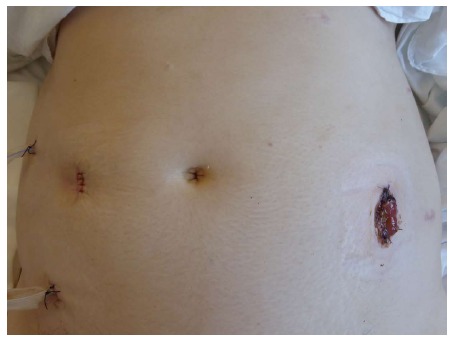
Laparoscopic Hartmann’s procedure for perforated Hinchey III diverticulitis in a 39 years old female: End colostomy and drains. On the right iliac fossa a large 12 mm port was used for introducing the endostapler and for distal colonic resection. On the left flank, a fourth port was inserted for the assistant surgeon. The sigmoid was then extracted from the left flank by enlarging the port to a 4 cm incision. The end colostomy was then fashioned on the left flank using the same incision. Provided by personal courtesy of Dr. S. Di Saverio, MD, FACS, FRCS.
Figure 5.

Resection with primary anastomosis for Hinchey IV diverticulis in a young patient: Functional and aesthetic outcome. A suprapubic 12 mm trocar was used for introducing the endostapler and performing the fully intracorporeal anastomosis. The specimen was then extracted by enlarging the suprapubic incision to a 4 cm minilaparotomy. Provided by personal courtesy of Dr. S. Di Saverio, MD, FACS, FRCS.
ACUTE CHOLECYSTITIS
On average, 36% of cholecystectomies are performed for acute cholecystitis[60]. Cholelithiasis causes 90% of the cases of acute cholecystitis[61]; and the remaining 10% of acalculous cholecystitis[62] is usually due to other secondary conditions such as trauma, burns, recent surgery, multisystem organ failure, parenteral nutrition, AIDS or ischemia[61]. Gallstones are estimated to affect about 10%-15% of Western populations[63-66], of which 1% to 4% will develop acute cholecystitis or symptomatic cholelithiasis every year[67].
The prevalence and the superiority of laparoscopic cholecystectomy (LC) over the standard open procedure for the treatment of acute cholecystitis is well accepted. In the US about 1.5 million cholecystectomies are performed annualy[68], of which 70%-90% are carried out laparoscopically[68,69].
In the past, there were concerns with LC due to the higher morbidity rates in emergency procedures and the higher conversion rate to an open procedure[70]. Severe inflammation and fibrotic adhesions are the main reasons for conversion in early and delayed laparoscopic cholecystectomy respectively[71,72] and are the most important causes associated with bile duct injury[73]. Although retrospective studies reported a larger number of bile duct injuries associated with early laparoscopic surgery[74,75], no significant differences have ever been found in randomized trials[69]. The optimal timing of surgery in cases of acute cholecystitis has always been a topic of debate. Not long ago, patients were managed conservatively for the purpose of cooling down the inflammatory process so that operations could be performed weeks later. Current data suggest that early laparoscopic cholecystectomy for acute cholecystitis is superior to late or delayed laparoscopic cholecystectomy in terms of outcome and costs[68,76]. During the first 72 h surgical dissection may be easiest because of the lack of organized adhesions[77], reducing the risk of bile duct injuries and decreasing the rate of complications.
The concept of early cholecystectomy has now been discussed by some authors in terms of what should be considered the “golden hours”. In fact, although guidelines recommend laparoscopic cholecystectomy within the first 48-72 h after symptom onset[78-80], a recent randomized trial has showed laparoscopic cholecystectomy performed within 24 h of admission to be superior when compared to delayed laparoscopic cholecystectomy[81].
Transumbilical single-incision laparoscopic cholecystectomy (SILC) has recently been introduced with the intent to improve cosmetic results by leaving no visible exterior abdominal scars. Since the surgical evidence is hidden within the umbilicus, SILC subsequently decreases postoperative pain and accelerates postoperative recovery as well. Interestingly however, randomized trials comparing SILC vs LC showed no differences in the Visual Analog Scale pain score or postoperative analgesic administration[82,83]. It is likely that total wound tension may rise non-linearly with increasing incision length[84] and so tension across multiple incisions may be less than the total tension for a single incision of the same total length[84]. Accordingly, using two small trocars should be better than using a single large trocar[82]. In addition, despite the smaller skin incision in SILS, the total size of fascial defects may be equal to the size required for classic laparoscopy.
Even though SILC has been associated with slightly longer surgical times[82,83], mostly due to the advanced laparoscopic skills required to perform it, the procedure may also negatively affect postoperative complication rates. Because of the short follow-up time available, data regarding incisional hernia rates are sparse and more comparative evidence is still needed. Theoretically, the larger fascial incision with SILS would increase the risk of postoperative hernias.
Finally, heterogenity exists among the procedures described as SILC in scientific literature, especially regarding the employment of different multiport devices and instruments.
SILC may be considered as a safe alternative to LC for the treatment of gallstone-related disease in selected uncomplicated patients. However, further study will be required before widespread use of this technique can be advocated.
PPU
Although the incidence of PPU drastically decreased after the identification of Helicobacter pylori as the prime cause with the subsequent introduction of proton pump inhibitor therapy in clinical practice[85,86], the diagnosis of PPU has been increasing over the past decade possibly due to the larger-scale use of nonsteroidal anti-inflammatory drugs[87].
The surgical treatment of PPU consists of the repair of gastric or duodenal defects by direct suturing with or without placement of an omental patch, peritoneal lavage and drainage.
The attempt to laparoscopically repair a PPU was first described at the beginning of the laparoscopic era many years ago[88,89]. The laparoscopic approach to PPU has several advantages including the confirmation of the diagnosis, the subsequent identification of the ulcer and possibly its closure, with lavage of the peritoneal cavity, all without the need for a laparotomy (Figures 6 and 7). Nevertheless, early randomized trials did not find any advantage of laparoscopic PPU repair as compared with the open approach[90].
Figure 6.
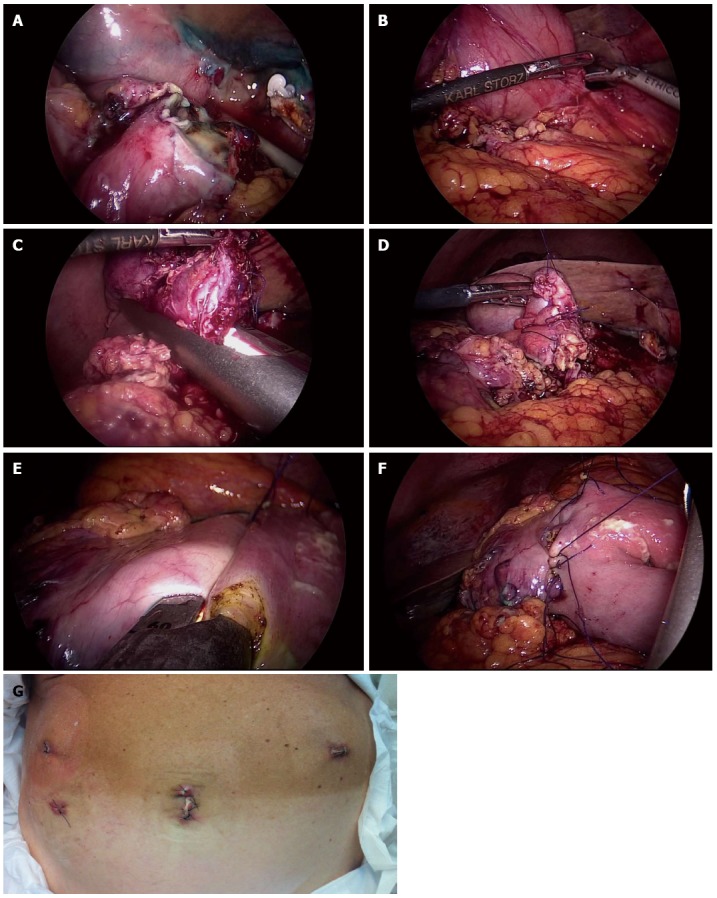
A four-trocar laparoscopic gastroduodenal resection for duodenal perforation. A: “Open-book” duodenal perforation; B: Dissecting the inflamed pylorus from the head of the pancreas; C: Duodenal resection; D: Oversewing the duodenal stump; E: Performing latero-lateral intra-corporeal stapled anastomosis on the posterior stomach wall; F: Closing the enterotomy with interrupted stitches; G: Functional and aesthetic outcome. Provided by personal courtesy of Dr. S. Di Saverio, MD, FACS, FRCS.
Figure 7.

Nine post-operative days after laparoscopic repair of a perforated peptic ulcer: functional and aesthetic outcome. Provided by personal courtesy of Dr. S. Di Saverio, MD, FACS, FRCS.
Throughout the most recent literature, laparoscopy has emerged as a feasible and safe, effective alternative to the traditional open treatment of PPU, if conducted by expert operators on properly selected patients[91]. Notwithstanding, only a few randomized trials were conducted comparing laparoscopic vs open repair of PPU and none of them reported statistically significant differences with regard to post-operative pain or complications[90]. The exception to this is a recent randomized, controlled trial showing laparoscopic repair of PPU to be associated with decreased post-operative pain, hospital length of stay and morbidity[92].
Although laparoscopy for PPU provides potential advantages over open repair in terms of postoperative morbidity and mortality, published data are sparse and further randomized controlled trials with larger sample sizes are needed to arrive at substantiated conclusions.
ABDOMINAL TRAUMA
The old assumption that laparoscopy in abdominal trauma must be absolutely avoided because it is correlated with a high incidence of complications is yesterday’s medicine[93].
Laparoscopic exploration may offer decisive information and thereby prevent delays in providing definitive treatment[94-96]. Laparoscopy must be reserved for hemodynamically-stable patients in selected cases. Early series have demonstrated that laparoscopy can reduce negative laparotomies[96], with a decrease in morbidity and mortality rates related to the additional surgical trauma[95].
Laparoscopy may also be useful in hemodynamically-stable patients with suspected hollow viscus injuries or with diaphragmatic lesions when radiological imaging is doubt. In such cases, non-operative management (NOM) cannot be recommended because of the high risk of suspected lesions[97,98]. In this role, laparoscopy may avoid a negative laparotomy in more than 50% of cases[97,99]. Laparoscopy may also be therapeutic and allow definitive treatment for many types of injuries such as the repair of diaphragmatic or hollow viscus lesions by direct suturing (Figures 8 and 9). Moreover, if detected, a mesenteric laceration, often the cause of intra-abdominal bleeding after trauma, may be treated laparoscopically.
Figure 8.
A large completely perforated jejunum mesenteric border with a 180° laceration of the wall. A: Peritoneal penetration; B: Laparoscopic exploration and individuation of the site of the perforation; C: Wide perforation of the ileus; D: Performing latero-lateral intra-corporeal stapled anastomosis after a limited jejunal resection; E: Functional and aesthetic outcome. Provided by personal courtesy of Dr. S. Di Saverio, MD, FACS, FRCS.
Figure 9.
Laparoscopic repair of intestine perforation following a blunt abdominal trauma. A: Individuation of the site of perforation; B: Defect repair by direct suture; C: Functional and aesthetic outcome. Provided by personal courtesy of Dr. S. Di Saverio, MD, FACS, FRCS.
In cases of NOM failure, only in hemodynamically-stable patients, should a laparoscopic approach be attempted first.
Delayed laparoscopy can also be proposed, both for diagnostic and therapeutic purposes[100,101], in cases of hepatic-related complications such as bleeding, biloma, hepatic abscess or necrosis and the development of abdominal compartment syndrome[102-104].
CONCLUSION
Surgery, as a scientific endeavor, is an everchanging, evolving discipline. Laparoscopy is the direct result of surgical progress. For emergency surgery, laparoscopy has changed the approach to acute cholecystitis and is now recognized as the standard of care in the management of acute appendicitis. In addition, laparoscopy has been utilized for the treatment of many other emergency conditions demonstrating its potential to impact many other diseases traditionally treated with open surgery.
Supported by recent scientific literature, we feel that laparoscopy can no longer be considered only for elective patients. We must leave outdated, negative attitudes regarding emergency laparoscopy and extend this minimally-invasive surgical technique to a wider spectrum of acute abdominal cases.
ACKNOWLEDGMENTS
All intraoperative and postoperative pictures are courtesy of Dr. Salomone Di Saverio, MD, FACS, FRCS, Attending Surgeon, and are taken from his own patient’s database and library of personal surgical procedures. All laparoscopic procedures shown in the images have been performed by Dr. Salomone Di Saverio, MD, FACS, FRCS.
Footnotes
Conflict-of-interest statement: The authors have nothing to disclose.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: May 7, 2015
First decision: July 21, 2015
Article in press: November 19, 2015
P- Reviewer: Desire P S- Editor: Yu J L- Editor: A E- Editor: Ma S
References
- 1.Di Saverio S. Emergency laparoscopy: a new emerging discipline for treating abdominal emergencies attempting to minimize costs and invasiveness and maximize outcomes and patients’ comfort. J Trauma Acute Care Surg. 2014;77:338–350. doi: 10.1097/TA.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 2.Paterson-Brown S. Emergency laparoscopic surgery. Br J Surg. 1993;80:279–283. doi: 10.1002/bjs.1800800305. [DOI] [PubMed] [Google Scholar]
- 3.Di Saverio S, Bassi M, Smerieri N, Masetti M, Ferrara F, Fabbri C, Ansaloni L, Ghersi S, Serenari M, Coccolini F, et al. Diagnosis and treatment of perforated or bleeding peptic ulcers: 2013 WSES position paper. World J Emerg Surg. 2014;9:45. doi: 10.1186/1749-7922-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Navez B, Tassetti V, Scohy JJ, Mutter D, Guiot P, Evrard S, Marescaux J. Laparoscopic management of acute peritonitis. Br J Surg. 1998;85:32–36. doi: 10.1046/j.1365-2168.1998.00531.x. [DOI] [PubMed] [Google Scholar]
- 5.Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993-2008. J Surg Res. 2012;175:185–190. doi: 10.1016/j.jss.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 6.Larsson PG, Henriksson G, Olsson M, Boris J, Ströberg P, Tronstad SE, Skullman S. Laparoscopy reduces unnecessary appendicectomies and improves diagnosis in fertile women. A randomized study. Surg Endosc. 2001;15:200–202. doi: 10.1007/s004640000255. [DOI] [PubMed] [Google Scholar]
- 7.McBurney C. IV. The Incision Made in the Abdominal Wall in Cases of Appendicitis, with a Description of a New Method of Operating. Ann Surg. 1894;20:38–43. doi: 10.1097/00000658-189407000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Semm K. Endoscopic appendectomy. Endoscopy. 1983;15:59–64. doi: 10.1055/s-2007-1021466. [DOI] [PubMed] [Google Scholar]
- 9.Heinzelmann M, Simmen HP, Cummins AS, Largiadèr F. Is laparoscopic appendectomy the new ‘gold standard’? Arch Surg. 1995;130:782–785. doi: 10.1001/archsurg.1995.01430070104022. [DOI] [PubMed] [Google Scholar]
- 10.Kehagias I, Karamanakos SN, Panagiotopoulos S, Panagopoulos K, Kalfarentzos F. Laparoscopic versus open appendectomy: which way to go? World J Gastroenterol. 2008;14:4909–4914. doi: 10.3748/wjg.14.4909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang MT, Wei PL, Wu CC, Lai IR, Chen RJ, Lee WJ. Needlescopic, laparoscopic, and open appendectomy: a comparative study. Surg Laparosc Endosc Percutan Tech. 2001;11:306–312. doi: 10.1097/00129689-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Ignacio RC, Burke R, Spencer D, Bissell C, Dorsainvil C, Lucha PA. Laparoscopic versus open appendectomy: what is the real difference? Results of a prospective randomized double-blinded trial. Surg Endosc. 2004;18:334–337. doi: 10.1007/s00464-003-8927-x. [DOI] [PubMed] [Google Scholar]
- 13.Lintula H, Kokki H, Vanamo K, Valtonen H, Mattila M, Eskelinen M. The costs and effects of laparoscopic appendectomy in children. Arch Pediatr Adolesc Med. 2004;158:34–37. doi: 10.1001/archpedi.158.1.34. [DOI] [PubMed] [Google Scholar]
- 14.Long KH, Bannon MP, Zietlow SP, Helgeson ER, Harmsen WS, Smith CD, Ilstrup DM, Baerga-Varela Y, Sarr MG. A prospective randomized comparison of laparoscopic appendectomy with open appendectomy: Clinical and economic analyses. Surgery. 2001;129:390–400. doi: 10.1067/msy.2001.114216. [DOI] [PubMed] [Google Scholar]
- 15.Oka T, Kurkchubasche AG, Bussey JG, Wesselhoeft CW, Tracy TF, Luks FI. Open and laparoscopic appendectomy are equally safe and acceptable in children. Surg Endosc. 2004;18:242–245. doi: 10.1007/s00464-003-8140-y. [DOI] [PubMed] [Google Scholar]
- 16.Olmi S, Magnone S, Bertolini A, Croce E. Laparoscopic versus open appendectomy in acute appendicitis: a randomized prospective study. Surg Endosc. 2005;19:1193–1195. doi: 10.1007/s00464-004-2165-8. [DOI] [PubMed] [Google Scholar]
- 17.Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K. Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg. 2012;16:1929–1939. doi: 10.1007/s11605-012-1972-9. [DOI] [PubMed] [Google Scholar]
- 18.Wei B, Qi CL, Chen TF, Zheng ZH, Huang JL, Hu BG, Wei HB. Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg Endosc. 2011;25:1199–1208. doi: 10.1007/s00464-010-1344-z. [DOI] [PubMed] [Google Scholar]
- 19.Harrell AG, Lincourt AE, Novitsky YW, Rosen MJ, Kuwada TS, Kercher KW, Sing RF, Heniford BT. Advantages of laparoscopic appendectomy in the elderly. Am Surg. 2006;72:474–480. [PubMed] [Google Scholar]
- 20.McCahill LE, Pellegrini CA, Wiggins T, Helton WS. A clinical outcome and cost analysis of laparoscopic versus open appendectomy. Am J Surg. 1996;171:533–537. doi: 10.1016/s0002-9610(96)00022-0. [DOI] [PubMed] [Google Scholar]
- 21.Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2010;(10):CD001546. doi: 10.1002/14651858.CD001546.pub3. [DOI] [PubMed] [Google Scholar]
- 22.Bennett J, Boddy A, Rhodes M. Choice of approach for appendicectomy: a meta-analysis of open versus laparoscopic appendicectomy. Surg Laparosc Endosc Percutan Tech. 2007;17:245–255. doi: 10.1097/SLE.0b013e318058a117. [DOI] [PubMed] [Google Scholar]
- 23.Di Saverio S, Mandrioli M, Sibilio A, Smerieri N, Lombardi R, Catena F, Ansaloni L, Tugnoli G, Masetti M, Jovine E. A cost-effective technique for laparoscopic appendectomy: outcomes and costs of a case-control prospective single-operator study of 112 unselected consecutive cases of complicated acute appendicitis. J Am Coll Surg. 2014;218:e51–e65. doi: 10.1016/j.jamcollsurg.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Pelosi MA, Pelosi MA. Laparoscopic appendectomy using a single umbilical puncture (minilaparoscopy) J Reprod Med. 1992;37:588–594. [PubMed] [Google Scholar]
- 25.Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A. 1999;9:361–364. doi: 10.1089/lap.1999.9.361. [DOI] [PubMed] [Google Scholar]
- 26.Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278–1287. doi: 10.1016/S0140-6736(15)00275-5. [DOI] [PubMed] [Google Scholar]
- 27.Hua J, Gong J, Xu B, Yang T, Song Z. Single-incision versus conventional laparoscopic appendectomy: a meta-analysis of randomized controlled trials. J Gastrointest Surg. 2014;18:426–436. doi: 10.1007/s11605-013-2328-9. [DOI] [PubMed] [Google Scholar]
- 28.Markar SR, Karthikesalingam A, Di Franco F, Harris AM. Systematic review and meta-analysis of single-incision versus conventional multiport appendicectomy. Br J Surg. 2013;100:1709–1718. doi: 10.1002/bjs.9296. [DOI] [PubMed] [Google Scholar]
- 29.Chow A, Purkayastha S, Nehme J, Darzi LA, Paraskeva P. Single incision laparoscopic surgery for appendicectomy: a retrospective comparative analysis. Surg Endosc. 2010;24:2567–2574. doi: 10.1007/s00464-010-1004-3. [DOI] [PubMed] [Google Scholar]
- 30.St Peter SD, Adibe OO, Juang D, Sharp SW, Garey CL, Laituri CA, Murphy JP, Andrews WS, Sharp RJ, Snyder CL, et al. Single incision versus standard 3-port laparoscopic appendectomy: a prospective randomized trial. Ann Surg. 2011;254:586–590. doi: 10.1097/SLA.0b013e31823003b5. [DOI] [PubMed] [Google Scholar]
- 31.Park YH, Kang MY, Jeong MS, Choi H, Kim HH. Laparoendoscopic single-site nephrectomy using a homemade single-port device for single-system ectopic ureter in a child: initial case report. J Endourol. 2009;23:833–835. doi: 10.1089/end.2009.0025. [DOI] [PubMed] [Google Scholar]
- 32.Frutos MD, Abrisqueta J, Lujan J, Abellan I, Parrilla P. Randomized prospective study to compare laparoscopic appendectomy versus umbilical single-incision appendectomy. Ann Surg. 2013;257:413–418. doi: 10.1097/SLA.0b013e318278d225. [DOI] [PubMed] [Google Scholar]
- 33.Teoh AY, Chiu PW, Wong TC, Poon MC, Wong SK, Leong HT, Lai PB, Ng EK. A double-blinded randomized controlled trial of laparoendoscopic single-site access versus conventional 3-port appendectomy. Ann Surg. 2012;256:909–914. doi: 10.1097/SLA.0b013e3182765fcf. [DOI] [PubMed] [Google Scholar]
- 34.Garey CL, Laituri CA, Ostlie DJ, Snyder CL, Andrews WS, Holcomb GW, St Peter SD. Single-incision laparoscopic surgery in children: initial single-center experience. J Pediatr Surg. 2011;46:904–907. doi: 10.1016/j.jpedsurg.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 35.Ponsky TA, Diluciano J, Chwals W, Parry R, Boulanger S. Early experience with single-port laparoscopic surgery in children. J Laparoendosc Adv Surg Tech A. 2009;19:551–553. doi: 10.1089/lap.2009.0092. [DOI] [PubMed] [Google Scholar]
- 36.Muensterer OJ, Puga Nougues C, Adibe OO, Amin SR, Georgeson KE, Harmon CM. Appendectomy using single-incision pediatric endosurgery for acute and perforated appendicitis. Surg Endosc. 2010;24:3201–3204. doi: 10.1007/s00464-010-1115-x. [DOI] [PubMed] [Google Scholar]
- 37.Di Saverio S, Coccolini F, Galati M, Smerieri N, Biffl WL, Ansaloni L, Tugnoli G, Velmahos GC, Sartelli M, Bendinelli C, et al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2013 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2013;8:42. doi: 10.1186/1749-7922-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bastug DF, Trammell SW, Boland JP, Mantz EP, Tiley EH. Laparoscopic adhesiolysis for small bowel obstruction. Surg Laparosc Endosc. 1991;1:259–262. [PubMed] [Google Scholar]
- 39.Cirocchi R, Abraha I, Farinella E, Montedori A, Sciannameo F. Laparoscopic versus open surgery in small bowel obstruction. Cochrane Database Syst Rev. 2010;(2):CD007511. doi: 10.1002/14651858.CD007511.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johnson KN, Chapital AB, Harold KL, Merritt MV, Johnson DJ. Laparoscopic management of acute small bowel obstruction: evaluating the need for resection. J Trauma Acute Care Surg. 2012;72:25–30; discussion 30-31; quiz 317. doi: 10.1097/TA.0b013e31823d8365. [DOI] [PubMed] [Google Scholar]
- 41.Suter M, Zermatten P, Halkic N, Martinet O, Bettschart V. Laparoscopic management of mechanical small bowel obstruction: are there predictors of success or failure? Surg Endosc. 2000;14:478–483. doi: 10.1007/s004640000104. [DOI] [PubMed] [Google Scholar]
- 42.Bailey IS, Rhodes M, O’Rourke N, Nathanson L, Fielding G. Laparoscopic management of acute small bowel obstruction. Br J Surg. 1998;85:84–87. doi: 10.1046/j.1365-2168.1998.00535.x. [DOI] [PubMed] [Google Scholar]
- 43.Levard H, Boudet MJ, Msika S, Molkhou JM, Hay JM, Laborde Y, Gillet M, Fingerhut A. Laparoscopic treatment of acute small bowel obstruction: a multicentre retrospective study. ANZ J Surg. 2001;71:641–646. doi: 10.1046/j.0004-8682.2001.02222.x. [DOI] [PubMed] [Google Scholar]
- 44.Grafen FC, Neuhaus V, Schöb O, Turina M. Management of acute small bowel obstruction from intestinal adhesions: indications for laparoscopic surgery in a community teaching hospital. Langenbecks Arch Surg. 2010;395:57–63. doi: 10.1007/s00423-009-0490-z. [DOI] [PubMed] [Google Scholar]
- 45.Andersen JC, Bundgaard L, Elbrønd H, Laurberg S, Walker LR, Støvring J. Danish national guidelines for treatment of diverticular disease. Dan Med J. 2012;59:C4453. [PubMed] [Google Scholar]
- 46.Shahedi K, Fuller G, Bolus R, Cohen E, Vu M, Shah R, Agarwal N, Kaneshiro M, Atia M, Sheen V, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol. 2013;11:1609–1613. doi: 10.1016/j.cgh.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85–109. [PubMed] [Google Scholar]
- 48.Rodkey GV, Welch CE. Changing patterns in the surgical treatment of diverticular disease. Ann Surg. 1984;200:466–478. doi: 10.1097/00000658-198410000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007;357:2057–2066. doi: 10.1056/NEJMcp073228. [DOI] [PubMed] [Google Scholar]
- 50.Salem L, Flum DR. Primary anastomosis or Hartmann’s procedure for patients with diverticular peritonitis? A systematic review. Dis Colon Rectum. 2004;47:1953–1964. doi: 10.1007/s10350-004-0701-1. [DOI] [PubMed] [Google Scholar]
- 51.Gooszen AW, Tollenaar RA, Geelkerken RH, Smeets HJ, Bemelman WA, Van Schaardenburgh P, Gooszen HG. Prospective study of primary anastomosis following sigmoid resection for suspected acute complicated diverticular disease. Br J Surg. 2001;88:693–697. doi: 10.1046/j.1365-2168.2001.01748.x. [DOI] [PubMed] [Google Scholar]
- 52.Schilling MK, Maurer CA, Kollmar O, Büchler MW. Primary vs. secondary anastomosis after sigmoid colon resection for perforated diverticulitis (Hinchey Stage III and IV): a prospective outcome and cost analysis. Dis Colon Rectum. 2001;44:699–703; discussion 703-705. doi: 10.1007/BF02234569. [DOI] [PubMed] [Google Scholar]
- 53.Toro A, Mannino M, Reale G, Cappello G, Di Carlo I. Primary anastomosis vs Hartmann procedure in acute complicated diverticulitis. Evolution over the last twenty years. Chirurgia (Bucur) 2012;107:598–604. [PubMed] [Google Scholar]
- 54.Vermeulen J, Coene PP, Van Hout NM, van der Harst E, Gosselink MP, Mannaerts GH, Weidema WF, Lange JF. Restoration of bowel continuity after surgery for acute perforated diverticulitis: should Hartmann’s procedure be considered a one-stage procedure? Colorectal Dis. 2009;11:619–624. doi: 10.1111/j.1463-1318.2008.01667.x. [DOI] [PubMed] [Google Scholar]
- 55.Zorcolo L, Covotta L, Carlomagno N, Bartolo DC. Safety of primary anastomosis in emergency colo-rectal surgery. Colorectal Dis. 2003;5:262–269. doi: 10.1046/j.1463-1318.2003.00432.x. [DOI] [PubMed] [Google Scholar]
- 56.McDermott FD, Collins D, Heeney A, Winter DC. Minimally invasive and surgical management strategies tailored to the severity of acute diverticulitis. Br J Surg. 2014;101:e90–e99. doi: 10.1002/bjs.9359. [DOI] [PubMed] [Google Scholar]
- 57.Gaertner WB, Kwaan MR, Madoff RD, Willis D, Belzer GE, Rothenberger DA, Melton GB. The evolving role of laparoscopy in colonic diverticular disease: a systematic review. World J Surg. 2013;37:629–638. doi: 10.1007/s00268-012-1872-x. [DOI] [PubMed] [Google Scholar]
- 58.Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy) Surg Laparosc Endosc. 1991;1:144–150. [PubMed] [Google Scholar]
- 59.Andeweg CS, Mulder IM, Felt-Bersma RJ, Verbon A, van der Wilt GJ, van Goor H, Lange JF, Stoker J, Boermeester MA, Bleichrodt RP. Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Dig Surg. 2013;30:278–292. doi: 10.1159/000354035. [DOI] [PubMed] [Google Scholar]
- 60.Glasgow RE, Cho M, Hutter MM, Mulvihill SJ. The spectrum and cost of complicated gallstone disease in California. Arch Surg. 2000;135:1021–1025; discussion 1025-1027. doi: 10.1001/archsurg.135.9.1021. [DOI] [PubMed] [Google Scholar]
- 61.Kimura Y, Takada T, Kawarada Y, Nimura Y, Hirata K, Sekimoto M, Yoshida M, Mayumi T, Wada K, Miura F, et al. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:15–26. doi: 10.1007/s00534-006-1152-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Williamson RC. Acalculous disease of the gall bladder. Gut. 1988;29:860–872. doi: 10.1136/gut.29.6.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Janzon L, Aspelin P, Eriksson S, Hildell J, Trell E, Ostberg H. Ultrasonographic screening for gallstone disease in middle-aged women. Detection rate, symptoms, and biochemical features. Scand J Gastroenterol. 1985;20:706–710. doi: 10.3109/00365528509089199. [DOI] [PubMed] [Google Scholar]
- 64.Jørgensen T. Prevalence of gallstones in a Danish population. Am J Epidemiol. 1987;126:912–921. doi: 10.1093/oxfordjournals.aje.a114728. [DOI] [PubMed] [Google Scholar]
- 65.Muhrbeck O, Ahlberg J. Prevalence of gallstone disease in a Swedish population. Scand J Gastroenterol. 1995;30:1125–1128. doi: 10.3109/00365529509101618. [DOI] [PubMed] [Google Scholar]
- 66.Tazuma S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic) Best Pract Res Clin Gastroenterol. 2006;20:1075–1083. doi: 10.1016/j.bpg.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 67.Halldestam I, Enell EL, Kullman E, Borch K. Development of symptoms and complications in individuals with asymptomatic gallstones. Br J Surg. 2004;91:734–738. doi: 10.1002/bjs.4547. [DOI] [PubMed] [Google Scholar]
- 68.Gurusamy KS, Davidson C, Gluud C, Davidson BR. Early versus delayed laparoscopic cholecystectomy for people with acute cholecystitis. Cochrane Database Syst Rev. 2013;6:CD005440. doi: 10.1002/14651858.CD005440.pub3. [DOI] [PubMed] [Google Scholar]
- 69.Gurusamy K, Samraj K, Gluud C, Wilson E, Davidson BR. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 2010;97:141–150. doi: 10.1002/bjs.6870. [DOI] [PubMed] [Google Scholar]
- 70.Ambe P, Weber SA, Christ H, Wassenberg D. Cholecystectomy for acute cholecystitis. How time-critical are the so called “golden 72 hours”? Or better “golden 24 hours” and “silver 25-72 hour”? A case control study. World J Emerg Surg. 2014;9:60. doi: 10.1186/1749-7922-9-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Peng WK, Sheikh Z, Nixon SJ, Paterson-Brown S. Role of laparoscopic cholecystectomy in the early management of acute gallbladder disease. Br J Surg. 2005;92:586–591. doi: 10.1002/bjs.4831. [DOI] [PubMed] [Google Scholar]
- 72.Lo CM, Liu CL, Fan ST, Lai EC, Wong J. Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. 1998;227:461–467. doi: 10.1097/00000658-199804000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Richardson MC, Bell G, Fullarton GM. Incidence and nature of bile duct injuries following laparoscopic cholecystectomy: an audit of 5913 cases. West of Scotland Laparoscopic Cholecystectomy Audit Group. Br J Surg. 1996;83:1356–1360. doi: 10.1002/bjs.1800831009. [DOI] [PubMed] [Google Scholar]
- 74.Russell JC, Walsh SJ, Mattie AS, Lynch JT. Bile duct injuries, 1989-1993. A statewide experience. Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg. 1996;131:382–388. doi: 10.1001/archsurg.1996.01430160040007. [DOI] [PubMed] [Google Scholar]
- 75.Söderlund C, Frozanpor F, Linder S. Bile duct injuries at laparoscopic cholecystectomy: a single-institution prospective study. Acute cholecystitis indicates an increased risk. World J Surg. 2005;29:987–993. doi: 10.1007/s00268-005-7871-4. [DOI] [PubMed] [Google Scholar]
- 76.Johner A, Raymakers A, Wiseman SM. Cost utility of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Surg Endosc. 2013;27:256–262. doi: 10.1007/s00464-012-2430-1. [DOI] [PubMed] [Google Scholar]
- 77.Zhu B, Zhang Z, Wang Y, Gong K, Lu Y, Zhang N. Comparison of laparoscopic cholecystectomy for acute cholecystitis within and beyond 72 h of symptom onset during emergency admissions. World J Surg. 2012;36:2654–2658. doi: 10.1007/s00268-012-1709-7. [DOI] [PubMed] [Google Scholar]
- 78.Mayumi T, Takada T, Kawarada Y, Nimura Y, Yoshida M, Sekimoto M, Miura F, Wada K, Hirota M, Yamashita Y, et al. Results of the Tokyo Consensus Meeting Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:114–121. doi: 10.1007/s00534-006-1163-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Miura F, Takada T, Strasberg SM, Solomkin JS, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Yoshida M, Mayumi T, et al. TG13 flowchart for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:47–54. doi: 10.1007/s00534-012-0563-1. [DOI] [PubMed] [Google Scholar]
- 80.Takada T, Strasberg SM, Solomkin JS, Pitt HA, Gomi H, Yoshida M, Mayumi T, Miura F, Gouma DJ, Garden OJ, et al. TG13: Updated Tokyo Guidelines for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:1–7. doi: 10.1007/s00534-012-0566-y. [DOI] [PubMed] [Google Scholar]
- 81.Gutt CN, Encke J, Köninger J, Harnoss JC, Weigand K, Kipfmüller K, Schunter O, Götze T, Golling MT, Menges M, et al. Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304) Ann Surg. 2013;258:385–393. doi: 10.1097/SLA.0b013e3182a1599b. [DOI] [PubMed] [Google Scholar]
- 82.Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S. Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg. 2011;254:22–27. doi: 10.1097/SLA.0b013e3182192f89. [DOI] [PubMed] [Google Scholar]
- 83.Lee PC, Lo C, Lai PS, Chang JJ, Huang SJ, Lin MT, Lee PH. Randomized clinical trial of single-incision laparoscopic cholecystectomy versus minilaparoscopic cholecystectomy. Br J Surg. 2010;97:1007–1012. doi: 10.1002/bjs.7087. [DOI] [PubMed] [Google Scholar]
- 84.Blinman T. Incisions do not simply sum. Surg Endosc. 2010;24:1746–1751. doi: 10.1007/s00464-009-0854-z. [DOI] [PubMed] [Google Scholar]
- 85.Coghlan JG, Gilligan D, Humphries H, McKenna D, Dooley C, Sweeney E, Keane C, O’Morain C. Campylobacter pylori and recurrence of duodenal ulcers--a 12-month follow-up study. Lancet. 1987;2:1109–1111. doi: 10.1016/s0140-6736(87)91545-5. [DOI] [PubMed] [Google Scholar]
- 86.Bashinskaya B, Nahed BV, Redjal N, Kahle KT, Walcott BP. Trends in Peptic Ulcer Disease and the Identification of Helicobacter Pylori as a Causative Organism: Population-based Estimates from the US Nationwide Inpatient Sample. J Glob Infect Dis. 2011;3:366–370. doi: 10.4103/0974-777X.91061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gunshefski L, Flancbaum L, Brolin RE, Frankel A. Changing patterns in perforated peptic ulcer disease. Am Surg. 1990;56:270–274. [PubMed] [Google Scholar]
- 88.Mouret P, François Y, Vignal J, Barth X, Lombard-Platet R. Laparoscopic treatment of perforated peptic ulcer. Br J Surg. 1990;77:1006. doi: 10.1002/bjs.1800770916. [DOI] [PubMed] [Google Scholar]
- 89.Nathanson LK, Easter DW, Cuschieri A. Laparoscopic repair/peritoneal toilet of perforated duodenal ulcer. Surg Endosc. 1990;4:232–233. doi: 10.1007/BF00316801. [DOI] [PubMed] [Google Scholar]
- 90.Sanabria A, Villegas MI, Morales Uribe CH. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev. 2013;2:CD004778. doi: 10.1002/14651858.CD004778.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bertleff MJ, Lange JF. Laparoscopic correction of perforated peptic ulcer: first choice? A review of literature. Surg Endosc. 2010;24:1231–1239. doi: 10.1007/s00464-009-0765-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, Tai YP, Li MK. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg. 2002;235:313–319. doi: 10.1097/00000658-200203000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Villavicencio RT, Aucar JA. Analysis of laparoscopy in trauma. J Am Coll Surg. 1999;189:11–20. doi: 10.1016/s1072-7515(99)00052-6. [DOI] [PubMed] [Google Scholar]
- 94.Ortega AE, Tang E, Froes ET, Asensio JA, Katkhouda N, Demetriades D. Laparoscopic evaluation of penetrating thoracoabdominal traumatic injuries. Surg Endosc. 1996;10:19–22. doi: 10.1007/s004649910003. [DOI] [PubMed] [Google Scholar]
- 95.Sosa JL, Arrillaga A, Puente I, Sleeman D, Ginzburg E, Martin L. Laparoscopy in 121 consecutive patients with abdominal gunshot wounds. J Trauma. 1995;39:501–504; discussion 504-506. doi: 10.1097/00005373-199509000-00017. [DOI] [PubMed] [Google Scholar]
- 96.Sosa JL, Baker M, Puente I, Sims D, Sleeman D, Ginzburg E, Martin L. Negative laparotomy in abdominal gunshot wounds: potential impact of laparoscopy. J Trauma. 1995;38:194–197. doi: 10.1097/00005373-199502000-00007. [DOI] [PubMed] [Google Scholar]
- 97.Leppäniemi A, Haapiainen R. Diagnostic laparoscopy in abdominal stab wounds: a prospective, randomized study. J Trauma. 2003;55:636–645. doi: 10.1097/01.TA.0000063000.05274.A4. [DOI] [PubMed] [Google Scholar]
- 98.Sauerland S, Agresta F, Bergamaschi R, Borzellino G, Budzynski A, Champault G, Fingerhut A, Isla A, Johansson M, Lundorff P, et al. Laparoscopy for abdominal emergencies: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc. 2006;20:14–29. doi: 10.1007/s00464-005-0564-0. [DOI] [PubMed] [Google Scholar]
- 99.Chol YB, Lim KS. Therapeutic laparoscopy for abdominal trauma. Surg Endosc. 2003;17:421–427. doi: 10.1007/s00464-002-8808-8. [DOI] [PubMed] [Google Scholar]
- 100.Letoublon C, Chen Y, Arvieux C, Voirin D, Morra I, Broux C, Risse O. Delayed celiotomy or laparoscopy as part of the nonoperative management of blunt hepatic trauma. World J Surg. 2008;32:1189–1193. doi: 10.1007/s00268-007-9439-y. [DOI] [PubMed] [Google Scholar]
- 101.Marzano E, Rosso E, Oussoultzoglou E, Collange O, Bachellier P, Pessaux P. Laparoscopic treatment of biliary peritonitis following nonoperative management of blunt liver trauma. World J Emerg Surg. 2010;5:26. doi: 10.1186/1749-7922-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Chen RJ, Fang JF, Lin BC, Hsu YB, Kao JL, Kao YC, Chen MF. Selective application of laparoscopy and fibrin glue in the failure of nonoperative management of blunt hepatic trauma. J Trauma. 1998;44:691–695. doi: 10.1097/00005373-199804000-00024. [DOI] [PubMed] [Google Scholar]
- 103.Kozar RA, Moore JB, Niles SE, Holcomb JB, Moore EE, Cothren CC, Hartwell E, Moore FA. Complications of nonoperative management of high-grade blunt hepatic injuries. J Trauma. 2005;59:1066–1071. doi: 10.1097/01.ta.0000188937.75879.ab. [DOI] [PubMed] [Google Scholar]
- 104.Kozar RA, Moore FA, Cothren CC, Moore EE, Sena M, Bulger EM, Miller CC, Eastridge B, Acheson E, Brundage SI, et al. Risk factors for hepatic morbidity following nonoperative management: multicenter study. Arch Surg. 2006;141:451–458; discussion 458-459. doi: 10.1001/archsurg.141.5.451. [DOI] [PubMed] [Google Scholar]


