Abstract
Brucellosis is a multisystem disease with various clinical symptoms. Neurobrucellosis is a rare but serious manifestation of brucellosis. A 60-year-old man with a previous diagnosis of brucellar spondylitis presented with sudden onset of aphasia and numbness of the right upper extremity. Cerebral angiography showed diffuse narrowing and dilatation on the distal branches of both the anterior cerebral artery (ACA) and the left middle cerebral artery (MCA) which indicated cerebral vasculitis, and the patient's Brucella agglutinin titer was 1:1280. After combined antimicrobial and steroid therapy was started, the patient's condition improved significantly, and he was discharged after 1 month. Antimicrobial therapy was continued for 16 months on an outpatient basis, and the last Brucella agglutinin titer was 1:40. To our knowledge, this is the first case of relapsed neurobrucellosis with vasculitis in Korea to have been treated successfully.
Keywords: Brucellosis, Neurobrucellosis, Cerebral vasculitis
Introduction
Brucellosis is a disease caused by infection with Gram-negative microorganisms of the genus Brucella. Although it has been eradicated in most European and North American countries, it is still an important public health problem throughout the world, in particular in the Mediterranean region including Turkey, the Arabian Peninsula, the Indian subcontinent, Mexico and some parts of Central and South America [1,2]. In Korea, the first brucellosis patients were reported in 2002, and incidence is gradually increasing. There is an occupational risk for farmers, veterinarians, and slaughterhouse workers [3] because humans can become infected by direct contact with an infected animal, the consumption of dairy products, and/or inhalation of infectious particles. It is a systemic, zoonotic disease that can persist for years if not treated, and can cause various complications depending on the organs affected [4]. Nervous system involvement, known as neurobrucellosis, is rare, but an important complication of systemic brucellosis infection [2]. The clinical spectrum of neurobrucellosis is heterogeneous. It can present with diverse symptoms and may imitate many other neurologic diseases. Frequently reported presentations include acute/subacute/chronic meningitis, meningoencephalitis, myelopathy, polyradiculitis, mononeuritis, and vasculitis [5,6]. Here we present an unusual case of relapsed neurobrucellosis with vasculitis.
Case Report
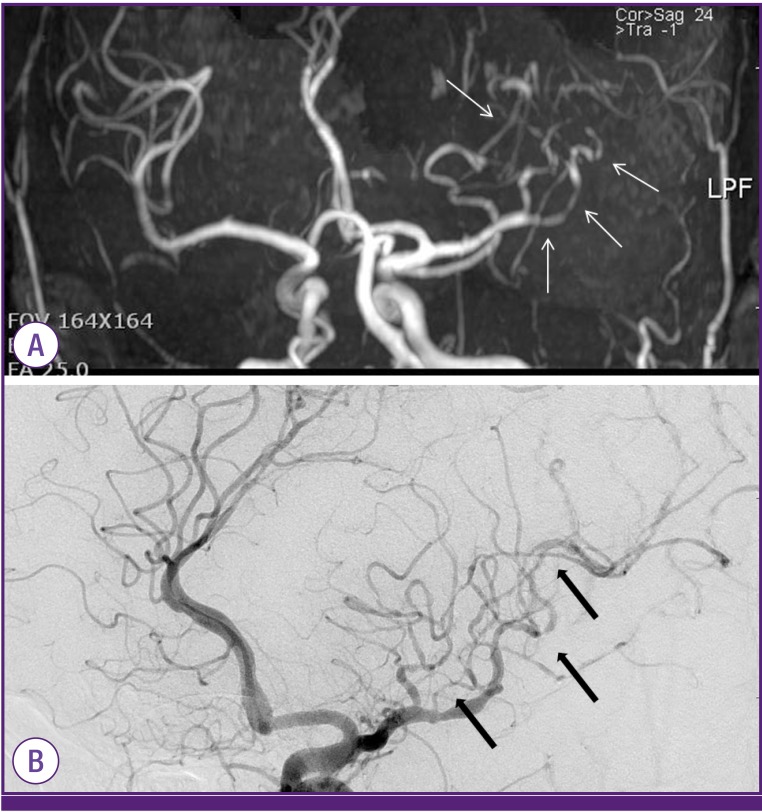
A 60-year-old man was referred to our hospital for sudden onset of aphasia and numbness of the right upper extremity. His medical history revealed that he was a farmer. He had been diagnosed with brucellosis spondylitis and treated for 4 months with doxycycline and rifampin at another hospital 8 months earlier. His initial serum agglutination test (SAT) result for Brucella was 1:1000, and the titer decreased to 1:40 after treatment. After the management of spondylitis, he stopped working as a farmer. On arrival at the hospital, he was alert, oriented, and afebrile. A systemic examination was unremarkable. A neurologic examination revealed ataxia and dysarthria. Magnetic resonance imaging (MRI) and cerebral angiography revealed diffuse narrowing and dilatation on the distal branches of both the anterior cerebral artery (ACA) and left middle cerebral artery (MCA), which indicated vasculitis (Fig. 1). His SAT was 1:1280. Cerebrospinal fluid (CSF) opening pressure was within normal limits. A CSF study showed his white blood cell count (WBC) was 46/mm3 (96% lymphocytes), and his protein level was 196 mg/dL. PCR for Mycobacterium tuberculosis and CSF cultures for other bacteria were negative. Results of all laboratory analyses, including erythrocyte sedimentation rate, complete blood count, fasting blood sugar, antinuclear antibody, and urine analysis were normal. The results of other tests for infection with human immunodeficiency virus, hepatitis B and C virus, and venereal disease were all negative in serum, and blood cultures for other bacteria were negative. CSF tests for herpes simplex virus and cytomegalovirus were negative. On the basis of clinical history, serological data, and MRI and cerebral angiography findings, vasculitis involvement of neurobrucellosis was diagnosed. Treatment was initiated with rifampicin (600 mg/day PO), doxycycline (100 mg PO, q 12 h), and trimethoprim/sulfamethoxazole (20 mg TMP/kg/day IV divided every 8 h) for 1 month. After discharge, rifampicin, doxycycline, and trimethoprim/sulfamethoxazole (80/400 mg PO, q12 h) were continued for 16 months. Prednisolone (1 mg/kg) was initiated and maintained for 6 months with tapering. The neurologic symptoms improved completely, and SAT decreased gradually to 1:40.
Figure 1. (A) MRI (B) Cerebral angiography. Scans demonstrate occlusion of branches of the left MCA, multiple vascular cutoff signs, vascular contour irregularities, and stenosis (arrows).
MCA, middle cerebral artery.
Discussion
Brucellosis is known to present in four different forms, namely, acute, subacute, chronic, and relapse [2]. Even with the appropriate treatment, the incidence of brucellosis relapse remains high, ranging from 5% to 40% of patients in the largest series reported to date [7,8]. In Korea, Kim et al., reported that the treatment failure rate (26%) and relapse rate (14%) are higher in brucellar spondylitis than in other types of brucellosis [9]. Also, Park et al. reported a case of recurrent brucellar meningoencephalitis in a patient previously diagnosed with brucellar spondylitis [10]. In our case, relapsed neurobrucellosis with vasculitis occurred in a patient who was previously diagnosed with brucellar spondylitis, and he was treated successfully.
Although the rate of brucellosis relapse is high, the time to relapse is not known. Our case, relapsed neurobrucellosis with vasculitis, was diagnosed 4 months after termination of initial treatment for brucellar spondylitis, and recurrent brucellar meningoencephalitis was diagnosed 3 months after termination of initial treatment for brucellar spondylitis [10]. Also, brucellosis-induced prosthetic valve endocarditis was diagnosed 2 months after the termination of treatment for the initial systemic brucellosis [11]. According to these relapsed brucellosis cases, the time to relapse was 2 to 4 months following the termination of initial treatment.
Neurobrucellosis is an important complication of systemic brucellosis infection [2] with a reported incidence rate between 3% and 13% [4]. Neurobrucellosis involves several areas of the central and peripheral nervous systems and may develop at any stage of the disease. The most common presentation is a typical meningitis or meningoencephalitis that has an acute or subacute onset [1,2,4].
Cerebrovascular involvement in neurobrucellosis is explained by two mechanisms. The first mechanism is due to rupture of a mycotic, and the other is an inflammatory process of the vessels, namely arteritis with resultant lacunar infarcts, small hemorrhages, or venous thromboses [6,12,13,14]. Cerebral angiography demonstrated diffuse narrowing and dilatation on the distal branch of both the ACA and the left MCA, multiple vascular cutoff signs, vascular contour irregularities, and stenosis, which is consistent with vasculitis.
Diagnosis of neurobrucellosis is based on: (1) clinical findings consistent with neurobrucellosis; (2) pleocytosis with predominant lymphocytes and elevated protein concentration in CSF; (3) positive results of either blood or bone marrow or CSF culture or positive serologic tests; (4) clinical improvement following antibiotic therapy against brucellosis, and (5) no other alternative diagnosis [6,14]. Our patient met all of the criteria; neurologic symptoms, pleocytosis with predominant lymphocytes and elevated protein level in CSF, positive serologic test (1:1280) and clinical improvement after antibiotic treatment.
There are no specific guidelines for antibiotic regimens or duration of treatment for neurobrucellosis [5]. The duration of treatment varies from 8 weeks to 2 years depending upon the individual. Recent reports recommend a regimen that combines three or four antibiotics for neurobrucellosis [15]. Drugs such as doxycycline, rifampicin, and trimethoprim-sulfamethoxazole have been found to be effective because of their ability to penetrate the central nervous system (CNS) and their synergistic actions [5,13,14]. Tetracycline and streptomycin are good for systemic brucellosis, although their CNS penetration is poor [4,16,17]. Our patient was treated with a combination of doxycycline, rifampicin, and trimethoprim/sulfamethoxazole with steroid therapy for 16 months and thereafter was free of all neurologic symptoms.
The prognosis for neurobrucellosis varies according to clinical presentation. For example, in cases with meningitis, the prognosis is usually good; however, in cases with encephalic or spinal cord involvement, mortality is not negligible and sequelae are more frequent [18]. Fortunately, in this case, neurological sequelae were not observed.
This case is of clinical importance for two reasons. First, to the best of our knowledge, this is the first case of cerebrovascular involvement in neurobrucellosis in relapsed brucellosis to be reported in Korea. Second, it highlights the importance of including relapsed brucellosis in the differential diagnosis when unexplained neurologic or other infectious symptoms develop after initial brucellosis treatment, especially if they occur within 2-4 months following the termination of initial brucellosis treatment.
References
- 1.Young EJ. An overview of human brucellosis. Clin Infect Dis. 1995;21:283–289. quiz 290. doi: 10.1093/clinids/21.2.283. [DOI] [PubMed] [Google Scholar]
- 2.Young EJ. Brucella species. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 7th ed. Philadelphia: Elsevier Churchill Livingstone; 2010. pp. 2921–2925. [Google Scholar]
- 3.Lee CS, Kwon KS, Baek BK, Park SW, Lee HB. A three-year follow-up study of human brucellosis in Korea. Infect Chemother. 2007;39:196–201. [Google Scholar]
- 4.Pappas G, Akritidis N, Bosilkovski M, Tsianos E. Brucellosis. N Engl J Med. 2005;352:2325–2336. doi: 10.1056/NEJMra050570. [DOI] [PubMed] [Google Scholar]
- 5.Bashir R, Al-Kawi MZ, Harder EJ, Jinkins J. Nervous system brucellosis: diagnosis and treatment. Neurology. 1985;35:1576–1581. doi: 10.1212/wnl.35.11.1576. [DOI] [PubMed] [Google Scholar]
- 6.Haji-Abdolbagi M, Rasooli-Nejad M, Jafari S, Hasibi M, Soudbakhsh A. Clinical and laboratory findings in neurobrucellosis: a review of 31 cases. Arch Iran Med. 2008;11:21–25. [PubMed] [Google Scholar]
- 7.Solera J, Martínez-Alfaro E, Espinosa A, Castillejos ML, Geijo P, Rodríguez-Zapata M. Multivariate model for predicting relapse in human brucellosis. J Infect. 1998;36:85–92. doi: 10.1016/s0163-4453(98)93342-4. [DOI] [PubMed] [Google Scholar]
- 8.Buzgan T, Karahocagil MK, Irmak H, Baran AI, Karsen H, Evirgen O, Akdeniz H. Clinical manifestations and complications in 1028 cases of brucellosis: a retrospective evaluation and review of the literature. Int J Infect Dis. 2010;14:e469–e478. doi: 10.1016/j.ijid.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 9.Kim YS, Sill CY, Oh WS, Kwon KT, Lee H, Lee SH, Son JS, Kim SW, Chang HH, Jung SI, Ko KS, Park MY, Peck KR, Song JH. Clinical characteristics of human brucellosis in South Korea. Infect Chemother. 2006;38:334–343. [Google Scholar]
- 10.Park SH, Chon JM, Jang HC, Lee JY, Lee SS, Kim SH. Recurrent brucellar meningoencephalitis. J Korean Neurol Assoc. 2008;2:390–392. [Google Scholar]
- 11.Amirghofran AA, Karimi A, Emaminia A, Sharifkazemi MB, Salaminia S. Brucellosis relapse causing prosthetic valve endocarditis and aortic root infective pseudoaneurysm. Ann Thorac Surg. 2011;92:e77–e79. doi: 10.1016/j.athoracsur.2011.03.144. [DOI] [PubMed] [Google Scholar]
- 12.al Deeb SM, Yaqub BA, Sharif HS, Phadke JG. Neurobrucellosis: clinical characteristics, diagnosis, and outcome. Neurology. 1989;39:498–501. doi: 10.1212/wnl.39.4.498. [DOI] [PubMed] [Google Scholar]
- 13.Hernández MA, Anciones B, Frank A, Barreiro P. Neurobrucellosis and cerebral vasculitis. Neurologia. 1988;3:241–243. [PubMed] [Google Scholar]
- 14.Adaletli I, Albayram S, Gurses B, Ozer H, Yilmaz MH, Gulsen F, Sirikci A. Vasculopathic changes in the cerebral arterial system with neurobrucellosis. AJNR Am J Neuroradiol. 2006;27:384–386. [PMC free article] [PubMed] [Google Scholar]
- 15.McLean DR, Russell N, Khan MY. Neurobrucellosis: clinical and therapeutic features. Clin Infect Dis. 1992;15:582–590. doi: 10.1093/clind/15.4.582. [DOI] [PubMed] [Google Scholar]
- 16.Hernndez Prez MA, Anciones Rodriguez B, Garcia AF, Diez-Tejedor E, Barreiro Tella P. Treatment of nervous system brucellosis with rifampicin and doxycycline. Neurology. 1986;36:1408–1409. doi: 10.1212/wnl.36.10.1408-b. [DOI] [PubMed] [Google Scholar]
- 17.Yetkin AM, Bulut C, Erdinc FS, Oral B, Tulek N. Evaluation of the clinical presentations in neurobrucellosis. Int J Infect Dis. 2006;10:446–452. doi: 10.1016/j.ijid.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 18.Ceran N, Turkoglu R, Erdem I, Inan A, Engin D, Tireli H, Goktas P. Neurobrucellosis: clinical, diagnostic, therapeutic features and outcome. Unusual clinical presentations in an endemic region. Braz J Infect Dis. 2011;15:52–59. [PubMed] [Google Scholar]