Abstract
Aim
The aim of this study is to evaluate differences in terms of the setup errors observed using kV planar image compared to CBCT for oesophageal cancer patients.
Background
Planar kV images are quick to acquire but only allow the observation of bony structures. CBCT allows the evaluation of soft tissues, which includes the oesophagus (and tumour) and OAR, giving a more accurate verification of the positioning.
Materials and Methods
All patients were imaged with both techniques between January 2012 and March 2014 were included in the study (16 patients, 212 kV images and 116 CBCT images). Differences between the setup errors observed on the two images modalities were studied. A correlation study between TNM staging, tumour location and immobilization systems with setup errors was also done. Finally, the calculation of systematic and random errors allowed to determine the CTV–PTV margin.
Results
A significant discrepancy (p < 0.05) between the setup errors observed with kV and CBCT was observed in the lateral direction. No statistical correlation was found between setup errors and tumour location, immobilization system or TNM staging. The CTV–PTV margin was smaller with CBCT in the vertical (0.6 cm vs. 0.9 cm) and longitudinal (0.7 cm vs. 1 cm) directions and smaller with kV for the lateral directions (0.8 cm vs. 0.9 cm).
Conclusions
The chosen modality influences the setup error observed which will influence the correction applied. Allowing a better observation of the volumes of interest, CBCT should be the modality of choice in this pathology. The CTV–PTV margins could be shrunk if CBCT is used.
Keywords: Setup errors, kV, CBCT, Oesophagus carcinoma, CTV–PTV margin
1. Background
The use of ionizing radiation to cause damage in biomolecules that cause the cell death is the basic principle of Radiation Oncology, but if, on one hand, the death of cancer cells is the objective, the radiation therapy, on the other hand, is not precise enough to only damage cancer cells, so healthy tissues are also irradiated, resulting in unwanted side-effects.
The best dose prescription and dose distribution are proposed to achieve the best result, although the dose distribution that is achieved on the treatment planning system is not what happens in reality due to some differences between the planned position (acquired on planning CT scan) and the actual position of the patient on the treatment unit.
Nowadays, dose administration has been improved by the raising of special techniques that are being used more often due to their proven advantages,1 including intensity modulated techniques and arc therapy. Those advantages can only be achieved if there is accuracy in the delivery of this dose; for that reason, quality assurance of the patient position in treatment unit should be part of the treatment procedure2: radiological images are acquired in treatment position and compared with the corresponding planning images. Nowadays, a variety of image techniques are available such as planar MV images, planar kV images, CBCT, in-room systems, etc.3
Since the opening of our new radiotherapy department with three linear accelerators equipped with On-Board Imager® (Varian Medical Systems, Palo Alto, USA) (in addition to EPID for portal MV imaging), it is possible to acquire planar kV and CBCT images of the patient at the treatment position.
There are several differences between both techniques: with CBCT, it becomes possible to observe soft tissues4, 5, 6, 7, 8, 9 (including the oesophagus, the tumour and the OAR). The kV images are quicker to acquire and with lower exposure to the patient but they have low contrast for soft tissues,8, 9, 10, 11, 12, 13 the objective of this study is to evaluate if there are significant differences in terms of setup errors observed between the two techniques in this particular tumour location.
The main objective of this study is to verify if there are differences in the setup errors when they are observed with planar kV or CBCT. Regarding that with the CBCT it is possible to visualize soft tissue, including the target and the OAR,4, 5, 6, 7, 8 if significant differences are observed that suggest that the planar kV is not an accurate way to predict the position of the structures of interest.
Although with the kV it is possible to determine setup errors by the matching of bony structures, internal movement of the organs cannot be observed (only with CBCT). So, the eventual differences between the errors observed would result from this internal movement of the organs.
The correlation between the setup errors was observed and the following variables were studied: TNM staging, location of the tumour and immobilization system. In addition, the necessary CTV–PTV margins were evaluated according to the image modality used, regarding the possibility of shrinking this margin, allowing the reduction of the OAR irradiation.14, 15
2. Methods and materials
The patients treated between January 2012 and the end of this research in March 2014 were included if during their treatment they had both verification images being studied: planar kV or CBCT. A total of 16 patients were included resulting in a total of 212 kV images and 116 CBCT analysed. The average age of the patients in the sample is 62 ± 9-years-old, and other descriptives of the sample can be observed in Table 1.
Table 1.
Sample descriptives.
| N | % | |
|---|---|---|
| Sex | ||
| Feminine | 1 | 6.3 |
| Masculine | 15 | 93.8 |
| Number of images analysed | ||
| kV | 212 | 64.6 |
| CBCT | 116 | 35.4 |
| Immobilization | ||
| Thermoplastic mask | 13 | 81.3 |
| Thorax board | 3 | 18.8 |
| Tumour location | ||
| Cervical | 3 | 18.8 |
| Upper thoracic | 10 | 62.5 |
| Mid-thoracic | 3 | 18.8 |
| T staging | ||
| T2 | 2 | 12.5 |
| T3 | 9 | 56.3 |
| T3/4 | 2 | 12.5 |
| T4 | 3 | 18.8 |
| N staging | ||
| Nx | 10 | 62.5 |
| N0 | 2 | 12.5 |
| N1 | 2 | 12.5 |
| N2 | 2 | 12.5 |
| M staging | ||
| M0 | 15 | 93.8 |
| M1 | 1 | 6.3 |
Those patients underwent radiotherapy to the oesophagus using conformal technique or IMRT. The decision regarding the technique used is individual and it is based on the technique that best satisfies the target coverage and OAR constraints.
The standard verification methodology at the department is the online evaluation of orthogonal acquisition of kV images with On Board Imager® (Varian Medical Systems, Palo Alto, USA). In some cases, for clinical (e.g. tumour shrinkage) or technical (e.g. overlap of bony structures) reasons a CBCT would be acquired either after a kV image or as a single modality. After deciding what the best image verification modality would be to each particular case, from that moment on, only one modality would be used since the use of both modalities would be considered an unnecessary extra dose to the patient. The setup error was calculated as the shift between the setup position and the final treatment position (after image analysis).
According to the protocol at the institution, a verification image is acquired on the three first days after which the average observed setup error is calculated and if the average is above 3 mm a shift is applied daily. A weekly imaging verification is performed and if the patient presents a setup error greater than 3 mm an image is acquired the next day and if it persists the average is recalculated and applied from that moment onwards. The number of total images acquired for each patient varied according to the total number of fractions and whether the setup errors were within the tolerance.
All images were analysed by the radiographers and/or radiation oncologists and the correction of the setup error was performed prior to irradiation; these were the data collected.
For the study of the equivalence between kV and CBCT, the data from the observed setup errors were collected. For each patient, it was studied whether the observed error was the same for kV or CBCT and the same procedure was done for the whole sample.
The study of correlation between the setup errors and the staging, immobilization and tumour location was done in order to assess if these specific variables influenced the global result. The immobilization used in the department is different according to the tumour location: cranial lesions use thermoplastic mask (TPM) and caudal lesions use a commercial thorax support.
In order to compare if there would be any benefit using any of the two modalities being studied, a calculation was made of the CTV–PTV margins according to the verification image used, using the van Herk's formula16:
where ∑setup corresponds to the systematic error of the population and σsetup to the random errors of the population, a and b are constant values. van Herk16 proposed that a and b should be 2.5 and 0.7 to allow that 90% of patients receive 95% of the prescribed dose at CTV resulting in 1% TCP loss in the population.
The systematic error of the population corresponds to the standard deviation of the individual means and the random error of the population is the mean of the individual standard deviations.
The aim of this study was to evaluate the differences between planar kV and CBCT imaging with respect to the observation of inter-fraction movements. However, it is important to take into consideration that the movement of the patient during the treatment (intra-fraction) is an aspect that should be considered in the decision making: definition of margins, treatment technique used, verification modality used, etc.
3. Results
Several image methods were developed along the IGRT evolution, but the best modality for each location is still a work in progress, and some tumour locations are extensively studied (e.g. prostate cancer) but in other locations, like oesophagus, the publications are scarce.
3.1. Assessment of differences between planar kV and CBCT
For the assessment of statistical differences between the two image modalities a Related-Samples Wilcoxon Signed Rank test was used to compare paired samples. The selection of this test was based on the fact that there was no evidence of a normal distribution (Shapiro–Wilk test17, 18), so a paired-sample student's t test (0.05 significance level) would not be adequate.
The analysis was done taking into consideration that there is a relationship between the images from the same patient although the kV and CBCT images from the same patient were not taken on the same position. In other words, it was analysed if for each patient the mean setup error (systematic error) observed with kV is different from the one observed with CBCT. The results of this test showed that there are significant differences (p = 0.003) between what is observed in kV and CBCT images in the lateral direction.
Research of verification image differences in other regions or with other image modalities is very common. Those studies show that there are variations in terms of the observed setup error.7, 19, 20, 21
Although the planar kV images are quicker to acquire and to observe apart from offering a lower dose to the patient,8, 11, 12 the advantages of using a 3D verification image are the possibility of observing soft tissues with good contrast, like the tumour or the oesophagus, and providing a more accurate match of the area being treated.5, 10, 19
3.2. Correlation between tumour location and immobilization system with setup errors
It was not possible to establish a relation between location and setup errors due to the reduced number of patients in the sample. A consensus is not found in the literature regarding this subject; some authors did not find a correlation between the location and setup errors22 but there are findings that show a greater movement in the distal regions of the oesophagus.23, 24, 25
Regarding the immobilization system, due to the small number of patients with CBCT that used the thoracic board, no statistical significance was achieved, so it is not possible to observe a correlation between the image and immobilization system.
3.3. Correlation between staging and setup errors
The Spearman test (R) was used to correlate the T and N staging with the size of setup errors observed with both image modalities.
In general, the higher the T staging, the lower the setup errors (R < 0) and higher N staging is correlated with increased setup errors (R > 0) – except for the lateral direction when CBCT is used.
It is important to note that the only case where a moderate correlation can be observed is when the N stating is higher and the longitudinal errors are increased when using CBCT (R = 0.58 and p = 0.018). Most cases showed a poor correlation (−0.4 < R < 0.4) as seen in Table 2.
Table 2.
R value from the Spearman test for the correlation between the setup errors observed with both image modalities and T and N staging for the three orthogonal directions. The only case where a moderated correlation was observed is in bold.
| Stage | Vertical |
Longitudinal |
Lateral |
|||
|---|---|---|---|---|---|---|
| kV | CBCT | kV | CBCT | kV | CBCT | |
| T | −0.17 | −0.30 | −0.14 | −0.05 | −0.18 | −0.24 |
| N | 0.24 | 0.27 | 0.19 | 0.58 | 0.05 | −0.08 |
Because there was only one patient with M1 staging and because the distance metastases are not related with the setup errors at the primary site, no statistical analysis was performed.
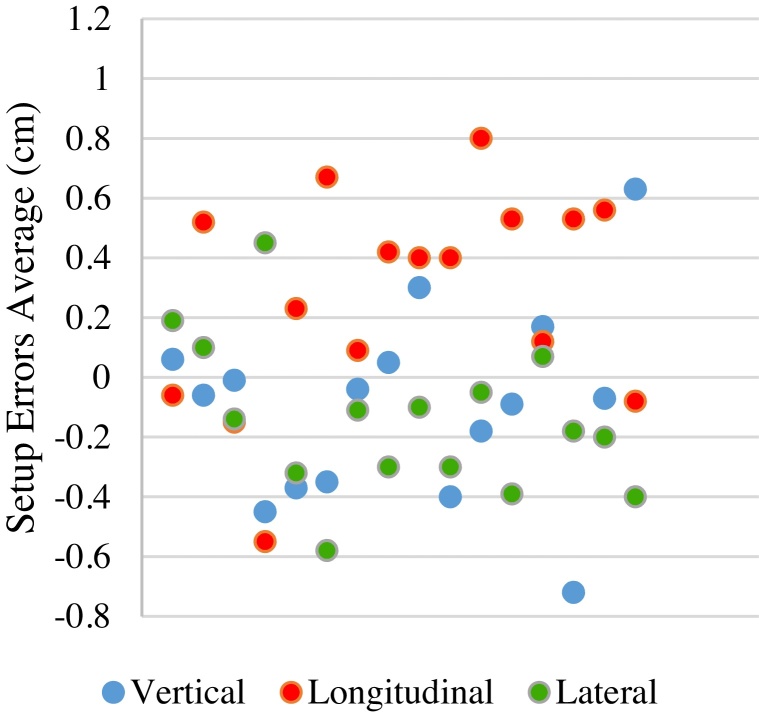
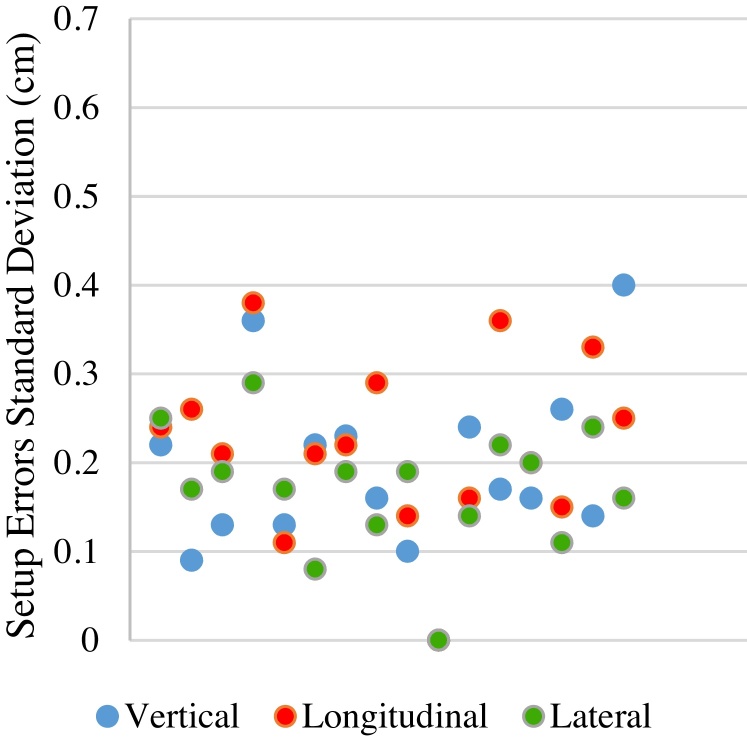
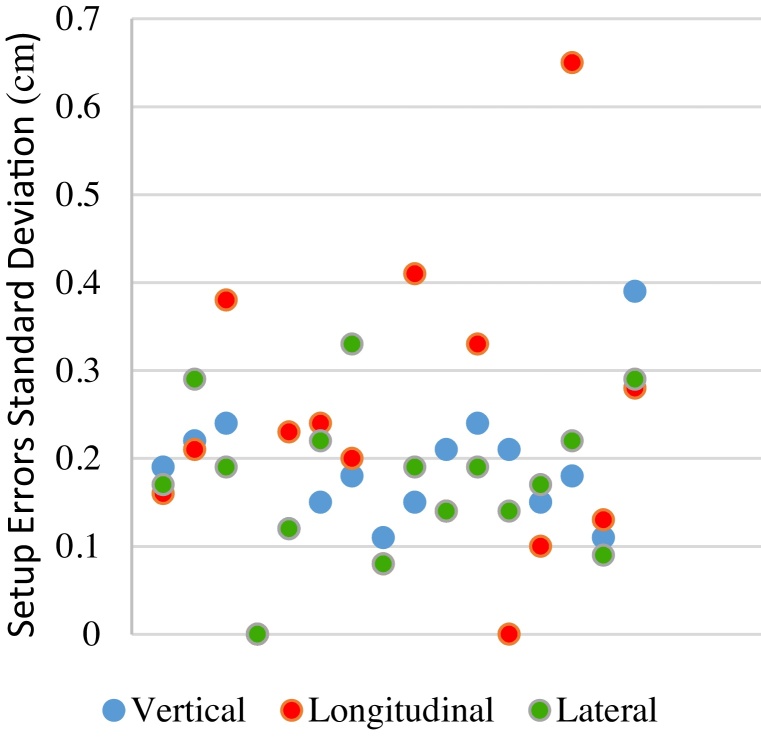
3.4. Random and systematic setup errors
The random and systematic errors were calculated in order to calculate the CTV–PTV margin. Graph 1, Graph 2, Graph 3, Graph 4 show the distribution of the individual random and systematic errors for both image modalities. It is possible to observe more disperse systematic errors (further away from zero) with kV images. The systematic errors cause a higher impact on the tumour control and side effects than the random errors, since they cause a higher risk of sub-irradiation of parts of the target volume and over-irradiation of the surrounding healthy tissues.26
Graph 1.
Individual systematic errors distribution observed with planar kV image.
Graph 2.
Individual systematic errors distribution observed with CBCT.
Graph 3.
Individual random errors distribution observed with planar kV image.
Graph 4.
Individual random errors distribution observed with CBCT.
3.5. CTV–PTV margin according to image modality
From the systematic and random errors the CTV–PTV margin can be calculated using the van Herk's formula.16 It was possible to calculate the adequate margin that should be applied to keep the 1% of TCP loss in the population. The margin was calculated in each direction and for each image modality as seen in Table 3.
Table 3.
CTV–PTV margin for each direction and verification image modality.
| Image modality | Direction (cm) |
||
|---|---|---|---|
| Vertical | Longitudinal | Lateral | |
| kV | 0.9 | 1.1 | 0.8 |
| CBCT | 0.6 | 0.7 | 0.9 |
With the kV images, we observe setup errors that lead to a higher CTV–PTV margins in the vertical and longitudinal directions, and the same occurs to CBCT regarding the lateral direction.
It is important to note that the number of patients is reduced to calculate an appropriate margin between CTV and PTV; however, the objective was to calculate the difference between the two modalities.
A reduction of margins in RT would allow a reduction of the quantity and dose at the OAR, resulting in a reduction of side effects, which would allow an increase in the dose prescribed.8, 12, 14, 27, 28
In Table 4, our findings are compared to other authors’ for the same region. The Hawkins et al.20 study compared planar MV images instead of kV images, being our reference for planar images (bony structures). Yamashita et al.,20 Hawkins et al.22 and Yang et al.29 calculated the systematic and random errors and the CTV–PTV margin (Msetup) with CBCT. It can be observed that with the kV images all the aspects are higher with planar images than CBCT, both in our study as in the references.
Table 4.
CTV–PTV margin for oesophageal cancer according to image modality used for the three orthogonal directions.
| Direction | ∑setup (cm) | σsetup (mm) | Msetup (cm) | Author |
|---|---|---|---|---|
| Planar image | ||||
| Vertical | 0.12 | 0.24 | 0.5 | Hawkins et al.a |
| 0.32 | 0.19 | 0.94 | This study | |
| Longitudinal | 0.27 | 0.33 | 0.9 | Hawkins et al.a |
| 0.36 | 0.22 | 1.05 | This study | |
| Lateral | 0.19 | 0.29 | 0.7 | Hawkins et al.a |
| 0.26 | 0.17 | 0.76 | This study | |
| CBCT | ||||
| Vertical | 0.4 | 0.1 | 0.8 | Yamashita et al. |
| 0.14 | 0.20 | 0.5 | Hawkins et al. | |
| 0.2 | 0.16 | 0.61 | Yang et al. | |
| 0.20 | 0.18 | 0.61 | This study | |
| Longitudinal | 0.38 | 0.41 | 1.23 | Yamashita et al. |
| 0.17 | 0.39 | 0.7 | Hawkins et al. | |
| 0.4 | 0.1 | 0.8 | Yang et al. | |
| 0.21 | 0.22 | 0.67 | This study | |
| Lateral | 0.2 | 0 | 5 | Yamashita et al. |
| 0.13 | 0.26 | 0.5 | Hawkins et al. | |
| 0.23 | 0.24 | 0.75 | Yang et al. | |
| 0.31 | 0.18 | 0.89 | This study | |
CTV–PTV margins calculated based on MV portal images.
4. Conclusion
The main conclusion of this study is that the setup errors observed in both image modalities are not the same, which will result in different corrections and consequently in different treatments. This was statistically significant for the lateral direction (p < 0.05).
It is important to note that if the errors observed are different, the better image to access tumours in oesophagus would be CBCT because it is a soft tissue.5, 10, 19 Based on the findings of this study and on the literature, we suggest that CBCT should be integrated in the image verification protocol of the institution.
An additional and positive finding was that with the CBCT the setup errors observed were smaller than with planar kV, resulting in lower necessary CTV–PTV margins. That will mean less irradiation of healthy tissues. This adds reasoning to the use of CBCT as a primary image verification modality for this pathology.
No significant correlations were found between setup errors and tumour location, immobilization system used or staging, possibly due to the small sample. For that reason, a specific tailored study is suggested to determine which modality provides a better accuracy for different locations, immobilization systems and staging.
The limitations of this study then resumes to a small sample. An issue that should be considered is that the implementation of CBCT would require an extra workload to the department, which can be an issue regarding the heavy workload that Radiotherapy departments are nowadays subject to. Studies report the possibility of a protocol with a mix of both imaging techniques for other regions13 that can be studied further for the oesophagus.
If the proposed inclusion of CBCT in the protocol is put into practice, soon we would have a good sample to repeat the study and confirm the results and maybe find correlations that could not be found; this is highly recommended by the authors.
Conflict of interest
None declared.
Financial disclosure
None declared.
References
- 1.Gomez-Millan J., Fernández J.R., Medina Carmona J.A. Current status of IMRT in head and neck cancer. Rep Pract Oncol Radiother. 2013;18:371–375. doi: 10.1016/j.rpor.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cendales R., Torres F., Arbelaez J., Gaitan A., Vasquez J., Bobadilla I. Displacements of fiducial markers in patients with prostate cancer treated with image guided radiotherapy: a single-institution descriptive study. Rep Pract Oncol Radiother. 2015;20:38–42. doi: 10.1016/j.rpor.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perez C.A., Mutic S. Advances and future of Radiation Oncology. Rep Pract Oncol Radiother. 2013;18:329–332. doi: 10.1016/j.rpor.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grainger R., Allison D., Adam A., Dxon A. Churchil Livingstone Publishers; 2001. Diagnostic radiology: a textbook of medical imaging. [Google Scholar]
- 5.Jaffray D., Kupelian P., Djemil T., Macklis R.M. Review of image-guided radiation therapy. Expert Rev Anticancer Ther. 2007;7:89–103. doi: 10.1586/14737140.7.1.89. [DOI] [PubMed] [Google Scholar]
- 6.Sriram P., Syamkumar S.A., Kumar J.S., Prabakar S., Dhanabalan R., Vivekanandan N. Adaptive volumetric modulated arc treatment planning for esophageal cancers using cone beam computed tomography. Phys Med. 2012;28:327–332. doi: 10.1016/j.ejmp.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 7.Borst G.R., Sonke J.J., Betgen A., Remeijer P., van Herk M., Lebesque J.V. Kilo-voltage cone-beam computed tomography setup measurements for lung cancer patients; first clinical results and comparison with electronic portal-imaging device. Int J Radiat Oncol. 2007;68:555–561. doi: 10.1016/j.ijrobp.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 8.Bissonnette J.-P., Purdie T.G., Higgins J.A., Li W., Bezjak A. Cone-beam computed tomographic image guidance for lung cancer radiation therapy. Int J Radiat Oncol. 2009;73:927–934. doi: 10.1016/j.ijrobp.2008.08.059. [DOI] [PubMed] [Google Scholar]
- 9.Snir J.A., Battista J.J., Bauman G., Yartsev S. Evaluation of inter-fraction prostate motion using kilovoltage cone beam computed tomography during radiotherapy. Clin Oncol. 2011;23:625–631. doi: 10.1016/j.clon.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Dandan Z. The use of cone beam computed tomography in image-guided radiotherapy. Radiology. 2012 [open access] [Google Scholar]
- 11.Walter C., Boda-Heggemann J., Wertz H. Phantom and in-vivo measurements of dose exposure by image-guided radiotherapy (IGRT): MV portal images vs. kV portal images vs. cone-beam CT. Radiother Oncol. 2007;85:418–423. doi: 10.1016/j.radonc.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Cohen R.J., Paskalev K., Litwin S., Price R., Feigenberg S.J., Konski A. Original article: esophageal motion during radiotherapy: quantification and margin implications: esophageal motion during radiotherapy. Dis Esophagus. 2010;23:473–479. doi: 10.1111/j.1442-2050.2009.01037.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adamczyk M., Piotrowski T., Adamiak E. Evaluation of combining bony anatomy and soft tissue position correction strategies for IMRT prostate cancer patients. Rep Pract Oncol Radiother. 2012;17:104–109. doi: 10.1016/j.rpor.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yeung A.R., Li J.G., Shi W. Tumor localization using cone-beam CT reduces setup margins in conventionally fractionated radiotherapy for lung tumors. Int J Radiat Oncol. 2009;74:1100–1107. doi: 10.1016/j.ijrobp.2008.09.048. [DOI] [PubMed] [Google Scholar]
- 15.Grills I.S., Hugo G., Kestin L.L. Image-guided radiotherapy via daily online cone-beam CT substantially reduces margin requirements for stereotactic lung radiotherapy. Int J Radiat Oncol. 2008;70:1045–1056. doi: 10.1016/j.ijrobp.2007.07.2352. [DOI] [PubMed] [Google Scholar]
- 16.Van Herk M., Remeijer P., Lebesque J.V. Inclusion of geometric uncertainties in treatment plan evaluation. Int J Radiat Oncol. 2002;52:1407–1422. doi: 10.1016/s0360-3016(01)02805-x. [DOI] [PubMed] [Google Scholar]
- 17.Razali N., Wah Y. Power comparisons of Shapiro–Wilk, Kolmogorov–Smirnov, Lilliefors and Anderson–Darling tests. J Stat Model Anal. 2011;2:21–33. [Google Scholar]
- 18.Piotrowski T., Rodrigues G., Bajon T., Yartsev S. Method for data analysis in different institutions: example of image guidance of prostate cancer patients. Phys Med. 2014;30:249–251. doi: 10.1016/j.ejmp.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 19.Li H., Zhu X.R., Zhang L. Comparison of 2D radiographic images and 3D cone beam computed tomography for positioning head-and-neck radiotherapy patients. Int J Radiat Oncol Biol Phys. 2008;71:916–925. doi: 10.1016/j.ijrobp.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 20.Hawkins M.A., Aitken A., Hansen V.N., McNair H.A., Tait D.M. Set-up errors in radiotherapy for oesophageal cancers – is electronic portal imaging or conebeam more accurate? Radiother Oncol J Eur Soc Ther Radiol Oncol. 2011;98:249–254. doi: 10.1016/j.radonc.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Topolnjak R., Sonke J.J., Nijkamp J. Breast patient setup error assessment: comparison of electronic portal image devices and cone-beam computed tomography matching results. Int J Radiat Oncol Biol Phys. 2010;78:1235–1243. doi: 10.1016/j.ijrobp.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 22.Yamashita H., Haga A., Hayakawa Y. Patient setup error and day-to-day esophageal motion error analyzed by cone-beam computed tomography in radiation therapy. Acta Oncol. 2010;49:485–490. doi: 10.3109/02841861003652574. [DOI] [PubMed] [Google Scholar]
- 23.Gao X.-S., Qiao X., Wu F. Pathological analysis of clinical target volume margin for radiotherapy in patients with esophageal and gastroesophageal junction carcinoma. Int J Radiat Oncol Biol Phys. 2007;67:389–396. doi: 10.1016/j.ijrobp.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 24.Sasidharan S., Allison R., Jenkins T., Wolfe M., Mota H., Sibata C. Interfraction esophagus motion study in Image Guided Radiation Therapy (IGRT) Int J Radiat Oncol Biol Phys. 2005;63:S91–S92. [Google Scholar]
- 25.Dieleman E.M.T., Senan S., Vincent A., Lagerwaard F.J., Slotman B.J., van Sörnsen de Koste J.R. Four-dimensional computed tomographic analysis of esophageal mobility during normal respiration. Int J Radiat Oncol Biol Phys. 2007;67:775–780. doi: 10.1016/j.ijrobp.2006.09.054. [DOI] [PubMed] [Google Scholar]
- 26.The Royal College of Radiologists, Institute of Physics and Engineering in Medicine & The College of Radiographers . 2008. On target ensuring geometric accuracy in radiotherapy. [Google Scholar]
- 27.Van Dyk J. 2011. Definitions of target volumes and organs at risk, Canada. [Google Scholar]
- 28.Adamczyk M., Piotrowski T., Adamiak E., Malicki J. Dosimetric consequences of prostate-based couch shifts on the precision of dose delivery during simultaneous IMRT irradiation of the prostate, seminal vesicles and pelvic lymph nodes. Phys Med. 2014;30:228–233. doi: 10.1016/j.ejmp.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Yang H. 2014. Setup errors analysis by Cone-Beam CT (CBCT)-based imaged-guided intensity modulated radiotherapy for esophageal cancer.http://www.aapm.org/meetings/2014AM/PRAbs.asp?mid=90&aid=24185 [Google Scholar]